Abstract
Introduction
Coronavirus disease 2019 (COVID-19) has caused many concerns in the dental field regarding aerosol production and the transmission of the severe acute respiratory syndrome coronavirus 2 virus during dental procedures. Because of the abrupt arrival of COVID-19, there has been little to no published research on the efficacy of dental suction devices in the removal of aerosols related to COVID-19 or the impact extraoral suction devices have on patients’ experiences. Therefore, the aim of this study was to measure the amount of aerosol produced during endodontic access preparation for root canal therapy with and without the use of an extraoral dental suction device and to gather information through a survey regarding patients’ experiences.
Methods
Aerosol measurements were recorded in 8 closed-door resident operatories each morning before the procedures, 1 minute during the procedure, and 15 minutes after the access was complete. The CICADA DTO KN99 Extraoral Dental Suction Device (Foshan Cicada, Guangdong, China) was placed in 4 operatories, whereas no DTO extraoral suction device was used in 4 control operatories. Twenty cases with DTO and 20 cases without it were completed, and the data were analyzed.
Results
Aerosols 1 minute after access were higher with and without DTO. There was a significant reduction after 15 minutes when the DTO device was used compared to high-volume suction alone. Composite and zirconia produced the most aerosols at 1 minute.
Conclusion
The results show that the reduction of aerosols is enhanced when the extraoral suction device is used in combination with traditional high-volume evacuation. However, the increased noise level when using the device can have a negative impact on patients’ dental experience.
Key Words: Aerosols, endodontic access preparation, endodontics, extraoral evacuation device, high-volume suction
Significance.
The utility of an extraoral evacuation device in endodontics was the focus of this study. The study investigated the variation in time, aerosol particle size and number, the surface cut during access preparations, and the patients’ reactions.
The practice of dentistry has many biological risks that pose a daily challenge for the dental team. Dentists and dental assistants work in close proximity to their patients, which puts them at higher risk for microbial infections via aerosols. Major concerns have been raised regarding the working environment, and efforts continue to be made to minimize the dissemination of the microbial pathogens in generated aerosols1.
The severe acute respiratory syndrome coronavirus 2 virus, which is responsible for coronavirus disease 2019 (COVID-19), and many other infectious agents can be transmitted in the dental operatory via aerosols through inhalation, fomites, and/or nonintact skin and mucous membranes. In addition, particulate dust and aerosols from composites and other restorative materials, such as amalgam, zirconia, porcelain, and different metals, may be detrimental to health if inhaled. These microscopic particles may become aerosolized and could penetrate deep into the lungs, surpassing the natural defense mechanism of mucus and cilia. Existing studies have revealed that chronic inhalation of respirable dust and microscopic particles may cause local and systemic toxicity when absorbed or even provoke more serious conditions such as pneumoconiosis2. With the increase in cases of COVID-19 throughout the world, there is a concern of transmission via respiratory droplets and aerosols during dental procedures. Droplets are classically described as larger entities (>5 μm) that rapidly drop to the ground by force of gravity, typically within 3 to 6 ft of the source. Aerosols are smaller particles (<5 μm) that rapidly evaporate in the air, leaving behind droplet nuclei that are small enough and light enough to remain suspended in the air for hours3. Realistic management of all dental procedures that generate aerosols in everyday practice in the era of a pandemic is more pertinent than ever2.
To address the transmission of COVID-19 and microscopic particles via aerosols, the protocol for dental personnel has changed to reduce exposure to the virus by using preprocedural mouth rinses4 and using additional technologies to enhance evacuation protocols5.
Increased use of N95/KN95 respirators has been recommended by the Centers for Disease Control and Prevention and other state and national regulatory bodies to help reduce transmission. Protective eyewear with side shields (including goggles and face masks), high-volume evacuators, appropriate positioning of the patients, and dental dams were recognized as the foremost engineering protection strategies1. However, if severe acute respiratory syndrome coronavirus 2 is carried by aerosols that can remain suspended in the air for prolonged periods, these measures would provide only partial or temporary protection, and 6 ft of separation would not provide protection from aerosols that remain suspended in the air or are carried by currents3. Studies have demonstrated that these aerosols can travel up to 27 ft3 , 6, 7, 8.
Several studies have illustrated the contamination of surfaces in endodontic offices via aerosol8 , 9. These and other studies have demonstrated that every surface in the dental operatory was contaminated after the use of an air turbine6 , 10. It has also been shown that dental operatories are at a much higher level of contamination than public spaces. A systematic review by Laheij et al11 concluded that bioaerosols are generated from multiple sources in the dental office, which include dental instruments and human activity. Reducing the transmission of the infections caused by aerosol production is a very important area of concern in these times. One classic study indicated that, together with a preprocedural mouth rinse and the rubber dam, a high-volume evacuator should be used during dental treatment12.
Dental dam usage during endodontic procedures is considered the standard of care. However, there is controversy over their effectiveness in clinical practice. In 2 older studies, there was a significant reduction in bacterial airborne contamination when dental dams were used13 , 14. Conversely, another study found that the use of a dental dam was associated with significantly higher bacterial aerosol levels despite its purported clinical benefits6. One recent study showed the efficacy of extraoral evacuation, especially when combined with preprocedural mouth rinse, close to the patient and the provider during periodontal scaling15. However, the degree to which aerosol dissemination from different surfaces and at different times during endodontic access preparation and the need for additional technologies, such as extraoral evacuation, have not been fully explored.
Several studies have been performed using patient survey responses to certain aspects of dental treatment, including quality of life studies before and after treatment, patient preferences regarding treatment plans, and patient experiences during treatment4 , 12. There is a multitude of factors involved with studying patient responses to dental treatment, and different models have been adapted to best record patient experiences. A study by Azarpazhooh et al16 first published an attempt to apply the Gelberg-Andersen behavioral model to investigate patients’ preferences during the treatment of teeth with apical periodontitis. In this model, the authors highlighted the importance of evaluating demographics, financial situation, education level, and especially dental health behavior patterns when developing patient surveys related to specific experiences.
One survey used to assess quality of life in relation to oral disease is the Oral Health Impact Profile, which was developed by Slade and Spencer17. It is based on a model of disease and associated consequences derived from the International Classification of Impairments, Disabilities, and Handicaps. It measures self-reported dysfunction, discomfort, and disability18. The recognition of the importance of patient satisfaction has led to the development of specific dental treatment–related patient satisfaction measures, which apply scaling methods such as visual analog scales, adjectival scales, or semantic differential scales19 , 20. A visual analog scale is a way to measure subjective characteristics or attitudes that cannot be directly measured. An adjectival scale is a method in which the individual is measured against a set benchmark. A semantic differential scale measures a person’s subjective perception of and affective reactions to the properties of concepts, objects, and events by making use of a set of bipolar scales. Some studies have chosen to use a mail-out survey design, with varying levels of participation16. However, enhanced aerosol control measures, especially ones that generate noise during the operation, have not been sufficiently evaluated relative to their direct effect on patients’ experiences during the endodontic appointment, which is a part of their overall experience with the endodontic treatment.
Therefore, the purpose of this study was to measure the levels and particle sizes of aerosols produced during endodontic access preparations while using an extraoral dental evacuation device in the tooth structure as well as different restorative materials through which the access was created. A patient survey was obtained at the end of the procedure to evaluate patient experience with the use of this device. Our hypothesis was that there would be no change in recorded aerosol levels and particle sizes while using an extraoral evacuation unit compared with a control with traditional high-volume evacuation alone during endodontic access. We further hypothesized that patients would not rate their dental treatment experience negatively when the extraoral evacuation device was in operation during the endodontic procedure.
Materials and Methods
Extraoral Evacuation Device and Experimental Conditions
This study was approved by the Institutional Review Board at the University of Alabama at Birmingham (protocol #300006944). In this study, the CICADA DTO KN99 Extraoral Dental Evacuation Device (Foshan Cicada, Guangdong, China) was used. All procedures and measurements were performed and recorded in closed-door operatories. Before initiating root canal therapy, the patients were required to rinse with 50/50 hydrogen peroxide/water for 60 seconds due to institutional guidelines. Forty adult patients were randomly assigned to 1 of 2 equal groups: an experimental group that had the extraoral evacuation device activated and a control group without the device. The unit was placed in the same position for each procedure (ie, at the foot of each patient, 6 ft from the operator with the evacuation hood 8 inches from the patient’s mouth). The sample size was determined using G∗Power (version 3.1.9.6; Universität Kiel, Kiel, Germany) based on an effect size of 0.4, an alpha error of 0.05, and power or 1 − beta error of 0.8. The minimal total sample using these parameters was 34; therefore, we selected 40 patients, which increased the power to 0.85. Once anesthesia had been implemented, a dental dam was placed to isolate the tooth requiring treatment. A preoperative aseptic swab of 4% sodium hypochlorite was used to disinfect the field. A Kavo (Biberach an der Riss, Germany) high-speed handpiece with water spray coolant was used to access all teeth. Traditional high-volume evacuation was performed on all endodontic accesses. The extraoral dental evacuation device was activated on power setting #3, which is the setting recommended by the manufacturer, for the experimental group.
Measurement of Aerosol Production
The Temtop PMD 331 Air Quality Handheld Particle Counter 7 Channels (Temtop, San Jose, CA) was used to evaluate the particle size and the number of particles in the droplets and aerosols produced. The Temtop Particle Counter was placed 4 ft away from the patient’s oral cavity, and a sampling time of 60 seconds was used as recommended by the manufacturer. Three recordings were done for each case: a preoperative aerosol measurement of 60 seconds was recorded in the operatory each morning before beginning any procedure, another was recorded 1 minute after initiation of the access preparation, and a third postoperative recording 15 minutes after the access was completed.
Patient Survey
A survey was given to each patient at the end of the procedure to help in assessing patient experience and the feasibility of using the extraoral evacuation in the current dental practice environment. It was important to keep the survey brief and direct because patients were in variable emotional and physical conditions directly after their respective procedure(s). The aim of this survey was in evaluating the patient response to the noise and intrusion level of the extraoral evacuation unit in conjunction with endodontic treatment. No protected health information was collected on the patient.
The patients were administered a list of the following 5 questions and asked to answer with a scale of 1 to 10 using a semantic differential scale with labeled end points21:
-
1.
How satisfied were you with your dental treatment?
-
2.
How painful was your dental treatment?
-
3.
Would you consider your treatment time-consuming or fast?
-
4.
Would you consider your treatment unpleasant or pleasant?
-
5.
How would you rate the noise level of the dental treatment?
Statistical Analysis
Sample means and standard deviations were summarized by time, evacuation method, bur type, and tooth or restorative material cut. Because of the repeated measurements of airborne particles during a procedure (preoperative, at 1 minute, and at 15 minutes), we used repeated measures analysis of variance (ANOVA) treating time as a within-subject factor. We examined 3 between factors: the surface material being cut, the bur type used, and the evacuation method used during the procedure. Separate repeated measures ANOVA models were built for each of the between-subject factors. P values are reported for the significance of the between-subject factors, within-subject factors, and their interaction. A P value < .05 was considered significant. Normality assumption was examined using histograms and normal probability plots. The normality assumption was deemed reasonable. Finally, a repeated measures ANOVA model including all 3 between factors simultaneously was constructed to examine their adjusted P values. All tests were conducted using SAS 9.4 (SAS Institute, Cary, NC) or R 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria). Analyses of the patient survey data were performed by comparing the results of patients who had the extraoral evacuation device used during their procedure and those who did not using the unpaired t test.
Results
Total Levels of Aerosol Production
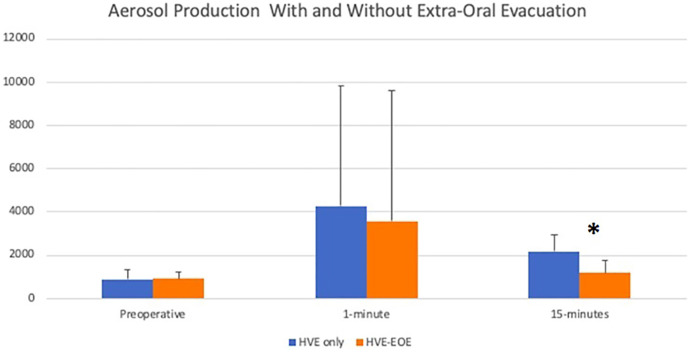
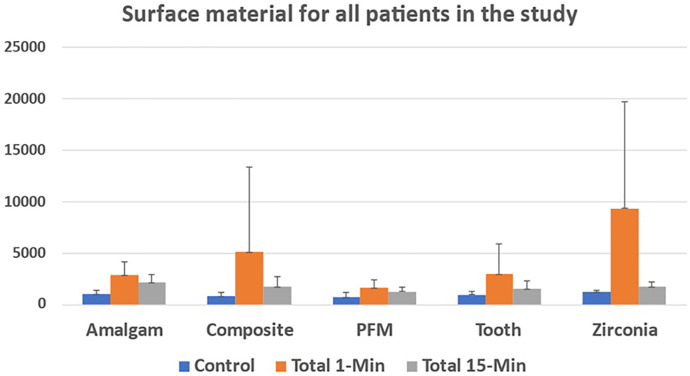
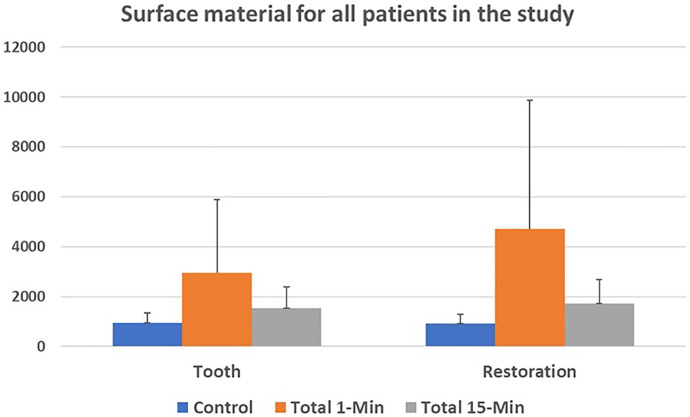
The levels of aerosol production increased at 1 minute into the access preparation compared with baseline levels and then decreased at 15 minutes, with the only difference by bivariate analysis at 15 minutes (P < .0001) (Fig. 1 ). A similar pattern in the levels of aerosols produced from each surface material was produced at the different time points (Fig. 2 ). Composite and zirconia produced the most aerosols at the 1-minute mark, but both also had a high standard deviation compared with the other materials.
Figure 1.
Aerosol production with and without extraoral evacuation.
Figure 2.
The surface material for all patients in the study.
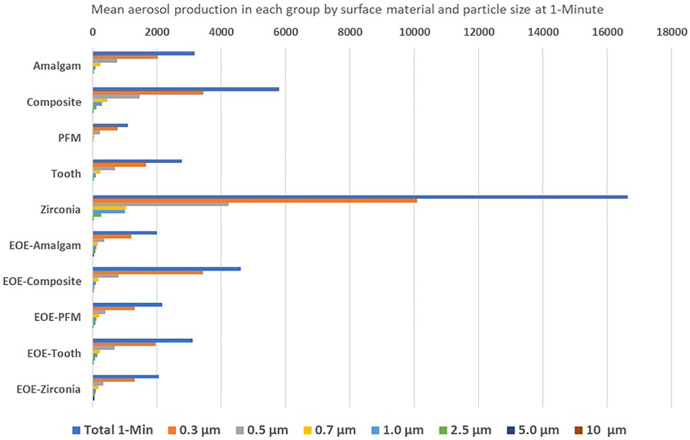
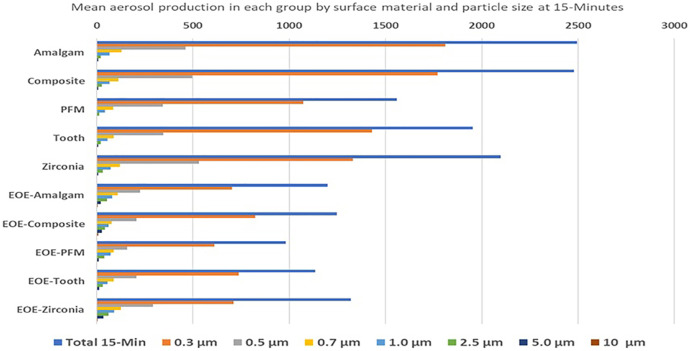
Data on the particle sizes produced in the aerosols are shown in Figures 3 and 4 . The data showed that the highest levels of particle sizes detected were the smallest, and progressively lower levels of the larger particle sizes were detected with all surface materials. A comparison of the levels of particles detected with tooth versus restorative materials is shown in Figure 5 .
Figure 3.
The mean aerosol production in each group by surface material and particle size at 1 minute.
Figure 4.
The mean aerosol production in each group by surface material and particle size at 15 minutes.
Figure 5.
The surface material for all patients in the study.
Table 1 shows the statistical models for the analyses that included the time of measurement, surface material, and bur type. These analyses indicated that, in addition to significant variation across the preoperative, 1-minute, and 15-minute times (P < .001), the between factor of evacuation type and the interaction of evaluation type and time were statistically significant (P = .0022 and .0023, respectively). However, a separate repeated measures ANOVA examining the effects of bur type and the interaction of bur type with time did not demonstrate statistical significance (P = .4539 and .2292, respectively), although the within-factor measuring variation due to time was significant (P < .001). A repeated measures ANOVA examining the effects of material type produced similar results, with material type and the interaction of material type with time not demonstrating statistical significance (P = .4496 and .8168, respectively), although the within-factor measuring variation due to time was significant (P < .001). One final repeated measures ANOVA was built including all 3 between factors (ie, evacuation method, bur type, and material type). This model again indicated variation due to time (P < .001), evacuation type (P = .0043), and the interaction between time and evacuation type and time (P = .0087). All other effects and interactions did not achieve statistical significance. The test of evacuation type and time was significant; follow-up tests were conducted at each time point, producing P values of 0.6590, 0.0405, and .0002 for preoperative, 1-minute, and 15-minute comparisons, respectively.
Table 1.
Analysis of the Data With All Variables: High-Volume Evacuation (HVE) and Extraoral Evacuation (EVE)
| Between factor |
Within factor |
Hypothesis tests |
|||
|---|---|---|---|---|---|
| Evacuation | Preoperative | 1 minute | 15 minutes | Effect | P value |
| HVE only (n = 18) | 837.4 ± 431.6 | 2676.3 ± 1476.1 | 2211.8 ± 793.9 | Evacuation | .0022 |
| HVE-EVE (n = 18) | 915.2 ± 339.7 | 1790.0 ± 520.3 | 1175.2 ± 552.9 | Time | <.0001 |
| Interaction | .0023 | ||||
| Bur type | Effect | P value | |||
|---|---|---|---|---|---|
| 330 (n = 13) | 1130.3 ± 355.6 | 2551.1 ± 1541.6 | 1610.9 ± 842.9 | Bur Type | .4539 |
| Diamond (n = 3) | 925.3 ± 470.8 | 1772.3 ± 589.8 | 1286.3 ± 289.4 | Time | <.0001 |
| Round carbide (n = 20) | 703.9 ± 306.2 | 2097.4 ± 950.0 | 1808.3 ± 918.8 | Interaction | .2992 |
| Surface Material |
Effect | P value | |||
|---|---|---|---|---|---|
| Amalgam (n = 8) | 994.6 ± 416.9 | 2841.4 ± 1327.8 | 2125.0 ± 840.6 | Material | .4496 |
| Composite (n = 13) | 749.2 ± 346.5 | 1991.7 ± 765.5 | 1736.2 ± 975.0 | Time | <.0001 |
| PFM (n = 2) | 727.0 ± 455.4 | 1692.0 ± 756.6 | 1270 ± 407.3 | Interaction | .1556 |
| Tooth (n = 13) | 928.4 ± 398.4 | 2256.2 ± 1428.8 | 1512.5 ± 791.4 | ||
| Zirconia (n = 1) | 1322.0 ± 0 | 2059 ± 0 | 1319 ± 0 | ||
PFM, Porcelain fused to metal.
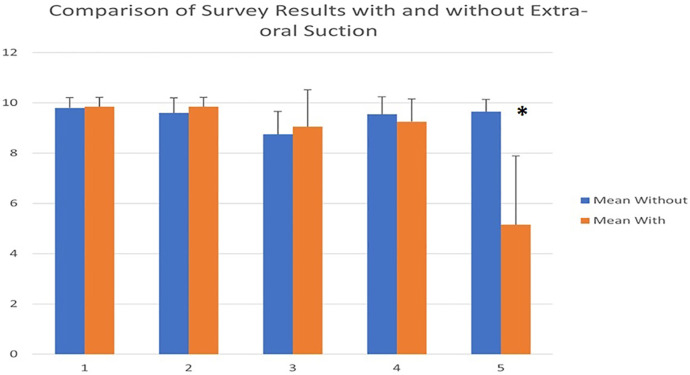
A t test was used to evaluate the results of the patient survey. The results indicated that there was statistical significance only for question 5, which was the question regarding the noise level (Fig. 6 , P < .0001). Very little variation was noted among the survey results for the other 4 questions (P > .05).
Figure 6.
A comparison of survey results with and without extraoral suction.
Discussion
Aerosol generation during routine endodontic access is a concern in that it may contribute to the cross-infection risk, especially in the era of COVID-19. In endodontics, the use of high-speed and low-speed handpieces with coolant, ultrasonics, and lasers produces spatters, droplets, and aerosols that can reach a considerable distance, carrying potentially infective agents7. Previous investigations highlighted the pathogenic load of bioaerosols in dentistry8 , 9 , 22. The findings of the present study showed that aerosols are measurable preoperatively, significantly increase at 1 minute into the access preparation, and decrease at 15 minutes after completion of the procedure. This study also showed that there was a significant difference in the presence of aerosols 15 minutes after access when an extraoral dental evacuation device was used. The authors are not aware of other studies that compared the aerosol levels at different times during endodontic access preparation with control for the surface material and the type of bur used.
The randomization of patients used in this study resulted in the inclusion of different surface materials and bur types in both groups; however, the study was only powered for the effect size of the main variable of interest. Future studies should evaluate whether restorative materials result in higher amounts of aerosols, which was not revealed to be statistically significant in this study. Some of the particles present in aerosols generated during endodontic procedures would be expected to be larger and heavier compared with others and therefore should not remain suspended in the air as long as the smaller particles. This study showed that endodontic access preparations through composite or zirconia had a much higher particle content in the aerosols at the 1-minute time frame compared with the tooth structure, with that number being dramatically reduced by the 15-minute measurement; however, these differences were not statistically significant. Variations in surface material aerosols may be due to larger particle sizes dropping out of the air much more quickly or from the high evacuation systems running for 15 minutes after access.
Another finding in this study was that there was a much higher concentration of 0.3-μm and 0.5-μm particles in the aerosols than any other sizes at both reading times. This is to be expected and supports other studies that show the smaller the particle size in the aerosols, the longer they will remain suspended in the air and the longer it takes for them to settle on a surface. The smaller size also allows them to drift much farther away from the patient and clinician before settling on surfaces8; therefore, they were much more likely to be detected at 4 ft away from the source of production. Studies have shown that they can be carried by currents up to 27 ft away5 , 17. Therefore, it is critical to try and eliminate as much of the aerosols as possible in the dental operatories during endodontic procedures.
When comparing the difference in the number of particles in the aerosols generated when accessing natural tooth structure versus accessing through restorations, the main difference was seen at the 1-minute measurement after access began. Accessing through a restoration produced a higher concentration of particles in the aerosols; however, this difference was not statistically different (data not shown). This supports the study by Iliadi et al2 and shows that the water can mix with the dust generated from cutting restorative materials and produce a much higher concentration in the aerosols. This can be detrimental for the dental personnel, who are at risk of inhaling this daily, and shows the value of removing the particles from the air and wearing adequate respirators and face shields.
In this study, the extraoral evacuation device had its evacuation hood 8 inches (∼20 cm) from the patient’s mouth. In this location, it reduced the amount of aerosol by 16% 1 minute into the procedure and by 46% 15 minutes after the procedure (Fig. 1). In a recent study, placement of an extraoral evacuation device 10 cm away from the mouth resulted in negligible bacterial contamination by aerosols compared with 20 cm away, where more dental aerosols containing bacteria were detected15 Taken together, these data provide the clinician with the relative efficacy to be expected of this technology.
Regarding the patient survey, the results of this study indicate that patients viewed the noise negatively. The extraoral dental evacuation device generates a high level of noise, registering about 45 dB even on setting 3. This noise level makes communicating with the patient more difficult but not impossible. Another incidental finding that may be important to some patients and clinicians was the generation of heat by the machine. This study was conducted in closed-door operatories, and by the 15-minute mark, a large amount of heat was generated by the extraoral dental evacuation device. This was associated anecdotally with a high level of discomfort for the providers performing the procedures. Further studies may need to include a survey question regarding the level of discomfort associated with the heat produced by the extraoral dental evacuation device. Taken together, the effects of the noise and the heat generation may dissuade many practitioners from using these devices, especially because it is not known whether the reduction of aerosol with these devices is clinically significant.
Conclusions
This study showed that aerosols may remain suspended in the air for extended periods of time. The surface material cut and the bur type were not statistically significant in the amount of aerosol generated. Currently, high-volume evacuation alone has been the primary way that most clinicians have attempted to remove the aerosols produced while practicing dentistry. The results of our study demonstrate the value of the high-volume evacuation plus the extraoral dental evacuation device and allow the clinician to determine whether the extra cost, noise, and possible heat generation with the use of the extraoral dental evacuation device is warranted. The reduction of aerosols is of paramount importance to the health and well-being of the clinician and staff in a dental practice because they are at constant risk of exposure to aerosols that may carry infectious diseases. This study adds more data to assess the risk and benefit of using 1 additional technology available to the practitioner.
CRediT authorship contribution statement
Barton Barrett: Conceptualization, Data acquisition, Data curation, Writing – original draft, Writing – review & editing. Jason McGovern: Conceptualization, Data acquisition, Data curation, Writing – original draft, Writing – review & editing. William Catanzaro: Conceptualization, Data acquisition, Data curation, Writing – original draft, Writing – review & editing. Shandra Coble: Data curation, Writing – review & editing. David Redden: Formal analysis, Writing – original draft, Writing – review & editing. Ashraf F. Fouad: Conceptualization, Methodology, Data acquisition, Data curation, Formal analysis, Writing – review & editing.
Acknowledgments
The authors thank Drs David Clanton and Nathan Nunnelee for their assistance with the conception and execution of the study.
All authors deny any conflict of interest related to this study.
References
- 1.Koletsi D., Belibasakis G.N., Eliades T. Interventions to Reduce Aerosolized Microbes in Dental Practice: A Systematic Review with Network Meta-analysis of Randomized Controlled Trials. J Dent Res. 2020;99:1228–1238. doi: 10.1177/0022034520943574. [DOI] [PubMed] [Google Scholar]
- 2.Iliadi A., Koletsi D., Eliades T., Eliades G. Particulate Production and Composite Dust during Routine Dental Procedures. A Systematic Review with Meta-Analyses. Materials (Basel) 2020;13 doi: 10.3390/ma13112513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klompas M., Baker M.A., Rhee C. Airborne Transmission of SARS-CoV-2: Theoretical Considerations and Available Evidence. JAMA. 2020;324:441–442. doi: 10.1001/jama.2020.12458. [DOI] [PubMed] [Google Scholar]
- 4.Kumbargere Nagraj S., Eachempati P., Paisi M., et al. Preprocedural mouth rinses for preventing transmission of infectious diseases through aerosols in dental healthcare providers. Cochrane Database Syst Rev. 2022;8:CD013826. doi: 10.1002/14651858.CD013826.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choudhary S., Durkin M.J., Stoeckel D.C., et al. Comparison of aerosol mitigation strategies and aerosol persistence in dental environments. Infect Control Hosp Epidemiol. 2022:1–6. doi: 10.1017/ice.2022.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Amad S.H., Awad M.A., Edher F.M., et al. The effect of rubber dam on atmospheric bacterial aerosols during restorative dentistry. J Infect Public Health. 2017;10:195–200. doi: 10.1016/j.jiph.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 7.Ionescu A.C., Cagetti M.G., Ferracane J.L., et al. Topographic aspects of airborne contamination caused by the use of dental handpieces in the operative environment. J Am Dent Assoc. 2020;151:660–667. doi: 10.1016/j.adaj.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bahador M., Alfirdous R.A., Alquria T.A., et al. Aerosols Generated during Endodontic Treatment: A Special Concern during the Coronavirus Disease 2019 Pandemic. J Endod. 2021;47:732–739. doi: 10.1016/j.joen.2021.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rayyan A., Ather A., Hargreaves K., Ruparel N.B. Effect of sodium hypochlorite in dental unit waterline on aerosolized bacteria-generated from endodontic procedures. J Endod. 2022;48:1248–1256. doi: 10.1016/j.joen.2022.07.006. [DOI] [PubMed] [Google Scholar]
- 10.Rautemaa R., Nordberg A., Wuolijoki-Saaristo K., Meurman J.H. Bacterial aerosols in dental practice - a potential hospital infection problem? J Hosp Infect. 2006;64:76–81. doi: 10.1016/j.jhin.2006.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laheij A., de Soet J.J., Crielaard W., et al. [Cross contamination: spatters, aerosols, and biofilm in dental practices] Ned Tijdschr Tandheelkd. 2021;128:221–227. doi: 10.5177/ntvt.2021.04.20100. [DOI] [PubMed] [Google Scholar]
- 12.Harrel S.K., Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135:429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cochran M.A., Miller C.H., Sheldrake M.A. The efficacy of the rubber dam as a barrier to the spread of microorganisms during dental treatment. J Am Dent Assoc. 1989;119:141–144. doi: 10.14219/jada.archive.1989.0131. [DOI] [PubMed] [Google Scholar]
- 14.Samaranayake L.P., Reid J., Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC J Dent Child. 1989;56:442–444. [PubMed] [Google Scholar]
- 15.Takenaka S., Sotozono M., Yashiro A., et al. Efficacy of combining an extraoral high-volume evacuator with preprocedural mouth rinsing in reducing aerosol contamination produced by ultrasonic scaling. Int J Environ Res Public Health. 2022;19:6048. doi: 10.3390/ijerph19106048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azarpazhooh A., Dao T., Figueiredo R., et al. A survey of patients' preferences for the treatment of teeth with apical periodontitis. J Endod. 2013;39:1534–1541. doi: 10.1016/j.joen.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 17.Slade G.D., Spencer A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 18.Slade G.D., Strauss R.P., Atchison K.A., et al. Conference summary: assessing oral health outcomes--measuring health status and quality of life. Community Dent Health. 1998;15:3–7. [PubMed] [Google Scholar]
- 19.Chapko M.K., Bergner M., Green K., et al. Development and validation of a measure of dental patient satisfaction. Med Care. 1985;23:39–49. doi: 10.1097/00005650-198501000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Corah N.L., O'Shea R.M., Pace L.F., Seyrek S.K. Development of a patient measure of satisfaction with the dentist: the Dental Visit Satisfaction Scale. J Behav Med. 1984;7:367–373. doi: 10.1007/BF00845270. [DOI] [PubMed] [Google Scholar]
- 21.Dugas N.N., Lawrence H.P., Teplitsky P., Friedman S. Quality of life and satisfaction outcomes of endodontic treatment. J Endo. 2002;28:819–827. doi: 10.1097/00004770-200212000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Zemouri C., de Soet H., Crielaard W., Laheij A. A scoping review on bio-aerosols in healthcare and the dental environment. Plods One. 2017;12:e0178007. doi: 10.1371/journal.pone.0178007. [DOI] [PMC free article] [PubMed] [Google Scholar]