Abstract
Objective
To evaluate the clinical curative effect of Ilizarov external fixation and ankle arthrodesis in the treatment of elderly traumatic ankle arthritis.
Methods
From June 2013 to August 2019, 72 patients with elderly traumatic ankle arthritis were treated with arthrodesis through Ilizarov external fixation technique in our institution. Conventional double‐feet standing X‐ray films were taken before and after operation. The tibiotalar angle on X‐ray image was measured to evaluate the degree of talipes varus and valgus. The Foot and Ankle pain score of American Orthopaedics Foot and Ankle Society (AOFAS) and Visual Analog Scale (VAS) were compared by using paired t‐test to evaluate the functional recovery.
Results
All of the patients acquired effective postoperative 18–49 months follow‐up, with an average of 31.5 months. All patients were included in the analysis, among which 38 cases were males and 34 cases were females, with an average of 65.4 years (ranging from 60 to 74). All ankles achieved bony fusion; the clinical healing time was 12.7 weeks on average (11–18 weeks). The AOFAS score was 45.36 ± 6.43 preoperatively and 80.25 ± 9.16 at 12 months post‐operation, with a statistically significant difference (p < 0.0001). The VAS score was 8.56 ± 1.85 on average preoperatively and 2.72 ± 0.83 at 12 months post‐operation, with a statistically significant difference (p < 0.0001). The tibiotalar angle was 101.93° ± 4.12° preoperatively and 94.45° ± 2.37° at 12 months post‐operation, with a statistically significant difference (p < 0.0001). The results of the functional evaluation indicated that 44 patients (61.1%) had excellent results, 18 (25%) had good results, and 10 (13.9%) had fair results.
Conclusion
Our study demonstrated that it is possible to obtain satisfactory outcome with Ilizarov external fixation and ankle arthrodesis in the treatment of elderly traumatic ankle arthritis.
Keywords: arthrodesis, elderly traumatic ankle arthritis, end‐stage, Ilizarov external fixation
Elderly traumatic ankle arthritis brings much inconvenience to patients' daily lives; surgical treatment is usually demanding and challenging. This study aimed to evaluate the clinical curative effect of Ilizarov external fixation and ankle arthrodesis in the treatment of elderly traumatic ankle arthritis. Satisfactory curative effect can be obtained through Ilizarov external fixation and ankle arthrodesis in the treatment of elderly traumatic ankle arthritis.
Introduction
Traumatic ankle osteoarthritis is characterized by a series of pathological changes, including ankle joint cartilage degeneration, intra‐articular inflammation, secondary hyperplasia, and ossification. 1 , 2 In recent years, with the aging of the society and the extension of the life span of the population, the research on the prevention and treatment of degenerative diseases in elderly patients has become a multidisciplinary and active research topic. Elderly traumatic ankle arthritis brings about disadvantages to routine activities and quality of life, such as pain and activity restriction. 3 Epidemiological studies 4 have shown that the causes of ankle joint osteoarthritis include peripheral fractures of the ankle (62%), ligament injury (16%), secondary reasons (13%) such as rheumatoid arthritis, hemophilia, and osteonecrosis, as well as the primary lesions (9%). Compared to other lower limbs arthritis, ankle osteoarthritis arises at a younger age and progresses faster, developing into end‐stage within 10–20 years after the initial injury. 5
Since elderly traumatic ankle arthritis brings much inconvenience to patients' daily lives, surgical treatment is usually demanding and challenging. 6 Although the implant materials are experiencing continuous development, total ankle arthroplasty is still limited to patients with low activity requirements, patients with lightweight, approximately typical bony structure, and fine bone and soft tissue condition. 7 , 8 Ankle arthrodesis is deemed as the gold standard in the management of end‐stage ankle arthritis. 9 As a limb‐sparing operation, ankle arthrodesis is a crucial alternative in patients with severe ankle pathologic conditions that may warrant a below‐knee amputation. 10 More than 40 different surgical techniques have been described to achieve ankle arthrodesis, such as plate fixation, screw fixation, Ilizarov external fixation, Taylor external fixation, and arthroscopic ankle arthrodesis, etc. 6 , 10 Despite the many technologies proposed for ankle arthrodesis, it is frequently associated with comorbidities including hindfoot arthritis, delayed or nonunion, tibial stress fractures, infection, and compromised wound healing, which can subsequently result in a prolonged period of hospitalization and rehabilitation. 11 , 12
The application of circumferential fixation for ankle arthrodesis was first introduced by Ilizarov. 13 The rationale of using the Ilizarov circular frame is to provide dynamic axial compression and fixed stable angle fixation, the percutaneous technique is reasonably helpful in case of chronic deformity and poor skin conditions and to avoid using internal fixation materials in case of infection. 14 , 15 The Ilizarov method has been proved useful in many complicated issues and contributes a favorable effect on improving the patient quality of life. 16 , 17 , 18 However, reports about the effects of arthrodesis through Ilizarov external fixation on elderly traumatic ankle arthritis are still lacking. Thus, the present study aimed to retrospectively analyze the data on arthrodesis through Ilizarov external fixation in the treatment of elderly traumatic ankle arthritis in our institution to: (i) evaluate the feasibility and application prospects of Ilizarov external fixation for elderly traumatic ankle arthritis; (ii) summarize the advantages of this technique in terms of motor function promotion, pain alleviation, and deformity correction; (iii) analyze the complications and prevention measures, providing a reference for future management of elderly traumatic ankle arthritis through Ilizarov external fixation.
Patients and Methods
Patient Characteristics
From June 2013 to August 2019, 72 patients with elderly traumatic ankle arthritis were treated with arthrodesis through Ilizarov external fixation technique in our institution. Conventional double‐feet standing X‐ray films were taken before and after operation. This study was carried out in the orthopaedics trauma center in our institution, which was mandated by the ethics committee of the hospital (Ethics Code: 2021 Review 251). The imaging materials and original medical records of these elderly traumatic ankle arthritis patients were inspected by two senior orthopaedic surgeons who took no part in the surgery. The inclusion criteria complied with the PICOS principle. Patients included were: (i) diagnosed with end‐stage traumatic ankle arthritis; (ii) conservative treatment was ineffective for more than a year; (iii) over 60 years old; (iv) unilateral ankle affected. Exclusion criteria included: (i) bilateral lesions; (ii) younger than 60 years; (iii) severe systemic illness; (iv) current acute ankle infections.
Operative Technique
Anesthesia and Position
The operation was performed under general anesthesia. After anesthesia, the patient was set in a horizontal position, with the hip of the affected side being blocked up.
Approach and Exposure
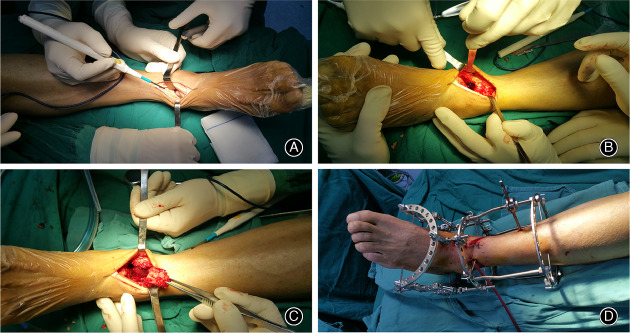
Through a 12‐cm midline longitudinal incision in the anterior lower part of the shank and along the talus, the skin, subcutaneous tissue, and the fascia were cut through layer by layer. The joint capsule was incised between the extensor hallucis longus tendon and the extensor digitorum longus tendon, the ankle was exposed ( Fig. 1A ), and the joint surface was cleaned.
Fig. 1.
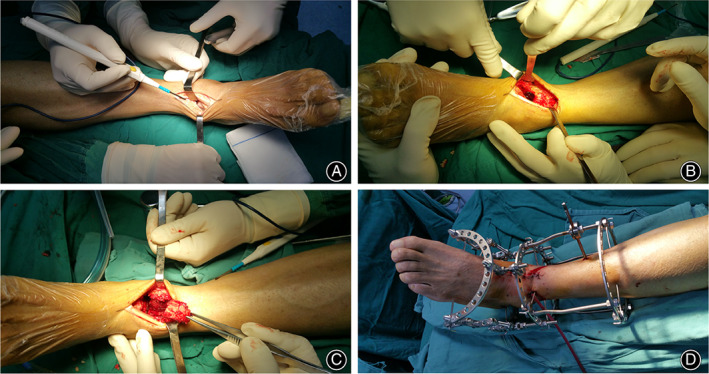
The surgical procedure. (A) exposure of ankle; (B) debridement of articular cartilage and sclerosis subchondral bone; (C) the harvest of cancellous bone; (D) installation of Ilizarov external frame
Pathological Changes and Resection
Articular cartilage and sclerosis subchondral bone were debrided with an osteotome, chisel, and curet until a large amount of fresh blood oozed from the bone surface, then rinsed repeatedly with saline water (Figure Fig. 1B ). A 4 × 3 × 1 cm bone block was harvested using osteotome at the distal tibia (Figure Fig. 1C ), rinsed repeatedly with saline water; the bleeding was closed with bone wax.
Fixation and Reconstruction
The Ilizarov circular frame was assembled step by step from the tibia to the ankle and then to the foot. The gyration center of ankle was connected to the gyration center of the Ilizarov circular frame, and the lower leg was placed in the central part of the circular frame, a Kirschner wire was then drilled through distal end of tibia. Two Kirschner wires were drilled crosswise through the lower middle tibia to secure the near‐end framework; following the adjustment of the gyration center, a Kirschner wire was drilled across the middle inferior part of metatarsal 1–5 in an inside‐out order. The foot fulcrum ring was fixed from the inside out perpendicular to the heel bone with a Kirschner wire. Two semi‐wires were placed behind the heel bone avoiding the tendo calcaneus, and a Kirschner wire was placed medial to the first metatarsal (Figure Fig. 1D ). The separated autogenous bone was squashed and filled into the ankle space, then covered using a gelfoam. The Ilizarov circular frame was fixed at 90° of the ankle joint after pressing.
Postoperative Treatment
Physical therapy, wound care, and disinfection of pin tracts were regularly exerted after the operation. The nuts of hinges were carefully adjusted when the local swelling of the lower extremity subsided. The skin color, sensation, and tension of limbs were observed closely during the process of treatment. Patients were encouraged to take early weight‐bearing walks with Ilizarov fixators, which were dismantled at 3 months on average.
Radiographic Evaluation
Radiographic examination was performed to evaluate the bony fusion and deformity correction. The angle between the tibia anatomic axis and the line segment of inside and outside of talus vertex was measured and defined as tibiotalar angle (TA).
Functional Evaluation
Postoperative follow‐up and physical examination were conducted by two senior clinical investigators of our group. Patients were explicitly inquired about their overall feeling with the external frames, restrictions of daily activities, ankle condition, postoperative complications, and other follow‐up treatment. Visual analog scale (VAS) scale and American Orthopaedic Foot and Ankle Society (AOFAS) scale were adopted to evaluate the functional recovery. The AOFAS score system includes nine aspects: pain, maximum walking distance, function, walking surfaces, sagittal motion, gait abnormality, ankle hindfoot stability, hindfoot motion, and alignment. The VAS was tested through a 10‐cm line with 0 on the left indicating “painless” while 10 on the right indicating “the most pain.” Functional recovery was divided into four classes: excellent, no pain, limping or restrictions of daily activities, with X‐ray film confirmed bony fusion; Good, slight pain, occasional claudication and movement are slightly limited, with X‐ray film confirmed bony fusion; Fair, moderate pain, limping and activity limitations, with X‐ray film confirmed bony fusion; Poor, pain obviously, with failed bony fusion.
Statistical Analysis
Statistical analyses were carried out via Statistical Package for the Social Sciences (SPSS 19.0, IBM, NYC, USA). All data were expressed as the mean value ± standard deviation (SD). The TA, AOFAS score, and VAS score were compared by using paired t‐test, in which a p value of less than 0.05 was deemed statistically significant.
Results
General Results
The average operation time of 72 patients was 139.76 ± 17.34 min (range, 121–164 min). All of the patients acquired effective postoperative 18–49 months follow‐up, with an average of 31.5 months. All patients were included in the analysis, among which 38 cases were males and 34 cases were females, with an average of 65.4 years (ranging from 60 to 74, Table 1). Thirty‐three cases were on the left side, 39 cases were on the right side. The body mass index (BMI) was 24.9 ± 3.9 kg/m2. The duration of symptoms was 11.5 years (ranging from 6 to 38 years). Major comorbidities included smoking history (41, 56.9%), diabetes mellitus (23, 31.9%), osteomyelitis (19, 26.4%), rheumatoid arthritis (11, 15.3%), lower limb discrepancy (9, 12.5%), and peripheral vascular disease (6, 8.3%).
TABLE 1.
Baseline characteristics and comorbidities of the patients went through Ilizarov external fixation and ankle arthrodesis
| Variable | Value |
|---|---|
| Age (years) | 65.4 (60–74) |
| Gender (male/female) | 38/34 |
| BMI (kg/m2) | 24.9 ± 3.9 |
| Side (left/right) | 33/39 |
| Duration of symptoms (years) | 11.5 (6–38) |
| Postoperative follow‐up (months) | 31.5 (18–49) |
| Smoking history | 41 (56.9%) |
| Diabetes mellitus | 23 (31.9%) |
| Osteomyelitis | 19 (26.4%) |
| Rheumatoid arthritis | 11 (15.3%) |
| Lower limb discrepancy | 9 (12.5%) |
| Peripheral vascular disease | 6 (8.3%) |
Abbreviation: BMI, body mass index.
Radiographic Improvement
All ankles achieved bony fusion; the clinical healing time was 12.7 weeks on average (11–18 weeks). Typical cases are shown in Figures Fig. 2 and Fig. 3. The TA was 101.93° ± 4.12° preoperatively and 94.45° ± 2.37° at 12 months post‐operation, with a statistically significant difference (p < 0.0001).
Fig. 2.

Typical case, female, 63 years old, pain after right ankle sprain for 10+ years. Diagnosis: Right ankle traumatic arthritis. (A) preoperative anteroposterior and lateral X‐ray films. (B) postoperative anteroposterior and lateral X‐ray films. (C) anteroposterior and lateral X‐ray films 6 months after the operation. (D) anteroposterior and lateral X‐ray films 12 months after the operation
Fig. 3.

Typical case, female, 68 years old, trauma caused right talus fracture 1+ years after surgery, walking pain 10+ months. Diagnosis: Right ankle traumatic arthritis. (A) preoperative anteroposterior and lateral X‐ray films. (B) postoperative anteroposterior and lateral X‐ray films. (C) anteroposterior and lateral X‐ray films 6 months after the operation. (D) anteroposterior and lateral X‐ray films 12 months after the operation
Functional Evaluation
The VAS score was 8.56 ± 1.85 on average preoperatively and 2.72 ± 0.83 at 12 months post‐operation, with a statistically significant difference (p < 0.0001, Table 2). The AOFAS score was 45.36 ± 6.43 preoperatively and 80.25 ± 9.16 at 12 months post‐operation, with a statistically significant difference (p < 0.0001). The results of the functional evaluation indicated that 44 patients (61.1%) had excellent results, 18 (25%) had good results, and 10 (13.9%) had fair results.
TABLE 2.
Pre‐operation and post‐operation evaluation data
| Pre‐operation | Post‐operation | t Value | p value | |
|---|---|---|---|---|
| VAS score | 8.56 ± 1.85 | 2.73 ± 0.87 | 24.41 | p < 0.0001 |
| AOFAS score | 45.36 ± 6.43 | 80.25 ± 9.16 | 26.45 | p < 0.0001 |
| TA | 101.93° ± 4.12° | 94.45° ± 2.37° | 13.35 | p < 0.0001 |
Complications
During the observation period, no continuous bleeding appeared in the incision area and pin tracts. Nine patients (12.5%, Table 3) developed slight pin tract infection, all settled with local wound care and antibiotic treatment. The radiograph results of seven patients (9.7%) indicated anterior dislocation of the talus; the problem was fixed shortly by adjusting the structure of the external fixator and tractive reduction. Five patients (6.94%) appeared with different degrees of midfoot pain, which was solved by taking nonsteroidal anti‐inflammatory drugs (NSAIDs).
TABLE 3.
Postoperative complications description of the patients
| Variable | Value |
|---|---|
| Pin tracts infection | 9 (12.5%) |
| Anterior dislocation of the talus | 7 (9.7%) |
| Midfoot pain | 5 (6.9%) |
Discussion
Our study indicated that Ilizarov external fixation and ankle arthrodesis ensures a high bony fusion rate and a satisfactory pain relief effect, corrects the deformity, and significantly improves ankle function for elderly traumatic ankle arthritis. The postoperative AOFAS scores and VAS scores were markedly improved compared with the preoperative values.
The Feasibility and Application Prospects of Ilizarov External Fixation
There are more than 40 surgery techniques reported in the works of literature, ranging from intramedullary nail to screw fixation, plate‐screw fixation, and external fixation technology. 3 , 10 , 19 , 20 Even though internal fixation is the most commonly used method for ankle arthrodesis up to now, the role of other techniques of fixation and stabilization has become increasingly apparent since complex ankle lesions have increased. Both internal and external fixation showed positive effects in obtaining reliable fixation, fusion, and reducing infection. 21 , 22 The drawbacks and advantages of each fusion strategy should be taken into account in determining the course of treatment so as to acquire an optimal clinical effect. 23
The Advantages of Ilizarov External Fixation
With a modular circular external fixator, the Ilizarov technique has demonstrated many advantages in ankle arthrodesis of complex cases, especially with comorbidities like bone defects, length discrepancies, distal tibia lesions, or the need for early ambulation with weight‐bearing, etc. 24 , 25 The characteristics of dynamic axial compression, and capacity to resist bending, torque, and shearing, enable the choice of early ambulation with weight‐bearing, which makes it an ideal fixation instrument in the management of complex ankle lesions. 25 , 26 Unlike internal fixation, Ilizarov external fixation arthrodesis technology can be used in cases where the bone and soft tissue conditions are poor, which can be used as first phase treatment in subjects with active infection. 27 Continuous compression or distraction by the circular frame can provide excellent mechanical stability, which allows the surgeon to rectify the alignment and compress or distract during or after the operation. 28 This provides a more desirable choice for patients deemed improper for reliable screw fixation.
Another advantage of the Ilizarov technique for ankle arthrodesis is its capacity to equilibrate the length discrepancy of lower extremities via simultaneous tibial lengthening through distraction osteogenesis. 29 Distal tibia osteotomy in the process of ankle arthrodesis has also been demonstrated to help accelerate bony fusion at the contact surface. 30 Apart from extremity lengthening, the theory of distraction osteogenesis can be applied to the adjustment of malalignment. 31 The capability to rectify the position and alignment of the forefoot and hindfoot by modulating the circular frame when needed in the course of regeneration is a distinct advantage of the Ilizarov technique. 32 Using these frames, any intraoperative errors can be addressed, early postoperative loss of position can be rectified, severe malalignment, septic arthritis, and failed fusion can be treated with a higher rate of success. 33 Hoover et al. 34 compared conventional crossed‐screw internal fixation to double external ankle fixation; the latter turned out to be more rigid constraints in both torsion and bending when compared to conventional crossed‐screw technique. A biomechanical study proved that cancellous bone screws provided better anti‐rotation stress in human specimens with superior bone quality. 35 In contrast, the external fixation demonstrated better anti‐rotation stress in models with poorer bone quality. 36 Moreover, the screw fixation is invalid in osteopenic models. 37
Management of Complications and Comorbidities
The Ilizarov technique is not without its drawbacks, including Kirschner wire breakage, incremental risk of superficial pin track infections, likely discomfort caused by circular external fixator, and so forth; with suitable peri‐operative care, especially proper postoperative nursing, these conditions can be reasonably solved. 38 Our study indicated that fair results could be acquired in these settings. If the patients are associated with comorbidities such as malignancy, significant vascular disease, diabetes, chronic hypoxia, severe scarring, malnutrition, liver or kidney failure, chronic lymphedema, immune deficiency, or long‐term smoking, ankle arthrodesis would be more challenging. 20 , 22 , 39 , 40 Being hard for bony fusion, these patients used to have no choice but to take the non‐operative therapy or amputation. Ilizarov external fixation technique has been used as the last limb salvage treatment for these complex cases and achieved a pleasing effect. 41 , 42 Kugan et al. 43 reported 48 cases with multiple comorbidities and treated with Ilizarov external fixation technology, the ankle fusion rate was 83%, and the patients’ postoperative clinical function improved significantly, without recurrence of deep primary infection. Although a few foreseeable complications do exist, such as needle breakage and pin site infection, they can be effectively resolved if they are detected in time and treated appropriately. Ilizarov external fixation technology thus can be used as an effective alternative to amputation in such patients. 44
Limitations
This study has several limitations. Firstly, the relatively small sample size. However, this is a single‐center study, and data are homogeneous thus eliminating the potential confounding factors. However, a multicentric study with more patients evaluated could better address the aims of the study. Secondly, this is a retrospective study. The risk factors we could analyze were restricted to the patients’ medical records.
Conclusion
To sum up, the treatment of elderly traumatic ankle arthritis is still a challenging problem; comprehensive consideration should be made based on lesion degree of ankle joint and hindfoot, comorbidities, the general condition, and relative risk factors. In addition, careful clinical and radiographic assessments help ensure rational decision‐making. A satisfactory curative effect can be obtained through Ilizarov external fixation and ankle arthrodesis in the treatment of elderly traumatic ankle arthritis. Attention should be paid to dynamic mechanical and gait analysis for patients who choose ankle arthrodesis and cohort outcomes should be compared in future studies. Future research should also focus on new types of 3D printed orthopaedic devices and nanoscale drug delivery technologies to achieve optimal therapeutic outcomes for these diseases.
COMPETING INTEREST
The authors declare that they have no competing interests.
AUTHOR CONTRIBUTIONS
Conceptualization, writing review and editing: Jun Li. Data analysis: Wenzhao Wang, Hai Yang. Data Curation: Bohua Li. Project administration: Lei Liu. All authors have read and approved the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethics approval was obtained from the Institutional Review Boards of West China Hospital, Sichuan University. All methods were performed following the relevant guidelines and regulations (Declaration of Helsinki).
AUTHORSHIP DECLARATION
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, all authors are in agreement with the manuscript.
ACKNOWLEDGMENTS
This study received funding from the National Natural Science Fund of China (NO. 81874002); the National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University (Z20192013); China Postdoctoral Science Foundation (2021M692279); West China hospital postdoctoral research and development fund (2019HXBH068); “Zero to One” Innovation Research Project of Sichuan University (2022SCUH0014). The authors thank Lihong Zhao for her warm help during the clinical case follow‐up and data collection.
REFERENCES
- 1. Alammar Y, Sudnitsyn A, Neretin A, Leonchuk S, Kliushin NM. Closed arthrodesis in infected neuropathic ankles using Ilizarov ring fixation. Bone Jt J. 2020;102‐b:470–7. [DOI] [PubMed] [Google Scholar]
- 2. Ewalefo SO, Dombrowski M, Hirase T, Rocha JL, Weaver M, Kline A, et al. Management of posttraumatic ankle arthritis: literature review. Curr Rev Musculoskelet Med. 2018;11:546–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Delco ML, Kennedy JG, Bonassar LJ, Fortier LA. Post‐traumatic osteoarthritis of the ankle: a distinct clinical entity requiring new research approaches. J Orthop Res. 2017;35:440–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Santos AL, Demange MK, Prado MP, Fernandes TD, Giglio PN, Hintermann B. Cartilage lesions and ankle osteoarthrosis: review of the literature and treatment algorithm. Rev Bras Ortop. 2014;49:565–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Braito M, Dammerer D, Kaufmann G, Fischler S, Carollo J, Reinthaler A, et al. Are our expectations bigger than the results we achieve? A comparative study analysing potential advantages of ankle arthroplasty over arthrodesis. Int Orthop. 2014;38:1647–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Suo H, Fu L, Liang H, Wang Z, Men J, Feng W. End‐stage ankle arthritis treated by ankle arthrodesis with screw fixation through the Transfibular approach: a retrospective analysis. Orthop Surg. 2020;12:1108–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kwon DG, Chung CY, Park MS, Sung KH, Kim TW, Lee KM. Arthroplasty versus arthrodesis for end‐stage ankle arthritis: decision analysis using Markov model. Int Orthop. 2011;35:1647–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li J, Lai Y, Li M, Chen X, Zhou M, Wang W, et al. Repair of infected bone defect with clindamycin‐tetrahedral DNA nanostructure complex‐loaded 3D bioprinted hybrid scaffold. Chem Eng J. 2022;435:134855. [Google Scholar]
- 9. Weatherall JM, Mroczek KJ, Mclaurin TM, Ding BC, Tejwani NC. Post‐traumatic ankle arthritis. Bull Hosp Jt Dis. 2013;71(1):104–12. [PubMed] [Google Scholar]
- 10. Gharehdaghi M, Rahimi H, Mousavian A. Anterior ankle arthrodesis with molded plate: technique and outcomes. Arch Bone Jt Surg. 2014;2:203–9. [PMC free article] [PubMed] [Google Scholar]
- 11. Gorman TM, Beals TC, Nickisch F, Saltzman CL, Lyman M, Barg A. Hindfoot arthrodesis with the blade plate: increased risk of complications and nonunion in a complex patient population. Clin Orthop Relat Res. 2016;474:2280–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang C, Xu C, Li M, Li H, Wang L, Zhong D, et al. Arthroscopic ankle fusion only has a limited advantage over the open operation if osseous operation type is the same: a retrospective comparative study. J Orthop Surg Res. 2020;15:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gubin AV, Borzunov DY, Marchenkova LO, Malkova TA, Smirnova IL. Contribution of G.A. Ilizarov to bone reconstruction: historical achievements and state of the art. Strategies Trauma Limb Reconstr. 2016;11:145–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li J, Li M, Wang W, Li B, Liu L. Evolution and development of Ilizarov technique in the treatment of infected long bone nonunion with or without bone defects. Orthop Surg. 2022;14:824–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rozis M, Benetos I, Afrati SR, Polyzois VD, Pneumaticos SG. Results and outcomes of combined cross screw and Ilizarov external fixator frame in ankle fusion. J Foot Ankle Surg. 2020;59:337–42. [DOI] [PubMed] [Google Scholar]
- 16. Illgner U, Budny T, Frohne I, Osada N, Siewe J, Wetz HH. Clinical benefit and improvement of activity level after reconstruction surgery of Charcot feet using external fixation: 24‐months results of 292 feet. BMC Musculoskeletal Disord. 2014;15:392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu Z, Xu C, Yu YK, Tu DP, Peng Y, Zhang B. Twenty years development of Tibial cortex transverse transport surgery in PR China. Orthop Surg. 2022;14:1034–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Slater GL, Sayres SC, O'Malley MJ. Anterior ankle arthrodesis. World J Orthop. 2014;5:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Popkov AV, Kononovich NA, Gorbach EN, Tverdokhlebov SI, Irianov YM, Popkov DA. Bone healing by using Ilizarov external fixation combined with flexible intramedullary nailing versus Ilizarov external fixation alone in the repair of tibial shaft fractures: experimental study. Sci World J. 2014;2014:239791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yasui Y, Hannon CP, Seow D, Kennedy JG. Ankle arthrodesis: a systematic approach and review of the literature. World J Orthop. 2016;7:700–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li J, Li B, Zhang Z, Wang S, Liu L. Ilizarov external fixation versus plate internal fixation in the treatment of end‐stage ankle arthritis: decision analysis of clinical parameters. Sci Rep. 2017;7:16155–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rabinovich RV, Haleem AM, Rozbruch SR. Complex ankle arthrodesis: review of the literature. World J Orthop. 2015;6:602–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nguyen MP, Pedersen DR, Gao Y, Saltzman CL, Amendola A. Intermediate‐term follow‐up after ankle distraction for treatment of end‐stage osteoarthritis. J Bone Jt Surg Am. 2015;97:590–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fragomen AT, Borst E, Schachter L, Lyman S, Rozbruch SR. Complex ankle arthrodesis using the Ilizarov method yields high rate of fusion. Clin Orthop Relat Res. 2012;470:2864–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Morasiewicz P, Dejnek M, Orzechowski W, Urbański W, Kulej M, Dragan SŁ, et al. Clinical evaluation of ankle arthrodesis with Ilizarov fixation and internal fixation. BMC Musculoskeletal Disord. 2019;20:167–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Malkova TA, Borzunov DY. International recognition of the Ilizarov bone reconstruction techniques: current practice and research (dedicated to 100(th) birthday of G. A Ilizarov). World J Orthop. 2021;12:515–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Li Y‐X, Liu X, Chen Y, Gan T‐J, Qin B‐Q, Ren Y, et al. Tibial cortex transverse distraction followed by open correction with internal fixation for management of foot and ankle deformity with ulcers. Orthop Surg. 2021;13:2081–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zang J, Sudnitsyn AS, Mo Z, Jiao S, Shi L, Zhao L, et al. Improved Ilizarov method for management of deformity and ulceration on foot and ankle of spina bifida. J Orthop Translat. 2021;28:140–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Khanfour AA. Versatility of Ilizarov technique in difficult cases of ankle arthrodesis and review of literature. Foot Ankle Surg. 2013;19:42–7. [DOI] [PubMed] [Google Scholar]
- 30. Nozaka K, Miyakoshi N, Kashiwagura T, Kasukawa Y, Saito H, Kijima H, et al. Effectiveness of distal tibial osteotomy with distraction arthroplasty in varus ankle osteoarthritis. BMC Musculoskeletal Disord. 2020;21:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. He X, Zhang H‐L, Hu Y‐C. Limb salvage by distraction osteogenesis for distal Tibial osteosarcoma in a young child: a case report. Orthop Surg. 2016;8:253–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wei M, Chen J, Guo Y, Sun H. The computer‐aided parallel external fixator for complex lower limb deformity correction. Int J Comput Assist Radiol Surg. 2017;12:2107–17. [DOI] [PubMed] [Google Scholar]
- 33. Bliven EK, Greinwald M, Hackl S, Augat P. External fixation of the lower extremities: biomechanical perspective and recent innovations. Injury. 2019;50(Suppl 1):S10–7. [DOI] [PubMed] [Google Scholar]
- 34. Hoover JR, Santrock RD, James WC 3rd. Ankle fusion stability: a biomechanical comparison of external versus internal fixation. Orthopedics. 2011;34(4). [DOI] [PubMed] [Google Scholar]
- 35. Cardoso GS, Amorim R, Penha FM, Horn FJ, Roesler CR, Marques JL. Biomechanical analysis of the behaviour at the metaphyseal‐diaphyseal junction of complex Tibial plateau fractures using two circular fixator configurations. Strategies Trauma Limb Reconstr. 2020;15:138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bestwick‐Stevenson T, Wyatt LA, Palmer D, Ching A, Kerslake R, Coffey F, et al. Incidence and risk factors for poor ankle functional recovery, and the development and progression of posttraumatic ankle osteoarthritis after significant ankle ligament injury (SALI): the SALI cohort study protocol. BMC Musculoskeletal Disord. 2021;22:362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Biz C, Hoxhaj B, Aldegheri R, Iacobellis C. Minimally invasive surgery for tibiotalocalcaneal arthrodesis using a retrograde intramedullary nail: preliminary results of an innovative modified technique. J Foot Ankle Surg. 2016;55:1130–8. [DOI] [PubMed] [Google Scholar]
- 38. Grivas TB, Magnissalis EA. The use of twin‐ring Ilizarov external fixator constructs: application and biomechanical proof‐of principle with possible clinical indications. J Orthop Surg Res. 2011;6:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Belluzzi E, Olivotto E, Toso G, Cigolotti A, Pozzuoli A, Biz C, et al. Conditioned media from human osteoarthritic synovium induces inflammation in a synoviocyte cell line. Connect Tissue Res. 2019;60:136–45. [DOI] [PubMed] [Google Scholar]
- 40. Sandiford N, Wong F, Back D, Chan O. Ankle arthrodesis in patients with haemophilia‐associated ankle arthropathy—does the technique influence the outcome? Foot. 2022;101908:101908. [DOI] [PubMed] [Google Scholar]
- 41. Biz C, Crimì A, Fantoni I, Vigo M, Iacobellis C, Ruggieri P. Functional outcome and complications after treatment of comminuted tibial fractures or deformities using Ilizarov bone transport: a single‐center study at 15‐ to 30‐year follow‐up. Arch Orthop Trauma Surg. 2021;141:1825–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ramos T, Ekholm C, Eriksson BI, Karlsson J, Nistor L. The Ilizarov external fixator‐‐a useful alternative for the treatment of proximal tibial fractures. A prospective observational study of 30 consecutive patients. BMC Musculoskeletal Disord. 2013;14:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kugan R, Aslam N, Bose D, McNally MA. Outcome of arthrodesis of the hindfoot as a salvage procedure for complex ankle pathology using the Ilizarov technique. Bone Jt J. 2013;95:371–7. [DOI] [PubMed] [Google Scholar]
- 44. Paget LDA, Aoki H, Kemp S, Lambert M, Readhead C, Stokes KA, et al. Ankle osteoarthritis and its association with severe ankle injuries, ankle surgeries and health‐related quality of life in recently retired professional male football and rugby players: a cross‐sectional observational study. BMJ Open. 2020;10:e036775. [DOI] [PMC free article] [PubMed] [Google Scholar]


