Abstract
Introduction
The Rothman Index (RI, PeraHealth, Inc. Charlotte, NC, USA) is a predictive model intended to provide continuous monitoring of a patient's clinical status. There is limited data to support its use in the risk stratification of patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). We hypothesized that low admission RI scores would correlate with higher rates of adverse outcomes in patients hospitalized for coronavirus disease 2019 (COVID-19).
Methods
Medical records of adult patients admitted to a single 1,200-bed tertiary academic center were retrospectively reviewed for demographic data, baseline characteristics, RI scores, admission to intensive care unit (ICU), need for mechanical ventilation, and inpatient mortality. Statistical analyses were performed using STATA statistical software, version 17 (Stata Corp LLC, College Station, TX, USA). Continuous variables were analyzed using the Mann-Whitney test, and categorical variables were analyzed using Fisher’s exact test. Both univariate and multivariate analyses were performed. A p-value <0.05 was considered statistically significant.
Results
Median admission RI score for the entire cohort was 63.0 (IQR 45.0 - 77.1). The cohort was divided by admission RI into a low-risk group (RI ≥70; n=70) and a high-risk group (RI <70; n=107). Compared to patients with low-risk RI, patients with high-risk RI had higher mortality (95.2%, 95% CI: 85.8 - 105 vs 4.8%, 95% CI: -5 - 14.2, p < 0.01), were more likely to require ICU admission (90.2%, 95% CI: 81.9 - 98.5 vs 9.8%, 95% CI: 1.5 - 18.1, p < 0.01) and mechanical ventilation (89.7%, 95% CI: 78.3 - 101 vs 10.3%, 95% CI: -1 - 21.7, p < 0.01), and had a longer median hospital length of stay (12 days, 95% CI: 9 - 14 vs 5 days, 95% CI: 4 - 7, p < 0.01).
Conclusions
High-risk RI was associated with increased admission to the ICU, mechanical ventilation, and mortality. These results suggest that it may be used as a tool to aid provider judgment in the setting of COVID-19.
Keywords: predictive models of mortality, risk of covid 19 mortality, covid-19 pandemic, mechanical ventilator, medical icu, risk assessment tools, sars-cov-2, rothman index, covid-19, coronavirus disease
Introduction
Since late 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread to all corners of the world causing a wide range of clinical diseases ranging from asymptomatic infections to severe coronavirus disease 2019 (COVID-19), including acute respiratory distress syndrome (ARDS). Estimates for patients who develop severe symptoms requiring admission to the intensive care unit (ICU) range from 5% to 20% [1] and around 1.56% of patients ultimately succumb to the disease [2].
Several factors including male gender, age, and presence of comorbidities (diabetes, hypertension, liver and heart disease) have been linked to increased mortality from the virus [3]. However, conflicting reports exist from different regions, assigning different weights to these predictors of outcome [4]. While some or all of these variables may be associated with adverse outcomes, they do not reflect the acuity of the presentation.
The Rothman Index (RI, PeraHealth, Inc. Charlotte, NC, USA) is a predictive model which uses continuous measurements of patient data from 26 non-static variables to measure physiologic acuity. A score based on vital signs, nursing assessments, laboratory results, and cardiac rhythm is calculated by measuring deviation from standard values, with a maximum score of 100 which signifies no deviation from standard values. A decrease in score correlates to a decrease in patient health. The RI was designed to be a score that is applicable to all types of patients, regardless of diagnosis, procedure, or environment [5]. The intention of the RI is to give providers quantifiable, continuous monitoring of a patient’s clinical status that is automatically generated by the electronic medical record (EMR).
Previously, studies have shown that RI was useful in early detection of deterioration of clinical status, resulting in reduced mortality and discharge to hospice [6]. It has shown predictive value in unplanned readmissions [7], post-discharge adverse events [5], 24-hr mortality, and one-year mortality [8,9]. However, other studies have not shown RI to effectively predict deterioration inwards [10] and it was not shown to be superior to a physician's judgment [11]. In other investigations, RI performs better than strictly vital sign-based acuity scores, such as the Modified Early Warning Score (MEWS), in identifying hospitalized patients who are at risk of dying within 24 hours [12].
A recent study conducted by PeraHealth, the developers of RI, has shown that RI has some use in risk stratification for patients with COVID-19; however, the accuracy and effectiveness of its implementation are of unknown significance [13].
Unique to the RI is its incorporation of nursing assessment into the overall score. The frequent head-to-toe monitoring of the patient can account for functional deteriorations that precede changes in vital signs or lab values, potentially making it more sensitive than other acuity scores [8,12]. This tool could allow for earlier detection of decline and earlier intervention, making it particularly useful in the setting of a novel disease when specific indicators of a worsening disease state are still unknown and physician judgment is still building. This study aims to assess the association of the RI in patients admitted to the hospital for COVID-19 with three clinically important outcomes: the need for mechanical ventilation, ICU admission, and inpatient mortality.
Materials and methods
All consecutive adult patients admitted to the hospital who tested positive for SARS-CoV-2 from April 2020 to July 2020 were reviewed in this retrospective cohort study at a single 1,200-bed tertiary academic center in North-central Florida. Waiver for written informed consent was obtained from the University of Florida Health System Institutional Review Board. Compliance with the World Medical Association Declaration of Helsinki was maintained during this retrospective cohort study.
Infection with SARS-CoV-2 was confirmed through nucleic acid amplification testing of nasopharynx swabs using real-time reverse-transcriptase polymerase chain reaction assays, carried out according to validated protocols [14].
EMRs were reviewed to collect data on demographics, baseline characteristics, admission RI scores, and outcomes of interest; the primary outcome was inpatient mortality, and secondary outcomes were the need for mechanical ventilation and admission to the ICU. High-risk RI was defined as <70 based on prior literature [6]. In order to dichotomize the groups for statistical analysis, RI ≥70 was considered low-risk. Patients who were admitted for a primary problem unrelated to COVID-19 with incidentally positive SARS-CoV-2 tests were excluded from the analysis. Incidentally positive was defined as having a positive SARS-CoV-2 nucleic acid amplification test ordered per hospital protocol but not exhibiting any of the most common symptoms of COVID-19, such as fever, cough, or dyspnea [15] and having a primary admission diagnosis that was not COVID-19.
As our data was not normally distributed, we utilized non-parametric statistics. Continuous variables were analyzed using the Mann-Whitney test and were presented using medians and interquartile ranges. Categorical variables were analyzed using Fisher’s exact test and were presented as percentages with 95% CI. Variables significant at the 0.10 level on univariate analysis were selected for multivariate analysis. Multivariate analysis was performed with a non-parametric logistic regression with odds ratios and CIs. Continuous variables such as age were recoded into quintiles for ease of analysis. Multivariate analysis results were presented as odds ratios with 95% CI and two-sided p-values. Alternative logistic regression models including only variables significant at the 0.05 level on univariate analysis were also performed to assess for robustness and since they yielded the same final results, they were not included in this paper. Two-sided p-values < 0.05 were considered statistically significant in multivariate analysis. No imputations were made for missing data. Statistical analyses were performed using STATA statistical software, version 17 (Stata Corp LLC, College Station, TX, USA) [16].
Results
A total of 210 patients were admitted to the hospital with a positive SARS-CoV-2 test during the time frame of the study. Thirty-one patients incidentally tested positive during admission for another primary diagnosis. These 31 patients did not exhibit the most common symptoms of COVID-19 [15] and hence were excluded from the analysis. Of the 179 patients admitted for COVID-19, RI could not be calculated in two patients.
Demographic data and baseline characteristics are shown in Table 1. The median age for the entire cohort was 58.4 years (IQR 45.1 - 70.2) and 39% of the cohort was male. No statistically significant differences were found for age or gender when compared for the primary (inpatient mortality) or secondary outcomes (need for mechanical ventilation, admission to the ICU).
Table 1. Univariate Analysis of Predictors of Intensive Care Unit Admission, Mechanical Ventilation, and In-Hospital Mortality in Patients Admitted with COVID-19.
Values displayed as percentages with 95% confidence intervals. ICU, intensive care unit; IQR, interquartile range.
| Variable | ICU Admission (n=51) | No ICU Admission (n=128) | p-value | Mechanically Ventilated (n=29) | Not Mechanically Ventilation (n=150) | p-value | Deceased (n=21) | Survived (n=156) | p-value |
| High Risk Rothman index | 90.2 (81.9 - 98.5) | 48.4 (39.6 - 57.2) | 0.000 | 89.7 (78.3 - 101.0) | 54.7 (46.6 - 62.8) | 0.000 | 95.2 (85.8 - 105) | 55.8 (47.9 - 63.6) | 0.000 |
| Age years (Median, IQR) | 60.7 (43.5 - 67.3) | 58 (45.6 - 71.65) | 0.062 | 62.7 (43.5 - 67.3) | 57.9 (45.6 - 70.4) | 0.049 | 57.8 (45.1 - 67.5) | 67.4 (58.3 - 78.2) | 0.094 |
| Elevated Troponin I | 32.0 (18.8 - 45.2) | 23.1 (15.1 - 31.2) | 0.248 | 34.5 (16.7 - 52.2) | 24.0 (16.6 - 31.5) | 0.250 | 42.9 (21.0 - 64.7) | 23.4 (16.2 - 30.5) | 0.066 |
| Renal Replacement Therapy | 13.7 (4.1 - 23.3) | 5.5 (1.49 - 9.45) | 0.118 | 20.7 (5.6 - 35.8) | 5.33 (1.7 - 9.0) | 0.013 | 6.96 (2.95 -11.0) | 14.3 (-1.16 - 29.7) | 0.216 |
| Obesity | 62.7 (49.3 - 76.2) | 48.4 (39.7 - 57.2) | 0.098 | 62.0 (44.0 - 80.2) | 50.7 (42.6 - 58.8) | 0.312 | 57.1 (35.3 - 78.9) | 51.9 (44.0 - 59.8) | 0.817 |
| CAD/CHF | 27.5 (15.0 - 39.9) | 28.9 (21.0 - 36.8) | 1.000 | 34.5 (16.8 - 52.2) | 27.3 (20.1 - 34.5) | 0.501 | 38.1 (16.7 - 59.5) | 27.2 (20.2 - 34.2) | 0.311 |
| Hyperlipidemia | 43.1 (29.3 - 57.0) | 36.7 (28.3 - 45.2) | 0.497 | 44.8 (26.3 - 63.4) | 37.3 (29.5 - 45.2) | 0.533 | 47.6 (25.6 - 69.7) | 37.3 (29.7 - 45.0) | 0.475 |
| Hypertension | 66.7 (53.5 - 79.8) | 61.7 (53.2 - 70.2) | 0.608 | 69.0 (51.7 - 86.2) | 62.0 (54.2 - 69.9) | 0.534 | 71.4 (51.5 - 91.4) | 62.0 (54.4 - 69.7) | 0.477 |
| Diabetes Mellitus | 42.0 (28.1 - 55.9) | 43.8 (35.1 - 52.4) | 0.868 | 50.0 (31.0 - 69.0) | 42.0 (34.0 - 50.0) | 0.534 | 50.0 (27.4 - 72.6) | 42.4 (34.6 - 50.2) | 0.633 |
| Reduced RV Systolic Function | 21.2 (67.4 - 35.7) | 83.3 (-3.2 - 19.9) | 0.277 | 21.7 (4.1 - 39.3) | 11.7 (0.5 - 23.0) | 0.461 | 21.4 (-1.4 - 44.2) | 14.0 (3.2 - 24.7) | 0.674 |
| Reduced LV Systolic Function | 21.2 (6.7 - 35.7) | 25.0 (6.9 - 43.1) | 0.759 | 17.4 (12.0 - 33.6) | 26.5 (11.0 - 41.8) | 0.529 | 28.6 (3.5 - 53.6) | 20.9 (8.4 - 33.5) | 0.715 |
| Male | 39.2 (25.6 - 52.8) | 39.1 (30.5 - 47.6) | 1.000 | 44.8 (26.3 - 63.4) | 38.0 (30.2 - 45.9) | 0.536 | 42.9 (21.0 - 64.7) | 38.6 (31.0 - 46.3) | 0.813 |
| Liver Disease | 3.9 (-1.5 - 9.4) | 10.2 (4.9 - 15.5) | 0.238 | 69.0 (-2.6 - 16.4) | 8.7 (4.2 - 13.2) | 1.000 | 4.8 (-4.6 - 14.2) | 8.9 (4.4 - 13.3) | 1.000 |
Age achieved a p-value of < 0.10 for all three outcomes and hence was included in all multivariate analyses. Obesity (defined as body mass index ≥30) was included in the multivariate analysis for ICU admission after achieving a p-value of <0.10 in univariate analysis. It was not included in the models for mortality or mechanical ventilation as it did not achieve a p-value of <0.10 in univariate analysis for these variables. Statistically significant differences with p-values <0.05 were noted in univariate analysis for age (62.7 vs. 57.9 years, p=0.049) and need for renal replacement therapy (20.7% vs 5.3%, p=0.013) with regards to the outcome of mechanical ventilation. Neither age nor the need for renal replacement therapy showed significant findings with regards to ICU admission or in-hospital mortality. Comorbidities like diabetes, dyslipidemia, hypertension, heart disease and liver disease did not differ in prevalence when segregated into groups by any of the outcomes of interest.
In addition to the comorbidities and baseline characteristics, we recorded data on troponin I elevation and echocardiographic findings regarding left or right ventricular dysfunction. These factors were not independently associated with mortality, the need for mechanical ventilation, or ICU admission in univariate analysis. Troponin elevation did, however, achieve the threshold of p <0.10 to be included in the multivariate analysis for in-hospital mortality.
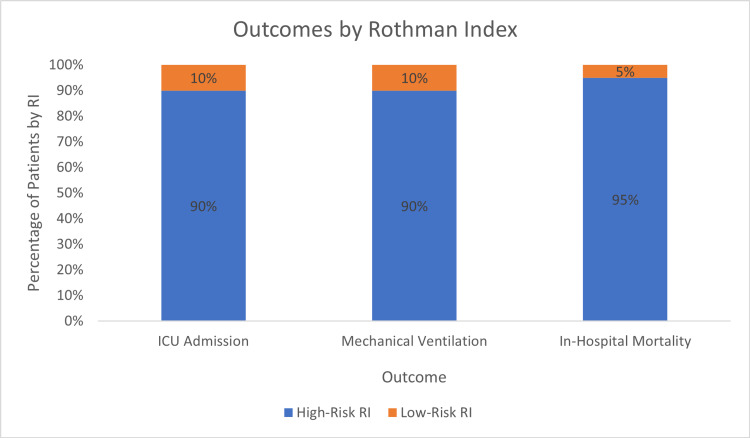
Median RI score on admission for the entire cohort was 63.0 (IQR 45.0 - 77.1). Patients who died in the hospital had lower median RI scores than patients who survived (32.1 vs. 65.5, p <0.001). Lower RI scores were also associated with increased ICU utilization (45.9 vs. 70.0, p <0.001) and the need for mechanical ventilation (41.5 vs. 65.8, p <0.001). When RI scores were dichotomized into high-risk scores (RI <70) or low-risk scores (RI ≥70), p-values were <0.001 on univariate analysis for all three outcomes and hence, selected for multivariate analysis. 95.2% of patients who had a COVID-19-attributable death while in the hospital had a high-risk RI score. 90% of patients who were admitted to the ICU at some point during their hospital course had a high-risk RI score on admission. Similarly, 89.7% of patients that required mechanical ventilation had a high-risk RI score on admission (Figure 1).
Figure 1. Outcomes by Rothman Index.
ICU, intensive care unit; RI, Rothman index.
Multivariate analyses are presented in Tables 2-4 for each of the selected outcomes. Obesity was independently associated with need for ICU admission (OR 2.16, 1.01 - 4.61; p=0.046). Age was not independently associated with any of the outcomes in multivariate analyses. Renal replacement therapy was not independently associated with the need for mechanical ventilation and troponin elevation was not independently associated with in-hospital mortality. A high-risk RI score (<70) was the only variable that showed consistent independent association with ICU utilization (OR 13.05, 4.66 - 36.57; p< 0.001), mechanical ventilation (OR 6.69, 1.88 - 23.78; p=0.003) and death (OR 12.58, 1.59 - 99.39; p=0.016).
Table 2. Multivariate Analysis of Predictors of Intensive Care Unit Admission in Patients Admitted with COVID-19.
CI, confidence interval.
| Variable | Odds Ratio | 95% CI | p-value |
| High-Risk Rothman Index | 13.05 | 4.66 - 36.57 | 0 |
| Age | 0.81 | 0.61 - 1.08 | 0.155 |
| Obesity | 2.16 | 1.01 - 4.61 | 0.046 |
Table 4. Multivariate Analysis for Predictors of In-Hospital Mortality in Patients Admitted with COVID-19.
CI, confidence interval.
| Variable | Odds Ratio | 95% CI | p-value |
| High-Risk Rothman Index | 12.58 | 1.59 - 99.39 | 0.016 |
| Age | 1.22 | 0.82 - 1.81 | 0.322 |
| Elevated Troponin | 1.44 | 0.52 - 3.94 | 0.481 |
Table 3. Multivariate Analysis of Predictors of Mechanical Ventilation in Patients Admitted with COVID-19.
CI, confidence interval.
| Variable | Odds Ratio | 95% CI | p-value |
| High Risk Rothman Index | 6.69 | 1.88 - 23.78 | 0.003 |
| Age | 0.89 | 0.65 - 1.24 | 0.497 |
| Renal Replacement Therapy | 3.04 | 0.94 - 9.88 | 0.065 |
Discussion
When faced with the same disease, certain patients will have a more severe clinical course and many efforts have been made to find factors to separate individuals at increased risk of poor outcomes. Age is considered to be a major factor in disease mortality, but age may only be a proxy for the number and severity of comorbidities a given person may have. Scores like the Charlson comorbidity score have been created to account for the increased risk of any given patient [17]; similarly, comorbidities may in turn be a surrogate marker for acuity. A major outcome predictor for a given illness in patients with the same age and number of comorbidities may be their acuity, which can be evaluated by tools like the RI. RI holistically assesses a patient’s clinical status based on vital signs, laboratory values, and nursing assessments among other variables. Lower values correlate to more severe acuity. It has been used to detect early clinical deterioration to further improve care and identify patients at increased risk of mortality [6], but it has yet to be widely accepted in clinical practice. In this single-center retrospective study, we evaluated the association between RI on admission and relevant clinical outcomes to assess the potential utility of RI to predict important clinical outcomes in patients with a primary diagnosis of COVID-19. High-risk RI on admission was associated with higher mean hospital length of stay and led more frequently to ICU utilization, mechanical ventilation, and death.
As a novel disease, healthcare providers have not been able to reliably predict deterioration in patients with COVID-19. There are few predictive tools to stratify patients and guide care. Gong et al. conducted a retrospective review of 372 COVID-19 patients in China to identify patient characteristics and laboratory values on admission associated with developing the severe disease [18]. To improve risk stratification, they created a nomogram based on age, serum lactate dehydrogenase, C-reactive protein, coefficient of variation of red blood cell distribution width, blood urea nitrogen, direct bilirubin, and albumin levels. While this risk stratification tool may be used in patients with those laboratory values available on admission, it has limited use in patients without them, and it requires manual stratification of patients which is subject to human error. Additionally, given the differential expression of the angiotensin-converting enzyme 2 (ACE2) receptor protein for SARS-CoV-2 between populations [19], this prediction tool may not be valid for patient populations found in the United States. RI is an alternative method for evaluating clinical status that does not require all parameters to be filled and additionally, incorporates vital signs and nursing assessments.
The RI was created to assist clinicians in the early detection of patient deterioration [5]. It has been assessed as a predictive tool for outcomes in several clinical scenarios including both surgical and medical contexts. Alarhayem et al. performed a retrospective review of 1,445 surgical patients transferred from the surgical ICU (SICU) to the surgical floor and found that patients readmitted to the SICU had lower pretransfer and post-transfer RI scores [9], suggesting RI may assist in determining which patients are ready for discharge from the SICU to the surgical floor. In another study, among 2,687 patients who underwent elective spine surgery, RI was significantly inversely correlated with adverse events and readmission within 30 days of discharge [20]. Gotur et al. retrospectively evaluated 194 adult patients admitted to the medical ICU and found that patients with RI < 50 had a higher risk of adverse events post-discharge from the ICU [21]. Thus, RI may be useful in guiding medical ICU discharge decision-making. Additionally, in a prospective study, Arnold et al. compared physician judgment to RI for predicting clinical deterioration in a general hospital ward and found that the combination of physician judgment and RI outperformed either alone [11]. Another retrospective study of 227 patients with advanced cancer admitted to an institution showed RI scores <60 to be associated with longer length of stay, more palliative care, and hospice referrals, and increased mortality [22]. These studies highlight that RI may have predictive ability for several outcomes across different contexts, both surgical and medical. However, the efficacy of RI to predict patient deterioration in COVID-19 is not fully known.
Data is lacking in the evaluation of the association between RI scores and clinical outcomes in patients infected with SARS-CoV-2. Beals et al. conducted a multicenter retrospective study of 18,157 patients, 3,499 of which were infected with SARS-CoV-2 [23]. Admission RI provided the predictive ability of in-hospital mortality in both SARS-CoV-2-infected and non-SARS-CoV-2-infected patients. Stratification by admission of the RI into high-risk and low-risk groups also demonstrated increased mortality in high-risk patients. The discriminating ability of admission RI to predict the need for ICU admission was fair to good. The study highlights the predictive ability of admission RI to predict mortality and potentially ICU admission in patients admitted with COVID-19. Notably, the study does not differentiate patients admitted for COVID-19 management from patients admitted for other medical reasons who incidentally test positive for COVID-19 during admission. Thus, the predictive ability for mortality and ICU admission in this cohort may be confounded by patients experiencing other underlying medical conditions in the setting of asymptomatic SARS-CoV-2 infection. In the present study, patients admitted to our institution with a positive SARS-CoV-2 laboratory test were categorized based on the reason for admission. Patients who were not admitted for symptomatic COVID-19 were excluded from the study. Thus, the current study provides a better characterization of the predictive ability of admission RI for outcomes in the management of COVID-19.
While our study contributes to understanding the potential ability of admission RI to stratify patients and predict mortality, need for mechanical ventilation, and ICU admission, it has limitations warranting discussion. As a retrospective study, definitive conclusions may not be made about the predictive ability of RI but rather only about the associations between RI and outcomes. Confounding variables may not have been recorded during the retrospective review of the EMR, potentially influencing conclusions made from this study. Multivariate analysis helps to mitigate the role of confounding variables recorded but does not influence the effect of confounding variables that may have been missed.
Conclusions
In conclusion, there are few applicable risk prediction models for the stratification of patients admitted for COVID-19. While healthcare provider judgment is essential to delivering high-quality care, a metric for early detection of patient deterioration in a novel disease such as COVID-19 can assist provider judgment. The RI provides a continuous variable assessing a patient’s clinical status and has been shown in several non-COVID-19 contexts to have stratification abilities for outcomes such as ICU readmission, hospital readmission, and mortality. Data evaluating the utility of RI in patients admitted for COVID-19 is lacking. In this study, stratification of admission RI by severity showed that high-risk admission RI in COVID-19 was independently associated with mortality, the need for mechanical ventilation, and ICU admission, and had more predictive value than traditional risk factors. Low admission RI scores should prompt healthcare providers to have heightened vigilance and a lower threshold for advancing care unless provider judgment determines further care to be futile. Prospective studies may be helpful to evaluate the incorporation of RI into clinical practice and its effects on clinical decision-making, resource utilization, and clinical outcomes. Furthermore, the association between admission RI and outcomes associated with new coronavirus variants as well as RI’s predictive ability for vaccinated and unvaccinated individuals should be explored.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. University of Florida Institutional Review Board issued approval IRB202000908
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Cummings MJ, Baldwin MR, Abrams D, et al. Lancet. 2020;395:1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention: COVID data tracker. [ Dec; 2021 ]. 2021. https://covid.cdc.gov/covid-data-tracker/ https://covid.cdc.gov/covid-data-tracker/
- 3.COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. Li LQ, Huang T, Wang YQ, et al. J Med Virol. 2020;92:577–583. doi: 10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clinical and demographic characteristics of patients dying from COVID-19 in Italy vs China. Lippi G, Mattiuzzi C, Sanchis-Gomar F, Henry BM. J Med Virol. 2020;92:1759–1760. doi: 10.1002/jmv.25860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Development and validation of a continuous measure of patient condition using the Electronic Medical Record. Rothman MJ, Rothman SI, Beals J IV. J Biomed Inform. 2013;46:837–848. doi: 10.1016/j.jbi.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Identifying patients at increased risk for unplanned readmission. Bradley EH, Yakusheva O, Horwitz LI, Sipsma H, Fletcher J. Med Care. 2013;51:761–766. doi: 10.1097/MLR.0b013e3182a0f492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Rothman Index is associated with postdischarge adverse events after hip fracture surgery in geriatric patients. McLynn RP, Ottesen TD, Ondeck NT, Cui JJ, Rubin LE, Grauer JN. Clin Orthop Relat Res. 2018;476:997–1006. doi: 10.1007/s11999.0000000000000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mortality reduction associated with proactive use of EMR-based acuity score by an RN team at an urban hospital. Rothman M, Rimar J, Coonan S, Allegretto S, Balcezak T. BMJ Qual Saf. 2015;24:734–735. [Google Scholar]
- 9.Application of electronic medical record-derived analytics in critical care: Rothman Index predicts mortality and readmissions in surgical intensive care unit patients. Alarhayem AQ, Muir MT, Jenkins DJ, Pruitt BA, Eastridge BJ, Purohit MP, Cestero RF. J Trauma Acute Care Surg. 2019;86:635–641. doi: 10.1097/TA.0000000000002191. [DOI] [PubMed] [Google Scholar]
- 10.Impact of Rothman index on delay of ICU transfer for hematology and oncology patients deteriorating in wards. Fitzpatrick N, Guck D, Van de Louw A. Crit Care. 2018;22:331. doi: 10.1186/s13054-018-2268-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Comparing the predictive ability of a commercial artificial intelligence early warning system with physician judgement for clinical deterioration in hospitalised general internal medicine patients: a prospective observational study. Arnold J, Davis A, Fischhoff B, et al. BMJ Open. 2019;9:0. doi: 10.1136/bmjopen-2019-032187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Measuring the modified early warning score and the Rothman index: advantages of utilizing the electronic medical record in an early warning system. Finlay GD, Rothman MJ, Smith RA. J Hosp Med. 2014;9:116–119. doi: 10.1002/jhm.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Identification on admission of COVID-19 patients at risk of subsequent rapid clinical deterioration. Beals J, Barnes J, Durand D, et al. medRxiv. 2020 [Google Scholar]
- 14.World Health Organization: Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance, 28 January 2020. [ Jan; 2021 ]. 2020. https://apps.who.int/iris/handle/10665/330893 https://apps.who.int/iris/handle/10665/330893
- 15.Determine the most common clinical symptoms in COVID-19 patients: a systematic review and meta-analysis. Alimohamadi Y, Sepandi M, Taghdir M, Hosamirudsari H. J Prev Med Hyg. 2020;61:0–12. doi: 10.15167/2421-4248/jpmh2020.61.3.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.StataCorp: STATA statistical software: release 17. [ Mar; 2022 ]. 2021. https://www.stata.com/ https://www.stata.com/
- 17.A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Charlson ME, Pompei P, Ales KL, MacKenzie CR. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.A tool for early prediction of severe coronavirus disease 2019 (COVID-19): a multicenter study using the risk nomogram in Wuhan and Guangdong, China. Gong J, Ou J, Qiu X, et al. Clin Infect Dis. 2020;71:833–840. doi: 10.1093/cid/ciaa443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Comparative genetic analysis of the novel coronavirus (2019-nCoV/SARS-CoV-2) receptor ACE2 in different populations. Cao Y, Li L, Feng Z, et al. Cell Discov. 2020;6:11. doi: 10.1038/s41421-020-0147-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Rothman Index as a predictor of postdischarge adverse events after elective spine surgery. McLynn RP, Ondeck NT, Cui JJ, Swanson DR, Shultz BN, Bovonratwet P, Grauer JN. Spine J. 2018;18:1149–1156. doi: 10.1016/j.spinee.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Analysis of Rothman Index data to predict postdischarge adverse events in a medical intensive care unit. Gotur DB, Masud F, Paranilam J, Zimmerman JL. J Intensive Care Med. 2020;35:606–610. doi: 10.1177/0885066618770128. [DOI] [PubMed] [Google Scholar]
- 22.Palliative referrals in advanced cancer patients: utilizing the Supportive and Palliative Care Indicators Tool and Rothman Index. Chan AS, Rout A, Adamo CR, Lev I, Yu A, Miller K. Am J Hosp Palliat Care. 2022;39:164–168. doi: 10.1177/10499091211017873. [DOI] [PubMed] [Google Scholar]
- 23.Stratifying deterioration risk by acuity at admission offers triage insights for coronavirus disease 2019 patients. Beals J IV, Barnes JJ, Durand DJ, et al. Crit Care Explor. 2021;3:0. doi: 10.1097/CCE.0000000000000400. [DOI] [PMC free article] [PubMed] [Google Scholar]