Abstract
Introduction
High salt intake has been connected with the increase of many non‐communicable diseases (NCDs) worldwide. Like other middle‐income countries, Iran is experiencing a considerable increase in NCDs, necessitating attempts to reduce dietary salt intake. As in Iran there is uncertainty about the existing rate of salt intake. The present study aimed to estimate mean salt intake of Iranian population by systematically reviewing existing literature.
Methods
This research is a systematic review and meta‐analysis (PRISMA Protocol) of published article data, with no time constraint until the end of 2020, to estimate mean salt intake of Iranian population. A comprehensive literature search was performed on international databases of Medline, Science Direct, PubMed, Embase, Scopus, Springer, Online Library Wiley, Web of Science, Cochrane, and Google Scholar and domestic data bases of Iranmedex, Magiran, SID, and Medlib. Subgroup analysis was conducted for gender, region, measurement method, and age group. Research homogeneity was evaluated by I 2 statistic. We reviewed all studies which met inclusion criteria. STATA Ver.13.1 was used to perform meta‐analysis.
Results
Meta‐analysis of data from 32 studies showed that the average salt intake in all ages was 9.674 g/day (95% CI, 9.033–10.316 g/day). The lowest estimation of salt intake was 9.33 g/day (95% CI, 7.75–10.91 g/day) which was estimated from studies which used point collection method, and the highest estimate using the food reminder questionnaire was 10.41 g/day (95% CI, 8.49–12.34 g/day). Also, the average weight salt intake for men over 18 years old in different cities was 10.39 g/day (95% CI, 9.01–11.78 g/day), for women over 18 years in different cities 9.52 g/day (95% CI, 8.42–10.62 g/day), and children and adolescents was estimated at 5.664 g/day (95% CI, 2.91–8.41 g/day).
Conclusion
The intake of salt in the Iranian population is near twice the WHO recommendation. Therefore, it is necessary to consider effective strategies and interventions to reduce dietary salt intake in Iran as a health priority.
Keywords: Iran, meta‐analysis, salt intake, sodium, systematic review
1. INTRODUCTION
High salt intake has been associated with the development of many non‐communicable diseases (NCDs) worldwide. 1 The high salt intake appears to be harmful to humans and is a primary cause of several NCDs with a detrimental effect on blood pressure. 2 Excessive salt intake is associated with kidney disease, an increased risk of obesity, osteoporosis, and gastric cancer. 3 , 4 It also increases the risk of cardiovascular diseases (CVDs), cardiac thrombosis, asthma, and gastric ulcer. 5 Excessive salt intake is the world's seventh leading cause of death responsible for cardiovascular disease, 6 Generally accounting for 20% of cardiac deaths, 13% of stroke deaths, and 11% of deaths from ischemic heart disease. 7 The World Health Organization (WHO) has set salt reduction as the main priority in the fight against NCDs. 8 Many studies have found that lowering daily salt intake can greatly improve patients' health. 9 , 10 According to a UK study, cutting salt intake to 6 g/day could save the lives of 2.5 million individuals globally from stroke and ischemic heart disease. 11 In general, a decrease in salt intake to 5 g/day results in a 23% reduction in strokes and a 17% reduction in CVDs risk factors. 12 , 13 As a result, the WHO recommends that individuals consume 5 g/day. 14 To that end, WHO member countries have committed to a 30% reduction in salt intake by 2025. 15 Although the recommendation of 5–6 g of salt per day would have a major effect on blood pressure and cardiovascular disease reduction, it could be regarded as a satisfying solution. Indeed community would benefit from further reduction of salt intake (3 g daily salt intake) in the form of much greater prevention of related diseases, 16 it is extremely effective for disease prevention, particularly in low‐ and middle‐income countries. 17 It is one of the most cost‐effective strategies for lowering premature death and disability in these societies. 18 Like other middle‐income countries, Iran is experiencing a considerable increase in NCDs, necessitating attempts to reduce salt intake in Iran. 19 As a result, data characterizing the problem's nature and magnitude are necessary. The national salt reduction policy should be executed in accordance with current knowledge regarding the mean salt intake in the country. This study was conducted with the aim of systematic review and meta‐analysis of the mean salt intake in Iran.
2. METHOD
The current study provides a systematic review and meta‐analysis (PRISMA Protocol) of published article data, with no time constraint until the end of 2020, to characterize the mean salt intake of Iranian populations.
2.1. Data sources and search strategy
National and international electronic databases, including Medline, Science Direct, PubMed, Embase, Scopus, Iranmedex, Magiran, SID, Springer, Online Library Wiley, Web of Science, Medlib, Cochrane, and Google Scholar, were searched for related articles using the keywords of “sodium” or “salt,” “Iran,” and “intake,” “ingest*,” “eat*,” “consume*,” “diet,*” “urine*,” or excrete. Due to the insensitivity of national databases to search operators (AND, OR, NOT), the search on these databases was restricted to Persian keywords (S.P.; V.Y.‐F.). We reviewed the sources of the articles to see if there were any further relevant articles. At the end of the search, two authors separately (S.P.; R.G.) reviewed the list of abstracts identified by them, as well as the full texts of the eligible abstracts. A third researcher (M.A.E.) reviewed the articles in disagreement between the two researchers.
2.2. Inclusion and exclusion criteria
The analysis included studies that examined urine sodium using any collection method (such as urine stop sampling, overnight urine samples, and 12‐ or 24‐h urine collection), daily dietary salt intake (Food Frequency Questionnaire (or any self‐report method. There were no age or gender limitations in Iranian populations (men, women, and children). Studies with convenience sampling (Because the results are not generalizable to the community) or those on specific populations were excluded (e.g., patients with hypertension). Furthermore, we excluded papers for which we did not have full‐text access.
2.3. Quality assessment
The researchers employed the National Institute of Health (NIH) quality assessment checklists to assess the articles' quality. The NIH quality assessment forms were provided based on the study design (cohort, case–control, cross‐section, etc.). Various aspects of bias sources, study rigor, and so on have been assessed. 20 Two referees assessed the quality of the studies (S.P.; R.G.). If the two authors differed about the study's results, a third researcher reviewed them.
2.4. Data extraction
The authors provided the following information in Excel after reviewing the text of related studies: year of publication, year of data collection, city, the scope of the study (national or community‐based study), sample size, salt intake in men and women (with SD), and sodium intake reporting method. When studies did not report the mean daily salt intake in grams, multiple conversion formulas were employed to determine the average. A single researcher gathered the data, which was subsequently verified by another (S.P.). If there was a disagreement at this point, the third researcher reviewed the article (M.A.).
2.5. Outcome measures
The mean population salt intake was estimated as g/day. Secondary results were also obtained based on the mean salt intake by sex, location, study type, and salt reporting method (urine or dietary analysis).
2.6. Data synthesis
Because the mean and SD were the main indices evaluated in this study, the mean salt intake (with 95% CI) was estimated in the primary and secondary analyses using the inverse variance‐weighted average method. The I 2 statistic was used to assess the research homogeneity. Due to the homogeneity of the research, it was unnecessary to utilize different models for combination, because of zero I 2 we applied fixed‐effects meta‐analysis. Begg's funnel plot was used to analyze publication bias. STATA was used to analyze the data (version 13.1) and a p value of less than 0.05 was considered statistically significant.
2.7. Subgroup analysis
Given that some social, economic, geographical, and cultural parameters and the type of measurement tool may affect the pattern of behavior in salt intake, so sensitivity analysis was conducted for gender, region, measurement method, and age group. To analyze the sensitivity of the gender parameter, in studies reported aggregated results for both genders we classified them as both.
2.8. Geographical distribution
We used Geographic Information System (GIS) to determine the prevalence of salt consumption by geographical area. GIS is the most important tool in providing statistics and disease information in the form of visual presentation. 21 Equal interval model was used, so that the distance between the province that had the highest amount of salt consumption and the province that had the lowest amount, is divided into five categories with equal interval.
3. RESULTS
Out of 1788 abstracts, 1695 were removed due to duplication and irrelevance, and 76 papers were then reviewed. Finally, 32 studies met the inclusion criteria (Figure 1). The total number of samples in these studies, which gave information on Iran's provinces' daily population intake between 1980 and 2020, was 34,223 people. There were 27 cross‐sectional studies (n = 33,186), 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 one randomized controlled trial (n = 100), 49 three case–control studies (n = 771), 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 and one quasi‐experimental research (n = 166). 51 Two studies 39 , 41 involved children and adolescents, whereas four involved only women. 29 , 43 , 48 , 52 Table 1 shows the general characteristics and data of each study.
Figure 1.
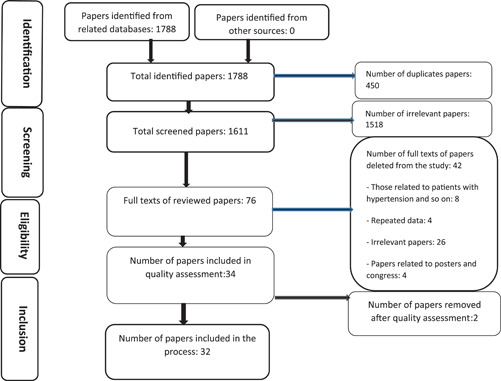
Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) flow diagram for the selection of publications included in our analysis
Table 1.
The investigations of the salt intake of Iran, included in the meta‐analysis
| Study | Year | City | Sample | Method of Assessment | Mean salt intake g/day | ||
|---|---|---|---|---|---|---|---|
| All | Men | Women | |||||
| Page et al. 22 | 1981 | Ilam | 130 | Overnight urine samples | 10.01 | ND | ND |
| Rahmani et al. 24 | 2000 | Ilam | 75 | Spot urine sample | 9.98 | ND | ND |
| 61 | 11.6 | ||||||
| Azizp et al. 25 | 2001 | Rasht | 327 | Food Frequency Questionnaire | 7.2 | ND | ND |
| Sari | 356 | 7.7 | |||||
| Rafiei et al. 26 | 2001 | Isfahan | 850 | Sodium intake in a 24‐h period | 9.7 | 9.6 | 9.75 |
| Rafiei et al. 27 | 2008 | Isfahan | 912 | Sodium intake in a 24‐h period | 9.9 | 11.1 | 9.6 |
| Nazeri et al. 28 | 2010 | Tehran | 639 | Sodium intake in 24 h | ND | ND | 9.67 |
| Motlagh et al. 29 | 2010 | Yazd | 252 | Food Frequency Questionnaire | ND | ND | 10.09 |
| Nazeri et al. 30 | 2010 | Tehran | 156 | Sodium intake in a 24‐h period | 9.1 | 10.4 | 8.7 |
| Nazeri et al. 31 | 2011 | Tehran | 242 | Sodium intake in 24 h | 9.3 | ND | ND |
| Khosravi et al. 23 | 2012 | Isfahan | 1052 | Sodium intake in 24 h | 8.11 | 7.59 | 8.17 |
| 374 | 13.29 | 14.29 | 11.49 | ||||
| 806 | 12.355 | 13.29 | 9.93 | ||||
| Naghibi et al. 33 | 2012 | Sari | 416 | Food Frequency Questionnaire | 12.8 | ND | ND |
| Kelishadi et al. 39 | 2013 | Isfahan | 500 | Spot urine sample | 7.08 (child) | ND | ND |
| Haghigat dost et al. 34 | 2013 | Isfahan | 806 | Sodium intake in 24 h | 9.82 | ND | ND |
| Atazadegan et al. 32 | 2014 | Shiraz | 68 | Food Frequency Questionnaire | 10.89 | ND | ND |
| Garipour et al. 37 | 2014 | Isfahan | 410 | Sodium intake in 24 h | 10.44 | ND | ND |
| Moeini et al. 52 | 2014 | Isfahan | 45 | Spot urine sample | ND | ND | 10.47 |
| 47 | ND | 10.23 | |||||
| Mirzaei et al. 38 | 2014 | Yazd | 213 | Sodium intake in 24 h | 9.13 | 10.02 | 7.56 |
| Jafari et al. 50 | 2016 | Kerman | 310 | Spot urine sample | 9.5 | ND | ND |
| 346 | 8.8 | ||||||
| Mohammadifard et al. 40 | 2017 | Isfahan | 796 | Sodium intake in 24 h | 10.77 | 11.03 | 10.17 |
| Soltani et al. 43 | 2017 | Yazd | 195 | Food Frequency Questionnaire | ND | ND | 9.36 |
| Rafiei et al. 41 | 2017 | Isfahan | 374 | Sodium intake in 24 h | 5.05 (Child) | ND | ND |
| Akhondzadeh et al. 49 | 2018 | Yazd | 100 | Sodium intake in 24 h | 8.35 | ND | ND |
| Rezaei et al. 42 | 2018 | Iran | 18635 | Sodium intake in 24 h | 9.68 | 9.74 | 9.32 |
| Mohammadifard et al. 36 | 2019 | Isfahan | 183 | Sodium intake in 24 h | 9.5 | 9.6 | 9.5 |
| 51 | 9.7 | 9.76 | 9.86 | ||||
| 218 | 9.6 | 10.31 | 9.2 | ||||
| 402 | 10.02 | 11.43 | 9.28 | ||||
| Arsang‐Jang et al. 35 | 2019 | Isfahan | 1059 | Sodium intake in 24 h | 9.9 | 9.71 | 9.81 |
| 374 | 10.06 | 10.31 | 9.81 | ||||
| 806 | 10.29 | 11.43 | 9.28 | ||||
| Abadi et al. 44 | 2019 | Yazd | 110 | Sodium intake in 24 h | 9.35 | 9.82 | 8.87 |
| Ghorbani et al. 53 | 2019 | Isfahan | 23 | Sodium intake in 24 h | 10.03 | ND | ND |
| Khosravi et al. 45 | 2019 | Isfahan | 1099 | Sodium intake in 24 h | 11.66 | ND | ND |
| Mohammadifard et al. 46 | 2020 | Isfahan | 79 | Sodium intake in 24 h | 9.54 | ND | ND |
| Mohammadifard et al. 47 | 2020 | Isfahan | 912 | Sodium intake in 24 h | 9.64 | 10.2 | 9.7 |
| Layeghiasl et al. 51 | 2020 | Yasuj | 166 | Spot urine sample | 14.34 | ND | ND |
| Ghaseminasab parizi et al. 48 | 2020 | Shiraz | 67 | Food Frequency Questionnaire | ND | ND | 8.42 |
Abbreviation: ND, no data.
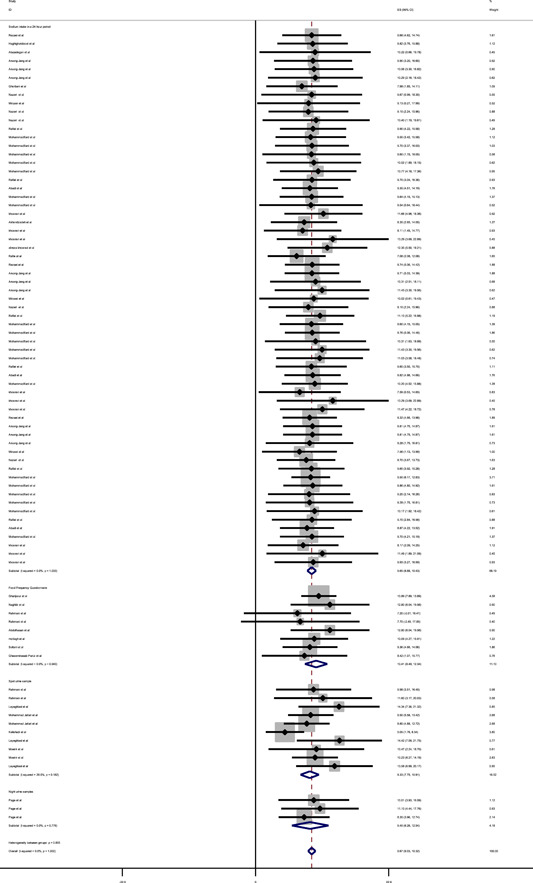
3.1. Overall mean daily salt intake
Based on the data set (24‐h urine, overnight, spot, and questionnaire) and fixed effects pooling model (I 2 = 0.0%), salt intake was estimated to be 9.674 g/day (95% CI, 9.033–10.316 g/day) for all ages (Table 2). Eliminating individual studies had no effect on the estimate. In addition, 21 studies estimated salt intake to be 9.655 g/day using a 24‐h urine collection (n = 31058) (95% CI, 8.878–10.432 g/day), 23 , 26 , 27 , 28 , 30 , 31 , 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 44 , 45 , 46 , 47 , 49 and five studies estimated salt intake to be 9.328 g/day using a stop urine sampling method (n = 1550) (95% CI, 7.749–10.907 g/day). 24 , 39 , 50 , 51 , 52 One study estimated salt intake to be 9.403 g/day using overnight urine samples collection (n = 166) (95% CI, 6.264–12.542 g/day) and six studies estimated salt intake to be 10.411 g/day using the Food Frequency Questionnaires (n = 1449) (95% CI, 8.485–12.337 g/day) 25 , 29 , 32 , 33 , 43 , 48 (Appendix A1).
Table 2.
Summary of fixed‐effects meta‐analysis of salt intake, Iran
| Subgroups | Salt g/day (Overall) | 95% CI | Number of studies |
|---|---|---|---|
| Measurement method | |||
| 24‐h urine collection | 9.65 | 8.88–10.43 | 20 |
| Spot urine sample | 9.33 | 7.75–10.91 | 5 |
| Overnight urine samples | 9.40 | 6.264–12.54 | 1 |
| Food Frequency Questionnaire | 10.41 | 8.49–12.34 | 6 |
| Sex | |||
| Men | 10.393 | 9.011–11.776 | 11 |
| Women | 9.517 | 8.417–10.617 | 16 |
| Both | 9.975 | 8.947–11.003 | 25 |
| Age group | |||
| Children | 5.66 | 2.915–8.414 | 2 |
| Adults | 9.905 | 9.245–10.565 | 30 |
| Area of residence | |||
| Urban | 10.053 | 9.055–11.051 | 30 |
| Rural | 10.206 | 6.677–13.736 | 3 |
A funnel plot was used to check publication bias (p values for Begg's and Egger's tests were 0.33 and 0.183, respectively), which ruled out the possibility of bias (Figure 2).
Figure 2.
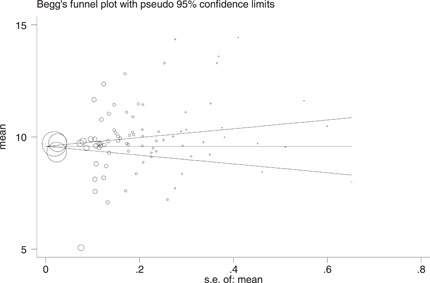
Publication bias for mean salt intake studies
3.2. Subgroup analysis
Furthermore, 11 studies determined that the weighted mean salt intake for men over the age of 18 in diverse cities was 10.393 g/day (95% CI, 9.011–11.776 g/day). 23 , 26 , 27 , 28 , 35 , 36 , 38 , 40 , 42 , 44 , 47 It was 9.52 g/day for women over 18 years (95% CI, 8.42–10.62 g/day) 23 , 26 , 27 , 28 , 29 , 35 , 36 , 38 , 40 , 42 , 43 , 44 , 47 , 48 , 52 and 5.664 g/day for children and adolescents (95% CI, 2.915–8.414 g/day) in 15 studies 39 , 41 (Appendix B1). Also, the review of available data shows that the mean salt intake of rural residents (10.2 g/day) is greater than that of urban residents (10.05 g/day). A 24‐h urine collection was used to assess the mean salt intake in all provinces and cities.
3.3. Geographical distribution
The current study indicated high salt intake prevalence from south to northwest Iran. Among Iranian provinces, Lorestan residents consumed the most salt (13.05 g per day), while Bushehr residents consumed the least salt intake (8.16 g per day) (Figure 3).
Figure 3.
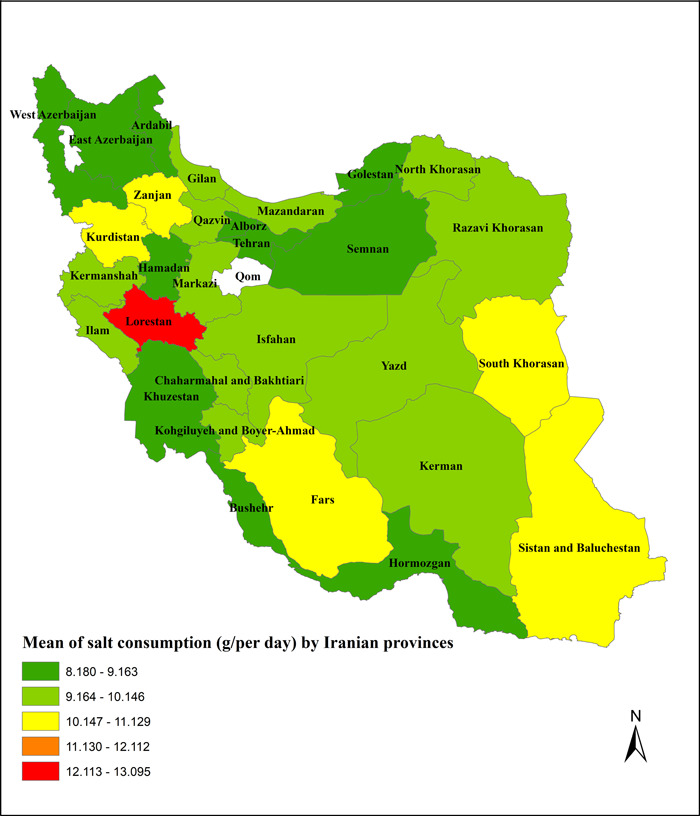
Mean salt intake (g/day) in provinces of Iran
4. DISCUSSION
In the current systematic review, the mean population salt intake from 1981 to 2020 in Iran was estimated to be 9.674 g/day, that is, 4.674 g/day more than WHO recommendation. Although the mean salt intake was determined using a variety of methodologies (24‐h, spot urine sampling, overnight urine samples, and Food Frequency Questionnaire), all of the data confirm that salt intake exceeds the WHO's NCDs prevention recommendation. Even at 9.4 g/day (overnight urine samples), the amount is twice the level recommended by the WHO. Two systematic review studies found that the mean salt intake in Australia was 9.6 g/day, 10.98 g/day 54 , 55 in India, and 10.49 and 12 g/day in Latin America and Asia, respectively. 56 , 57
The difference in mean salt intake between studies is predictable because they have used different measuring tools. While 24‐h urine collection is considered normal practice, there are reservations about its use due to the frequent sampling and high expense. As a result, various methods such as spot urine sampling, overnight urine samples, and planned urine tests have been examined to develop policies to reduce salt intake. 58 Because calculating salt intake using a 24‐h urine collection is beyond the capabilities of many countries, effective interventions to reduce salt consumption, promote health, and prevent disease can be made based on the results of alternative methods. 59 One of the key factors contributing to excessive salt intake is a lack of awareness about the source and amount of salt taken by individuals, 51 which has resulted in the highest mortality rate among nations with NCDs prevention measures. 60 As a result, these countries may reduce salt intake and, like other countries, meet their objective to reduce NCDs mortality by 2025 by designing and implementing effective interventions.
In this study, men's salt intake was assessed to be 10.393 g/day, greater than women's (9.517 g/day). A study similar to the current one compared men's (10.1 g/day) to women's (7.3 g/day) salt intake in Australia, as well as men's (9.61 g/day) and women's (6.61 g/day) salt intake in India. 54 , 55 The mean salt intake of Japanese and Slovenian men was higher than that of women. 25 , 61 According to the Canadian Public Health Association, more than 85% of males and 60% consume too much salt. 51 Since most studies have found that men consume more salt than women, this mismatch can be explained by low‐energy intake in women and gender differences. Furthermore, Iranian women consume more salt than women in other countries. This difference is most likely due to increased fast foods, canned products, and bread. 62 It may be argued that strategies and interventions based on community needs are required to minimize salt intake in Iran.
The mean salt intake in children was reported to be 5.66 g/day in this study; a study in Australian children assessed salt intake to be higher than 5.9 g/day. 63 In children, a maximum intake of 4.75 g/day (from <500 to <1900 mg/day) is recommended. 64 The significant amount of salt in children's meals is one of the causes behind their high‐salt consumption. 39 However, lowering salt intake is recognized as a national health priority in Iran and is recommended by the WHO. 14 , 65 Health authorities should evaluate the quantity of salt consumed by children as a priority for individual and public health.
In this study, rural adults consumed more salt than urban adults, which could be attributed to the inclusion of salt in rural meals, particularly among men, and a lack of information about the association between excessive salt intake and related diseases, particularly hypertension. 66 Furthermore, our estimations reveal that salt intake is high in our provinces and varies by province. One possible explanation is that the individuals in these regions have varying dietary patterns and food diversity due to Iran's wide size and diverse population groupings. 42 Therefore, planning and identifying alternate approaches for improving the community's food pattern can be advantageous, depending on the intake pattern in each region.
Estimating the range of variances in the amount of salt consumed in the studies, on the other hand, was predictable due to using different measuring methods. As previously stated, the amount of 9.4 (7.26–12.54) g/day is still more than the maximum amount recommended by WHO. The study's findings are diverse, which is unsurprising considering the diversity of the samples, the techniques used to determine the amount of salt consumed, and the study designs. As a result, multiple measures are necessary, including monitoring the population's salt intake, identifying the key sources of salt in the diet, and developing successful salt‐reduction initiatives.
Since 2009, the Ministry of Health and its affiliates have reduced population salt intake through various strategies, including product labeling and restrictions on certain goods, such as bread. 67 However, the effectiveness of these strategies is unknown, as population salt intake has not yet been reduced. Although salt intake has decreased over time, a review of the periodic study examining salt intake in a large sample of the Iranian population in 2016 showed that salt intake has remained constant. 42 Furthermore, the results of another study conducted in the same population over time reveal no decrease in salt consumption. 36 Several countries such as the United Kingdom, Finland, and Japan have lowered general population salt intake through public education, partnership with the food sector, novel salt formulations in foods, and executive rules. 7 The Japanese government began a sustained effort in the 1960s to reduce the mean salt intake from 13.5 to 10.6 g by 2010. Various interventions may be employed to reduce salt levels and achieve the desired results, including education, social involvement, mobile applications, advertising, alternative use, and tax increases. However, due to the small number of samples and lack of repetition in the same sample in all studies, the analysis of the available data cannot reveal the change in the quantity of salt consumed by the population over time.
According to the WHO, one of the most effective ways to reduce salt intake is to organize public campaigns and interventions aimed at increasing recipients' knowledge and assisting them in making healthy food choices, gradually reducing salt in factory food products, and increasing easy and cost‐effective access to healthy foods. 68 However, implementing health programs without proper planning and knowledge might waste resources. 69 As a result, research can be conducted to discover barriers and facilitators, predispose to change programs and increase effectiveness, and advocate for the adoption of salt reduction legislation. 70 Although lowering society's salt intake is challenging, multiple measures can achieve a 30% decrease in mean salt intake by 2025 and reduce NCDs mortality in Iran.
A common limitation among the selected studies was the inconsistent methodology they followed to ascertain sodium consumption, that is, some relied on 24 h urine samples. In contrast, others used spot samples, and others used Food Frequency Questionnaire for data collection. For this, we brought the results separately for each of the data collection methods. Additionally, they relied on differential equations to compute 24 h sodium consumption. Furthermore, the included studies did not study proportionate samples by age, gender, and living area (urban/rural), which should be considered when interpreting the current study results.
However, to have comparable results across the country, we suggest that related organizations (e.g., WHO or cardiology associations) should update standard guidelines for researchers who want to estimate sodium intake in the world.
5. CONCLUSION
According to this review, the Iranian population consumes salt over twice more than amount recommended by WHO. Based on the evidence of salt consumption, WHO recommends that all countries implement a salt reduction program on the basis of the evidence linking salt and CVDs. Iran, like many other countries, is working in this regard. It is evident that to reduce salt consumption, measures must be taken which take into account the sources of salt intake and the unique characteristics of each place. Individuals must also be educated on how to moderate their regular salt consumption. As a result, it is critical to investigate effective ways for reducing salt intake and to implement various strategies effectively; consequently, numerous heart attacks, strokes and other blood pressure‐related diseases could be avoided.
AUTHOR CONTRIBUTIONS
Sirous Pourkhajoei: Conceptualization; data curation; formal analysis; investigation; methodology; software; validation; visualization; writing – original draft; writing – review and editing. Vahid Yazdi‐Feyzabadi: Conceptualization; data curation; investigation; methodology; software; validation; visualization; writing – review and editing. Mohammadreza Amiresmaeili: Conceptualization; data curation; investigation; methodology; supervision; validation; visualization; writing – review and editing. Nouzar Nakhaee: Conceptualization; data curation; investigation; methodology; validation; visualization; writing – review and editing. Reza Goudarzi: Conceptualization; data curation; formal analysis; investigation; methodology; supervision; software; validation; visualization; writing – original draft; writing – review and editing.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author (Reza Goudarzi) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ACKNOWLEDGMENTS
No. 98001171 was approved by ethical committee of Kerman University of Medical Sciences. The Ethic approval Code is IR.KMU.REC.1399.294.
APPENDIX A.
Figure A1.
Summary of fixed‐effects meta‐analysis of salt intake, Iran, by measurement method
APPENDIX B.
Figure B1.
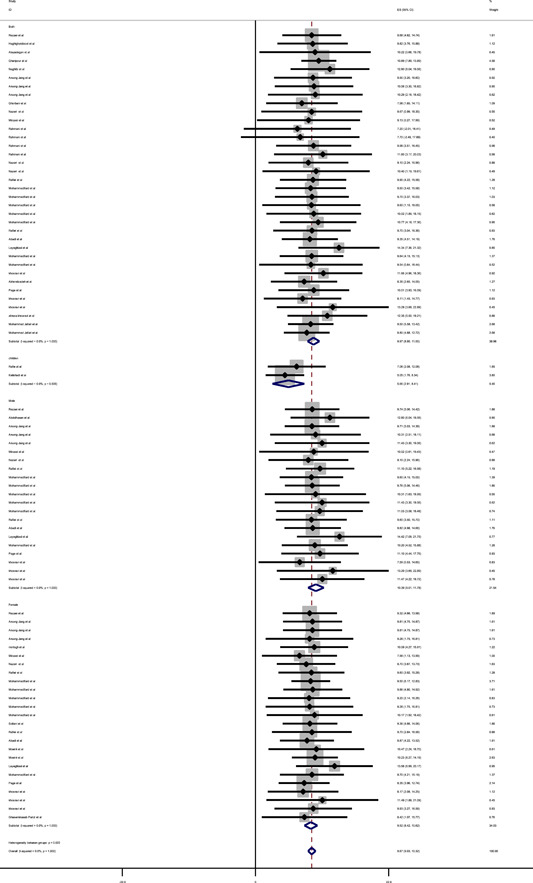
Summary of fixed‐effects meta‐analysis of salt intake, Iran, sex
Pourkhajoei S, Yazdi‐Feyzabadi V, Amiresmaeili M, Nakhaee N, Goudarzi R. Mean population salt intake in Iran: A systematic review and meta‐analysis. Health Sci Rep. 2022;5:e855. 10.1002/hsr2.855
DATA AVAILABILITY STATEMENT
The data are available upon request to the corresponding author after signing appropriate documents in line with ethical application and the decision of the Ethics Committee.
REFERENCES
- 1. He FJ, Li J, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta‐analysis of randomised trials. BMJ. 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 2. O'donnell M, Mente A, Rangarajan S, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371(7):612‐623. [DOI] [PubMed] [Google Scholar]
- 3. Alwan A. Global Status Report on Noncommunicable Diseases 2010. World Health Organization; 2011. [Google Scholar]
- 4. McGuire S. Institute of Medicine. 2013. Sodium Intake in populations: assessment of evidence. Washington, DC: The National Academies Press, 2013. Adv Nutr. 2014;5(1):19‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kunkulberga D, Murniece E, eds., Salt and bread: Latvia's experience. Proceedings of the Latvian Academy of Sciences. De Gruyter; 2013.
- 6. Mozaffarian D, Fahimi S, Singh GM, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371(7):624‐634. [DOI] [PubMed] [Google Scholar]
- 7. He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009;23(6):363‐384. [DOI] [PubMed] [Google Scholar]
- 8. Sánchez G, Peña L, Varea S, et al. Conocimientos, percepciones y comportamientos relacionados con el consumo de sal, la salud y el etiquetado nutricional en Argentina, Costa Rica y Ecuador. Rev Panam Salud Pública. 2012;32:259‐264. [DOI] [PubMed] [Google Scholar]
- 9. Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta‐analyses. BMJ. 2013;346:f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Provincial, Territorial Ministers of Health . Reducing the Sodium Intake of Canadians: A Provincial and Territorial Report on Progress and Recommendations for Future Action. Provincial and Territorial Ministers of Health (Canada); 2012.
- 11. Almedawar MM, Nasreddine L, Olabi A, et al. Sodium intake reduction efforts in Lebanon. Cardiovasc Diagn Ther. 2015;5(3):178‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Israr T, Rakha A, Sohail M, Rashid S, Shehzad A. Salt reduction in baked products: strategies and constraints. Trends Food Sci Technol. 2016;51:98‐105. [Google Scholar]
- 13. Kloss L, Meyer JD, Graeve L, Vetter W. Sodium intake and its reduction by food reformulation in the European Union—a review. NFS J. 2015;1:9‐19. [Google Scholar]
- 14. World Health Organization . Guideline: Sodium Intake for Adults and Children. World Health Organization; 2012. [PubMed]
- 15. Ronto R, Wu JH, Singh GM. The global nutrition transition: trends, disease burdens and policy interventions. Public Health Nutr. 2018;21(12):2267‐2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. He FJ, MacGregor GA. How far should salt intake be reduced. Hypertension. 2003;42(6):1093‐1099. [DOI] [PubMed] [Google Scholar]
- 17. Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370(9604):2044‐2053. [DOI] [PubMed] [Google Scholar]
- 18. Ortega RM, López‐Sobaler AM, Ballesteros JM, et al. Estimation of salt intake by 24 h urinary sodium excretion in a representative sample of Spanish adults. Br J Nutr. 2011;105(5):787‐794. [DOI] [PubMed] [Google Scholar]
- 19. Mohammadifard N, Fahimi S, Khosravi A, et al Advocacy strategies and action plans for reducing salt intake in Iran. Report. 2012. [PubMed]
- 20. National Heart L, Institute B . Study Quality Assessment Tools. 2019. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- 21. Kamel Boulos MN, Geraghty EM. Geographical Tracking and Mapping of Coronavirus Disease COVID‐19/Severe Acute Respiratory Syndrome Coronavirus 2 (SARS‐CoV‐2) Epidemic and Associated Events Around the World: How 21st Century GIS Technologies are Supporting the Global Fight against Outbreaks and Epidemics. BioMed Central; 2020:1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Page LB, Vandevert D, Nader K, Lubin N, Page JR. Blood pressure of Qash'qai pastoral nomads in Iran in relation to culture, diet, and body form. Epidemiology of Arterial Blood Pressure. Springer; 1980:401‐420. [DOI] [PubMed] [Google Scholar]
- 23. Khosravi A, Kelishadi R, Sarrafzadegan N, et al. Impact of a community‐based lifestyle intervention program on blood pressure and salt intake of normotensive adult population in a developing country. J Res Med Sci. 2012;17(3):235‐241. [PMC free article] [PubMed] [Google Scholar]
- 24. Rahmani M, Koohkan A, Allahverdian S, Hedayati M. Comparison of dietary iodine intake and urinary excretion in urban and rural households of Ilam in 2000. Iranian J Endocrinol Metab. 2000;2(1):31‐37. [Google Scholar]
- 25. Azizi F, Rahmani M, Allahverdian S, Hedayati M. Effects of salted food consumption on urinary iodine and thyroid function tests in two provinces in the Islamic Republic of Iran. East Mediterr Health J. 2001. 2001;7(1‐2):115‐120. [PubMed] [Google Scholar]
- 26. Rafiei M, Beshtam M, Sarafzadegan N, et al. 24‐hour urinary sodium and potassium levels and their relationship with blood pressure in adults in Isfahan (1998‐99). J School Med. 2002;60(5):406‐415(in Persian). [Google Scholar]
- 27. Rafiei M, Boshtam M, Sarraf‐Zadegan N, Seirafian S. The relation between salt intake and blood pressure among Iranians. Kuwait Med J. 2008;40(3):191‐195. [Google Scholar]
- 28. Nazeri P, Mirmiran P, Mehrabi Y, Hedayati M, Delshad H, Azizi F. Evaluation of iodine nutritional status in Tehran, Iran: iodine deficiency within iodine sufficiency. Thyroid. 2010;20(12):1399‐1406. [DOI] [PubMed] [Google Scholar]
- 29. Motlagh Z, Mazloomy S, Mozaffari Khosravi M, Morowatisharifabad M, Askarshahi H. Salt intake among women refer to Medical Health Centers, Yazd, Iran, 2011. J Shahid Sadoughi Univ Med Sci. 2011;19(4):550‐560(in Persian) [Google Scholar]
- 30. Nazeri P, Mirmiran P, Delshad H, Hedayati M, Azizi F. Evaluation of urinary iodine concentration and iodine content of households salt in south of Tehran. Iran J Endocrinol Metab. 2010;12(3):294‐299 (in Persian). [Google Scholar]
- 31. Nazeri P, Mirmiran P, Asghari G, et al. Differences between subjects with sufficient and deficient urinary iodine in an area of iodine sufficiency. J Endocrinol Invest. 2011;34(9):e302‐e307. [DOI] [PubMed] [Google Scholar]
- 32. Atazadegan M, Rahmdel S, Abdollahzadeh S, Mazloomi S. Estimation of the dietary intake of table salt by the population of shiraz(IRAN) using duplicate portion sampling. Nutr Food Sci Res. 2014; 21(1):81‐84. [Google Scholar]
- 33. Naghibi SA, Yahyazadeh R, Yazdani Cherati J. Knowledge, attitude referred to health centers on salt intake. J Mazandaran Univ Med Sci. 2012;22(95):99‐104. [Google Scholar]
- 34. Haghighatdoost F, Sarrafzadegan N, Khosravi A, et al. Is the association between salt intake and blood pressure mediated by body mass index and central adiposity. Arch Iran Med. 2013;16(30‐):167‐171. [PubMed] [Google Scholar]
- 35. Arsang‐Jang S, Mansourian M, Mohammadifard N, et al. Temporal trend analysis of stroke and salt intake: a 15‐year population‐based study. Nutr Neurosci. 2019;24:1‐11. [DOI] [PubMed] [Google Scholar]
- 36. Mohammadifard N, Khosravi A, Salas‐Salvadó J, et al. Trend of salt intake measured by 24‐hour urine collection samples among Iranian adults population between 1998 and 2013: The Isfahan salt study. Nutr Metab Cardiovasc Dis. 2019;29(12):1323‐1329. [DOI] [PubMed] [Google Scholar]
- 37. Gharipour M, Khosravi A, Mohamadifard N, Gharipour A, Sarrafzadegan N. The value of salt intake to predict metabolic syndrome: a population base study In Iran. Nutr Food Sci Res. 2014;22(8):45‐67. [Google Scholar]
- 38. Mirzaei M, Soltani M, Namayandeh M, GharahiGhehi N. Sodium and potassium intake of urban dwellers: nothing changed in Yazd, Iran. J Health Popul Nutr. 2014;32(1):111. [PMC free article] [PubMed] [Google Scholar]
- 39. Kelishadi R, Gheisari A, Zare N, Farajian S, Shariatinejad K. Salt intake and the association with blood pressure in young Iranian children: first report from the Middle East and north Africa. Int J Prev Med. 2013;4(4):475‐483. [PMC free article] [PubMed] [Google Scholar]
- 40. Mohammadifard N, Khaledifar A, Khosravi A, et al. Dietary sodium and potassium intake and their association with blood pressure in a non‐hypertensive Iranian adult population: Isfahan salt study. Nutr Diet. 2017;74(3):275‐282. [DOI] [PubMed] [Google Scholar]
- 41. Rafie N, Mohammadifard N, Khosravi A, Feizi A, Safavi SM. Relationship of sodium intake with obesity among Iranian children and adolescents. ARYA Atheroscler. 2017;13(1):1. [PMC free article] [PubMed] [Google Scholar]
- 42. Rezaei S, Mahmoudi Z, Sheidaei A, et al. Salt intake among Iranian population: the first national report on salt intake in Iran. J Hypertens. 2018;36(12):2380‐2389. [DOI] [PubMed] [Google Scholar]
- 43. Soltani S, Vafa M, Zairi F, Sarbakhsh P, Niroumand M, Najarzadeh A. Investigating the relationship between sodium intake and some bone health indicators in retired female employees of Yazd province. Razi J Med Sci. 2017;24(156):9‐21 (in Persian). [Google Scholar]
- 44. Abadi AD‐R, Mozaffari‐Khosravi H, Nemayandeh M, Soltani MH, Mirzaei M, Abargouei AS. Sodium status and its association with overweight and obesity in adults living in Yazd, Iran. J Nutr Food Security. 2019;4(3):191‐199. [Google Scholar]
- 45. Khosravi A, Mohammadifard N, Gharipour M, et al. Low correlation between morning spot and 24‐hour urine samples for estimating sodium intake in an Iranian population: Isfahan Salt Study. Int J Vitam Nutr Res. 2019;89:185‐191. [DOI] [PubMed] [Google Scholar]
- 46. Mohammadifard N, Marateb H, Mansourian M, et al. Can methods based on spot urine samples be used to estimate average population 24 h sodium excretion? Results from the Isfahan Salt Study. Public Health Nutr. 2020;23(2):202‐213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mohammadifard N, Haghighatdoost F, Nouri F, Khosravi A, Sarrafzadegan N. Is urinary sodium excretion related to anthropometric indicators of adiposity in adults. J Res Med Sci. 2020;25:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ghaseminasab Parizi M, Fararouei M, Jafarian F, et al. Comparison of fat and sodium intake among female students of Shiraz University of Medical Sciences living at home or dormitories. Int J Nutr Sci. 2020;5(1):38‐42. [Google Scholar]
- 49. Akhondzadeh K, Najafi Ghezeljeh T, Haghani H. The effect of the education program on the adherence intention to the dietary sodium restriction and the amount of sodium intake in patients with chronic heart failure. Iran Red Crescent Med J. 2018;20(S1):e12925. [Google Scholar]
- 50. Jafari M, Mohammadi M, Ghazizadeh H, Nakhaee N. Feasibility and outcome of reducing salt in bread: a community trial in Southern Iran. Glob J Health Sci. 2016;8(12):163. [Google Scholar]
- 51. Layeghiasl M, Malekzadeh J, Shams M, Maleki M. Using social marketing to reduce salt intake in Iran. Front Public Health. 2020;8:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Moeini M, Hosseini H, Maleki F, Sharifi Rad G. The effect of an educational plan based on the health belief model on salt consumption of the women at hypertension risk. Nurs Midwifery J. 2014;12(2):94‐100. [Google Scholar]
- 53. Ghorbani S, Hatamian H, Mahmoudzadeh A, et al. The association between salt and potassium intake with multiple sclerosis. Caspian J Neurol Sci. 2019;5(1):23‐27. [Google Scholar]
- 54. Land MA, Neal BC, Johnson C, Nowson CA, Margerison C, Petersen KS. Salt consumption by Australian adults: a systematic review and meta‐analysis. Med J Aust. 2018;208(2):75‐81. [DOI] [PubMed] [Google Scholar]
- 55. Johnson C, Praveen D, Pope A, et al. Mean population salt consumption in India: a systematic review. J Hypertens. 2017;35(1):3‐9. [DOI] [PubMed] [Google Scholar]
- 56. Carrillo‐Larco RM, Bernabe‐Ortiz A. Sodium and salt consumption in Latin America and the Caribbean: a systematic‐review and meta‐analysis of population‐based studies and surveys. Nutrients. 2020;12(2):556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Powles J, Fahimi S, Micha R, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3(12):e003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ji C, Sykes L, Paul C, et al. Systematic review of studies comparing 24‐hour and spot urine collections for estimating population salt intake. Rev Panam Salud Públ. 2012;32:307‐315. [DOI] [PubMed] [Google Scholar]
- 59. Huang L, Crino M, Wu JH, et al. Mean population salt intake estimated from 24‐h urine samples and spot urine samples: a systematic review and meta‐analysis. Int J Epidemiol. 2016;45(1):239‐250. [DOI] [PubMed] [Google Scholar]
- 60. Loloei S, Pouraram H, Majdzadeh R, Takian A, Goshtaei M, Djazayery A. Policy analysis of salt reduction in bread in Iran. AIMS Public Health. 2019;6(4):534‐545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ribič CH, Zakotnik JM, Vertnik L, Vegnuti M, Cappuccio FP. Salt intake of the Slovene population assessed by 24 h urinary sodium excretion. Public Health Nutr. 2010;13(11):1803‐1809. [DOI] [PubMed] [Google Scholar]
- 62. Beard TC, Hornsby H, Dwyer T, Woodward DR, Ball PJ, von Witt RJ. The Hobart Salt Study 1995: few meet national sodium intake target. Med J Aust. 1997;166(8):404‐407. [DOI] [PubMed] [Google Scholar]
- 63. Grimes CA, Riddell LJ, Campbell KJ, He FJ, Nowson CA. 24‐h urinary sodium excretion is associated with obesity in a cross‐sectional sample of Australian schoolchildren. Br J Nutr. 2016;115(6):1071‐1079. [DOI] [PubMed] [Google Scholar]
- 64. Gidding SS, Dennison BA, Birch LL, et al. Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics. 2006;117(2):544‐559. [DOI] [PubMed] [Google Scholar]
- 65. Fahimi S, Pharoah P. Reducing salt intake in Iran: priorities and challenges. Arch Iran Med. 2012;15(2):110‐112. [PubMed] [Google Scholar]
- 66. Reyhani P, Azabdaftari F, Ebrahimi‐Mamagani M, Asghari‐Jafarabadi M, Shokrvash B. The predictors of high dietary salt intake among hypertensive patients in Iran. Int J Hypertens. 2020;2020:6748696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. World Health Organization . Creating an Enabling Environment for Population‐Based Salt Reduction Strategies: Report of a Joint Technical Meeting Held by WHO and the Food Standards Agency, United Kingdom, July 2010; 2010.
- 68. World Health Organization . Reducing Salt Intake in Populations: Report of a WHO Forum and Technical Meeting, 5–7 October 2006, Paris, France; 2007.
- 69. Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38(3):791‐813. [DOI] [PubMed] [Google Scholar]
- 70. Cappuccio FP, Capewell S, Lincoln P, McPherson K. Policy options to reduce population salt intake. BMJ. 2011;343:d4995. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available upon request to the corresponding author after signing appropriate documents in line with ethical application and the decision of the Ethics Committee.


