Abstract
Purpose
Extended-spectrum beta-lactamase-producing (ESBL) Enterobacteriaceae, which includes Escherichia coli, has emerged as a global health threat. ESBL enzymes including CTX-M, TEM, and SHV are the most detected. Here, a systematic review was developed to assess the status of ESBLs in E. coli considering studies performed in the human, animal, food, and environmental realms in South America.
Methods
Following PRISMA guidelines, a systematic review was performed using the PubMed database as a primary source to identify studies containing data on ESBL-producing E. coli in South America. To obtain a comprehensive sample, studies in English, Spanish, and Portuguese were included from 1990 to April 2021. Inclusion such as the reporting of sample origin and diagnostic method and exclusion criteria such as review/letter articles were established to complete data extraction steps.
Results
Amongst 506 articles retrieved, 130 met the inclusion criteria. Brazil reported 65 (50%) of publications, followed by Argentina, and Ecuador with 11.5% each. According to the category of studies, human studies represented the 56%, animals the 20%, environmental the 11%, and food studies the 6%. Interestingly, studies assessing more than one category (ie, interdisciplinary) represented the 7%. Prevalence of ESBL producing E. coli in animal, food, and environmental studies was widely superior compared to human sources. In clinical studies, Brazil presented the greatest diversity in terms of ESBLs, featuring CTX-M, TEM, SHV, TOHO, OXA, and AmpC. CTX-M enzymes were the most frequent variants with 89.4% detections.
Conclusion
The present One Health review of 130 studies conducted over the past 21 years found ESBLs producing E. coli distributed across human, animal, food, and environmental samples across South America. There is a need to increment studies in underrepresented countries and to strengthen multi-sectoral antimicrobial resistance research and surveillance. This information can be used as basis for subsequent implementation of monitoring programs, targeting potential critical points of transmission sources.
Keywords: extended-spectrum beta-lactamase, Escherichia coli, South America, One Health
Introduction
The antimicrobial resistance phenomena existed long time before humans were implementing antibiotics.1 Bacteria have several mechanisms to evade the action of antimicrobials. One of the most important in humans, animals, and the environment is the enzyme-mediated breaking of the beta-lactam ring of penicillin and its derivatives. Penicillins are the widest group of antibiotics.2
Enzyme-mediated resistance is a worldwide public health problem recognized by the World Health Organization (WHO) due to its rapid expansion and the generation of multidrug-resistant (MDR) bacteria that are increasingly difficult to eliminate.3,4 The current increase and dispersion of penicillin, carbapenem, and cephalosporin resistance is driven by a group of enzymes known as beta-lactamases. These enzymes, commonly found in well-known human environments, have been discovered in apparently unsuitable localities such as soils or glaciers in Antarctica, which have probably never encountered beta-lactam antibiotics previously.5
Beta-lactamases enzymes were first described in 1940, England; isolated from an E. coli, which prompted antibiotic resistance research.6,7 In early 1980s, TEM-1, TEM-2 (isolated from a patient in Temoneira in Athens, Greece), and SHV-1 (sulfhydryl variable, active site) circulating beta-lactamases were found capable to hydrolyze the beta-lactamic ring of cephalosporins8 and therefore resistance was soon reported.9 Single-point mutations in these enzymes allowed beta-lactamases to break penicillin and its derivatives, as well as the first, the second, and third generation cephalosporins, and even monobactams.10–13
In 1988 and 1989, the first isolate of SHV-ESBL was found in clinical samples from Argentina and Chile, respectively.14 Since then, different types of enzymes have been detected in South America with different predominating enzymes, namely, TEM and SHV, and CTX-M, the latter currently being the most widespread ESBL group in the region.7
Apart from human detections, beta-lactamases have been found in non-human specimens, animals, and the environment. The presence of ESBL genes in aquatic ecosystems has been studied in E. coli in different parts of the world, for example, in Mur River in Europe (ie, Austria)15 and in Yamato River in Asia (Japan)16 with blaCTX-M-1 and blaCTX-M-14 as the most prevalent ESBL genes, respectively.
Livestock and other animals used as food sources are a well-known reservoir of antibiotic-resistant microorganisms, despite the lack of literature exploring this topic. For example, few studies have explored veterinary sources of ESBLs, in stark contrast with the amount of data from humans.17 In 1988, ESBLs were detected for the first time in a dog in Japan with a strain of CTX-M-3-producing E. coli. ESBL types SHV-1, TEM-1, and OXA have been frequently described in E. coli and Salmonella spp. of animals and food of animal origin in Spain, Germany, the US, and the United Kingdom (UK).17
In South America, as in the rest of the world, human clinical studies of ESBLs in E. coli are abundant.18 Conversely, the current status of beta-lactam resistance in non-clinical scenarios such as their presence in healthy carriers, food matrices, animals, and the environment is scarce.19 Nevertheless, evidence suggests that limited access to public health services and lack of hygiene can contribute to the spread of ESBLs within communities.13,20 Moreover, the use of antibiotics as growth promoters in livestock animals favors the dissemination of different types of beta-lactamases CTX-M in food matrices.2,21 Finally, the poor management of hospital wastewater may result in discharge of multidrug-resistant coliforms (such as E. coli ESBL+) into natural waterbodies.22 All this evidence demonstrates the importance of conducting studies using a One Health approach, namely, understanding the dynamics surrounding human and animal health, and the environment, to develop strategies to monitor and control beta-lactam resistance.23
Due to the aforementioned arguments, in this study we have aimed to develop a systematic review of the current status of ESBLs in one of the most relevant and ubiquitous bacteria, E. coli, in South America, considering studies performed in the human, animal, and environmental realms to present a comprehensive summary offering updated information for practitioners across different fields.
Methods
Protocol and Search Strategy
This systematic review was developed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.24 The scientific literature was obtained from the NCBI-PubMed database on April 5th, 2021, including studies in English, Spanish, and Portuguese published since 1990 until 2021. Search terms included “Escherichia coli” AND “ESBL” OR “beta-lactamase” OR “β-lactamase”, plus the names of countries/territories that belong the South American region: ie, “Ecuador” OR “Peru” OR “Brazil” OR “Argentina” OR “Chile” OR “Colombia” OR “Venezuela” OR “Uruguay” OR “Paraguay” OR “Bolivia” OR “Suriname” OR “Guyana” OR “French Guiana”. All terms included the PubMed Title/Abstract criterion so that only studies that contained the searched keywords in their title and/or in their abstract were considered.
Additional articles found manually in Scopus, SciELO, and latindex databases were also included in this review. These articles were not found in the initial search because their title and/or abstract not included the search terms mentioned above; however, they had other keywords such as “CTX-M”, “resistomes”, “multidrug-resistant” or “multi-resistant”. These studies presented relevant epidemiological information related to CTX-M beta-lactamases.
Study Selection
The selection of the studies was carried out by two separate reviewers (VV and AM) using the Rayyan QCRI bibliographic manager to review only titles and abstracts of the selected articles. The first phase consisted in the removal of duplicated studies and the inclusion of those related to E. coli and South America while excluding reviews/letters and studies not focused on ESBLs.
After the first round of selection, a detailed review of the selected articles was implemented. During this eligibility phase, only those studies conducted in humans, animals, and/or the environment with complete information (ie, sample origin and ESBL positive cases detected either by phenotypic or molecular tests) were included for the final analysis. At this stage, exclusion criteria allowed the rejection of [1] case reports, [2] studies in Enterobacteriaceae and other bacterial families that did not report data on ESBLs in E. coli, [3] articles unavailable in full-text, and [4] studies conducted in regions different from South America.
Data Extraction
Studies selected were tabulated and introduced in a Microsoft Excel 2016 spreadsheet with their general information (ie, author, year, country, and URL). Data to be evaluated included (i) detection methods, (ii) type and origin of samples, (iii) prevalence of E. coli, (iv) prevalence of E. coli with ESBL phenotype, (v) prevalence of E. coli with ESBL genotype, (vi) ESBL types, and (vii) identification of clones by multi-locus sequence typing (MLST) of clinical importance. The three-prevalence parameters (points iii, iv, and v) were independently reported for each South American country; these values were obtained by dividing the number of samples found in each category (E. coli, E. coli with ESBL phenotype, and E. coli with ESBL genotype) with the total sample size (n). Relevant data are presented in statistical graphs.
Data Analysis
Descriptive statistics were obtained for all the studied parameters (eg, sample origin and source, E. coli prevalence, etc.) and are shown with 95% confidence intervals when appropriate. ESBL types and CTX-M variants were further categorized using descriptive statistics and their proportions were depicted per country in maps of the region using barplots and pie charts according to each of the established categories, that is, human clinical cases, human healthy carriers, animal, food, and environmental studies using R programming language version 3.6.3 and QGIS 2.18 “Las Palmas”.
Results
Studies Included
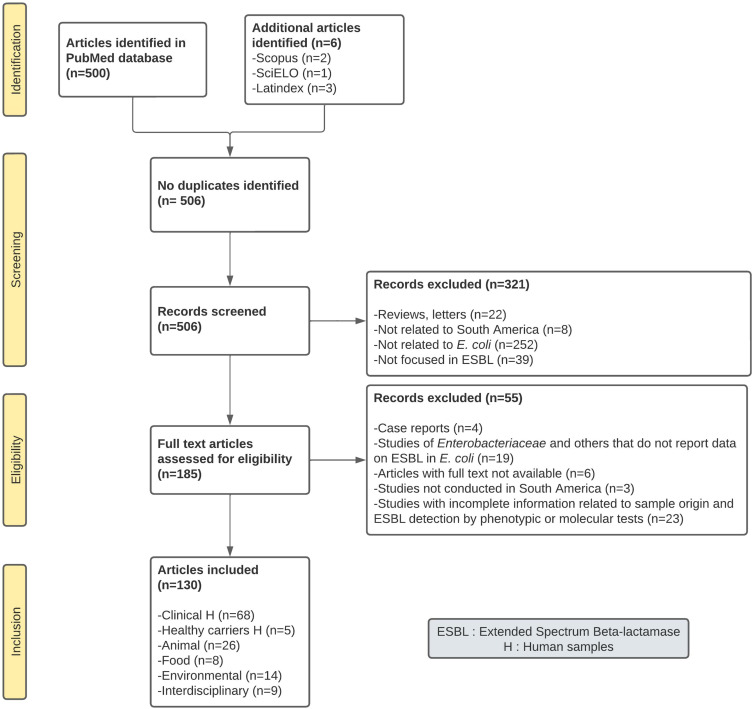
The total number of articles found in PubMed from 1990 to April 2021 was 500; additionally, six articles were also included from SciElo and Latindex databases for a total of 506 articles. During the first screening phase, 321 studies were excluded because they were either reviews/letters or articles that deviate from the theme of this review. During the eligibility phase, 55 studies were discarded due to their lack of detail. A total of 130 articles were included in this review (Figure 1).
Figure 1.
PRISMA flow diagram for study categorization and selection of the 130 studies included in this systematic review. Data came from PubMed and additional databases between 1990–2021.
Notes: Adapted from Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89.25 Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/legalcode).
Abbreviation: ESBL, extended spectrum beta-lactamases.
ESBLs Detection Methods for E. coli
From the 130 articles included, 25 used phenotypic tests, the three commonest being the disc diffusion, the minimum inhibitory concentration (MIC), and the VITEK system; the latter also used for bacterial identification. On the other hand, 14 articles used molecular tests including PCR (ie, either endpoint, multiplex, or quantitative) and sequencing to determine the presence of beta-lactamase coding genes. Ninety-one publications (70%) used both phenotypic and molecular tests for gene and bacteria identification.
Classification of Studies
The studies were classified into six categories according to the origin of the sample: two categories for human studies (clinical cases and healthy carriers), followed by animal, food, environmental, and interdisciplinary studies, here labeled as those analyzing more than one category at the same time. More than half of the studies corresponded to human samples (56%; n=73/130). From them, 52% (n=68/130) corresponded to isolations from human clinical studies and 4% (n=5/130) corresponded to studies on human healthy carriers, the smallest category on our analysis. Samples isolated from animals and the environment corresponded to 20% (n=26/130) and 11% (n=14/130), respectively. Interdisciplinary studies corresponded to 7% (n=9/130). Samples isolated from food corresponded to the 6% of the publications studied (n=8/130).
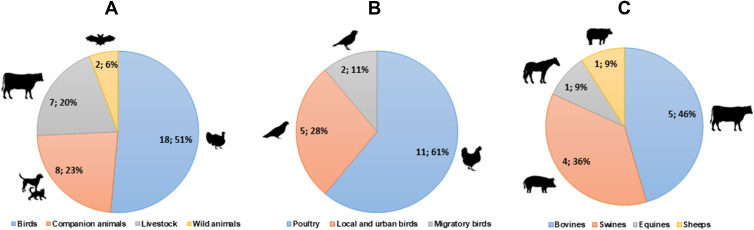
In addition, animal samples were sub-classified into birds, companion animals, livestock, and wild animals (Figure 2). Birds were investigated in more than half of animal-oriented studies (51%; n=18/35), followed by domestic animals (23%; n=8/35), farm animals (20%; n=7/35), and wild animals (6%; n=2/35; Figure 2A). A subcategorization of birds showed that poultry was the most studied with 61% (n=11/18) of publications, followed by urban species such as doves and pigeons with 28% (n=5/18), and migratory bird data in 11% of studies (n=2/18; Figure 2B). A subcategorization of livestock showed that cattle and pigs represented 46% (n=5/11) and 36% (n=4/11) of the, respectively, farm animals studied (Figure 2C). It is important to mention that in some publications, more than one type of farm animal was studied.
Figure 2.
Classification and sub-classification of ESBLs producing E. coli studies developed in animal samples. (A) General classification of animals identified and their distribution in number of studies and percentages (n;%). (B) Animal studies in birds: sub-groups identified and their distribution in number of studies and percentages. (C) Animal studies in livestock: sub-groups identified and their distribution in number of studies and percentage.
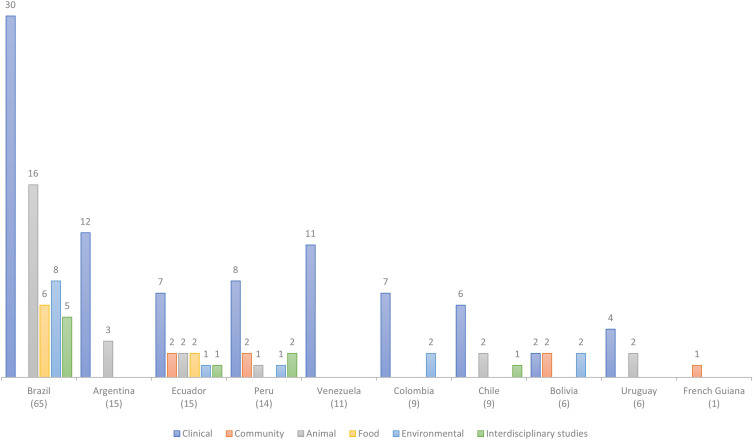
ESBL Producing E. coli Studies per Country
Fifty percent of the studies (n=65/130) was carried out in Brazil, followed by Argentina, and Ecuador with 11.5% (n=15/130) each. As it can be seen, Brazil exceeds with 50 studies to all other countries (Figure 3). It is worth noting that a fraction of the studies identified (n=7/130) were developed in more than one country; thus, at least 5.4% of the studies occurred as international multicenter approaches.
Figure 3.
Categorization of 130 studies included in this systematic review from PubMed and additional databases between 1990–2021. Color bars represent the number of studies conducted in South American countries and number of studies per country categorized by sample type examined.
As expected, a further categorization of sample type per country showed the predominance of samples from human clinical origin (Figure 3). For example, in Brazil, 46.2% (n=30/65) of the included studies corresponded to clinical isolations; moreover, in Venezuela, 100% of their research (n=12/12) were focused on nosocomial samples. Brazil, despite having the highest number of studies in the region, lacked studies on human healthy carriers. This pattern was similar across the rest of the countries analyzed, namely, predominance of human clinical samples followed by either one or two studies including any of the other studied categories (ie, healthy carriers, animal, or environmental sample types). Exceptions included French Guiana with a unique study focused on human healthy carriers, and Ecuador (n=15 studies) with at least one publication across each sample type category (Figure 3).
Prevalence and Distribution of ESBLs Producing E. coli
In South America, the prevalence of ESBLs at the level of the animal, food, and environment was larger than the prevalence from human sources (ie, either clinical cases or healthy carriers) (Table 1). The same pattern was evident in each country analyzed. Brazil presented the greatest number of samples of each category except for the healthy carriers, where data were absent. Details of these results per country are described in Supplementary Table 1.
Table 1.
Prevalence of E. coli Isolates According to Their Sample Sourc. Comparison of Prevalence of ESBL Determination by Phenotypic and Genotypic Methods Across Six Categories in 130 Studies from South America Between 1990 and 2021 (N=203057)
| Categories of Sample | Sample Size | E. coli Isolates | Phenotype of ESBL-Producing E. coli | Genotype of ESBL-Producing E. coli | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (N) | (n) | % | [95% CI] | (n) | (%) | [95% CI] | (n) | (%) | [95% CI] | |
| Clinical (H) | 185,203 | 28,348 | 15.3 | [0.151–0.155] | 3719 | 13.1 | [0.12–0.14] | 3509 | 1.9 | [0.018–0.02] |
| Healthy Carriers (H) | 7861 | 1105 | 14.1 | [0.133–0.149] | 490 | 6.2 | [0.057–0.067] | 139 | 1.8 | [0.02–0.2] |
| Animal | 6616 | 3607 | 54.5 | [0.533–0.557] | 1418 | 21.4 | [0.204–0.224] | 1195 | 18.1 | [0.1–0.2] |
| Food | 1860 | 1401 | 75.3 | [0.733–0.773] | 193 | 10.4 | [0.09–0.118] | 580 | 31.2 | [0.3–0.333] |
| Environment | 1517 | 553 | 36.5 | [0.341–0.389] | 191 | 12.6 | [0.109–0.143] | 187 | 12.3 | [0.106–0.14] |
Abbreviations: N, total samples of each category; H, human samples; 95% CI, 95% confidence Intervals.
ESBL Types and Enzymes Variants
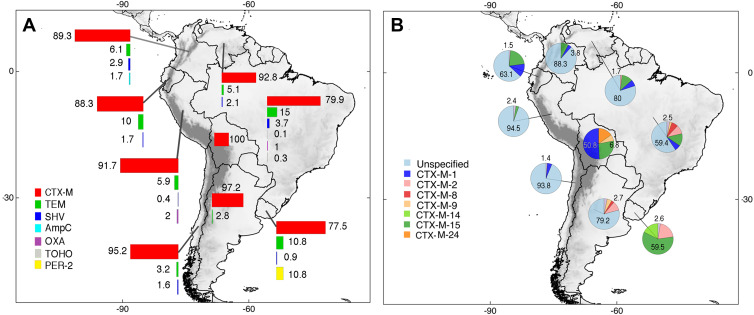
Human Clinical Studies
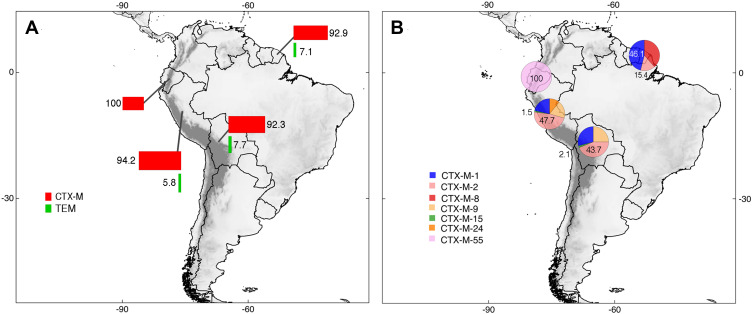
The total number of ESBLs genes in clinical samples was 3509. The South American distribution of ESBLs based on the selected studies shows that Brazil was the country with the highest number of detections with 21.3% (n=788/3701). Also, Brazil presented the highest diversity of ESBL types reporting CTX-M, TEM, SHV, TOHO, OXA, and AmpC enzymes. Surprisingly, PER-2 enzymes were only found in Uruguay. CTX-M enzymes were the most prevalent in South America with at least 89.4% (n=3309/3701) identifications. CTX-M enzymes variants recognized were usually reported as unspecified across countries/territories with few exceptional publications. For instance, multiple Bolivian studies reported the presence of CTX-M-1 (50.8%; n=67/132). Similarly, studies from Uruguay consistently reported the presence of CTX-M-15 (59.5%, n=47/79). These results are shown in more detail in Figure 4 and Supplementary Table 2.
Figure 4.
Distribution of ESBLs types (A) and CTX-M enzyme variants (B) in clinical human studies developed in South America. Unspecified = CTX-M enzyme present but variant unreported. Pie charts are showing the maximum and minimum percentages for each country. Complete information can be found in the main text and Supplementary Table 2.
Human Healthy Carriers Studies
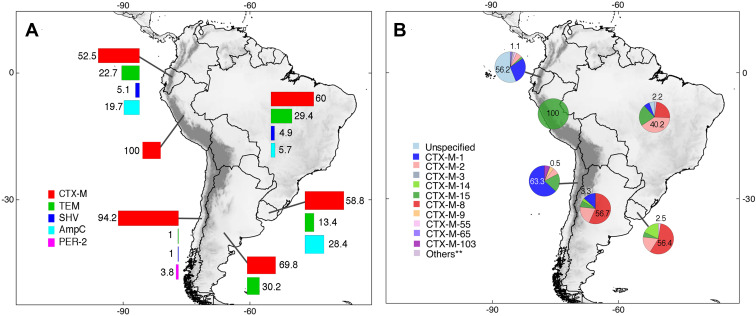
Epidemiological data focused on isolations from healthy carriers in South America were limited. Only Ecuador, Peru, Bolivia, and French Guiana reported ESBLs from this category; thus, the total number of ESBLs in this context was 204. The enzymes CTX-M (96%; n=195/204) and TEM (4%; n=9/204) were the only ESBLs found. The CTX-M-2 enzyme variants were most prevalent in Peru (47.7%; n=31/65) and Bolivia (43.7%; n=21/48). In French Guiana, the enzyme CTX-M-1 was the most significant variant with a prevalence of 46.1% (n=6/13). Conversely, only CTX-M-55 enzyme variants were reported in Ecuador (n=69/69). These results are depicted in more detail in Figure 5 and Supplementary Table 2.
Figure 5.
Distribution of ESBLs types (A) and CTX-M enzyme variants (B) identified in the context of healthy carriers human studies developed in South America. Pie charts are showing the maximum and minimum percentages for each country; complete information can be found in the main text and Supplementary Table 2.
Animal Studies
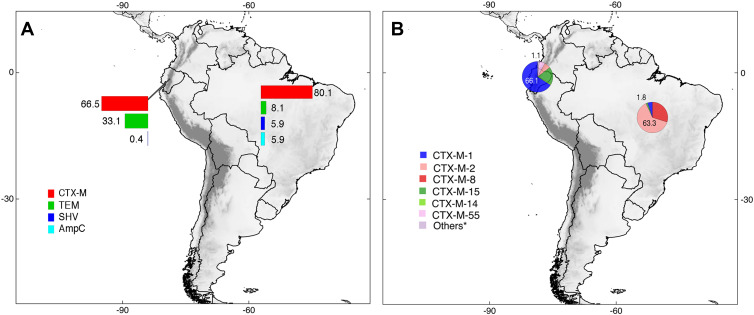
Six South American countries reported epidemiologic data in animals. The total number of ESBLs in animal samples was 1191. ESBL types identified included CTX-M, TEM, SHV, PER-2, and AmpC. CTX-M enzymes were the most prevalent (64.5%; n=768/1191). CTX-M enzyme variants featured included CTX-M-1 in Ecuador (28.4%; n=50/176) and Chile (63.3%; n=124/196); CTX-M-2 in Brazil (40.2%; n=127/316); and CTX-M-8 in Brazil (23.4%; n=74/316), Argentina (56.7%; n=17/30), and Uruguay (56.4%; n=22/39). Many CTX-M variants were recorded in Ecuador although the higher proportion (56.2%, n=99/176) of cases was represented by unknown variants. In Peru, only CTX-M-15 enzymes were reported (n=11/11). These results can be observed in more detail in Figure 6 and Supplementary Table 2.
Figure 6.
Distribution of ESBLs types (A) and CTX-M enzyme variants (B) identified in animals and developed in South America. Unspecified = CTX-M enzyme present but variant unreported. **Others = Variants of CTX-M enzymes with <1% of prevalence. Pie charts are showing the maximum and minimum percentages for each country; complete information can be found in the main text and Supplementary Table 2.
Food Studies
Only two countries (Ecuador and Brazil) published studies about ESBL detection in food. The total number of ESBLs in food samples was 520, among them, CTX-M, TEM, SHV, and AmpC were identified. CTX-M enzymes were the most prevalent (73.6%; n=383/520). Considering CTX-M variants, CTX-M-1 in Ecuador with 66.1% (n=109/165) and CTX-M-2 in Brazil with 63.3% (n=138/218) were found. These results can be observed in detail through Figure 7 and Supplementary Table 2.
Figure 7.
Distribution of ESBLs types (A) and CTX-M enzyme variants (B) identified in food and developed in South America. *Others = Variants of CTX-M enzymes with <1% of prevalence. Pie charts are showing the maximum and minimum percentages for each country; complete information can be found in the main text and in Supplementary Table 2.
Environmental Studies
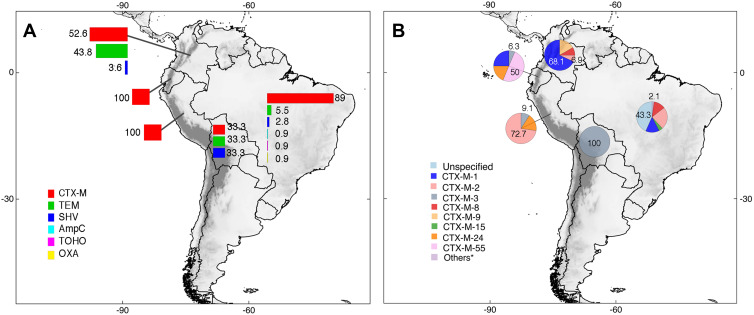
Environmental studies were found in five South American countries. The total number of ESBLs in environmental samples was 276. ESBL types identified included CTX-M, TEM, SHV, TOHO, OXA, and AmpC. Similar as it was obtained in results from the other categories (ie, human clinical cases, human healthy carriers, animals, and food studies), CTX-M enzymes were the most prevalent (71.4%; n=197/276). Among CTX-M variants, CTX-M-1 in Colombia (68.1%; n=49/72), CTX-M-2 in Peru (72.7%; n=8/11), and CTX-M-55 in Ecuador (50%; n=8/16) were reported. In Brazil, CTX-M variants were unknown in most cases, representing 43.3% (n=42/97) of all detections. In Bolivia, CTX-M-3 was the variant detected in their unique report (n=1/1). These results can be traced in detail in Figure 8 and Supplementary Table 2.
Figure 8.
Distribution of ESBLs types (A) and CTX-M enzyme variants (B) identified in the environment and developed in South America. Unspecified = CTX-M enzyme present but variant unreported. *Others = Variants of CTX-M enzymes with <1% of prevalence. Pie charts are showing the maximum and minimum percentages for each country; complete information can be found in the main text and Supplementary Table 2.
Clones of Epidemiological Importance
A total of 59 different clones were described in 31 studies. The clone E. coli ST131 represented 48.4% of the total of detected clones in the studies (n=15/31), followed by ST10 with 29% (n=9/31). The clones ST405, ST648, and ST38 accounted for 13% (n=4/31) each; ST410 and ST744 for 10% (n=3/31) each; followed by clones ST90, ST117, and ST155 representing the 6.4% (n=2/31). All the remaining clones were represented by a single detection across the reporting studies (3%; n=1/31 each; Supplementary Table 3). It is worth to mention that the presence of these clones was conditioned to their detection per country; thus, Brazil was the country that reported more clones (55%; n=38/59) followed by Peru (17.4%; n=12/59), Ecuador, Uruguay (11.6%; n=8/59 each), Chile (5.8%; n=4/59), and single reports of clones from Colombia, Argentina, and French Guiana (1.4%; n=1/59 each).
Discussion
The present systematic review of the literature provides relevant information on the distributions of ESBLs in E. coli in South America. To our knowledge, this is the first attempt that addresses the presence of ESBLs across different categories, going beyond human-derived clinical samples, to also consider samples from human healthy carriers, animals, environmental, and food isolations, echoing calls of multidisciplinary, One Health approaches, to comprehend the presence of antibiotic resistance mechanisms.
Of the 130 studies included in this review, Brazil contributed with more than half the research of this topic (n=65/130; Figure 3). These results correspond with evidence showing different levels of scientific production in South America where Brazil is recognized as a regional leader.25–28 The other South American countries had at least one publication on ESBLs producing E. coli,29 which is far from ideal and should prompt efforts to understand beta-lactam resistance and their importance in public health.2,3 Despite the low scientific production of Ecuador compared to the rest of South American countries,27,28 Ecuador was the country with the second highest research contribution in the region in this review (n=15/130), together with Argentina (Figure 3).
Considering the limitations of many South American laboratories (eg, logistics, equipment, infrastructure, others),30,31 we expected that the inclusion of molecular tests that require higher costs and increased technical expertise32 would have been lower compared to phenotypic tests. Consequently, in this review, phenotypic tests (n=25/130) were implemented in 11 more publications than molecular tests (n=14/130); however, most of the publications used both phenotypic and molecular tests (70%; n=91/130) for identification, which allows a more precise detection and therefore improvement of ESBLs epidemiological surveillance in E. coli.33 Some human clinical or environmental studies used molecular methods directly for ESBLs genes’ detection. Ideally, both detection methods should be implemented since neither is exempt from limitations. First, methods such as PCR are less effective in the presence of unknown mutations of new unreported ESBL variants, especially when these mutations appear at primer hybridization sites.33 Second, methods based on disk diffusion can report problems with interpretation when co-resistance events occur.34 Thus, new techniques for identifying ESBLs are being developed and have proven to be more sensitive, specific, efficient, and even provide other advantages such as point-of-care detections.35 One of the more recent options is the CRISPR-Cas9-based detection method with optical DNA mapping, which was used to identify blaCTX-M-15 and blaCTX-M-14 genes in E. coli from clinical urinary tract infections in Sweden.36
Up to 52% (n=68/130) of studies corresponded to human clinical samples, which depicts the lack of research about antimicrobial resistance from non-human oriented sources.19 For example, for this review, Venezuela contributed with publications only within this category (Figure 3). Reviews such as that of Guzmán et al37 expose the clinical situation in Venezuela but lack an analysis of antimicrobial resistance from animals, food products, or the environment.
Among the categories established in our review, ESBL detections from human healthy carriers, at the community level, were mostly underrepresented (n=5/130; Figure 3). Onduru et al evidenced a similar pattern in a review for African countries38 where human clinical studies represented the 74%, while studies performed on healthy carriers contributed only with the 15%. It is known that healthy carriers are an important reservoir for the transmission of beta-lactamases and therefore act as spreaders to healthy individuals or environmental settings. Further studies including surveillance at these scales might unveil a hidden pattern for the epidemiology of bacterial resistance in human populations.39,40
For this review, One Health studies were categorized as interdisciplinary, considering that they analyzed samples across different interfaces: human-animal,41–43 human-environment,44,45 human-food,46 animal-environment,47 human-animal-food,48 and animal-food-environment.49 The number of interdisciplinary studies included in this review was low (7%; n=9/130; Figure 3). Similarly, O’Neal et al review for Central America50 and Escher et al review for Africa51 found small numbers of One Health-related studies. Thus, apart from South America, other world regions also struggle to incorporate One Health approaches to their experimental designs; a reality that might be tackled with international cooperation, executing multi-sectorial action plans as proposed by the WHO.52 Many of the clinical studies included in the present review were “international multicenter studies”, which are characterized by promoting joint research across several countries, albeit these alliances are usually focused on human clinical samples.53 These types of studies might be a good example to follow to include a cooperative approach to address questions in the ecology and veterinary fields.
Considering animal publications, those for human consumption were more studied than other groups. Of these, 61% came from poultry in birds and 82% from bovines and swine in livestock. This can be explained due to awareness of the impact of antibiotic use as prophylactic treatment or most commonly as growth promoters for fattening. There is extensive evidence showing how this practice promotes the spread and therefore the risk of zoonotic antibiotic resistance mechanism contaminations through the food chain.54–56 Nevertheless, for this review, urban and migratory birds contributed with the 28% and 11% of ESBLs in E. coli, respectively. Recently, studies of migratory birds have incriminated their feces in the environment as possible contributors to the international spread of antimicrobial resistance.57–59 Studies focusing on this animal group should be encouraged to assess the validity of this hypothesis.
Veterinary publications have noticed a zoonotic transmission risk from pet animals, favored by their proximity to their owners.60–62 A similar trend can be stressed for the potential spillover of ESBLs; however, studies from pet animals were also underrepresented in our systematic review with only a 23%. Studies focused on wild animals were even less represented in our review (6%; n=2/35; Figure 2A). Wildlife might be an important source for the spread of resistance mechanisms as they act as bridges between the urban and sylvatic environments, especially mammals.63 Another example is that, in Brazil, fishes have been found to contribute to the spread of ESBLs in natural waterbodies and its marine fauna.64,65
In South America, higher values of ESBL producing E. coli prevalence were obtained from animal, food, and environmental sources compared to human samples (Table 1). In our review, one of these results showed a prevalence of E. coli with ESBL genotype of 18.1% in animals and 12.3% in the environment compared to 1.9% in clinical studies. These results were analogous among the majority of South American countries and similar to observations in Tanzania, the Netherlands, and other regions of the world where ESBLs from animal and environmental sources showed between a 10 to 20% higher prevalence than humans.66–68 Therefore, although apparently many of the E. coli resistance mechanisms are acquired in the clinical setting, prevalence in animals and environmental sources predominate and should be further studied.
CTX-M enzymes were the most prevalent, with more than 50% detections in each country and category analyzed in this review (ie, human clinical samples, human healthy carriers, animal, food, and environment; Figures 4–8). Similar results have been reported in the rest of the world. For example, in Africa CTX-M prevalence reaches an 81.5%.38 In Iran, CTX-M enzyme prevalence reached 31.2% followed by TEM with 27.6%.69 It is worth to mention that the prevalence analyzed here only accounted for E. coli, thus it might be an underestimation if including other bacterial species such as K. pneumoniae, which usually harbor TEM or SHV enzymes.70–72
Apart from the best-known enzymes (ie, TEM, SHV, and CTX-M), TOHO, reported for the first time in Japan in 1993,73 was also found in South America among human clinical and environmental studies (Figures 4A and 8A). Thus, in little less than three decades, TOHO enzymes have spread to a completely different region albeit its low prevalence (<0.1%; n=1/3701). Other types of beta-lactamases that are worth highlighting are the OXA (<0.1%; n=17/3701) and AmpC (<0.1%; n=9/3701) enzymes. Both show a different resistance spectrum to the most common resistant enzymes. OXA enzymes can hydrolyze more effectively antibiotics such as carbapenems,74 while AmpC is not inhibited by clavulanic acid.75 The ESBL enzymes PER-2, with similar spectrum to TEM and SHV enzymes,76 were only found in Uruguay with a low prevalence (Figure 4A). However, Celenza et al76 have reported PER-2 isolated from Enterobacteriaceae in Bolivian hospitals, which suggests the existence of PER-2-carrying E. coli in this country. Although detected, CTX-M enzyme variants were poorly reported (Figure 4B). Detection of variants is one of the most important clinical data because each one has differences in their antibiotic response.77–79 It is worth noting that in other regions of the world such as Nigeria, Tunisia, and the Netherlands, CTX-M-15 variant isolated from clinical settings is usually detected with a prevalence ranging from 67.9% to 83.3%.80–82
Considering animal studies, the presence of CTX-M-8 enzyme variant was frequently described in countries such as Brazil, Argentina, and Uruguay (Figure 6B). Because CTX-M-8 was first isolated from Enterobacteriaceae in Brazil,83 the most likely scenario involves it spread across animals from neighboring countries, despite the lack of reports of CTX-M-8 in Chile, Peru, and Ecuador according to our review. For these countries, the variants CTX-M-1 and CTX-M-15 were detected, as has been seen in goat samples from Tunisia, pigs from Portugal, horses from the UK, and processed beef from Germany.84–87
From food studies, the main types of CTX-M enzymes detected included the CTX-M-1 in Ecuador and the CTX-M-2 in Brazil (Figure 7B); results were consistent with reports from Germany88,89 and Algeria90 where the CTX-M-1 variant is the most prevalent. However, as only few studies address the presence of antibiotic resistant enzymes in food-related sources, more research is granted to confirm their role as a mechanism of spread with public health consequences.
The enzymes of type TOHO, OXA, and AmpC from environmental studies were found only in Brazil (Figure 8A). These types of ESBLs had an overall low prevalence. For CTX-M enzyme variants from environmental sources, there was a great variability of detection across South American countries, namely, the enzyme CTX-M-1 in Colombia, CTX-M-3 enzyme in Ecuador/Bolivia, and the CTX-M-2 enzyme in Peru/Brazil (Figure 8B). Lines of research that go beyond the simple detection of ESBLs in the environment should be encouraged as has been done in other regions of the world. For example, in Nigeria, Lebanon, Vietnam, and India, there are studies assessing the impact of antibiotic release on hospital wastewater correlated with patterns on resistance acquisition in E. coli.91–94 Research from the UK, Tanzania, and the Dominican Republic95–97 have revealed the importance of IncF plasmids found in natural waterbodies. Being a conjugative plasmid, IncF is related to the dissemination of blaCTX-M-15 by horizontal gene transfer.98,99 Finally, other exemplary studies show how activated sludge from wastewater treatment plants can be a source of high prevalence of CTX-M as demonstrated in Japan,100 Austria,101 and India.102
The E. coli clones ST131 and ST10 were found across South America (Supplementary Table 3). These results are consistent with a study conducted in Canada in which 96/209 (46%) E. coli strains corresponded to the clonal complex ST131103 and with one developed in the Netherlands where from 112 strains belonging to E. coli, 21% belonged to ST131 and 17% to ST10,82 demonstrating the worldwide high prevalence of the ST131 clone. These clones are known to be a major reservoir of plasmids carrying resistant genes to multiple antibiotics, including blaTEM, blaSHV, and blaCTX-M.104 The influence of international travel on the dissemination of these clones has been studied in countries such as Germany, where the ST131 clone ranges between 19% and 30%, or the Netherlands, where the ST131 clone prevalence reaches a 21.4%.82,105 For the purposes of this argument, it is worth to mention that Woerther et al106 reported the international clone ST10 in healthy carriers from a remote community at French Guiana, which begs the question on how this clone was acquired within an isolated population.
Limitations
Our results are based on a systematic review of published academic literature. Potentially, there is relevant information among the grey literature (eg, thesis) that might complement the results presented here; however, we rely on the quality of peer-review publications to assess the status of E. coli ESBLs in South America with certainty. Similarly, our analysis excluded articles in the category of “reviews” that sometimes present pieces of original research, but we believe that their overall contribution in the presented information may be negligible. Furthermore, while we comprehensibly reviewed each of the 130 manuscripts included in this study, data heterogeneity across different countries and publications is a challenge that was overcome with some heuristic categorizations, which are the basis of any systematic review.
Finally, it is worth noticing that although manuscripts included in the present review were considered of high quality by the individual assessment of their results, we are aware that potentially some of them might be published in journals considered predatory. We believe that science should be judged by their findings instead of the journal in which it was published, and for this review we can trust in the reliability of the studies analyzed.
Conclusions
ESBLs producing E. coli in South America are widely distributed and show a high diversity of enzyme variants. ESBLs in human samples are the most studied, mainly in those linked to hospital environments (inpatient and outpatient). However, ESBLs in food and animal samples are the most prevalent. Countries such as Brazil present more studies on ESBL surveillance involving various sample sources. CTX-M enzymes are the most common and diverse of the types of beta-lactamases found and show a high prevalence across all the studied categories. ST131 and ST10 are the most widespread clones in the studies included in this review.
In order to fully characterize the situation of E. coli ESBLs in South America, a greater contribution from underrepresented countries of the region should be encouraged. These contributions ideally should emphasize the role of sources different from human clinical settings such as animals, environmental, and food matrices, together with detections from human healthy carriers. Concerns related to transmission of resistant mechanisms among human healthy carriers, zoonotic sources, as well as the spread of ESBLs in aquatic ecosystems, reveal the importance of developing studies beyond the human clinical-centered view of health. Furthermore, the importance of animal and environmental health should be explored since ESBL genes in both realms have been detected in South America and the rest of the world.
Efforts to increase the epidemiological surveillance of the region to detect predominant types of ESBLs and the presence of new variants, as well as the distribution of ST clones, should be a priority considering their different roles in antibiotic resistance and their traceability to detect infection sources. At this point, the inclusion of both phenotypic and molecular tests, as well as the development of new detection techniques, should facilitate surveillance efforts to further the understanding of ESBL distribution in South America.
Finally, the information presented in this review can be used as basis for subsequent implementation of monitoring programs, targeting potential critical points of transmission sources. Following the One Health concept, the development of contingency plans in different areas like hospitals, broiler breeding sites, and wastewater treatment plants might contribute to the identification of resistant enzymes and their spreading, which ideally should be controlled if not completely halted; within this objective, a multi-sectoral and multi-disciplinary cooperation will be of utmost importance.
Supplementary Materials
To a better description of findings of this work, the following supporting information can be downloaded. Supplementary Table 1: Number of samples identified (frequencies) and % prevalence of E. coli, E. coli with ESBL phenotype, and E. coli with ESBL genotype in South America from human clinical samples, human healthy carriers, animal, food, and environmental studies. Data from 130 studies included in systematic review between 1990 and 2021. Supplementary Table 2: Percentages of different beta-lactamase enzymes identified across South American countries and CTX-M variants for human clinical samples, human healthy carriers, animal, food, and environmental studies. Data from 130 studies included in systematic review between 1990 and 2021. Supplementary Table 3: E. coli ST clones found in studies in South America per country and author. Data from 130 studies included in systematic review between 1990 and 2021. Supplementary Table 4: Summary Data Base and list of studies included in the systematic review and general data from 130 studies included between 1990 and 2021. Supplementary Table 5: List of additional references included in the systematic review.107–225
Acknowledgments
Our thanks to the Universidad de las Américas for financing the APCs of this work. Special thanks to Adriana Gallegos-Ordoñez for her help in proofreading of English language and support in the writing of this work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bradford PA. Extended-spectrum β-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Micro Rev. 2001;14:933–951. doi: 10.1128/CMR.14.4.933-951.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Behzadi P, García-Perdomo HA, Karpiński TM, Issakhanian L. Metallo-ß-lactamases: a review. Mol Biol Rep. 2020;47(8):6281–6294. doi: 10.1007/s11033-020-05651-9 [DOI] [PubMed] [Google Scholar]
- 3.Issakhanian L, Behzadi P. Antimicrobial agents and urinary tract infections. Curr Pharm Des. 2019;25(12):1409–1423. doi: 10.2174/1381612825999190619130216 [DOI] [PubMed] [Google Scholar]
- 4.Hozzari A, Behzadi P, Kerishchi Khiabani P, Sholeh M, Sabokroo N. Clinical cases, drug resistance, and virulence genes profiling in Uropathogenic Escherichia coli. J Appl Genet. 2020;61(2):265–273. doi: 10.1007/s13353-020-00542-y [DOI] [PubMed] [Google Scholar]
- 5.Hernández J, Stedt J, Bonnedahl J, et al. Human-associated extended-spectrum β-lactamase in the Antarctic. Appl Environ Microbiol. 2012;78(6):2056–2058. doi: 10.1128/AEM.07320-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bush K. Past and present perspectives on β-lactamases. Antimicrob Agents Chemother. 2018;62(10). doi: 10.1128/AAC.01076-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Villegas MV, Kattan JN, Quinteros MG, Casellas JM. Prevalence of extended-spectrum β-lactamases in South America. Clin Micro Infect. 2008;14:154–158. doi: 10.1111/j.1469-0691.2007.01869.x [DOI] [PubMed] [Google Scholar]
- 8.Rada AM, Hernández-Gómez C, Restrepo E, Villegas MV. Distribution and molecular characterization of beta-lactamases in Gram-negative bacteria in Colombia, 2001–2016. Biomédica. 2019;39:199–220. doi: 10.7705/biomedica.v39i3.4351 [DOI] [PubMed] [Google Scholar]
- 9.Paterson D, Bonomo R. Extended-spectrum β-lactamases: a clinical update. Clin Microbiol Rev. 2005;18(4):657. doi: 10.1128/CMR.18.4.657-686.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mella MS, Zemelman MC, Bello TH, Dominguez YM, Gonzalez RG, Zemelman ZR. Microbiological properties, classification and structure-activity relationship of cephalosporins and importance of fourth generation cephalosporins. Rev Chil Infectol. 2001;18(1):7–19. [Google Scholar]
- 11.Polanco-Hinostroza F, Loza-Munarriz R. Resistencia antibiótica en infecciones urinarias en niños atendidos en una institución privada, periodo 2007 – 2011 [Antibiotic resistance in urinary tract infections in children cared for in a private institution, period 2007 – 2011]. Rev Medica Hered. 2013;24(3):210–216. [Google Scholar]
- 12.Oliveira C, Amador P, Prudêncio C, Tomaz C, Tavares P, Fernandes R. ESBL and AmpC β-lactamases in clinical strains of Escherichia coli from Serra da Estrela, Portugal. Medicina. 2019;55(6):272. doi: 10.3390/medicina55060272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Behzadi P, Behzadi E. The microbial agents of urinary tract infections at central laboratory of Dr. Shariati Hospital, Tehran, Iran. Turk Klin Tip Bilim. 2008;28(4):445–449. [Google Scholar]
- 14.Paterson D, Hujer K, Hujer A, et al. Extended-spectrum β-lactamases in Klebsiella pneumoniae bloodstream isolates from seven countries: dominance and widespread prevalence of SHV- and CTX-M-type β-lactamases. Antimicrob Agents Chemother. 2003;47(11):3554–3560. doi: 10.1128/AAC.47.11.3554-3560.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zarfel G, Lipp M, Gürtl E, et al. Troubled water under the bridge: screening of River Mur water reveals dominance of CTX-M harboringEscherichia coli and for the first time an environmental VIM-1 producer in Austria. Sci Total Environ. 2017;593-594:399–405. doi: 10.1016/j.scitotenv.2017.03.138 [DOI] [PubMed] [Google Scholar]
- 16.Gomi R, Matsuda T, Matsumura Y, et al. Whole-genome analysis of antimicrobial-resistant and extraintestinal pathogenic Escherichia coli in river water. Appl Environ Microbiol. 2017;83(5). doi: 10.1128/AEM.02703-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carattoli A. Animal reservoirs for extended spectrum beta-lactamase producers. Clin Microbiol Infect. 2008;14:117–123. doi: 10.1111/j.1469-0691.2007.01851.x [DOI] [PubMed] [Google Scholar]
- 18.McEwen SA, Collignon PJ. Antimicrobial resistance: a one health perspective. Microbiol Spectr. 2018;6(2). doi: 10.1128/microbiolspec.ARBA-0009-2017 [DOI] [PubMed] [Google Scholar]
- 19.Rousham EK, Unicomb L, Islam MA. Human, animal and environmental contributors to antibiotic resistance in low-resource settings: integrating behavioural, epidemiological and One Health approaches. Proc Biol Sci. 2018;285(1876). doi: 10.1098/rspb.2018.0332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Founou RC, Founou LL, Essack SY. Clinical and economic impact of antibiotic resistance in developing countries: a systematic review and meta-analysis. PLoS One. 2017;12(12):e0189621. doi: 10.1371/journal.pone.0189621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aworh MK, Kwaga J, Okolocha E, et al. Extended-spectrum ß-lactamase-producing Escherichia coli among humans, chickens and poultry environments in Abuja, Nigeria. One Health Outlook. 2020;2(8). doi: 10.1186/s42522-020-00014-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alonso CA, Zarazaga M, Sallem RB, Jouini A, Slama KB, Torres C. Antibiotic resistance in Escherichia coli in husbandry animals: the African perspective. Lett Appl Microbiol. 2017;64(5):318–334. doi: 10.1111/lam.12724 [DOI] [PubMed] [Google Scholar]
- 23.Destoumieux-Garzón D, Mavingui P, Boetsch G, et al. The one health concept: 10 years old and a long road ahead. Front Vet Sci. 2018;5:14. doi: 10.3389/fvets.2018.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(89). doi: 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.González G, Park J, Huamaní C, Ramos JM. Dominance and leadership in research activities: collaboration between countries of differing human development is reflected through authorship order and designation as corresponding authors in scientific publications. PLoS One. 2017;12(8):e0182513. doi: 10.1371/journal.pone.0182513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glänzel W, Leta J, Thijs B. Science in Brazil. Part 1: a macro-level comparative study. Scientometrics. 2006;67:67–86. doi: 10.1007/s11192-006-0055-7 [DOI] [Google Scholar]
- 27.Carvajal-Tapia AE, Carvajal-Rodríguez E. Status of scientific production in medicine in South America. 1996-2016. Rev Fac Med. 2018;66(4):595–600. doi: 10.15446/revfacmed.v66n4.67215 [DOI] [Google Scholar]
- 28.Carvajal-Tapia AE, Carvajal-Rodríguez E. Producción científica en ciencias de la salud en los países de América Latina, 2006-2015: análisis a partir de SciELO [Scientific production in health sciences in Latin American countries, 2006–2015: analysis from SciELO]. Revista Interamericana de Bibliotecología. 2019;42(1):15–21. Spanish. [Google Scholar]
- 29.Ciocca D, Delgado G. The reality of scientific research in Latin America; an insider’s perspective. Cell Stress Chaperones. 2017;22:847–852. doi: 10.1007/s12192-017-0815-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ashley E, Recht J, Chua A, et al. An inventory of supranational antimicrobial resistance surveillance networks involving low- and middle-income countries since 2000. J Antimicrob Chemother. 2018;73(7):1737–1749. doi: 10.1093/jac/dky026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pfaller M, Segreti J. Overview of the epidemiological profile and laboratory detection of extended-spectrum β-lactamases. Clin Infect Dis. 2006;42(Suppl 4):S153–S163. doi: 10.1086/500662 [DOI] [PubMed] [Google Scholar]
- 32.Thomas S. Antimicrobial Resistance: Global Challenges and Future Interventions. 1st ed. Singapore: Springer; 2020. [Google Scholar]
- 33.Pitout J, Hossain A, Hanson N. Phenotypic and molecular detection of CTX-M-beta-lactamases produced by Escherichia coli and Klebsiella spp. J Clin Microbiol. 2004;42(12):5715–5721. doi: 10.1128/JCM.42.12.5715-5721.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Calvo J, Cantón R, Cuenca FF, Mirelis B, Navarro F. Procedimientos En Microbiología Clínica [Procedures in Clinical Microbiology]. 1st ed. Cercenado E, Cantón R, eds. Spain: SEIMC; 2011. Spanish. [Google Scholar]
- 35.Jia F, Li X, Zhang C, Tang X. The expanded development and application of CRISPR system for sensitive nucleotide detection. Protein Cell. 2020;11:624–629. doi: 10.1007/s13238-020-00708-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Müller V, Rajer F, Frykholm K, et al. Direct identification of antibiotic resistance genes on single plasmid molecules using CRISPR/Cas9 in combination with optical DNA mapping. Sci Rep. 2016;6(1). doi: 10.1038/srep37938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guzmán M, Labarca JA, Villegas MV, Gotuzzo E; Latin America Working Group on Bacterial Resistance. Extended spectrum β-lactamase producers among nosocomial Enterobacteriaceae in Latin America. Braz J Infect Dis. 2014;18(4):421–433. doi: 10.1016/j.bjid.2013.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Onduru G, Mkakosya R, Aboud S, Rumisha S. Genetic determinants of resistance among ESBL-producing Enterobacteriaceae in healthy carriers and hospital settings in East, Central, and Southern Africa: a systematic review and meta-analysis of prevalence. Can J Infect Dis Med Microbiol. 2021;2021:1–9. doi: 10.1155/2021/5153237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Storberg V. ESBL-producing Enterobacteriaceae in Africa – a non-systematic literature review of research published 2008–2012. Infect Ecol Epidemiol. 2014;4(1):20342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ebrahimi F, Mózes J, Mészáros J, et al. Asymptomatic faecal carriage of ESBL producing Enterobacteriaceae in Hungarian healthy individuals and in long-term care applicants: a shift towards CTX-M producers in the healthy carriers. Infect Dis. 2016;48(7):557–559. doi: 10.3109/23744235.2016.1155734 [DOI] [PubMed] [Google Scholar]
- 41.Borges CA, Tarlton NJ, Riley LW. Escherichia coli from commercial broiler and backyard chickens share sequence types, antimicrobial resistance profiles, and resistance genes with human extraintestinal pathogenic Escherichia coli. Foodborne Pathog Dis. 2019;16(12):813–822. doi: 10.1089/fpd.2019.2680 [DOI] [PubMed] [Google Scholar]
- 42.Hernandez J, Johansson A, Stedt J, et al. Characterization and comparison of extended-spectrum β-lactamase (ESBL) resistance genotypes and population structure of Escherichia coli isolated from Franklin’s gulls (Leucophaeus pipixcan) and humans in Chile. PLoS One. 2013;8(9):e76150. doi: 10.1371/journal.pone.0076150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murray M, Salvatierra G, Dávila A, et al. Market Chickens as a Source of Antibiotic-Resistant Escherichia coli in a Peri-Urban Healthy carriers in Lima, Peru. Front Microbiol. 2021;12:635871. doi: 10.3389/fmicb.2021.635871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dias-Gonçalves V, Meirelles F, Cataldo M, et al. Detection of multidrug-resistant Enterobacteriaceae isolated from river waters flowing to the Guanabara Bay and from clinical samples of hospitals in Rio de Janeiro, Brazil. Biomedica. 2019;39(Suppl 1):S135–S149. doi: 10.7705/biomedica.v39i0.4391 [DOI] [PubMed] [Google Scholar]
- 45.Pehrsson E, Tsukayama P, Patel S, et al. Interconnected microbiomes and resistomes in low-income human habitats. Nature. 2016;533:212–216. doi: 10.1038/nature17672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koga V, Maluta R, da Silveira W, et al. Characterization of CMY-2-type beta-lactamase-producing Escherichia coli isolated from chicken carcasses and human infection in a city of South Brazil. BMC Microbiol. 2019;19:174. doi: 10.1186/s12866-019-1550-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brisola MC, Crecencio RB, Bitner DS, et al. Escherichia coli used as a biomarker of antimicrobial resistance in pig farms of Southern Brazil. Sci Total Environ. 2019;647:362–368. doi: 10.1016/j.scitotenv.2018.07.438 [DOI] [PubMed] [Google Scholar]
- 48.Ortega D, de Janon S, Villavicencio F, et al. Broiler farms and carcasses are an important reservoir of multi-drug resistant Escherichia coli in Ecuador. Front Vet Sci. 2020;7:547843. doi: 10.3389/fvets.2020.547843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gazal L, Medeiros L, Dibo M, et al. Detection of ESBL/AmpC-producing and fosfomycin-resistant Escherichia coli from different sources in poultry production in Southern Brazil. Front Microbiol. 2021;11:604544. doi: 10.3389/fmicb.2020.604544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.O’Neal L, Alvarez D, Mendizábal R, Ramay B, Graham J. Healthy carriers-acquired antimicrobial resistant Enterobacteriaceae in Central America: a one health systematic review. Int J Environ Res Public Health. 2020;17(20):7622. doi: 10.3390/ijerph17207622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Escher N, Muhummed A, Hattendorf J, Vonaesch P, Zinsstag J. Systematic review and meta-analysis of integrated studies on antimicrobial resistance genes in Africa-a one health perspective. Trop Med Int Health. 2021;26(10):1153–1163. doi: 10.1111/tmi.13642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.World Health Organization [WHO]. Global action plan on antimicrobial resistance; 2016. Available from: http://www.emro.who.int/health-topics/drug-resistance/global-action-plan.html. Accessed May 14, 2021.
- 53.Bangdiwala S, De Paula C, Ramiro L, Muñoz S. Coordinación de estudios multicéntricos internacionales: estructura administrativa y reglamentación [Coordination of international multicenter studies: administrative structure and regulations]. Salud Pública de México. 2003;45(1):58–66. Spanish. doi: 10.1590/S0036-36342003000100008 [DOI] [PubMed] [Google Scholar]
- 54.Kumar Y. Antimicrobial Resistance: A Global Threat. London: IntechOpen; 2019. [Google Scholar]
- 55.Wang Y, Hu Y, Cao J, et al. Antibiotic resistance gene reservoir in live poultry markets. J Infect. 2019;78(6):445–453. doi: 10.1016/j.jinf.2019.03.012 [DOI] [PubMed] [Google Scholar]
- 56.Bacanlı M, Başaran N. Importance of antibiotic residues in animal food. Food Chem Toxicol. 2019;125:462–466. doi: 10.1016/j.fct.2019.01.033 [DOI] [PubMed] [Google Scholar]
- 57.Silva GG, Campana EH, Vasconcelos PC, et al. Ocorrência de Escherichia coli produtora de KPC em psitaciformes resgatados do tráfico na Paraíba, Brasil [Occurrence of KPC-Producing Escherichia coli in Psittaciformes Rescued from Trafficking in Paraíba, Brazil]. Int J Environ Res Public Health. 2021;18(1):95. Portuguese. doi: 10.3390/ijerph18010095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Islam MS, Nayeem MMH, Sobur MA, et al. Virulence determinants and multidrug resistance of Escherichia coli isolated from migratory birds. Antibiot. 2021;10(2):190. doi: 10.3390/antibiotics10020190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wu J, Huang Y, Rao D, Zhang Y, Yang K. Evidence for environmental dissemination of antibiotic resistance mediated by wild birds. Front Microbiol. 2018;9:745. doi: 10.3389/fmicb.2018.00745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pomba C, Rantala M, Greko C, et al. Public health risk of antimicrobial resistance transfer from companion animals. J Antimicrob Chemother. 2017;72(4):957–968. doi: 10.1093/jac/dkw481 [DOI] [PubMed] [Google Scholar]
- 61.Melo LC, Oresco C, Leigue L, et al. Prevalence and molecular features of ESBL/pAmpC-producing Enterobacteriaceae in healthy and diseased companion animals in Brazil. Vet Microbiol. 2018;221:59–66. doi: 10.1016/j.vetmic.2018.05.017 [DOI] [PubMed] [Google Scholar]
- 62.Riwu KHP, Effendi MH, Rantam FA. A review of extended spectrum β-lactamase (ESBL) producing Klebsiella pneumoniae and multidrug resistant (MDR) on companion animals. Syst Rev Pharm. 2020;11(7):8. [Google Scholar]
- 63.Poo-Muñoz DA, Elizondo-Patrone C, Escobar LE, et al. Fleas and ticks in carnivores from a domestic-wildlife interface: implications for public health and wildlife. J Med Entomol. 2016;53(6):1433–1443. doi: 10.1093/jme/tjw124 [DOI] [PubMed] [Google Scholar]
- 64.Sellera FP, Fernandes MR, Moura Q, Carvalho MPN, Lincopan N. Extended-spectrum-β-lactamase (CTX-M)-producing Escherichia coli in wild fishes from a polluted area in the Atlantic Coast of South America. Mar Pollut Bull. 2018;135:183–186. doi: 10.1016/j.marpolbul.2018.07.012 [DOI] [PubMed] [Google Scholar]
- 65.Almeida MVA, Cangussú ÍM, Carvalho ALS, Brito ILP, Costa RA. Drug resistance, AmpC-β-lactamase and extended-spectrum β-lactamase-producing Enterobacteriaceae isolated from fish and shrimp. Rev Inst Med Trop Sao Paulo. 2017;59. doi: 10.1590/s1678-9946201759070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Seni J, Moremi N, Matee M, et al. Preliminary insights into the occurrence of similar clones of extended-spectrum beta-lactamase-producing bacteria in humans, animals and the environment in Tanzania: a systematic review and meta-analysis between 2005 and 2016. Zoonoses Public Health. 2018;65(1):1–10. doi: 10.1111/zph.12387 [DOI] [PubMed] [Google Scholar]
- 67.Dorado A, Smid JH, van Pelt W, et al. Molecular relatedness of ESBL/AmpC-producing Escherichia coli from humans, animals, food and the environment: a pooled analysis. J Antimicrob Chemother. 2018;73(2):339–347. doi: 10.1093/jac/dkx397 [DOI] [PubMed] [Google Scholar]
- 68.Pormohammad A, Nasiri MJ, Azimi T. Prevalence of antibiotic resistance in Escherichia coli strains simultaneously isolated from humans, animals, food, and the environment: a systematic review and meta-analysis. Infect Drug Resist. 2019;12:1181. doi: 10.2147/IDR.S201324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jabalameli L, Beigverdi R, Ranjbar HH, Pouriran R, Jabalameli F, Emaneini M. Phenotypic and genotypic prevalence of extended-spectrum β-lactamase-producing Escherichia coli: a systematic review and meta-analysis in Iran. Microb Drug Resist. 2021;27(1):73–86. doi: 10.1089/mdr.2019.0396 [DOI] [PubMed] [Google Scholar]
- 70.Malik T, Naim A, Saeed A. Molecular detection of TEM, SHV and CTX-M genes among gram-negative Klebsiella isolates. Curr Drug Deliv. 2018;15(3):417–423. doi: 10.2174/1567201815666180101160108 [DOI] [PubMed] [Google Scholar]
- 71.Mondal AH, Siddiqui MT, Sultan I, Haq QMR. Prevalence and diversity of blaTEM, blaSHV and blaCTX-M variants among multidrug resistant Klebsiella spp. from an urban riverine environment in India. Int J Environ Health Res. 2018;29(2):117–129. doi: 10.1080/09603123.2018.1515425 [DOI] [PubMed] [Google Scholar]
- 72.Ramos DA, Pulgarín JAH, Gómez GAM, et al. Geographic mapping of Enterobacteriaceae with extended-spectrum β-lactamase (ESBL) phenotype in Pereira, Colombia. BMC Infect Dis. 2020;20(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tzouvelekis LS, Tzelepi E, Tassios PT, Legakis NJ. CTX-M-type β-lactamases: an emerging group of extended-spectrum enzymes. Int J Antimicrob Agents. 2000;14(2):137–142. doi: 10.1016/S0924-8579(99)00165-X [DOI] [PubMed] [Google Scholar]
- 74.Pitout JDD, Peirano G, Kock MM, Strydom KA, Matsumura Y. The global ascendency of OXA-48-type carbapenemases. Clin Microbiol Rev. 2020;33(1):e00102–e00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Martinez D. Betalactamasas tipo AmpC: generalidades y métodos para detección fenotípica [AmpC-type beta-lactamases: overview and methods for phenotypic detection]. Rev Soc Ven. 2009;29(2):78–83. Spanish. [Google Scholar]
- 76.Celenza G, Pellegrini C, Caccamo M, Segatore B, Amicosante G, Perilli M. Spread of blaCTX-M-type and blaPER-2 β-lactamase genes in clinical isolates from Bolivian hospitals. J Antimicrob Chemother. 2006;57(5):975–978. doi: 10.1093/jac/dkl055 [DOI] [PubMed] [Google Scholar]
- 77.D’Andrea MM, Arena F, Pallecchi L, Rossolini GM. CTX-M-type β-lactamases: a successful story of antibiotic resistance. Int J Med Microbiol. 2013;303(6–7):305–317. doi: 10.1016/j.ijmm.2013.02.008 [DOI] [PubMed] [Google Scholar]
- 78.He D, Chiou J, Zeng Z, Chan EWC, Liu JH, Chen S. Comparative characterization of CTX-M-64 and CTX-M-14 provides insights into the structure and catalytic activity of the CTX-M class of enzymes. Antimicrob Agents Chemother. 2016;60(10):6084–6090. doi: 10.1128/AAC.00917-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lubna M, Shamsi K, Abid A, Khan A. Significant role of Asn-247 and Arg-64 residues in close proximity of the active site in maintaining the catalytic function of CTX-M-15 type β-lactamase. RSC Adv. 2019;9(10):5325–5337. doi: 10.1039/C8RA10313E [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ogbolu DO, Alli OAT, Webber MA, Oluremi AS, Oloyede OM. CTX-M-15 is established in most multidrug-resistant uropathogenic Enterobacteriaceae and Pseudomonaceae from hospitals in Nigeria. Eur J Microbiol Immunol. 2018;8(1):20–24. doi: 10.1556/1886.2017.00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hassen B, Abbassi MS, Benlabidi S, et al. Genetic characterization of ESBL-producing Escherichia coli and Klebsiella pneumoniae isolated from wastewater and river water in Tunisia: predominance of CTX-M-15 and high genetic diversity. Environ Sci Pollut Res. 2020;27(35):44368–44377. doi: 10.1007/s11356-020-10326-w [DOI] [PubMed] [Google Scholar]
- 82.Louka C, Ravensbergen SJ, Ott A, et al. Predominance of CTX-M-15-producing ST131 strains among ESBL-producing Escherichia coli isolated from asylum seekers in the Netherlands. J Antimicrob Chemother. 2021;76(1):70–76. doi: 10.1093/jac/dkaa395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bonnet R, Sampaio JLM, Labia R, et al. A novel CTX-M β-lactamase (CTX-M-8) in cefotaxime-resistant Enterobacteriaceae isolated in Brazil. Antimicrob Agents Chemother. 2000;44(7):1936–1942. doi: 10.1128/AAC.44.7.1936-1942.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hassen B, Saloua B, Abbassi MS, et al. mcr-1 encoding colistin resistance in CTX-M-1/CTX-M-15- producing Escherichia coli isolates of bovine and caprine origins in Tunisia. First report of CTX-M-15-ST394/D E. coli from goats. Comp Immunol Microbiol Infect Dis. 2019;67:101366. doi: 10.1016/j.cimid.2019.101366 [DOI] [PubMed] [Google Scholar]
- 85.Fournier C, Aires S, Nordmann P, Poirel L. Occurrence of CTX-M-15- and MCR-1-producing Enterobacterales in pigs in Portugal: evidence of direct links with antibiotic selective pressure. Int J Antimicrob Agents. 2020;55(2):105802. doi: 10.1016/j.ijantimicag.2019.09.006 [DOI] [PubMed] [Google Scholar]
- 86.Isgren CM, Edwards T, Pinchbeck GL, et al. Emergence of carriage of CTX-M-15 in faecal Escherichia coli in horses at an equine hospital in the UK; increasing prevalence over a decade (2008–2017). BMC Vet Res. 2019;15(1):1–8. doi: 10.1186/s12917-019-2011-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Irrgang A, Falgenhauer L, Fischer J, et al. CTX-M-15-producing E. coli isolates from food products in Germany are mainly associated with an IncF-type plasmid and belong to two predominant clonal E. coli lineages. Front Microbiol. 2017;8:2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kaesbohrer A, Bakran-Lebl K, Irrgang A, et al. Diversity in prevalence and characteristics of ESBL/pAmpC producing E. coli in food in Germany. Vet Microbiol. 2019;233:52–60. doi: 10.1016/j.vetmic.2019.03.025 [DOI] [PubMed] [Google Scholar]
- 89.Schill F, Abdulmawjood A, Klein G, Reich F. Prevalence and characterization of extended-spectrum β-lactamase (ESBL) and AmpC β-lactamase producing Enterobacteriaceae in fresh pork meat at processing level in Germany. Int J Food Microbiol. 2017;257:58–66. doi: 10.1016/j.ijfoodmicro.2017.06.010 [DOI] [PubMed] [Google Scholar]
- 90.Yaici L, Haenni M, Métayer V, et al. Spread of ESBL/AmpC-producing Escherichia coli and Klebsiella pneumoniae in the healthy carriers through ready-to-eat sandwiches in Algeria. Int J Food Microbiol. 2017;245:66–72. doi: 10.1016/j.ijfoodmicro.2017.01.011 [DOI] [PubMed] [Google Scholar]
- 91.Adelowo OO, Caucci S, Banjo OA, et al. Extended Spectrum Beta-Lactamase (ESBL)-producing bacteria isolated from hospital wastewaters, rivers and aquaculture sources in Nigeria. Environ Sci Pollut Res. 2017;25(3):2744–2755. doi: 10.1007/s11356-017-0686-7 [DOI] [PubMed] [Google Scholar]
- 92.Daoud Z, Farah J, Sokhn S, et al. Multidrug-resistant Enterobacteriaceae in Lebanese hospital wastewater: implication in the one health concept. Microb Drug Resist. 2018;24(2):166–174. doi: 10.1089/mdr.2017.0090 [DOI] [PubMed] [Google Scholar]
- 93.Lien LTQ, Lan PT, Chuc NTK, et al. Antibiotic resistance and antibiotic resistance genes in Escherichia coli isolates from hospital wastewater in Vietnam. Int J Environ Res Public Health. 2017;14(7):699. doi: 10.3390/ijerph14070699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lamba M, Graham DW, Ahammad SZ. Hospital wastewater releases of carbapenem-resistance pathogens and genes in Urban India. Environ Sci Technol. 2017;51(23):13906–13912. doi: 10.1021/acs.est.7b03380 [DOI] [PubMed] [Google Scholar]
- 95.Dinatale A. Prevalence of Plasmid Genetic Elements Among ESBL-Producing E. coli Isolated from a UK River and the Effects of Waste Water Effluent Release [dissertation]. UK: University of Lincoln; 2017. [Google Scholar]
- 96.Baniga Z, Hounmanou YMG, Kudirkiene E, Kusiluka LJM, Mdegela RH, Dalsgaard A. Genome-based analysis of extended-spectrum β-lactamase-producing Escherichia coli in the aquatic environment and Nile Perch (Lates niloticus) of Lake Victoria, Tanzania. Front Microbiol. 2020;11:108. doi: 10.3389/fmicb.2020.00108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Calderón V, Bonnelly R, Del Rosario C, et al. Distribution of beta-lactamase producing gram-negative bacterial isolates in isabela river of Santo Domingo, Dominican Republic. Front Microbiol. 2021;11. doi: 10.3389/fmicb.2020.519169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mattila S, Ruotsalainen P, Ojala V, Tuononen T, Hiltunen T, Jalasvuori M. Conjugative ESBL plasmids differ in their potential to rescue susceptible bacteria via horizontal gene transfer in lethal antibiotic concentrations. J Antibiot. 2017;70(6):805–808. doi: 10.1038/ja.2017.41 [DOI] [PubMed] [Google Scholar]
- 99.Cortés G, Kim J, Mira P, Mota L, Barlow M, Camps M. Conjugative transfer of ESBL and aminoglycoside antibiotic resistance genes in Extraintestinal E. coli: implications for multidrug resistance evolution: in proceedings of the 1st International Electronic Conference on Antibiotics—the equal power of antibiotics and antimicrobial resistance. Sci Forum. 2021;2021:9747. [Google Scholar]
- 100.Urano N, Okai M, Tashiro Y, et al. Behavior of antibiotic-resistant fecal coliforms in the stream of a sewage treatment plant in Tokyo. Adv Microbiol. 2020;10(7):318–330. doi: 10.4236/aim.2020.107023 [DOI] [Google Scholar]
- 101.Galler H, Feierl G, Petternel C, et al. Multiresistant bacteria isolated from activated sludge in Austria. Int J Environ Res Public Health. 2018;15(3):479. doi: 10.3390/ijerph15030479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ali A, Sultan I, Mondal AH, Siddiqui MT, Gogry FA, Haq QMR. Lentic and effluent water of Delhi-NCR: a reservoir of multidrug-resistant bacteria harbouring blaCTX-M, blaTEM and blaSHV type ESBL genes. J Water Health. 2021;19(4):592–603. doi: 10.2166/wh.2021.085 [DOI] [PubMed] [Google Scholar]
- 103.Peirano G, Richardson D, Nigrin J, et al. High prevalence of ST131 isolates producing CTX-M-15 and CTX-M-14 among extended-spectrum-β-lactamase-producing Escherichia coli isolates from Canada. Antimicrob Agents Chemother. 2010;54(3):1327–1330. doi: 10.1128/AAC.01338-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jouini A, Klibi A, Elarbi I, et al. First detection of human ST131-CTX-M-15-O25-B2 clone and high-risk clonal lineages of ESBL/pAmpC-producing E. coli isolates from diarrheic poultry in Tunisia. Antibiot. 2021;10(6):670. doi: 10.3390/antibiotics10060670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ehlkes L, Pfeifer Y, Werner G, et al. No evidence of carbapenemase-producing Enterobacteriaceae in stool samples of 1544 asylum seekers arriving in Rhineland-Palatinate, Germany, April 2016 to March 2017. Eurosurveillance. 2019;24(8):1800030. doi: 10.2807/1560-7917.ES.2019.24.8.1800030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Woerther PL, Angebault C, Jacquier H, et al. Characterization of fecal extended-spectrum-β-lactamase-producing Escherichia coli in a remote healthy carriers during a long time period. Antimicrob Agents Chemother. 2013;57(10):5060–5066. doi: 10.1128/AAC.00848-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Daga AP, Koga VL, Soncini JGM, et al. Escherichia coli bloodstream infections in patients at a university hospital: virulence factors and clinical characteristics. Front Cell Infect Microbiol. 2019;9:191. doi: 10.3389/fcimb.2019.00191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Palmeira JD, Haenni M, Metayer V, Madec JY, Ferreira HMN. Epidemic spread of IncI1/pST113 plasmid carrying the Extended-Spectrum Beta-Lactamase (ESBL) blaCTX-M-8 gene in Escherichia coli of Brazilian cattle. Vet Microbiol. 2020;243:108629. doi: 10.1016/j.vetmic.2020.108629 [DOI] [PubMed] [Google Scholar]
- 109.Ortega-Paredes D, Haro M, Leoro-Garzón P, et al. Multidrug-resistant Escherichia coli isolated from canine faeces in a public park in Quito, Ecuador. J Glob Antimicrob Resist. 2019;18:263–268. doi: 10.1016/j.jgar.2019.04.002 [DOI] [PubMed] [Google Scholar]
- 110.Faccone D, Moredo FA, Giacoboni GI, et al. Multidrug-resistant Escherichia coli harbouring mcr-1 and blaCTX-M genes isolated from swine in Argentina. J Glob Antimicrob Resist. 2019;18:160–162. doi: 10.1016/j.jgar.2019.03.011 [DOI] [PubMed] [Google Scholar]
- 111.Vinueza-Burgos C, Ortega-Paredes D, Narváez C, De Zutter L, Zurita J. Characterization of cefotaxime resistant Escherichia coli isolated from broiler farms in Ecuador. PLoS One. 2019;14(4):e0207567. doi: 10.1371/journal.pone.0207567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cunha MPV, Oliveira MCV, Oliveira MGX, Menão MC, Knöbl T. CTX-M-producing Escherichia coli Isolated from urban pigeons (Columba livia domestica) in Brazil. J Infect Dev Ctries. 2019;13:1052–1056. doi: 10.3855/jidc.11441 [DOI] [PubMed] [Google Scholar]
- 113.Aristizábal-Hoyos AM, Rodríguez EA, Arias L, Jiménez JN. High clonal diversity of multidrug-resistant and extended spectrum beta-lactamase-producing Escherichia coli in a wastewater treatment plant. J Environ Manage. 2019;245:37–47. doi: 10.1016/j.jenvman.2019.05.073 [DOI] [PubMed] [Google Scholar]
- 114.Rumi MV, Mas J, Elena A, et al. Co-occurrence of clinically relevant β-lactamases and MCR-1 encoding genes in Escherichia coli from companion animals in Argentina. Vet Microbiol. 2019;230:228–234. doi: 10.1016/j.vetmic.2019.02.006 [DOI] [PubMed] [Google Scholar]
- 115.Hoepers PG, Silva PL, Rossi DA, et al. The association between extended spectrum beta-lactamase (ESBL) and ampicillin C (AmpC) beta-lactamase genes with multidrug resistance in Escherichia coli isolates recovered from turkeys in Brazil. Br Poult Sci. 2018;59(4):396–401. doi: 10.1080/00071668.2018.1468070 [DOI] [PubMed] [Google Scholar]
- 116.Chavez MV, Caicedo LD, Castillo JE. Occurrence of β-lactamase-producing gram-negative bacterial isolates in water sources in Cali City, Colombia. Int J Microbiol. 2019;2019:1375060. doi: 10.1155/2019/1375060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.De carvalho MPN, Fernandes MR, Sellera FP, et al. International clones of extended-spectrum β-lactamase (CTX-M)-producing Escherichia coli in peri-urban wild animals, Brazil. Transbound Emerg Dis. 2020;67(5):1804–1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Benavides JA, Shiva C, Virhuez M, et al. Extended-spectrum beta-lactamase-producing Escherichia coli in common vampire bats Desmodus rotundus and livestock in Peru. Zoonoses Public Health. 2018;65(4):454–458. doi: 10.1111/zph.12456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Guzmán M, Salazar E, Cordero V, et al. Multirresistencia a medicamentos y factores de riesgo asociados con infecciones urinarias por Escherichia coli adquiridas en la comunidad, Venezuela [Multidrug resistance and risk factors associated with healthy carriers-acquired urinary tract infections caused by Escherichia coli in Venezuela]. Biomedica. 2019;39(Suppl1):S96–S107. Spanish. [DOI] [PubMed] [Google Scholar]
- 120.Zurita J, Solís MB, Ortega-Paredes D, et al. High prevalence of B2-ST131 clonal group among extended-spectrum β-lactamase-producing Escherichia coli isolated from bloodstream infections in Quito, Ecuador. J Glob Antimicrob Resist. 2019;19:216–221. doi: 10.1016/j.jgar.2019.04.019 [DOI] [PubMed] [Google Scholar]
- 121.Sfaciotte RAP, Parussolo L, Melo FD, et al. Identification and characterization of multidrug-resistant extended-spectrum beta-lactamase-producing bacteria from healthy and diseased dogs and cats admitted to a veterinary hospital in Brazil. Microb Drug Resist. 2021;27(6):855–864. doi: 10.1089/mdr.2020.0043 [DOI] [PubMed] [Google Scholar]
- 122.Crecencio RB, Brisola MC, Bitner D, et al. Antimicrobial susceptibility, biofilm formation and genetic profiles of Escherichia coli isolated from retail chicken meat. Infect Genet Evol. 2020;84:104355. doi: 10.1016/j.meegid.2020.104355 [DOI] [PubMed] [Google Scholar]
- 123.Fernandes MR, Sellera FP, Moura Q, Esposito F, Sabino CP, Lincopan N. Identification and genomic features of halotolerant extended-spectrum-β-lactamase (CTX-M)-producing Escherichia coli in urban-impacted coastal waters, Southeast Brazil. Mar Pollut Bull. 2020;150:110689. doi: 10.1016/j.marpolbul.2019.110689 [DOI] [PubMed] [Google Scholar]
- 124.Freitas DY, Araújo S, Folador ARC, et al. Extended spectrum beta-lactamase-producing gram-negative bacteria recovered from an Amazonian lake near the City of Belém, Brazil. Front Microbiol. 2019;10:364. doi: 10.3389/fmicb.2019.00364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Fuentes-Castillo D, Farfán-López M, Esposito F, et al. Wild owls colonized by international clones of extended-spectrum β-lactamase (CTX-M)-producing Escherichia coli and Salmonella infantis in the Southern Cone of America. Sci Total Environ. 2019;674:554–562. doi: 10.1016/j.scitotenv.2019.04.149 [DOI] [PubMed] [Google Scholar]
- 126.Larson A, Hartinger SM, Riveros M, et al. Antibiotic-resistant Escherichia coli in drinking water samples from rural Andean households in Cajamarca, Peru. Am J Trop Med Hyg. 2019;100(6):1363–1368. doi: 10.4269/ajtmh.18-0776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Batalha de Jesus AA, Freitas AAR, de Souza JC, et al. High-level multidrug-resistant Escherichia coli isolates from wild birds in a large urban environment. Microb Drug Resist. 2019;25(2):167–172. doi: 10.1089/mdr.2018.0180 [DOI] [PubMed] [Google Scholar]
- 128.Lentz SAM, Adam FC, Rivas PM, et al. High levels of resistance to cephalosporins associated with the presence of extended-spectrum and AmpC β-lactamases in Escherichia coli from broilers in Southern Brazil. Microb Drug Resist. 2020;26(5):531–535. doi: 10.1089/mdr.2019.0050 [DOI] [PubMed] [Google Scholar]
- 129.Zurita J, Yánez F, Sevillano G, Ortega-Paredes D, Paz Y, Miño A. Ready-to-eat street food: a potential source for dissemination of multidrug-resistant Escherichia coli epidemic clones in Quito, Ecuador. Lett Appl Microbiol. 2020;70(3):203–209. doi: 10.1111/lam.13263 [DOI] [PubMed] [Google Scholar]
- 130.Miranda J, Pinto J, Faustino M, Sánchez-Jacinto B, Ramirez F. Resistencia antimicrobiana de uropatógenos en adultos mayores de una clínica privada de Lima, Perú [Antimicrobial resistance of uropathogens in older adults in a private clinic in Lima, Peru]. Rev Peru Med Exp Salud Publica. 2019;36(1):87–92. Spanish. doi: 10.17843/rpmesp.2019.361.3765 [DOI] [PubMed] [Google Scholar]
- 131.Ortega-Paredes D, Barba P, Mena-López S, Espinel N, Zurita J. Escherichia coli hyperepidemic clone ST410-A harboring blaCTX-M-15 isolated from fresh vegetables in a municipal market in Quito-Ecuador. Int J Food Microbiol. 2018;280:41–45. doi: 10.1016/j.ijfoodmicro.2018.04.037 [DOI] [PubMed] [Google Scholar]
- 132.Pavez M, Troncoso C, Osses I, et al. High prevalence of CTX-M-1 group in ESBL-producing Enterobacteriaceae infection in intensive care units in southern Chile. Braz J Infect Dis. 2019;23(2):102–110. doi: 10.1016/j.bjid.2019.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Umpiérrez A, Bado I, Oliver M, et al. Zoonotic potential and antibiotic resistance of Escherichia coli in neonatal calves in Uruguay. Microbes Environ. 2017;32(3):275–282. doi: 10.1264/jsme2.ME17046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Coppola N, Freire B, Umpiérrez A, et al. Transferable resistance to highest priority critically important antibiotics for human health in Escherichia coli strains obtained from livestock feces in Uruguay. Front Vet Sci. 2020;7:588919. doi: 10.3389/fvets.2020.588919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cyoia PS, Koga VL, Nishio EK, et al. Distribution of ExPEC virulence factors, blaCTX-M, fosA3, and mcr-1 in Escherichia coli isolated from commercialized chicken carcasses. Front Microbiol. 2019;9:3254. doi: 10.3389/fmicb.2018.03254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Nogueira S, Conte D, Maia FV, Dalla-Costa LM. Distribution of extended-spectrum β-lactamase types in a Brazilian tertiary hospital. Rev Soc Bras Med Trop. 2015;48(2):162–169. doi: 10.1590/0037-8682-0009-2015 [DOI] [PubMed] [Google Scholar]
- 137.Bartley PS, Domitrovic TN, Moretto VT, et al. Antibiotic resistance in Enterobacteriaceae from surface waters in Urban Brazil highlights the risks of poor sanitation. Am J Trop Med Hyg. 2019;100(6):1369–1377. doi: 10.4269/ajtmh.18-0726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Araque M, Labrador I. Prevalence of fecal carriage of CTX-M-15 beta-lactamase-producing Escherichia coli in healthy children from a Rural Andean Village in Venezuela. Osong Public Health Res Perspect. 2018;9(1):9–15. doi: 10.24171/j.phrp.2018.9.1.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Pereira JL, Volcão LM, Klafke GB, et al. Antimicrobial resistance and molecular characterization of extended-spectrum β-lactamases of Escherichia coli and Klebsiella spp. isolates from urinary tract infections in Southern Brazil. Microb Drug Resist. 2019;25(2):173–181. doi: 10.1089/mdr.2018.0046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Palma N, Pons MJ, Gomes C, et al. Resistance to quinolones, cephalosporins and macrolides in Escherichia coli causing bacteraemia in Peruvian children. J Glob Antimicrob Resist. 2017;11:28–33. doi: 10.1016/j.jgar.2017.06.011 [DOI] [PubMed] [Google Scholar]
- 141.Botelho LAB, Kraychete GB, Rocha PB, et al. CTX-M- and pAmpC-encoding genes are associated with similar mobile genetic elements in Escherichia coli isolated from different brands of Brazilian chicken meat. Microb Drug Resist. 2020;26(1):14–20. doi: 10.1089/mdr.2019.0043 [DOI] [PubMed] [Google Scholar]
- 142.Faccone D, Rapoport M, Albornoz E, et al. Plasmidic resistance to colistin mediated by mcr-1 gene in Escherichia coli clinical isolates in Argentina: a retrospective study, 2012–2018. Rev Panam Salud Publica. 2020;44:e55. doi: 10.26633/RPSP.2020.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Beirão EM, Rodrigues SDS, Andrade TK, et al. Activity of ceftolozane-tazobactam and comparators against gram-negative bacilli: results from the study for monitoring antimicrobial resistance trends (SMART - Brazil; 2016–2017). Braz J Infect Dis. 2020;24(4):310–321. doi: 10.1016/j.bjid.2020.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Villar HE, Aubert V, Baserni MN, Jugo MB. Maternal carriage of extended-spectrum beta-lactamase-producing Escherichia coli isolates in Argentina. J Chemother. 2013;25(6):324–327. doi: 10.1179/1973947813Y.0000000081 [DOI] [PubMed] [Google Scholar]
- 145.Colquechagua-Aliaga F, Sevilla-Andrade C, Gonzales-Escalante E. Enterobacterias productoras de betalactamasas de espectro extendido en muestras fecales en el Instituto Nacional de Salud del Niño, Perú [Extended-spectrum beta-lactamase (esbl)-producing Enterobacteriaceae in fecal samples at the National Institute of Child Health, Peru]. Rev Peru Med Exp Salud Publica. 2015;32(1):26–32. Spanish. [PubMed] [Google Scholar]
- 146.Chiluisa-Guacho C, Escobar-Perez J, Dutra-Asensi M. First detection of the CTXM-15 producing Escherichia coli O25-ST131 pandemic clone in Ecuador. Pathogens. 2018;7(2):42. doi: 10.3390/pathogens7020042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Palma N, Gomes C, Riveros M, et al. Virulence factors profiles and ESBL production in Escherichia coli causing bacteremia in Peruvian children. Diagn Microbiol Infect Dis. 2016;86(1):70–75. doi: 10.1016/j.diagmicrobio.2016.05.017 [DOI] [PubMed] [Google Scholar]
- 148.Sarmiento AF, Mejia MN, Rozas AB, Giraldo CA, Málaga G. Frecuencia y factores de riesgo para bacteriemia por enterobacterias productoras de betalactamasa de espectro extendido en pacientes de un hospital público de Lima, Perú [Frequency and risk factors for bacteremia caused by extended spectrum beta-lactamase-producing Enterobacteriaceae in patients of a public hospital in Lima, Peru]. Rev Peru Med Exp Salud Publica. 2018;35(1):62–67. Spanish. doi: 10.17843/rpmesp.2018.351.3601 [DOI] [PubMed] [Google Scholar]
- 149.Blanco VM, Maya JJ, Correa A, et al. Prevalencia y factores de riesgo para infecciones del tracto urinario de inicio en la comunidad causadas por Escherichia coli productor de betalactamasas de espectro extendido en Colombia [Prevalence and risk factors for extended-spectrum β-lactamase-producing Escherichia coli causing healthy carriers-onset urinary tract infections in Colombia]. Enferm Infecc Microbiol Clin. 2016;34(9):559–565. Spanish. doi: 10.1016/j.eimc.2015.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Chagas TP, Seki LM, Cury JC, et al. Multiresistance, beta-lactamase-encoding genes and bacterial diversity in hospital wastewater in Rio de Janeiro, Brazil. J Appl Microbiol. 2011;111(3):572–581. doi: 10.1111/j.1365-2672.2011.05072.x [DOI] [PubMed] [Google Scholar]
- 151.Vignoli R, García-Fulgueiras V, Cordeiro NF, et al. Extended-spectrum β-lactamases, transferable quinolone resistance, and virulotyping in extra-intestinal E. coli in Uruguay. J Infect Dev Ctries. 2016;10(1):43–52. doi: 10.3855/jidc.6918 [DOI] [PubMed] [Google Scholar]
- 152.Campos ACC, Andrade NL, Ferdous M, et al. Corrigendum: comprehensive molecular characterization of Escherichia coli isolates from urine samples of hospitalized patients in Rio de Janeiro, Brazil. Front Microbiol. 2020;11:599031. doi: 10.3389/fmicb.2020.599031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Gonçalves LF, De oliveira P, de Melo ABF, et al. Multidrug resistance dissemination by extended-spectrum β-lactamase-producing Escherichia coli causing healthy carriers-acquired urinary tract infection in the Central-Western Region, Brazil. J Glob Antimicrob Resist. 2016;6:1–4. doi: 10.1016/j.jgar.2016.02.003 [DOI] [PubMed] [Google Scholar]
- 154.Martinez P, Garzón D, Mattar S. CTX-M-producing Escherichia coli and Klebsiella pneumoniae isolated from healthy carriers-acquired urinary tract infections in Valledupar, Colombia. Braz J Infect Dis. 2012;16(5):420–425. doi: 10.1016/j.bjid.2012.05.001 [DOI] [PubMed] [Google Scholar]
- 155.Peirano G, Asensi MD, Pitondo-Silva A, Pitout JD. Molecular characteristics of extended-spectrum β-lactamase-producing Escherichia coli from Rio de Janeiro, Brazil. Clin Microbiol Infect. 2011;17(7):1039–1043. doi: 10.1111/j.1469-0691.2010.03440.x [DOI] [PubMed] [Google Scholar]
- 156.Andrade LN, Minarini LA, Pitondo-Silva A, et al. Determinants of beta-lactam resistance in meningitis-causing Enterobacteriaceae in Brazil. Can J Microbiol. 2010;56(5):399–407. doi: 10.1139/W10-020 [DOI] [PubMed] [Google Scholar]
- 157.Abreu AG, Marques SG, Monteiro-Neto V, Carvalho RM, Gonçalves AG. Infecção hospitalar e caracterização de Enterobactérias produtoras de β-lactamases de espectro ampliado no Nordeste do Brasil [Nosocomial infection and characterization of extended-spectrum β-lactamases-producing Enterobacteriaceae in Northeast Brazil]. Rev Soc Bras Med Trop. 2011;44(4):441–446. Portuguese. doi: 10.1590/S0037-86822011000400008 [DOI] [PubMed] [Google Scholar]
- 158.Villar HE, Baserni MN, Jugo MB. Faecal carriage of ESBL-producing Enterobacteriaceae and carbapenem-resistant Gram-negative bacilli in healthy carriers settings. J Infect Dev Ctries. 2013;7(8):630–634. doi: 10.3855/jidc.2900 [DOI] [PubMed] [Google Scholar]
- 159.Garrido D, Garrido S, Gutiérrez M, et al. Clinical characterization and antimicrobial resistance of Escherichia coli in pediatric patients with urinary tract infection at a third level hospital of Quito, Ecuador. Bol Med Hosp Infant Mex. 2017;74(4):265–271. doi: 10.1016/j.bmhimx.2017.02.004 [DOI] [PubMed] [Google Scholar]
- 160.Koga VL, Rodrigues GR, Scandorieiro S, et al. Evaluation of the antibiotic resistance and virulence of Escherichia coli strains isolated from chicken carcasses in 2007 and 2013 from Paraná, Brazil. Foodborne Pathog Dis. 2015;12(6):479–485. doi: 10.1089/fpd.2014.1888 [DOI] [PubMed] [Google Scholar]
- 161.Wollheim C, Guerra IM, Conte VD, et al. Nosocomial and healthy carriers infections due to class A extended-spectrum β-lactamase (ESBLA)-producing Escherichia coli and Klebsiella spp. in southern Brazil. Braz J Infect Dis. 2011;15(2):138–143. [PubMed] [Google Scholar]
- 162.Borges CA, Maluta RP, Beraldo LG, et al. Captive and free-living urban pigeons (Columba livia) from Brazil as carriers of multidrug-resistant pathogenic Escherichia coli. Vet J. 2017;219:65–67. doi: 10.1016/j.tvjl.2016.12.015 [DOI] [PubMed] [Google Scholar]
- 163.Soria-Segarra C, Soria-Baquero E, Cartelle-Gestal M. High prevalence of CTX-M-1-like enzymes in urinary isolates of Escherichia coli in Guayaquil, Ecuador. Microb Drug Resist. 2018;24(4):393–402. doi: 10.1089/mdr.2017.0325 [DOI] [PubMed] [Google Scholar]
- 164.Viana ALM, Cayô R, Avelino CC, Gales AC, Franco MC, Minarini LAR. Extended-spectrum β-lactamases in Enterobacteriaceae isolated in Brazil carry distinct types of plasmid-mediated quinolone resistance genes. J Med Microbiol. 2013;62(Pt 9):1326–1331. doi: 10.1099/jmm.0.055970-0 [DOI] [PubMed] [Google Scholar]
- 165.Bado I, Gutiérrez C, García-Fulgueiras V, et al. CTX-M-15 in combination with aac(6’)-Ib-cr is the most prevalent mechanism of resistance both in Escherichia coli and Klebsiella pneumoniae, including K. pneumoniae ST258, in an ICU in Uruguay. J Glob Antimicrob Resist. 2016;6:5–9. doi: 10.1016/j.jgar.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 166.Botelho LA, Kraychete GB, Costa JL, et al. Widespread distribution of CTX-M and plasmid-mediated AmpC β-lactamases in Escherichia coli from Brazilian chicken meat. Mem Inst Oswaldo Cruz. 2015;110(2):249–254. doi: 10.1590/0074-02760140389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Dropa M, Lincopan N, Balsalobre LC, et al. Genetic background of novel sequence types of CTX-M-8- and CTX-M-15-producing Escherichia coli and Klebsiella pneumoniae from public wastewater treatment plants in São Paulo, Brazil. Environ Sci Pollut Res Int. 2016;23(5):4953–4958. doi: 10.1007/s11356-016-6079-5 [DOI] [PubMed] [Google Scholar]
- 168.García-Fulgueiras V, Bado I, Mota MI, et al. Extended-spectrum β-lactamases and plasmid-mediated quinolone resistance in enterobacterial clinical isolates in the paediatric hospital of Uruguay. J Antimicrob Chemother. 2011;66(8):1725–1729. doi: 10.1093/jac/dkr222 [DOI] [PubMed] [Google Scholar]
- 169.Pallecchi L, Malossi M, Mantella A, et al. Detection of CTX-M-type beta-lactamase genes in fecal Escherichia coli isolates from healthy children in Bolivia and Peru. Antimicrob Agents Chemother. 2004;48(12):4556–4561. doi: 10.1128/AAC.48.12.4556-4561.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Quijada-Martínez P, Flores-Carrero A, Labrador I, Araque M. Estudio clínico y microbiológico de la infección urinaria asociada a catéter, en los servicios de medicina interna de un hospital universitario venezolano [Clinical and microbiological study of catheter-associated urinary tract infections in internal medicine services of a Venezuelan university hospital]. Rev Peru Med Exp Salud Publica. 2017;34(1):52–61. Spanish. doi: 10.17843/rpmesp.2017.341.2766 [DOI] [PubMed] [Google Scholar]
- 171.Minarini LA, Gales AC, Palazzo IC, Darini AL. Prevalence of healthy carriers-occurring extended spectrum beta-lactamase-producing Enterobacteriaceae in Brazil. Curr Microbiol. 2007;54(5):335–341. doi: 10.1007/s00284-006-0307-z [DOI] [PubMed] [Google Scholar]
- 172.Sartori L, Fernandes MR, Ienne S, et al. Draft genome sequences of two fluoroquinolone-resistant CTX-M-15-producing Escherichia coli ST90 (ST23 complex) isolated from a calf and a dairy cow in South America. J Glob Antimicrob Resist. 2017;11:145–147. doi: 10.1016/j.jgar.2017.10.009 [DOI] [PubMed] [Google Scholar]
- 173.Marusinec R, Kurowski KM, Amato HK, et al. Caretaker knowledge, attitudes, and practices (KAP) and carriage of extended-spectrum beta-lactamase-producing E. coli (ESBL-EC) in children in Quito, Ecuador. Antimicrob Resist Infect Control. 2021;10(1):2. doi: 10.1186/s13756-020-00867-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Jones RN, Guzman-Blanco M, Gales AC, et al. Susceptibility rates in Latin American nations: report from a regional resistance surveillance program (2011). Braz J Infect Dis. 2013;17(6):672–681. doi: 10.1016/j.bjid.2013.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Adrianzén D, Arbizu A, Ortiz J, Samalvides F. Mortalidad por bacteriemia causada por Escherichia coli y Klebsiella spp. productoras de beta lactamasas de espectro extendido: cohorte retrospectiva en un hospital de Lima, Perú [Mortality caused by bacteremia Escherichia coli and Klebsiella spp. extended-spectrum beta-lactamase- producers: a retrospective cohort from a hospital in Lima, Peru]. Rev Peru Med Exp Salud Publica. 2013;30(1):18–25. Spanish. doi: 10.1590/s1726-46342013000100004 [DOI] [PubMed] [Google Scholar]
- 176.Tedesco-Maiullari RM, Guevara A. Enterobatteri produttori di beta-lattamasi a spettro esteso in un ospedale in Venezuela [Enterobacteria producers of extended-spectrum beta-lactamase in a hospital from Venezuela]. Infez Med. 2012;20(2):93–99. Italian. [PubMed] [Google Scholar]
- 177.Di Conza JA, Badaracco A, Ayala J, Rodríguez C, Famiglietti A, Gutkind GO. β-lactamases produced by amoxicillin-clavulanate-resistant enterobacteria isolated in Buenos Aires, Argentina: a new blaTEM gene. Rev Argent Microbiol. 2014;46(3):210–217. doi: 10.1016/S0325-7541(14)70075-6 [DOI] [PubMed] [Google Scholar]
- 178.Da Silva KC, Cunha MP, Cerdeira L, et al. High-virulence CMY-2- and CTX-M-2-producing avian pathogenic Escherichia coli strains isolated from commercial turkeys. Diagn Microbiol Infect Dis. 2017;87(1):64–67. doi: 10.1016/j.diagmicrobio.2016.10.001 [DOI] [PubMed] [Google Scholar]
- 179.Fernandes MR, Sellera FP, Moura Q, Gaspar VC, Cerdeira L, Lincopan N. International high-risk clonal lineages of CTX-M-producing Escherichia coli F-ST648 in free-roaming cats, South America. Infect Genet Evol. 2018;66:48–51. doi: 10.1016/j.meegid.2018.09.009 [DOI] [PubMed] [Google Scholar]
- 180.Da Silva-dias RC, Borges-Neto AA, D’Almeida-Ferraiuoli GI, De-oliveira MP, Riley LW, Moreira BM. Prevalence of AmpC and other beta-lactamases in enterobacteria at a large urban university hospital in Brazil. Diagn Microbiol Infect Dis. 2008;60(1):79–87. doi: 10.1016/j.diagmicrobio.2007.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ferreira JC, Penha Filho RA, Andrade LN, Berchieri A, Darini AL. Detection of chromosomal bla(CTX-M-2) in diverse Escherichia coli isolates from healthy broiler chickens. Clin Microbiol Infect. 2014;20(10):623–626. doi: 10.1111/1469-0691.12531 [DOI] [PubMed] [Google Scholar]
- 182.Quiles MG, Menezes LC, Bauab C, et al. Diagnosis of bacteremia in pediatric oncologic patients by in-house real-time PCR. BMC Infect Dis. 2015;15:283. doi: 10.1186/s12879-015-1033-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Dias RCB, Vieira MA, Moro AC, et al. Characterization of Escherichia coli obtained from patients undergoing peritoneal dialysis and diagnosed with peritonitis in a Brazilian centre. J Med Microbiol. 2019;68(9):1330–1340. doi: 10.1099/jmm.0.001043 [DOI] [PubMed] [Google Scholar]
- 184.Ferreira CM, Ferreira WA, Almeida NC, Naveca FG, Barbosa M. Extended-spectrum beta-lactamase-producing bacteria isolated from hematologic patients in Manaus, State of Amazonas, Brazil. Braz J Microbiol. 2011;42(3):1076–1084. doi: 10.1590/S1517-83822011000300028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Rugini CL, Sobottka AM, Fuentefria DB. Occurrence and sensitivity profile of extended spectrum beta-lactamase-producing Enterobacteriaceae at a tertiary hospital in Southern Brazil. Rev Soc Bras Med Trop. 2015;48(6):692–698. doi: 10.1590/0037-8682-0211-2015 [DOI] [PubMed] [Google Scholar]
- 186.Oplustil CP, Nunes R, Mendes C; RESISTNET Group. Multicenter evaluation of resistance patterns of Klebsiella pneumoniae, Escherichia coli, Salmonella spp and Shigella spp isolated from clinical specimens in Brazil: RESISTNET Surveillance Program. Braz J Infect Dis. 2001;5(1):8–12. doi: 10.1590/S1413-86702001000100002 [DOI] [PubMed] [Google Scholar]
- 187.Tosin I, Silbert S, Sader HS. The use of molecular typing to evaluate the dissemination of antimicrobial resistance among Gram-negative rods in Brazilian hospitals. Braz J Infect Dis. 2003;7(6):360–369. doi: 10.1590/S1413-86702003000600002 [DOI] [PubMed] [Google Scholar]
- 188.Guevara N, Guzmán M, Merentes A, et al. Patrones de susceptibilidad antimicrobiana de bacterias gramnegativas aisladas de infecciones del tracto urinario en Venezuela: resultados del estudio SMART 2009-2012 [Antimicrobial susceptibility patterns of Gram-negative bacteria isolated in urinary tract infections in Venezuela: results of the SMART study 2009-2012]. Rev Chilena Infectol. 2015;32(6):639–648. Spanish. doi: 10.4067/S0716-10182015000700005 [DOI] [PubMed] [Google Scholar]
- 189.Casellas JM, Tomé G, Bantar C, et al. Argentinean collaborative multicenter study on the in vitro comparative activity of piperacillin-tazobactam against selected bacterial isolates recovered from hospitalized patients. Diagn Microbiol Infect Dis. 2003;47(3):527–537. doi: 10.1016/S0732-8893(03)00131-7 [DOI] [PubMed] [Google Scholar]
- 190.Motta RN, Oliveira MM, Magalhães PS, et al. Plasmid-mediated extended-spectrum beta-lactamase-producing strains of Enterobacteriaceae isolated from diabetes foot infections in a Brazilian diabetic center. Braz J Infect Dis. 2003;7(2):129–134. doi: 10.1590/S1413-86702003000200006 [DOI] [PubMed] [Google Scholar]
- 191.Rossi F, García P, Ronzon B, Curcio D, Dowzicky MJ. Rates of antimicrobial resistance in Latin America (2004-2007) and in vitro activity of the glycylcycline tigecycline and of other antibiotics. Braz J Infect Dis. 2008;12(5):405–415. doi: 10.1590/S1413-86702008000500012 [DOI] [PubMed] [Google Scholar]
- 192.Casella T, Rodríguez MM, Takahashi JT, et al. Detection of blaCTX-M-type genes in complex class 1 integrons carried by Enterobacteriaceae isolated from retail chicken meat in Brazil. Int J Food Microbiol. 2015;197:88–91. doi: 10.1016/j.ijfoodmicro.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 193.De Oliveira CF, Salla A, Lara VM, Rieger A, Horta JA, Alves SH. Prevalence of extended-spectrum beta-lactamases-producing microorganisms in nosocomial patients and molecular characterization of the SHV-type isolates. Braz J Microbiol. 2010;41(2):278–282. doi: 10.1590/S1517-83822010000200002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Seki LM, Pereira PS, de Souza-conceição M, et al. Molecular epidemiology of CTX-M producing Enterobacteriaceae isolated from bloodstream infections in Rio de Janeiro, Brazil: emergence of CTX-M-15. Braz J Infect Dis. 2013;17(6):640–646. doi: 10.1016/j.bjid.2013.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Salgado-Caxito M, Benavides JA, Munita JM, et al. Risk factors associated with faecal carriage of extended-spectrum cephalosporin-resistant Escherichia coli among dogs in Southeast Brazil. Prev Vet Med. 2021;190:105316. doi: 10.1016/j.prevetmed.2021.105316 [DOI] [PubMed] [Google Scholar]
- 196.Vignoli R, Varela G, Mota MI, et al. Enteropathogenic Escherichia coli strains carrying genes encoding the PER-2 and TEM-116 extended-spectrum beta-lactamases isolated from children with diarrhea in Uruguay. J Clin Microbiol. 2005;43(6):2940–2943. doi: 10.1128/JCM.43.6.2940-2943.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Hernández E, Araque M, Millán Y, Millán B, Vielma S. Prevalencia de beta-lactamasa CTX-M-15 en grupos filogenéticos de Escherichia coli uropatógena aisladas en pacientes de la comunidad en Mérida, Venezuela [Prevalence of beta-lactamase CTX-M-15 in phylogenetic groups of uropathogenic Escherichia coli isolated from patients in the healthy carriers of Merida, Venezuela]. Invest Clin. 2014;55(1):32–43. Spanish. [PubMed] [Google Scholar]
- 198.Saba-Villarroel PM, Gutkind GO, Di Conza JA, Radice MA. First survey on antibiotic resistance markers in Enterobacteriaceae in Cochabamba, Bolivia. Rev Argent Microbiol. 2017;49(1):50–54. doi: 10.1016/j.ram.2016.10.002 [DOI] [PubMed] [Google Scholar]
- 199.Lago A, Fuentefria SR, Fuentefria DB. Enterobactérias produtoras de ESBL em Passo Fundo, estado do Rio Grande do Sul, Brasil [ESBL-producing enterobacteria in Passo Fundo, state of Rio Grande do Sul, Brazil]. Rev Soc Bras Med Trop. 2010;43(4):430–434. Portuguese. doi: 10.1590/S0037-86822010000400019 [DOI] [PubMed] [Google Scholar]
- 200.Marchetti L, Buldain D, Gortari-Castillo L, Buchamer A, Chirino-Trejo M, Mestorino N. Pet and stray dogs as reservoirs of antimicrobial-resistant Escherichia coli. Int J Microbiol. 2021;2021:6664557. doi: 10.1155/2021/6664557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Wozniak A, Villagra NA, Undabarrena A, et al. Porin alterations present in non-carbapenemase-producing Enterobacteriaceae with high and intermediate levels of carbapenem resistance in Chile. J Med Microbiol. 2012;61(Pt 9):1270–1279. doi: 10.1099/jmm.0.045799-0 [DOI] [PubMed] [Google Scholar]
- 202.Queiroz ML, Antunes P, Mourão J, Merquior VL, Machado E, Peixe LV. Characterization of extended-spectrum beta-lactamases, antimicrobial resistance genes, and plasmid content in Escherichia coli isolates from different sources in Rio de Janeiro, Brazil. Diagn Microbiol Infect Dis. 2012;74(1):91–94. doi: 10.1016/j.diagmicrobio.2012.05.019 [DOI] [PubMed] [Google Scholar]
- 203.Salinas L, Loayza F, Cárdenas P, et al. Environmental spread of Extended Spectrum Beta-Lactamase (ESBL) producing Escherichia coli and ESBL genes among children and domestic animals in Ecuador. Environ Health Perspect. 2021;129(2):27007. doi: 10.1289/EHP7729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Bartoloni A, Sennati S, Di Maggio T, et al. Antimicrobial susceptibility and emerging resistance determinants (blaCTX-M, rmtB, fosA3) in clinical isolates from urinary tract infections in the Bolivian Chaco. Int J Infect Dis. 2016;43:1–6. doi: 10.1016/j.ijid.2015.12.008 [DOI] [PubMed] [Google Scholar]
- 205.Vasques MR, Bello AR, Lamas C, Correa J, Pereira JA. β-lactamase producing enterobacteria isolated from surveillance swabs of patients in a cardiac intensive care unit in Rio de Janeiro, Brazil. Braz J Infect Dis. 2011;15(1):28–33. [PubMed] [Google Scholar]
- 206.Mendo-Lopez R, Jasso L, Guevara X, et al. Multidrug-resistant microorganisms colonizing lower extremity wounds in patients in a tertiary care hospital, Lima, Peru. Am J Trop Med Hyg. 2017;97(4):1045–1048. doi: 10.4269/ajtmh.17-0235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Gaitán CSL, Espinal MPA. Caracterización molecular de Escherichia coli y Klebsiella pneumoniae productores de beta-lactamasas de espectro extendido en hospitales de la Región Caribe, Colombia [Molecular characterization of extended-spectrum beta-lactamases-producing Escherichia coli and Klebsiella pneumoniae in hospitals of the Caribean Region, Colombia]. Rev Chilena Infectol. 2009;26(3):239–246. Spanish. [PubMed] [Google Scholar]
- 208.Sennati S, Santella G, Di Conza J, et al. Changing epidemiology of extended-spectrum β-lactamases in Argentina: emergence of CTX-M-15. Antimicrob Agents Chemother. 2012;56(11):6003–6005. doi: 10.1128/AAC.00745-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Ferreira JC, Penha-Filho RA, Andrade LN, Berchieri Junior A, Darini AL. Evaluation and characterization of plasmids carrying CTX-M genes in a non-clonal population of multidrug-resistant Enterobacteriaceae isolated from poultry in Brazil. Diagn Microbiol Infect Dis. 2016;85(4):444–448. doi: 10.1016/j.diagmicrobio.2016.05.011 [DOI] [PubMed] [Google Scholar]
- 210.Abreu AG, Marques SG, Monteiro-Neto V, Gonçalves AG. Extended-spectrum β-lactamase-producing Enterobacteriaceae in healthy carriers-acquired urinary tract infections in São Luís, Brazil. Braz J Microbiol. 2013;44(2):469–471. doi: 10.1590/S1517-83822013005000038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Hawser SP, Bouchillon SK, Hoban DJ, et al. Low frequency of ertapenem-resistant intra-abdominal isolates of Escherichia coli from Latin America: susceptibility, ESBL-occurrence, and molecular characterisation (SMART 2008–2009). J Chemother. 2012;24(1):6–11. doi: 10.1179/1120009X12Z.0000000003 [DOI] [PubMed] [Google Scholar]
- 212.Quinteros M, Radice M, Gardella N, et al. Extended-spectrum beta-lactamases in Enterobacteriaceae in Buenos Aires, Argentina, public hospitals. Antimicrob Agents Chemother. 2003;47(9):2864–2867. doi: 10.1128/AAC.47.9.2864-2867.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Flamm RK, Sader HS, Jones RN. Ceftaroline activity tested against contemporary Latin American bacterial pathogens (2011). Braz J Infect Dis. 2014;18(2):187–195. doi: 10.1016/j.bjid.2013.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Nordberg V, Quizhpe-Peralta A, Galindo T, et al. High proportion of intestinal colonization with successful epidemic clones of ESBL-producing Enterobacteriaceae in a neonatal intensive care unit in Ecuador. PLoS One. 2013;8(10):e76597. doi: 10.1371/journal.pone.0076597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Fernandes MR, Sellera FP, Esposito F, Sabino CP, Cerdeira L, Lincopan N. Colistin-resistant mcr-1-positive Escherichia coli on public beaches, an infectious threat emerging in recreational waters. Antimicrob Agents Chemother. 2017;61(7):e00234–17. doi: 10.1128/AAC.00234-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Redondo C, Chalbaud A, Alonso G. Frequency and diversity of CTX-M enzymes among extended-spectrum beta-lactamase-producing Enterobacteriaceae isolates from Caracas, Venezuela. Microb Drug Resist. 2013;19(1):42–47. doi: 10.1089/mdr.2012.0079 [DOI] [PubMed] [Google Scholar]
- 217.Villar HE, Jugo MB, Macan A, Visser M, Hidalgo M, Maccallini GC. Frequency and antibiotic susceptibility patterns of urinary pathogens in male outpatients in Argentina. J Infect Dev Ctries. 2014;8(6):699–704. doi: 10.3855/jidc.3766 [DOI] [PubMed] [Google Scholar]
- 218.Moreno A, Bello H, Guggiana D, Domínguez M, González G. Extended-spectrum beta-lactamases belonging to CTX-M group produced by Escherichia coli strains isolated from companion animals treated with enrofloxacin. Vet Microbiol. 2008;129(1–2):203–208. doi: 10.1016/j.vetmic.2007.11.011 [DOI] [PubMed] [Google Scholar]
- 219.Pallecchi L, Bartoloni A, Fiorelli C, et al. Rapid dissemination and diversity of CTX-M extended-spectrum beta-lactamase genes in commensal Escherichia coli isolates from healthy children from low-resource settings in Latin America. Antimicrob Agents Chemother. 2007;51(8):2720–2725. doi: 10.1128/AAC.00026-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Báez J, Hernández-García M, Guamparito C, et al. Molecular characterization and genetic diversity of ESBL-producing Escherichia coli colonizing the migratory Franklin’s gulls (Leucophaeus pipixcan) in Antofagasta, North of Chile. Microb Drug Resist. 2015;21(1):111–116. doi: 10.1089/mdr.2014.0158 [DOI] [PubMed] [Google Scholar]
- 221.Conte D, Palmeiro JK, da Silva Nogueira K, et al. Characterization of CTX-M enzymes, quinolone resistance determinants, and antimicrobial residues from hospital sewage, wastewater treatment plant, and river water. Ecotoxicol Environ Saf. 2017;136:62–69. doi: 10.1016/j.ecoenv.2016.10.031 [DOI] [PubMed] [Google Scholar]
- 222.Nascimento T, Cantamessa R, Melo L, et al. International high-risk clones of Klebsiella pneumoniae KPC-2/CC258 and Escherichia coli CTX-M-15/CC10 in urban lake waters. Sci Total Environ. 2017;598:910–915. doi: 10.1016/j.scitotenv.2017.03.207 [DOI] [PubMed] [Google Scholar]
- 223.Flores R, Albornoz C, Hurtado J, Montaño V, Santa-Cruz A. Enterobacterias productoras de B-lactamasas de espectro-extendido y plásmido-AmpC en aguas de riego, zona Maica, Cochabamba [Extended-spectrum B-lactamase and plasmid ampc B-lactamase-producing Enterobacteriaceae in water sources for irrigation in Maica’s zone, Cochabamba]. Rev Cient Cienc Med. 2019;22(2):15–21. Spanish. [Google Scholar]
- 224.Guzman-Otazo J, Gonzales-Siles L, Poma V, et al. Diarrheal bacterial pathogens and multi-resistant Enterobacteria in the Choqueyapu River in La Paz, Bolivia. PLoS One. 2019;14(1):e0210735. doi: 10.1371/journal.pone.0210735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Ortega-Paredes D, Barba P, Mena-López S, Espinel N, Crespo V, Zurita J. High quantities of multidrug-resistant Escherichia coli are present in the Machángara urban river in Quito, Ecuador. J Water Health. 2020;18(1):67–76. doi: 10.2166/wh.2019.195 [DOI] [PubMed] [Google Scholar]