Abstract
Objective
Conventional localization technique of V point for full‐endoscopic posterior cervical foraminotomy and discectomy (FPCD) required repeated fluoroscopies, especially in patients with short and thick necks. To address this issue, the present study aimed to introduce a new localization technique of V point, and further evaluate its efficacy.
Methods
A K‐wire was inserted and fixed at the pedicle eye under A/P fluoroscopy, then a working channel was established quickly along with it. Thirty‐four patients who underwent minimally invasive FPCD assisted by the new technique were included in this study. The clinical and radiological data were collected and analyzed, including radiation dose, operative time, positioning time, visual analog scale (VAS) for neck and arm pain, neck disability index (NDI) scores, Cobb angle of operative level and range of motion of the cervical spine.
Results
All operations were performed successfully, and no iatrogenic nerve or vascular injury occurred. None of the patients needed to be transferred to open surgery or revision surgery. The mean radiation dose was found to be1.68 ± 0.36 mSv. The mean positioning time observed was 10.68 ± 5.42 min and the average operation time was 81.18 ± 10.87 min. The operation time significantly declined as the number of patients increased. A significant difference in operation time between the first (96.22 ± 10.36 min) and last quartile (75.00 ± 3.84 min) of cases was observed (t = 4.82, P < 0.001). The VAS scores for neck and arm pain, and NDI scores were significantly improved after surgery (P VAS−Neck<0.0001, P VAS−Arm<0.0001, P NDI<0.0001). Based on MacNab criteria, the excellent plus good rate was 91.17%. The Cobb angle of operative level and range of motion of the cervical spine were significantly improved postoperatively (t = 2.846, P OA = 0.015; t = 2.232, P ROM−CA = 0.026).
Conclusion
The new image‐assisted V point localization technique is simple and useful with little radiation exposure and short positioning time. FPCD assisted by the new technique could be a safe and effective alternative on properly selected patients.
Keywords: Efficacy, fluoroscopy‐guided, Full‐endoscopy, Localization technique, Posterior cervical foraminotomy and discectomy
Here, we introduced a new localization technique that the V point could be easily and quickly determined by fixing a k‐wire at the pedicle eye under the A/P X‐ray guidance, and the working tube could easily be inserted along the K‐wire, avoiding repeated fluoroscopies.

Introduction
Cervical radiculopathy is a degenerative disease, characterized by radiating pain, numbness in the neck and affected upper limbs due to lateral herniated intervertebral discs or narrowed intervertebral foramina. 1 Surgical decompression is necessary when conservative treatment fails or neurological function keeps worsening. There are several surgical approaches for such cases, including posterior cervical laminoforaminotomy (PCL), anterior cervical discectomy and fusion (ACDF), and cervical disc replacement. Traditional PCL without additional stabilization can preserve the mobility of operative segments at the cost of longer incision and more extensive muscle dissection. It may increase the risk of postoperative axial neck pain and in turn affect segmental stability. 2 , 3 ACDF has been regarded as the standard surgical procedure for the operation of cervical radiculopathy with good clinical results. 4 , 5 , 6 , 7 , 8 Nonetheless, subsequent problems are also becoming increasingly prominent, such as limited cervical movement, adjacent segment disease, pseudarthrosis, and access‐related complications. 9 , 10 , 11 , 12 , 13 , 14 Human cervical disc replacement was firstly reported by Fernstrom et al.. 15 Even though it achieved good short‐term efficacy, there were many complications, such as prosthesis loosening and ossification around the prosthesis.
In 1989, Hijikata 16 first described the percutaneous technology of cervical spine surgery, but with limited surgical indications, and only “soft” intervertebral disc herniation from the intervertebral disc level is acceptable. In 2007, Ruetten et al. 17 successfully performed full‐endoscopic posterior cervical foraminotomy for patients with lateral disc herniations based on the “key‐hole” technique. It can complete the grinding of part of the bony structure. Patients with the foramina stenosis compressed by bony structure can obtain good results. Hence, its surgical indications are relatively extensive than before. In 2016, Deng et al. 18 successfully performed percutaneous full‐endoscopic anterior transcorporeal cervical discectomy, which maximally protects the normal intervertebral disc tissue and reduces the risk of degeneration of adjacent segments. Furthermore, in the case of large free intervertebral disc, subtotal vertebral resection can be avoided and better results can be obtained. In the past decades, with the continuous development and maturity of endoscopic spine system, endoscopic spine surgery with less trauma, quick recovery and better function retention has aroused much interest. Compared with open surgery, the full endoscopic technique preserves the mobility of the segment and ensures sufficient decompression. It avoids excessive stripping of the posterior cervical muscle groups, reducing intraoperative bleeding, soft tissue injury and postoperative axial pain. 19 Several studies have demonstrated that full endoscopic cervical spine surgery is a safe, effective and promising alternative to conventional procedures on properly selected patients. 20 , 21 , 22
The “key‐hole” technique is the basis of minimally invasive full endoscopic posterior cervical foraminotomy and discectomy (FPCD). And accurate localization of the “V” point (the intersection of the upper and lower lamina with the articular process)is a crucial step of the “key‐hole” technique. Conventionally, the lateral x‐ray‐guided method was used to ensure accurate localization of V point. However, for patients with short and thick necks, lateral x‐ray‐guided method had some limitations in clear positioning of the V point and working tube. Also, it required repeated fluoroscopies during surgery and increased radiation exposure. 23 In recent years, the application of the O‐arm navigation system in FPCD has addressed the limitations of the lateral x‐ray guided method for patients with short and thick necks or lower‐level cervical diseases. The technique has also provided a visible trajectory for working canal insertion, thus increasing the accuracy and efficiency. 23 However, high price and radiation exposure of the O‐arm navigation system have limited its wide‐scale application.
The aim of the present study was: (i) to introduce a new localization technique of V point; (ii) to assess its technical advantage; and (iii) to evaluate the clinical outcomes of patients who underwent FPCD assisted by the new localization technique.
Methods
Study Design and Patients
This retrospective study included 34 patients who underwent minimally invasive FPCD assisted by the new technique between January 2016 and December 2018 at the department of spine surgery of Renji Hospital. The inclusion criteria were: (i) patients with severe unilateral upper limb radiating pain with or without neck pain; (ii) conservative treatment was ineffective for more than 3 months; (iii) mono‐segmental cervical lateral disc herniation or foraminal stenosis verified by CT or MRI; and (iv) complete clinical and radiological data available. The exclusion criteria were as follows: (i) cervical myelopathy or definite spinal instability or deformity; and (ii) history of cervical surgery. All operations were performed by the same team. The follow up period was 2 years, and no one was lost at follow‐up at any time points. The study was approved by the Ethics Committee of Baoshan Branch of Renji Hospital (IRB No: 2021‐lw‐015), and all patients provided written informed consent.
Data Collection
Data on patient demographics, including age at the time of surgery, gender, body mass index, symptom duration, operation level, hospital stay, hospital costs, operation time, positioning time, blood loss, radiation frequency and dose, intraoperative adverse events, postoperative complication and reoperation rates were collected and analyzed. Positioning time referred to the time between the start of the operation and the insertion of the working channel. Visual analogue scale (VAS) for neck pain and arm pain, neck disability index (NDI),and modified MacNab criteria were used as clinical outcome measurements before the operation and picture archiving and communication1week, 3 months, 1 year and 2 years after surgery.
Radiological parameters were analyzed before the operation and 1 week and 2 years after the operation using picture archiving and communication (PACS) system, including C2‐C7 angle (cervical curvature, CA),the segmental Cobb angle of the operative level (OA), and the range of motion (ROM) of the cervical spine and operative level. The C2‐C7 angle is defined as the acute angle formed by the lines paralleling to the posterior margins of the C2 and C7 vertebra. The ROM of the operative level refers to the difference between the Cobb angle on the flexion lateral radiograph and the Cobb angle on the extension lateral radiograph of the surgical segment. The ROM of the cervical spine refers to the difference between Angle C2‐C7 on the cervical flexion lateral radiograph and Angle C2‐C7 on the cervical extension lateral radiograph. 24 (Fig. 1).All data were measured by three independent doctors and reviewed by the corresponding authors. The mean of three was considered for further analysis.
Fig. 1.
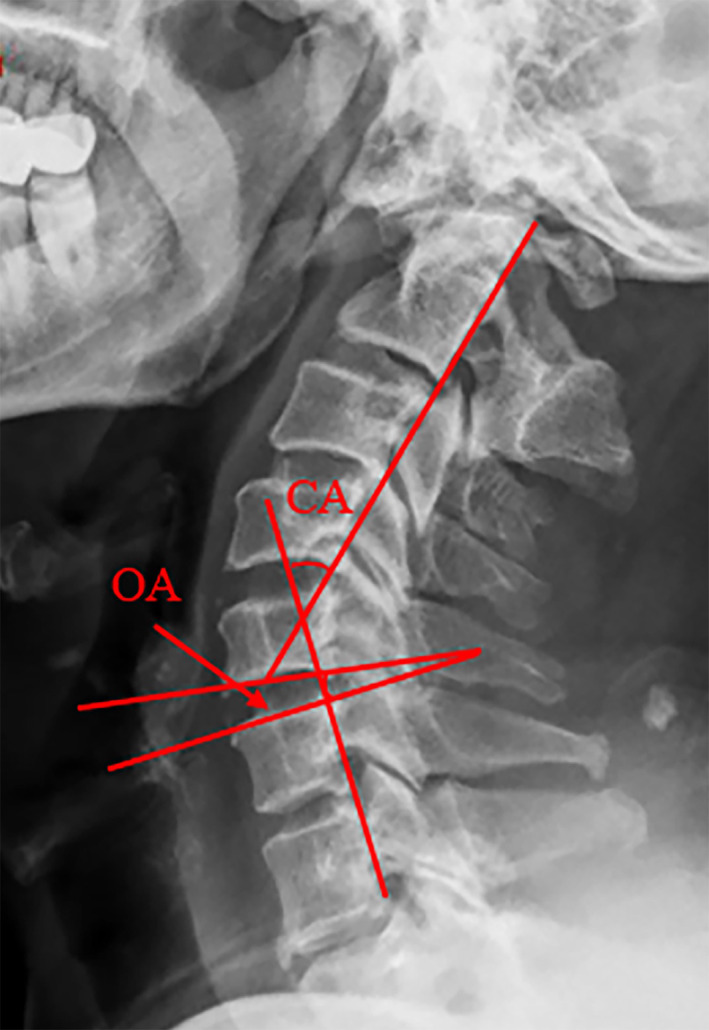
Measurement of radiological parameters. The OA (segmental Cobb angle of the operative level)refers to the acute angle formed by the line paralleling to the inferior endplate of upper vertebra and the line paralleling to the superior endplate of lower vertebra. The CA (C2‐C7 angle) is defined as the acute angle formed by the lines paralleling to the posterior margins of the C2 and C7 vertebra
New Localization Technique and Surgical Procedure of FPCD
The patient was placed in the prone position with his/her head fixed in the Mayfield frame under general anesthesia. The arms were placed beside the body and secured with tape (Fig. 2A). The operative level was defined by anterior–posterior (A/P) fluoroscopy (i.e., C6/7, Fig. 2B–D).
Fig. 2.
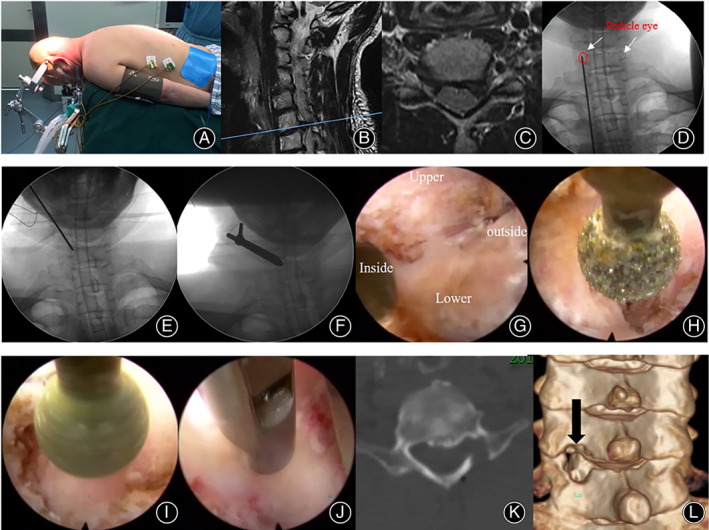
New localization technique, and surgical procedure of FPCD. (A) the patient was placed in prone position; (B–C) preoperative MRI; (D–E): a K‐wire was fixed at the pedicle eye under A/P fluoroscopy; (F) a dilator was inserted slowly along the K‐wire, and the working tube was inserted through the dilator; (H–J): key‐hole technique and decompression; (K–L). postoperative CT
New Localization Technique of V Point
A K‐wire was placed on the back of the neck, pointing to the pedicle on the affected side as seen by A/P fluoroscopy (Fig. 2D). A transverse incision approximately 1 cm in length was made centered on the C7 pedicle eye. Under the guidance of A/P fluoroscopy, the K‐wire was inserted with the tip located on the pedicle eye of C7 pedicle. Once the position was confirmed, the K‐wire was fixed with a hammer (Fig. 2E). After blunt dissection of the surrounding soft tissue, a dilator was inserted slowly along the K‐wire. Keeping the K‐wire still, the working tube was inserted through the dilator, after which the dilator was removed. A trepan was placed inside the working channel to clean the soft tissue from the bone surface. The operation continued under visual control and continuous irrigation with 0.9% saline solution. The 5.9 mm endoscope was inserted to confirm the position of the K‐wire, and the K‐wire was removed (Fig. 2F).
Full Endoscopic Posterior Cervical Foraminotomy and Discectomy
The soft tissue on the surface of the facet joint was cleaned with a gasification knife, and the medial muscle tissue at the back of the neck was cauterized to confirm the location of the upper and lower articular processes and the V point (the intersection of the upper and lower lamina with the articular process) (Fig. 2G). A key‐hole foraminotomy was performed centered on the V point by partly removing the inferior and superior articular process using a high‐speed burr (Fig. 2H,I). The lateral ligamentum flavum was resected carefully, and the spinal cord and nerves were identified. Discectomy was performed under the armpit of the C7 nerve root to remove the intervertebral disc tissue. The area was probed carefully to avoid missing any free discs or incomplete resection (Fig. 2J). Finally, the wound was closed after thorough hemostasis using bipolar radiofrequency coagulation. The keyhole foraminotomy could be extended laterally or craniocaudally if necessary. Postoperative CT scan of the cervical spine was performed to identify the decompression and keyhole range (Fig. 2K,L). Afterward, all patients were required to wear a collar for 1 month.
Statistical Analysis
IBM SPSS (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY, USA) was used to analyze the data in this retrospective study. Paired t‐tests were used to compare preoperative and postoperative clinical outcomes and radiological parameters. Continuous variables were presented as mean ± standard deviation, and categorical data was expressed as frequency or percentages. A P value less than 0.05 was considered to indicate a statistically significant difference.
Results
The mean radiation dose was 1.68 ± 0.36 mSv. There was no measurable blood loss due to continuous irrigation. All operations were performed successfully, and no iatrogenic nerve or vascular injury occurred intraoperatively. None of the patients needed to be transferred to open surgery and none of them needed reoperation immediately after surgery. No permanent complication was observed in the postoperative follow‐up. Only one patient suffered temporary arm pain at 1 week after surgery. According to MacNab criteria, 28 out of 34 patients were excellent, three out of 34 patients were good, and other three patients were fair at 2 years after surgery, which brought a rate of excellent and good vertebral function of 91.17%. The demographic and clinical characteristics of the included patients were summarized in Table 1.
TABLE 1.
The demographic and clinical characteristics of included patients
| Characteristics | Number |
|---|---|
| Age (years) | 54.75 ± 9.74 |
| Gender (male/female) | 34(15/19) |
| BMI (kg/m2) | 24.56 ± 3.24 |
| Symptom duration (months) | 6.12 ± 2.36 |
| Operation level | |
| C3/4 | 0 |
| C4/5 | 11 |
| C5/6 | 14 |
| C6/7 | 9 |
| Affected side (left/right) | 14/20 |
| Operative time (mins) | 81.18 ± 10.87 |
| Positioning time (mins) | 10.68 ± 5.42 |
| Radiation frequency (No.) | 8.38 ± 1.78 |
| Radiation dose (mSv) | 1.68 ± 0.36 |
| Hospital stays (days) | 4.52 ± 1.22 |
| Hospital costs (dollar) | 3500.68 ± 368.44 |
| Intraoperative adverse events | 0 |
| Postoperative complications | 0 |
Abbreviation: BMI: Body mass index.
Learning Curve
The mean positioning time was 10.68 ± 5.42 min and the average operation time was 81.18 ± 10.87 min (Table 1). A learning curve was observed as seen in Fig. 3. The operation time significantly declined as the number of patients increased. The mean operation time in the first quartile of cases (96.22 ± 10.36 min) was significantly higher than that in the last quartile (75.00 ± 3.84 min) (t = 4.82, P < 0.001).
Fig. 3.
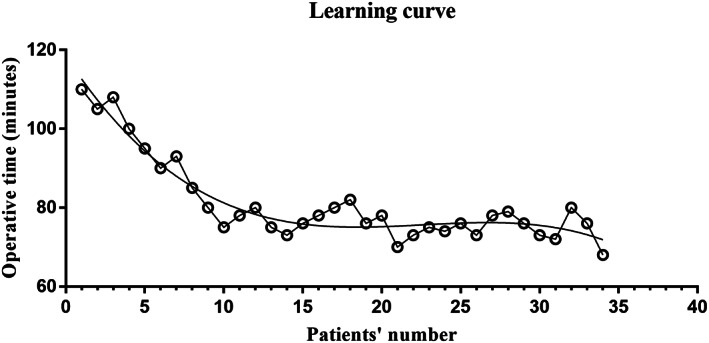
Learning curve of FPCD assisted by the new technique. The operation time significantly declined as the number of patients increased. The mean operation time in the first quartile of cases (96.22 ± 10.36 min) was significantly higher than that in the last quartile (75.00 ± 3.84 min) (t = 4.82, P < 0.001)
Clinical Evaluation
The VAS for neck pain was 7.25 ± 1.00 preoperatively, 2.06 ± 0.77 at 1 week postoperatively, and 0.25 ± 0.45 at 2 years postoperatively (Table 2). The VAS for arm pain was 8.12 ± 1.12, 2.18 ± 0.91, 0.19 ± 0.40 preoperatively, 1 week postoperatively, and 2 years postoperatively, respectively (Table 3). In addition, the NDI scores were 43.56 ± 16.78 preoperatively, 23.14 ± 8.76 at 1 week postoperatively, and 3.22 ± 3.32 at 2 years postoperatively (Table 4). Significant improvement in NDI scores (P<0.0001) and VAS scores for neck pain (P<0.0001) and arm pain (P<0.0001) were found after surgery.
TABLE 2.
The VAS for neck pain
| Variables | VAS for neck pain | t value | p value |
|---|---|---|---|
| Preoperative | 7.25 ± 1.00 | ||
| 1 week after surgery | 2.06 ± 0.77* | 12.35 | <0.0001 |
| 3 months after surgery | 1.44 ± 0.51* | 13.28 | <0.0001 |
| 1 year after surgery | 0.50 ± 0.63* | 14.66 | <0.0001 |
| 2 years after surgery | 0.25 ± 0.45* | 15.12 | <0.0001 |
Abbreviation: VAS, Visual analogue scores
Note: *Comparison of preoperative VAS.
TABLE 3.
The VAS for arm pain
| Variables | VAS for arm pain | t value | p value |
|---|---|---|---|
| Preoperative | 8.12 ± 1.12 | ||
| 1 week after surgery | 2.18 ± 0.91* | 11.87 | <0.0001 |
| 3 months after surgery | 1.56 ± 0.52* | 13.24 | <0.0001 |
| 1 year after surgery | 0.81 ± 0.75* | 13.45 | <0.0001 |
| 2 years after surgery | 0.19 ± 0.40* | 14.92 | <0.0001 |
Abbreviation: VAS, Visual analogue scores
Note: *Comparison of preoperative VAS.
TABLE 4.
The NDI scores
| Variables | NDI scores | t value | p value |
|---|---|---|---|
| Preoperative | 43.56 ± 16.78 | ||
| 1 week after surgery | 23.14 ± 8.76* | 8.64 | <0.0001 |
| 3 months after surgery | 16.69 ± 6.54* | 9.48 | <0.0001 |
| 1 year after surgery | 9.56 ± 4.77* | 10.92 | <0.0001 |
| 2 years after surgery | 3.22 ± 3.32* | 12.24 | <0.0001 |
Abbreviation: NDI, Neck disability index
Note: *Comparison of preoperative NDI scores.
Radiological Results
The radiological results of included patients were shown in Table 5. The CA and ROM‐CA were significantly improved at 2 years after surgery (t = 2.846, P OA = 0.015;t = 2.232, P ROM−CA = 0.026). However, there was no significant differences between preoperative and postoperative in CA and ROM‐OA.
TABLE 5.
Preoperative and postoperative radiological data of the included patients
| Variables | Preoperative | 1 week | 2 years | t value | p value |
|---|---|---|---|---|---|
| CA (°) | 10.22 ± 5.34 | 10.86 ± 4.88 | 10.74 ± 5.12 | 0.063 | 0.942 |
| OA (°) | 4.12 ± 3.76 | 2.04 ± 3.34 | 1.96 ± 2.88* | 2.846 | 0.015 |
| ROM‐CA (°) | 24.45 ± 8.76 | 28.84 ± 9.48 | 31.34 ± 10.14* | 2.232 | 0.026 |
| ROM‐OA (°) | 5.94 ± 2.32 | 6.32 ± 3.44 | 6.23 ± 2.88 | 0.059 | 0.864 |
Abbreviations: CA, Angle of cervical curvature; OA, Cobb angle of operative level; ROM, Range of motion
Note: *Significant difference between preoperative and 2 years postoperatively.
Discussion
In this study, a new localization technique of the V point for FPCD was introduced. The results showed that the new technique was simple and fast, with little radiation exposure and short positioning time. FPCD assisted by the new technique was a safe and effective alternative to conventional procedures on properly selected patients.
Introduction of the New Localization Technique of the V Point
FPCD was initially performed by Ruetten et al. in 2007. 17 Accurate localization of the V point (the intersection of the upper and lower lamina with the articular process) is a crucial step for the successful completion of FPCD. Even though the spinal endoscope system has improved in recent years, the conventional localization technique initially reported by Ruetten et al., namely lateral x‐ray‐guided localization method, remains the most commonly used localization technique in clinical practice. 17 , 25 , 26 First, they marked the line of spinal joint in the neck back under posterior‐anterior x‐ray control. Determination of the segment, the performance of skin incision, and blunt insertion of a dilator were performed under the lateral x‐ray control. The entire process cannot be visualized, and repeated fluoroscopies are needed to determine the V point. Moreover, for patients with short and thick necks or lower‐level cervical diseases, it is difficult to achieve clear positioning of the surgical level and working tube with the technique. To address these issues, in the present study, we introduced a new localization technique that the V point could be easily and quickly determined by fixing a k‐wire at the pedicle eye under the A/P x‐ray guidance, and the working tube could easily be inserted along the K‐wire. The results also demonstrated the superiorities of the new technique in radiation exposure and positioning time.
Evaluation of the Advantage of the New Technique
Recently, Zhang et al. 23 introduced the application of O‐arm navigation system in FPCD, which could not only address the issue of conventional technique in clear positioning of the V point and working tube, but could also provide a visible trajectory for working channel insertion, thus increasing the accuracy and efficiency. However, the exorbitant price limited its wide application, and the higher radiation dose of intraoperative CT scan (approximately 10 mSv per patient) and extra surgical time due to registration and planning were inevitable. In this study, the average radiation dose was 1.68 ± 0.36 mSv, and the mean positioning time for the V point was 10.68 ± 5.42 min, which may be lower, shorter and more acceptable than those with the conventional technique. However, a further comparative study is required to confirm this. The results could be attributed to two reasons. First, the new technique could quickly determine the V point along the K‐wire by simply locating and fixing the K‐wire to the corresponding pedicle eye via A/P x‐ray, decreasing the radiation exposure and positioning time. Second, when determining the V point, the new technique could avoid repeated fluoroscopies and further reduce the radiation amount and exposure. In addition, for patients with short and thick necks or lower‐level diseases, there was no need to consider the disturbance of the shoulder on the lateral x‐ray, because the new technique is assisted by A/P x‐ray instead of lateral x‐ray.
In this study, the average operation time was 81.18 ± 10.86 min, which was shorter than the operation times observed while using the O‐arm navigation system (86.0 ± 19.6 min) and the conventional x‐ray guidance‐based technique (90–94 min). 25 The shortened operation time might be due to the quick positioning of the V point achieved with the new technique. The new image‐assisted technique could easily and quickly position the V point without repeated operations. However, the O‐arm navigation technique required additional time for registration and the conventional technique required repeated fluoroscopies, which increased their operation times. Moreover, a learning curve was observed. For doctors with rich experience in endoscopic operation and clinical experience, 15 cases of learning could achieve a stable learning curve.
Evaluation of the Clinical Outcomes of the New Technique
The results showed that the VAS for neck and arm pain and NDI score significantly improved after surgery. Based on the modified MacNab criteria, the rate of excellent and good vertebral function was 91.17% at 2 years after surgery, which indicated that FPCD assisted by the new technique was an effective procedure for patients with lateral disc herniation and/or foramen stenosis. The ROM‐CA significantly improved after surgery. This may be because the preoperative ROM of cervical spine was limited due to neck pain or arm pain caused by nerve compression, and it recovered after the surgical removal of compression. The common complications of FPCD include postoperative paresthesia, cerebrospinal fluid leakage due to dural sac injury or dural sac tear, spinal instability and nucleus pulposus residue. 17 , 22 In this study, no permanent complication was observed due to accurate localization and careful operation. Recurrence of disc herniation occurred only in one patient at 2 years after surgery, without the necessity for reoperation. This could be attributed to accurate localization and careful operation. However, the small sample size might be another cause of the low complication rates. Moreover, the new technique used a fairly paramedian approach with minimal medial angulation, which might be safer than the conventional technique. Sufficient decompression is the key to ensuring the efficacy of FPCD surgery, but excessive bone resection could lead to postoperative spinal instability. Hence, preoperative cervical CT or MRI was particularly important to specify the location of the herniated disc and determine the range of bone resection. In this study, we first removed a small part of the inferior facet, followed by slowly removing the superior facet. This step was followed by removal of the medial one‐third of the pedicle and grinding the medial edge of the pedicle to the posterior edge of the vertebral body. A probe was also used to observe the medial edge of the pedicle during the operation to avoid the instability caused by excessive resection of facet joints.
Highlights, Pitfalls, and Experience Performing the Surgery
The new A/P x‐ray guided localization technique of the V point overcomes several limitations of the conventional localization technique (lateral x‐ray guided). It is a simple and useful technique, enjoying the clinical advantage of short positioning time with little radiation exposure. It is also applicable for patients with short and thick neck or lower‐level cervical diseases. FPCD assisted by the new technique is a safe and effective procedure on properly selected patients.
However, the new technique has some potential pitfalls. The K‐wire may slide out laterally due to the abnormal surgical position of patients and may cause dural leakage or spinal cord injury. The surgeon needs to be familiar with the anatomy of the relevant approach, as the K‐wire is inserted only under the guidance of A/P fluoroscopy. Unfamiliarity with the anatomy of cervical region may require more fluoroscopies to insert K‐wire into the pedicle eye, which may further increase the radiation exposure. Also, it is important to maintain the middle position of the cervical spine at the initial stage of surgical preparation, because the pedicle eye is the cardinal mark of the new technique. Inaccurate localization of the pedicle eye may cause undesirable events.
Limitations and Strengths
The present study reported a new localization technique which addressed several defects of the conventional technique, and it is simple and useful in clinical practice. However, the study has several limitations. First, the sample size of this retrospective study was small; therefore, a large sample randomized controlled trial is required to verify the findings in future. Second, the duration of follow‐up may be too short for long‐term complications, and a long‐term follow‐up is also warranted in future research. Third, the superiority of the new localization technique needs further comparisons with the traditional positioning method.
Conclusion
The new image‐assisted technique is a simple and useful localization technique of V point in clinical practice, with little radiation exposure and short positioning time. FPCD assisted by the new technique is a safe and effective alternative on the properly selected patients. By fixing a k‐wire at the pedicle eye under the A/P x‐ray guidance, the V point could be easily and quickly determined, and the working tube could easily be inserted along the K‐wire, shortening positioning time and avoiding repeated radiation. However, the superiority of the A/P fluoroscopy guided localization technique needs further comparisons with the traditional positioning method in future.
Author Contributions
Guibin Zhong: Conceptualization; Data curation; Writing the manuscript. Fan Feng: Data curation; Formal analysis; Writing the manuscript. Xinjin Su: Methodology. Xiuyuan Chen: Formal analysis. Junduo Zhao: Methodology. Hongxing Shen: Conceptualization; Methodology. Jianwei Chen: Conceptualization; Methodology; Supervision; Review and Editing. Lifeng Lao: Conceptualization; Methodology; Supervision; Review and Editing.
Ethics Statement
This work had received the approval from Ethics Committee in our hospital (No. 202‐1w‐015).
Acknowledgments
This work was supported by the grants from National Natural Science Foundation (81802216,).
The first 2 authors contributed equally to this work.
Contributor Information
Jianwei Chen, Email: jwchenbone@126.com.
Lifeng Lao, Email: spinelao@163.com.
References
- 1. Abumi K, Panjabi MM, Kramer KM, Duranceau J, Oxland T, Crisco JJ. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine (Phila Pa 1976). 1990;15(11):1142–7. [DOI] [PubMed] [Google Scholar]
- 2. Hermantin FU, Peters T, Quartararo L, Kambin P. A prospective, randomized study comparing the results of opendiscectomy with those of video‐assistedarthroscopic microdiscectomy. J Bone Joint Surg Am. 1999;81:958–65. [DOI] [PubMed] [Google Scholar]
- 3. Schick U, Döhnert J, Richter A, König A, Vitzthum HE. Microendoscopic lumbar discectomy versus open surgery: anintraoperative EMG study. Eur Spine J. 2002;11:20–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schroeder GD, Kurd MF, Millhouse PW, Vaccaro AR, Hilibrand AS. Performing an anterior cervical discectomy and fusion. Clin Spine Surg. 2016;29:186–90. [DOI] [PubMed] [Google Scholar]
- 5. Wen Z, Lu T, Wang Y, Liang H, Gao Z, He X. Anterior cervical corpectomy and fusion and anterior cervical discectomy and fusion using titanium mesh cages for treatment of degenerative cervical pathologies: a literature review. Med Sci Monit. 2018;24:6398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zou S, Gao J, Xu B, Lu X, Han Y, Meng H. Anterior cervical discectomy and fusion (ACDF) versus cervical disc arthroplasty (CDA) for two contiguous levels cervical disc degenerative disease: a meta‐analysis of randomized controlled trials. Eur Spine J. 2017;26:985–97. [DOI] [PubMed] [Google Scholar]
- 7. Brigham CD, Tsahakis PJ. Anterior cervical foraminotomy and fusion. Surgical technique and results. Spine (Phila Pa 1976). 1995;20(7):766–70. [PubMed] [Google Scholar]
- 8. Fraser JF, Härtl R. Anterior approaches to fusion of the cervical spine: a meta‐analysis of fusion rates. J Neurosurg Spine. 2007;6:298–303. [DOI] [PubMed] [Google Scholar]
- 9. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007;32(21):2310–7. [DOI] [PubMed] [Google Scholar]
- 10. Alhashash M, Shousha M, Boehm H. Adjacent segment disease after cervical spine fusion: evaluation of a 70 patient long‐term follow‐up. Spine (Phila Pa 1976). 2018;43(9):605–9. [DOI] [PubMed] [Google Scholar]
- 11. Pedram M, Castagnera L, Carat X, Macouillard G, Vital JM. Pharyngolaryngeal lesions in patients undergoing cervical spine surgery through the anterior approach: contribution of methylprednisolone. Eur Spine J. 2003;12:84–90. [DOI] [PubMed] [Google Scholar]
- 12. Wang MC, Chan L, Maiman DJ, Kreuter W, Deyo RA. Complications and mortality associated with cervical spine surgery for degenerative disease in the United States. Spine (Phila Pa 1976). 2007;32(3):342–7. [DOI] [PubMed] [Google Scholar]
- 13. Song K, Nima A, Alexandra S, et al. Complications after 3‐ and 4‐level anterior cervical diskectomy and fusion. World Neurosurg. 2019;130:e1105–10. [DOI] [PubMed] [Google Scholar]
- 14. Kelly MP, Eliasberg CD, Riley MS, Ajiboye RM, NF SH. Reoperation and complications after anterior cervical discectomy and fusion and cervical disc arthroplasty: a study of 52,395 cases. Eur Spine J. 2018;27:1432–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fernström U. Arthroplasty with intercorporal endoprothesis in herniated disc and in painful disc. Acta Chir Scand Suppl. 1966;357:154–9. [PubMed] [Google Scholar]
- 16. Hijikata S. Percutaneous nucleotomy. A new concept technique and 12 years' experience. Clin Orthop Relat Res. 1989;238:9–23. [PubMed] [Google Scholar]
- 17. Ruetten S, Komp M, Merk H, Godolias G. A new full‐endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9‐mm endoscopes: prospective 2‐year results of 87 patients. Minim Invasive Neurosurg. 2007;50:219–26. [DOI] [PubMed] [Google Scholar]
- 18. Deng ZL, Chu L, Chen L, Yang JS. Anterior transcorporeal approach of percutaneous endoscopic cervical discectomy for disc herniation at the C4‐C5 levels: a technical note. Spine J. 2016;16:659–66. [DOI] [PubMed] [Google Scholar]
- 19. Ahn Y, Keum HJ, Shin SH. Percutaneous endoscopic cervical discectomy versus anterior cervical discectomy and fusion: a comparative cohort study with a five‐year follow‐up. J Clin Med. 2020;9:undefined. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang C, Wu J, Zheng W, Li C, Zhou Y. Posterior endoscopic cervical decompression: review and technical note. Neurospine. 2020;17:S74–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhang Y, Ouyang Z, Wang W. Percutaneous endoscopic cervical foraminotomy as a new treatment for cervical radiculopathy: a systematic review and meta‐analysis. Medicine (Baltimore). 2020;99:e22744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shen J, Telfeian AE, Shaaya E, Oyelese A, Fridley J, Gokaslan ZL. Full endoscopic cervical spine surgery. J Spine Surg. 2020;6:383–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhang C, Wu J, Xu C, Zheng W, Pan Y, Li C, et al. Minimally invasive full‐endoscopic posterior cervical foraminotomy assisted by O‐arm‐based navigation. Pain Physician. 2018;21:E215–23. [PubMed] [Google Scholar]
- 24. Lee SH, Lee JC, Tauchi R, Daniel Riew K. Influence of the number of cervical fusion levels on cervical spine motion and health‐related quality of life. Spine (Phila Pa 1976). 2016;41(8):E474–80. [DOI] [PubMed] [Google Scholar]
- 25. Wan Q, Zhang D, Li S, Liu W, Wu X, Ji Z, et al. Posterior percutaneous full‐endoscopic cervical discectomy under local anesthesia for cervical radiculopathy due to soft‐disc herniation: a preliminary clinical study. J Neurosurg Spine. 2018;29:351–7. [DOI] [PubMed] [Google Scholar]
- 26. Lee U, Kim CH, Chung CK, Choi Y, Yang SH, Park SB, et al. The recovery of motor strength after posterior Percutaneous endoscopic cervical Foraminotomy and discectomy. World Neurosurg. 2018;115:e532–8. [DOI] [PubMed] [Google Scholar]


