Abstract
A 74-year-old patient presented with hematochezia and a history of liver cirrhosis with repeated bleeding from esophageal and rectal varices. Endoscopic examination revealed multiple rectal varices with positive red color signs. Ascites, severe portosystemic thrombosis and a splenorenal shunt were diagnosed on a contrast-enhanced dynamic computed tomography examination. From a transjugular approach, we circumvented thrombosed regions by maneuvering double balloon catheters through the shunt and dilated left colic marginal vein. We managed to successfully obliterate the varices.
Keywords: Liver cirrhosis, Rectal varices, Splenorenal shunt, Portal thrombosis, Antegrade transvenous sclerotherapy, Double balloon catheters technique
Introduction
Portosystemic collateral pathways may manifest as varices which are dilated, meandering veins that form in a submucosal or subepithelial region of the gastrointestinal system [1]. Interventional radiologists are involved in managing gastro-esophageal varices, as they are a frequent complication of portal hypertension in patients with liver cirrhosis [2]. The varices can also develop in ectopic places such as the rectum, duodenum, jejunum, ileum, and colon. Rupture of anorectal varices can be especially dangerous due to the diameter of the abnormal vessels and the massive, life-threatening bleeding that follows [3].
In this report, we present a difficult yet successful procedure of obliterating rectal varices accessed from a transjugular approach via portosystemic collaterals, in a patient with portal thrombosis and ascites.
Case report
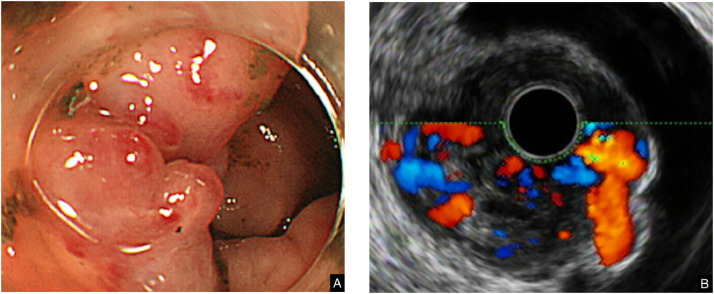
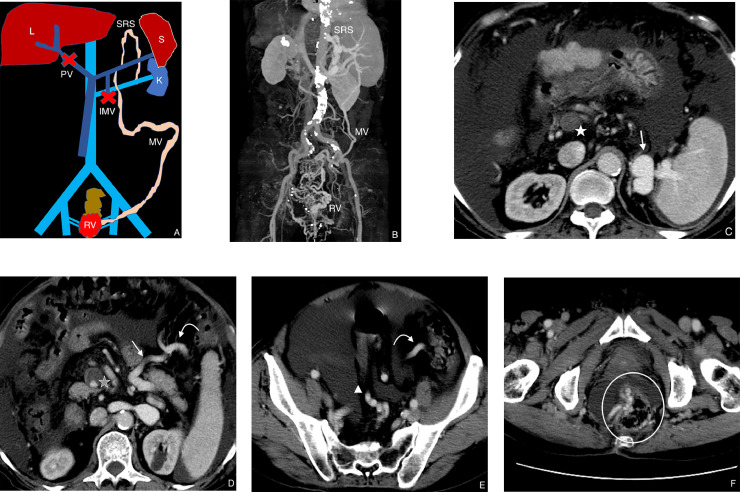
A 74-year-old man was admitted to our hospital with complaints of intermittent episodes of hematochezia. He had a medical history of recurrent bleeding from rectal varices and esophageal varices ruptures, both developed due to alcoholic liver disease and progressing cirrhosis. Previous bleeding incidents had been treated with endoscopic procedures. Laboratory tests revealed elevated levels of BUN (35 mg/dL, normal range: 6-24 mg/dL), total bilirubin (1.8 ml/dL, normal range: up to 1.2 mg/dL), creatinine (1.58 mg/dL, normal range: 0.74-1.35 mg/dL) and prothrombin time (PT 15.5 sec, normal range 11.5-14.5 sec; PT-INR 1.25, normal range: 08-1.2, with PT% at 55%), as well as decreased levels of hemoglobin (8.0 g/dL, normal range for males: 13.8-17.2 g/dL), platelets (8.0 × 104 /μL, normal range: 15-45 × 104 /μL), and albumin (2.6 mg/dL, normal range: 3.4-5.4 mg/dL). These laboratory findings translated into model for end-stage liver disease (MELD) score of 16, and albumin-bilirubin (ALBI) score of -1.23, grade 3. Due to significant ascites the Child-Pugh score was elevated to 10 (class C). This suggested a decompensated stage of the disease. Rectal endoscopy revealed multiple varices protruding into the lumen of the rectum with positive RC (red color) signs, but active bleeding was not observed (Fig. 1A). Rectal Doppler ultrasound confirmed that blood flow was present in the varices (Fig. 1B). Contrast-enhanced dynamic computed tomography (CT) findings included ascites, thrombosis of the portal, superior mesenteric and inferior mesenteric veins, a spontaneous splenorenal shunt, dilated colic marginal vein, and multiple rectal varices (Fig. 2).
Fig. 1.
Rectal endoscopy examination revealed multiple varices protruding into the lumen of the rectum with positive RC signs (A). Rectal Doppler ultrasound confirmed that blood flow was present in the varices (B).
Fig. 2.
A-B: diagram of relevant anatomical landmarks in a coronal plane and its corresponding maximum intensity projection (MIP) image. IMV, thrombosed inferior mesenteric vein; K, kidney; L, liver; MV, dilated left colic marginal vein; PV, thrombosed portal vein; S, spleen; SRS, splenorenal shunt; RV, rectal varices. (C-F) Preprocedural contrast-enhanced dynamic CT, portal phase axial images. Straight arrow—splenorenal shunt, bent arrow—dilated left colic marginal vein, white star—thrombosed portal vein, gray star—thrombosed superior mesenteric vein, arrowhead—superior rectal vein, circle—rectal varices.
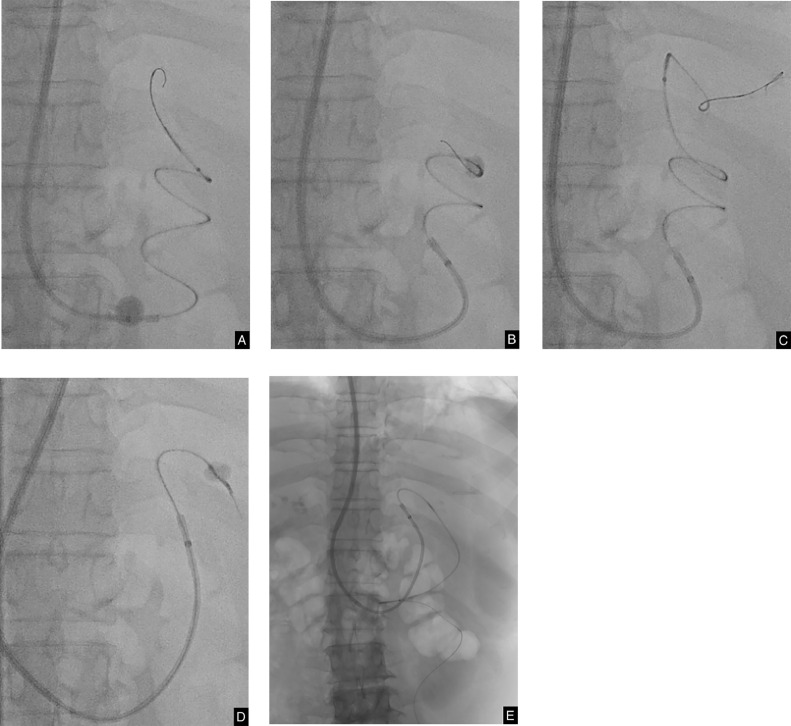
Since the varices persisted despite multiple endoscopic treatments, an IR approach was chosen. Portal thrombosis, significant ascites and multiple outflow vessels draining into the bilateral internal iliac veins excluded TIPS (transjugular intrahepatic portosystemic shunt) or procedures with a retrograde approach. We elected to perform antegrade transvenous sclerotherapy from the transjugular approach, using the shunt and the marginal vein as a pathway to access the varices. Due to the length and meandering course of the pathway, we decided on using double balloon catheters to slowly straighten out and move through the vessels. This technique is performed in endoscopies [4], but to our knowledge its use in endovascular procedures has not been reported. Two balloon catheters of 9Fr and 5Fr sizes (CANDIS Coaxial And Double Interruption System Balloon Catheter, Medikit Co. Ltd, Tokyo, Japan) were inserted into the splenorenal shunt over a guidewire. 9Fr catheter balloon was inflated and placed near the entry to the shunt (Fig. 3A). 5Fr catheter was advanced into the shunt, and its balloon was inflated and fixed against the vessel wall, while paying special attention to the applied pressure. A 9Fr balloon was deflated and its catheter was also advanced into the shunt (Fig. 3B). 5Fr catheter with deflated balloon was slowly moved through (Fig. 3C). A 5Fr balloon was then inflated, and the 9Fr catheter was moved closer to the 5Fr balloon, which straightened out the shunt. (Fig. 3D). A microcatheter (PROGREAT 150 cm, Terumo Corporation, Tokyo, Japan) with the guidewire were then inserted and advanced through the marginal vein (Fig. 3E). The microcatheter tip was placed in the superior rectal vein. First, the outflow veins of the varices were embolized with 2 mL of n-Butyl cyanoacrylate (Histoacryl, B. Braun Melsungen AG, Melsungen, Germany) mixed with lipiodol in a 1:9 ratio. Next, varices were obliterated by 10 mL of 5% EOI mixture made by combining equal amounts of 10% ethanolamine oleate (OLDAMIN, FUJI Chemical Industry, Toyama, Japan) with iopamidol 300 mgI/ml (IOPAMIDOL, Hikari Pharmaceuticals, Tokyo, Japan). Finally, the inflow vessel was obliterated with metal coiling (TORNADO Embolization Coil, COOK Medical Japan G.K., Tokyo, Japan).
Fig. 3.
DSA images of the procedure. A 9Fr catheter balloon is inflated and fixed near the entry to the shunt; 5Fr catheter and the guidewire are advanced into the shunt (A). A 5Fr balloon is inflated and fixed against the vessel wall; 9Fr balloon is deflated and its catheter is advanced into the shunt (B). A 5Fr catheter with deflated balloon is slowly advanced forward (C). A 5Fr balloon is inflated, and the 9Fr catheter is moved closer to the 5Fr balloon; this unwinds the shunt, which now appears as a straight vessel (D). Microcatheter and the guidewire are advanced through the marginal vein (E).
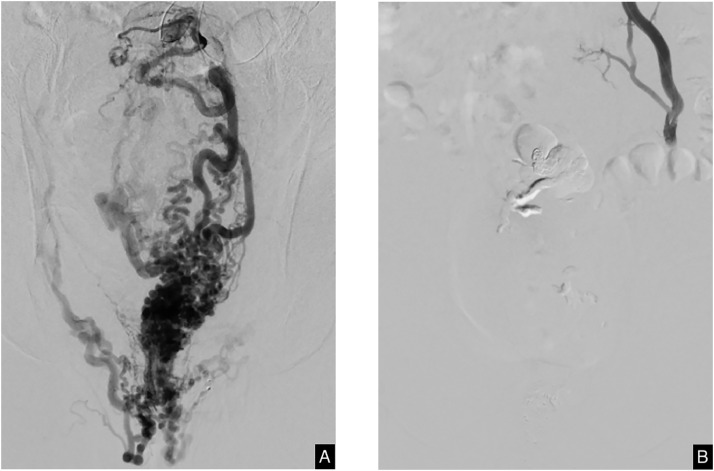
Complete obliteration of the varices was confirmed both on post-procedural digital subtraction angiography (DSA) images (Fig. 4), and on a 1-week follow-up contrast-enhanced CT scan (Fig. 5). On a 2-year follow-up endoscopic examination, no variceal recurrence was observed.
Fig. 4.
Large rectal varices seen on the DSA image before sclerotherapy (A). Post-treatment image shows virtually no contrast flowing through the varices (B).
Fig. 5.
One-week follow-up contrast-enhanced CT images confirmed the variceal obliteration (circle).
Discussion
Varices in portal hypertension are collateral pathways that develop in patients with portal hypertension [3,5,6], defined as hepatic venous pressure gradient over 10 mmHg [7]. The most common underlying cause is liver cirrhosis. Other possible conditions include idiopathic portal hypertension, extrahepatic portal vein obstruction, tumors, pancreatitis, surgeries, and congenital diseases [2,8]. Rectum is a common location for ectopic varices, which develop in 3%-75% patients with portal hypertension [9] and between 38% and 95% in liver cirrhosis [8]. Probability of bleeding is considered to be low: Robertson et al reports 2%-5% of all variceal bleeds [8], Vidal et al reports 8% [10], although other studies indicate the incidence might be higher [6,8,11]. If left untreated, however, rectal varices might lead to rupture and hemorrhage massive enough to be fatal.
In our patient, we opted to perform antegrade transvenous sclerotherapy from the transjugular approach. We successfully used collateral vessel communications (splenorenal shunt, dilated marginal vein) as an antegrade approach to access and obliterate the recurrent varices. Our literature search suggests that no similar case has been reported before. We believe this approach is viable for patients with complications that would otherwise exclude them from endovascular procedures. Furthermore, we believe our case is unique in its application of double balloon catheters to move through the collateral vessels. While double balloon endoscopies and enteroscopies have been described [4], such techniques have seen little coverage in IR reports.
Currently, there is no consensus or standardization on treatment of the rectal varices, although management algorithms have been proposed [8,12]. Endoscopic variceal ligation and endoscopic injection sclerotherapy are usually the first choice due to low invasiveness [13], although in our case multiple endoscopic treatments proved unsuccessful in controlling the varices. Among IR procedures, TIPS is an effective method that was introduced into rectal variceal treatment by Katz et al. [3]. While generally safe, re-bleeding episodes following the procedure have been reported [14]. It is also not recommended for patients in risk of developing hepatic encephalopathy [5], even though earlier studies demonstrated success in patients with decompensated liver disease [10]. TIPS and trans-TIPS approach were not viable in our patient due to extensive portal, superior mesenteric vein (SMV) and inferior mesenteric vein (IMV) thrombosis. Percutaneous transhepatic or trans-splenic obliteration [15] was abandoned since it requires a direct puncture into the portal branch or splenic branch—a contraindication in patients with ascites and portal, SMV and IMV thrombosis. Balloon-occluded antegrade transvenous sclerotherapy from the prone position, accessed via the greater sciatic foramen and puncturing the superior rectal vein has also been reported [16]. However, we had concerns that large-volume ascites in our patient would hinder the procedure. Balloon-occluded retrograde transvenous obliteration (BRTO), introduced in 1996 by Kanagawa et al [17], is considered a gold standard in treating gastric varices. There are reports in the literature that demonstrate successful management of rectal varices with this technique [13], but it is not applicable in most cases. This is because rectal varices tend to develop multiple outflow vessels [13] (as in our patient, with multiple outflow veins draining into both internal iliac veins), and the retrograde transvenous approach is of limited efficacy. Furthermore, studies following treatment of gastric varices showed that BRTO does not decrease portal pressure, leading to development or exacerbation of esophageal varices [5,8].
Our approach has its limitations. The pathway is not straightforward and presupposes the existence of viable collateral vessels, thus it is not guaranteed to be applicable in every case. Furthermore, these collateral vessels, contrary to arteries, may rupture when too much pressure is applied, thus an utmost care must be taken during balloon inflation.
Conclusion
Rectal varices were accessed and treated from the transjugular approach by successfully navigating through the available splenorenal shunt and marginal vein. Double balloon catheters may be useful in endovascular procedures to advance through meandering vessels.
Patient consent
Written informed consent was obtained from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Sharma M, Rameshbabu CS. Collateral pathways in portal hypertension. J Clin Exp Hepatol. 2012;2:338–352. doi: 10.1016/j.jceh.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watanabe N, Toyonaga A, Kojima S, Takashimizu S, Oho K, Kokubu S, et al. Current status of ectopic varices in Japan: results of a survey by the Japan Society for Portal Hypertension: current status of ectopic varices in Japan. Hepatol Res. 2010;40:763–776. doi: 10.1111/j.1872-034X.2010.00690.x. [DOI] [PubMed] [Google Scholar]
- 3.Katz JA, Rubin RA, Cope C, Holland G, Brass CA. Recurrent bleeding from anorectal varices: successful treatment with a transjugular intrahepatic portosystemic shunt. Am J Gastroenterol. 1993;88:1104–1107. [PubMed] [Google Scholar]
- 4.Palermo M, Neto MG. Gallbladder stones in bariatrics and management of choledocholithiasis after gastric bypass. Int J Gastrointest Interv. 2019;8:26–34. doi: 10.18528/ijgii180035. [DOI] [Google Scholar]
- 5.Lee A, Suhardja TS, Nguyen TC, Chouhan HS. Management options for rectal variceal bleeding in the setting of hepatic encephalopathy. ANZ J Surg. 2021;91:49–54. doi: 10.1111/ans.15982. [DOI] [PubMed] [Google Scholar]
- 6.Garrido M, Gonçalves B, Ferreira S, Rocha M, Salgado M, Pedroto I. Treating untreatable rectal varices. GE - Port. J Gastroenterol. 2019;26:420–424. doi: 10.1159/000496121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bandali MF, Mirakhur A, Lee EW, Ferris MC, Sadler DJ, Gray RR, et al. Portal hypertension: Imaging of portosystemic collateral pathways and associated image-guided therapy. World J Gastroenterol. 2017;23:1735. doi: 10.3748/wjg.v23.i10.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robertson M, Thompson AI, Hayes PC. The management of bleeding from anorectal varices. Curr Hepatol Rep. 2017;16:406–415. doi: 10.1007/s11901-017-0382-6. [DOI] [Google Scholar]
- 9.Yoshino K, Imai Y, Nakazawa M, Chikayama T, Ando S, Sugawara K, et al. Therapeutic strategy for patients with bleeding rectal varices complicating liver cirrhosis: therapeutic strategy for rectal varices. Hepatol Res. 2014;44:1088–1094. doi: 10.1111/hepr.12232. [DOI] [PubMed] [Google Scholar]
- 10.Vidal V, Joly L, Perreault P, Bouchard L, Lafortune M, Pomier-Layrargues G. Usefulness of transjugular intrahepatic portosystemic shunt in the management of bleeding ectopic varices in cirrhotic patients. Cardiovasc Intervent Radiol. 2006;29:216–219. doi: 10.1007/s00270-004-0346-4. [DOI] [PubMed] [Google Scholar]
- 11.Shudo R, Yazaki Y, Sakurai S, Uenishi H, Yamada H, Sugawara K. Clinical study comparing bleeding and nonbleeding rectal varices. Endoscopy. 2002;34:189–194. doi: 10.1055/s-2002-20289. [DOI] [PubMed] [Google Scholar]
- 12.Maslekar S, Toh E-W, Adair R, Bate JP, Botterill I. Systematic review of anorectal varices. Colorectal Dis. 2013;15:e702–e710. doi: 10.1111/codi.12417. [DOI] [PubMed] [Google Scholar]
- 13.Nagai K, Miyayama S, Yamashiro M, Tohyama J, Kawamura K, Sanada T. Successful treatment of bleeding rectal varices with balloon-occluded retrograde transvenous obliteration in a patient with a history of sigmoidectomy. Interv Radiol. 2016;1:19–22. doi: 10.22575/interventionalradiology.1.1_19. [DOI] [Google Scholar]
- 14.Sakib SMN, Kobayashi K, Jawed M. Potential pitfalls in transjugular portosystemic shunt placement for bleeding rectal varices. Case Rep Gastroenterol. 2015;9:296–301. doi: 10.1159/000439164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Minamiguchi H, Kawai N, Sato M, Ikoma A, Sanda H, Nakata K, et al. Successful treatment of endoscopically unmanageable rectal varices by balloon-occluded antegrade transvenous sclerotherapy followed by microcoil embolization. J Vasc Interv Radiol. 2013;24:1399–1403. doi: 10.1016/j.jvir.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 16.Ono Y, Kariya S, Nakatani M, Yoshida R, Kono Y, Kan N, et al. Balloon-occluded antegrade transvenous sclerotherapy to treat rectal varices: a direct puncture approach to the superior rectal vein through the greater sciatic foramen under CT fluoroscopy guidance. Cardiovasc Intervent Radiol. 2015;38:1320–1324. doi: 10.1007/s00270-015-1174-4. [DOI] [PubMed] [Google Scholar]
- 17.Kanagawa H, Mima S, Kouyama H, Gotoh K, Uchida T, Okuda K. Treatment of gastric fundal varices by balloon-occluded retrograde transvenous obliteration. J Gastroenterol Hepatol. 1996;11:51–58. doi: 10.1111/j.1440-1746.1996.tb00010.x. [DOI] [PubMed] [Google Scholar]