Highlights
-
•
The joint associations between steps volume and intensity with health are unknown.
-
•
Increasing 1000 steps/day yielded lower hospitalization (5%) and mortality (13%).
-
•
Every 1 step/min increment reduced hospitalization (5%) and mortality (11%) risk.
-
•
These associations appear to be linear.
-
•
Increasing step volume and intensity jointly may result in larger health gains.
Keywords: Aging, Follow-up, Objective, Physical activity, Walking
Abstract
Purpose
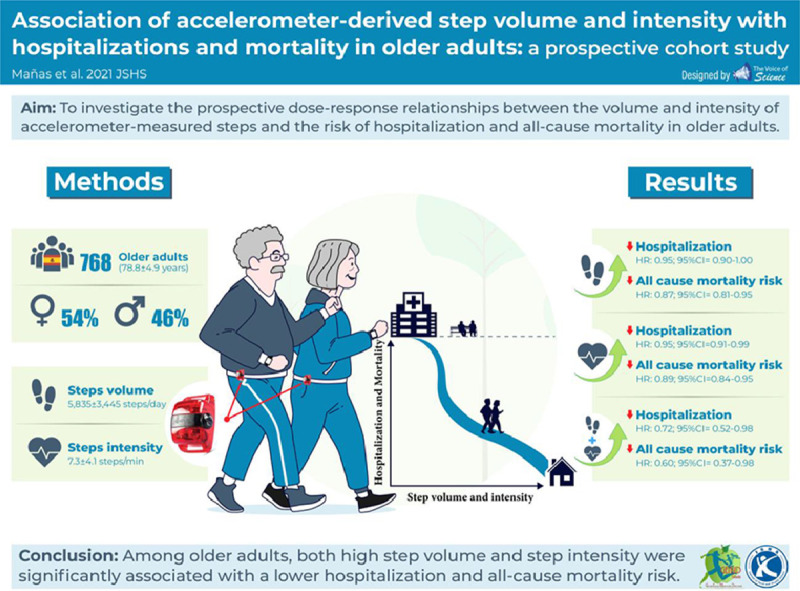
This study aimed to examine the associations of accelerometer-derived steps volume and intensity with hospitalizations and all-cause mortality in older adults.
Methods
This prospective cohort study involved 768 community-dwelling Spanish older adults (78.8 ± 4.9 years, mean ± SD; 53.9% females) from the Toledo Study for Healthy Aging (2012–2017). The number of steps per day and step cadence (steps/min) were derived from a hip-mounted accelerometer worn for at least 4 days at baseline. Participants were followed-up over a mean period of 3.1 years for hospitalization and 5.7 years for all-cause mortality. Cox proportional hazards regression models were used to estimate the individual and joint associations between daily steps and stepping intensity with hospitalizations and all-cause mortality.
Results
Included participants walked 5835 ± 3445 steps/day with an intensity of 7.3 ± 4.1 steps/min. After adjusting for age, sex, body mass index (BMI), education, income, marital status and comorbidities, higher step count (hazard ratio (HR) = 0.95, 95% confidence interval (95%CI: 0.90–1.00, and HR = 0.87, 95%CI: 0.81–0.95 per additional 1000 steps) and higher step intensity (HR = 0.95, 95%CI: 0.91–0.99, and HR = 0.89, 95%CI: 0.84–0.95 per each additional step/min) were associated with fewer hospitalizations and all-cause mortality risk, respectively. Compared to the group having low step volume and intensity, individuals in the group having high step volume and intensity had a lower risk of hospitalization (HR = 0.72, 95%CI: 0.52–0.98) and all-cause mortality (HR = 0.60, 95%CI: 0.37–0.98).
Conclusion
Among older adults, both high step volume and step intensity were significantly associated with lower hospitalization and all-cause mortality risk. Increasing step volume and intensity may benefit older people.
Graphical abstract
1. Introduction
Walking is ubiquitous to daily life activities. Walking is the most common physical activity, particularly in older people.1,2 Walking is free, does not require a high level of fitness or special equipment, and can be done almost anywhere, which makes it a very practical activity.3 In addition, the development of wearable devices, such as smartphones or pedometers, has enabled the monitoring of walking activity (e.g., the number of steps) in a simple and accessible manner, which makes walking an attractive and feasible target for improving the overall health of the population.
Step volume (i.e., number of steps in a given day) has been associated with a lower incidence of cardiovascular events, hypertension, diabetes, and obesity risk.4, 5, 6, 7 A greater number of steps has also been linked to lower mortality risk, although the evidence is limited because of the use of self-reported walking measures. For example, some studies, such as the study by Dwyer et al.,8 have shown an inverse and linear dose–response relationship between pedometer-measured steps per day and all-cause mortality in individuals between the ages of 50 years and 80 years. Hansen et al.9 observed a nonlinear dose–response pattern between daily steps and subsequent reduction in risk of all-cause mortality in a predominantly healthy sample of middle-aged adults. Lee et al.10 found that 4363 daily steps were significantly associated with lower mortality rates compared to the referent (i.e., 2718 steps/day) among older women in the United States. In contrast, few previous studies have assessed the associations between step intensity and health. Lee et al.10 reported that the effect of step intensity disappears after controlling for total steps per day. Similar results were recently reported in a nationally representative cohort of U.S. adults in the United States who were 40 years off age or older.11
Most of the previous studies included middle-aged adults in their analyses, which may underestimate the relationship between steps and hospitalizations and all-cause mortality in older populations.8,9,11 Furthermore, none of these studies have investigated the combined association of volume and intensity of steps with the risk of premature mortality,8, 9, 10 and none of them have explored the dose-response of these associations in other relevant endpoints, such as hospitalization. Additionally, the 2018 Physical Activity Guidelines Advisory Committee revealed the need for more research on the association between steps and health outcomes.12 Detecting the components of healthy aging that can be translated into intuitive and easily quantifiable recommendations is essential in order for more feasible and tailored health policies and programs to be developed. To this end, the aim of this study was to describe the prospective dose-response relationships between the volume (steps/day) and intensity (steps/min) of accelerometer-measured steps and the risk of hospitalization and all-cause mortality in a population-based cohort of community-dwelling older adults.
2. Methods
2.1. Study design and participants
Data were drawn from the Toledo Study for Healthy Aging (TSHA), the details of which have been reported elsewhere.13 Briefly, the TSHA is a population-based prospective cohort study originally conceived to explore the determinants and consequences of aging and frailty in older adults from Toledo, Spain. In the present study, we used data from participants with valid accelerometer records from the second (2012–2014) and third (2015–2017) TSHA waves and available hospitalization and mortality information at the censoring time. Signed informed consent was obtained from all participants prior to involvement in the study. The study was approved by the Clinical Research Ethics Committee of the Toledo Hospital Complex and was conducted according to the ethical standards defined in the 1964 Declaration of Helsinki.
2.2. Measurements
2.2.1. Stepping volume and intensity
Stepping volume and intensity were measured by accelerometry (ActiTrainer and ActiGraph wGT3X-BT; ActiGraph, Pensacola, FL, USA), as previously described.14,15 In brief, all participants were asked to wear the accelerometer on the left hip during waking hours of 1 whole week, with the exception of water activities. Monitors were set to record accelerometer counts in 1-min epochs. Nonwear time was defined as 60 consecutive minutes or longer of 0 intensity counts, with no more than 2 min of counts between 0 and 100.16 The study included data only from participants with at least 4 valid days with 8 or more hours per day of wear time.17,18 Steps were determined using the manufacturer's step algorithm. To calculate step volume, we summed steps across all compliant days and divided this by the number of compliant days to obtain mean steps per day. For step intensity, the total step count was divided by the total valid minutes of accelerometer wear time to obtain steps per minute throughout the measurement period.
2.2.2. Hospitalization
Dates of hospitalizations were ascertained by reviewing the Toledo Hospital Complex records and were defined as the occurrence of a first admission to the hospital during follow-up through December 2016. The mean follow-up for hospitalization was 3.13 years (ranged 0.02–5.24 years).
2.2.3. Mortality
Vital status and dates of death were ascertained through data provided by the Spanish National Death Index (Ministry of Health, Consumer Affairs and Social Welfare). Participants were followed-up to death or March 2019, whichever came first. Mean follow-up for mortality was 5.74 years (ranged 1.30–7.48 years).
2.2.4. Confounding variables
Covariates were selected based on the literature and the biological plausibility for confounding the main associations of interest.9,11,19 Participants self-reported their age and sex. Education (no studies, primary school completed, secondary school completed, or more), marital status (single, married/living together, widowed, or divorced/separated), and income (coded into 3 categories ranging from any income to EUR 3000/month) were also self-reported in face-to-face interviews. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). The Charlson Comorbidity Index was used to account for comorbidity status of participants in the study.20 Diseases included in this index and their weighting are myocardial infarction, congestive heart failure, peripheral vascular disease, dementia, cerebrovascular disease, chronic lung disease, connective tissue disease, ulcer, chronic liver disease, and diabetes (Weight 1); hemiplegia, moderate or severe kidney disease, diabetes with complication, tumor, leukemia, and lymphoma (Weight 2); moderate or severe liver disease (Weight 3); metastatic solid tumor and acquired immunodeficiency syndrome (Weight 6).
2.2.5. Analytical approach
Summary statistics were used to describe variables of interest. Mean ± SD and frequency (percentage) are provided for continuous and categorical variables, respectively. Descriptive variables were compared between participants retained and participants not retained due to invalid data from accelerometry or missing variables, with an independent t test or χ2 test used for continuous and categorical variables, respectively.
Cox proportional hazards regression models were used to estimate hazard ratios (HR) and 95% confidence intervals (95%CIs) for the associations between daily steps and step intensity with hospitalizations and all-cause mortality. Two separate models were fitted for each of the outcomes (i.e., 1 set of models with steps per min as the main predictor of interest and a separate set of models with number of daily steps as the main predictor of interest). Initial models (Model 1) estimated HRs of hospitalizations and mortality, adjusting for accelerometer wear time. Model 2 additionally adjusted for potential confounders: age, sex, and BMI. In Model 3, sociodemographic variables such as education, income and marital status were also included as covariates. Given the close relationship among hospitalization, mortality and comorbidity, we additionally adjusted for comorbidity status in Model 4. For all regression models related to step intensity, the accelerometer wear-time covariate was removed.
Participants were also categorized into 4 mutually exclusive behavioral groups in order to investigate the joint associations between step volume and step intensity with the risk of hospitalization and all-cause mortality. Categories for low step volume (i.e., at or below the 50th percentile) and intensity (i.e., at or below the 50th percentile) vs. high step volume (i.e., above the 50th percentile) and intensity (i.e., above the 50th percentile) were compared solely because they were the only categories that presented a large enough sample size (356 vs. 355 participants, respectively). The data were analyzed using the same models as described above (excluding accelerometer wear time).
In addition, sensitivity analyses were conducted. These analyses excluded participants who experienced events within the first 2 years of follow-up.21
Statistical analyses were conducted using R software (R project Version 3.5.1; Foundation for Statistical Computing, Vienna, Austria). Significance levels were set at p < 0.05.
3. Results
After removing 103 individuals who had invalid accelerometer data, the final sample was made up of 768 individuals (n corresponding to Model 1 for mortality). Participants included in this analysis had an age of 78.8 ± 4.9 years, mean ± SD, and 53.9% were women. They had a higher educational level and greater comorbidities than those excluded from the study. The baseline characteristics of included and excluded participants are displayed in Table 1. In the analytical sample, the accelerometer was worn for 12.8 ± 1.4 h/day, during which the participants performed 5835 ± 3445 steps/day with intensity of 7.3 ± 4.1 steps/min.
Table 1.
Comparison of characteristics between those included and excluded from the study (mean ± SD or n (%)).
| Included sample (n = 768) | Excluded sample (n = 103) | p | |
|---|---|---|---|
| Age (year) | 78.8 ± 4.9 | 77.4 ± 5.6 | 0.065 |
| Sex | 0.309 | ||
| Male | 354 (46.1) | 42 (40.8) | |
| Female | 414 (53.9) | 61 (59.2) | |
| BMI (kg/m2) | 30.3 ± 4.8 | 30.7 ± 5.5 | 0.558 |
| Education | <0.001 | ||
| None | 251 (32.7) | 70 (68.0) | |
| Primary school | 240 (31.3) | 24 (23.3) | |
| Secondary or more | 273 (35.5) | 7 (6.8) | |
| Missing | 4 (0.5) | 2 (1.9) | |
| Income | 0.620 | ||
| Low | 368 (47.9) | 50 (48.5) | |
| Medium | 298 (38.8) | 34 (33.0) | |
| High | 56 (7.3) | 9 (8.8) | |
| Missing | 46 (6.0) | 10 (9.7) | |
| Marital status | 0.225 | ||
| Single | 42 (5.5) | 1 (1.0) | |
| Married | 540 (70.3) | 73 (70.9) | |
| Widower | 170 (22.1) | 26 (25.2) | |
| Separated/divorced | 12 (1.6) | 1 (1.0) | |
| Missing | 4 (0.5) | 2 (1.9) | |
| Charlson comorbidity indexa | 2.1 ± 1.8 | 1.8 ± 1.4 | 0.045 |
| Accelerometry | |||
| Valid wear time (min) | 786.3 ± 82.4 | — | |
| Steps/day | 5835 ± 3445 | — | |
| Steps/min | 7.3 ± 4.1 | — |
Note: Boldface type indicates statistical significance (p < 0.05).
Quantifies an individual's burden of disease with a weighted composite score in which the higher the score, the more comorbidity. Three or more points is considered high risk of hospitalization and mortality.36
Abbreviation: BMI = body mass index.
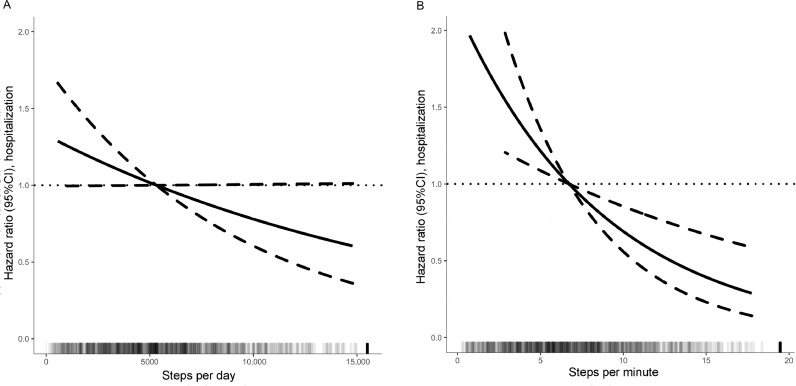
A total of 201 participants out of 760 participants (26.4% of the analytical sample) were hospitalized during a mean follow-up of 3.1 years. Associations between total steps and intensity of steps with risk for hospitalization are shown in Table 2. Higher daily step-count and higher step intensity were both associated with lower risk of hospitalization (HR = 0.94, 95%CI: 0.89–0.99 per additional 1000 step counts, and HR = 0.94, 95%CI: 0.90–0.98 for an additional steps/min, respectively, for Model 1). Adjustments for age, sex, BMI, and sociodemographic confounders did not alter any associations (Model 2 and Model 3). For the most complete model that also adjusted for comorbidity status (Model 4), results were similar, although confidence intervals overlapped. Fig. 1A and Fig. 1B display the dose–response relationship between hospitalizations and step volume and intensity, respectively. We observed a linear dose–response association between daily steps and step intensity with risk of hospitalization. Compared with the referent, a 50% higher total step count was associated with an approximately 12% lower risk.
Table 2.
Hazard ratios and 95%CIs for hospitalization and all-cause mortality by step volume and step intensity.
| Hazard ratio (95%CI) |
||||
|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | Model 4d | |
| Hospitalization | ||||
| Steps/day (per additional 1000 steps) | 0.94 (0.89–0.99)⁎ | 0.95 (0.90–1.00)⁎ | 0.95 (0.90–1.00)⁎ | 0.95 (0.90–1.00) |
| Steps/min | 0.94 (0.90–0.98)⁎ | 0.95 (0.91–0.99)⁎ | 0.95 (0.91–0.99)⁎ | 0.95 (0.91–0.99)⁎ |
| All-cause mortality | ||||
| Steps/day (per additional 1000 steps) | 0.88 (0.81–0.95)⁎ | 0.87 (0.81–0.95)⁎ | 0.87 (0.80–0.94)⁎ | 0.87 (0.81–0.95)⁎ |
| Steps/min | 0.89 (0.84–0.95)⁎ | 0.89 (0.84–0.95)⁎ | 0.89 (0.83–0.95)⁎ | 0.89 (0.84–0.95)⁎ |
Notes: The estimate reported is the effect on either mortality or hospitalization for every unit increase in the predictor of interest. The reference is the median value for each predictor of interest (5310 for daily steps and 6.7 for steps/min).
Abbreviations: 95%CI = 95% confidence interval; BMI = body mass index.
Adjusted for accelerometer wear time (covariate excluded in the steps/min models).
Adjusted for Model 1 variables plus age, sex, and BMI.
Adjusted for Model 2 variables plus education, income, and marital status.
Adjusted for Model 3 variables plus comorbidities.
Significant at p < 0.05.
Fig. 1.
Dose–response relationship between step volume, step intensity, and risk of hospitalization. (A) Steps per day and (B) Steps per minute. Hazard ratios (solidline) with 95%CIs (dotted lines) for the most adjusted model (i.e., Model 4). Exposures are modelled in its continuous form and use the median as a reference (5310 for daily steps (A); and 6.7 for steps/min (B)). Darker colors in the lower bars represent a higher sample clustering (top-coded at the 99th percentile). 95%CI = 95% confidence interval.
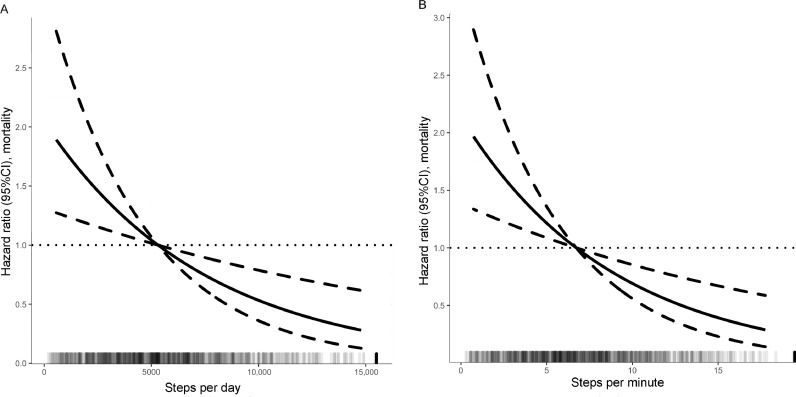
A total of 89 deaths (11.6% of the analytical sample) occurred during an average follow-up of 5.7 years. Table 2 also provides the results of the association between step volume and step intensity and all-cause mortality, with the same levels of adjustment as above. Higher numbers of daily steps and higher step intensity were associated with significantly lower mortality. Hazards ratios for Model 1 were HR = 0.88, 95%CI: 0.81–0.95 for every additional 1000 steps/day, and HR = 0.89, 95%CI: 0.84–0.95 for each additional steps/min in intensity. Further adjustments for potential confounders did not attenuate the observed associations (Models 2, 3, and 4). The dose–response relationship between all-cause mortality and step volume and intensity are shown in Fig. 2A and Fig. 2B, respectively. A linear dose–response association between all-cause mortality and daily steps and step intensity was detected. Compared with the referent, a 50% higher total step count was associated with an approximately 25% lower risk.
Fig. 2.
Dose-response relationship between step volume, step intensity and all-cause mortality. (A) Steps per day and (B) Steps per minute. Hazard ratios (solid line) with 95%CIs (dotted lines) for the most-adjusted model (i.e., Model 4). Exposures are modeled in continuous form and use the median as a reference (5310 for daily steps (A); and 6.7 for steps/min (B)). Darker colors in the lower bars represent a higher sample clustering (top-coded at 99th percentile). 95%CI = 95% confidence interval.
Next, we examined the joint associations between step volume and step intensity with the risk of hospitalization and all-cause mortality (Table 3). The group having high step volume and intensity (8627 ± 2526 steps/day and 10.7 ± 3.0 steps/min, respectively) had a significantly lower risk of hospitalization and all-cause mortality by 32% and 41%, respectively, compared to the reference group (the group having low step volume and intensity) (3050 ± 1361 steps/day and 3.9 ± 1.7 steps/min, respectively). Results were materially unchanged following adjustment for sex, age, BMI, sociodemographic factors, and comorbidity (Models 2, 3, and 4).
Table 3.
Joint associations between step volume and step intensity with the risk of hospitalization and all-cause mortality.
| Hazard ratio (95%CI); Low vs. high step volume and intensity |
|||||
|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | Model 4d | ||
| Hospitalization (n = 711) | 1 (Reference) | 0.68 (0.51–0.90)* | 0.73 (0.53–0.99)* | 0.71 (0.52–0.98)* | 0.72 (0.52–0.98)* |
| All-cause mortality (n = 719) | 1 (Reference) | 0.59 (0.38–0.92)* | 0.60 (0.37–0.96)* | 0.59 (0.36–0.96)* | 0.60 (0.37–0.98)* |
* Significant at p < 0.05.
Abbreviations: 95%CI = 95% confidence interval; BMI = body mass index.
Raw model.
Adjusted for Model 1 variables plus age, sex, and BMI.
Adjusted for Model 2 variables plus education, income, and marital status.
Adjusted for Model 3 variables plus comorbidities.
When these analyses were re-run excluding participants with a follow-up periods of less than 2 years, the results remained consistent (Supplementary Table 1).
4. Discussion
In this study, we observed a linear dose–response relationship between daily steps and step intensity with the risk of hospitalization and all-cause mortality in older adults. Compared with individuals who took fewer steps and at a lower intensities, those with higher step volumes and intensities had a 28% and 40% lower risk of hospitalization and all-cause mortality, respectively. Encouraging older adults to increase their total daily steps and their step intensity may have significant public health implications.
Our study provides a unique contribution to the literature because it adds to the limited data available on the relationship between device-measured steps and mortality. It also provides data where there once was an absence of data on the association between steps and the risk of hospitalization. Previous studies conducted with older adults have also shown that a greater number of steps is associated with lower mortality. Yamamoto et al.22 showed that older adults in the highest quartile of daily steps (i.e., 10, 241 steps/day) had a 54% lower risk of death compared to the least active group (i.e., 3394 steps/day). However, Yamamoto et al.22 did not observe a significant linear relationship between daily step count and all-cause mortality, probably because of a small sample size and selection bias. Lee et al.10 observed a nonlinear dose–response pattern between step volume and mortality in women in the United States, with benefits starting from as few as 4363 daily steps and flattening out from 8442 steps per day. In results that were similar to those in our study, Dwyer et al.8 observed an inverse and linear dose–response relationship between steps per day and all-cause mortality, showing a 6% lower risk for every additional 1000 steps per day. Nonetheless, our analyses showed more remarkable results in the risk of all-cause mortality (i.e., 13% for every additional 1000 steps per day). These results were similar to the results found in a study of a British cohort of older men, which reported a 14% lower risk for every additional 1000 steps per day.23 We also found a 5% lower risk for hospital admission per every additional 1000 steps per day. Previous research has already reported the benefits of physical activity in reducing the risk of hospitalization,24, 25, 26 but ours is the first study to analyze the association between steps and risk of hospitalization.
Previous investigations have reported that higher walking speeds performed through field tests were associated with a lower risk of mortality.27,28 However, these studies were not conducted in free-living conditions. Some exceptions, such as the study by Lee et al.,10 have found no significant association between intensity and all-cause mortality risk after accounting for total steps per day. Similar results were also found in a recent study using a sample of adults from the National Health and Nutrition Examination Survey.11 In contrast, our findings support the idea that higher step intensity among free-living populations is associated with a 5% lower risk for hospitalization and an 11% lower risk for all-cause mortality for every additional step per minute. There may be 2 reasons for the discrepancy between our results and the results from previous studies. First, previous studies defined step intensity differently. For example, in the studies by Lee et al.10 and Saint-Maurice et al.,11 diverse peaks of cadence were used, whereas we used the average step intensity throughout the measurement period. Second, these 2 studies10,11 adjusted for step volume. We decided not to adjust for step volume because of the high correlation between step intensity and total step count. Interestingly, the same high correlation between these 2 measures has been reported in a study by Saint-Maurice et al.11
Our study also provides novel estimations on the joint associations of step volume and intensity with risk of hospitalization and mortality. In our study, participants doing more steps and doing them with more intensity had lower risk of hospitalization and early mortality compared to those doing fewer steps and doing them with less intensity. Interestingly, few participants were clustered into the group having low step volume and high step intensity or into the group having high step volume and low step intensity. Instead, a majority of participants were classified into the group having low step volume and low step intensity or into the group having high step volume and high step intensity. This observation is of interest because it suggests that both step volume and step intensity are highly correlated and that modeling them as covariates rather than as joint associations may introduce bias. The comparison of the 2 extreme groups (low volume and intensity as well as high volume and intensity) may have determined the found association. Whether this association is present when comparing intermediate groups might be determined in future studies using larger samples.
Our findings provide novel and relevant insights that can guide the development of future interventions seeking to improve the health of older adults. Those individuals who performed 50% more steps compared to the median reference (5310 steps per day) had a 12% and 25% lower risk of hospitalization and mortality, respectively. This difference of 2650 daily steps (∼2 km) may be feasible only for older adults who are more fit than others. However, the association between these variables is inversely linear, so individuals who are most inactive should be encouraged to increase the number of their steps. A similar approach should be used regarding step intensity. Steps can be intuitively understood by almost everyone, and the results presented here can, therefore, be easily translated into public health recommendations or used in the form of clinical advice. Increasing both the volume and the intensity of steps can be accomplished through a wide range of activities (e.g., purposely walking or walking that is embedded in chores), is relatively inexpensive or even free, and can easily be adapted to the physical fitness and characteristics of the person; thus, walking can be a very practical recommendation. It is relevant that previous studies have shown a high correlation when comparing the brand of accelerometer used in our study with different available commercial devices,29,30 although these other devices may overestimate the total number of steps.30,31
The key strengths of our work include the fact that it involved a relatively large sample of community-dwelling older adults at an advanced age and had a mean follow-up of 5.7 years. Our study sample also comprised a free-living population, and we derived the number of steps by using accelerometer-measured steps over 7 days of administration. Accelerometers are capable of capturing step data continuously and storing the data in memory, thus avoiding participant errors in self-reporting the details of their physical activity and avoiding other inconveniences, such as misreported or missing data.32,33 Another advantage of using devices to measure steps is that they take into account the steps involved in any type of ambulatory activity (e.g., household chores, gardening, and sports) rather than just conscious walks. To our knowledge, this is the first study estimating the joint associations between step volume and step intensity with long-term outcomes, including the risk of all-cause mortality and the risk of hospitalization, an outcome with limited evidence. Furthermore, our analyses controlled for many potential confounders, including comorbidity status, thus statistically reducing bias.
Some limitations to our study must be acknowledged. The data reported here are observational, and residual confounding may still persist from unmeasured confounders. There is also the possibility of reverse causality due to short-term follow-up. However, the results from the sensitivity analysis performed after removing participants with a follow-up of fewer than 2 years remained similar. There were significant differences in some characteristics between retained individuals and those excluded because of missing data. Thus, the results may not be generalizable to nonretained individuals, and it is unclear whether our estimates may be applicable to other populations who have a different comorbidity or physical activity statuses. Furthermore, hospitalization was ascertained only by reviewing Toledo Hospital Complex registers. Although this facility is the reference hospital for the Toledo province, where the full sample lived at baseline, some participants may have traveled or moved out of the area during follow-up, so some hospitalization events might not have been reported. In addition, the cause of hospitalization could not be retrieved. Additionally, accelerometers do not detect nonambulatory movements such as those produced by swimming or cycling. Therefore, the estimations in our study could be potentially biased, although these nonambulatory exercise activities are not common among older adults. Last, our study includes only a single step evaluation and, therefore, does not account for changes in step counts over time. However, other studies have shown a relatively high stability of accelerometer measurements over the years.34,35
5. Conclusion
The current study extends the contemporary evidence confirming that a greater number of daily steps is significantly associated with a lower risk of all-cause mortality and a lower risk of hospitalization. Additionally, we observed that step intensity is related to the mortality and hospitalization risk. The associations are based on a linear dose–response pattern. When the step volume and intensity were jointly analyzed, the group having high step volume and intensity had a 28% and 40% lower risk of hospitalization and all-cause mortality, respectively, compared with the group having low step volume and intensity. From a public health perspective, interventions targeting both step volume and step intensity in older adults may result in important public health benefits.
Acknowledgments
Acknowledgments
The authors thank the cohort members, investigators, research associates, and team members who assisted us in our study. This work was supported by the Biomedical Research Networking Center on Frailty and Healthy Aging (CIBERFES) and by European Regional Development Fund (FEDER) funds from the European Union (CB16/10/00477, CB16/10/00456, and CB16/10/00464). Our work was further funded by grants from the government of Castilla-La Mancha (PI2010/020; Institute of Health Sciences, 03031-00), by the Spanish government (Spanish Ministry of Economy and Competitiveness (Ministerio de Economía y Competitividad), Institute of Health Carlos III (Instituto de Salud Carlos III), PI10/01532, PI031558, PI11/01068) and by European grants (Seventh Framework Programme: FRAILOMIC FP7-305483-2). The funders played no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Authors’ contributions
AM participated in the data collection, contributed to the data curation and to conception and design of the study, performed the analyses, interpreted the data, drafted the original manuscript, and revised and edited the manuscript; BdPC contributed to conception and design of the study, performed the analyses, interpreted the data, drafted the original manuscript, and revised and edited the manuscript; UE interpreted the data and revised and edited the manuscript; IRG participated in the data collection and revised the manuscript; JLR and JACC contributed to the data curation and revised the manuscript; LRM got the funding and revised the manuscript; FJGG and IA got the funding, coordinated the study and revised the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2021.05.004.
Supplementary materials
References
- 1.Ham SA, Kruger J, Tudor-Locke C. Participation by US adults in sports, exercise, and recreational physical activities. J Phys Act Health. 2009;6:6–14. doi: 10.1123/jpah.6.1.6. [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health Human Services . United States Department of Health and Human Services; Washington, DC: 2008. 2008 Physical Activity Guidelines for Americans. [Google Scholar]
- 3.Tudor-Locke C. Walk more (frequently, farther, faster): The perfect preventive medicine. Prev Med. 2012;55:540–541. doi: 10.1016/j.ypmed.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 4.Dwyer T, Ponsonby AL, Ukoumunne OC, et al. Association of change in daily step count over five years with insulin sensitivity and adiposity: Population based cohort study. BMJ. 2011;342:c7249. doi: 10.1136/bmj.c7249. [DOI] [PubMed] [Google Scholar]
- 5.Sisson SB, Camhi SM, Church TS, Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps/day and metabolic syndrome. Am J Prev Med. 2010;38:575–582. doi: 10.1016/j.amepre.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Inoue S, Ohya Y, Tudor-Locke C, Yoshiike N, Shimomitsu T. Step-defined physical activity and cardiovascular risk among middle-aged Japanese: the National Health and Nutrition Survey of Japan 2006. J Phys Act Health. 2012;9:1117–1124. doi: 10.1123/jpah.9.8.1117. [DOI] [PubMed] [Google Scholar]
- 7.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: A systematic review. JAMA. 2007;298:2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 8.Dwyer T, Pezic A, Sun C, et al. Objectively measured daily steps and subsequent long term all-cause mortality: The tasped prospective cohort study. PloS One. 2015;10 doi: 10.1371/journal.pone.0141274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hansen BH, Dalene KE, Ekelund U, et al. Step by step: Association of device-measured daily steps with all cause-mortality–A prospective cohort study. Scand J Med Sci Sports. 2020;30:1705–1711. doi: 10.1111/sms.13726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee IM, Shiroma EJ, Kamada M, Bassett DR, Matthews CE, Buring JE. Association of step volume and intensity with all-cause mortality in older women. JAMA Intern Med. 2019;179:1105–1112. doi: 10.1001/jamainternmed.2019.0899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saint-Maurice PF, Troiano RP, Bassett DR, Jr., et al. Association of daily step count and step intensity with mortality among US adults. JAMA. 2020;323:1151–1160. doi: 10.1001/jama.2020.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.US Department of Health Human Services 2018 Physical Activity Guidelines Advisory Committee scientific report; Washington, DC; United States Department of Health and Human Services; 2018. [Google Scholar]
- 13.Garcia-Garcia FJ, Gutierrez Avila G, Alfaro-Acha A, et al. The prevalence of frailty syndrome in an older population from Spain: The Toledo Study for Healthy Aging. J Nutr Health Aging. 2011;15:852–856. doi: 10.1007/s12603-011-0075-8. [DOI] [PubMed] [Google Scholar]
- 14.Manas A, Del Pozo-Cruz B, Guadalupe-Grau A, et al. Reallocating accelerometer-assessed sedentary time to light or moderate- to vigorous-intensity physical activity reduces frailty levels in older adults: An isotemporal substitution approach in the TSHA study. J Am Med Dir Assoc. 2018;19 doi: 10.1016/j.jamda.2017.11.003. 185.e1–e6. [DOI] [PubMed] [Google Scholar]
- 15.Manas A, del Pozo-Cruz B, Rodríguez-Gómez I, et al. Dose–response association between physical activity and sedentary time categories on ageing biomarkers. BMC Geriatr. 2019;19:270. doi: 10.1186/s12877-019-1284-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colley R, Connor Gorber S, Tremblay MS. Quality control and data reduction procedures for accelerometry-derived measures of physical activity. Health Rep. 2010;21:63–69. [PubMed] [Google Scholar]
- 17.Chudyk AM, McAllister MM, Cheung HK, McKay HA, Ashe MC. Are we missing the sitting? Agreement between accelerometer non-wear time validation methods used with older adults' data. Cogent Med. 2017;4 doi: 10.1080/2331205X.2017.1313505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rodríguez-Gómez I, Mañas A, Losa-Reyna J, et al. The impact of movement behaviors on bone health in elderly with adequate nutritional status: Compositional data analysis depending on the frailty status. Nutrients. 2019;11:582. doi: 10.3390/nu11030582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oftedal S, Holliday EG, Attia J, et al. Daily steps and diet, but not sleep, are related to mortality in older Australians. J Sci Med Sport. 2020;23:276–282. doi: 10.1016/j.jsams.2019.09.018. [DOI] [PubMed] [Google Scholar]
- 20.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Celis-Morales CA, Welsh P, Lyall DM, et al. Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all cause mortality: Prospective cohort study of half a million UK Biobank participants. BMJ. 2018;361:k1651. doi: 10.1136/bmj.k1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yamamoto N, Miyazaki H, Shimada M, et al. Daily step count and all-cause mortality in a sample of Japanese elderly people: A cohort study. BMC Public Health. 2018;18:540. doi: 10.1186/s12889-018-5434-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jefferis BJ, Parsons TJ, Sartini C, et al. Objectively measured physical activity, sedentary behaviour and all-cause mortality in older men: Does volume of activity matter more than pattern of accumulation? Br J Sports Med. 2019;53:1013–1020. doi: 10.1136/bjsports-2017-098733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sanchez-Sanchez JL, Izquierdo M, Carnicero-Carreño JA, García-García FJ, Rodríguez-Mañas L. Physical activity trajectories, mortality, hospitalization, and disability in the Toledo Study of Healthy Aging. J Cachexia Sarcopenia Muscle. 2020;11:1007–1017. doi: 10.1002/jcsm.12566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li CL, Chu SJ, Sheu JT, Huang LYG. Impact of physical activity on hospitalization in older adults: A cohort from Taiwan, China. Arch Gerontol Geriatr. 2011;53:141–145. doi: 10.1016/j.archger.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 26.Peeters GG, Gardiner PA, Dobson AJ, Brown WJ. Associations between physical activity, medical costs and hospitalisations in older Australian women: Results from the Australian Longitudinal Study on Women's Health. J Sci Med Sport. 2018;21:604–608. doi: 10.1016/j.jsams.2017.10.022. [DOI] [PubMed] [Google Scholar]
- 27.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Veronese N, Stubbs B, Volpato S, et al. Association between gait speed with mortality, cardiovascular disease and cancer: A systematic review and meta-analysis of prospective cohort studies. J Am Med Dir Assoc. 2018;19:981–988. doi: 10.1016/j.jamda.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 29.Reid RER, Insogna JA, Carver TE, et al. Validity and reliability of Fitbit activity monitors compared to ActiGraph GT3X+ with female adults in a free-living environment. J Sci Med Sport. 2017;20:578–582. doi: 10.1016/j.jsams.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 30.Toth L.P., Park S., Springer C.M., Feyerabend M.D., Steeves J.A., Bassett D.R. Video-recorded validation of wearable step counters under free-living conditions. Med Sci Sports Exerc. 2018;50:1315–1322. doi: 10.1249/MSS.0000000000001569. [DOI] [PubMed] [Google Scholar]
- 31.Collins JE, Yang HY, Trentadue TP, Gong Y, Losina E. Validation of the Fitbit Charge 2 compared to the ActiGraph GT3X+ in older adults with knee osteoarthritis in free-living conditions. PloS One. 2019;14 doi: 10.1371/journal.pone.0211231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sallis JF, Saelens BE. Assessment of physical activity by self-report: Status, limitations, and future directions. Res Q Exerc Sport. 2000;71(Suppl.2):S1–14. [PubMed] [Google Scholar]
- 33.Warren JM, Ekelund U, Besson H, Mezzani A, Geladas N, Vanhees L. Assessment of physical activity—A review of methodologies with reference to epidemiological research: A report of the exercise physiology section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2010;17:127–139. doi: 10.1097/HJR.0b013e32832ed875. [DOI] [PubMed] [Google Scholar]
- 34.Keadle SK, Shiroma EJ, Kamada M, Matthews CE, Harris TB, Lee IM. Reproducibility of accelerometer-assessed physical activity and sedentary time. Am J Prev Med. 2017;52:541–548. doi: 10.1016/j.amepre.2016.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saint-Maurice PF, Sampson JN, Keadle SK, Willis EA, Troiano RP, Matthews CE. Reproducibility of accelerometer and posture-derived measures of physical activity. Med Sci Sports Exerc. 2020;52:876–883. doi: 10.1249/MSS.0000000000002206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Formiga F, Moreno-Gonzalez R, Chivite D, Franco J, Montero A, Corbella X. High comorbidity, measured by the Charlson Comorbidity Index, associates with higher 1-year mortality risks in elderly patients experiencing a first acute heart failure hospitalization. Aging Clin Exp Res. 2018;30:927–933. doi: 10.1007/s40520-017-0853-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.