Condensation.
Women with posttraumatic stress disorder (PTSD) related to traumatic childbirth show similarly elevated psychophysiological responses as individuals with PTSD related to other traumatic events.
Keywords: Delivery, Obstetric, Diagnosis, Heart Rate, Maternal Health, Maternal Morbidity, Peripartum Period, Postpartum PTSD, Postpartum Depression, Script Driven Imagery, Stress Disorders, Post-Traumatic, Birth Trauma, Caesarean Section
OBJECTIVE
Posttraumatic stress disorder (PTSD) results from a specific, psychologically traumatic event, e.g., war, accidents, physical and sexual assaults. Increasing evidence indicates childbirth and its attendant circumstances can be experienced as a traumatic event and cause posttraumatic symptoms or even full PTSD.1 This condition is not limited to pregnancy loss, stillbirth, and prematurity. It can develop after a full-term, healthy birth, with an estimated prevalence between 4.6-6.3% and clinically significant symptoms in up to 16.8% of postpartum women.1 Provisional diagnosis of maternal, childbirth-related PTSD (CB-PTSD) primarily relies on subjective report using questionnaires targeting PTSD DSM symptom severity in the past month and resulting from childbirth as the index trauma.1 Because some PTSD symptoms may overlap with other mental postpartum conditions (e.g., depression)2, we investigated whether CB-PTSD is characterized by the elevated psychophysiological reactivity observed in PTSD stemming from combat and other traumatic stressors.3
STUDY DESIGN
Thirty-four (34) women aged approximately 35 years, with an immediate postpartum Peritraumatic Distress Inventory score >21, were recruited through hospital announcements. Average gestational delivery week was 38.76. The 13 with a subsequent PTSD-5 Checklist score >43 were classified as CB-PTSD; the remaining 21 as no CB-PTSD (Table). The study was approved by the Massachusetts General Brigham Human Research Committee. After giving written, informed consent following a full explanation of the procedures, patients were assessed using an established method that quantified skin conductance (SC), heart rate (HR), and left lateral frontalis and corrugator electromyogram (EMG) responses during script-driven mental imagery of their childbirth experience.
Table.
Demographics, childbirth factors, and overall physiological responsivity during childbirth imagery by maternal PTSD status
| Measures | CB-PTSD n = 13 |
No-CB-PTSD n = 21 |
|||
|---|---|---|---|---|---|
| n (%)/ M (SD) | n (%)/ M (SD) | χ2/ t | OR (95% CI) | p | |
| At delivery | |||||
| Age (years) | 30.53 (3.63) | 32.94 (5.10) | −1.49 | 0.15 | |
| Primiparity | 9 (69.23) | 17 (80.95) | 0.61 | 0.53 (0.11-2.63) | 0.68 |
| Sleep deprivation (before childbirth, ≤6 hours) | 10 (76.92) | 19 (90.48) | 1.18 | 0.35 (0.05-2.46) | 0.35 |
| Medication for pain | 12 (92.31) | 15 (71.43) | 2.14 | 4.80 (0.51-45.50) | 0.21 |
| Medication for induction | 7 (53.85) | 15 (71.43) | 1.09 | 0.47 (0.11-1.98) | 0.46 |
| Degree of pain in labor/delivery | 11 (84.62) | 17 (80.95) | 0.07 | 1.29 (0.20-8.31) | 1.00 |
| Obstetrical complications | 10 (76.92) | 16 (76.19) | 0.00 | 1.04 (0.20-5.34) | 1.00 |
| Mode of delivery | |||||
| Vaginal/Natural | 4 (30.77) | 6 (28.57) | 0.02 | 1.11 (0.25-5.04) | 1.00 |
| Vaginal Assisted | 2 (15.38) | 3 (14.29) | 0.01 | 1.09 (0.16-7.59) | 1.00 |
| Planned Cesarean | 0 | 0 | |||
| Unplanned Cesarean | 7 (53.85) | 12 (57.14) | 0.04 | 0.88 (0.22-3.52) | 1.00 |
| Gestational age (weeks) | 39.23 (1.83) | 38.48 (2.55) | 0.93 | 0.36 | |
| NICU admission | 6 (46.15) | 6 (28.57) | 1.09 | 2.14 (0.51-9.08) | 0.46 |
| Skin-to-skin contact | 9 (69.23) | 10 (47.62) | 1.52 | 2.48 (0.58-10.62) | 0.30 |
| Rooming in | 9 (69.23) | 14 (66.67) | 0.02 | 1.13 (0.25-4.98) | 1.00 |
| At informed consent and psychometric testing | |||||
| Age (years) | 34.29 (4.90) | 35.65 (5.40) | −0.74 | 0.47 | |
| Years postpartum | 3.77 (3.88) | 2.71 (2.84) | 0.91 | 0.37 | |
| Married | 11 (84.62) | 20 (95.24) | 1.13 | 0.28 (0.02-3.39) | 0.54 |
| Bachelor’s degree ≥ | 10 (76.92) | 18 (85.71) | 0.43 | 0.56 (0.09-3.29) | 0.65 |
| Employed | 9 (69.23) | 14 (66.67) | 0.02 | 1.13 (0.25-4.98) | 1.00 |
| Household income (≥100K) | 5 (38.46) | 11 (52.38) | 0.62 | 0.57 (0.14-2.32) | 0.50 |
| Non-Hispanic White | 9 (69.23) | 18 (85.71) | 1.33 | 0.38 (0.07-2.05) | 0.39 |
| Acute stress response to childbirth | 38.08 (7.33) | 33.76 (6.75) | 1.75 | 0.09 | |
| CB-PTSD symptoms | 50.77 (5.15) | 24.38 (13.00) | 6.96 | 0.00 | |
| Breastfeeding | 12 (92.31) | 16 (76.19) | 1.44 | 3.75 (0.39-36.43) | 0.37 |
| At physiological testing | |||||
| Overall physiological responsivity | 0.51 (0.21) | 0.33 (0.17) | 2.73 | 0.01 | |
Note. CB-PTSD = childbirth-related posttraumatic stress disorder, based on PTSD Checklist-5 score> 43; At delivery time point is in regard to the traumatic childbirth; Sleep deprivation defined as less than 6 hours of sleep on the night before the childbirth; Degree of pain in labor/delivery refers to at least “great” degree; NICU = Neonatal intensive care unit; Acute stress response = immediate, self-reported negative cognitive, emotional, and physiological responses to childbirth based on the Peritraumatic Distress Inventory; Overall physiological responsivity to childbirth imagery refers to average posterior probability (PPrb) score, using skin conductance, heart rate and frontalis electromyogram responses during two childbirth script-driven imageries per patient. Breastfeeding status (yes/no) pertains to currently or in the past. Physiological testing was conducted on average 13 days after informed consent and psychometric testing.
OR = odd ratios, 95% CI = 95% confidence interval; significance estimates from t- or Fisher's exact tests.
The primary analyses were univariate and multivariate analysis of variance. As an ancillary, a composite (univariate) measure of physiological responsivity was calculated as the “posterior probability” (PPrb) of a patient’s belonging to the PTSD reference group using an a priori discriminant function derived from a large sample of PTSD and non-PTSD individuals who had experienced other, non-childbirth related traumatic events and had undergone the same psychophysiological procedure.4
RESULTS
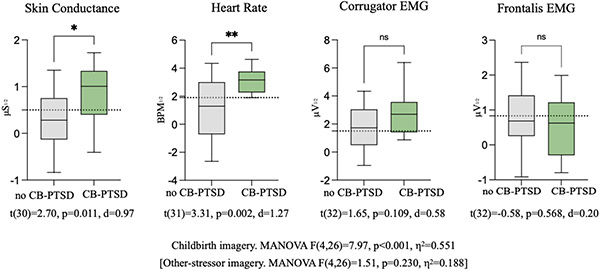
CB-PTSD patients were more physiologically responsive during imagery of their childbirth experiences, compared to no CB-PTSD patients (Figure). Mean univariate physiologic responses of the CB-PTSD group were largely above working PTSD cutoffs (dotted lines) from previous studies of individuals exposed to other traumas such as combat, sexual abuse, motor vehicle accidents.5 No significant psychophysiological group differences were observed during imagery of a non-childbirth-related, stressful event that was used as a control. These findings suggest that CB-PTSD patients exhibit physiological responses similar to those of other PTSD individuals.
Figure. Physiological responsivity during childbirth imagery by maternal PTSD status.
The figure shows the physiological responses of patients with and without provisional CB-PTSD during mental imagery of personal childbirth traumatic events. Data are displayed as box and whisker plots. Boxes span the first and third quartiles, with the horizontal lines representing the median, and whiskers the minimum to maximum values. Gray boxes represent no CB-PTSD. Green boxes represent CB-PTSD. Dashed lines represent empirical cutoffs for PTSD based on previous research. The square root of the average physiological values is derived from 2 personal scripts concerning labor, delivery, or immediate postpartum stressful events. Differences in degrees of freedom in t tests analyses are owing to missing data. Other stressors refer to traumatic events that are non-childbirth-related. (Mean values for skin conductance, heart rate, corrugator EMG, and frontalis EMG for the no CB-PTSD group are 0.33, 1.12, 1.76, and 0.78 and for the CB-PTSD group 0.92, 3.15, 2.64, and 0.61, respectively).
CONCLUSION
Our work provides a validation of the clinical reality of the CB-PTSD diagnosis. Women with CB-PTSD show similarly elevated physiological responses during mental imagery of the traumatic childbirth experience as found in PTSD resulting from other types of traumas. Their physiological alterations are evoked by childbirth. Our findings encourage revising the formal recognition of mental illness with postpartum onset by expanding the spectrum to include disorders of traumatic stress. A simplified physiological assessment, performed during routine obstetric care, of women endorsing clinically significant childbirth-related peritraumatic distress may aid in the identification of those likely to meet CB-PTSD diagnosis.
ACKNOWLEDGMENTS
We would like to thank Ms. Amanda King and Mr. Gus Mayopoulos for taking part in performing the physiological assessments. All authors were affiliated with Massachusetts General Hospital, were without conflicts of interest, and agreed to be included.
Funding source.
S.D. was supported by awards from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R21HD100817), the Massachusetts General Hospital Executive Committee on Research (ECOR) (ISF award), the Massachusetts General Hospital Psychiatry Department, and the Harvard Mind Brain and Behavior (faculty award). The sponsors were not involved in the performance of the study.
Footnotes
Disclosure statement. The authors report no conflicts of interest.
Information related to this study was presented at the NIH pregnancy and Maternal Conditions that Increase Risk of Morbidity and Mortality Virtual Workshop 2020; International Marcé Society for Perinatal Mental Health biennial meeting, October 2020 and the Marcé Society of North America biennial meeting, October 2021 (virtual).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Dekel S, Stuebe C, Dishy G. Childbirth Induced Posttraumatic Stress Syndrome: A Systematic Review of Prevalence and Risk Factors. Front Psychol. 2017; 11;8:560. doi: 10.3389/fpsyg.2017.00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dekel S, Ein-Dor T, Dishy GA, Mayopoulos PA. Beyond postpartum depression: posttraumatic stress-depressive response following childbirth. Arch Womens Ment Health. 2020; 23:557–564. doi: 10.1007/s00737-019-01006-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pitman RK, Orr SP, Forgue DF, de Jong JB, Claiborn JM. Psychophysiologic assessment of posttraumatic stress disorder imagery in Vietnam combat veterans. Arch Gen Psychiatry. 1987; 44:970–575. doi: 10.1001/archpsyc.1987.01800230050009 [DOI] [PubMed] [Google Scholar]
- 4.Bauer MR, Ruef AM, Pineles SL, Japuntich SJ, Macklin ML, Lasko NB, Orr SP. Psychophysiological assessment of PTSD: A potential research domain criteria construct. Psychol Assess. 2013; 25:1037–43. doi: 10.1037/a0033432 [DOI] [PubMed] [Google Scholar]
- 5.Brunet A, Thomas E, Saumier D. Trauma reactivation plus propranolol is associated with durably low physiological responding during subsequent script-driven traumatic imagery. Can J Psychiatry. 2014; 59: 228–232. doi: 10.1177/070674371405900408 [DOI] [PMC free article] [PubMed] [Google Scholar]