Abstract
The effects of the COVID-19 pandemic on mental health are likely to worsen as the epidemic progresses and will last long even after the pandemic has passed. The present study developed a coronaphobia scale during the pandemic to measure its psychological effects such as fear, anxiety, and depression in the majority of the cases in the United Arab Emirates (UAE). It is a 35-item scale that measures anxiety symptoms connected with COVID-19 and may be used to identify people who require mental health treatment. Based on 618 adults, the reliability and validity of these items were appropriate. The scales were distributed via social media using a Google form. Internal consistency, reliability analysis, and structural equation models, particularly confirmatory factor analysis, were carried out. The elevated scores on the coronaphobia scale were associated with social phobia, anxiety, stress, and depression. The coronaphobia score distinguishes well between those with and without dysfunctional anxiety (85% specificity and 90% sensitivity). These results support the coronaphobia scale as a valid and effective tool for clinical practice and research.
Keywords: Development, Coronaphobia scale, COVID-19, Psychometric, UAE
Development; Coronaphobia scale; COVID-19; Psychometric; UAE.
1. Introduction
The greatest challenge experienced by humanity in the 21st century is the negative impact of the Corona Virus Disease, 2019 (COVID-19) on the population’s mental health. This virus was initially identified in Wuhan, a city in China. The virus causes severe acute respiratory syndrome (Silva et al., 2020). World Health Organization March 2020 declared it as the state of the pandemic because of the rapid increase in the number of COVID-19 cases, deaths, and speed of infection (Ghebreyesus, 2020).
It has been known that the population affected by the virus experienced emotional distress and psychological symptoms (Brooks et al., 2020; Gualano et al., 2020). The individuals affected by COVID-19 are likely to experience mental health issues due to the fear of death and extended periods of social isolation (Taylor, 2019a, Taylor, 2019b; Torales et al., 2020; Raphael, 2006; Xiang et al., 2020). Some previous studies have shown that increases in mental health issues due to COVID-19 have also resulted in an increased level of anxiety, denial, fear, stress, depression, insomnia, and anger among individuals (Roy et al., 2020; Zandifar and Badrfam, 2020; Cao et al., 2020; Wang et al., 2020). A study conducted by Becerra-Garcia et al. (2020) about how different countries around the world were forced to adopt quarantine measures during the pandemic. The study analyzed different psychopathological symptoms shown by the Spanish population during lockdown due to COVID-19. These were based on socio-demographic, occupational, and environmental contexts. The results of the study showed that groups based on socio-demographics and occupational-context variables had high psychological issues.
Another study by Barbeito et al. (2021) examined the public interest existing on the internet by examining VRBs in Google Trends related to various mental health issues and their association with COVID-19 in Spain. The study found that anxiety as a mental health problem has gained public interest on the internet in the context of COVID-19. The study also found that public concern arisen after a week after the rise in the cases of COVID-19 and is even greater after introducing control measures that restricted any type of mobility or activity. The study concluded that there is a need for information about anxiety at a specific time as the pandemic is evolving.
Post-traumatic stress disorder (PTSD) mainly focuses on disaster mental health research; however, there is no evidence regarding psychological symptoms amid the COVID-19 pandemic that fulfills PTSD diagnostic criteria (Raphael, 2006; Liu et al., 2020). Similar to the outbreaks like H1N1 (Barbeito et al., 2021) and SARS (Wheaton et al., 2012), anxiety symptoms are seen foreseeably. One of the recent studies by Rajkumar (2020) revealed anxiety as the most common symptom among various mental health symptoms. There is an association between high anxiety levels and socially disrupted behaviors such as exaggerated interpretation of minor symptoms and panic-buying (Cheng et al., 2004). An association has also been observed between increased anxiety levels regarding viral contagion and certain adaptive behaviors that include maintaining social distancing, handwashing, and getting vaccinated (Rajkumar, 2020).
As observed in the previous pandemics, there is an increase in anxiety levels with other psychopathologies among individuals (Liu et al., 2020; Asmundson and Taylor, 2020). One of the previous studies showed that individuals display specific forms of anxiety-related stress in viral outbreaks; although, there might be a similarity between symptoms of COVID-19 and generalized anxiety (Taylor, 2019a, Taylor, 2019b). For instance, Wang et al. (2020) showed that most individuals displayed extreme fear of getting infected, along with continuous worry about their family members, despite maintaining social distancing and following other safety precautions.
Anxiety associated with COVID-19 is also influenced by health risk perception related to the probability of contracting the virus (Maunder et al., 2003). A study conducted by Commodari et al. (2020) evaluated the impact of psychological and socio-demographic variables on perceived personal and comparative susceptibility to the COVID-19 virus. The study found that only 5 percent of the participants believed that they would contract the virus even though 5.9 percent thought that this probability was higher than that of other people of the same age and gender. Moreover, the study found that gender and marital status positively affected the perceived risk of contracting the virus, and self-efficacy, empathy, and imagination were significant predictors of perceived personal susceptibility. The study suggests that to empower the population in adopting necessary preventive measures meant to stop the rapid growth of the virus, an adequate psycho-educational intervention program is a must to avoid disastrous consequences at both the health and economic level.
Similarly, another study by Ding et al. (2020) also aimed to study the construction of a conceptual framework for risk perception and depression of people in a public health crisis and examined how the mental health of people during the current crisis is affected by risk perception and factors associated with it such as distance perception of the crisis and support prevention and control policies. The findings of the study showed that risk perception and its factors had a significant impact on the mental health of people in a public health crisis. The study also suggests that risk perception plays a vital role in affecting the mental health of people in public health crisis therefore, such health policies aimed to improve the mental well-being of the people should consider risk perception. Some studies also focused on finding the impact of COVID-19 on the quality of life and mental health of specific populations such as students and pregnant women.
In line with this, a study conducted by Biviá-Roig et al. (2020) aimed to evaluate the influence of confinement due to the current pandemic on eating, exercising, and quality of life habits among pregnant women in Spain. The study adopted an internet-based cross-sectional survey to collect data about diet, exercise, health-related quality of life information, and the perceived hurdles of pregnant women before and after confinement. The study results showed that there was a decrease in levels of physical activities as well as health-related quality of life levels. The number of hours spent sitting increased by 50 percent but there was no significant difference found in the eating habit of these respondents. The study concluded by suggesting that there is a need to implement specific online programs aimed to promote the culture of exercise which can help in reducing stress levels and improve health-related quality of life in pregnant women during the confinement period.
Another study by Commodari and La Rosa (2020) aimed to give a general overview of the perceived risk associated with COVID-19 and the psychological experience of quarantine among adolescents in Italy. The study used an online survey questionnaire to get a response about perceived health risks related to the pandemic, knowledge, and information on controlling the pandemic, opinions, and beliefs on stage 2 of the quarantine, and the psychological experiences related to it. The study results showed low perceived comparative susceptibility and seriousness but they were aware of the restriction measures mandatory to stop the spread of the virus and they also agreed to the restrictions and limitations imposed by the government. The female participants living in the red zone showed more psychologically negative feelings about the quarantine experience but no significant difference could be found in the regions where teenagers of the study sample lived, this result of the study led to the formulation of the hypothesis that participants negative feelings were perhaps more related to the adolescent period than the pandemic.
Recently, there is the emergence of certain measures to evaluate specific fears about COVID-19. In a similar context, the COVID-19 Peritraumatic Distress Index (CPDI) questionnaire was developed by Qiu et al. (2020) to assess various aspects of COVID-19 that included; depression, anxiety, and different phobias. The study was conducted in China, and the results revealed that psychological distress was experienced by approximately 35% of the total population. A more concise tool, Fear of COVID-19 (FCV–19S), was developed by Ahorsu et al. (2020) for addressing fear related to COVID-19. A total of 7 items were included in this scale after a thorough review of participant interviews, valid fear scales, and evaluations done by the experts. A stable unidimensional structure with robust psychometric properties is reported to assess the factor structure. Sakib et al. (2020) and Harper et al. (2021) adopted this scale in UK and India and, showed that the scale was sustainable for assessing psychometric properties and predicting the positive behavioral changes among individuals that include social distancing and maintaining hand hygiene. It has become significant to evaluate factor structure, psychometric properties, and imperative/culture-specific factors on a scale as COVID-19 has affected almost all the nations worldwide. In a similar context, one instrument named Cancer Worry Scale was developed by Lerman et al. (1991) that measured worry regarding various health-related aspects. This scale was adapted from Peruvian culture (Commodari et al., 2020b), which helped gauge the worry associated with the transmission of viruses affecting the respiratory system (Qiu et al., 2020). However, there is a need for a specific instrument to validate the measures of worry linked with COVID-19 transmission.
Recently, the Coronavirus Anxiety Scale (CAS) development has been observed for identifying the individuals affected by uncertainties and fear of increased pandemic crisis, particularly (Lerman et al., 1991). CAS is a five-item mental health assessment scale that helps in identifying the probable cases of individuals experiencing dysfunctional anxiety about the COVID-19 outbreak and crisis (Caycho-Rodríguez et al., 2018). The items present in this CAS scale help in tapping psychologically-based anxiety and fear reactions towards COVID-19. In one of the research studies by Asmundson and Taylor (2020), anxiety associated with COVID-19 is denoted as ‘Coronaphobia’. Ro et al. (2017) presented strong validity (construct and factorial-related), reliability (confirmatory factor analysis, exploratory factor analysis), and equivalent measurement across race, gender, and age of different individuals. The study also showed that scores attained through the CAS scale were associated with a diagnosis of COVID-19, coping with drug addiction, hopelessness, impairment, and suicidal ideation. These associations prove to support CAS as a measure of mental health status as there is a significant relationship between COVID-19 anxiety and clinical disturbances across interpersonal, behavioral, and psychological processes (Ahorsu et al., 2020).
COVID-19 has some significant social effects on individuals (Milman et al., 2020). Therefore, it is important to assess the psychometric characteristics for different regions because the responses may differ between different societies, rather than just comparing between translated versions. The researchers are aware of the role of anxiety in molding behavior during the viral epidemic and the risk that anxiety might lead to long-term mental health issues (Midorikawa et al., 2021). Mental health experts, public health decision-makers, and other stakeholders during the pandemic need access to data on the prevalence of anxiety and other negative psychological reactions in the communities. COVID-19-related measures have been developed in response to this problem. More objectively, among the existing tools, none has been validated for the UAE setting that can assess COVID-19 anxiety. Given the importance and urgency of the situation, there is a need for assistance by filling this gap and providing an instrument that can detect oscillations in COVID-19 anxiety levels. Therefore, the present study has created a collection of questions that can accurately measure this form of anxiety. As a result, it is both relevant and critical to construct a brief and valid tool to capture an individual's anxiety about COVID-19. It can contribute to building a broad and clear understanding of symptoms and how to deal with them and put the correct foundation for preparing appropriate treatment intervention programs. The study intended to develop a Coronaphobia scale consisting of thirty-eight items to evaluate psychometric (emotional and symptomatic properties) that impact the health of the United Arab Emirates (UAE) population during the pandemic.
2. Material and methods
2.1. Participants and procedure
The study adopted a convenience sampling technique to recruit participants from the social media platform (Twitter, Facebook) The study used convenience sampling as the study was conducted at the time of COVID-19 as the study using an online survey form (Tanner, 2018). The minimal sample size of this study was based on G∗ Power software. The study included 700 participants from UAE using the convenience sampling technique to fill the survey; 618 participants responded with an 88% response rate. Before the initiation of the project, the study was approved by the Ethical Committee of Ajman University, College of Humanities and Sciences, Ajman City, UAE on 28 June 2020 [Ethical No H–H–F-2020-June -28]. Each participant signed a written consent form which was sent along with the questionnaire. However, the participants are required to first fill out the consent form and send it back before proceeding to the actual questionnaire to show that they were participating in the study of their own will. Therefore, the study has only included those participants which have to send signed forms prior.
Moreover, the study was conducted following the principles of the Declaration of Helsinki. All participants were informed about the aim of the study, and data were collected through an online survey form between June 2020 and August 2020. It was also ensured that all the participants spend at least an hour in the last four weeks either watching media or thinking about COVID-19. This was ensured by asking participants about time spent consuming media and thinking about COVID-1. The study mainly focuses on social phobia, anxiety, stress, and depression about COVID-19 and its outbreak. The study did not include participants already suffering from psychological comorbidities and this was assured by having a dedicated section related to health history in the questionnaire with the help of which all the responses from the participants excluded those who had a history of psychological comorbidities.
Participants' baseline characteristics are demonstrated in Table 1. The respondents primarily included females (61.3%) and males (38.7%) with a mean age of 31.2, SD ± (13.3) range (17–65) years. The participation primarily included mostly married (49%), educational level of the sample was university level (75%). Regarding occupation, most of the participants were students (37%). The results on the CPS showed 18.4% of participants with mild social phobia and stress during the pandemic, 57.9% of the respondents presented moderate anxiety, stress, depression, and social phobia; and 23.6% presented severe anxiety, stress, depression, and social phobia in terms of emotional and symptomatic factors.
Table 1.
Baseline characteristics.
| Total (N = 618) | N (%) | |
|---|---|---|
| Age | ||
| (Mean, SD) | 31.2±(13.3) | Range (17–65) |
| Gender | ||
| Male | 1 | 239 (38.7) |
| Female | 2 | 379 (61.3) |
| Marital Status | ||
| Married | 1 | 303 (49) |
| Unmarried | 2 | 289 (47) |
| Divorced | 3 | 19 (3) |
| Widow | 4 | 7 (1) |
| Educational Level | ||
| Master or PhD | 1 | 98 (16) |
| University level | 2 | 463 (75) |
| Secondary | 3 | 47 (8) |
| less than Secondary | 4 | 9 (1) |
| Occupation | ||
| Government employee | 1 | 194 (31) |
| Private employee | 2 | 71 (12) |
| Student | 3 | 227 (37) |
| Self Employed | 4 | 25 (4) |
| Unemployed | 5 | 101 (16) |
| Retired | 6 | 0 (0) |
2.2. Analytical approach
A sequence of factor analytic approaches was used to assess various psychological symptoms to find a limited and reliable sample of anxiety symptoms that best represent the latent concept of coronavirus anxiety (Thompson, 2004). An internal replicability approach was used to address the effects of sampling error, using bias-corrected bootstrap Maximum Likelihood estimations (2,000 samples) with one-half of the study's data being subjected to a series of confirmatory factor analysis (CFA) and the other half being subjected to a principal component analysis (PCA). The five most significant and typical symptoms of coronavirus anxiety were determined using the PCA, and the replicability of the PCA results was tested using the CFA.
A series of different group CFAs were also conducted to see if the construct coronavirus phobia is measured the same way across demographic groups. Using a series of correlations and receiver operating characteristic (ROC) analyses, the full data set was then utilized to investigate the construct validity and diagnostic viability of the coronavirus phobia symptoms. SPSS version 26.0 was used to carry out statistical analysis. On the other hand, AMOS version 25.0 was used to run CFA.
The standard for shaping the five symptoms of the CAS was grounded on the properties of a psychometrically sound items (Ford et al., 1986). Particularly, the symptoms have to be taken out of the PCA's first component as they have the highest potential squared correlations with the rest of the item pool. To be taken into consideration for the CAS, the five symptoms with the highest loadings on the first component had to also provide high pattern/structure coefficients (>0.40), high commonality coefficients (>0.40), and low cross-loadings (<0.40) with the second component.
The qualities of a psychometrically sound item were used to determine the five symptoms for the CAS (Caycho-Rodríguez et al., 2018) because they account for the largest potential squared correlations among the item pool, the symptoms had to be retrieved from the first component of the PCA. Conventional criteria were used to determine CFA model fit and measurement invariance (Ro et al., 2017). A chi-square/df value of 2 was defined as an appropriate model fit for a CFA model, as was a standardized root-mean-square residual (SRMR) value of 0.05, root-mean-square-error of approximation (RMSEA) value of 0.10, and comparative fit index (CFI) and Tucker Lewis index (TLI) value of >0.90. Both sufficient models fit statistics, and a non-significant value (p > 0.05) on a chi-square difference test was used to determine measurement invariance.
Based on psychiatric screening test research, criteria for assessing the diagnostic validity of the Coronaphobia scale as a mental health screener and an optimum cutoff value for scoring the CAS were developed (Milman et al., 2020; Midorikawa, 2021). A good screening test should have an area under the curve (AUC) value of at least 0.70 and be graphically represented by a ROC curve with a convex form in the top left corner of the graph. To be deemed practical for mental health screening, the ideal cutoff score must have a sensitivity value of >80% and a specificity value of >70%.
3. Results
3.1. Reliability
This study developed a questionnaire to assess emotional and symptomatic factors influencing the UAE population during COVID-19. The questionnaire was evaluated for its reliability through Cronbach’s Alpha Coefficients. The Cronbach value achieved for the four factors, social phobia, anxiety, stress, and depression (including 35 items), were found to be 0.743, 0.783, 0.805, and 0.753, respectively, indicating increased reliability and internal consistency (Table 2).
Table 2.
Questionnaire reliability.
| Cronbach’s Alpha | Factors (No. of items) |
|---|---|
| 0.743 | Social phobia (8) |
| 0.783 | Anxiety (10) |
| 0.805 | Stress (10) |
| 0.753 | Depression (7) |
3.2. Screening of data
The preliminary data screening suggested that 35 items of the coronaphobia scale were appropriate for conducting confirmatory factor analysis (Bernardo et al., 2020). There were no issues relating to missing data, singularity, sample size, multi-collinearity, and non-normality. Further, the correlation matrices were estimated to be factorable (KaiserMeyer–Olkin test = 0.98; Bartlett’s test of sphericity = p < 0.001). Chi-square set and t-tests revealed that the PCA sample (n = 311) was not socio-demographically different from the CFA sample (n = 307).
3.3. Principal component analysis
Thirty-five COVID-19 symptoms corresponding to social phobia, anxiety, stress, and depression were subjected to a principal component analysis with Varimax rotation. A two-component structure was identified through the results, accounting for 78.52% of the total variance explained. For the Coronaphobia scale, the five strongest loadings were chosen as they seem to be well exceeded the criteria for the items that are psychometrically sound (Table 3). Precisely, the structure coefficients ranged from 0.851 to 0.907, and commonality coefficients ranged from 0.725 to 0.823. The distinct and physiological reactions of social phobia, anxiety, stress, and depression related to COVID-19 are assessed by these items and are highly reliable as a cluster (α = 0.93).
Table 3.
Coronaphobia scale properties from principal component analysis.
| Items | LD | h2 | M | SD | Item correlation |
|---|---|---|---|---|---|
| Social phobia | 0.851 | 0.725 | 2.568 | 0.620 | 0.068∗∗∗ |
| Anxiety | 0.894 | 0.800 | 2.539 | 0.621 | 0.078∗∗ |
| Stress | 0.907 | 0.823 | 2.444 | 0.631 | 0.036 |
| Depression | 0.891 | 0.793 | 2.420 | 0.682 | 0.037 |
LD = structure coefficients; h2 = extracted communality coefficients; M = mean; SD = standard deviation; ∗ = significant correlation coefficient values at 0.01.
3.4. Confirmatory factor analysis
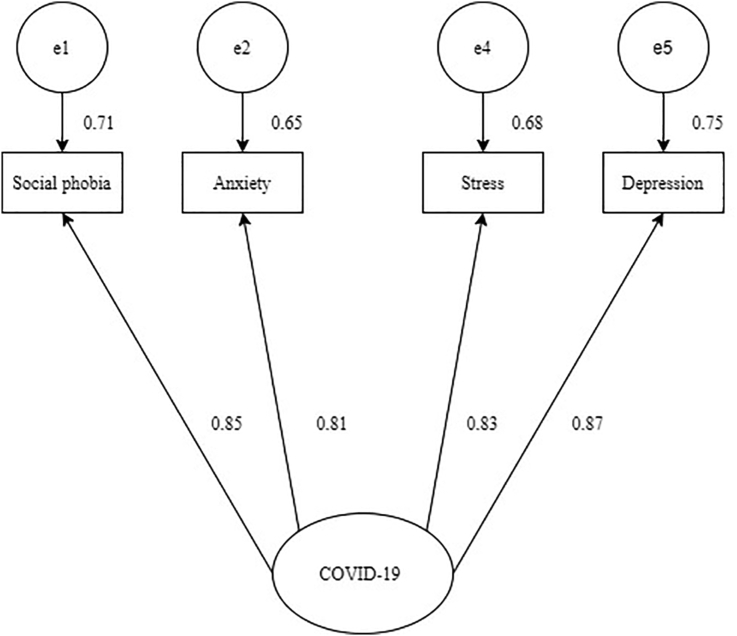
A CFA test was run to identify the symptoms in principal component analysis cohered to the COVID-19 phobia construct. Figure 1 supports the findings of principal component analysis as it shows a single-factor model [X2 (5) = 2.78, p = 0.75] yielding an excellent fit for all indices [X2/df ratio = 0.54; CFI = 1.00 TLI = 1.00; SRMR = 0.01; RMSEA = 0.00 (0.00, 0.05; 90% CI)]. The analysis of parameter estimations showed that stress and depression were stronger indicators of COVID-19 anxiety in people. The measurement of COVID-19 phobia seems to be valid for people, although the strength of the indicators might vary among different genders.
Figure 1.
CFA model.
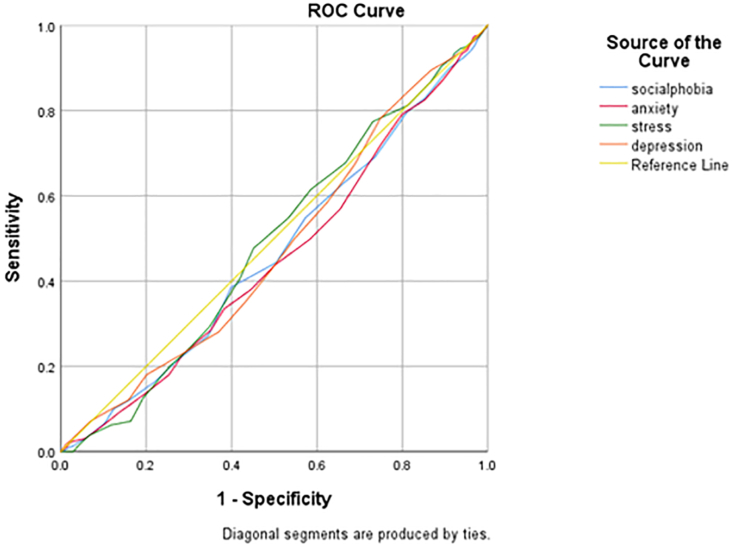
3.5. Receiver operating characteristic analysis
The diagnostic viability of the Coronaphobia scale as a mental health screening tool was evaluated through receiver operating characteristic (ROC) analyses. This helped determine a cut score for differentiating individuals experiencing clinically significant impairment because of COVID-19 (individuals with scores of >20) compared to the individuals who were not disabled by COVID-19 but were anxious. Figure 2 shows the ROC displaying the convex pattern indicating a good discrimination ability. While, the area under the curve (AUC) demonstrated solid diagnostic accuracy for the Coronaphobia scale (AUC (social phobia) = 0.465, AUC (anxiety) = 0.453, AUC (stress) = 0.488, AUC (depression) = 0.475, p < .001). These results support the fact that the Coronaphobia scale is a diagnostically accurate mental health screening tool having strong classification features.
Figure 2.
Area under the ROC curve.
The mean change in the response variable for one unit of change in the predictor variable while maintaining other predictors in the model constant is represented by regression coefficients. This statistical control provided by regression is significant because it separates the importance of one variable from the rest of the model’s variables. Table 4 shows no significant value as the p-values are >0.05. The p-value for social phobia (0.480), anxiety (0.170), stress (0.555), and depression (0.759) are greater than the common alpha level of 0.05, indicating no statistical significance.
Table 4.
Regression an.
| Model | Unstandardized Coefficients |
Standardized Coefficients |
t | P-value | |
|---|---|---|---|---|---|
| B | Std. Error | Beta | |||
| (Constant) | 1.767 | .090 | 19.533 | .000 | |
| Social phobia | -.034 | .048 | -.043 | -.706 | .480 |
| Anxiety | -.074 | .054 | -.094 | -1.375 | .170 |
| Stress | .034 | .058 | .044 | .591 | .555 |
| Depression | .016 | .051 | .022 | .307 | .759 |
4. Discussion
The main focus of this study was on the development and evaluation of properties of a brief mental health screener to be used by professionals readily for identifying probable cases of social phobia, anxiety, stress, and depression associated with COVID-19. The Coronaphobia scale is considered a measuring instrument of COVID-19-related psychopathology validated on individuals complaining about anxiety experienced during the pandemic. The psychometrically sound items for the Coronaphobia scale were identified through principal and component analysis. The results revealed high reliability, thematic consistency, and stability of the Coronaphobia scale. The major findings showed that the scale items assess different factor structures with appropriate psychometric indications, including factorial loads. Furthermore, the measured dependability coefficients imply that it has a high level of internal consistency.
The current study’s findings add to the validity and reliability of previous scales by proving the robust psychometric features within the communities in UAE. In some circumstances, there might be some benefit for the individual by minimizing risky behaviors and promoting virus-mitigating responses (Bernardo et al., 2020; Thompson, 2004; Ford et al., 1986). Fear symptomology has been linked to developing common mental diseases like depression, anxiety, and drug abuse disorders (Brown, 2015). Another Coronavirus Anxiety Scale comprised five somatic-based symptoms of fear and anxiety that are triggered by thoughts or information about the coronavirus (Lee et al., 2020).
In comparison to the Coronaphobia scale, Generalized Anxiety Disorder 7 (GAD-7) is considered a popular measurement tool for diagnosing anxiety disorder symptoms. However, the scale is slightly low compared to the Coronaphobia scale (Ro et al., 2017). The State-Trait Inventory provides another measure of anxiety for Cognitive and Somatic Anxiety (STICSA), which also falls below the constructs present in the Coronaphobia scale (Ford et al., 1986). The sensitivity and specificity (77% and 71%, respectively) of the General Health Questionnaire (GHQ) were measured in primary care research for assessing anxiety, social impairment, and depression (Spitzer et al., 2006). Another Coronavirus Anxiety Scale version adapted by Brazil found that total scores were higher among women and participants with a history of an anxiety disorder (Padovan-Neto et al., 2021).
Internal consistency, convergent, and discriminant validity were all high on the overall scale and subscales. Compared to the recently created FCV-19S, the results suggest that the Coronaphobia scale was more significantly linked with existing measures of anxiety and depression (Maunder et al., 2003). The Coronaphobia scale was also more strongly connected with anxiety measures than depression measures. It was reliable in predicting those diagnosed with severe anxiety; therefore, it is considered a potential instrument for assessing the intensity and frequency of COVID-related anxiety.
The scale items were created by referencing existing anxiety measures initially, then evaluating recognized anxiety symptoms reported by clinically referred cases in the UAE. However, a closer look at the 35 items revealed that they might be used by various people with proper translation and adaptation. However, some of the items are particular to the COVID-19 epidemic; therefore, it is unclear if they would be useful in other coronavirus pandemics with different modes of transmission and preventative practices.
The fears about the pandemic will certainly linger because there is no clear estimate of when the pandemic will end. Indeed, such fears may persist even when the pandemic has passed, as with earlier viral pandemics (Van et al., 2013). The availability of a reliable and accurate multidimensional measure of coronavirus-pandemic-related anxiety will be extremely useful in identifying individuals experiencing severe unfavorable emotional responses both during and after the pandemic. The Coronaphobia scale provides data that might guide therapeutic approaches and observe if mental health therapies effectively reduce anxiety symptoms over time.
Given the size of this expanding health catastrophe, the clinical and research advantages of quickly screening patients for dysfunctional anxiety due to the virus are enormous (Cheng et al., 2004). For instance, health care professionals must be physically and psychologically fit to perform efficiently on the front lines during the pandemic. However, as the number of illnesses and fatalities rises and medical resources grow scarcer, many healthcare professionals are feeling the pressure of this pandemic. According to recent studies, a significant number of them suffer from sadness, anxiety, and sleeplessness, which are said to be caused by a variety of causes, including fear of contracting the virus and transmitting it to their friends and family (Tabachnick et al., 2007).
On the contrary, higher levels of concern about transmission are linked to decreased happiness and a negative attitude toward health in general. This suggests that anxiety is linked to reporting health since it influences the assessment of experienced symptoms (Asselmann et al., 2014; Alsan et al., 2020). Similarly, the links between concerns of perceived health and well-being are consistent with the symptom perception theory. Individuals with lower levels of happiness and positive emotions are more likely to pay attention to body sensations and perceive them as sickness symptoms, prompting them to share their concerns openly (Lu et al., 2020; Howren and Suls, 2011).
This study has several significant implications. Empirically, research done throughout the COVID-19 pandemic might benefit from integrating a COVID-19-associated fear evaluation as a potential explanatory factor connected to possible vulnerability or resistance. Furthermore, determining the levels of this specific fear in various populations might help decision-makers, health practitioners, and physicians identify more fearful individuals during the current epidemic and devise educational initiatives targeted at the right people.
Apart from the significant implications, the study has a few limitations. The study used online modalities, which may make the measure unavailable to some people, and answering questions online may increase anxiety or produce other negative emotional reactions in some people. However, given the need for quarantine and physical separation during some pandemic stages, online polls may be the only choice. Moreover, the study did not include a structured diagnostic evaluation to investigate its construct validity which would have offered more relevant information on the Coronaphobia scale’s diagnostic value. Despite its size, the sample was not typical of the adult population. Therefore, future research needs to consider a broader range of adult samples from various nations would aid in establishing the validity and usability of the Coronaphobia scale.
5. Conclusion
The findings suggest that a Coronaphobia scale is a helpful tool for learning more about how people react and adjust to information about the danger of COVID-19 transmission. Knowing the degree of anxiety about transmission based on this scale would help in designing and assessing the efficacy of psychological interventions aimed at reducing the amount of fear associated with the presence of COVID-19. It is also beneficial for identifying the most vulnerable people who could acquire anxiety due to their fear of transmission. To summarize, the findings show that the Coronaphobia scale is a viable and reliable unidimensional tool for measuring COVID-19 transmission anxiety and its emotional impact on individuals. However, seeing the relationship between COVID-19-related anxiety, fear, stress, depression, and social phobia, it is a threat to the well-being of individuals. Therefore, the policymakers should implement programs related to psycho-education on coping skills and adverse thoughts regarding the Coronavirus by mental health professionals more explicit and accurate. The policymakers also should make sure that information that is provided to the population must be explicit and accurate to avoid pain situations. In addition, it also provides the base for future researchers to check the scale designed by the current study and see if it can measure/detect clinical anxiety which further recommends psychological intervention. Future studies need to focus on measuring the degree and duration of anxiety to assess the evidence for convergent validity.
Declarations
Author contribution statement
Rasha Abdelrahman, phD: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, design tools and data analysis; Wrote the paper, Wrote the discusion. Fouad Mohamed Aldawash: Analyzed and interpreted the data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data included in article/supp. material/referenced in article.
Declaration of interest's statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Ahorsu D.K., Lin C.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addiction. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsan M., Stantcheva S., Yang D., Cutler D. Disparities in coronavirus 2019 reported incidence, knowledge, and behaviour among US adults. JAMA Netw. Open. 2020;3(6):e2012403. doi: 10.1001/jamanetworkopen.2020.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson G.J., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: what all decision-makers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020;71 doi: 10.1016/j.janxdis.2020.102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asselmann E., Wittchen H.U., Lieb R., Höfler M., Beesdo-Baum K. Associations of fearful spells and panic attacks with incident anxiety, depressive, and substance use disorders: a 10-year prospective-longitudinal community study of adolescents and young adults. J. Psychiatr. Res. 2014;55:8–14. doi: 10.1016/j.jpsychires.2014.04.001. [DOI] [PubMed] [Google Scholar]
- Barbeito S., Becerra-García J.A., Sánchez-Gutiérrez T., Calvo A. COVID-19 Pandemic and Mental Health in Spain: an Analysis of Their Relationship Using Google Trends. Revista de psiquiatría y salud mental. 2021 doi: 10.1016/j.rpsm.2021.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becerra-García J.A., Giménez Ballesta G., Sánchez-Gutiérrez T., Barbeito Resa S., Calvo Calvo A. Psychopathological symptoms during Covid-19 quarantine in Spanish general population: a preliminary analysis based on sociodemographic and occupational-contextual factors. Rev. Esp. Salud Publica. 2020 [PMC free article] [PubMed] [Google Scholar]
- Bernardo A.B., Mendoza N.B., Simon P.D., Cunanan A.L.P., Dizon J.I.W.T., Tarroja M.C.H., Saplala J.E.G. Coronavirus pandemic anxiety scale (CPAS-11): development and initial validation. Curr. Psychol. 2020:1–9. doi: 10.1007/s12144-020-01193-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biviá-Roig G., La Rosa V.L., Gómez-Tébar M., Serrano-Raya L., Amer-Cuenca J.J., Caruso S., Lisón J.F. Analysis of the impact of the confinement resulting from COVID-19 on the lifestyle and psychological wellbeing of Spanish pregnant women: an internet-based cross-sectional survey. Int. J. Environ. Res. Publ. Health. 2020;17(16):5933. doi: 10.3390/ijerph17165933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T.A. Guilford publications; 2015. Confirmatory Factor Analysis for Applied Research. [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatr. Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caycho-Rodríguez T., Ventura-León J., Noe-Grijalva M., BarbozaPalomino M., Arias Gallegos W.L., Reyes-Bossio M., Rojas-Jara C. 2018. Initial psychometric evidence of a brief measure of cancer worry [Evidencias psicométricas iniciales de una medida breve sobre preocupación por el cáncer] [Google Scholar]
- Cheng S.K., Wong C.W., Tsang J., Wong K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol. Med. 2004;34(7):1187–1195. doi: 10.1017/s0033291704002272. [DOI] [PubMed] [Google Scholar]
- Commodari E., La Rosa V.L. Adolescents in quarantine during COVID-19 pandemic in Italy: perceived health risk, beliefs, psychological experiences and expectations for the future. Front. Psychol. 2020:2480. doi: 10.3389/fpsyg.2020.559951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commodari E., La Rosa V.L., Coniglio M.A. Health risk perceptions in the era of the new coronavirus: are the Italian people ready for a novel virus? A cross-sectional study on perceived personal and comparative susceptibility for infectious diseases. Public health. 2020;187:8–14. doi: 10.1016/j.puhe.2020.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Y., Xu J., Huang S., Li P., Lu C., Xie S. Risk perception and depression in public health crises: evidence from the COVID-19 crisis in China. Int. J. Environ. Res. Publ. Health. 2020;17(16):5728. doi: 10.3390/ijerph17165728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford J.K., MacCallum R.C., Tait M. The application of exploratory factor analysis in applied psychology: a critical review and analysis. Person. Psychol. 1986;39(2):291–314. [Google Scholar]
- Ghebreyesus T.A. World health organization. WHO Director-General’s opening remarks at the media briefing on COVID-19-25. 2020 https://www.who.int/dg/speeches/detail/who-director-general-s-openingremarks-at-the-media-briefing-on-covid-19%2D%2D-11-march2020 Retrieved from: [Google Scholar]
- Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int. J. Environ. Res. Publ. Health. 2020;17(13):4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addiction. 2021;19(5):1875–1888. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howren M.B., Suls J. The symptom perception hypothesis revised: depression and anxiety play different roles in concurrent and retrospective physical symptom reporting. J. Pers. Soc. Psychol. 2011;100(1):182. doi: 10.1037/a0021715. [DOI] [PubMed] [Google Scholar]
- Lee S.A. Measuring coronaphobia: the psychological basis of the coronavirus anxiety scale. Dusunen Adam. 2020;33(2):107–108. [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatr. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatr. Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ (Can. Med. Assoc. J.) 2003;168(10):1245–1251. [PMC free article] [PubMed] [Google Scholar]
- Midorikawa H., Aiba M., Lebowitz A., Taguchi T., Shiratori Y., Ogawa T., Tachikawa H. Confirming validity of the Fear of COVID-19 Scale in Japanese with a nationwide large-scale sample. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0246840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milman E., Lee S.A., Neimeyer R.A. Social isolation and the mitigation of coronavirus anxiety: the mediating role of meaning. Death Stud. 2020:1–13. doi: 10.1080/07481187.2020.1775362. [DOI] [PubMed] [Google Scholar]
- Padovan-Neto F.E., Lee S.A., Guimarães R.P., Godoy L.D., Costa H.B., Zerbini F.L.S., Fukusima S.S. OMEGA-J. Death Dying; 2021. Brazilian Adaptation of the Coronavirus Anxiety Scale: A Psychometric Investigation of a Measure of Coronaphobia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General psychiatr. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 y salud mental: una revisión de la literatura existente. Asian J. Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raphael B. Overview of the development of psychological support in emergencies. Adv. Disaster Ment. Health Psychol. Support. 2006;6 [Google Scholar]
- Ro J.S., Lee J.S., Kang S.C., Jung H.M. Worry experienced during the 2015 Middle East respiratory syndrome (MERS) pandemic in Korea. PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0173234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian j. psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakib N., Bhuiyan A.K.M., Hossain S., Al Mamun F., Hosen I., Abdullah A.H., et al. Psychometric validation of the bangla fear of COVID-19 scale: confirmatory factor analysis and rasch analysis. Int. J. Ment. Health Addiction. 2020:1–12. doi: 10.1007/s11469-020-00289-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva W.A.D., de Sampaio Brito T.R., Pereira C.R. COVID-19 anxiety scale (CAS): development and psychometric properties. Curr. Psychol. 2020:1–10. doi: 10.1007/s12144-020-01195-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tabachnick B.G., Fidell L.S., Ullman J.B. Vol. 5. pearson; Boston, MA: 2007. pp. 481–498. (Using Multivariate Statistics). [Google Scholar]
- Tanner K. second ed. Chandos Publishing; 2018. Survey Designs. Research Methods; pp. 159–192. [Google Scholar]
- Taylor S. Cambridge scholars publishing; 2019. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. [Google Scholar]
- Taylor S. Cambridge Scholars Publishing; 2019. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. [Google Scholar]
- Thompson B. 2004. Exploratory and Confirmatory Factor Analysis: Understanding Concepts and Applications. Washington, DC; p. 10694. [Google Scholar]
- Torales J., O’Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatr. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Van Dam N.T., Gros D.F., Earleywine M., Antony M.M. Establishing a trait anxiety threshold that signals likelihood of anxiety disorders. Hist. Philos. Logic. 2013;26(1):70–86. doi: 10.1080/10615806.2011.631525. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognit. Ther. Res. 2012;36(3):210–218. [Google Scholar]
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatr. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A., Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian j. psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/supp. material/referenced in article.