Abstract
Objective.
In the United States, adult cannabis use has increased over time, but less information is available about U.S. time trends in cannabis use disorder, including among veterans, an important population subgroup, or whether such trends differ by age (<35 years, 35–64 years, ≥ 65 years), sex or race/ethnicity.
Methods.
Veterans Health Administration (VHA) electronic health records from 2005–2019 (n’s: 4,403,027 to 5,797,240) were used to identify the percent of VHA patients seen in the U.S. each year with a cannabis use disorder diagnosis (ICD-9-CM, 1/1/2005–9/30/2015; ICD-10-CM, 10/1/2015–12/31/2019). Trends in cannabis use disorder diagnoses were examined by age, and by race/ethnicity and sex within age groups. Given the transition in ICD coding, differences in trends were tested within two periods: 2005–2014 (ICD-9-CM) and 2016–2019 (ICD-10-CM).
Results.
In 2005, among VHA patients age <35, 35–64 and ≥ 65, 1.70%, 1.59%, and 0.03% were diagnosed with cannabis use disorder; by 2019, this had increased to 4.84%, 2.86% and 0.74%, respectively. Although males had consistently higher prevalence of cannabis use disorder than females, between 2016–2019, prevalence increased more in female than male patients <35 years. Black patients had consistently higher prevalence of cannabis use disorder than other race/ethnic groups, and increases were greater in Black than White patients among those <35 years in both periods.
Conclusions.
Since 2005, diagnoses of cannabis use disorder have increased substantially in VHA patients, as they have in the general population and other patient populations. Possible explanations warranting investigation include decreasing perception of risk, changing laws, increasing cannabis potency, stressors related to growing socioeconomic inequality, and use of cannabis to self-treat pain. The public and professionals should be educated about the increases in cannabis use disorder in general in the U.S., including among patients treated at the VHA.
INTRODUCTION
Cannabis use disorder is characterized by problematic patterns of cannabis use leading to clinically significant distress or impairment, accompanied by symptoms such as tolerance, withdrawal, continued use despite mental or physical problems, and neglect of other activities in order to use (1). Individuals with cannabis use disorder are likely to have considerable impairment in social and role/emotional functioning (2, 3). A recent meta-analysis showed that 22% of individuals with past-year cannabis use developed cannabis use disorder, and 33% of frequent users (weekly or more often) developed cannabis dependence (4). Despite these risks, Americans increasingly perceive cannabis as harmless (5–7), states are legalizing cannabis for medical and recreational use, cannabis products are becoming more potent (8), and among U.S. adults, rates of cannabis use and frequent use are increasing (5, 9–11).
Given these changes in perceptions, laws, potency, and rates of use, determining whether the prevalence of adult cannabis use disorder has increased over time is of considerable interest. Across three national household surveys conducted in 1991–1992, 2001–2002 and 2012–2013, the prevalence of DSM-IV cannabis use disorder more than doubled, from 1.2% to 2.9% (9, 12, 13). However, in the yearly 2002–2014 National Surveys on Drug Use and Health (NSDUH), despite increases in adult frequent cannabis users, the prevalence of DSM-IV past-year cannabis use disorder remained stable at ~1.5% (5). Further examination of NSDUH data up to 2017 using a proxy DSM-5 diagnosis showed that the prevalence of cannabis use disorder increased 24%, from 2.1% to 2.6%, largely due to increases in DSM-5-defined mild cases (10).
National electronic health record (EHR) patient databases provide additional sources of information on time trends, offering important advantages including data based on clinical interviews, diagnoses that are likely to capture more severe cases especially in need of treatment and services, and very large sample sizes (14), potentially enabling study of change over time conditions that are too rare to study in some population subgroups, e.g., individuals in minority race/ethnic groups aged ≥65 years. EHR studies indicate an increase in the prevalence of ICD-9-CM (15) cannabis use disorder in hospital inpatients between 2002–2011 (16) and between 1998–2014 (17), in inpatients in 27 states between 1997–2014 (18), and in Veterans Health Administration (VHA) patients between 2002–2009 (19). Limitations of these EHR studies include that the most recent year reported was 2014, that three of the studies covered inpatients only (16–18), and that ICD-9-CM was used, which was replaced by ICD-10-CM in 2015. Further, only one study tested for differences between demographic subgroups (13, 16), finding that in the general population, increases were greater in males, Blacks and young adults age 18–29 between 2001–2002 to 2012–2013 (13, 16). More information is needed to identify population subgroups with disparities in risk for cannabis use disorder (20).
The VHA is the nation’s largest integrated healthcare system, with over five million veterans receiving VHA healthcare each year. VHA patients are more likely than the general population to be characterized by low socioeconomic status, and disability and painful medical conditions often incurred or aggravated during military service (21–24). These characteristics all increase the risk for cannabis use disorder (2, 16, 24, 25), making VHA patients an important population group in which to understand trends in the prevalence of cannabis use disorder. The VHA offers extensive evidence-based treatment for substance use disorders (26–28). However, time trends in cannabis use disorder in the VHA have not been examined for over 10 years (19). To inform potentially increasing need for services in the VHA, and to add an additional piece of information on U.S. trends in cannabis use disorders, we analyzed national VHA EHR data to study trends in cannabis use disorder prevalence by age, sex, and race/ethnicity for the years 2005–2019, a period spanning a major change in the U.S. cannabis landscape, and also the transition from ICD-9-CM to ICD-10-CM.
METHODS
Sample
We analyzed VA EHR data from 1/1/2005 to 12/31/2019. Data were obtained through the VA Corporate Data Warehouse (CDW), a data repository for all documented care provided at a VA facility or paid for by the VA, including patient demographics and diagnostic codes. The study was approved by Institutional Review Boards at the VA Puget Sound, New York Harbor Healthcare Systems, and New York State Psychiatric Institute.
We identified all veterans who received outpatient VA care across the U.S. (at least one primary care, emergency department, or mental health clinic encounter) in a given year for each year from 2005 to 2019 (range of n’s per year: 4,403,027 to 5,797,240). From among these patients, we created 15 yearly data sets, one for each year from 2005 to 2019. Patients were excluded if in a given year, they received hospice/palliative care (range, n=7,774 to 80,440) or resided outside the 50 U.S. states or Washington DC (range, n=53,270 to 66,221).
Measures
The primary study outcome was an ICD diagnosis of cannabis use disorder. Aggregate counts of cannabis use disorder were calculated for each year, 2005 to 2019. The classification system for patient records transitioned from ICD-9-CM to ICD-10-CM during the last quarter of 2015, so two sets of ICD diagnostic codes were used: ICD-9-CM from 1/1/2005 to 9/30/2015, and ICD-10-CM from 10/1/2015 to 12/31/2019 (no period existed when both sets of codes were in use). ICD-9-CM codes included 305.2X (cannabis abuse) and 304.3X (cannabis dependence). ICD-10-CM codes included F12.1 (abuse) and F12.2 (dependence). ICD-9-CM codes for abuse and dependence and ICD-10-CM codes for abuse and dependence were combined because the criteria for these disorders form a unidimensional construct (1). Codes indicating remission (ICD-9-CM 304.33, 305.33; ICD-10-CM F12.11, F12.21) were excluded, i.e., counted as no cannabis use disorder, as was the ICD-10-CM code F12.90, which indicates unspecified, uncomplicated cannabis use.
Demographic characteristics included sex (males, females), age (<35 years, 35–64 years, ≥ 65 years), and race/ethnicity: non-Hispanic White; non-Hispanic Black; Hispanic; non-Hispanic Asian or Pacific Islander; non-Hispanic other (American Indian/Alaskan Native or multiple races) and unknown.
Statistical analysis
The yearly proportions of patients with cannabis use disorder diagnoses was calculated as the number of patients diagnosed with a cannabis use disorder in a particular calendar year divided by the total number of patients in that year. Given highly unbalanced numbers of VHA patients across the age range, with most ≥ 65 years and fewer than 10% below 35 years, all analyses were stratified by age groups (<35 years, 35–64 years, ≥ 65 years). The degree of change (i.e. trends) in cannabis use disorder diagnoses over time was tested using logistic regression models that included study year, age category, year X age category, and sex and race/ethnicity as control variables. The predicted diagnostic prevalences of cannabis use disorder (i.e. adjusted proportions) in each year, the changes in the diagnostic prevalences, the differences in those trends between age groups, and the associated 95% confidence intervals were all obtained from the margins command in Stata version 17 (29) based on the fitted logistic regression model. Given the mid-year transition from ICD-9-CM to ICD-10-CM in 2015, we estimated changes in the predicted diagnostic prevalence of cannabis use disorder for two periods: the earlier 2005–2014 period (complete years when ICD-9-CM was used) and the more recent 2016–2019 period (complete years when ICD-10-CM was used). To further test for differential changes in cannabis use disorder diagnoses over time by sex and race/ethnicity groups, similar logistic regression models were run separately within each of the three age groups that included interaction terms with sex or race/ethnicity (respectively) and controlled for continuous age. Because the data represent a census (not a sample) of all VHA patients who received outpatient VA care each year, no additional statistical control was made for the fact that patients can appear in the data across multiple years. Relatedly, confidence intervals are provided but are based on standard statistical methods assuming sampling distributions; census data do not necessarily warrant uncertainty estimates of this type.
RESULTS
E-Table 1 shows patient demographic characteristics in 2005 and 2019. Most were male (77.0%−98.2%), although female representation increased considerably by 2019 (e.g., 19.8% in those <35 years). While White patients were in the majority (59.0%−88.8%), by 2019, minority representation had increased in all age groups. For example, in patients younger than 35 years, 13.3% were Hispanic, and among patients age 35–64, 25.7% were Black.
Overall trends by age group
Figure 1 shows overall cannabis use disorder diagnoses for each year, 2005–2019 by age group generated from the logistic regression model that controlled for sex and race/ethnicity; Table 1 shows model-predicted diagnostic prevalences in 2005, 2014, 2016 and 2019. In 2005, cannabis use disorder was diagnosed at similar rates in patients <35 years (1.70%) and 35–64 years (1.59%) and at a much lower rate in patients age ≥ 65 (.03%). By 2014, cannabis use disorder diagnoses increased in all groups (to 4.55%, 2.94% and .54% among those <35, 35–64 and ≥ 65 years), with significantly greater increases in those <35 years than in other age groups. In 2016, the first full year after transition to ICD-10-CM, cannabis use disorder diagnoses dropped slightly, and then subsequently resumed increases, reaching 4.84%, 2.86% and 0.74% among those age <35, 35–64 and ≥ 65 years by 2019. Significantly greater increases occurred between 2016–2019 in patients <35 years compared to patients ≥ 65 years.
Figure 1.
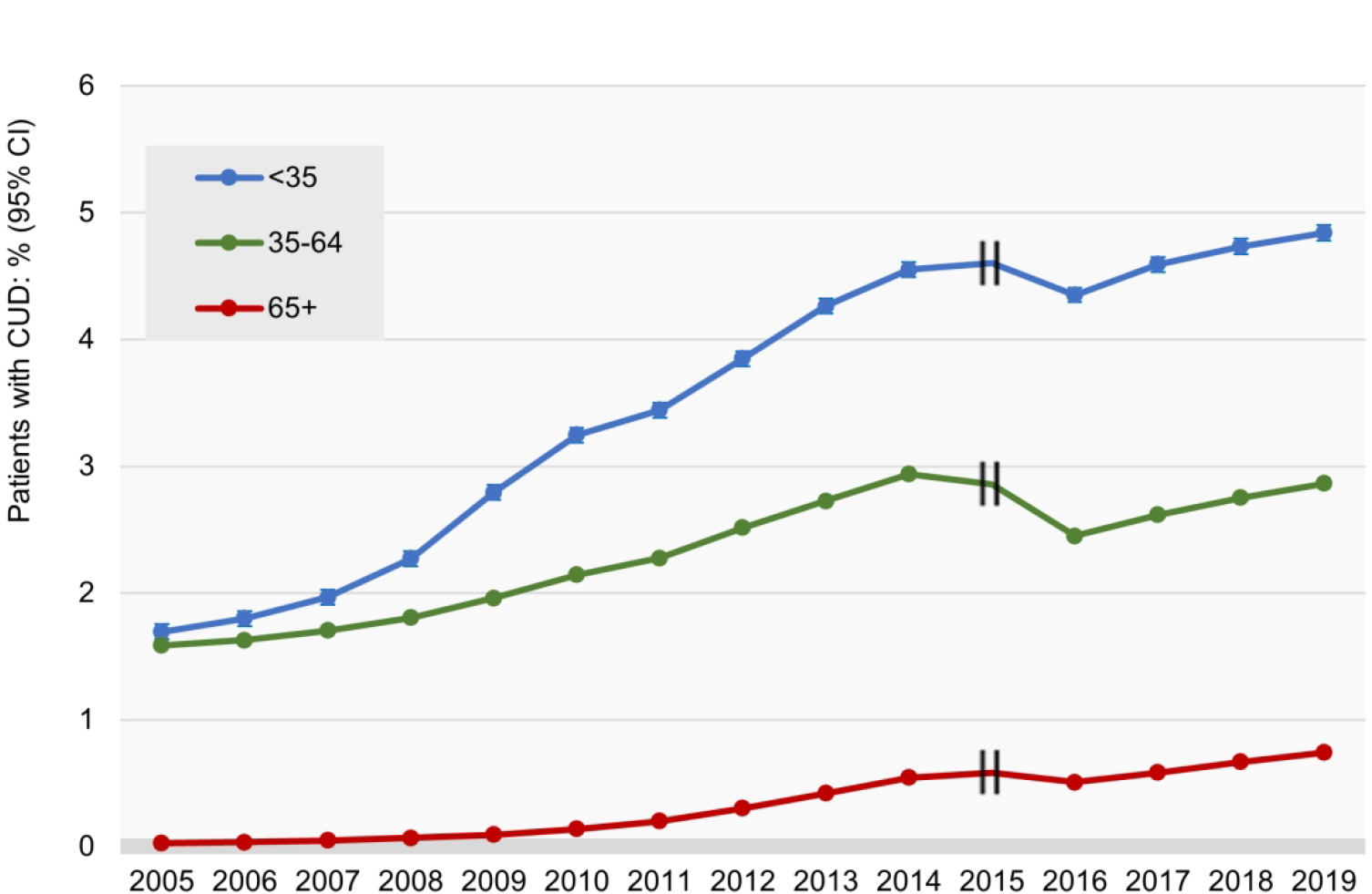
VHA Patients Diagnosed with Cannabis Use Disorder, by age group: 1/1/2005–9/30/2015, ICD-9-CM; 10/1/2015–12/31/2019, ICD-10-CM*
∥ - 2015 data omitted due to ICD-9 to ICD-10 transition on 10/1/2015
* Predicted yearly diagnostic prevalences from a logistic regression model that controlled for sex and race/ethnicity. Confidence intervals are very small due to the large sample sizes
Table 1.
Change in the Predicted Diagnostic Prevalence of Cannabis Use Disorder in VHA patients, 2005–2019, by Age Category
| Predicted prevalence of cannabis use disorder, 2005–2014 | Predicted prevalence of cannabis use disorder, 2016–2019 | |||||||
|---|---|---|---|---|---|---|---|---|
| 2005 % (95% CI) | 2014 % (95% CI) | 2005–2014 Change (95% CI) | Difference in age group changes, 20052014 (95% CI) | 2016 % (95% CI) | 2019 % (95% CI) | 2016–2019 Change (95% CI) | Difference in age group changes, 2016–2019 (95% CI) | |
|
| ||||||||
| <35 | 1.70 (1.63, 1.76) | 4.55 (4.49, 4.61) | 2.85 (2.77, 2.94) | Reference group | 4.35 (4.29, 4.41) | 4.84 (4.78, 4.90) | 0.49 (0.40, 0.57) | Reference group |
| 35–64 | 1.59 (1.57, 1.61) | 2.94 (2.92, 2.96) | 1.35 (1.32, 1.38) | −1.50 (−1.59, −1.41) | 2.45 (2.43, 2.47) | 2.86 (2.84, 2.89) | 0.41 (0.38, 0.44) | −0.07 (−0.16, 0.02) |
| ≥ 65 | 0.03 (0.03, 0.03) | 0.54 (0.54, 0.55) | 0.52 (0.51, 0.52) | −2.34 (−2.42, −2.25) | 0.51 (0.50, 0.52) | 0.74 (0.73, 0.75) | 0.24 (0.22, 0.25) | −0.25 (−0.34, −0.16) |
CI = Confidence Interval Adjusted for sex and race/ethnicity
Patients ages 35–64 and ≥65 increased significantly less than patients <35 (the reference group), as shown by negative difference in differences and confidence intervals that did not include 0.0.
Trends by sex
Across age groups, males were more likely to be diagnosed with cannabis use disorder than females. From 2005–2019 and within both time periods, cannabis use disorder diagnoses increased in males and in females. (Table 2; e-Figures 1A–1C).
Table 2.
Change in the Predicted Diagnostic Prevalence of Cannabis Use Disorder in VHA patients, 2005–2019, by Sex and Age Category
| Predicted prevalence of cannabis use disorder, 2005–2014 | Predicted prevalence of cannabis use disorder, 2016–2019 | |||||||
|---|---|---|---|---|---|---|---|---|
| 2005 % (95% CI) | 2014 % (95% CI) | 2005 to 2014 Change (95% CI) | Difference in gender changes, 2005–2014 (95% CI) | 2016 % (95% CI) | 2019 % (95% CI) | 2016 to 2019 Change (95% CI) | Difference in gender changes, 2016–2019 (95% CI) | |
|
| ||||||||
| <35 | ||||||||
| Women | 0.60 (0.53, 0.67) | 2.11 (2.02, 2.21) | 1.51 (1.40, 1.63) | Reference Group | 2.21 (2.12, 2.30) | 2.83 (2.73, 2.93) | 0.62 (0.49, 0.76) | Reference Group |
| Men | 1.85 (1.78, 1.92) | 4.71 (4.64, 4.77) | 2.86 (2.76, 2.96) | 1.35 (1.20, 1.50) | 4.46 (4.40, 4.52) | 4.89 (4.82, 4.96) | 0.43 (0.34, 0.52) | −0.19 (−0.36, −0.03) |
|
| ||||||||
| 35–64 | ||||||||
| Women | 0.88 (0.83, 0.93) | 1.55 (1.51, 1.60) | 0.67 (0.61, 0.74) | Reference Group | 1.32 (1.28, 1.36) | 1.61 (1.57, 1.65) | 0.29 (0.24, 0.35) | Reference Group |
| Men | 1.75 (1.73, 1.77) | 3.23 (3.20, 3.25) | 1.47 (1.44, 1.51) | 0.80 (0.73, 0.87) | 2.65 (2.62, 2.67) | 3.03 (3.00, 3.05) | 0.38 (0.35, 0.41) | 0.09 (0.03, 0.15) |
|
|
||||||||
| ≥65 | ||||||||
| Women | 0.02 (0.00, 0.03) | 0.17 (0.14, 0.20) | 0.16 (0.12, 0.19) | Reference Group | 0.20 (0.18, 0.23) | 0.34 (0.31, 0.37) | 0.13 (0.09, 0.17) | Reference Group |
| Men | 0.04 (0.03, 0.04) | 0.44 (0.44, 0.45) | 0.40 (0.40, 0.41) | 0.25 (0.21, 0.28) | 0.45 (0.44, 0.46) | 0.77 (0.76, 0.78) | 0.32 (0.31, 0.34) | 0.19 (0.15, 0.23) |
CI = Confidence Interval
Models include year, sex, year X sex, race/ethnicity, continuous age
In patients age 18–34 (e-Figure 1A), ICD-9-CM cannabis use disorder diagnoses increased between 2005–2014 from 1.85% to 4.71% in males and 0.60% to 2.11% in females. The increase was significantly greater in males than in females. By 2019, ICD-10-CM cannabis use disorder was diagnosed in 4.89% of males and 2.83% of females. Between 2016–2019, the increase was significantly greater in females than in males.
Among patients age 35–64 (e-Figure 1B), ICD-9-CM cannabis use disorder diagnoses increased between 2005–2014 from 1.75% to 3.23% in males and from 0.88% to 1.55% in females. In patients ≥ 65 (e-Figure 1C), ICD-9-CM cannabis use disorder diagnoses increased from 0.04% to 0.44% in males and 0.02% to 0.17% in females. By 2019, ICD-10-CM cannabis use disorder diagnoses had reached 3.03% in males and 1.61% in females age 35–64, and 0.77% in males and 0.34% in females age ≥ 65. During both time periods, the increase in cannabis use disorder diagnoses was greater in males than females among patients age 35–64 and ≥ 65.
Trends by race/ethnicity
Across time and within both time periods, cannabis use disorder diagnoses increased in all race/ethnic groups. Across race/ethnic groups, Black patients were consistently more likely to be diagnosed with cannabis use disorder than others (Table 3; e-Figures 2A–2C).
Table 3.
Estimated Change in the Predicted Diagnostic Prevalence of Cannabis Use Disorder in VHA patients, 2005–2019, by Race/Ethnicity and Age Category
| Predicted prevalence of cannabis use disorder, 2005–2014 | Predicted prevalence of cannabis use disorder, 2016–2019 | |||||||
|---|---|---|---|---|---|---|---|---|
| 2005 % (95% CI) | 2014 % (95% CI) | 2005–2014 Change (95% CI) | Difference in race/ethnic changes, 2005–2014 (95% CI) | 2016 % (95% CI) | 2019 % (95% CI) | 2016–2019 Change (95% CI) | Difference in race/ethnic changes, 2016–2019 (95% CI) | |
|
| ||||||||
| <35 | ||||||||
| White | 1.70 (1.62, 1.77) | 4.05 (3.99, 4.12) | 2.36 (2.26, 2.46) | Reference group | 3.86 (3.80, 3.93) | 4.16 (4.09, 4.23) | 0.30 (0.20, 0.40) | Reference group |
| Black | 2.04 (1.89, 2.19) | 6.35 (6.17, 6.53) | 4.31 (4.08, 4.55) | 1.96 (1.70, 2.21) | 6.01 (5.84, 6.18) | 7.14 (6.95, 7.32) | 1.13 (0.88, 1.38) | 0.83 (0.56, 1.10) |
| Hispanic/Latino | 1.06 (0.90, 1.22) | 3.33 (3.18, 3.48) | 2.27 (2.05, 2.48) | −0.09 (−0.33, 0.15) | 3.35 (3.21, 3.49) | 3.83 (3.68, 3.98) | 0.48 (0.27, 0.68) | 0.18 (−0.05, 0.41) |
| Other/Multiple | 1.54 (1.25, 1.83) | 3.32 (3.10, 3.55) | 1.78 (1.41, 2.15) | −0.57 (−0.96, −0.19) | 3.08 (2.87, 3.29) | 3.51 (3.29, 3.73) | 0.43 (0.13, 0.74) | 0.14 (−0.18, 0.45) |
| Unknown | 0.55 (0.44, 0.67) | 2.13 (1.94, 2.33) | 1.58 (1.35, 1.81) | −0.78 (−1.03, −0.53) | 2.21 (2.02, 2.40) | 2.78 (2.57, 2.98) | 0.57 (0.29, 0.85) | 0.27 (−0.03, 0.56) |
|
| ||||||||
| 35–64 | ||||||||
| White | 1.26 (1.24, 1.28) | 2.73 (2.70, 2.76) | 1.47 (1.44, 1.50) | Reference group | 2.28 (2.26, 2.31) | 2.68 (2.65, 2.71) | 0.40 (0.36, 0.43) | Reference group |
| Black | 2.94 (2.89, 2.99) | 4.32 (4.26, 4.37) | 1.38 (1.31, 1.45) | −0.09 (−0.17, −0.01) | 3.48 (3.43, 3.53) | 3.90 (3.85, 3.95) | 0.42 (0.35, 0.49) | 0.02 (−0.06, 0.10) |
| Hispanic/Latino | 1.43 (1.35, 1.51) | 2.28 (2.20, 2.36) | 0.86 (0.74, 0.97) | −0.61 (−0.73, −0.50) | 1.88 (1.81, 1.95) | 2.14 (2.08, 2.21) | 0.26 (0.17, 0.36) | −0.13 (−0.23, −0.03) |
| Other/Multiple | 1.62 (1.51, 1.72) | 2.53 (2.42, 2.65) | 0.92 (0.76, 1.07) | −0.55 (−0.71, −0.39) | 2.09 (1.99, 2.19) | 2.27 (2.18, 2.37) | 0.18 (0.04, 0.32) | −0.22 (−0.36, −0.07) |
| Unknown | 0.97 (0.89, 1.04) | 1.43 (1.34, 1.51) | 0.46 (0.35, 0.58) | −1.01 (−1.13, −0.89) | 1.14 (1.06, 1.21) | 1.42 (1.34, 1.49) | 0.28 (0.18, 0.38) | −0.12 (−0.23, −0.01) |
|
| ||||||||
| ≥65 | ||||||||
| White | 0.02 (0.02, 0.02) | 0.34 (0.33, 0.35) | 0.32 (0.31, 0.33) | Reference group | 0.35 (0.35, 0.36) | 0.67 (0.66, 0.68) | 0.32 (0.30, 0.33) | Reference group |
| Black | 0.16 (0.14, 0.18) | 1.04 (1.01, 1.07) | 0.88 (0.85, 0.92) | 0.56 (0.53, 0.60) | 1.03 (1.00, 1.06) | 1.52 (1.49, 1.56) | 0.50 (0.45, 0.54) | 0.18 (0.13, 0.23) |
| Hispanic/Latino | 0.05 (0.03, 0.08) | 0.50 (0.46, 0.54) | 0.44 (0.40, 0.49) | 0.13 (0.08, 0.17) | 0.49 (0.45, 0.53) | 0.80 (0.75, 0.85) | 0.31 (0.25, 0.37) | −0.01 (−0.07, 0.06) |
| Other/Multiple | 0.05 (0.03, 0.08) | 0.49 (0.45, 0.54) | 0.44 (0.39, 0.49) | 0.12 (0.07, 0.18) | 0.49 (0.45, 0.54) | 0.76 (0.70, 0.82) | 0.27 (0.19, 0.35) | −0.05 (−0.13, 0.03) |
| Unknown | 0.03 (−0.02, 0.08) | 0.47 (0.34, 0.60) | 0.44 (0.30, 0.58) | 0.12 (−0.02, 0.26) | 0.46 (0.33, 0.59) | 0.66 (0.52, 0.79) | 0.20 (0.01, 0.39) | −0.12 (−0.31, 0.07) |
CI = Confidence Interval
Models include year, race/ethnicity, year X race/ethnicity, sex, continuous age
Among those age 18–34 (Table 3; e-Figure 2A), ICD-9-CM cannabis use disorder diagnoses increased between 2005–2014 from 2.04% to 6.35% in Black patients, from 1.06% to 3.33% in Hispanic patients, from 1.70% to 4.05% in White patients, and from 1.54% to 3.32% in the Mixed/Other group. By 2019, ICD-10-CM cannabis use disorder was diagnosed in 7.14% of Black patients, 3.83% of Hispanic patients, 4.16% of White patients, and 3.51% in the Mixed/Other group. With White patients as the reference group, cannabis use disorder diagnoses increased significantly more in Black patients during both earlier and later time periods.
In those age 35–64 (Table 3; e-Figure 2B) ICD-9-CM cannabis use disorder diagnoses increased between 2005–2014 from 2.94% to 4.32% in Black patients, from 1.43% to 2.28% in Hispanic patients, from 1.26% to 2.73% in White patients, and from 1.62% to 2.53% in the Mixed/Other group. By 2019, ICD-10-CM cannabis use disorder was diagnosed in 3.90% of Black patients, 2.14% of Hispanic patients, 2.68% of White patients, and 2.27% in the Mixed/Other group. Between 2005–2014, compared to White patients, cannabis use disorder diagnoses in all other groups increased significantly less, while between 2016–2019, compared to White patients, increases in Black patients did not differ significantly, but Hispanic patients and the multiple/other group increased significantly less than White patients.
In those age ≥ 65 (Table 3; e-Figure 2C), ICD-9-CM cannabis use disorder diagnoses between 2005–2014 increased from 0.16% to 1.04% in Black patients, from 0.05% to 0.50% in Hispanic patients, from 0.02% to 0.34% in White patients, and from 0.05% to 0.49% in the Mixed/Other group. By 2019, ICD-10-CM cannabis use disorder diagnoses had increased to 1.52% in Black patients, 0.80% in Hispanic patients, 0.67% in White patients, and 0.76% in the Mixed/Other group. Compared to White patients, the increase in cannabis use disorder diagnoses was significantly greater in all other race/ethnic groups between 2005–2014, while only the increase in Black patients was significantly greater between 2016–2019.
DISCUSSION
We examined time trends in diagnoses of cannabis use disorder from 2005 to 2019 among patients treated in the VHA. The years examined represent a period of substantial change in the cannabis landscape in the U.S, and also transition from ICD-9-CM to ICD-10-CM. Cannabis use disorder diagnoses more than doubled overall in the VHA, from 0.85% in 2005 to 1.92% in 2019. Increases were found across age, sex and race/ethnic subgroups of patients. Study findings are consistent with other U.S. studies showing increases in the adult prevalence of cannabis use and cannabis use disorder during the last 20 years, including general population surveys (5, 9, 10, 25) and electronic health record studies (16–19). The present study, which extends findings from an earlier VHA study showing increasing cannabis use disorder diagnoses from 2002–2009 (19), indicates that cannabis use disorder continued to increase. Collectively, these studies indicate increases over time in cannabis use disorder among U.S. adults.
Both cannabis-specific factors and larger societal-level forces could explain the overall increases. One cannabis-specific factor is the increasing perception that cannabis is not a harmful substance (5–7). This perception could lead to more users and more cases of cannabis use disorder among these users, given that 20%−33% of cannabis users develop cannabis use disorder (4). Another cannabis-specific factor is increasing legalization, as suggested by national survey findings on adult cannabis use and cannabis use disorder (30–32). Determining whether state legalization of cannabis for medical or recreational use is selectively associated with increased rates of cannabis use disorder among VHA patients is a complex undertaking that is outside the scope of the present study, but this should be done in the future. Yet another cannabis-specific factor is the increasing Δ9 THC potency of licit and illicit cannabis products (8, 33, 34), since higher potency predicts increased risk for progression from use to cannabis use disorder symptoms (35). Further studies of all these factors are needed, including in VHA patients.
Larger societal-level forces could also help explain the overall increases. Cannabis is used for varying reasons and motives, including to cope with stress, which is strongly associated with cannabis use disorder symptoms (36). The years 2005–2019 were stressful for many Americans, encompassing a major recession and unequally distributed economic recovery. Fears of economic losses, and actual job loss could have increased stress, for which cannabis may have been increasingly used to cope, leading to increased cannabis use disorder prevalence, including among VHA patients, whose socioeconomic level is lower compared to other veterans and to US adults as a whole (23, 37, 38). Studies are needed to investigate these speculative explanations.
Our findings indicated that generally, male VHA patients had higher rates of cannabis use disorder diagnoses than females and also greater increases in cannabis use disorder diagnoses over time (the only exception being patients below age 35 during 2016–2019). The general results are consistent with studies in the US general population, one showing that the prevalence of cannabis use increased more in males than females between 2007–2014 (25), and the other showing a wider ‘gender gap’ in adult cannabis use disorder prevalence in 2012–2013 than in 2001–2002 (13). Speculatively, economic factors also help explain these trends. Although females consistently earn less than males (39), sex differences in earnings have decreased over time because male incomes have largely stagnated, while female incomes have increased (40, 41). Increased earnings are clearly advantageous for females, but they could have led to loss of perceived status, self-esteem and increased psychological distress in males, increasing male use of cannabis to cope, and thus greater increases in cannabis use disorder in males than females over time. These factors could have particularly impacted male VHA patients, given their lower socioeconomic level compared to other veterans and other U.S. adults, and the fact that service-related disabilities may have limited their employment opportunities.
The one exception to the greater male increases in cannabis use disorder in VHA patients occurred in the youngest age group (<35 years) in 2016–2019, when females had the greater rate of increase. This is consistent with a meta-analysis of birth cohorts showing that the traditional ‘gender gap’ in cannabis use narrowed considerably in recently-born birth cohorts due to greater increases in females than males (42). This may be due to societal-level changes in norms regarding gender-appropriate behaviors, of which cannabis use is one example. Another reason could be the growing numbers of younger female soldiers exposed to combat in recent wars (43), leading to increased post-discharge stress in younger female veterans with accompanying cannabis use and cannabis use disorder.
Results also indicated that Black patients had higher rates of cannabis use disorder than White patients, and that in patients aged 18–34 and ≥ 65 years, cannabis use disorder diagnoses increased more in Black than White patients (although this was not the case during the earlier period for patients age 35–64, when Whites increased considerably). The Black/White differences in change that were found are consistent with shifts shown in national surveys. For example, while rates of cannabis use were higher in White adolescents in 1991, this difference had reversed and rates had become higher in Black adolescents by 2018 (44, 45). In addition, the prevalence of cannabis use disorder was higher in Black than White adults in 2001–2002, a difference that had widened by 2012–2013 (13). Black individuals face multiple severe stressors, e.g., interpersonal and structural discrimination, and socioeconomic disadvantage that increased between 2005–2019 (46, 47). Perceived racial discrimination predicts subsequent substance use (48–50), and structural racism may have similar associations (51, 52). This could have led to increasingly prevalent cannabis use to cope with stress and consequent cannabis use disorder among Black adults, including VHA patients.
In addition, racial disparities in pain management may have contributed to greater increases in cannabis use disorder among the Black VHA patients. In adults in the general population, pain has been shown to be increasingly associated with CUD over time (53). Service-related injuries are common in VHA patients, and over one-third have chronic pain (54). The VHA has developed a national strategy to deliver safe and effective pain management (55–57), and also emphasizes racial equality in healthcare (58). Nevertheless, during the 2005–2019 period of changing cannabis norms and laws, racial disparities in VHA pain management could have led some Black patients to increasingly self-treat pain with cannabis, leading to higher rates of cannabis use disorder within this group. The only studies known to us with information by race/ethnic group on authorized medical cannabis use or informal self-treatment did not show race/ethnic differences (59, 60). However, both studies are now quite old. Considerable attention has recently been devoted to the importance of identifying and addressing racial disparities in medical care and potential consequences of such disparities. Studies are needed to fill the gaps in knowledge about race/ethnic differences in medical use of cannabis, especially given the increases in rates of cannabis use and cannabis use disorder in Black adults found in this study and others.
We know of no substantive explanation for the 2015–2016 drop in cannabis use disorder diagnoses in the VHA across age, sex and race/ethnic groups. This drop did not occur in the general population (61). However, it coincided with the VHA transition from ICD-9-CM to ICD-10-CM, which presented many challenges for EHR-based health research (17). Studies of the effects of the transition in rates of medical conditions have been inconsistent (62, 63). Studies specifically addressing alcohol (64), opioid (65) and cannabis use disorders (66) were conducted among hospital (63–66) and emergency department (ED) patients. Results showed increases rather than decreases in prevalence after the ICD-10-CM transition, attributed to use of the greater number of relevant categories available in ICD-10-CM. However, these studies addressed patients in acute care, not those seen on an ongoing outpatient basis in a large integrated healthcare system, the situation for most VHA patients. In a subset of VHA patients, the ICD-10-CM transition had little effect on 2016 diagnoses of medical conditions, but was followed by decreases in alcohol, drug and tobacco diagnoses (63), with no explanation offered.
Seeking to explain the decrease, we considered provider behaviors. VHA medical providers must add ICD codes to the EHR for new conditions, and actively remove codes for resolved/remitted conditions. For cannabis use disorder, the definition of remission may be unclear and its occurrence difficult to assess. Thus, during the years that ICD-9-CM was used, active removal of cannabis use disorder diagnostic codes may not have seemed warranted, leaving a diagnosis entered at an earlier time automatically carried forward year-to-year. However, after the ICD-10-CM transition, all ICD-9-CM codes were removed, requiring providers to re-enter codes for current conditions into the EHR. If current cannabis use disorder symptoms were not obvious, no code for ICD-10-CM cannabis use disorder would have been entered, resulting in an apparent drop in cannabis use disorder diagnoses. Subsequently, after the VHA completed the transition to ICD-10-CM in 2016, new or clearly continuing cannabis use disorder cases would be entered by providers. As our findings demonstrate, the four-year ICD-10-CM period was characterized by steady increases in cannabis use disorder diagnoses across age, sex and race/ethnic groups, indicating that once the ICD-10-CM transition was completed, cannabis use disorder diagnoses in VHA patients continued to increase.
Several study limitations are noted. VHA patients are not representative of all veterans or all adults. The ICD diagnoses we analyzed were not based on research interviews, but rather, provider diagnoses. Providers are most likely to be aware of and diagnose severe disorder (14), so mild cases of cannabis use disorder that might have been detected with research interviews could have been missed. While directly interviewing several million patients a year over the time period we covered is not feasible, the use of provider diagnoses in the EHR provides an opportunity to examine change over time in a large population. Our results should be interpreted as potentially representing increases over time in moderate-to-severe cases of cannabis use disorder (i.e., those most in need of care), but not necessarily increases in mild cases. Another source of potential surveillance bias is the possibility that patients were increasingly treated over time for another condition that was associated with cannabis use disorder, in which case cannabis use disorder diagnoses would have appeared to increase, although the increase would have been artifactual. Additionally, VHA providers could have become increasingly aware of the existence of cannabis use disorder and hence were more likely to diagnose it, leading to artifactual but not actual increases in rates. Alternatively, as public attitudes towards cannabis become more positive, providers may also have changed their views of cannabis, becoming less likely to perceive, diagnose and note cannabis use disorder in the electronic medical record. This would have led to an artifactual attenuation of any observed increase in cannabis use disorder. The present VHA datasets do not enable us to investigate these possibilities, but in support of our findings, we note their consistency with other national studies, including those not relying on data from treated patients (9, 12, 25, 67). Another limitation is that the VHA database does not include a variable for cannabis use, so trends in cannabis use disorder diagnoses within users could not be examined.
However, the study also had notable strengths. These include a large source of data with very large sample sizes across many years, including four years of data after the introduction of ICD-10-CM, permitting examination of trends before and after the nomenclature transition. This permitted examination of trends by age, sex and race/ethnicity. To our knowledge, this is the first large EHR study to examine trends in cannabis use disorder diagnoses since 2016.
In summary, the present study provides important information on increases in cannabis use disorder in VHA patients since 2005. While these trends were found across age, sex and race/ethnic subgroups, the increases were especially pronounced in male and in Black patients. The VHA offers an extensive and robust array of evidence-based substance disorder treatments (26–28), but updated information on the extent of cannabis use disorders in VHA patients has not been available for many years. Many individuals can use cannabis without harms, and cannabis use does not have the same mortality/overdose risk profile as opioids or cocaine (68). However, cannabis use disorder is a diagnosable disorder with multiple risks of its own that is now more likely to occur among cannabis users than is commonly assumed (4). Therefore, information from the present study suggests a growing need for screening and treatment in the VHA for patients with cannabis use disorders. In addition, this study adds to the extant literature indicating increases in the prevalence of cannabis use disorder among U.S. adults over the last two decades. While an earlier household survey suggested that the increases were largely due to growing numbers of mild cases (10), the present study of VHA patients, with its reliance on the more severe cases likely to be known to providers and recorded in the EHR, suggests increases in severe cases as well. Evolving cannabis norms, laws, and products, promoted by the growing, multi-billion-dollar cannabis industry (69), may be exerting an upward pressure on cannabis use disorder rates in VHA patients as well as in the general population, leading to a growing public health problem. Clinicians and the public should be educated about this problem, while policymakers should work towards policies that minimize it. Public and professional awareness of the risks (4), consequences (3), and increasing prevalence of cannabis use disorder would benefit adults in general, and veterans in particular, including those who receive treatment in the VHA.
Supplementary Material
Funding:
This study was funded by NIDA grant R01DA048860 and the New York State Psychiatric Institute. Manuscript preparation was supported by resources from the VA Centers of Excellence in Substance Addiction Treatment and Education.
Footnotes
Conflicts of Interest: Dr. Hasin receives support from Syneos Health for an unrelated project on measurement of opioid addiction in pain patients. Dr. Saxon has received consulting fees from Indivior, travel support from Alkermes, research support from Medicasafe, and royalties from UpToDate.
Contributor Information
Deborah S. Hasin, Columbia University and New York State Psychiatric Institute.
Andrew J. Saxon, VA Puget Sound Health Care System and University of Washington.
Carol Malte, VA Puget Sound Health Care System.
Mark Olfson, Columbia University and New York State Psychiatric Institute.
Katherine M. Keyes, Columbia University.
Jaimie L. Gradus, Boston University.
Magdalena Cerdá, New York University.
Charles C. Maynard, VA Puget Sound Health Care System and University of Washington.
Salomeh Keyhani, San Francisco VA Health System and University of California at San Francisco.
Silvia S. Martins, Columbia University.
David S. Fink, New York State Psychiatric Institute.
Ofir Livne, Columbia University.
Zachary Mannes, Columbia University.
Melanie M. Wall, Columbia University and New York State Psychiatric Institute.
REFERENCES
- 1.Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, et al. Prevalence and Correlates of DSM-5 Cannabis Use Disorder, 2012–2013: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry. 2016;173(6):588–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gutkind S, Fink DS, Shmulewitz D, Stohl M, Hasin D. Psychosocial and health problems associated with alcohol use disorder and cannabis use disorder in U.S. adults. Drug Alcohol Depend. 2021;229(Pt B):109137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leung J, Chan GCK, Hides L, Hall WD. What is the prevalence and risk of cannabis use disorders among people who use cannabis? a systematic review and meta-analysis. Addict Behav 2020;109:106479. [DOI] [PubMed] [Google Scholar]
- 5.Compton WM, Han B, Jones CM, Blanco C, Hughes A. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiatry. 2016;3(10):954–64. [DOI] [PubMed] [Google Scholar]
- 6.Levy NS, Mauro PM, Mauro CM, Segura LE, Martins SS. Joint perceptions of the risk and availability of Cannabis in the United States, 2002–2018. Drug Alcohol Depend. 2021;226:108873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han BH, Funk-White M, Ko R, Al-Rousan T, Palamar JJ. Decreasing perceived risk associated with regular cannabis use among older adults in the United States from 2015 to 2019. J Am Geriatr Soc. 2021;69(9):2591–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ElSohly MA, Chandra S, Radwan M, Majumdar CG, Church JC. A Comprehensive Review of Cannabis Potency in the United States in the Last Decade. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6(6):603–6. [DOI] [PubMed] [Google Scholar]
- 9.Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, et al. Prevalence of Marijuana Use Disorders in the United States Between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;72(12):1235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Compton WM, Han B, Jones CM, Blanco C. Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug Alcohol Depend. 2019;204:107468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration. 2019 NSDUH Detailed Tables [Internet]. 2020. [cited 2021 Oct 27]. Available from: https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables.
- 12.Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291(17):2114–21. [DOI] [PubMed] [Google Scholar]
- 13.Hasin DS, Shmulewitz D, Sarvet AL. Time trends in US cannabis use and cannabis use disorders overall and by sociodemographic subgroups: a narrative review and new findings. Am J Drug Alcohol Abuse. 2019;45(6):623–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Casey JA, Schwartz BS, Stewart WF, Adler NE. Using Electronic Health Records for Population Health Research: A Review of Methods and Applications. Annu Rev Public Health. 2016;37:61–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) [Internet]. 2015. [cited 2021 Nov 12]. Available from: https://www.cdc.gov/nchs/icd/icd9cm.htm.
- 16.Charilaou P, Agnihotri K, Garcia P, Badheka A, Frenia D, Yegneswaran B. Trends of cannabis use disorder in the inpatient: 2002 to 2011. Am J Med. 2017;130(6):678–87 e7. [DOI] [PubMed] [Google Scholar]
- 17.Singh JA. Time-trends in hospitalizations with cannabis use disorder: A 17-year U.S. national study. Subst Abus. 2021:1–7. [DOI] [PubMed] [Google Scholar]
- 18.Shi Y Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend. 2017;173:144–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonn-Miller MO, Harris AH, Trafton JA. Prevalence of cannabis use disorder diagnoses among veterans in 2002, 2008, and 2009. Psychol Serv 2012;9(4):404–16. [DOI] [PubMed] [Google Scholar]
- 20.Mahajan S, Caraballo C, Lu Y, Valero-Elizondo J, Massey D, Annapureddy AR, et al. Trends in Differences in Health Status and Health Care Access and Affordability by Race and Ethnicity in the United States, 1999–2018. JAMA. 2021;326(7):637–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vespa JE. Those Who Served: America’s Veterans From World War II to the War on Terror - American Community Survey Report: United States Census Bureau; 2020. [cited 2021 Nov 29]. Available from: https://www.census.gov/library/publications/2020/demo/acs-43.html. [Google Scholar]
- 22.Wong ES, Wang V, Liu CF, Hebert PL, Maciejewski ML. Do Veterans Health Administration Enrollees Generalize to Other Populations? Med Care Res Rev 2016;73(4):493–507. [DOI] [PubMed] [Google Scholar]
- 23.Meffert BN, Morabito DM, Sawicki DA, Hausman C, Southwick SM, Pietrzak RH, et al. US Veterans Who Do and Do Not Utilize Veterans Affairs Health Care Services: Demographic, Military, Medical, and Psychosocial Characteristics. Prim Care Companion CNS Disord 2019;21(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fink DS, Stohl M, Mannes ZL, Shmulewitz D, Wall MM, Gutkind S, et al. Comparing mental and physical health of U.S. veterans by VA healthcare use: Implications for generalizability of research in the VA electronic health records. Under review. [DOI] [PMC free article] [PubMed]
- 25.Carliner H, Mauro PM, Brown QL, Shmulewitz D, Rahim-Juwel R, Sarvet AL, et al. The widening gender gap in marijuana use prevalence in the U.S. during a period of economic change, 2002–2014. Drug Alcohol Depend. 2017;170:51–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Department of Veteran Affairs. Substance Use 2022. [cited 2022 Mar 19]. Available from: https://www.mentalhealth.va.gov/substance-use/treatment.asp.
- 27.Perry C, Liberto J, Milliken C, Burden J, Hagedorn H, Atkinson T, et al. The management of substance use disorders: Synopsis of the 2021 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline. Ann Intern Med. In press. [DOI] [PubMed] [Google Scholar]
- 28.DeMarce JM, Gnys M, Raffa SD, Kumpula M, Karlin BE. Dissemination of cognitive behavioral therapy for substance use disorders in the Department of Veterans Affairs Health Care System: Description and evaluation of Veteran outcomes. Subst Abus 2021;42(2):168–74. [DOI] [PubMed] [Google Scholar]
- 29.StataCorp. Stata Statistical Software: Relaase 17. College Station, TX: StataCorp LLC; 2021. [Google Scholar]
- 30.Cerda M, Mauro C, Hamilton A, Levy NS, Santaella-Tenorio J, Hasin D, et al. Association Between Recreational Marijuana Legalization in the United States and Changes in Marijuana Use and Cannabis Use Disorder From 2008 to 2016. JAMA Psychiatry. 2020;77(2):165–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hasin DS, Sarvet AL, Cerda M, Keyes KM, Stohl M, Galea S, et al. US Adult Illicit Cannabis Use, Cannabis Use Disorder, and Medical Marijuana Laws: 1991–1992 to 2012–2013. JAMA Psychiatry. 2017;74(6):579–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, et al. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend. 2016;169:26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC. Changes in Cannabis Potency Over the Last 2 Decades (1995–2014): Analysis of Current Data in the United States. Biol Psychiatry. 2016;79(7):613–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spindle TR, Bonn-Miller MO, Vandrey R. Changing landscape of cannabis: novel products, formulations, and methods of administration. Curr Opin Psychol. 2019;30:98–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arterberry BJ, Treloar Padovano H, Foster KT, Zucker RA, Hicks BM. Higher average potency across the United States is associated with progression to first cannabis use disorder symptom. Drug Alcohol Depend. 2019;195:186–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bresin K, Mekawi Y. Do marijuana use motives matter? Meta-analytic associations with marijuana use frequency and problems. Addict Behav. 2019;99:106102. [DOI] [PubMed] [Google Scholar]
- 37.Maynard C, Batten A, Liu CF, Nelson K, Fihn SD. The Burden of Mental Illness Among Veterans: Use of VHA Health Care Services by Those With Service-connected Conditions. Med Care. 2017;55(11):965–9. [DOI] [PubMed] [Google Scholar]
- 38.Maynard C, Nelson K. Compensation for Veterans With Service Connected Disabilities: Current Findings and Future Implications. J Disabil Policy Stud 2020;31(1):57–62. [Google Scholar]
- 39.Barroso A, Brown A. Gender pay gap in U.S. held steady in 2020 [Internet]. Pew Research Center; 2021. [cited 2021 Nov 12]. Available from: https://www.pewresearch.org/fact-tank/2021/05/25/gender-pay-gap-facts/. [Google Scholar]
- 40.Greenstone M, Looney A. Trends. Milken Inst Rev. 2011;13(3):8–16. [Google Scholar]
- 41.Price C, Edwards K. Trends in Income From 1975 to 2018. RAND Corporation. 2020;WR-A516–1. [Google Scholar]
- 42.Chapman C, Slade T, Swift W, Keyes K, Tonks Z, Teesson M. Evidence for Sex Convergence in Prevalence of Cannabis Use: A Systematic Review and Meta-Regression. J Stud Alcohol Drugs. 2017;78(3):344–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Street AE, Vogt D, Dutra L. A new generation of women veterans: stressors faced by women deployed to Iraq and Afghanistan. Clin Psychol Rev. 2009;29(8):685–94. [DOI] [PubMed] [Google Scholar]
- 44.Hamilton AD, Jang JB, Patrick ME, Schulenberg JE, Keyes KM. Age, period and cohort effects in frequent cannabis use among US students: 1991–2018. Addiction. 2019;114(10):1763–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Keyes KM, Wall M, Feng T, Cerda M, Hasin DS. Race/ethnicity and marijuana use in the United States: Diminishing differences in the prevalence of use, 2006–2015. Drug Alcohol Depend. 2017;179:379–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kochhar R, Cilluffo A. How wealth inequality has changed in the U.S. since the Great Recession, by race, ethnicity and income [Internet]. Pew Research Center; 2017. [cited 2021 Nov 12]. Available from: https://www.pewresearch.org/fact-tank/2017/11/01/how-wealth-inequality-has-changed-in-the-u-s-since-the-great-recession-by-race-ethnicity-and-income/. [Google Scholar]
- 47.Moss E, McIntosh K, Edelberg W, Broady K. The Black-white wealth gap left Black households more vulnerable [Internet]. The Brookings Institution; 2020. [cited 2021 Nov 12]. Available from: https://www.brookings.edu/blog/up-front/2020/12/08/the-black-white-wealth-gap-left-black-households-more-vulnerable/. [Google Scholar]
- 48.Gibbons FX, Etcheverry PE, Stock ML, Gerrard M, Weng CY, Kiviniemi M, et al. Exploring the link between racial discrimination and substance use: what mediates? What buffers? J Pers Soc Psychol. 2010;99(5):785–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gerrard M, Stock ML, Roberts ME, Gibbons FX, O’Hara RE, Weng CY, et al. Coping with racial discrimination: the role of substance use. Psychol Addict Behav. 2012;26(3):550–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Borrell LN, Jacobs DR Jr., Williams DR, Pletcher MJ, Houston TK, Kiefe CI. Self-reported racial discrimination and substance use in the Coronary Artery Risk Development in Adults Study. Am J Epidemiol. 2007;166(9):1068–79. [DOI] [PubMed] [Google Scholar]
- 51.Amaro H, Sanchez M, Bautista T, Cox R. Social vulnerabilities for substance use: Stressors, socially toxic environments, and discrimination and racism. Neuropharmacology. 2021;188:108518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Farahmand P, Arshed A, Bradley MV. Systemic Racism and Substance Use Disorders. Psychiatr Ann 2020;50(11):494–8. [Google Scholar]
- 53.Hasin DS, Shmulewitz D, Cerda M, Keyes KM, Olfson M, Sarvet AL, et al. U.S. Adults With Pain, a Group Increasingly Vulnerable to Nonmedical Cannabis Use and Cannabis Use Disorder: 2001–2002 and 2012–2013. Am J Psychiatry. 2020;177(7):611–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bastian LA, Heapy A, Becker WC, Sandbrink F, Atkins D, Kerns RD. Understanding Pain and Pain Treatment for Veterans: Responding to the Federal Pain Research Strategy. Pain Med. 2018;19(suppl_1):S1–S4. [DOI] [PubMed] [Google Scholar]
- 55.U.S. Department of Veterans Affairs. VA Research on Pain Management [Internet]. 2020. [cited 2021 Nov 12]. Available from: https://www.research.va.gov/topics/pain.cfm#intro.
- 56.U.S. Department of Veterans Affairs. Opioid Safety Initiative (OSI) [Internet]. 2017. [cited 2021 Nov 12]. Available from: https://www.va.gov/painmanagement/opioid_safety_initiative_osi.asp.
- 57.Kerns RD, Brandt CA, Peduzzi P. NIH-DoD-VA Pain Management Collaboratory. Pain Med. 2019;20(12):2336–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.U.S. Department of Veterans Affairs. Office of Health Equity [Internet]. 2021. [cited 2021 Nov 12]. Available from: https://www.va.gov/HEALTHEQUITY/index.asp.
- 59.Wall MM, Liu J, Hasin DS, Blanco C, Olfson M. Use of marijuana exclusively for medical purposes. Drug Alcohol Depend. 2019;195:13–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lin LA, Ilgen MA, Jannausch M, Bohnert KM. Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addict Behav 2016;61:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Center for Behavioral Health Statistics and Quality. 2016 National Survey on Drug Use and Health: Detailed Tables Rockville, MD: Substance Abuse and Mental Health Services Administration; 2017. [cited 2021 Dec 2]. Available from: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf. [Google Scholar]
- 62.Hsu MC, Wang CC, Huang LY, Lin CY, Lin FJ, Toh S. Effect of ICD-9-CM to ICD-10-CM coding system transition on identification of common conditions: An interrupted time series analysis. Pharmacoepidemiol Drug Saf 2021;30(12):1653–74. [DOI] [PubMed] [Google Scholar]
- 63.Yoon J, Chow A. Comparing chronic condition rates using ICD-9 and ICD-10 in VA patients FY2014–2016. BMC Health Serv Res. 2017;17(1):572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Heslin KC, Barrett ML. Shifts in Alcohol-Related Diagnoses After the Introduction of International Classification of Diseases, Tenth Revision, Clinical Modification Coding in U.S. Hospitals: Implications for Epidemiologic Research. Alcohol Clin Exp Res. 2018;42(11):2205–13. [DOI] [PubMed] [Google Scholar]
- 65.Heslin KC, Owens PL, Karaca Z, Barrett ML, Moore BJ, Elixhauser A. Trends in Opioid-related Inpatient Stays Shifted After the US Transitioned to ICD-10-CM Diagnosis Coding in 2015. Med Care. 2017;55(11):918–23. [DOI] [PubMed] [Google Scholar]
- 66.Hall KE, Yang H, Goulding D, Contreras E, James KA. Interrupted time series analysis of cannabis coding in Colorado during the ICD-10-CM transition. Inj Prev 2021;27(S1):i66–i70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.O’Neill-Dee C, Spiller HA, Casavant MJ, Kistamgari S, Chounthirath T, Smith GA. Natural psychoactive substance-related exposures reported to United States poison control centers, 2000–2017. Clin Toxicol (Phila). 2019:1–8. [DOI] [PubMed] [Google Scholar]
- 68.National Institute on Drug Abuse. Overdose Death Rates [Internet]. 2021. [cited 2021 Nov 12]. Available from: https://www.drugabuse.gov/drug-topics/trends-statistics/overdose-death-rates.
- 69.D’Souza D. The Future of the Marijuana Industry in America [Internet]. Investopedia; 2021. [cited 2021 Nov 12]. Available from: https://www.investopedia.com/articles/investing/111015/future-marijuana-industry-america.asp. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


