Abstract
Intracranial aneurysms are now treatable with coils, stents, and flow diverters in recent years. For saccular aneurysms with broad necks and short domes, stent-assisted coiling has become a common technique, but over time, the complications—both intraprocedural and in a delayed fashion—occur more frequently than coiling alone. Nonstent or balloon-assisted coiling results in lower aneurysm recanalization, lower aneurysm rupture or re-rupture, or lower aneurysm retreatment. This paper illustrates a successful coiling of wide-neck unruptured aneurysm in the trifurcation of the left P2 posterior cerebral artery done without the assistance of stents or balloons.
Keywords: Primary coiling, Wide-neck aneurysm, Unruptured aneurysm, Posterior cerebral artery
Introduction
Brain aneurysm, an abnormal dilatation of cerebral vessels’ anterior wall, is a condition that is estimated to be found in 2.8% of the population. Although aneurysm rupture occurs only in 0.25% of all aneurysms, it can result in stroke or even death [1]. One of the treatment options of brain aneurysm is endovascular treatment which includes coiling. For wide-neck aneurysm, defined as aneurysm neck diameter of 4 mm or greater or dome-to-neck ratio of less than 2, the coiling procedure can be done with the assistance of a balloon or stent to prevent the protrusion of the coil into the parent artery [2]. Balloon- and stent-assisted coiling, unfortunately, are not without any complications, as they may cause thrombus formation and thromboembolic events. In this manuscript, we describe a patient with a wide-neck unruptured aneurysm in the trifurcation of the P2 segment treated with coiling using 3D coils and without assistance of stents or balloons.
Case report
A 28-year-old woman presented with persistent chronic headaches and auditory hallucinations. No hemiparesis was reported. Her laboratory results were normal. The patient had no history of subarachnoid hemorrhage, neurological deficits, hypertension, diabetes mellitus, head trauma, or drug abuse. Her brain MRI showed an incidental finding of an aneurysm in the left posterior circulation (Fig. 1A). From the contrast-enhanced CT angiography, the aneurysm had saccular shape and was in the trifurcation of the left P2 posterior cerebral artery (Fig. 1B).
Fig. 1.
(A) The patient's FLAIR sequence of brain MRI. A saccular flow void is visualized at the left paracistern (red circle); (B) an aneurysm is visualized by CTA at the trifurcation of the left P2 posterior cerebral artery, located at a similar site as the brain MRI (blue arrow).
The patient then underwent a DSA diagnostic examination in a conscious state for measurement and mapping of the aneurysm. An introducer sheath was inserted for the access to the carotid artery. With the help of a guidewire, a vertebral catheter was placed in the internal carotid artery. DSA results showed a wide-neck saccular type aneurysm in the trifurcation of the P2 segment of the left posterior cerebral artery, which branches into the medial inferior temporal artery, posterior inferior temporal artery, and distal branches of P2 posterior cerebral artery (Fig. 2).
Fig. 2.
The same aneurysm, located in the trifurcation of the left P2 posterior cerebral artery, as shown by DSA.
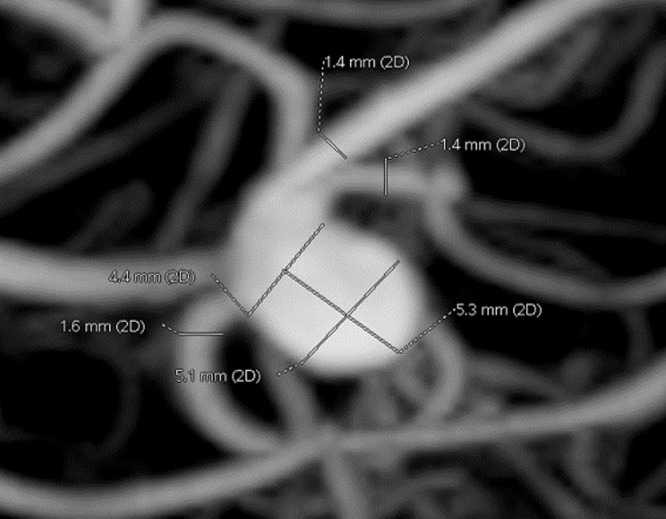
The endovascular coiling procedure was performed under general anesthesia. An angiography catheter was placed in the left vertebral artery, then rotational angiography with 3-dimensional (3D) image reconstruction using Innova 3100 (GE Healthcare, Innova 3100, BUC France) was conducted to establish the aneurysm location and configuration, which eventually determines the procedure plans for the working position. The depth, height, and width of the aneurysm were measured by the 3D reconstructed angiographic images. The diameters of the distal P2 segment and proximal P3 segment of the left posterior artery were approximately 1.6 mm and 1.4 mm, respectively. The aneurysm neck diameter was 4.4 mm, while its dome width and height were approximately 5.1 mm and 5.3 mm, respectively. The dome-to-neck ratio was 1.15 and its aspect ratio was 1.20 (Fig. 3). Based on these measurements, it was found that the dome diameter was greater than the neck diameter. Therefore, 3D coiling was possible without the assistance of stents or balloons.
Fig. 3.
The measurement of the aneurysm's dimensions was done using a 3D image reconstruction of the DSA.
A 6 Fr Fargomax guiding catheter (Balt, France) was placed in the basilar artery and a 1.7 Fr Excelsior SL-10 microcatheter (Stryker, United States), with a Microvention Traxcess 14 EX guidewire (Terumo, Japan) was placed in the left posterior cerebral artery. Coiling was done using 3D Optima Coil System Complex-10 Supersoft 5 mm × 8 cm (Balt, France), 3D ev3 Axium Prime 4 mm × 8 cm (Medtronic, US), 3D Optima Coil System Complex-10 Supersoft 4 mm × 6 cm (Balt, France), Optima Coil System Helical-10 Supersoft 4 mm × 6 cm (Balt, France), and Microvention HydroSoft Helical-10 3 mm × 6 cm (Terumo, Japan) respectively (Fig. 4). After every coiling, a DSA was performed to ensure there was no protrusion into the parent artery. The placement of fully packed coils in the aneurysm sac without any protrusion was shown in the final DSA (Fig. 5). The procedure was successful and did not cause any complications. After the procedure, aspirin (80 mg) and clopidogrel (75 mg) were given orally for 6 months, followed by lifetime aspirin (80 mg).
Fig. 4.
The insertion of coils into the aneurysm. The tip of the microcatheter is positioned in the aneurysm sac at the trifurcation of the left P2 posterior cerebral artery during the insertion of coils.
Fig. 5.
Final DSA after 5 coils were packed into the aneurysm. There is no blood flow into the aneurysm as well as protrusion of coils into the parent artery (white arrow).
Discussion
Optimal management of unruptured aneurysms remains controversial. However, aneurysms’ dimensions smaller than 10 mm are excellent candidates for coiling [2]. The coils will alter the blood flow pattern, which then lead to thrombosis. The decision for coiling is based on aneurysm morphology, aneurysm parent vessel relationship, patient preference, and patient's comorbidities. Wide-neck aneurysms can be coiled with or without the assistance of balloons [3].
In this patient, an aneurysm in the left posterior circulation was incidentally found on brain MRI. Therefore, a CT angiography (CTA) examination was performed to determine the location of the aneurysm. CTA is one of the modalities that can be used for the diagnosis as well as the screening of unruptured aneurysms. The sensitivity ranges from 53% (95% confidence interval [CI], 44%-62%) for 2 mm aneurysms up to 95% (95% CI, 92%-97%) for 7 mm aneurysms, while the overall specificity is around 98.9% (95% CI, 91.5%-99.99%) [4]. This patient was treated because the persistent headaches impaired her quality of life.
A study by Papadopoulos et al. [5] explained potential difficulties during the procedure in relation to aneurysm morphology, such as size and the location of the aneurysms. The usage of stents promotes neointimal growth, leading to progressive aneurysm occlusion. In this case, the coiling was done by adjusting the shape of the aneurysm from 3D image reconstruction. After the procedure, the coil did not obstruct the parent artery.
The aneurysm in this case is treated using 3D coils as they have superiority over helical coils regarding homogenous aneurysm filling because of their conformability. 3D coils are stiffer than helical coils because of their configuration, but they can decrease the recanalization rate of embolized aneurysms, shown by follow-up imaging after 6 months as reported by Lubicz et al. [6].
Several posterior cerebral aneurysm cases have also been reported [7], [8], [9]. In these cases, the aneurysms were treated with a number of modalities, including embolization, coiling, as well as the use of stents and flow diverters. Cases treated with these modalities show favorable outcomes, both clinically and radiologically. However, several complications may arise from the use of the aforementioned modalities to treat posterior cerebral aneurysms, which included stroke and intracranial hemorrhage. To date, no articles were found regarding the use of coiling without stents or balloons to treat posterior cerebral aneurysms.
Primary coiling may pose several complications during or after the procedure. The rate of procedure-related complications ranges from 1% to 19%, with the most common complication being thromboembolic events. Thromboembolic events may occur because of the metal surface of the stents. Several studies, which compared stent-assisted coiling (SAC), coiling alone, and balloon-assisted coiling (BAC), showed similar periprocedural complications. Long-term complications of coiling, such as in-stent stenosis and recanalization after SAC, remain a controversy as reports show a variable rate of complications, with in-stent stenosis ranging from 1.2% to 5.3% and recanalization ranging from 10% to 13.9% [10].
In a meta-analysis study, complications due to SAC and coiling alone were thromboembolism, transient ischemic attack, aneurysm rupture, coil protrusion, coil fracture, and migration of the coil. This study found no significant difference in the occurrence of complications between stent-assisted and coiling alone (17.6% and 15.9%, respectively) [11]. Wang et al compared the outcomes and complications between traditional coiling, SAC, and BAC. Aneurysms treated with stents have better clinical outcomes than traditionally coiled or BAC groups, but no significant differences were found in the rates of complications [12].
Dual antiplatelet therapy using a combination of 80 mg aspirin and 75 mg clopidogrel was given for 6 months after the procedure, followed by a lifelong single antiplatelet. However, evidence regarding the use of antiplatelet for the prevention of thromboembolic events in the coiling procedure of unruptured aneurysms is still limited and there are currently no guidelines that strongly recommend antiplatelet therapy for coiling of unruptured aneurysms [13], [14], [15], [16].
In this case report, the aneurysm was successfully treated by coiling without the assistance of stents or balloons. Coiling itself is still possible if the width of the dome was wider than the neck of the aneurysm as it prevents protrusion of the coil into the parent artery.
Conclusion
Primary coiling of a wide-neck unruptured aneurysm in the trifurcation of the P2 segment of the posterior cerebral artery has been successfully performed. There were no complications reported during and after the procedure. From this case, 3-dimensional coiling without stents or balloons is still possible if the width of the dome of the aneurysm is greater than its neck. This coiling technique may be used as a treatment method for complex aneurysms in the P2 posterior cerebral artery.
Author declaration
Intellectual property
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
Research ethics
Written consent to publish potentially identifying information, such as details or the case and photographs, was obtained from the patient(s) or their legal guardian(s).
Authorship
All listed authors meet the ICMJE criteria. We attest that all authors contributed significantly to the creation of this manuscript, each having fulfilled criteria as established by the ICMJE.
One or more listed authors do(es) not meet the ICMJE criteria.
We believe these individuals should be listed as authors because:
We confirm that the manuscript has been read and approved by all named authors.
We confirm that the order of authors listed in the manuscript has been approved by all named authors.
Contact with the editorial office
The corresponding author declared on the title page of the manuscript is: Prijo Sidipratomo
This author submitted this manuscript using his/her account (ORCID).
We understand that this corresponding author is the sole contact for the editorial process (including ORCID and direct communications with the office). He/she is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs.
We confirm that the email address shown below is accessible by the corresponding author, is the address to which corresponding author's ORCID account is linked, and has been configured to accept email from the editorial office of Radiology Case Reports:
sidipratomo@yahoo.com
We understand that this author is the sole contact for the Editorial process (including ORCID and direct communications with the office). He/she is responsible for communicating with the other authors, including the corresponding author, about progress, submissions of revisions and final approval of proofs.
Patient consent
The authors have obtained consent from the patient for their data, including their medical history and imaging studies, to be published in this case report.
Acknowledgment
The authors thank Komang Shary Karismaputri, MD, Anindyagari, MD, Alvyn Yeremia Pribadi, MD, Albert Novianto, MD, and Rizky Nugroho, MD for their assistance in writing the manuscript.
Footnotes
Competing Interests: We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Funding: No funding was received for this work.
References
- 1.Toth G, Cerejo R. Intracranial aneurysms: review of current science and management. Vasc Med (United Kingdom) 2018;23(3):276–288. doi: 10.1177/1358863X18754693. [DOI] [PubMed] [Google Scholar]
- 2.Tawk RG, Hasan TF, D'Souza CE, Peel JB, Freeman WD. Diagnosis and treatment of unruptured intracranial aneurysms and aneurysmal subarachnoid hemorrhage. Mayo Clin Proc. 2021;96(7):1970–2000. doi: 10.1016/j.mayocp.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Il Jo K, Yang N-R, Jeon P, Kim KH, Hong SC, Kim JS. Treatment outcomes with selective coil embolization for large or giant aneurysms: Prognostic implications of incomplete occlusion. J Korean Neurosurg Soc. 2018;61(1):19–27. doi: 10.3340/jkns.2016.0101.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson BG, Brown RD, Amin-Hanjani S, Broderick JP, Cockroft KM, Connolly ES, et al. Guidelines for the management of patients with unruptured intracranial aneurysms: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2368–2400. doi: 10.1161/STR.0000000000000070. [DOI] [PubMed] [Google Scholar]
- 5.Papadopoulos F, Antonopoulos C, Geroulakos G. Stent-assisted coiling of unruptured intracranial aneurysms with wide neck. Asian J Neurosurg. 2020;15(4):821. doi: 10.4103/ajns.AJNS_57_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lubicz B, Leclerc X, Gauvrit JY, Lejeune JP, Pruvo JP. Three-dimensional packing with complex orbit coils for the endovascular treatment of intracranial aneurysms. 2005;26(6):1342-48. [PMC free article] [PubMed]
- 7.Qin X, Xu F, Maimaiti Y, Zheng Y, Xu B, Leng B, et al. Endovascular treatment of posterior cerebral artery aneurysms: a single center's experience of 55 cases. J Neurosurg. 2017;126(4):1094–1105. doi: 10.3171/2016.1.JNS152447. [DOI] [PubMed] [Google Scholar]
- 8.Bender MT, Colby GP, Jiang B, Lin LM, Campos JK, Xu R, et al. Flow diversion of posterior circulation cerebral aneurysms: a single-institution series of 59 cases. Clin Neurosurg. 2019;84(1):206–216. doi: 10.1093/neuros/nyy076. [DOI] [PubMed] [Google Scholar]
- 9.Maus V, Mpotsaris A, Dorn F, Möhlenbruch M, Borggrefe J, Stavrinou P, et al. The use of flow diverter in ruptured, dissecting intracranial aneurysms of the posterior circulation. World Neurosurg. 2018;111(2018):e424–e433. doi: 10.1016/j.wneu.2017.12.095. [DOI] [PubMed] [Google Scholar]
- 10.Aguilar-Salinas P, Brasiliense LB, Santos R, Cortez GM, Gonsales D, Aghaebrahim A, et al. Safety and efficacy of stent-assisted coiling in the treatment of unruptured wide-necked intracranial aneurysms: a single-center experience. Cureus. 2019;11(6):e4847. doi: 10.7759/cureus.4847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hong Y, Wang YJ, Deng Z, Wu Q, Zhang JM. Stent-assisted coiling versus coiling in treatment of intracranial aneurysm: a systematic review and meta-analysis. PLoS One. 2014;9(1) doi: 10.1371/journal.pone.0082311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang F, Chen X, Wang Y, Bai P, Wang HZ, Sun T, et al. Stent-assisted coiling and balloon-assisted coiling in the management of intracranial aneurysms: a systematic review & meta-analysis. J Neurol Sci. 2016;364:160–166. doi: 10.1016/j.jns.2016.03.041. [DOI] [PubMed] [Google Scholar]
- 13.Li Y, Zhang X, Guo Z, Zhu J, Xu R, He Z, et al. Standard vs. modified antiplatelet therapy based on thromboelastography with platelet mapping for preventing bleeding events in patients undergoing stent-assisted coil for a ruptured intracranial aneurysm. Front Neurol. 2021;11(January):1–9. doi: 10.3389/fneur.2020.615829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hwang G, Huh W, Lee JS, Villavicencio JB, Villamor RBV, Ahn SY, et al. Standard vs modified antiplatelet preparation for preventing thromboembolic events in patients with high on-treatment platelet reactivity undergoing coil embolization for an unruptured intracranial aneurysm: a randomized clinical trial. JAMA Neurol. 2015;72(7):764–772. doi: 10.1001/jamaneurol.2015.0654. [DOI] [PubMed] [Google Scholar]
- 15.Almekhlafi MA, Al Sultan AS, Kuczynski AM, Brinjikji W, Menon BK, Hill MD, et al. Antiplatelet therapy for prevention of thromboembolic complications in coiling-only procedures for unruptured brain aneurysms. J Neurointerv Surg. 2020;12(3):298–302. doi: 10.1136/neurintsurg-2019-015173. [DOI] [PubMed] [Google Scholar]
- 16.Harada K, Kakumoto K, Oshikata S, Uda K, Kajihara M, Higo N, et al. The indication for long-term oral antiplatelet therapy after endovascular embolization of unruptured intracranial aneurysms. J Neurol Res. 2016;6(4):72–80. [Google Scholar]