Abstract
Objective:
This study examined the impact of COVID-19 policies reducing barriers to telehealth-delivered buprenorphine for opioid use disorder (OUD) on buprenorphine treatment across different modalities (phone, video, in-person).
Methods:
We conducted a national retrospective cohort study with interrupted time series analyses to examine the impact of policy changes in March 2020 on buprenorphine treatment for OUD in the Veterans Health Administration, during pre-COVID-19 (March 2019 to February 2020) and post-COVID-19 (March 2020 to February 2021) periods. We also examined trends in use of phone, video and in-person visits for buprenorphine treatment and compared patient demographics and buprenorphine retention across the pre- and post-COVID-19 periods.
Results:
The number of patients receiving buprenorphine increased from 13,415 in March 2019 to 15,339 in February 2021. By February 2021, phone visits were used by the most patients (50.2%, 4,456), followed by video (32.4%, 2,870) and in-person (17.4%, 1,544). During the pre-COVID-19 period, patients receiving buprenorphine increased by 103 patients per month (p<0.001). Post-COVID-19 policy changes, there was an immediate increase of 265 patients in the first month and the number continued to increase but by 47 patients each month (p<0.001). Patients receiving buprenorphine post-COVID-19 had similar demographic characteristics to those pre-COVID-19, but percent reaching 90-day retention on buprenorphine decreased from 49.6% to 47.7% (p<0.05) while days on buprenorphine increased from 203.8 to 208.7 (p<0.001).
Conclusions:
The number of patients receiving buprenorphine continued to increase after COVID-19 policy changes, but the delivery shifted to telehealth visits, suggesting reversal of COVID-19 policies must be carefully considered.
Introduction
The COVID-19 pandemic has sparked a rapid, unprecedented expansion of telehealth-delivered care, including delivery of buprenorphine treatment for opioid use disorder (OUD), an effective treatment that can help reduce mortality in this vulnerable patient population (1,2). Key policy changes were issued in March 2020 at the beginning of the pandemic to decrease barriers to telehealth-delivery of buprenorphine treatment in order to sustain treatment for patients with OUD across the US. These key changes included: 1) eliminating the initial in-person visit requirement for telehealth-delivered buprenorphine treatment under the public health emergency exception of the Ryan Haight Online Pharmacy Consumer Protection Act, 2) expanding coverage of telehealth services including to patients at home by the Center for Medicare and Medicaid services and other insurance companies, and 3) guidance from the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Drug Enforcement Administration (DEA) allowing prescribing of buprenorphine treatment through phone visits (rather than requiring video), an important modality given disparities in access to internet and digital technologies (3).
At the same time, further acceleration of overdose mortality since the start of COVID-19 suggests there may either be an increase in treatment need or a decrease in treatment utilization in this population who may be particularly vulnerable to impacts of COVID-19, underscoring the importance of examining trends in buprenorphine treatment since the start of COVID-19 (4). Prior research has examined shifts in delivery of buprenorphine early in the pandemic (5,6). However, studies are needed to examine longer-term patterns across telehealth modalities, including phone and video, and changes in the characteristics of patients who are receiving treatment to inform future policies and inform current debates on reversing the temporary policy changes implemented during COVID-19. It is also imperative to examine these trends within the Veterans Health Administration (VHA) system—VHA is the largest addiction treatment provider in the country and provides a view of treatment across the US, and ensuring access to buprenorphine is a leading VHA priority (7). The objective of this study was to examine effects of COVID-19-related policy changes reducing barriers to telehealth delivery of buprenorphine treatment for patients with OUD across the national VHA. We examined shifts in overall treatment receipt, delivery modalities (video, phone and in-person), treatment retention, and demographic characteristics of patients receiving treatment.
Methods
We examined national VHA data to compare trends in buprenorphine treatment across the 12 months before and after federal-level COVID-19 policy changes were implemented in March 2020. These policy changes decreased barriers to tele-buprenorphine for OUD (3). The pre-COVID-19 period was defined as the 12 months from March 2019 through February 2020, and the post-COVID-19 period was defined as the 12 months from March 2020 through February 2021. Data were obtained from VHA’s Corporate Data Warehouse.
Cohort definition
Monthly rolling cohorts of VHA patients with OUD diagnosis during the two-year study period were examined. Patients in each monthly cohort included VHA patients age 18 or older with at least one VHA outpatient encounter with an OUD diagnosis in the 12 months prior to and including the month of interest.
Outcomes
We examined the monthly number of patients with buprenorphine treatment, defined as patients with days supply of buprenorphine for OUD covering at least one day that month. Because we found a decreasing trend in the monthly number of patients with a diagnosis of OUD during the two-year study period, as a sensitivity analysis, we also examined the proportion of patients each month receiving buprenorphine treatment among those with OUD. A patient was counted in each month that they received treatment during the study period even if they started and stopped treatment multiple times during the study period. In addition to monthly number of patients receiving buprenorphine treatment, as in other studies (5), we also examined two mutually exclusive monthly measures: number of patients continuing buprenorphine treatment, defined as those who received any buprenorphine for OUD in the prior 3 months and the number of patients newly initiating buprenorphine, defined as those with no buprenorphine fills covering any days in the prior 3 months.
Using similar approaches to our prior work (8), we examined visit modalities for buprenorphine treatment (i.e., phone, video or in-person) monthly throughout the study period (see Appendix Table 1 in the online supplement for modality definitions). Visits for buprenorphine treatment were defined as visits with the same provider as the person prescribing buprenorphine treatment for OUD.
For each unique patient who received buprenorphine for OUD in the pre- and post-COVID-19 periods, we collected data on patient demographics (age, sex, race and rural/urban residence), number of treatment visits, otal days supplied of buprenorphine and 90-day retention on buprenorphine (9–11). Number of treatment visits for buprenorphine were totaled for each patient within each pre- and post-COVID-19 period, and total days of buprenorphine supplied for each patient was determined by aggregating total days supply of buprenorphine within each pre- and post-COVID-19 period. 90-day retention was defined as having at least one episode of buprenorphine treatment for at least 90 total days, allowing gaps in treatment of no more than 30 days. Thus, patients who meet the 90-day retention criteria could have gaps in treatment up to 30 days, though must have at least 90 total days of treatment starting from the date of the first fill.
Analysis
Monthly numbers of patients receiving buprenorphine treatment for OUD over the study period were examined using interrupted time series analyses to estimate changes in buprenorphine prescribing following COVID-19-related policy changes implemented in March 2020. This method adjusted for baseline levels and trends to more robustly examine change in treatment after a policy change (12,13) and also accounted for correlation of data over time using the autoregression procedure (13). Patients who received buprenorphine for OUD in the pre- and post-COVID periods were compared on demographic characteristics, buprenorphine retention, and number of treatment visits using generalized estimating equation (GEE) with an indicator for the post-COVID period to account for correlation of patients included in both periods. This study was deemed exempt from review by the VA Ann Arbor Healthcare System Institutional Review Board.
Results
Total number of VHA patients receiving buprenorphine for OUD increased from 13,415 in March 2019 to 15,339 in February 2021 (14%, Figure 1). During this same period, the number of patients receiving any substance use disorder (SUD) treatment in the VHA (not just OUD treatment) decreased from 138,745 to 129,806 (6% decrease). Interrupted time series analysis showed that in the 12-month pre-pandemic period, buprenorphine treatment was increasing at a rate of 103 patients per month (p<0.001 Table 1). In the 12-month period after the start of COVID-19-related policy changes, the number of patients receiving treatment continued to increase, but at a rate of 47 patients per month (p<0.001), which was lower than the pre-pandemic rate of increase (p<0.001). The number of patients continuing buprenorphine increased at a rate of 107 per month (p<.001) during the 12 months prior to the policy changes, and the rate continued to increase at 53 patients per month (p<0.001) after the COVID-19 policy changes, although the rate of increase was lower (p<.001) than the pre-pandemic period. The number of patients newly initiating buprenorphine decreased overall across both periods, but the rate of decrease was not significant and no significant difference in the rates was seen between the pre- vs. the post-COVID-19 period.
Figure 1.
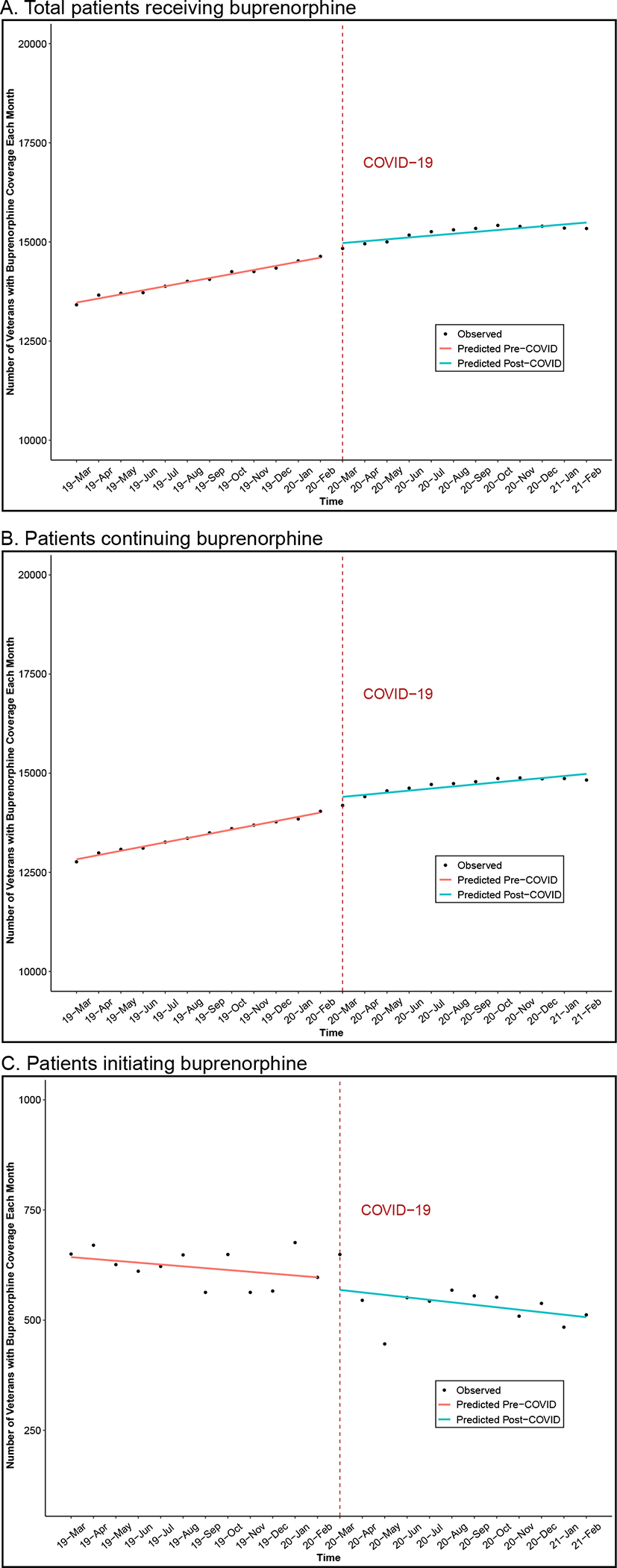
Trends in number of patients in the Veterans Health Administration receiving buprenorphine for opioid use disorder (OUD; March 2019-Feburary 2021)
Table 1.
Interrupted time series analyses examining number of patients receiving buprenorphine for OUD before (3/2019–2/2020) and after (3/2020–2/2021) COVID-19 telehealth policy changes
| Pre-COVID-19 telehealth policy changes | Post-COVID-19 telehealth policy changes | Post- compared to pre-COVID-19 changes | ||||||
|---|---|---|---|---|---|---|---|---|
| Monthly Rate1 | p-value | Immediate change in number of patients | p-value | Monthly Rate1 | p-value | Rate Difference | p-value | |
| All buprenorphine patients | 102.96 | <0.001 | 264.72 | 0.003 | 47.07 | < 0.001 | −55.89 | <0.001 |
| Patients initiating buprenorphine | −4.17 | 0.16 | −24.38 | 0.60 | −5.62 | 0.23 | −1.45 | 0.79 |
| Patients continuing buprenorphine | 107.13 | <0.001 | 289.10 | 0.006 | 52.69 | <0.001 | −54.44 | 0.001 |
Change per month in the number of patients receiving buprenorphine treatment
We also conducted sensitivity analyses examining trends in monthly proportions of patients receiving buprenorphine among those with OUD each month. In the 12-month period after the start of COVID-19-related policy changes, the proportion of patients receiving treatment continued to increase, but this time at a rate not significantly different than the pre-pandemic trend (Appendix, Table 2 in the online supplement). The proportion of patients continuing buprenorphine also increased but was not significantly different than the pre-pandemic trends. For the proportion of patients newly initiating buprenorphine, similar to the primary results, there was no significant difference in the rates post- compared to pre-COVID-19.
Among patients receiving a buprenorphine treatment visit each month, the proportion of telehealth visits (phone and video) increased dramatically from 11.9% (1,025 of 8,589 visits) in March 2019 to 82.6% (7,326 of 8,870 visits) in February 2021 (Figure 2). Of all buprenorphine treatment visits, proportion of phone visits increased and remained the most prevalent modality in February 2021 (50.2%, 4,456 of 8,870 visits), followed by video (32.4%, 2,870) and in-person (17.4%, 1,544). Among 4,720 patients newly initiating buprenorphine in the one-year period after the start of COVID-19, 64.4% (3,039) were phone visits, 40.5% (1,910) video visits, and 20.4% (962) in-person visits. Note that some patients could have received more than one buprenorphine treatment visit and with more than one type of modality. Among 13,462 patients continuing buprenorphine in the one-year period after the start of COVID-19, 86.7% (11,667) received phone visits, 46.7% (6,287) video visits, and 6.0% (807) in-person visits. In the post-COVID period, the proportion of patients receiving video or phone visits did not differ substantially by rural/non-rural residence (Appendix, Table 3 in the online supplement).
Figure 2.
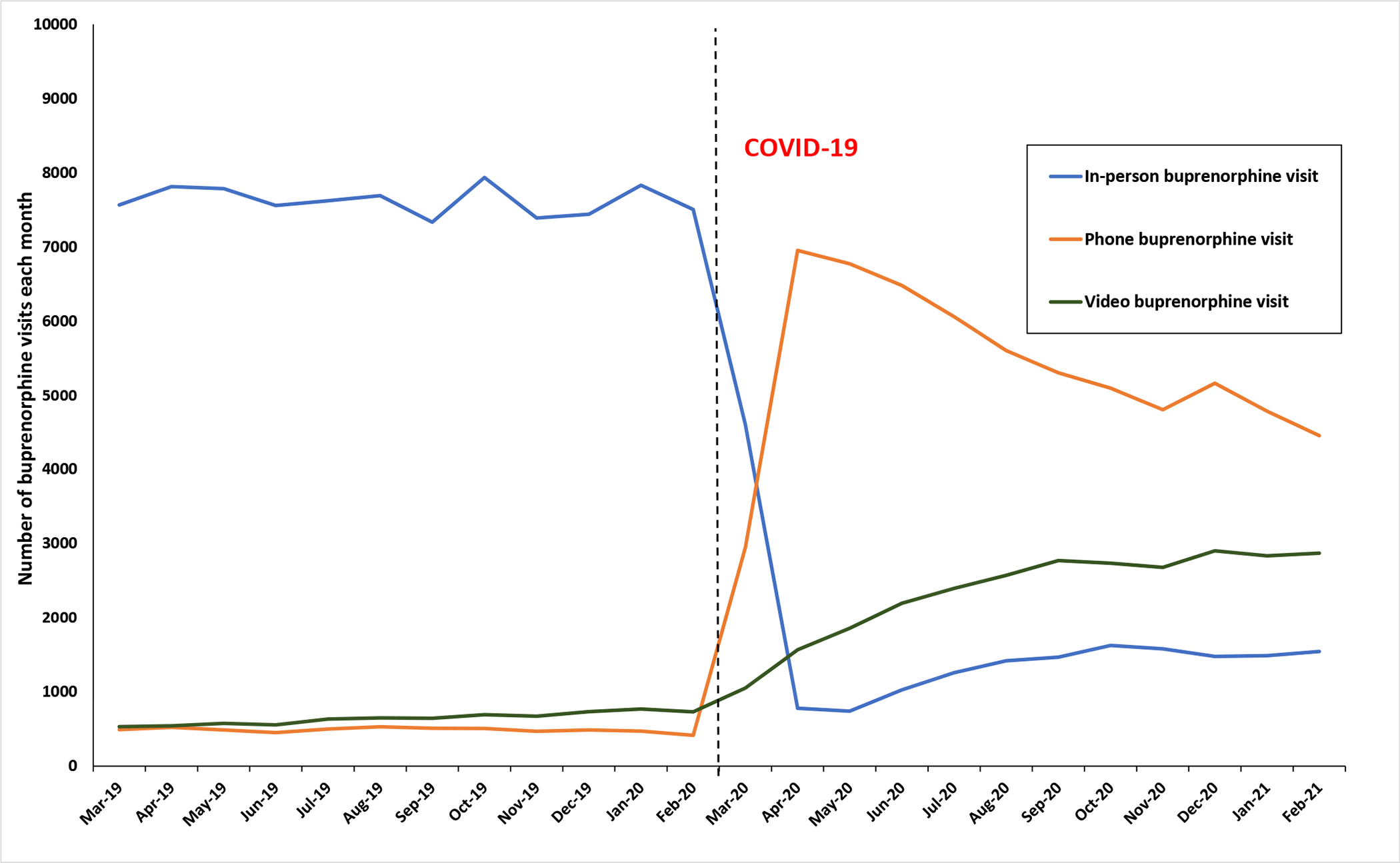
Trends in number of buprenorphine treatment visits for OUD across modalities in the Veterans Health Administration (March 2019-Feburary 2021)
Compared with patients who received buprenorphine for OUD during the one-year post-COVID-19 policy changes, those who received buprenorphine for OUD in the one-year pre-COVID-19 period were significantly more likely to live in urban areas (86% compared to 82%) and less likely other/unknown areas (2% compared to 5% compared, p<0.001), but did not differ significantly in terms of age groups, sex, or race/ethnicity (Table 2). During the pre-COVID-19 period, 49.6% of patients were retained on buprenorphine at least 90 days compared to 47.7% post-COVID-19 (p<0.05). Pre-COVID-19, the average days supplied of buprenorphine treatment was 203.8 compared to 208.7 (p<0.001) and average number of treatment visits was 5.3 (SD 3.3) compared to 5.4 visits (SD 3.2, p=0.07) post-COVID-19.
Table 2.
Comparing patient characteristics and treatment utilization among Veterans receiving buprenorphine for OUD before and after COVID-19 related telehealth policy changes
| Pre-COVID-19 telehealth policy changes (3/2019–2/2020) N = 18,012 | Post-COVID-19 telehealth policy changes (3/2020–2/2021) N = 18,182 | p-value | |||
| Mean | SD | Mean | SD | ||
| Age in years | 49.4 | 13.9 | 49.3 | 13.9 | 0.72 |
| Age groups | % | N | % | N | |
| 18–29 | 3.4 | 615 | 3.2 | 584 | 0.53 |
| 30–44 | 40.8 | 7,347 | 41.4 | 7,523 | |
| 45–64 | 37.7 | 6,788 | 37.5 | 6,819 | |
| 65+ | 18.1 | 3,262 | 17.9 | 3,256 | |
| Female | 7.9 | 1421 | 7.9 | 1436 | 0.98 |
| Race/Ethnicity | |||||
| White, non-Hispanic | 77.7 | 14,003 | 78.0 | 14,182 | 0.64 |
| Black, non-Hispanic | 11.4 | 2,058 | 11.0 | 2,004 | |
| Hispanic | 5.2 | 942 | 5.2 | 952 | |
| Other/unknown | 5.6 | 1,009 | 5.7 | 1,044 | |
| Rurality | |||||
| Urban | 86.0 | 15,483 | 82.4 | 14,989 | <0.001 |
| Rural | 12.0 | 2,162 | 12.2 | 2,213 | |
| Other/Unknown | 2.0 | 367 | 5.4 | 980 | |
| Patients with ≥ 90 day buprenorphine retention | 49.6 | 8,932 | 47.7 | 8,664 | <0.05 |
| Mean | SD | Mean | SD | ||
| Average days on buprenorphine treatment | 203.8 | 156.0 | 208.7 | 113.7 | <0.001 |
| Number of buprenorphine treatment visits | 5.3 | 3.3 | 5.4 | 3.2 | 0.07 |
Discussion
This study in the national VHA found the number of patients receiving buprenorphine for OUD treatment continued to increase following COVID-19-related policy changes to decrease barriers to telehealth, albeit at a slower rate. However, delivery of care changed dramatically during this period; the majority of visits shifted to telehealth, with phone visits outnumbering video visits. These findings suggest that although COVID-19 substantially changed the way in which OUD care is delivered, policy changes that were rapidly implemented in order to decrease barriers to telehealth, allowed delivery of this life-saving treatment to be sustained during the pandemic.
These findings build on prior studies in other patient populations that examined telehealth delivery of buprenorphine in the initial months of the pandemic (5,14,15), and show that buprenorphine treatment continued to be sustained one year after policy changes, primarily through a large-scale transition to phone and video visits. This unprecedented shift allowed clinicians to continue care in a patient population who may be particularly vulnerable to COVID-19-related care disruptions. People with substance use disorders, including OUD, have higher burden of comorbid conditions putting them at higher risk for COVID-19, which may cause greater reduction of in-person healthcare (16,17). People with OUD are also more vulnerable to psychosocial disruptions (e.g. financial challenges, job loss, exacerbation of comorbid mental health disorder) that may affect care utilization (18), which may have contributed to the lower 90-day retention we found in the post-COVID period. Additional studies are needed that specifically compare retention across treatment modalities post-COVID to better disaggregate the effects of COVID-19 from treatment modalities on outcomes. However, it is reassuring to see that overall buprenorphine treatment utilization did not decline, as it did occur for other key healthcare services in the setting of the pandemic across the US (19–21), including other VHA SUD services as found in this study. In patients receiving buprenorphine for OUD, there was a slight increase in the proportion of patients whose residence (i.e., rural/urban) was unknown, but no other changes in patient demographic characteristics were observed (including for race/ethnicity) suggesting that the transition to phone and video telehealth was not associated with major shifts in the demographics of the population receiving buprenorphine (22,23).
Despite the apparent success of maintaining delivery of buprenorphine through telehealth during the pandemic, it remains critical to continue prioritizing increased access to this treatment. These results suggest that the transition to telehealth supported ongoing increases in number of patients who were already in treatment, specifically through increased days of treatment among those receiving buprenorphine. It is possible that making treatment more accessible through telehealth makes it easier for patients who are already in treatment to stay in treatment, which is a crucial consideration in future policy decisions. However, we did not observe any increases in patients initiating buprenorphine treatment. This may indicate that increasing the number of new patients on buprenorphine via both in-person and telehealth visits may be a bigger challenge, one that cannot be overcome through policies allowing increased telehealth delivery alone. Clinicians have also described greater comfort using telehealth with patients they have already seen in person and feeling less comfortable initiating buprenorphine treatment via telehealth (15). If providers’ discomfort with initiating buprenorphine treatment via telehealth is preventing use of telehealth to increase access for patients with untreated OUD, additional guidance and support around telehealth delivery may be needed (24).
This study also found that phone visits were the most commonly used treatment modality during the post-COVID-19 period. During COVID-19, the VHA made substantial investments to support video telehealth including providing VHA internet-connected devices (e.g., tablets) to Veterans, while also providing trainings (25). Despite these investments, phone visits still greatly outnumbered video, suggesting that even with increased availability of video-enabled devices, there are remaining barriers to video visits in this patient population. These may include internet service availability, comfort with technology, and knowledge about using video telehealth (26–28). Notwithstanding persistent barriers to video visits and the current predominance of phone visits for buprenorphine, phone visits for buprenorphine is currently being contested and it is uncertain if this modality will be supported in the long term by policymakers (29). Given the large number of patients who are currently receiving buprenorphine via telehealth, any policy changes must be thoughtfully considered, including any changes that would eliminate or reduce phone access. It will be critical for providers to thoughtfully transition patients back to in-person care, if this is required, and a hybrid model blending in-person and virtual visits may be needed. Some patients have only known buprenorphine treatment via telehealth, with many—potentially more frequently from disadvantaged groups—engaging via phone rather than video (30). There could be major unintended consequences, including worsening existing treatment disparities, if these modalities are suddenly disrupted.
There are several limitations to this study. While VHA is the country’s largest single addiction treatment provider, and Veterans are an important population at higher risk for overdose (31) and with similar prevalence of OUD compared to the non-Veteran population (32), additional studies are needed outside of VHA. In particular, the VHA implemented infrastructure to support telehealth care delivery more broadly during COVID-19 (25), which may have resulted in trends in buprenorphine delivery that differ from other settings. Additionally, it was not possible to include a control group unaffected by COVID-19-related buprenorphine policy changes in this interrupted time series analysis, as these changes were enacted at the federal level and simultaneously affected all patients with OUD across the country. It is therefore possible that outside factors occurring contemporaneously with policy changes impacted observed changes in buprenorphine utilization. Telehealth use and the data on telehealth visits may have also varied across VHA facilities due to differences in facility-level policies, infrastructure, coding of telehealth visits and other factors. Also, this study focused on how COVID-19-related policies impacted treatment receipt, retention, and modality of delivery buprenorphine treatment only. It is possible that a shift to telehealth will have broad implications for how OUD care is delivered. Therefore, future research should examine the effects of telehealth modalities on additional measures of treatment quality, patient experience and outcomes. Finally, we did not examine use of psychotherapy and other treatments commonly used in patients with OUD and other SUDs. Given the finding that overall SUD care decreased during this study period, studies are needed to examine COVID-19 impacts on treatment and outcomes in other SUD patient populations.
This study found that in the national VHA healthcare system, buprenorphine treatment for OUD was maintained during the COVID-19 pandemic through a rapid shift to telehealth, suggesting any future changes to telehealth policies must be carefully considered as this could have major implications for patient care. We found although the number of patients receiving buprenorphine continued to increase throughout the study period, the number initiating care did not increase. This finding suggests that while maintaining policies that allow telehealth for buprenorphine delivery may be an important tool for improving retention, and therefore important for preventing overdose and other adverse outcomes, other efforts in addition to these are urgently needed to improve access for patients with untreated OUD to better link and engage patients in treatment via telehealth or in-person. Additional studies are needed in other healthcare systems, as well as studies examining how changes in treatment modality affect other treatment outcomes. Although the pandemic has presented acute challenges for healthcare and has likely substantially affected the lives of people with OUD, it may have also fostered innovations in care delivery.
Supplementary Material
Acknowledgments:
LAL is supported by a US Department of Veterans Affairs Health Services Research & Development Career Development Award (CDA 18-008) and funding from the VA Office of Connected Care (OCC 21-11) and CDC R49 CE003085. MCF is supported by a predoctoral training award from the Veterans Affairs Puget Sound Research & Development Service.
Disclosures:
LAL consults on telehealth for substance use disorder treatment for National Committee for Quality Assurance with funding from Alkermes and for Providers Clinical Support System with funding from SAMHSA.
Footnotes
Previous presentation: Addiction Health Services Research 2021
References
- 1.Larochelle MR, Bernson D, Land T, Stopka TJ, Wang N, Xuan Z, et al. Medication for Opioid Use Disorder After Nonfatal Opioid Overdose and Association With Mortality: A Cohort Study. Ann Intern Med. 2018. Jun 19; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dupouy J, Palmaro A, Fatséas M, Auriacombe M, Micallef J, Oustric S, et al. Mortality Associated With Time in and Out of Buprenorphine Treatment in French Office-Based General Practice: A 7-Year Cohort Study. Ann Fam Med. 2017. Jul;15(4):355–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin LA, Fernandez AC, Bonar EE. Telehealth for Substance-Using Populations in the Age of Coronavirus Disease 2019: Recommendations to Enhance Adoption. JAMA Psychiatry. 2020. Jul 1; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC). Increase in Fatal Drug Overdoses Across the United States Driven by Synthetic Opioids Before and During the COVID-19 Pandemic [Internet]. 2020. [cited 2021 Jun 5]. Available from: https://emergency.cdc.gov/han/2020/han00438.asp
- 5.Huskamp HA, Busch AB, Uscher-Pines L, Barnett ML, Riedel L, Mehrotra A. Treatment of Opioid Use Disorder Among Commercially Insured Patients in the Context of the COVID-19 Pandemic. JAMA. 2020. Dec 15;324(23):2440–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen TD, Gupta S, Ziedan E, Simon KI, Alexander GC, Saloner B, et al. Assessment of Filled Buprenorphine Prescriptions for Opioid Use Disorder During the Coronavirus Disease 2019 Pandemic. JAMA Intern Med. 2021. Apr 1;181(4):562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wyse JJ, Gordon AJ, Dobscha SK, Morasco BJ, Tiffany E, Drexler K, et al. Medications for Opioid Use Disorder in the Department of Veterans Affairs (VA) Health Care System: Historical Perspective, Lessons Learned and Next Steps. Subst Abus. 2018. Mar 29;0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin L, Fortney J, Bohnert A, Coughlin L, Zhang L, Piette J. Comparing telemedicine to in-person buprenorphine treatment in US Veterans with opioid use disorder. Journal of Substance Abuse Treatment. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weintraub E, Seneviratne C, Anane J, Coble K, Magidson J, Kattakuzhy S, et al. Mobile Telemedicine for Buprenorphine Treatment in Rural Populations With Opioid Use Disorder. JAMA Network Open. 2021. Aug 27;4(8):e2118487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cunningham C, Giovanniello A, Sacajiu G, Whitley S, Mund P, Beil R, et al. Buprenorphine Treatment in an Urban Community Health Center: What to Expect. Fam Med. 2008;40(7):500–6. [PMC free article] [PubMed] [Google Scholar]
- 11.Zheng W, Nickasch M, Lander L, Wen S, Xiao M, Marshalek P, et al. Treatment Outcome Comparison Between Telepsychiatry and Face-to-face Buprenorphine Medication-assisted Treatment for Opioid Use Disorder: A 2-Year Retrospective Data Analysis. J Addict Med. 2017. Apr;11(2):138–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002. Aug;27(4):299–309. [DOI] [PubMed] [Google Scholar]
- 13.Turner SL, Karahalios A, Forbes AB, Taljaard M, Grimshaw JM, Cheng AC, et al. Design characteristics and statistical methods used in interrupted time series studies evaluating public health interventions: a review. J Clin Epidemiol. 2020. Jun;122:1–11. [DOI] [PubMed] [Google Scholar]
- 14.Tofighi B, McNeely J, Walzer D, Fansiwala K, Demner A, Chaudhury CS, et al. A Telemedicine Buprenorphine Clinic to Serve New York City: Initial Evaluation of the NYC Public Hospital System’s Initiative to Expand Treatment Access during the COVID-19 Pandemic. J Addict Med. 2021. Feb 5; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett M, Huskamp HA. Treatment of opioid use disorder during COVID-19: Experiences of clinicians transitioning to telemedicine. J Subst Abuse Treat. 2020. Nov;118:108124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murphy SM, Yoder J, Pathak J, Avery J. Healthcare utilization patterns among persons who use drugs during the COVID-19 pandemic. J Subst Abuse Treat. 2021. Feb;121:108177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry. 2021. Jan;26(1):30–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cowan E, Khan MR, Shastry S, Edelman EJ. Conceptualizing the effects of the COVID-19 pandemic on people with opioid use disorder: an application of the social ecological model. Addict Sci Clin Pract. 2021. Jan 7;16(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laing S, Johnston S. Estimated impact of COVID-19 on preventive care service delivery: an observational cohort study. BMC Health Serv Res. 2021. Oct 16;21(1):1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vamos EP, Khunti K. Indirect effects of the COVID-19 pandemic on people with type 2 diabetes: time to urgently move into a recovery phase. BMJ Qual Saf. 2021. Oct 22;bmjqs-2021–014079. [DOI] [PubMed] [Google Scholar]
- 21.Patt D, Gordan L, Diaz M, Okon T, Grady L, Harmison M, et al. Impact of COVID-19 on Cancer Care: How the Pandemic Is Delaying Cancer Diagnosis and Treatment for American Seniors. JCO Clinical Cancer Informatics. 2020. Nov 1;(4):1059–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Finlay AK, Harris AHS, Timko C, Yu M, Smelson D, Stimmel M, et al. Disparities in Access to Medications for Opioid Use Disorder in the Veterans Health Administration. J Addict Med. 2021. Apr 1;15(2):143–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine Treatment Divide by Race/Ethnicity and Payment. JAMA Psychiatry. 2019. Sep 1;76(9):979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Telehealth for Opioid Use Disorder Toolkit: Guidance to Support High-Quality Care - PCSS [Internet]. Providers Clinical Support System. 2021. [cited 2021 Oct 25]. Available from: https://pcssnow.org/telehealth-for-opioid-use-disorder-toolkit-guidance-to-support-high-quality-care/ [Google Scholar]
- 25.US Department of Veterans Affairs. Connecting Veterans to Telehealth Care [Internet]. 2021. May. Available from: https://connectedcare.va.gov/sites/default/files/telehealth-digital-divide-fact-sheet.pdf [Google Scholar]
- 26.Der-Martirosian C, Wyte-Lake T, Balut M, Chu K, Heyworth L, Leung L, et al. Implementation of Telehealth Services at the US Department of Veterans Affairs During the COVID-19 Pandemic: Mixed Methods Study. JMIR Form Res. 2021. Sep 23;5(9):e29429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Benjenk I, Franzini L, Roby D, Chen J. Disparities in Audio-only Telemedicine Use Among Medicare Beneficiaries During the Coronavirus Disease 2019 Pandemic. Med Care. 2021. Nov 1;59(11):1014–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang L, Weiss J, Ryan EB, Waldman J, Rubin S, Griffin JL. Telemedicine increases access to buprenorphine initiation during the COVID-19 pandemic. J Subst Abuse Treat. 2021. May;124:108272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Drug Enforcement Administration. Use of Telephone Evaluations to Initiate Buprenorphine Prescribing. 2020. Mar. [Google Scholar]
- 30.Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021. Jan;27(1):21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bohnert ASB, Ilgen MA, Galea S, McCarthy JF, Blow FC. Accidental poisoning mortality among patients in the Department of Veterans Affairs Health System. Med Care. 2011. Apr;49(4):393–6. [DOI] [PubMed] [Google Scholar]
- 32.Rhee TG, Rosenheck RA. Comparison of opioid use disorder among male veterans and non-veterans: Disorder rates, socio-demographics, co-morbidities, and quality of life. Am J Addict. 2019. Jan 21; [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


