Abstract
Background
Mental health conditions are common among adolescents and young adults, yet few receive adequate mental health treatment. Many young people seek support and information online through social media, and report preferences for digital interventions. Thus, digital interventions deployed through social media have promise to reach a population not yet engaged in treatment, and at risk of worsening symptoms.
Objective
In this scoping review, we aimed to identify and review empirical research on social media-based interventions aimed at improving adolescent and young adult mental health. A secondary objective was to identify the features and functionalities of platforms described as social media.
Methods
Adhering to the PRISMA-ScR guidelines for scoping reviews, the search was conducted in PubMed MEDLINE; Embase Central Register of Controlled Trials (Wiley); PsycINFO (Ebsco); Scopus; Web of Science; IEEE Xplore; ACM Digital Library; and ClinicalTrials.gov from inception until November 2021. Studies were included if they involved adolescents or young adults (10–26 years of age) that meet clinical, or subclinical, levels of a mental health condition and include a pre- and post-assessment of mental health outcomes.
Results
Among the 18,380 references identified, 15 met full inclusion criteria and were published between 2017 and 2021–this included four randomized controlled trials, seven non-randomized pre-post trials, and four were experimental or quasi-experimental designs. Just five studies were delivered through an existing social media site (Facebook or Pixtori), with the remainder focused on purpose-built networks. Three studies involved adolescents or young adults who self-reported a mental health condition, seven involved young people diagnosed with a mental health condition by a clinician or who scored above a clinical threshold on valid clinical measure, three involved college students without a mental health inclusion criterion, and two studies focused on young people with a cancer diagnosis.
Conclusions
The review highlights innovations in the delivery of mental health interventions, provides preliminary evidence of the ability of social media interventions to improve mental health outcomes, and underscores the need for, and merit of, future work in this area. We discuss opportunities and challenges for future research, including the potential to leveragei existing peer networks, the use of just-in-time interventions, and scaling interventions to meet need.
Keywords: Social media, Intervention, Mental health, Social networking, Adolescent, Young adult
Highlights
-
•
Social media interventions appear to be feasible and acceptable among young people with mental health symptoms
-
•
Social media interventions may also improve mental health symptoms among young people
-
•
This remains an emerging field, with further evaluation studies of social media interventions for mental health required.
1. Introduction
Adolescents and young adults (AYA) experience high rates of mental health conditions, yet have low rates of mental health service utilization (Lipari et al., 2016; Substance Abuse and Mental Health Services Administration (SAMHSA), 2019). Structural barriers, including financial and access constraints, as well as attitudinal barriers such as stigma, medical mistrust, and preferences for self-management, all impact AYA's interest in, and use of, traditional face-to-face treatment. Many young people endorse interest in digital mental health (DMH) treatments which have the potential to reduce some of these common barriers and increase access to evidence-based treatments while supporting user autonomy, especially among underserved individuals (Pretorius et al., 2020, Pretorius et al., 2019; Renn, 2019).
Digital tools, such as smartphones, apps, and social media platforms, are widely accessible, popular, and used daily by young adults and adolescents. As such, mental health interventions delivered in these formats are believed to fit more easily into the fabric of young people's daily lives. Several rigorous reviews document the feasibility and efficacy of web-based and app-based digital mental health interventions for young people with various mental health conditions (Garrido et al., 2019; Lattie et al., 2019). However, there is no review, to our knowledge, that focuses on the use of social media as a context to deploy mental health interventions. Social media have unique potential to improve mental health for young people at scale since they are spaces where young people go to exchange information, connect with peers and community, develop their identity, as well as share personal experiences of mental health (Berry et al., 2017; Guntuku et al., 2017; Wang et al., 2016). Indeed, 84 % of young adults have reported using a social media platform (Auxier and Anderson, 2021), and social media are used by those marginalized in mental health care (Saha et al., 2019) further suggesting social media's potential to be a potent delivery mechanism for DMH prevention and intervention among underserved populations.
To date, most research at the intersection of social media and mental health has explored retrospective social media content to understand community concerns or to identify linguistic and behavioral patterns to identify mental-health related risk. Less work has focused on leveraging social media as a context for mental health intervention. To understand the potential for social media in mental health intervention, a review of existing work is needed, and timely. Given that there are no existing reviews on this topic, our goal was to identify articles to describe this research space. We also aimed to identify common components across interventions, the populations they were meant to serve, and opportunities to build upon prior work. Social media may provide a context to deliver mental health interventions at scale, in a more equitable manner, and in a format that is acceptable and engaging to this young population.
1.1. Objective
The objective of this scoping review was to identify and review empirical research on social media-based interventions aimed at improving mental health conditions in AYAs. We used a broad definition of social media as an online space that allows for community interaction and the exchange of user-generated content (e.g., online discussion boards, forums) in line with other reviews (McKeon et al., 2022). We limited our search to interventions that were delivered mostly, or entirely, through social media and to studies examining the intentional implementation of a mental health intervention. This ultimately included purpose-built platforms with social media features. Since social media is a consistently evolving term, a secondary objective of this review was to identify the features and functionalities of platforms labeled as social media. This secondary objective would provide insight into social media-based components that may not necessarily be primarily delivered on a social media platform but still can be useful or complementary to interventions aimed at improving mental health conditions among AYAs.
2. Methods
This scoping review followed the Joanna Briggs Institute Scoping Review Methodology and is reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) guidelines (Tricco et al., 2018). The study protocol for this review was pre-registered through DigitalHub: https://digitalhub.northwestern.edu/files/62674cde-fb6b-408e-9197-b11966c48c7a. A librarian (LO) collaboratively developed the search strategies with review authors (KK, KW, JM), and in October 26th and November 11th 2021 ran searches in the following databases: PubMed MEDLINE; Embase (embase.com); Central Register of Controlled Trials (Wiley); PsycINFO (Ebsco); Scopus; Web of Science; IEEE Xplore; ACM Digital Library; and ClinicalTrials.gov. As a note, Medarxiv or Psycharxiv were not searched as stated in the published protocol as it was not possible to replicate the search string complexity in these databases. All databases were searched from inception with no language or date limits applied, and gray literature included. The search looked for articles on mental health, social media, interventions, and adolescents and young adults. A full list of search strategies and terms used is provided in the search strategy appendix (See Appendix A). We also screened the reference lists of key studies and relevant systematic reviews.
A pilot screen of 100 random articles was initially performed in Rayyan, a free review software, to clarify inclusion and exclusion criteria. Once criteria were solidified, Covidence systematic review software was used to manage the article screening and review process. Four reviewers (KK, KW, JM, DY) screened article titles and abstracts to determine if each article should be excluded or advanced to full-text screening. Reviewers conducting the title and abstract screening used predetermined criteria and each article was reviewed by a minimum of two reviewers independently.
At the full-text review stage, articles were systematically excluded in a stepped fashion based on the following criteria: (1) wrong article type (e.g., conference abstracts, protocols) (2) wrong setting (defined as not social media), (3) wrong study design (e.g., no pre- or post-test), (4) wrong outcomes (i.e., no mental health outcome), and (5) wrong age (i.e., 10 > mean age > 26). For example, if an article did not meet the first criteria (article type) it was excluded at that step. The wrong setting criteria differentiated between studies that included social networking for unstructured peer support, but that had no further delivery of content (or intervention) through the platform itself (e.g., a social networking component in addition to a web-based intervention would be excluded if there's no training and/or intervention delivered through the social network platform).
For the full-text review stage, we originally excluded articles that described interventions which included a social media component but were not “entirely delivered through social media.” However, this resulted in just 5 studies (1–5 in Table 1). We subsequently refined our definition to “mostly or entirely delivered through social media” to include a broader range of interventions that included social media, provided the social media features were essential for delivering the intervention (i.e. active clinical/therapeutic components of the intervention rather than general social support/networking). Studies, then, were included to reflect interventions that had a traditional or built social media/networking platform, even if this platform was not the primary focus of the program (e.g., Moderated Online Support Therapy; MOST). Throughout the full-text review process discrepancies were resolved via consensus discussions among at least two reviewers.
Table 1.
Characteristics of included studies.
| Author | Year | Country | Study design | N (analysis) | Population description | Social media platform |
|---|---|---|---|---|---|---|
| Firth | 2017 | United States | Randomized controlled trial | 39 | Undergraduate and graduate students | |
| Greer | 2019 | United States | Randomized controlled trial | 45 | Young adults (age 18–29 years) within 5 years of completing active cancer treatment | |
| Watkins | 2020 | United States | Quasi-experimental, pre-post design | 40 | Black men with self-reported anxiety or depression symptoms | |
| Yu | 2020 | Taiwan | Randomized controlled trial | 136 | College students recruited | |
| Pailler | 2020 | United States | Exploratory mixed-methods cohort study | 29 | Adolescent and young adult cancer patients (17–36) | Pixtori |
| Asbury | 2018 | United States | Randomized controlled trial | 51 | University women (and their friends/family) | Built network |
| Radovic | 2018 | United States | Non-randomized pre-post trial | 57 | Adolescents and young adults (aged 14–26 years) with a self-reported history of depressive and/or anxiety symptoms | Built network/blog |
| Karim | 2021 | United States | Non-randomized pre-post trial | 34 | Adolescents and young adults who self-report symptoms of depression and anxiety | Built network/blog |
| Ludwig | 2019 | United States | Non-randomized pre-post trial | 26 | Young people with schizophrenia spectrum disorder | Built network/MOST |
| Alvarez-Jimenez | 2018 | Australia | Uncontrolled pilot study | 14 | Young people at ultra-high risk for psychosis | Built network/MOST |
| Rice | 2018 | Australia | Non-randomized pre-post trial | 42 | Young people with depression | Built network/MOST |
| McEnery | 2019 | Australia | Non-randomized pre-post trial | 10 | Youth with first-episode psychosis (FEP) w/ social anxiety | Built network/MOST |
| Alvarez-Jimenez | 2020 | Australia | Uncontrolled, single-group design | 93 | AYAs with mental health conditions | Built network/MOST |
| Bailey | 2020 | Australia | Non-randomized pre-post trial | 20 | Young adult patients w/ recent suicidal ideation | Built network/MOST |
| Rice | 2020 | Australia | Uncontrolled pre-post design | 76 | Young people with social anxiety | Built network/MOST |
| Firth | 2017 | United States | Randomized controlled trial | 39 | Undergraduate and graduate students | |
| Greer | 2019 | United States | Randomized controlled trial | 45 | Young adults (age 18–29 years) within 5 years of completing active cancer treatment | |
| Watkins | 2020 | United States | Quasi-experimental, pre-post design | 40 | Black men with self-reported anxiety or depression symptoms | |
| Yu | 2020 | Taiwan | Randomized controlled trial | 136 | College students recruited | |
| Pailler | 2020 | United States | Exploratory mixed-methods cohort study | 29 | Adolescent and young adult cancer patients (17–36) | Pixtori |
| Asbury | 2018 | United States | Randomized controlled trial | 51 | University women (and their friends/family) | Built network |
| Radovic | 2018 | United States | Non-randomized pre-post trial | 57 | Adolescents and young adults (aged 14–26 years) with a self-reported history of depressive and/or anxiety symptoms | Built network/blog |
| Karim | 2021 | United States | Non-randomized pre-post trial | 34 | Adolescents and young adults who self-report symptoms of depression and anxiety | Built network/blog |
| Ludwig | 2019 | United States | Non-randomized pre-post trial | 26 | Young people with schizophrenia spectrum disorder | Built network/MOST |
| Alvarez-Jimenez | 2018 | Australia | Uncontrolled pilot study | 14 | Young people at ultra-high risk for psychosis | Built network/MOST |
| Rice | 2018 | Australia | Non-randomized pre-post trial | 42 | Young people with depression | Built network/MOST |
| McEnery | 2019 | Australia | Non-randomized pre-post trial | 10 | Youth with first-episode psychosis (FEP) w/ social anxiety | Built network/MOST |
| Alvarez-Jimenez | 2020 | Australia | Uncontrolled, single-group design | 93 | AYAs with mental health conditions | Built network/MOST |
| Bailey | 2020 | Australia | Non-randomized pre-post trial | 20 | Young adult patients w/ recent suicidal ideation | Built network/MOST |
| Rice | 2020 | Australia | Uncontrolled pre-post design | 76 | Young people with social anxiety | Built network/MOST |
After expanding our inclusion criteria as detailed above, we commenced with data extraction from the articles included for review. A pilot was run on an initial sample of 3 studies to ensure agreement among extractors, resulting in refinement of the extraction table. Extraction was done by two or more reviewers with consensus determined by the first author (KK). Data extraction categories included: (1) type of intervention (clinical/theoretical), (2) intervention components, (3) population studied, (4) intervention duration, (5) primary outcome (mental health condition).
2.1. Study quality
Consistent with the PRISMA-ScR guidelines and the framework proposed by Arksey and O'Malley, a quality appraisal was not conducted (Arksey and O'Malley, 2005; Tricco et al., 2018).
2.2. Data extraction
A qualitative synthesis was completed by study design and intervention characteristics.
3. Results
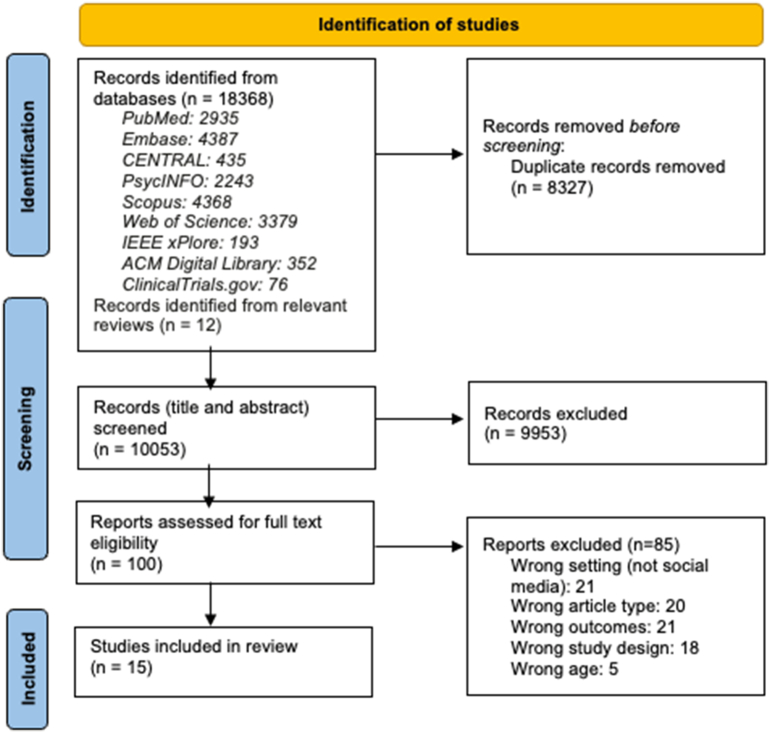
A total of 18,380 references were identified across all databases and bibliographies of identified reviews (18,368 from databases, 12 from reviews). After de-duplication, 10,053 articles remained and were subjected to title and abstract screening, 9953 were excluded, and the full texts of 100 studies were downloaded and screened for inclusion and exclusion. Of these 100 studies, 85 were excluded, leaving 15 articles for this review. Fig. 1 provides an overview of the article selection process.
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
In line with our first objective, we present an overview of empirical research on social media-based interventions in 3.1, 3.2. Due to significant variability in the level of detail study authors included about the interventions, we were unable to conduct a systematic coding of features and functionalities in line with our second objective. Instead, we present a narrative overview of common features in Section 3.3 Features and functionalities.
3.1. Study characteristics
Table 1 presents a general description of studies and is ordered social media platform and year. All studies were published between 2017 and 2021, with the majority based in the US. Samples sizes ranged from small pilot trials (n = 10) to larger scale randomized controlled trials (n = 136). Most studies recruited young people diagnosed with a mental health condition by a clinician or who scored above a clinical threshold on valid clinical measure (Alvarez-Jimenez et al., 2020, Alvarez-Jimenez et al., 2018; Bailey et al., 2020; Ludwig et al., 2021; McEnery et al., 2021; Rice et al., 2020, Rice et al., 2018), with others focused on young people with self-reported mental health conditions (Karim et al., 2021; Radovic et al., 2018; Watkins et al., 2020), a cancer diagnosis (Greer et al., 2019; Pailler et al., 2020), and college students (Asbury et al., 2018; Frith and Loprinzi, 2017; Yu, 2020). The most common study design was non-randomized pre-post trial. Ten studies focused on custom built platforms with social media features, e.g., Moderated Online Social Therapy (MOST) and three purpose-built blogs, whereas Facebook was the most common existing social media site.
3.2. Types of interventions
Table 2 presents a summary of the intervention studies. Notably, five studies were delivered through an existing social media site (Facebook or Pixtori) and the remainder of studies focused on purpose-built networks. This included two studies focused on the SOVA platform, a social media website for young people (Karim et al., 2021; Radovic et al., 2018). Seven studies delivered therapeutic content through the purpose-built MOST framework. In general, interventions ranged in length from 2 to 12 weeks with some having an undefined intervention period with a follow-up assessment (Alvarez-Jimenez et al., 2018; Karim et al., 2021). All studies in the review included a validated mental health measure of depression or anxiety. Other indicators of well-being such as subjective or psychological well-being, perceived stress, quality of life, positive youth development and mechanisms of the social media component including social support and loneliness were also commonly assessed.
Table 2.
Summary of intervention characteristics and findings.
| Author/year | Duration | Theory/model | Characteristics of intervention | Comparison group | Additional support/facilitators | Mental health outcomes | Key findings |
|---|---|---|---|---|---|---|---|
| Firth et al., 2017 | 8 weeks | Wellness intervention informed by transtheoretical model of behavior change. Aimed to increase awareness of specific tools necessary to engage cognitive and behavioral processes of change. | • This intervention involved a private Facebook group that revealed 1–2 new statuses each day for 8 weeks targeting each of the stages of change from the TTM (precontemplation, contemplation, preparation, action, and maintenance). | Static Facebook page (96 statuses were already posted) | NA | Anxiety (OASIS) | • Significant decrease in anxiety in the dynamic FB group from pre to post (p = .003). • Significant group-by time interaction (p = .03). |
| Greer et al., 2019 | 4 weeks | Positive psychology intervention based on broaden and build theory and stress and coping theory. Aimed to deliver cognitive and behavioral skills (e.g., acknowledging positive events, gratitude, positive reappraisal, acts of kindness, mindfulness, personal strengths, attainable goals) to reduce psychosocial distress. | • Vivibot is an automated (decision-tree-based) chatbot delivered via Facebook messenger. • Included seven conversational teaching lessons and seven practice lessons (noticing and acknowledging positive events, savoring positive events, gratitude) repeated 3× to create 28 days of content. • Interactions were dyadic, between participant and bot and included daily emotion ratings, video, survivor material, and periodic check-ins. |
Waitlist control (Access to intervention after 4 weeks) | NA | Depression, Anxiety (PROMIS) | • No significant between group differences on depression (p = .77) or anxiety (p = .09). |
| Watkins et al., 2020 | 5 weeks | Targeted behavioral health intervention informed by social determinants of health, social cognitive theory, and theories of social networking/support. Aimed to promote mental health, progressive definitions of manhood, and social support | • Young Black Men, Masculinities, and Mental Health (YBMen) is social media-based psychoeducation intervention facilitated through private Facebook group. • Included culturally sensitive prompts referencing popular culture to encourage action plans development and promote group problem-solving. • Prompts were delivered via moderators, with facilitated group discussion including content/posts shared daily, likes, social interaction/replies, daily discussion questions. |
NA | Moderator involved in FB group | Depression (PHQ9, GMDS); Secondary: Conformity (CMNI) and Social support (ISEL) | • Significant decrease in depressive symptoms from pre to post via PHQ9 [Pre: 7.55(4.75), Post (PHQ-9): 5.50(4.26)] (p < .01; z = −2.05) and GMDS [Pre: 10.15(6.45), Post: 8.11(6.42)] (p < .05, z = −1.76). |
| Yu et al., 2020 | 2 weeks | Positive psychology interventions based on character strengths and virtue theory, savoring theory, and the “three good things” intervention. Photo intervention aimed to promote emotional sharing, social support, and happiness using self-disclosure. Gratitude intervention aimed to promote the expression of gratitude and to improve emotional status. | • Two Facebook interventions: “Photo diary” group was instructed to take and post photos to exercise strength and virtues. “Expression of gratitude” group was instructed to post a declaration of gratitude to someone on their Facebook wall. • Posting for both groups was meant to occur every 2–3 days, and users could then receive social support and “likes” from their Facebook friends. |
Placebo control (assessment completion, no intervention) | NA | Depression (CES-D) Secondary: Happiness (GHS) | • Significant between group effect on depression for photo group, compared to control (post-test p = .002, 4w follow-up p = .01). • No effect for gratitude group, compared to control (post-test p = .07, follow-up p = .08). • Significant effects at follow-up for happiness in both groups (p = .02; p = .04). |
| Pailler et al., 2020 | 10 weeks | Meaning-based intervention adapted from a manualized meaning-centered psychotherapy intervention. Aimed to help cancer patients sustain and enhance a sense of meaning, purpose, and peace through facilitating social sharing, narrative, and creativity. | • Photographs of Meaning Program for Adolescent and Young Adult cancer patients and survivors (POM-AYA) is delivered through the mobile application, Pixtori. • Included weekly emails or text messages to introduce participants to theme and encourage participation. • Participants posted photos to the cohort portal 2× per week, where they could be viewed and interacted with by others. |
NA | Moderator involved to facilitate engagement (text, email) | Depression (BDI-II) Secondary: Quality of Life (Peds), Spiritual Well-being (FACIT-Sp) | • Significant decrease in depression (p = .02). • Significant increase in quality of life (p = .02). • No effect for spiritual wellbeing (p = .34). |
| Asbury et al., 2018 | 10 weeks | Online journal intervention informed by socioemotional selectivity theory. Aimed to strengthen family connections through supporting self-disclosure of feelings and thoughts about everyday life events. | • FamilyeJournal is purpose-built group journaling platform. • Participants and family members formed a closed group that received weekly prompts from researchers to reflect on thoughts and feelings. Family members could then reply to and comment on participant responses, ideally 3× per week. • Platform revealed responses to prompts after active engagement with prompts to discourage lurking. |
No descriptor | NA | Depression, Anxiety (DASS) | • Significant between group difference for depression, with treatment showing reductions. • No significant difference in anxiety. |
| Radovic et al., 2018 | 6 weeks | Psychoeducation and social support intervention aimed to increase mental health literacy. | • Supporting our valued adolescents (SOVA) is a moderated anonymous blog-based social media website. • Included researcher-developed posts delivering positive content; motivational quotes or videos; psychoeducation on anxiety and depression; mental health resources via website links; question prompts to promote discussion; group sessions; 24/7 moderation. • Participants could respond and comment on peers' posts. |
NA | Site moderation via trained peer moderators and clinical graduate students and clinicians | Depression (PHQ9), Anxiety (SCARD-C) Secondary: Positive Youth Development (PYDSF) | • Significant pre- to post (6 wk) difference in depression (p = .04). • Significant pre- to post (6 wk) difference in PYD (p < .001). • No effect on anxiety (p = .34). |
| Karim et al., 2021 | 3 months | Strengths-based approach focused on self-disclosure, emotion regulation, meaning making and social support, aimed to increase psychological health and positive functioning. | • The SOVA Blogging Ambassador Program is an intervention accompanying SOVA. • Participants create blog posts and share with the online community where they can then receive peer support. • Participants were asked to write one blog post a month and comment at least four times a month on other blog post. |
Natural group comparison (e.g., those who blogged and those who did not) | Site moderation via trained peer moderators and clinical graduate students and clinicians | Depression (PHQ9), Anxiety (SCARD-C) Secondary: self-esteem (RSE), Positive Youth Development (PYD) | • No significant effect for main outcomes depression (p = .41) or anxiety (p = .22). • Significant increase in self-esteem (p = .01, d = 0.45). • Significant increase in PYD (p = .002, d = 0.62) and confidence (p = .002, d = 0.60). |
| Ludwig et al., 2021 | 12 weeks | Positive psychology and mindfulness intervention informed by Cognitive Behavioral Therapy. Aimed to foster social connection and deliver psychoeducation. | • Horyzons is a MOST intervention. • Included psychoeducation modules; Discussion boards e.g., The Café (a wall/newsfeed), Talk-It-Out (a forum to discuss specific issues and go through problem-solving steps), Team Up (personal goal tracking and sharing). • Moderators tailored content through weekly messaging. |
NA | Moderator for supportive accountability and treatment and goal tailoring (clinical, peer) | Depression (BDI-II) Psychotic Symptoms (Positive and Negative Syndrome Scale & Brief Symptom Inventory) Secondary: Psychological Wellbeing | • Improvements in psychosis related symptoms (neg: d = −0.19; pos: −0.03) • Decrease in depressive (d = 0.04) • Increase in psychological well-being (d = 0.011) |
| Alvarez-Jimenez et al., 2018 | 8 weeks | Informed by strengths-based therapy (broaden and build) and self-determination theory. Aimed to improve social functioning. | • MOMENTUM is a MOST intervention. • Included psychoeducation modules; Discussion forums e.g., the Cafe (a wall/newsfeed); Talk-It-Out (a forum to discuss specific issues and go through problem-solving steps); Behavioral tasks (“Do Its”); Peer and expert moderation. • Moderators tailored content through weekly messaging. |
NA | Moderator for supportive accountability and treatment and goal tailoring (clinical, peer) | Depression (MADRS); At risk mental states (CAARMS) Secondary: Subjective well-being (SWLS), Perceived stress (PSS) | • No significant effect for depression. • Significant effects on targets (e.g., mindfulness (p = .04, d = 0.66), strengths use (p = .03, d = 0.70) and social functioning (p < .001, d = 1.83)). |
| Rice et al., 2018 | 12 weeks | Positive psychology, mindfulness, and strength-based intervention designed as a supplement to face-to-face therapy and aimed at relapse prevention through the development of social support and skills. | • Rebound is a MOST intervention. • Included psychoeducation modules; Discussion boards e.g., Talk it Out (a forum for problem-solving); Behavioral tasks (“Actions”) • Moderators tailored content through weekly messaging. |
NA | Moderator for supportive accountability and treatment and goal tailoring (clinical, peer) | Depression (MADRS) Secondary: Functioning (SOFAS), Strength use scale, Social connectedness, Social support, Worry, Anxiety | • Significant decrease in depression scores MADRS (p = .014, d = 0.45). • Nonsignificant increase in strength use (P = .09, d = 0.29). • All other variables not significant. |
| McEnery et al., 2021 | 8 weeks | Informed by integrated CBT model for Social Anxiety Disorder, aimed at psychoeducation and social support for social anxiety. | • EMBRACE is MOST intervention. • Included psychoeducation modules with evidence-based therapeutic content delivered via comics; Discussion board with “talking points”; Behavioral experiments (“Actions”); Peer and expert moderators. • Moderators tailored content through weekly messaging. |
NA | Moderator for supportive accountability and treatment and goal tailoring (clinical, peer) | Social Anxiety (LSAS; SIAS), Depression and Stress (DASS) Secondary: Loneliness (UCLA) | • Significant decrease in social anxiety via SIAS (p = .0005 d = −1.70) and LASA (p = .002, d = −1.35). • No significant effects for depression (p = .50, d = −0.22) or loneliness (p = .48, d = −0.23). |
| Alvarez-Jimenez et al., 2020 | 1–9 weeks | Strengths-based psychosocial intervention meant to be a supplement to face-to-face treatment, aimed at improving conditions for high-risk adolescents. | • MOST+ is an integrated version of the MOST intervention that included real-time clinician delivered web chat counseling. • Included psychoeducation modules with evidence-based therapeutic content delivered via comics; Discussion forums e.g., the Cafe (a wall/newsfeed); Talk-It-Out (a forum to discuss specific issues and go through problem-solving steps); Behavioral tasks (“Do Its”); Peer and expert moderation; on demand web chat with clinicians. • Moderators tailored content through weekly messaging. • Peer-to-peer networking components were enabled only for those with low-risk scores. |
Partial vs full access (full includes peer to peer social networking) | Moderator for supportive accountability and treatment and goal tailoring (clinical, peer); On demand counseling | Depression (PHQ9) Secondary: Psychological Distress (K10); Perceived Stress (PSS); Mental wellbeing (WEMWS) | • Significant decrease in depression (p = .008, d = −0.29). • Significant decrease in psychological distress (p < .001, d = −0.39) and perceived stress (p < .001, d = −0.44). • Significant increase in mental wellbeing (p < .001, d = 0.51). |
| Bailey et al., 2020 | 8 weeks | Cognitive-behavioral intervention informed by the interpersonal theory of suicide. Aimed at providing psychoeducation and exercises related to mindfulness, self-compassion, mental health strengths. | • Affinity is MOST intervention delivered as a supplement to traditional face-to-face treatment. • Included psychoeducation modules with evidence-based therapeutic content delivered via comics; Discussion boards e.g., the Cafe (a wall/newsfeed); Talk-It-Out (a forum to discuss specific issues and go through problem-solving steps); Behavioral tasks (“Do Its”); Peer and expert moderators. • Private direct messaging function between users. |
NA | Moderator for supportive accountability and treatment and goal tailoring (clinical, peer) | Suicidal Ideation (ASIQ), Depression (PHQ9); Secondary: Interpersonal Needs (INQ) | • Significant decrease in suicidal ideation (p = .033, d = −0.57). • Significant decrease in depression (p = .016, d = −0.94). • Significant effects on targets (thwarted belongingness p = .006, =.96; perceived burdensomeness p = .005, d = −0.52). |
| Rice et al., 2020 | 12 weeks | Psychosocial and cognitive behavioral intervention aimed to improve symptoms and promote social connectedness among young people with social anxiety. | • Entourage is a MOST intervention, adapted for young men. • Included psychoeducation modules targeting cognitive strategies with evidence-based therapeutic content delivered via bespoke comics; Discussion boards e.g., the Wall (an open forum); Talking Points (prompts to discuss the symptoms depicted in comics); Talk-It-Out (a forum to discuss specific issues and go through problem-solving steps); Behavioral tasks (“Actions”) • Moderators tailored content through weekly messaging. |
NA | Moderator for supportive accountability and treatment and goal tailoring (clinical, peer) | Depression and suicidality (PHQ9; MDRS), Social Anxiety (LSAS) Secondary: Wellbeing (SWEMWBS) | • Significant decrease in anxiety (p < .001, d = 0.73) • Significant decrease in depression and suicidality (PHQ-9 full scale: p < .001, d = 0.66; suicidality item: p = .026, d = 0.27) • Significant increase in wellbeing (SWEMWBS; p < .001, d = 0.50). |
Note. NA = not applicable; MOST = Moderated Online Support Therapy; CBT = Cognitive Behavioral Therapy.
Of the studies that leveraged an existing social media platform, the features of the platform were most often used to deliver psychoeducational content and encourage cross-dialogue between participants. This included two private Facebook groups (Frith and Loprinzi, 2017; Watkins et al., 2020), one private Pixtori group (Pailler et al., 2020), one intervention facilitated through public Facebook accounts (Yu, 2020) and one intervention that involved chatbot-participant interactions through Facebook messenger (Greer et al., 2019). Of the studies that focused on built platforms, the exchange of moderated social support was common as well as delivery of psychoeducation and prompted reflections. Often interventions delivered content and allowed for interaction in several formats including text, audio, reminders, and graphics.
The degree to which participants received additional support in their use of the social media intervention varied across studies. While some studies involved no researcher and/or clinician support, most involved human support ranging from non-clinical support to increase engagement (e.g., supportive accountability) or risk management to more clinical support including interactions with a clinician and or/moderator to tailor treatment and treatment goals. Several involved light moderation for risk management purposes or to facilitate intervention use, with just over half involving more active moderation with both supportive accountability (engagement) and treatment and goal tailoring.
Interventions differed in their theoretical origins with many based on strengths-based (Alvarez-Jimenez et al., 2018; Bailey et al., 2020; Karim et al., 2021; Ludwig et al., 2021; Radovic et al., 2018; Rice et al., 2018) or positive psychology approaches (Greer et al., 2019; Ludwig et al., 2021; Rice et al., 2018; Yu, 2020), providing psychoeducation and skills/exercises for young people to improve symptoms. Additionally, cognitive-behavioral therapy (Ludwig et al., 2021; McEnery et al., 2021; Rice et al., 2020), and health behavioral models were also common (Frith and Loprinzi, 2017; Watkins et al., 2020).
Although pre-post measurements were commonly used, the small and underpowered sample sizes and exploratory analyses limit the interpretation of results, particularly intervention effectiveness. Twelve studies reported a significant effect on mental health outcomes measured: depression (Alvarez-Jimenez et al., 2020; Bailey et al., 2020; Rice et al., 2020, Rice et al., 2018; Watkins et al., 2020; Yu, 2020), anxiety (Asbury et al., 2018; Frith and Loprinzi, 2017; Ludwig et al., 2021; McEnery et al., 2021; Pailler et al., 2020; Rice et al., 2020), and psychosis (Ludwig et al., 2021), two reported no main effect for a mental health outcome but significant effects on targets or mechanistic outcomes (e.g., mindfulness, social functioning, self-esteem) (Alvarez-Jimenez et al., 2018; Karim et al., 2021). Of the four randomized controlled trials, two reported a significant between group effect on depression (Yu et al., 2020; Asbury et al., 2018), one reported a significant between group difference on anxiety (Firth et al., 2017), and one did not find a significant effect on depression or anxiety (Greer et al., 2019). In this study, Greer et al. note, however, that the reduction in anxiety symptoms was comparable to other psychosocial interventions for people with cancer and that the active control condition appeared to have some benefit.
3.3. Features and functionalities
A number of technical features or functionalities were mentioned across studies, including user-generated posts or content sharing, open forums, prompted (structured) forums, commenting, reactions, private chat, expert moderation, peer moderation, interactive modules, user profiles, tagging capacity, on-demand chat counseling, face-to-face peer meet ups, and chatbots. Prompted forums (n = 13), the ability to post and/or share user-generated content (n = 11), comment on peer posts (n = 11), delivery of content through modules (n = 7), show agreement or support with reactions (n = 7) and create user profiles (n = 5) were most common. In terms of moderation eight interventions involved expert moderation and five had peer moderators. Finally, one intervention each enabled users to interact with peers through private chats, tag content and communicate with an automated chatbot.
4. Discussion
This scoping review identifies empirical studies focused on social media interventions to improve mental health among AYAs. We identified 15 articles – most of which examined the feasibility and acceptability of interventions, rather than intervention efficacy. Consequently, mental health outcomes – such as depression and anxiety – were often assessed in an exploratory manner. We also found that most studies involved purpose-built social media platforms, rather than already existing general purpose (or publicly available) social media, and involved participants who had already contacted, or were receiving, mental health services. We briefly discuss findings corresponding to our two objectives holistically and then highlight opportunities and challenges for future work.
4.1. Intervention commonalities and differences
Across studies, interventions were informed by prior research on social support and expressive writing, targeting mechanisms such as the social sharing of emotions, social connection, and reflection. Social media platforms were primarily used as contexts to deliver psychoeducational and skills-based content, and to promote social support. Though interventions often drew from evidence-based treatments for depression and anxiety including cognitive behavioral therapy, positive psychology interventions, and strengths-based practices, they were eclectic in their approach and did not consistently conform to one treatment approach.
The most common functionality that characterized social media interventions in our review, was that platforms allowed the exchange of user-generated content through forums with varying degrees of structure (e.g., prompted, unprompted). Most interventions utilized multiple channels for interaction and engagement with content. This included being able to post content publicly, comment on other's content, engage with peers or experts (e.g., clinicians/coaches) in private channels (direct messages) as well as “liking” or acknowledging content through a one-click reactions (e.g., likes). However, studies differed in how many channels of interaction they included, with some being structured for a simple back and forth between participants and others involving more complex interactions through interrelated channels such as general discussion boards, task-focused group forums, action-oriented behavioral prompts to facilitate skill building, and psychoeducational content.
Nearly all interventions involved some human support or facilitation from clinicians, clinical researchers, or trained volunteers – though the intensity of this support varied. For example, human support was commonly used to facilitate and moderate peer interactions whereas in structured or purpose-built forums human supporters were used to prompt specific reflections and/or interactions between participants. In some studies, this simply involved researchers posting prompts (See Table 2; e.g., Watkins et al., 2020), while others allowed clinicians or moderators to post content themselves and interact with participants (See Table 2; e.g., Pailler et al., 2020). The MOST interventions often involved one-on-one contact with a clinician as part of the larger intervention program (See Table 2; Radovic et al., 2018; Karim et al., 2021; Ludwig et al., 2021; Rice et al., 2018, Rice et al., 2020; McEnery et al., 2021; Bailey et al., 2020; Alvarez-Jimenez et al., 2018, Alvarez-Jimenez et al., 2020).
When compared to work on digital interventions in other formats we note overlap in the psychotherapeutic approaches or models used, and the tendency to include low-intensity human-support (e.g., moderation, coaching). Additionally, there were significant reductions in mental health symptoms across most studies, with small to moderate effect sizes for the randomized controlled trials, which is consistent with effect sizes reported in meta-analyses of digital interventions (Goldberg et al., 2022; Linardon et al., 2019). Similar challenges are also noted. For example, though Greer et al.'s study did not find a significant effect of the Facebook intervention, effect sizes were comparable to other digital interventions, and the study designed used an active control. Meta-analyses of other digital interventions commonly show diminished intervention effects in studies with active controls (e.g., Firth et al., 2017).
4.2. Opportunities and challenges for future work
Social media platforms are not new; there have been at least 15 years of generative research on these platforms, which have evolved in name and format from web-forums and online communities with limited functionality to social networking sites and now, social media (boyd and Ellison, 2007). Despite this vast literature, our review returned only 15 articles, signaling a dearth in research examining social media-based interventions to prevent and improve mental health. Key opportunities for social media interventions and speculation on possible reasons and challenges for limited work in this domain are presented below.
4.2.1. Leveraging existing peer networks through social media
Though all studies demonstrated innovation in the delivery of mental health interventions to AYAs, surprisingly few studies in our review utilized AYAs existing social media networks, or known peers, as part of the intervention itself. In fact, just two studies did this – one study (Asbury et al., 2018) involved an individual and their close family members in weekly writing prompts via a blog and the other (Yu, 2020) focused on the impact of posting different types of content to a Facebook network. Participants' social contacts may have been infrequently integrated within interventions due to the practical challenges of controlling for existing social network size, activity, and heterogeneity within an individuals' social network. Social media are not closed or siloed environments, but rather are exposed to the same kinds of disturbances, randomness, unseen forces, and variability as the offline world, making it extremely difficult to isolate and reproduce the effects attributable to interventions. The fact that commercial social media platforms are difficult to control for the purposes of intervention development and evaluation, may at least partially explain why there are so many built networks and platforms (e.g., the MOST/MOST+ projects detailed in Table 2) in our sample. Built networks and platforms allow researchers to exert control over aspects of the social media platform itself, enabling them to turn on and off certain features or functionality to examine between-group differences. Dismantling studies in purpose-built spaces may help determine the specific social media features that make the largest contributions to improved mental health outcomes.
There has been some innovation involving existing networks for mental health intervention in the space of suicide prevention (La Sala et al., 2021; Robinson et al., 2018). In this work, youths were involved in co-design workshops to develop messages for use in a suicide prevention campaign. Following this, a 12-week suicide prevention campaign was delivered via direct messages through social media. Participants reported improvements in willingness to intervene if they saw peer posts about suicide, as well as greater self-efficacy and confidence in communicating safely about suicide on social media. Further, Yu (2020) and Asbury et al. (2018) showed preliminary benefits of the interventions and highlight an opportunity to strengthen existing network connections, which may, in turn, support reduced mental health symptom severity over time. Moving forward existing networks may be a potential area of focus.
4.2.2. Efficiently reaching large, diverse populations not involved in treatment
The vast majority of studies focused on treatment-engaged populations, or college-student convenience samples. While this work is valuable and needed, not utilizing social media to reach individuals who are not yet treatment-engaged, and who are from groups typically under-represented in treatment, feels like a missed opportunity. Recent work has shown the ability to efficiently recruit individuals from diverse backgrounds via social media. One recent study of a single session intervention for depression among young people (ages 13–16) recruited over 3800 eligible participants in a matter of 2.5 weeks by advertising via Instagram advertisements, with about 80 % of the adolescents identifying with a sexual minority identity (Schleider et al., 2022). Additionally, a recent Australian-based study examined different recruitment pathways within a small geographic region and found that recruitment for a 4-week transdiagnostic DMH intervention was substantially more efficient via social media, recruiting 1986 eligible individuals relative to 180 eligible individuals recruited via posted advertisements in general practitioners' offices, and 120 recruited via posted advertisements in pharmacies. We believe the success of social media-based recruitment provides some evidence for the potential impact of interventions deployed through these platforms. Further, AYAs are known to spend significant amounts of time on social media sites (Auxier and Anderson, 2021), suggesting interventions deployed within these sites may be more engaging, desirable and can be delivered more seamlessly.
One potential explanation for the focus on treatment-engaged populations in our sample may be that the studies outlined in this review represent early feasibility work in the nascent field of social media based mental health interventions and, therefore, use recruitment and sampling methods that are more conservative than might be used for studies of interventions with more established efficacy (e.g., the broader digital mental health intervention field). Nevertheless, the promise of online recruitment through social media (Smith et al., 2021) underscores the untapped potential of social media to deliver evidence-based interventions for non-treatment-engaged or marginalized populations (Smith et al., 2021).
4.2.3. Deploying individualized and just-in-time interventions
Interventions in this review largely focused on social media as a space to host a group of people and deliver an intervention, rather than as an opportune context for personalized, individual interventions. Despite significant advancement in computational methods and predictive modeling in the social media space, there were no studies in our final sample that leveraged these methodologies to prospectively identify at-risk individuals or proactively deliver targeted interventions. While an often-cited implication of these methodological advances is to use the quantitative power and volume of data from commercial social media platforms to attempt to predict and identify at-risk individuals; predictive modeling is not yet in a place where it can be comfortably and confidently deployed for sophisticated targeted interventions.
The largest barrier, at present, is the lack of construct validity or “ground truth” (Chancellor and De Choudhury, 2020). When computational models use language and interaction patterns, they generally infer risk status, but this inference is often de-coupled from classification data such as diagnostic codes or real-world events such as suicide or self-harm attempts. Therefore, the inferences made by prediction algorithms may not perform well when applied to entire social media platform corpuses. There may also be cultural, linguistic, or other factors that moderate how well classification algorithms are able to perform, e.g., (Reuel et al., 2022). Moreover, computational risk-prediction or classification carries with it inherent harm (Pendse et al., 2022). Recent research raises concerns about the impact of unaccountable actors, privacy violations, and difficult to understand classification algorithms that may amplify existing social stigma and bias (Chancellor et al., 2019). For example, if an algorithm infers a high risk of suicidal behavior based on a social media post, and contacts emergency services for a wellness check, but the emergency service is untrained to handle mental health crises, this well-intended action may endanger the individual who made the post more than a lighter touch intervention. Alternatively, if that wellness check resulted in an unnecessary hospitalization, it may similarly cause direct harm (Ward-Ciesielski and Rizvi, 2021) to the individual as unnecessary psychiatric hospitalization has the potential to be iatrogenic.
In addition to advancement and testing of predictive modeling for mental health, and the development of standards for risk modeling in intervention, it may be worthwhile to consider smaller scale non-automated interventions based on simple decision-tree logic that can provide personalized content for users who opt-in to participation.
4.2.4. Building incentive structures for cross collaboration among social media and academia
To fully integrate mental health interventions in social media spaces, academia-industry partnerships will be needed. We did not see evidence of such partnership in the interventions included in the review and this may be because there is currently little support to modify or manipulate commercial social media platforms' affordances or features as an “outsider” (e.g., there is little research support from social media corporations due to the proprietary nature of their platform features).
Commercial social media companies already actively deploy mental health interventions within their platforms. Specifically, many commercial social media platforms deploy interventions aimed at reducing harm and contagion from posts about self-harm and suicide, sexual assault, eating disorders, and other experiences that may have substantial mental health implications. For example, some platforms provide automated content warnings, privacy screens and warnings when graphic content is described or displayed, and referrals to crisis services or wellness checks on behalf of users (Gomes de Andrade et al., 2018). Unfortunately, due to the proprietary nature of these commercial platforms and the disincentive to partner with academic groups for research, it is not always clear how effective or even acceptable these platform-based interventions are. In some instances, these interventions have received unfavorable reactions from users (Smith and Cipolli, 2022). Moreover these interventions do change behavior, including the way users interact with the platform (Fulcher et al., 2020). Therefore, moving forward there is a need for incentive structures and pathways to productive collaboration among social media/industry partners and clinicians and researchers working in academia. Developing mental health interventions through social media will require user-centered research as well as sustainment plans that fit within social media platforms' existing workflows.
4.2.5. Scaling interventions through social media safely and ethically
Most interventions discussed were designed to reach a target group of recruited participants and were not focused on intervention scalability, though this is one potential benefit to deploying interventions through social media. However, among the most complex challenges raised by this review are the potential ethical dilemmas surfaced by the prospect of social media-based interventions. All mental health interventions have potential side effects or negative consequences (Cuijpers et al., 2018; Mc Glanaghy et al., 2022; Parry et al., 2016). While many interventions have potential benefits that can outweigh potential harms, this is not universally true. Some interventions may actively harm large groups of people while others may generally be beneficial, but harm some individuals or select groups of people based on individual factors (Cuijpers et al., 2018). In the social media environment, the issue of harm or iatrogenic intervention effects is particularly relevant given the heterogeneous user-base and the mere fact that deploying an intervention through these platforms means that it has the potential to reach a large number of people. Despite good intentions, deploying interventions universally to all users at scale is not always appropriate. In fact, there are recent examples of interventions that, when deployed at scale, have performed differently than when evaluated in smaller controlled research settings. In one example a digital suicide prevention intervention that had previously been found to be safe and acceptable at a small scale (Whiteside et al., 2021), was shown to have iatrogenic effects and increase risk of self-harm events when scaled up (Simon et al., 2022). This paradox that what works well for select individuals does not necessarily work well for everyone means that interventions delivered via social media must be rigorously tested before being deployed at scale.
5. Limitations
This study is not without limitations. First, the papers included in this review focused narrowly on a relatively strict definition of social media and research that included a pre-post assessment of a mental health outcome. There may be other interventions that contain social media features or have a social media component that did not end up in our review because it did not include a mental health outcome, and/or the social media component was not described as being a part of the active intervention. Given that most of the included studies were formative and focused on intervention acceptability and feasibility, there are likely to be additional studies not yet ready for outcomes assessment. Relatedly, due to variability in the reporting of social media features we were unable to generate a comprehensive understanding of social components of social media-based interventions to address our section objective. Additionally, following Arksey and O'Malley's (2005) guidance this review did not include a consultation with stakeholders upon completion as recommended by Levac et al. (2010). Finally, due to the rapidly evolving nature of this research space, there is likely merit to building on this review in a shorter timeframe than what is conventional (e.g., 5 years).
6. Conclusion
Social media are used by many adolescents and young adults who experience mental health symptoms. As such, they may be a promising venue to deliver interventions aimed at ameliorating mental health symptoms among populations not yet in contact with mental health services. This scoping review provides an overview of the current state of social media-interventions targeting mental health in adolescents and young adults. Our results show the feasibility and potential for social media to deliver publicly accessible, no cost, mental health interventions, capable of impacting mental health outcomes. They also highlight the challenges inherent in delivering an intervention in a space that is dynamic and constantly evolving in a system that is not currently structured for the types of partnerships needed to properly evaluate and disseminate these interventions. Some challenges that merit further consideration are how to: identify those who are at risk for just-in-time intervention, build incentive structures for cross collaboration among social media and academia, and scale interventions in a way that is safe and ethical. Collectively, the findings from this review highlight innovations in the delivery of mental health interventions, provide preliminary evidence of the ability of social media interventions to improve mental health outcomes, and underscore the need and merit of future work in this area.
Funding
KK KW, JM, and DM were in part supported by grants from the National Institute for Mental Health (T32MH115882, R34MH128410, R43MH124960, and P50MH119029). DWY and MDC were partly supported through NIH grant R01MH117172 to De Choudhury and through a cooperative agreement with Northwell Health.
Declaration of competing interest
David C. Mohr, PhD has accepted honoraria and consulting fees from Otsuka Pharmaceuticals, Optum Behavioral Health, Centerstone Research Institute, and the One Mind Foundation, royalties from Oxford Press, and has an ownership interest in Adaptive Health, Inc. The other authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgements
N/A
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2022.100578.
Appendix A. Supplementary data
Search strategies and terms.
References
- Alvarez-Jimenez M., Gleeson J.F., Bendall S., Penn D.L., Yung A.R., Ryan R.M., Eleftheriadis D., D’Alfonso S., Rice S., Miles C., Russon P., Lederman R., Chambers R., Gonzalez-Blanch C., Lim M.H., Killackey E., McGorry P.D., Nelson B. Enhancing social functioning in young people at ultra high risk (UHR) for psychosis: a pilot study of a novel strengths and mindfulness-based online social therapy. Schizophr. Res. 2018;202:369–377. doi: 10.1016/j.schres.2018.07.022. [DOI] [PubMed] [Google Scholar]
- Alvarez-Jimenez M., Rice S., D’Alfonso S., Leicester S., Bendall S., Pryor I., Russon P., McEnery C., Santesteban-Echarri O., Da Costa G., Gilbertson T., Valentine L., Solves L., Ratheesh A., McGorry P.D., Gleeson J. A novel multimodal digital service (Moderated Online Social Therapy+) for help-seeking young people experiencing mental ill-health: pilot evaluation within a national youth e-mental health service. J. Med. Internet Res. 2020;22 doi: 10.2196/17155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H., O’Malley L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Asbury E.T., Casey J., Desai K. Family eJournal: benefits of online guided group journaling for women. JPMH. 2018;17:135–141. doi: 10.1108/JPMH-01-2018-0008. [DOI] [Google Scholar]
- Auxier B., Anderson M. Pew Research Center: Internet, Science & Tech; 2021. Social Media Use in 2021.https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ URL. (accessed 9.22.21) [Google Scholar]
- Bailey E., Alvarez-Jimenez M., Robinson J., D'Alfonso S., Nedeljkovic M., Davey C.G., Bendall S., Gilbertson T., Phillips J., Bloom L., Nicholls L., Garland N., Cagliarini D., Phelan M., McKechnie B., Mitchell J., Cooke M., Rice S.M. An enhanced social networking intervention for young people with active suicidal ideation: safety, feasibility and acceptability outcomes. IJERPH. 2020;17:2435. doi: 10.3390/ijerph17072435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry N., Lobban F., Belousov M., Emsley R., Nenadic G., Bucci S. #WhyWeTweetMH: understanding why people use Twitter to discuss mental health problems. J. Med. Internet Res. 2017;19 doi: 10.2196/jmir.6173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd Danah M., Ellison N.B. Social network sites: definition, history, and scholarship. J. Comput.-Mediat. Commun. 2007;13:210–230. doi: 10.1111/j.1083-6101.2007.00393.x. [DOI] [Google Scholar]
- Chancellor S., Birnbaum M.L., Caine E.D., Silenzio V.M.B., De Choudhury M. Proceedings of the Conference on Fairness, Accountability, and Transparency. Presented at the FAT* '19: Conference on Fairness, Accountability, and Transparency. ACM; Atlanta GA USA: 2019. A taxonomy of ethical tensions in inferring mental health states from social media; pp. 79–88. [DOI] [Google Scholar]
- Chancellor S., De Choudhury M. Methods in predictive techniques for mental health status on social media: a critical review. npj Digit. Med. 2020;3:43. doi: 10.1038/s41746-020-0233-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P., Reijnders M., Karyotaki E., de Wit L., Ebert D.D. Negative effects of psychotherapies for adult depression: a meta-analysis of deterioration rates. J. Affect. Disord. 2018;239:138–145. doi: 10.1016/j.jad.2018.05.050. [DOI] [PubMed] [Google Scholar]
- Firth J., Torous J., Nicholas J., Carney R., Rosenbaum S., Sarris J. Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. J. Affect. Disord. 2017;218:15–22. doi: 10.1016/j.jad.2017.04.046. [DOI] [PubMed] [Google Scholar]
- Frith E., Loprinzi P. Can Facebook reduce perceived anxiety among college students? Randomized controlled exercise trial using the transtheoretical model of behavior change. JMIR Ment. Health. 2017;4 doi: 10.2196/mental.8086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulcher J.A., Dunbar S., Orlando E., Woodruff S.J., Santarossa S. #selfharn on Instagram: understanding online communities surrounding non-suicidal self-injury through conversations and common properties among authors. Digit.Health. 2020;6 doi: 10.1177/2055207620922389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido S., Millington C., Cheers D., Boydell K., Schubert E., Meade T., Nguyen Q.V. What works and what doesn't work? A systematic review of digital mental health interventions for depression and anxiety in young people. Front. Psychiatry. 2019;10:759. doi: 10.3389/fpsyt.2019.00759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg S.B., Lam S.U., Simonsson O., Torous J., Sun S. Mobile phone-based interventions for mental health: a systematic meta-review of 14 meta-analyses of randomized controlled trials. PLOS Digit.Health. 2022;1(1) doi: 10.1371/journal.pdig.0000002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomes de Andrade N.N., Pawson D., Muriello D., Donahue L., Guadagno J. Ethics and artificial intelligence: suicide prevention on Facebook. Philos. Technol. 2018;31:669–684. doi: 10.1007/s13347-018-0336-0. [DOI] [Google Scholar]
- Greer S., Ramo D., Chang Y.-J., Fu M., Moskowitz J., Haritatos J. Use of the chatbot “Vivibot” to deliver positive psychology skills and promote well-being among young people after cancer treatment: randomized controlled feasibility trial. JMIR Mhealth Uhealth. 2019;7 doi: 10.2196/15018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guntuku S.C., Yaden D.B., Kern M.L., Ungar L.H., Eichstaedt J.C. Detecting depression and mental illness on social media: an integrative review. Curr. Opin. Behav. Sci. 2017;18:43–49. doi: 10.1016/j.cobeha.2017.07.005. [DOI] [Google Scholar]
- Karim S., Hsiung K., Symonds M., Radovic A. Experience of peer bloggers using a social media website for adolescents with depression or anxiety: proof-of-concept study. JMIR Form Res. 2021;5 doi: 10.2196/26183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Sala L., Teh Z., Lamblin M., Rajaram G., Rice S., Hill N.T.M., Thorn P., Krysinska K., Robinson J. Can a social media intervention improve online communication about suicide? A feasibility study examining the acceptability and potential impact of the #chatsafe campaign. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0253278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattie E.G., Adkins E.C., Winquist N., Stiles-Shields C., Wafford Q.E., Graham A.K. Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: systematic review. J. Med. Internet Res. 2019;21 doi: 10.2196/12869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac D., Colquhoun H. Scoping studies: advancing the methodology. O'Brien K.K., editor. Implement. Sci. 2010;5(1):1–9. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon J., Cuijpers P., Carlbring P., Messer M., Fuller-Tyszkiewicz M. The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry. 2019;18(3):325–336. doi: 10.1002/wps.20673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipari R.N., Hedden S., Blau G., Rubenstein L. SAMHSA; 2016. Adolescent Mental Health Service Use and Reasons for Using Services in Specialty, Educational, and General Medical Settings. [PubMed] [Google Scholar]
- Ludwig K.A., Browne J.W., Nagendra A., Gleeson J.F., D’Alfonso S., Penn D.L., Alvarez-Jimenez M. Horyzons USA: a moderated online social intervention for first episode psychosis. Early Interv.Psychiatry. 2021;15:335–343. doi: 10.1111/eip.12947. [DOI] [PubMed] [Google Scholar]
- Mc Glanaghy E., Jackson J., Morris P., Prentice W., Dougall N., Hutton P. Discerning the adverse effects of psychological therapy: consensus between experts by experience and therapists. Clin. Psychol.Psychother. 2022;29:579–589. doi: 10.1002/cpp.2648. [DOI] [PubMed] [Google Scholar]
- McEnery C., Lim M.H., Knowles A., Rice S., Gleeson J., Howell S., Russon P., Miles C., D’Alfonso S., Alvarez-Jimenez M. Social anxiety in young people with first-episode psychosis: pilot study of the EMBRACE moderated online social intervention. Early Interv.Psychiatry. 2021;15:76–86. doi: 10.1111/eip.12912. [DOI] [PubMed] [Google Scholar]
- McKeon G., Papadopoulos E., Firth J., Joshi R., Teasdale S., Newby J., Rosenbaum S. Social media interventions targeting exercise and diet behaviours in people with noncommunicable diseases (NCDs): a systematic review. Internet Interv. 2022;27 doi: 10.1016/j.invent.2022.100497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pailler M.E., Beaupin L.K., Brewer-Spritzer E., Grant P.C., Depner R.M., Levy K., Tenzek K.E. Reaching adolescent and young adult cancer patients through social media: impact of the photographs of meaning program. J.Adolesc.Young Adult Oncol. 2020;9:508–513. doi: 10.1089/jayao.2019.0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry G.D., Crawford M.J., Duggan C. Iatrogenic harm from psychological therapies – time to move on. Br. J. Psychiatry. 2016;208:210–212. doi: 10.1192/bjp.bp.115.163618. [DOI] [PubMed] [Google Scholar]
- Pendse S.R., Nkemelu D., Bidwell N.J., Jadhav S., Pathare S., De Choudhury M., Kumar N. CHI Conference on Human Factors in Computing Systems. Presented at the CHI '22: CHI Conference on Human Factors in Computing Systems, ACM, New Orleans LA USA. 2022. From treatment to healing: envisioning a decolonial digital mental health; pp. 1–23. URL. (accessed 9.22.21) [DOI] [Google Scholar]
- Pretorius C., Chambers D., Coyle D. Young people's online help-seeking and mental health difficulties: systematic narrative review. J. Med. Internet Res. 2019;21 doi: 10.2196/13873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pretorius C., McCashin D., Kavanagh N., Coyle D. Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, CHI '20. Association for Computing Machinery; New York, NY, USA: 2020. Searching for mental health: a mixed-methods study of young people’s online help-seeking; pp. 1–13. URL. (accessed 9.22.21) [DOI] [Google Scholar]
- Radovic A., Gmelin T., Hua J., Long C., Stein B.D., Miller E. Supporting our valued adolescents (SOVA), a social media website for adolescents with depression and/or anxiety: technological feasibility, usability, and acceptability study. JMIR Ment. Health. 2018;5 doi: 10.2196/mental.9441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renn B.N. Vol. 7. 2019. Preference for In-person Psychotherapy Versus Digital Psychotherapy Options for Depression: Survey of Adults in the U.S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuel A.-K., Peralta S., Sedoc J., Sherman G., Ungar L. Findings of the Association for Computational Linguistics: ACL 2022. Presented at the Findings of the Association for Computational Linguistics: ACL 2022. Association for Computational Linguistics; Dublin, Ireland: 2022. Measuring the language of self-disclosure across Corpora; pp. 1035–1047. [DOI] [Google Scholar]
- Rice S., Gleeson J., Davey C., Hetrick S., Parker A., Lederman R., Wadley G., Murray G., Herrman H., Chambers R., Russon P., Miles C., D’Alfonso S., Thurley M., Chinnery G., Gilbertson T., Eleftheriadis D., Barlow E., Cagliarini D., Toh J.-W., McAlpine S., Koval P., Bendall S., Jansen J.E., Hamilton M., McGorry P., Alvarez-Jimenez M. Moderated online social therapy for depression relapse prevention in young people: pilot study of a ‘next generation’ online intervention: online depression relapse prevention. Early Interv.Psychiatry. 2018;12:613–625. doi: 10.1111/eip.12354. [DOI] [PubMed] [Google Scholar]
- Rice S., O’Bree B., Wilson M., McEnery C., Lim M.H., Hamilton M., Gleeson J., Bendall S., D’Alfonso S., Russon P., Valentine L., Cagliarini D., Howell S., Miles C., Pearson M., Nicholls L., Garland N., Mullen E., McGorry P.D., Alvarez-Jimenez M. Leveraging the social network for treatment of social anxiety: pilot study of a youth-specific digital intervention with a focus on engagement of young men. Internet Interv. 2020;20 doi: 10.1016/j.invent.2020.100323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J., Hill N.T.M., Thorn P., Battersby R., Teh Z., Reavley N.J., Pirkis J., Lamblin M., Rice S., Skehan J. The #chatsafe project. Developing guidelines to help young people communicate safely about suicide on social media: a Delphi study. PLOS ONE. 2018;13 doi: 10.1371/journal.pone.0206584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha K., Kim S.C., Reddy M.D., Carter A.J., Sharma E., Haimson O.L., De Choudhury M. The language of LGBTQ+ minority stress experiences on social media. Proc. ACM Hum.-ComputInteract. 2019;3:1–22. doi: 10.1145/3361108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider J.L., Mullarkey M.C., Fox K.R., Dobias M.L., Shroff A., Hart E.A., Roulston C.A. A randomized trial of online single-session interventions for adolescent depression during COVID-19. Nat. Hum. Behav. 2022;6:258–268. doi: 10.1038/s41562-021-01235-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon G.E., Shortreed S.M., Rossom R.C., Beck A., Clarke G.N., Whiteside U., Richards J.E., Penfold R.B., Boggs J.M., Smith J. Effect of offering care management or online dialectical behavior therapy skills training vs usual care on self-harm among adult outpatients with suicidal ideation: a randomized clinical trial. JAMA. 2022;327:630. doi: 10.1001/jama.2022.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith D.M.Y., Lipson S.M., Wang S.B., Fox K.R. Online methods in adolescent self-injury research: challenges and recommendations. J. Clin. Child Adolesc. Psychol. 2021;1–12 doi: 10.1080/15374416.2021.1875325. [DOI] [PubMed] [Google Scholar]
- Smith H., Cipolli W. The Instagram/Facebook ban on graphic self-harm imagery: a sentiment analysis and topic modeling approach. Policy Internet. 2022;14:170–185. doi: 10.1002/poi3.272. [DOI] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2019. National Survey on Drug Use and Health 2019 (NSDUH-2019) [Google Scholar]
- Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., Hempel S., Akl E.A., Chang C., McGowan J., Stewart L., Hartling L., Aldcroft A., Wilson M.G., Garritty C., Lewin S., Godfrey C.M., Macdonald M.T., Langlois E.V., Soares-Weiser K., Moriarty J., Clifford T., Tunçalp Ö., Straus S.E. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Wang Y.-C., Burke M., Kraut R.E. Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing - CSCW '16. Presented at the the 19th ACM Conference. ACM Press; San Francisco, California, USA: 2016. Modeling self-disclosure in social networking sites; pp. 74–85. [DOI] [Google Scholar]
- Ward-Ciesielski E.F., Rizvi S.L. The potential iatrogenic effects of psychiatric hospitalization for suicidal behavior: a critical review and recommendations for research. Clin. Psychol. Sci. Pract. 2021;28:60–71. doi: 10.1111/cpsp.12332. [DOI] [Google Scholar]
- Watkins D.C., Goodwill J.R., Johnson N.C., Casanova A., Wei T., Allen J.O., Williams E.-D.G., Anyiwo N., Jackson Z.A., Talley L.M., Abelson J.M. An online behavioral health intervention promoting mental health, manhood, and social support for young black men: the YBMen project. Am. J. Mens Health. 2020;14 doi: 10.1177/1557988320937215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside U., Richards J., Simon G.E. Brief interventions via electronic health record messaging for population-based suicide prevention: mixed methods pilot study. JMIR Form Res. 2021;5 doi: 10.2196/21127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu S.-C. Does using social network sites reduce depression and promote happiness?: an example of Facebook-based positive interventions. Int. J. Technol. Hum. Interact. 2020;16:56–69. doi: 10.4018/IJTHI.2020070104. [DOI] [Google Scholar]
- Yu S.C., Sheldon K.M., Lan W.P., Chen J.H. Using social network sites to boost savoring: Positive effects on positive emotions. Int. J. Environ. Res. Public Health. 2020;17(17):6407. doi: 10.3390/ijerph17176407. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategies and terms.