This case-control study investigates the association between dementia diagnosis and suicide risk.
Key Points
Question
Is there an association between dementia diagnosis and a higher risk of suicide?
Findings
In this nationally representative case-control study including 594 674 persons in England from 2001 through 2019, dementia was found to be associated with increased risk of suicide in specific patient subgroups: those diagnosed before age 65 years (particularly in the 3-month postdiagnostic period), those in the first 3 months after diagnosis, and those with known psychiatric comorbidities.
Meaning
Given the current efforts to improve rates of dementia diagnosis, these findings emphasize the importance of concurrent implementation of suicide risk assessment for the identified high-risk groups.
Abstract
Importance
Patients with dementia may be at an increased suicide risk. Identifying groups at greatest risk of suicide would support targeted risk reduction efforts by clinical dementia services.
Objectives
To examine the association between a dementia diagnosis and suicide risk in the general population and to identify high-risk subgroups.
Design, Setting, and Participants
This was a population-based case-control study in England conducted from January 1, 2001, through December 31, 2019. Data were obtained from multiple linked electronic records from primary care, secondary care, and the Office for National Statistics. Included participants were all patients 15 years or older and registered in the Office for National Statistics in England with a death coded as suicide or open verdict from 2001 to 2019. Up to 40 live control participants per suicide case were randomly matched on primary care practice and suicide date.
Exposures
Patients with codes referring to a dementia diagnosis were identified in primary care and secondary care databases.
Main Outcomes and Measures
Odds ratios (ORs) were estimated using conditional logistic regression and adjusted for sex and age at suicide/index date.
Results
From the total sample of 594 674 patients, 580 159 (97.6%) were controls (median [IQR] age at death, 81.6[72.0-88.4] years; 289 769 male patients [50.0%]), and 14 515 (2.4%) died by suicide (median [IQR] age at death, 47.4 [36.0-59.7] years; 10 850 male patients [74.8%]). Among those who died by suicide, 95 patients (1.9%) had a recorded dementia diagnosis (median [IQR] age at death, 79.5 [67.1-85.5] years; median [IQR] duration of follow-up, 2.3 [1.0-4.4] years). There was no overall significant association between a dementia diagnosis and suicide risk (adjusted OR, 1.05; 95% CI, 0.85-1.29). However, suicide risk was significantly increased in patients diagnosed with dementia before age 65 years (adjusted OR, 2.82; 95% CI, 1.84-4.33), in the first 3 months after diagnosis (adjusted OR, 2.47; 95% CI, 1.49-4.09), and in patients with dementia and psychiatric comorbidity (adjusted OR, 1.52; 95% CI, 1.21-1.93). In patients younger than 65 years and within 3 months of diagnosis, suicide risk was 6.69 times (95% CI, 1.49-30.12) higher than in patients without dementia.
Conclusions and Relevance
Diagnostic and management services for dementia, in both primary and secondary care settings, should target suicide risk assessment to the identified high-risk groups.
Introduction
Risk of death from suicide may be increased after a dementia diagnosis, owing to both the psychological reaction to the diagnosis and the neuropsychiatric phenomenology of dementia syndromes.1,2 However, the relationship between dementia diagnosis and suicide risk has not been clearly demonstrated. For example, 1 cohort study3 in Denmark between 1990 and 2000 reported increased suicide risk in patients with dementia compared with those without dementia whereas a second more recent cohort study4 conducted between 1980 and 2016 demonstrated decreased suicide risk. The hospital-based nature of those studies potentially limits the generalizability of those results to the wider population. Further inconsistency in results was observed from a Korean study5 incorporating both patients with dementia and mild cognitive impairment, which pointed to the absence of a significant association between dementia and suicide risk; the inclusion of mild cognitive impairment may have modified the results.
Specific factors in relation to dementia have been suggested to be potential markers of suicide risk. According to a study6 in Georgia in the US, young age at dementia diagnosis and a recent diagnosis were independent predictors for suicide risk, but the study excluded most patients younger than 65 years. Young-onset dementia was also overlooked in other studies involving patients older than 607 and 658 years, which showed that a recent diagnosis was associated with a high risk of suicide death. Improved understanding of high-risk groups is required to support targeted suicide risk assessment in dementia services, especially in view of policy initiatives designed to deliver higher rates of timely dementia diagnosis.
In order to clarify the association between dementia and suicide risk, we used a large population data set that was able to capture dementia diagnoses from both community and hospital settings, as well as accurate data on causes of death. We hypothesized that relative to the general population, risk of suicide after a dementia diagnosis would be increased among those with young-onset dementia, those in the immediate postdiagnostic period, and those with known psychiatric comorbidities. We also sought to explore for, to our knowledge, the first time, whether acetylcholinesterase inhibitors and memantine might modify suicide risk among patients with dementia, and whether suicide risk was greater among those with unspecified dementia diagnoses, which is a proxy for the quality of diagnostic services.9
Methods
Study Design, Data Source, and Participants
This study was approved by the Medicine and Healthcare Products Regulatory Agency Independent Scientific Advisory Committee (reference number 20_186RA). The requirement for patient informed consent was waived as generic ethics approval is granted for the Clinical Practice Research Datalink (CPRD) database for the examination of deidentified patients in observational research. The study design was a case-control study in England between January 1, 2001, and December 31, 2019, using integrated electronic health records from 3 sources that allowed us to link information from primary care records, secondary care records, and death certificate data: the CPRD, the Hospital Episode Statistics (HES), and the Office for National Statistics (ONS). Covering 6.9% of the UK population and being nationally representative with regard to age, sex, and ethnicity,10 CPRD (both the GOLD and Aurum data sets) was used as the source for primary care records. Ethnicity captured in CPRD is usually self-reported by patients and can be collapsed into the 16 national standard ethnic categories of the 2001 census for England and Wales. In the UK, ethnicity data are mandatory and are collected by official statistics under the Race Relations Act of 1968. Ethnicity records in our study were collapsed into the following ethnic groups: African, Bangladeshi, British, Caribbean, Chinese, Indian, Irish, Pakistani, White and Asian, White and Black African, White and Black Caribbean, other Asian ethnic groups, other Black, other ethnic groups, other mixed ethnicities, and other White. Patients with missing ethnicity records were assigned a missing data value and included in the analysis. HES was used to complement data from secondary care inpatient records in England, and the ONS was used to obtain death records related to suicide in England. The ONS is regarded as the criterion standard for records of cause of death, including for suicide.11 Patients were eligible for inclusion in this study if they had linkable data across all 3 databases and fulfilled the CPRD threshold for data quality: acceptable patient records and up-to-standard general practice records (for CPRD GOLD). We followed the Reporting of Studies Conducted Using Observational Routinely Collected Data (RECORD) guidelines for reporting our study.12
Cases
We included all patients in England from 2001 through 2019 with a cause of death coded as suicide or open verdict (suspicious death of which the cause was not specified by the coroner verdict) in the ONS records who fulfilled the study’s criteria. The inclusion of open verdict is recommended practice in studies of suicide death, as a large majority of open verdicts are attributable to suicide.13 For patients to be included in the study, they had to be at least 15 years old at time of death, have at least 1 year of complete records in CPRD before death, and meet the rest of the study’s eligibility criteria.
Controls
Controls were selected from the same primary care practice as the corresponding patient case, and the selection process was conducted longitudinally over time through matching controls to patient cases on date of suicide death (risk-set sampling). The corresponding matched date of controls is hereafter known as the index date. For every patient who died by suicide, to maximize statistical efficiency, up to 40 live controls were selected from the cohort of individuals who met the study eligibility criteria. We chose a risk-set sampling approach in order that important time-dependent factors (like competing risks and loss to follow-up) were indirectly addressed.14,15 We only included controls who were at least 15 years old at index date and had at least 1 year of complete records in CPRD before the index date.
Exposure
Our exposure of interest was diagnosis of dementia in patients 45 years or older (at younger ages, diagnoses of dementia are likely to represent rare neurometabolic disorders16). We used records from CPRD and HES for codes that refer to a dementia diagnosis at any point in a patient’s clinical history up to the suicide/index date. A full list of dementia terms and codes is available in eAppendix 1 and eTables 1, 2, and 3 in the Supplement, together with data on the accuracy of dementia diagnosis records in CPRD (eTable 4 in the Supplement).17 Patients who were prescribed medications for dementia (donepezil, rivastigmine, galantamine, and memantine) but had no documented dementia diagnosis in either CPRD or HES were included as patients with dementia given that those medications are exclusively indicated for use in dementia.
We also examined suicide risk in patients with dementia by age at diagnosis and recency of diagnosis. For those factors, we obtained records of the earliest ever documented date of dementia diagnosis in either data set (CPRD or HES). We also performed a focused analysis of suicide risk stratified by age at diagnosis (<65 years or ≥65 years). As a proxy for quality of health care, we assessed suicide risk according to whether patients had a specific dementia subtype diagnosed or whether they had unspecified dementia.9 Although unspecified dementia may be applied as an interim diagnosis before dementia subtyping, in those who never receive a clear subtype diagnosis, it reflects a lack of access to appropriate specialist care.18 We therefore defined those who received any subsequent subtype diagnosis as specified dementia and only those who never received a clear dementia subtype diagnosis as unspecified dementia. We collated records from CPRD for the 4 licensed pharmacological treatments for Alzheimer disease (donepezil, rivastigmine, galantamine, and memantine) prescribed at any point up to suicide/index date.
Covariates
Sex and age at suicide/index date were included as covariates in all analyses. Given its strongly nonlinear association with dementia, age (at suicide/index date for cases and controls) was treated as a categorical variable divided into 10 quantiles. Further analysis included the presence or absence of psychiatric illnesses in patients with dementia. For psychiatric illnesses, we identified records in CPRD and HES of the following psychiatric illnesses: affective disorders; schizophrenia spectrum (and other psychosis); and anxiety, including obsessive-compulsive disorders, personality disorders, eating disorders, sleep disorders, and substance misuse. eAppendix 2 and eTables 5, 6, and 7 in the Supplement contain a full list of terms and codes used for psychiatric illnesses.
Statistical Analysis
Conditional logistic regression was used to estimate odds ratios (ORs). ORs in our study can be interpreted as rate ratios given the risk-set sampling nature of the study.15 Age (at suicide/index date for cases and controls) was fitted categorically into 10 quantiles in the multivariable model. Interaction with sex and age (at suicide/index date) was assessed using the likelihood ratio test (LRT) by fitting an interaction term. To obtain single P values across categories, the LRT was also used. All P values were 2-sided, and statistical significance was set at P < .05. Data analyses were performed using Stata software, version 17.0 (StataCorp).
Results
Of 70 065 533 patients with available records in CPRD, 23 339 028 patients (33.3%) were eligible for inclusion in our study, and 46 726 505 patients (66.7%) were excluded. As presented in Table 1, there were 594 674 patients in this study. A total of 14 515 patients (2.4%) died by suicide (median [IQR] age at death, 47.4 [36.0-59.7] years; 10 850 male patients [74.8%]; 3665 female patients [25.3%]) and 580 159 patients (97.6%) were controls (median [IQR] age at death, 81.6 [72.0-88.4] years; 289 769 male patients [50.0%]; 290 390 female patients [50.1%]). Of the 14 515 patients who died by suicide analyzed in our study, 14 240 cases (98.1% of cases) had 40 matched controls, and 275 cases (1.9% of cases) had between 9 and 39 matched controls. Patients from all recorded ethnicities were included as follows: Asian (including Bangladeshi, Indian, Pakistani, and other Asian ethnic groups): suicide cases, 300 (2.1%); controls, 21 344 (3.7%); Black (including African, Caribbean, and other Black): suicide cases, 225 (1.6%); controls, 14 856 (2.6%); White (including British, Irish, and other White ethnicities): suicide cases, 10 285 (70.9%); controls, 456 113 (78.6%); missing ethnicity records: suicide cases, 3484 (24%); controls, 76 953 (13.3%); mixed (including White and Asian, White and Black African, White and Black Caribbean, and other mixed ethnicities): suicide cases, 97 (0.7%); controls, 4060 (0.7%); and other ethnicities (including Chinese and other ethnic groups): suicide cases, 124 (0.9%); controls, 6833 (1.2%).
Table 1. Descriptive Statistics for Whole Samplea.
| Characteristic | No. (%) | |||
|---|---|---|---|---|
| Dementia (n = 4940 [0.8%]) | Whole sample (N = 594 674) | |||
| Suicide cases | Control | Suicide cases | Control | |
| All | 95 (1.9) | 4845 (98.1) | 14 515 (2.4) | 580 159 (97.6) |
| Sex | ||||
| Male | 58 (61.1) | 1758 (36.3) | 10 850 (74.8) | 289 769 (50.0) |
| Female | 37 (39.0) | 3087 (63.7) | 3665 (25.3) | 290 390 (50.1) |
| Age at death, median (IQR), yb | 79.5 (67.1-85.5) | 87.9 (82.6-92.3)c | 47.4 (36.0-59.7) | 81.6 (72.0-88.4)d |
| Age at diagnosis, median (IQR), y | 76.1 (65.4-82.6) | 80.5 (74.8-85.9) | NA | NA |
Abbreviation: NA, not applicable.
In patients with dementia and in the whole study sample, P values were all <.001 for differences in median age at death between those who died by suicide and those who died of other causes according to the Mann-Whitney U test.
Mortality data for those who did not die by suicide (controls) but died of other causes were based on death records from the Clinical Practice Research Datalink.
A total of 2281 of 4940 patients (46.17%) with dementia have death records from causes other than suicide.
A total of 49 920 of 580 159 control participants (8.6%) have death history from causes other than suicide.
Figure 1 depicts our sampling process. In total, there were 4940 patients identified with a dementia diagnosis (median [IQR] duration of follow-up, 2.3 [1.0-4.4] years; 8869 male patients [61.1%]) of whom 95 patients (1.9% of patients with dementia) had died by suicide. Patients with dementia who died by suicide had a median (IQR) age at death of 79.5 (67.1-85.5) years, which was significantly younger than the median (IQR) age of death of patients with dementia who died of causes other than suicide (87.9 [82.6-92.3] years). Patients with dementia who died by suicide also had a significantly younger age at diagnosis (median [IQR], 76.1 [65.4-82.6] years) compared with the age at diagnosis of patients with dementia who died of other causes (median [IQR], 80.5 [74.8-85.9] years).
Figure 1. Flowchart Demonstrating the Sampling Process Using Both CPRD (Clinical Practice Research Datalink) GOLD and Aurum Data Sets.
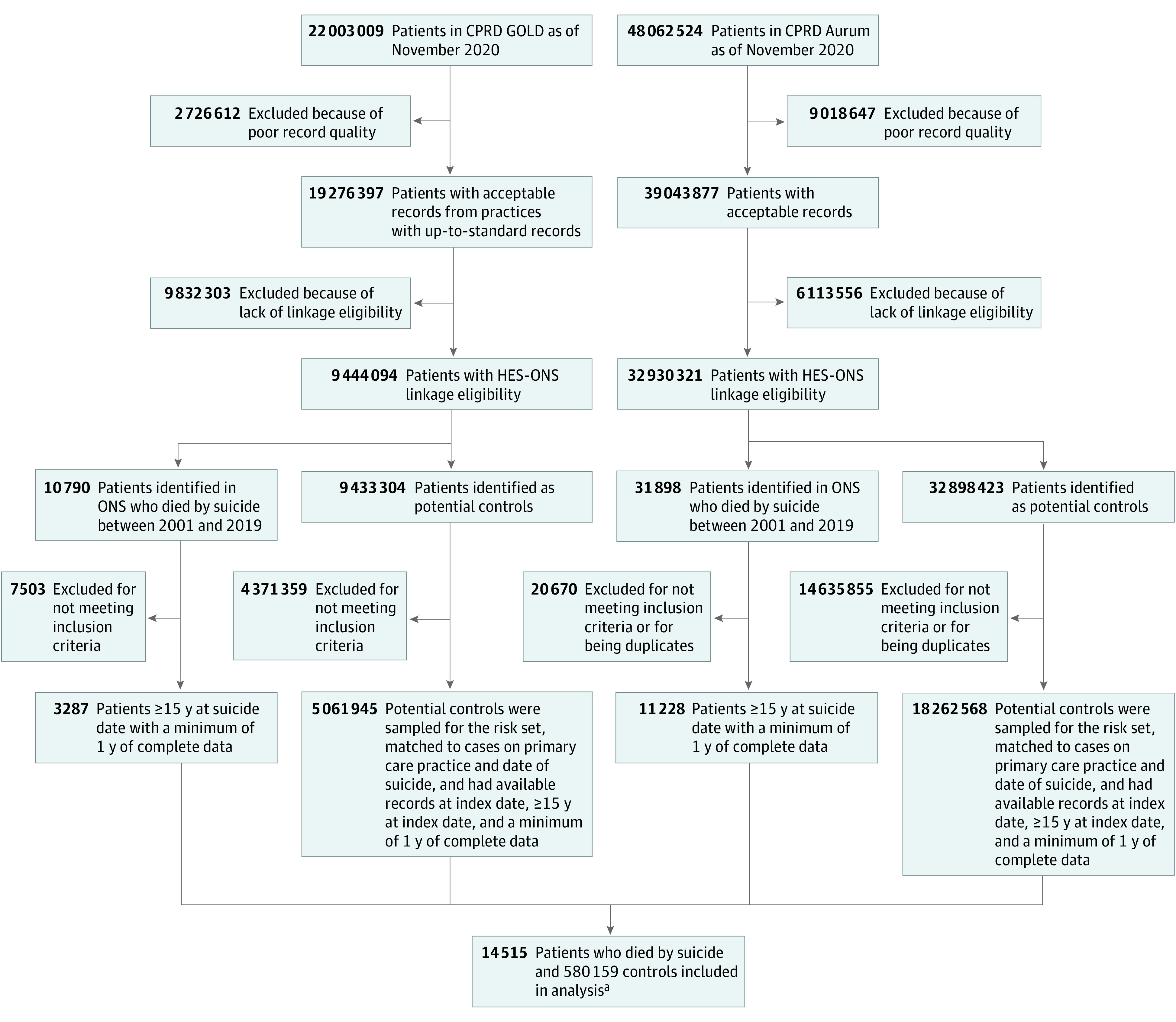
HES indicates Hospital Episode Statistics; ONS, Office for National Statistics.
aEach patient who died by suicide had 40 matched controls except for 275 patients, who had between 9 and 39 matched controls.
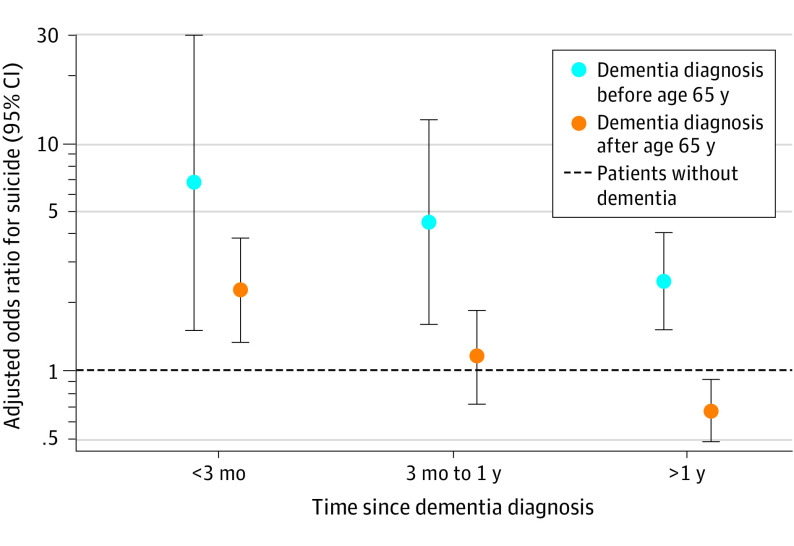
Risk of suicide according to different dementia characteristics is shown in Table 2 and Figure 2. There was overall no significant association between a dementia diagnosis and suicide risk (adjusted OR, 1.05; 95% CI, 0.85-1.29). However, compared with patients without a dementia diagnosis, patients who were diagnosed with dementia before the age of 65 years and patients who were within 3 months of receiving a dementia diagnosis were at 2.82 times (95% CI, 1.84-4.33) and 2.47 times (95% CI, 1.49-4.09) increased risk of suicide after adjusting for age and sex, respectively. In patients diagnosed with dementia before the age of 65 years, suicide risk was greatest in the first 3 months after a diagnosis (adjusted OR, 6.69; 95% CI, 1.49-30.12) and remained significantly increased even after 1 year of diagnosis (adjusted OR, 2.45; 95% CI, 1.50-4.02) compared with patients without a dementia diagnosis. In patients diagnosed with dementia at or after the age of 65 years, suicide risk was also significantly increased in the first 3 months after diagnosis (adjusted OR, 2.25; 95% CI, 1.31-3.86); however, the risk diminished after 1 year of diagnosis (adjusted OR, 0.66; 95% CI, 0.48-0.90). Figure 2 is a visual representation of the relative risk of suicide among those diagnosed with dementia before and after the age of 65 years relative to those without dementia in the 3 epochs after diagnosis.
Table 2. Relative Risk of Suicide in Patients With a Diagnosis of Dementia.
| Characteristic | Adjusted odds ratio (95% CI)a | P valueb |
|---|---|---|
| Dementia—whole sample | ||
| No dementia diagnosis | 1 [Reference] | .67 |
| Dementia diagnosis | 1.05 (0.85-1.29) | |
| Age at dementia diagnosis, y | ||
| No dementia diagnosis | 1 [Reference] | <.001 |
| 45 to <65 | 2.82 (1.84-4.33) | |
| 65 to <85 | 0.99 (0.76-1.30) | |
| 85+ | 0.56 (0.33-0.95) | |
| Recency of dementia diagnosis (nonoverlapping periods) | ||
| No dementia diagnosis | 1 [Reference] | .002 |
| 0 up to <3 mo | 2.47 (1.49-4.09) | |
| 3 mo to <1 y | 1.34 (0.87-2.08) | |
| 1 y+ | 0.84 (0.64-1.10) | |
| Age <65 y and recency of diagnosis | ||
| No dementia diagnosis | 1 [Reference] | <.001 |
| 0 up to <3 mo | 6.69 (1.49-30.12) | |
| 3 mo to <1 y | 4.50 (1.58-12.80) | |
| 1 y+ | 2.45 (1.50-4.02) | |
| Age ≥65 y and recency of diagnosis | ||
| No dementia diagnosis | 1 [Reference] | .04 |
| 0 up to <3 mo | 2.25 (1.31-3.86) | |
| 3 mo to <1 y | 1.14 (0.70-1.85) | |
| 1 y+ | 0.66 (0.48-0.90) | |
| Status of psychiatric diagnosis | ||
| No dementia diagnosis | 1 [Reference] | <.001 |
| Dementia without psychiatric diagnosis | 0.48 (0.31-0.74) | |
| Dementia with psychiatric diagnosis | 1.52 (1.21-1.93) | |
| Dementia specification | ||
| No dementia diagnosis | 1 [Reference] | .71 |
| Specific dementia diagnosis | 1.00 (0.76-1.31) | |
| Unspecified dementia diagnosis | 1.11 (0.82-1.52) | |
| Status of drugs for dementia | ||
| No dementia diagnosis | 1 [Reference] | .02 |
| Dementia without dementia medications (n = 4523) | 1.11 (0.90-1.37) | |
| Dementia prescribed dementia medications (n = 417) | 0.37 (0.12-1.14) | |
Adjusted for sex and age (at death date for suicide cases and at index date for controls).
P values across categories were tested using the likelihood ratio test.
Figure 2. Risk of Suicide Following Dementia Diagnosis, Stratified by Age at Diagnosis.
The figure shows odds ratios for suicide adjusted for sex and age at suicide/index date separately for those diagnosed with dementia before and after the age of 65 years relative to those without dementia in 3 epochs after diagnosis. The y-axis is displayed on a log scale. Error bars represent 95% CIs.
Relative to patients without dementia, patients with dementia without a psychiatric diagnosis were at a statistically significant lower risk of suicide (adjusted OR, 0.48; 95% CI, 0.31-0.74), whereas patients with both a diagnosis of dementia and a psychiatric comorbidity were at a statistically significant increased risk of suicide (adjusted OR, 1.52; 95% CI, 1.21-1.93). There was no statistically significant association in terms of dementia type specification and suicide risk. There was a 0.37 times reduced risk of suicide among patients who were prescribed medications for Alzheimer disease (95% CI, 0.12-1.14; P = .02 across categories); however, this was imprecisely estimated. There was no evidence of significant interaction with either sex or age (at suicide/index date) in the association between dementia and suicide risk.
Discussion
In this longitudinal, population-based, case-control study in England, results suggest that there was an increased risk of death from suicide associated with dementia in patients diagnosed before the age of 65 years, those with a recent dementia diagnosis (within 3 months), and those with existing diagnoses of psychiatric comorbidities. In particular, there was an association between increased suicide risk in patients who were diagnosed younger than 65 years in the 3-month postdiagnostic period.
The present study corroborates findings from earlier cohort studies that suggested younger age at dementia diagnosis6 and a recent dementia diagnosis7,8 as predictors for increased suicide risk. There could be several possible explanations as to why younger patients with dementia were affected by their diagnosis more than older age groups. The relative rarity and unexpectedness of the diagnosis in younger patients can possibly make the acceptance of and adjustment to the condition by younger age groups more difficult. Additionally, younger patients, more than older patients, with dementia may forecast worse outcomes of their disorder in relation to their life expectancy; they may perceive that they will live long enough to progressively experience the most severe form of the disorder. As explained by the interpersonal theory of suicide, perceived burdensomeness is a critical pillar for suicidal behavior19; that perception of burdensomeness may be higher in younger patients with dementia who are more likely to be in their work productive years as well as have family-caring responsibilities. Time since diagnosis is an important marker for suicide risk and the immediate period after being diagnosed appears to be particularly devastating for patients with early-onset dementia. This period is therefore critical for suicide risk assessment and prevention.
Another key factor contributing to suicidal behavior discussed by the interpersonal theory of suicide is the ability to engage in that behavior.19 This factor could in part explain the high suicide risk observed in patients with a recent dementia diagnosis. A recent diagnosis could reflect the stage of the disorder in which patients are conscious of the deficit as well as having the functional and cognitive capabilities to plan and execute suicide. There is, however, no consensus in the literature over the definition of a recent diagnosis of dementia nor the period during which the patient remains at high risk of suicide. Based on case reports, the period between dementia diagnosis and death of suicide ranged from several weeks20 to 2 to 3 years after diagnosis.21,22,23 In a Danish cohort study,3 suicide risk was documented to be highest in the first 6 months after hospital-diagnosed dementia, and in another national study in the US,8 suicide risk in older populations (≥65 years) was highest in the first 3 months postdiagnosis period. Nonetheless, given the high risk of both suicide attempt24 and suicide death associated with a recent dementia diagnosis, we suggest that the current efforts for prompt dementia diagnosis should be accompanied by suicide risk assessment measures focused on the period immediately after diagnosis and in those with young-onset dementia.
The presence of psychiatric illnesses is an important determinant of suicide risk in patients with dementia. With our current analysis, we do not know whether psychiatric illnesses played a role predominantly as a risk factor for both dementia25,26 and suicide27,28 or were a mediator in the association between dementia and suicide risk, or perhaps both. As potentially modifiable risk factors, screening and management of psychiatric illnesses in patients with dementia may help mitigate the increased suicide risk. Although we were unable to confirm an association between prescribing of pharmacological treatments for dementia and suicide risk, the statistical significance across strata may be related to a potential protective effect by these medications and/or by the social support and quality of care linked with the prescription of these medications.
Strengths and Limitations
There were several strengths in this study. To our knowledge, this was the first large population-based study in England that assessed the relative risk of suicide in patients with dementia. The analysis of a large nationally representative sample allows the generalizability of results to England’s population. Furthermore, using multiple integrated electronic databases created an optimal data set to test the hypotheses of interest. In England, primary care records are the main data repository for each patient, and a diagnosis of dementia would usually be recorded here after diagnosis by a specialist. The confidence in the specificity of a diagnosis of dementia in primary care was confirmed in previous research17; accuracy of these records was optimized further by additional ascertainment of records from secondary care data.29,30 The ability to link these with accurate causes of death from ONS data means that the combined data set here was likely to have ascertained both exposure and outcome more accurately and completely than in any previous study addressing suicide risk in dementia.
Nevertheless, we acknowledge that there were important limitations in this study. Despite the large sample size, the number of patients with a dementia diagnosis who had died of suicide was small, meaning that some of the subgroup analyses were imprecisely estimated. As a result, we were unable to meaningfully analyze whether specific dementia syndromes were more associated with suicide risk, as highlighted in other studies.31,32 We also lacked data to assess suicide risk in relation to other relevant information, such as the stage of dementia and the type and source of social care provided to patients with dementia.
Conclusions
Findings from this case-control study suggest that dementia was associated with increased risk of suicide in specific patient subgroups. These results have important implications for dementia screening and management and for suicide prevention, both within specialist dementia services and primary care settings. Based on our results, we suggest that the current efforts for timely dementia diagnosis take place hand in hand with robust risk assessment and support, in particular targeting patients with dementia who are most vulnerable to suicide. These include patients diagnosed before the age of 65 years (especially in the immediate postdiagnostic period), patients who have been recently diagnosed, and patients with a diagnosis of psychiatric illness.
eAppendix 1. Records of Dementia
eTable 1. Read Terms and Codes for Dementia diagnosis in CPRD GOLD
eTable 2. Medical Code IDs and Terms for Dementia Diagnosis in CPRD Aurum
eTable 3. ICD-10 Codes and Terms Used for Dementia Diagnosis in HES
eTable 4. Validity of Dementia Diagnoses in Clinical Practice Research Datalink
eAppendix 2. Records of Psychiatric Illnesses
eTable 5. Read Terms and Codes Used for Identifying Psychiatric Illnesses in CPRD GOLD
eTable 6. Medical Code IDs and Terms Used for Identifying Psychiatric Illnesses in CPRD Aurum
eTable 7. ICD-10 Codes and Categories Used for Identifying Psychiatric Illnesses in HES
References
- 1.Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA. 2002;288(12):1475-1483. doi: 10.1001/jama.288.12.1475 [DOI] [PubMed] [Google Scholar]
- 2.Ferreira MDC, Abreu MJ, Machado C, Santos B, Machado Á, Costa AS. Neuropsychiatric profile in early vs late-onset Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2018;33(2):93-99. doi: 10.1177/1533317517744061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Erlangsen A, Zarit SH, Conwell Y. Hospital-diagnosed dementia and suicide: a longitudinal study using prospective, nationwide register data. Am J Geriatr Psychiatry. 2008;16(3):220-228. doi: 10.1097/01.JGP.0000302930.75387.7e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erlangsen A, Stenager E, Conwell Y, et al. Association between neurological disorders and death by suicide in Denmark. JAMA. 2020;323(5):444-454. doi: 10.1001/jama.2019.21834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.An JH, Lee KE, Jeon HJ, Son SJ, Kim SY, Hong JP. Risk of suicide and accidental deaths among elderly patients with cognitive impairment. Alzheimers Res Ther. 2019;11(1):32. doi: 10.1186/s13195-019-0488-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Annor FB, Bayakly RA, Morrison RA, et al. Suicide among persons with dementia, Georgia, 2013-2016. J Geriatr Psychiatry Neurol. 2019;32(1):31-39. doi: 10.1177/0891988718814363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi JW, Lee KS, Han E. Suicide risk within 1 year of dementia diagnosis in older adults: a nationwide retrospective cohort study. J Psychiatry Neurosci. 2021;46(1):E119-E127. doi: 10.1503/jpn.190219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmutte T, Olfson M, Maust DT, Xie M, Marcus SC. Suicide risk in first year after dementia diagnosis in older adults. Alzheimers Dement. 2022;18(2):262-271. doi: 10.1002/alz.12390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jitlal M, Amirthalingam GNK, Karania T, et al. The influence of socioeconomic deprivation on dementia mortality, age at death, and quality of diagnosis: a nationwide death records study in England and Wales 2001–2017. J Alzheimers Dis. 2021;81(1):321-328. doi: 10.3233/JAD-210089 [DOI] [PubMed] [Google Scholar]
- 10.Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol. 2015;44(3):827-836. doi: 10.1093/ije/dyv098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas KH, Davies N, Metcalfe C, Windmeijer F, Martin RM, Gunnell D. Validation of suicide and self-harm records in the Clinical Practice Research Datalink. Br J Clin Pharmacol. 2013;76(1):145-157. doi: 10.1111/bcp.12059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Benchimol EI, Smeeth L, Guttmann A, et al. ; RECORD Working Committee . The Reporting of Studies Conducted Using Observational Routinely Collected Health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Linsley KR, Schapira K, Kelly TP. Open verdict vs suicide—importance to research. Br J Psychiatry. 2001;178(5):465-468. doi: 10.1192/bjp.178.5.465 [DOI] [PubMed] [Google Scholar]
- 14.Essebag V, Platt RW, Abrahamowicz M, Pilote L. Comparison of nested case-control and survival analysis methodologies for analysis of time-dependent exposure. BMC Med Res Methodol. 2005;5(1):5. doi: 10.1186/1471-2288-5-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed. Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 16.Sampson EL, Warren JD, Rossor MN. Young-onset dementia. Postgrad Med J. 2004;80(941):125-139. doi: 10.1136/pgmj.2003.011171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker VM, Davies NM, Kehoe PG, Martin RM. What is the impact of regulatory guidance and expiry of drug patents on dementia drug prescriptions in England? a trend analysis in the Clinical Practice Research Datalink. Alzheimers Res Ther. 2018;10(1):51. doi: 10.1186/s13195-018-0379-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drabo EF, Barthold D, Joyce G, Ferido P, Chang Chui H, Zissimopoulos J. Longitudinal analysis of dementia diagnosis and specialty care among racially diverse Medicare beneficiaries. Alzheimers Dement. 2019;15(11):1402-1411. doi: 10.1016/j.jalz.2019.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE Jr. The interpersonal theory of suicide. Psychol Rev. 2010;117(2):575-600. doi: 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Margo GM, Finkel JA. Early dementia as a risk factor for suicide. Hosp Community Psychiatry. 1990;41(6):676-678. doi: 10.1176/ps.41.6.676 [DOI] [PubMed] [Google Scholar]
- 21.Ferris SH, Hofeldt GT, Carbone G, Masciandaro P, Troetel WM, Imbimbo BP. Suicide in 2 patients with a diagnosis of probable Alzheimer disease. Alzheimer Dis Assoc Disord. 1999;13(2):88-90. doi: 10.1097/00002093-199904000-00005 [DOI] [PubMed] [Google Scholar]
- 22.Vega U, Kishikawa Y, Ricanati E, Friedland RP. Suicide and Alzheimer disease. Am J Geriatr Psychiatry. 2002;10(4):484-485. [PubMed] [Google Scholar]
- 23.Lim WS, Rubin EH, Coats M, Morris JC. Early-stage Alzheimer disease represents increased suicidal risk in relation to later stages. Alzheimer Dis Assoc Disord. 2005;19(4):214-219. doi: 10.1097/01.wad.0000189051.48688.ed [DOI] [PubMed] [Google Scholar]
- 24.Günak MM, Barnes DE, Yaffe K, Li Y, Byers AL. Risk of suicide attempt in patients with recent diagnosis of mild cognitive impairment or dementia. JAMA Psychiatry. 2021;78(6):659-666. doi: 10.1001/jamapsychiatry.2021.0150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Onyike CU. Psychiatric aspects of dementia. Continuum (Minneap Minn). 2016;22(2 Dementia):600-614. doi: 10.1212/CON.0000000000000302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nasisi CR. Dementia: psychosocial/mental health risk factors. J Nurse Pract. 2020;16(6):425-427. doi: 10.1016/j.nurpra.2020.03.013 [DOI] [Google Scholar]
- 27.Franklin JC, Ribeiro JD, Fox KR, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull. 2017;143(2):187-232. doi: 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization . Preventing Suicide: A Global Imperative. World Health Organization; 2014. [Google Scholar]
- 29.Padmanabhan S, Carty L, Cameron E, Ghosh RE, Williams R, Strongman H. Approach to record linkage of primary care data from Clinical Practice Research Datalink to other health-related patient data: overview and implications. Eur J Epidemiol. 2019;34(1):91-99. doi: 10.1007/s10654-018-0442-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sibbett RA, Russ TC, Deary IJ, Starr JM. Dementia ascertainment using existing data in UK longitudinal and cohort studies: a systematic review of methodology. BMC Psychiatry. 2017;17(1):239. doi: 10.1186/s12888-017-1401-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alothman D, Marshall CR, Tyrrell E, Lewis S, Card T, Fogarty A. Risk of mortality from suicide in patients with Huntington’s disease is increased compared to the general population in England. J Neurol. 2022;269(8):4436-4439. doi: 10.1007/s00415-022-11085-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lai AX, Kaup AR, Yaffe K, Byers AL. High occurrence of psychiatric disorders and suicidal behavior across dementia subtypes. Am J Geriatr Psychiatry. 2018;26(12):1191-1201. doi: 10.1016/j.jagp.2018.08.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Records of Dementia
eTable 1. Read Terms and Codes for Dementia diagnosis in CPRD GOLD
eTable 2. Medical Code IDs and Terms for Dementia Diagnosis in CPRD Aurum
eTable 3. ICD-10 Codes and Terms Used for Dementia Diagnosis in HES
eTable 4. Validity of Dementia Diagnoses in Clinical Practice Research Datalink
eAppendix 2. Records of Psychiatric Illnesses
eTable 5. Read Terms and Codes Used for Identifying Psychiatric Illnesses in CPRD GOLD
eTable 6. Medical Code IDs and Terms Used for Identifying Psychiatric Illnesses in CPRD Aurum
eTable 7. ICD-10 Codes and Categories Used for Identifying Psychiatric Illnesses in HES