Abstract
Objective
This study is aimed to investigate the clinical outcomes of a novel SSPS for fixation of the comminuted coronoid fracture.
Methods
A retrospective study was carried out in the patients with comminuted fractures of the coronoid treated by SPSS fixation between January 2014 and December 2018. A total of 17 patients (17 sides) was included in our study, including 11 male and six female, with a mean age range from 18 to 60. All cases started to functional rehabilitation immediately after the operation. Clinical outcomes were evaluated both radiographically and functionally at the follow‐up visit, including the elbow instability, range of motion and Mayo elbow performance score (MEPS).
Results
According to the O'Driscoll classification system, there was two side of type 1.2, two of type 2.1, four of type 2.2, three of type 2.3, two of 3.1 and four of type 3.2. The surgery was carried out by Kocher and anteromedial approach in 12 patients, posterior and anteromedial approach in four, anterior approach in one. The average operation time and intraoperative blood loss was 129.41±43.87 min and 115.29±104.65 ml. The median follow‐up time was 9 months (range, 6 to 15 months). The mean flexion, extension, pronation and supination motion was 138.76±8.67 degrees, 20.00±13.58, 82.94±5.32and 74.12±14.39 respectively at final follow up. The mean MEPS score was 89.76±8.46, including 11 excellent, 3 good and 3 fair result. The mean VAS score was 1.94±0.97. The mean union time of coronoid fractures was 2.77±0.31 months according to the established standard of healing. There were no significant differences in clinical outcomes among groups according to the O'Driscoll classification (P > .05) and ligament repair strategy (P > .05). No patient underwent instability or dislocation of the elbow during follow up. There were two cases with mild ulnar nerve symptoms which recovered totally at follow up. Meanwhile, there were three cases with heterotopic ossification of the elbow.
Conclusion
Our findings demonstrated that the SSPS can provide a reliable fixation for the comminuted coronoid fracture with satisfactory clinical outcomes.
Keywords: Coronoid process, Elbow, Fixation, Fracture, Spring plate, Suture
Comminuted coronoid fracture is a challengeable to manage in clinical practice. Herein, a suture‐preset spring plate system (SSPS) is devised and applied to fix the fracture. The hook‐like spring plate combined with the suture provide solid stability for the fracture reduction and its clinical outcomes are investigated.
Introduction
The comminuted fracture of the coronoid process typically occurs in the setting of complex fracture and dislocations. 1 , 2 The restoration or reconstruction of the height and shape of the coronoid process is crucial to the recovery of elbow function. 3 Unfortunately, this fracture is notorious for complications and poor clinical outcomes due to conflicts of elbow stability and early motion. 4 A repair surgery is often required to avoid recurrent instability or dislocation of the elbow which predisposes the patient to posttraumatic arthritis. 5
Some studies have investigated the coronoid fracture pattern and its fixation strategy, which are critical to achieve favorable outcomes. 6 , 7 , 8 , 9 However, the management of these fractures is still difficult to interpret in light of the heterogeneity of injury. The O'Driscoll classification system for coronoid process fracture is based on fracture location and size on computed tomography scans, which helps predict associated injuries and injury mechanism. 9 , 10 As for O'Driscoll type 1 coronoid fractures, the fragment is so large that it can be easily fixed, whereas type 1 and 2 fractures with comminution are difficult to handle. 11 Considering the serious risk of rapid post‐traumatic arthritis with the bony and soft tissue left untreated, the concept of “fracture‐fixation strategy” is stressed. However, the optimal management of the comminuted coronoid fracture remains to be investigated due to its various injury patterns. 12
Nowadays, the best fixation for coronoid fractures is debatable, 13 , 14 and fixation failure often leads to elbow instability, arthritis and stiffness. 15 Generally, the coronoid tip fracture is often treated by reattaching the anterior capsule with nonabsorbable sutures or wire securing through drill‐holes in the fracture bed. 16 Large intact anteromedial facet or base fractures can be fixed with a plate and screws. 17 Recently, arthroscopy‐assisted fixation of the coronoid fracture has been reported in some cases, but comparison studies with other techniques are still lacking. 18 Considering the screw fixation, the from anterior to posterior method showed less displacement than that of from posterior to anterior in a cadaveric study. 19 A previous study showed that the lasso technique was more stable than the suture anchors or screws fixation alone. 20 The suture anchors have a high prevalence of malunion and nonunion complication due to its limited holding strength of the fracture. 21 Further, a biomechanical comparison study of screw osteosynthesis and anatomical plating found that the plate osteosynthesis had better stability for large coronoid shear fractures. 22 However, in cases of coronoid fractures with comminution, the plate or suture could not provide enough stability individually. 6 , 23 Both of them cannot provide three‐dimensional stability of the coronoid fracture fragments. Meanwhile, due to its lack of anatomical shaping, it is easy to break due to its poor anti‐rotation ability during use. 24 , 25 Herein, suture‐preset spring plate system (SSPS) was devised to provide a biomechanically sound fixation to counteract the shear force in comminuted fractures. To the best of our knowledge, no study in the literature has specifically investigated the outcomes of comminuted coronoid fractures treated by such a system.
The present study aims to investigate: (i) whether the SSPS can fixed the comminuted coronoid fracture effectively; (ii) the clinical outcomes and functional recovery of this novel system; and (iii) whether the functional result varied among patients with different fracture subtype and ligament repair strategy. We hypothesized that our SSPS could provide solid fixation of the coronoid fracture and have good clinical results.
Methods
Inclusion and Exclusion Criteria
A retrospective study was carried out on the comminuted coronoid fracture treated by the SSPS fixation between January 2014 to December 2018. The institutional review board of our hospital approved the study (No. IRB‐2020‐133) and informed consent was obtained from each patient. The inclusion criteria were as follows: (i) patients aged over 18 years with comminuted coronoid fracture; (ii) the coronoid fracture was treated by SSPS fixation technique; and (iii) observation and check were followed up more than 6 months with outcome records for all the patients. The exclusion criteria were as follows: (i) open elbow fractures; (ii) pathological facture due to organic lesions; (iii) local infection around the fracture; and (iv) delayed or malunited fractures.
Surgery Process
Preoperative Evaluation
Preoperatively, the elbow fracture of each patient was examined by x‐ray (MULTIX Impact, Siemens, Shanghai, China) and CT (SOMATON Force, Siemens, Shanghai, China) scan to visualize the displacement. Meanwhile, the MRI (MAGNETOM Verio 3.0T, Siemens, Shanghai, China) was carried out to evaluate the ligament injury around the elbow. The coronoid process fracture was classified by the O'Driscoll classification system based on CT scanning. 26 Briefly, the coronoid fractures are divided into the following three types of fractures: tip (type 1); anteromedial facet (type 2); and base of the coronoid process (type 3). 27 Tip fractures were further divided into the subtype 1, involving ≤2 mm of the coronoid (i.e., flake fracture), and subtype 2, involving >2 mm. The anteromedial fractures are in turn divided into three subtypes according to the extent of their involvement of the anteromedial coronoid facet. Subtype 1 fractures affect the rim between the tip and the anterior half of the sublime tubercle; subtype 2 fractures also involve the tip; and subtype 3 fractures involve the whole sublime tubercle as well. The basal fractures are divided into two subtypes. Subtype 1 fractures affect the coronoid body and base; subtype 2 fractures through the body or base of the coronoid also involves a fracture of the olecranon. 28
Anesthesia and Approach
Briefly, the patient was placed in a supine position with the injured extremity supported on a hand table under general or regional anesthesia. Thereafter, a routine disinfection and draping procedure was conducted. The specific surgery approach depended on the coronoid fracture patter and concomitant injury. The anteromedial or basal coronoid fractures were managed with SSPS through an anteromedial approach. Anterior rim or anterolateral fracture was fixed through the anterior approach which elevated the brachialis muscle off its insertion on the proximal ulna.
SSPS Preparation
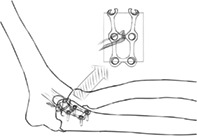
Indications for the SSPS fixation are as follows: (1) comminuted type 1 fracture which contributed to persistent elbow instability if left unfixed intraoperatively; and (2) comminuted type 2 and type 3 fractures. The brief diagram of this technique using SSPS is shown in Fig. 1.The SSPS was designed and prepared as following principles: (i) a single spring plate preset with suture for type 1 fracture; and (ii) a T‐shape plate or two spring plate for type 2 or type 3 fracture. The miniature plate (2 mm size) of the SSPS system was mainly provided by DePuy Synthes (West Chester, PA, USA) and Stryker Medical Technology Co. Ltd (Suzhou, China). The spring plate was made from above miniature plate, of which one terminal hole was cut off partly and the rest stump ends were bent to hook‐like tips as Fig. 2.
Fig. 1.
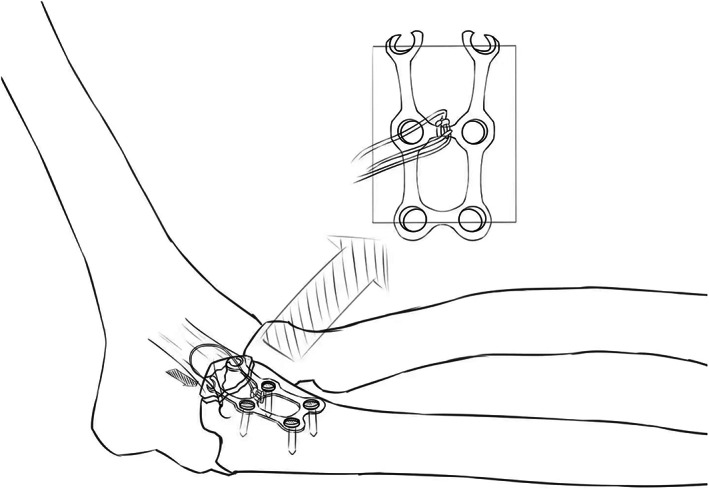
Diagram of the suture‐preset spring plate system (SSPS)
Fig. 2.
Suture‐preset spring plate system (SSPS) preparation intraoperatively. (A) A suture was preset on the miniature plate. (B) A pole at the end of the plate was partly cut off to form hook‐like structure. (C and D) The lateral view of the SSPS
Fracture Reduction and Fixation
After exposure of the coronoid fracture, preliminary reduction with K‐wires was performed and checked on fluoroscopy. Then, the coronoid fracture was fixed definitely with pre‐curved SSPS by 2 mm screws, which produce moderate compression. Prior to definitive closure, elbow stability was then evaluated with the goal being concentric stability with no observed posterior or posterolateral subluxation through a flexion‐extension arc of 30–130° with the forearm in neutral rotation, no valgus or supination stress was added. After that, the comminuted coronoid fractures were buttressed by the spring plate and the anterior capsule was reattached by the preset suture in in flexion of the elbow for convenience. The flexor‐pronator mass was then repaired using sutures (if a split of the flexor‐pronator mass had been performed) or suture anchors (if elevation of the entire flexor‐pronator mass from its origin on the medial epicondyle had been performed). Avulsion of the medial collateral ligament (MCL) from the medial epicondyle was also repaired at the same time if present. After that we performed the varus stress test under fluoroscopy with forearm pronation and checked whether the end point resistance was firm and the lateral radiohumeral joint congruency was maintained. If not, we repaired the lateral ulnar collateral ligament (LUCL) with suture anchor through the lateral approach.
In the setting of a terrible triad injury, the lateral structure was repaired in the first place. After repair, the valgus stress test with forearm supination was performed under fluoroscopy and checked whether the end point resistance was firm and the medial ulnohumeral joint congruency was maintained. If not, we repaired the MCL with suture anchor through the medial approach.
Postoperative Rehabilitation
Post‐operatively, all patients were started on gentle mobilization of the elbow on the first day following surgery, with gradual progression to passive and active‐assisted range of motion exercises as tolerated. Indometacin (25 mg) was given three times a day and lasted for 4 weeks to avoid heterotopic ossification. Active range of motion and strengthening exercises were permitted from the sixth week onwards. We did not routinely use a hinged elbow brace for our patients. The patients were visited and their recovery statuses were checked routinely thereafter for at least for 6 months.
Clinical Indicators
Fracture Union and Elbow Stability
Patients were routinely followed‐up in the outpatient setting with clinical and radiographic evaluation by the senior author at each follow‐up visit. The coronoid fracture union was mainly assessed by computed tomography scanning. In addition, standard antero‐posterior and lateral radiographs of the affected elbow were obtained routinely and used to detect subluxation or dislocation on the lateral view, narrowing of the humero‐ulnar, humero‐radial, or overall joint line. Union was defined as the nontender fracture site in a patient and continuous bridging callus in CT imaging.
Visual Analogue Score
The visual analogue score (VAS) score system used in social and behavioral sciences was adopted to measure the elbow pain. The VAS pain scoring standard (scores from 0 to 10) is as follows: 0 means painless; 1–3 means mild pain that the patient could endure; 4–6 means that patient is in pain that could be endured, but the patient is unable to sleep; and 7–10 means that patient has intense pain and is unable to tolerate the pain.
Elbow Mobility
Postoperative management with regard to the range of motion of the extremity was individualized according to the fracture stability and associated injuries. Range of motion, including elbow flexion, extension, pronation, and supination, was measured with a goniometer by a senior author.
MEPS Score
Functional outcomes were assessed with the Mayo elbow performance (MEP) scores, which graded the extent of elbow pain (range, 0–45), motion (0–20), stability (0–10), and function (0–25). The MEP scores were used to classify patients into different functional categories: excellent (≥90), good (75–89), fair (60–74), and poor (≤60).
Complications
Complications assessed included wound infection, postoperative elbow instability, malunion or non‐union, implant loosening or screw back‐out, re‐fracture, neurologic injury and heterotopic ossification. Elbow osteoarthritis was evaluated by the Broberg and Morrey classification: 0, normal joint with no joint line narrowing; 1, slight joint line narrowing and minimal osteophytosis; 2, moderate joint line narrowing (>50%) and osteophytosis; and 3, severe degenerative changes with gross destruction of the joint.
Statistical Analysis
The SPSS (version 18.0, SPSS Inc., Chicago, IL, USA) was applied to analyze the data in our study. The measurement data such as time from injury to surgery, follow‐up duration, fracture‐union time, range of motion, MEPS score and VAS was described as mean ± SD. The age was recorded as median, minimum and maximum value. The gender, afflicted side, injury patterns, fracture type, ligament repair, satisfaction classification and complications were described as categorical data n (%). Nonparametric Kruskal–Wallis and post hoc Dunn's tests were used to compare clinical outcomes between different O'Driscoll classification groups and ligament repair groups, and to analyze MEPS and VAS scores. P < 0.05 was considered statistically significant.
Results
General Results
A total of 17 patients (17 sides) who underwent SSPS fixation for the comminuted coronoid fracture of the elbow were registered for the study, including 11 males and six females with a median age of 49 years. There were five patients with the coronoid fracture on the left side, and 12 patients on the right side. According to the O'Driscoll classification system, there was two side of type 1.2, two of type 2.1, four of type 2.2, three of type 2.3, two of 3.1 and four of type 3.2. Demographics and details of the patients are summarized in Table 1.
TABLE 1.
Demographic data of patients
| All patients (n = 17) | |
|---|---|
| Age, median, years | 49 |
| Gender, n (%) | |
| Male | 11 (65) |
| Female | 6 (35) |
| Side of injury, n (%) | |
| Left | 5 (29%) |
| Right | 12 (71%) |
| Injury patterns, n (%) | |
| Fall from the ground | 6 (35%) |
| Fall from the height | 2 (12%) |
| Motor accident | 9 (53%) |
| Fracture type, n (%) | |
| O'Driscoll type 1 | 2 (12%) |
| O'Driscoll type 2 | 9 (53%) |
| O'Driscoll type 3 | 6 (35%) |
| TIS, mean (SD), days | 8.71 (3.12) |
| Ligament repair, n (%) | |
| No repair | 2 (12%) |
| MCL | 0 (0%) |
| LCL | 8 (47%) |
| MCL + LCL | 7 (41%) |
Abbreviations: LCL, lateral collateral ligament; MCL, medial collateral ligament; TIS, time from injury to surgery.
Intraoperative Outcomes
The surgery was carried out by Kocher and anteromedial approach in 12 patients, posterior and anteromedial approach in four, anterior approach in one. The average operation time was 129.41 ± 43.87 min, with the longest time of 180 min. The intraoperative blood loss was 115.29 ± 104.65 ml, ranging from 20 to 400 ml.
Clinical Outcomes
Fracture Union and Elbow Stability
All cases started to functional rehabilitation immediately after the operation and no failure of the fixation was found postoperatively. All the patients were followed up successfully with an median follow‐up time of 9 months (range, 6–15 months). The mean union time of the factures was 11.87 ± 1.33 weeks according to the established standard of healing. No patient underwent instability or dislocation of the elbow during follow up. The detailed clinical outcomes is summarized in the Table 2.
TABLE 2.
Results of SSPS fixation
| All patients (n = 17) | |
|---|---|
| Follow‐up time, mean (SD), months | 9.47 (2.55) |
| Fracture union time, mean (SD), weeks | 11.87 (1.33) |
| Total arc, mean (SD) | 118.76 (22.01) |
| Flexion, mean (SD) | 138.76 (8.67) |
| Extension, mean (SD) | 20 (13.58) |
| Forearm pronation, mean (SD) | 82.94 (5.32) |
| Forearm supination, mean (SD) | 74.12 (14.39) |
| MEPS score, mean (SD) | 89.35 (9.35) |
| Satisfaction classification, n (%) | |
| Excellent | 11 (64%) |
| Good | 3 (18%) |
| Fair | 2 (12%) |
| Poor | 1 (6%) |
| Complication, n (%) | |
| UN | 2 (12%) |
| HO | 3 (18%) |
| OA (B–M) | 5 (29%) |
| No | 12 (71%) |
| Grade I | 4 (24%) |
| Grade II | 1 (6%) |
| Grade III | 0 |
| VAS score, mean (SD) | 1.94 (0.97) |
Abbreviations: B–M, Broberg and Morrey classification; HO, heterotopic ossification; MEPS, Mayo elbow performance score; OA, osteoarthritis; SSPS, suture‐preset spring plate system; UN, ulnar neuropathy; VAS, visual analog scale.
Visual Analog Score
The VAS score was 1.94 ± 0.97 at the final follow‐up. There were four non‐specific painful thighs in the first 3 months, which were relieved by an oral analgesic drug. There were no significant differences in VAS scores among groups according to the O'Driscoll classification (P > 0.05) (Table 3) and ligament repair strategy (P > 0.05) (Table 4).
TABLE 3.
Difference in clinical outcomes among the O'Driscoll types (p value)
| Type I vs. type II | Type II vs. type III | Type I vs. type III | |
|---|---|---|---|
| VAS | 0.3504 | 0.1973 | 0.9506 |
| MEPS | 0.6521 | 0.1271 | 0.1566 |
Abbreviations: MEPS, Mayo elbow performance score; VAS, visual analog scale.
TABLE 4.
Difference in clinical outcomes among the subgroups of ligament repair (P value)
| No repair vs. LCL | No repair vs. LCL + MCL | LCL vs. LCL + MCL | |
|---|---|---|---|
| VAS | 0.0914 | 0.1129 | 0.9023 |
| MEPS | 0.1324 | 0.4799 | 0.2286 |
Abbreviations: LCL, lateral collateral ligament; LCL + MCL, medial collateral ligament; MEPS, Mayo elbow performance score; VAS, visual analog scale.
Elbow Mobility
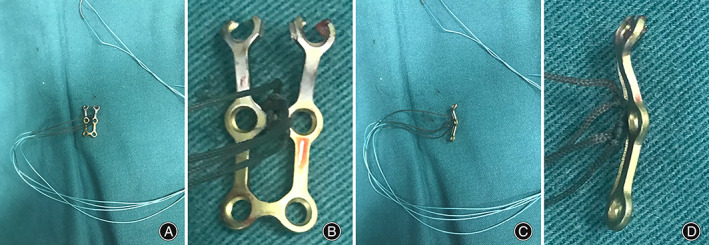
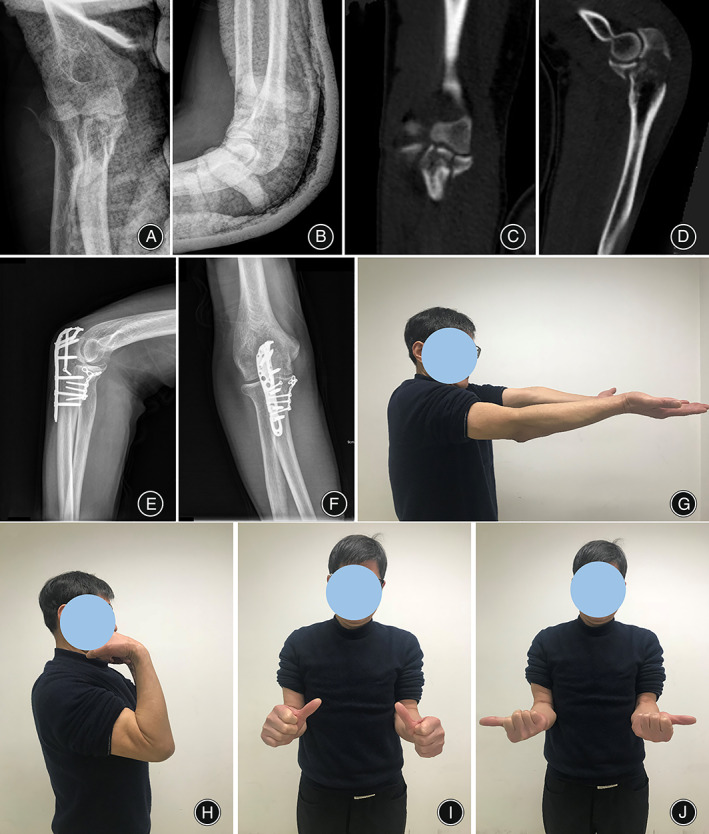
The mean elbow flexion and extension was 138.76 ± 8.67 and 20.00 ± 13.58 degree at the final follow‐up. A mild decrease in extension range of the elbow occurred in most of patients. Figures 3, 4, 5 present three typical cases that show the satisfactory clinical results of this SSPS fixation in different types of O'Driscoll classification.
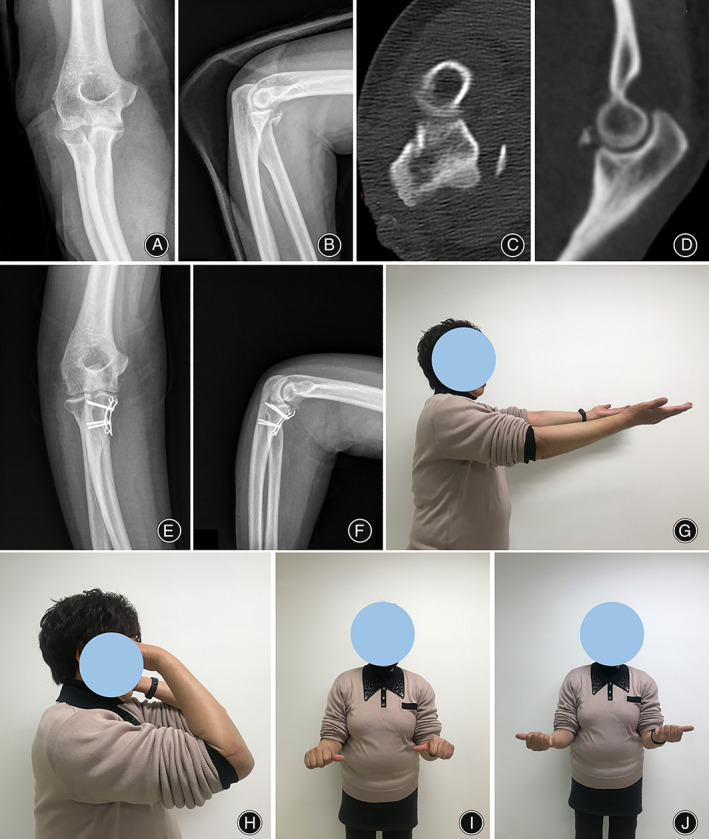
Fig. 3.
A typical case of the O'Driscoll type 1 fracture using suture‐preset spring plate system (SSPS) fixation. The preoperative X‐ray in AP (A) and lateral (B) view showed fracture of the coronoid process tip. (C and D) The fracture was comminuted in CT scan view. The X‐ray in AP (E) and lateral (F) view at 8 months postoperatively. The extension (G), flexion (H), pronation (I) and supination (J) showed good function recovery of the elbow at last follow up
Fig. 4.
A typical case of the O'Driscoll type 2 fracture using SSPS fixation. The preoperative X‐ray in AP (A) and lateral (B) view showed fracture of the tip and anteromedial region of the coronoid process. (C and D) The fracture was comminuted in CT scan view. The X‐ray in AP (E) and lateral (F) view of the fracture at 9 months after the operation. The extension (G), flexion (H), pronation (I) and supination (J) showed good function recovery of the elbow at last follow up
Fig. 5.
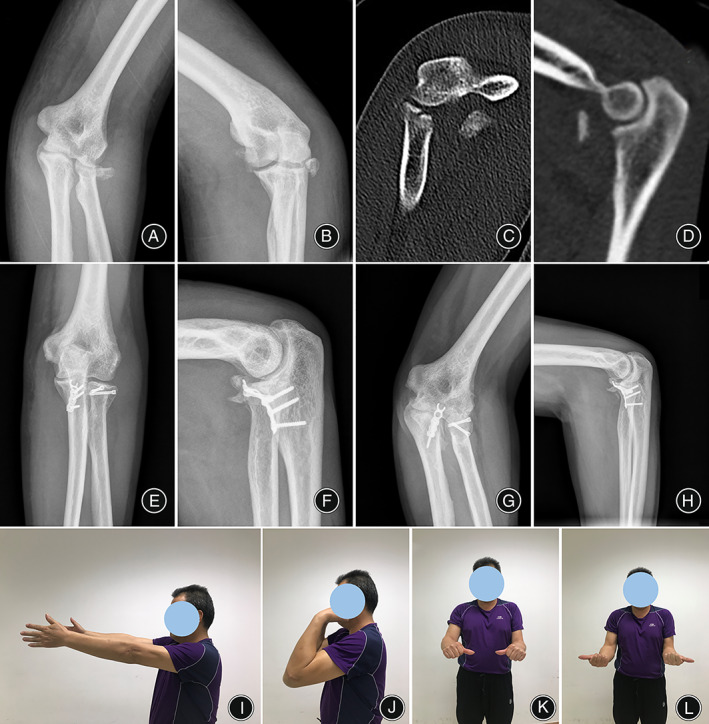
A typical case of the O'Driscoll type 3 fracture using suture‐preset spring plate system (SSPS) fixation. The preoperative X‐ray in AP (A) and lateral (B) view showed trans‐olecranon fracture of the coronoid process. (C and D) The fracture was comminuted in CT scan view. The x‐ray in AP (E) and lateral (F) view showed complete union of the fracture at 6 months after the operation. The x‐ray in AP (G) and lateral (H) view at 12 months postoperatively. The extension (I), flexion (J), pronation (K) and supination (L) showed good function recovery of the elbow at last follow up
MEPS Score
All the patients were satisfied with their improvement, and operation did not affect their work and daily activities. The average MEPS score was 89.35 ± 9.35, with 11 excellent, three good, two fair and one poor. There were no significant differences in MEPS score among groups according to the O'Driscoll classification (P > 0.05) (Table 3) and ligament repair strategy (P > 0.05) (Table 4).
Complications
For all the patients who had the operation, there were no major complications such as infection, compartment syndrome, or vascular complications. There were two cases with mild ulnar nerve symptoms which were treated by neurotrophic drug such as mecobalamin postoperatively and recovered totally at follow up. According to the Broberg–Morrey classification, there were four grade 1 and one grade 2 osteoarthritis in the elbow. There was no malunion or nonunion of the fracture in patients.
Discussion
Nowadays, the comminuted fracture of the coronoid process remains to be an extremely difficult injury to handle in the elbow. 29 It is widely accepted that the coronoid plays a vital role in maintaining the stability of the elbow joint by acting as a buttress against posterior transition and varus rotation of the ulna on the distal humerus. 30 In this study, we devised an SSPS to fix the comminuted coronoid process fracture. Our results indicated that: (i) the SSPS could provide solid fixation for the comminuted coronoid fracture with fine shaping; (ii) the SSPS fixation allows early elbow movement and promotes the fracture union with low complication incidence; and (iii) there are no significant differences in functional recovery among different fracture subtypes and ligament repair strategies.
Capsule Reattachment is Important for Elbow Stability
The optimal treatment for the coronoid fracture varies with the size of the fragment and is still controversial. Transverse fractures of the tip are associated with elbow dislocation and fracture of the radial head and are usually best fixed with a suture lasso using drill holes through the intact ulna. 31 The anatomical studies by Cage et al., Shimura et al. and Ablove et al. have confirmed that no ligaments attach to the tip of the coronoid process. The anterior capsule attachment site was located 2.36–6.4 mm distal to the coronoid tip. Therefore, the main effect of coronoid tip fixation is to reattach the anterior capsule. 9 , 15 , 32 A study by Luokkala et al. involving routine magnetic resonance imaging in patients with elbow dislocation showed that the anterior capsule attachment site was involved in 71% of cases. 33 It was reported that no reattachment of the anterior capsule had a higher risk of humero‐radial osteoarthritis. 34 Meanwhile, internal fixation of the coronoid fracture is classically recommended if the footprint of the anterior bundle of the MCL on the antero‐medial facet is involved. This ensures reattachment of the ligament, thereby improving medial stability of the elbow. Anteromedial fractures are usually part of a subluxation injury and are best addressed with a medial buttress plate. 35 We are of the view that with SSPS fixation, the anterior capsule is directly captured with reduction of the fracture fragment together. When fixation is secure, active stretching exercises can be started as soon as possible to regaining elbow and forearm motion. The early movement of the elbow is beneficial to the functional recovery of elbow for the patient.
Effectiveness of the SSPS for Comminuted Coronoid Fracture
Considering comminuted coronoid fracture, the surgical strategy was made on the mechanism of injury, the ability of the residual intact coronoid to maintain elbow stability and morphology patterns other than the size of the fracture fragment alone. 36 The anteromedial facet of the coronoid acts as a buttress to varus posteromedial instability which should be restored by a buttress plate. A biomechanical study demonstrated that operative fixation the anteromedial facet fracture in conjunction with LCL repair improved the elbow stability significantly. 7 In line with these findings, our surgical technique addressed spring plate fixation to buttress the comminuted fracture which involved the anteromedial coronoid fractures. The best fixation for small and/or comminuted tip fragments is still debatable. Some surgeons advocate that type 1 fractures may be excised or left alone, 1 whilst others would fix any associated coronoid fracture, regardless. 37 Garrigues et al. found that the suture lasso technique was more reliable than screws or suture anchors fixation. 38 The elbow stiffness is mainly derived from the scar and soft tissue contraction around due to immobilization. In comminuted coronoid process fracture together with small tip fragment, we used SSPS to provide a most rigid buttress effect of the coronoid. Furthermore, the suture reattachment of capsule with the small tip restored sound biomechanical stability. The clinical and radiographic results of our case series are comparable with other case series in the literature studying surgical fixation of coronoid fractures. Significantly, a functional elbow arc of motion at least 30–130 of flexion‐extension was achieved in all our patients, and persistent symptomatic elbow instability or major complications requiring revision surgery were observed in none. We believe this represents a satisfactory outcome in patients with a complex and challenging elbow injury.
Limitations of the Study
There still were some limitations in this study. First, this was a retrospective case series with no control group for comparison. Second, the sample size in our study is small due to the low incidence of comminuted coronoid fractures. Third, the time span of our cases is not consistent, there are other factors that might bias the osteoarthritis complications in this retrospective study. However, we believe that our study lends further support to various articles in the literature in recommending fixation of comminuted coronoid fractures, and is the first in the literature to show good outcomes with no significant complications using SSPS fixation technique.
Conclusion
Based on our findings, the SSPS fixation of coronoid process fractures had technical benefits and contribute to the restoration of elbow stability sufficiently, which permitted early mobilization and rehabilitation. Hence, this novel system and technique provides a reliable treatment for the comminuted coronoid fracture with predictable clinical outcomes.
Ethics Statement
This study was apporved by the institutional review board of our hospital (No. IRB‐2020‐133).
Author Contributions
Ruijian Yan: collection and assembly of data; data analysis and interpretation; manuscript writing. Yifan Wu: collection and analysis of data. Zhihui Xiang: collection and analysis of data; data interpretation. Sihao Li: data collection and interpretation, manuscript writing. Yiying Qi: collection of data; data analysis and interpretation. Hang Li: data analysis and interpretation. Chengyu Zhuang: conception and design; data analysis and interpretation; final approval of manuscript. Gang Feng: conception and design; data analysis and interpretation; revision of the manuscript, financial support, group leader.
Acknowledgments
This work was supported by the National key R&D program of China (2018YFA0701401), the Key R&D Program of Zhejiang Province (2021C03108), Joint Construction Project of Zhejiang Province and Health Ministry (WKJ‐ZJ‐2029), Foundation of Zhejiang Educational Committee (Y201839065, Y201941414, Zhejiang Natural Science Foundation (Y22H069063) The authors would like to acknowledge the staff of Orthopedic Lab of Zhejiang University for their assistance. None of the authors had professional or financial affiliations that biased this work. All authors disclose that they have no financial and personal relationships with other people or organizations that could inappropriately bias this work.
Ruijian Yan and Yifan Wu contributed equally to the work.
Contributor Information
Chengyu Zhuang, Email: zhuangchengyu@msn.com.
Gang Feng, Email: gangfeng@zju.edu.cn.
References
- 1. Ring D, Horst TA. Coronoid fractures. J Orthop Trauma. 2015;29(10):437–40. [DOI] [PubMed] [Google Scholar]
- 2. Vollans SR, van Riet RP. Elbow instability. J Orthop Trauma. 2016;30(4):310–6. [Google Scholar]
- 3. Long N, He S, Wu S, Huang F. Research progress of posteromedial rotatory instability of the elbow. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018;32(4):505–10. Chinese. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lewis TL, Ferran NA, Gooding BWT. Current concepts in shoulder and elbow fractures and dislocations. Surgery. 2016;34(3):122–8. [Google Scholar]
- 5. Mathew PK, Athwal GS, King GJ. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 2009;17(3):137–51. [DOI] [PubMed] [Google Scholar]
- 6. Park SM, Lee JS, Jung JY, Kim JY, Song KS. How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O'Driscoll classification and ligament injury. J Shoulder Elb Surg. 2015;24(1):74–82. [DOI] [PubMed] [Google Scholar]
- 7. Bellato E, Kim Y, Fitzsimmons JS, Berglund LJ, Hooke AW, Bachman DR, et al. Coronoid reconstruction using osteochondral grafts: a biomechanical study. J Shoulder Elb Surg. 2017;26(10):1794–802. [DOI] [PubMed] [Google Scholar]
- 8. Bellato E, O'Driscoll SW. Prosthetic replacement for coronoid deficiency: report of three cases. J Shoulder Elb Surg. 2017;26(3):382–8. [DOI] [PubMed] [Google Scholar]
- 9. Wells J, Ablove RH. Coronoid fractures of the elbow. Clin Med Res. 2008;6(1):40–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mellema JJ, Eygendaal D, van Dijk CN, Ring D, Doornberg JN. Fracture mapping of displaced partial articular fractures of the radial head. J Shoulder Elb Surg. 2016;25(9):1509–16. [DOI] [PubMed] [Google Scholar]
- 11. Kataoka T, Moritomo H, Miyake J, Murase T, Sugamoto K. Three‐dimensional suitability assessment of three types of osteochondral autograft for ulnar coronoid process reconstruction. J Shoulder Elb Surg. 2014;23(2):143–50. [DOI] [PubMed] [Google Scholar]
- 12. Colozza A, Menozzi M, Perna L, Cavaciocchi M, Martini I, Galavotti C, et al. Results of arthroscopically assisted reduction and fixation of antero‐medial coronoid facet fractures at short term follow‐up. J Shoulder Elb Surg. 2022; S1058‐2746(22)00425‐6. Epub ahead of print. PMID: 35550430. [DOI] [PubMed] [Google Scholar]
- 13. Reichel LM, Milam GS, Reitman CA. Anterior approach for operative fixation of coronoid fractures in complex elbow instability. Tech Hand Up Extrem Surg. 2012;16(2):98–104. [DOI] [PubMed] [Google Scholar]
- 14. Yang X, Chang W, Chen W, Liu S, Zhu Y, Zhang Y. A novel anterior approach for the fixation of ulnar coronoid process fractures. Orthop Traumatol Surg Res. 2017;103(6):899–904. [DOI] [PubMed] [Google Scholar]
- 15. Papatheodorou LK, Rubright JH, Heim KA, Weiser RW, Sotereanos DG. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res. 2014;472(7):2084–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McKee MD, Pugh DM, Wild LM, Schemitsch EH, King GJ. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures: surgical technique. J Bone Joint Surg Am. 2005;87(Suppl 1 (Pt 1)):22–32. [DOI] [PubMed] [Google Scholar]
- 17. Feng D, Zhang X, Jiang Y, Zhu Y, Wang H, Wu S, et al. Plate fixation through an anterior approach for coronoid process fractures: a retrospective case series and a literature review. Medicine (Baltimore). 2018;97(36):e12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Oh WT, Do WS, Oh JC, Koh IH, Kang HJ, Choi YR. Comparison of arthroscopy‐assisted vs. open reduction and fixation of coronoid fractures of the ulna. J Shoulder Elb Surg. 2021;30(3):469–78. [DOI] [PubMed] [Google Scholar]
- 19. Czerwonka N, Momenzadeh K, Stenquist DS, O'Donnell S, Kwon JY, Nazarian A, et al. Anatomic structures at risk during posterior to anterior percutaneous screw fixation of posterior malleolar fractures: a cadaveric study. Foot Ankle Spec. 2022;15(1):50–8. [DOI] [PubMed] [Google Scholar]
- 20. Iannuzzi NP, Paez AG, Parks BG, Murphy MS. Fixation of Regan‐Morrey type II coronoid fractures: a comparison of screws and suture lasso technique for resistance to displacement. J Hand Surg Am. 2017;42(1):e11–4. [DOI] [PubMed] [Google Scholar]
- 21. Nazifi O, Gunaratne R, D'Souza H, Tay A. The use of high strength sutures and anchors in olecranon fractures: a systematic review. Geriatr Orthop Surg Rehabil. 2021;12:2151459321996626. 10.1177/2151459321996626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rausch V, Jettkant B, Lotzien S, Rosteius T, Mempel E, Schildhauer TA, et al. Biomechanical comparison of screw osteosyntheses and anatomical plating for coronoid shear fractures of the ulna. Arch Orthop Trauma Surg. 2021;141(9):1509–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jeon IH, Oh CW, Kim PT. Minimal invasive percutaneous plate osteosynthesis for complex Monteggia fracture with type III coronoid process fracture. Injury. 2004;35(6):631–3. [DOI] [PubMed] [Google Scholar]
- 24. Yao S, Zhao C, Wu H, Cao Y. To cure coronoid process fractures of ulna through anterior approach of the elbow and frame shape plate internal fixation. Zhonghua Yi Xue Za Zhi. 2015;95(45):3678–80. Chinese. [PubMed] [Google Scholar]
- 25. Wegmann K, Knowles NK, Lalone EE, Hackl M, Müller LP, King GJW, et al. The shape match of the olecranon tip for reconstruction of the coronoid process: influence of side and osteotomy angle. J Shoulder Elb Surg. 2019;28(4):e117–24. [DOI] [PubMed] [Google Scholar]
- 26. Lindenhovius A, Karanicolas PJ, Bhandari M, van Dijk N, Ring D. Interobserver reliability of coronoid fracture classification: two‐dimensional versus three‐dimensional computed tomography. J Hand Surg Am. 2009;34(9):1640–6. [DOI] [PubMed] [Google Scholar]
- 27. O'Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–34. [PubMed] [Google Scholar]
- 28. Manidakis N, Sperelakis I, Hackney R, Kontakis G. Fractures of the ulnar coronoid process. Injury. 2012;43(7):989–98. [DOI] [PubMed] [Google Scholar]
- 29. Masood QM, Qulaghassi M, Grewal U, Bawale R, Kammela M, Singh B. Proximal ulna fractures in adults: a review of diagnosis and management. J Clin Orthop Trauma. 2021;20:101481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Watts AC, Singh J, Elvey M, Hamoodi Z. Current concepts in elbow fracture dislocation. Should Elb. 2021;13(4):451–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yoon RS, Tyagi V, Cantlon MB, Riesgo AM, Liporace FA. Complex coronoid and proximal ulna fractures are we getting better at fixing these? Injury. 2016;47(10):2053–9. [DOI] [PubMed] [Google Scholar]
- 32. Shimura H, Nimura A, Nasu H, Fujishiro H, Imatani J, Okawa A, et al. Joint capsule attachment to the coronoid process of the ulna: an anatomic study with implications regarding the type 1 fractures of the coronoid process of the O'Driscoll classification. J Shoulder Elb Surg. 2016;25(9):1517–22. [DOI] [PubMed] [Google Scholar]
- 33. Luokkala T, Temperley D, Basu S, Karjalainen TV, Watts AC. Analysis of magnetic resonance imaging‐confirmed soft tissue injury pattern in simple elbow dislocations. J Shoulder Elb Surg. 2019;28(2):341–8. [DOI] [PubMed] [Google Scholar]
- 34. Antoni M, Eichler D, Kempf JF, Clavert P. Anterior capsule re‐attachment in terrible triad elbow injury with coronoid tip fracture. Orthop Traumatol Surg Res. 2019;105(8):1575–83. [DOI] [PubMed] [Google Scholar]
- 35. Liu G, Hu J, Ma W, Li M, Xu R, Pan Z. Surgical treatment for terrible triad injury of the elbow with anteromedial coronoid fracture through a combined surgical approach. J Int Med Res. 2018;46(8):3053–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rhyou IH, Lee JH, Kim KC, Ahn KB, Moon SC, Kim HJ, et al. What injury mechanism and patterns of ligament status are associated with isolated coronoid, isolated radial head, and combined fractures? Clin Orthop Relat Res. 2017;475(9):2308–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wang YH, Meng QB, Wu JD, Ma JC, Liu F. Treatment of fractures of the ulnar coronoid process. Orthop Surg. 2009;1(4):269–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Garrigues GE, Wray WH, Lindenhovius AL, Ring DC, Ruch DS. Fixation of the coronoid process in elbow fracture‐dislocations. J Bone Joint Surg Am. 2011;93(20):1873–81. [DOI] [PubMed] [Google Scholar]


