Abstract
Aims
Gene x environment (G×E) interactions, i.e. genetic modulation of the sensitivity to environmental factors and/or environmental control of the gene expression, have not been reliably established regarding aetiology of psychotic disorders. Moreover, recent studies have shown associations between the polygenic risk scores for schizophrenia (PRS-SZ) and some risk factors of psychotic disorders, challenging the traditional gene v. environment dichotomy. In the present article, we studied the role of GxE interaction between psychosocial stressors (childhood trauma, stressful life-events, self-reported discrimination experiences and low social capital) and the PRS-SZ on subclinical psychosis in a population-based sample.
Methods
Data were drawn from the EUropean network of national schizophrenia networks studying Gene-Environment Interactions (EU-GEI) study, in which subjects without psychotic disorders were included in six countries. The sample was restricted to European descendant subjects (n = 706). Subclinical dimensions of psychosis (positive, negative, and depressive) were measured by the Community Assessment of Psychic Experiences (CAPE) scale. Associations between the PRS-SZ and the psychosocial stressors were tested. For each dimension, the interactions between genes and environment were assessed using linear models and comparing explained variances of ‘Genetic’ models (solely fitted with PRS-SZ), ‘Environmental’ models (solely fitted with each environmental stressor), ‘Independent’ models (with PRS-SZ and each environmental factor), and ‘Interaction’ models (Independent models plus an interaction term between the PRS-SZ and each environmental factor). Likelihood ration tests (LRT) compared the fit of the different models.
Results
There were no genes-environment associations. PRS-SZ was associated with positive dimensions (β = 0.092, R2 = 7.50%), and most psychosocial stressors were associated with all three subclinical psychotic dimensions (except social capital and positive dimension). Concerning the positive dimension, Independent models fitted better than Environmental and Genetic models. No significant GxE interaction was observed for any dimension.
Conclusions
This study in subjects without psychotic disorders suggests that (i) the aetiological continuum hypothesis could concern particularly the positive dimension of subclinical psychosis, (ii) genetic and environmental factors have independent effects on the level of this positive dimension, (iii) and that interactions between genetic and individual environmental factors could not be identified in this sample.
Key words: Genes × environment interactions, polygenic risk score for schizophrenia, psychosis, psychosocial stressors
Introduction
Both environmental and genetic factors are associated with an increased risk of developing psychotic disorders (van Os et al., 2010). The relationships between these factors have long been discussed, and the hypothesis of genes x environment (GxE) interactions was suggested several decades ago (Strahilevitz, 1974; Murray et al., 1986; Schulsinger et al., 1987). Such interaction can be defined as a genetic modulation of the sensitivity to environmental factors and/or environmental control of the gene expression (Kendler and Eaves, 1986). Numerous studies supported this hypothesis (Collip et al., 2013; Frydecka et al., 2020; Pries et al., 2020a), and particularly one from Caspi et al. (2005), in which a significant interaction between cannabis use in adolescence and the genetic variant Val158Met in the Catechol-O-Methyltransferase (COMT, which metabolises dopamine) gene was found. In this study, in comparison to Val/Val genotype, Met/Met and Met/Val genotypes had a protective effect against the risk of psychotic symptoms and disorders among cannabis users (in the group of subjects without cannabis use, the rates of psychotic symptoms and disorders were similar according to the different genotypes). Of note, although discrepant results have been reported in replication studies (Henquet et al., 2006; Zammit et al., 2007), a meta-analysis confirmed the small protective effect of the Val/Met heterozygous genotype [pooled OR = 0.947 95% CI (0.904–0.993), p = 0.023] (Costas et al., 2011). This meta-analysis, that did not take account of the cannabis use, hypothesised that both too high and too low levels of dopamine could be risk factors. Study of GxE interactions is difficult due to the need for large cohorts with well-characterised genetic and environmental data.
To deal with these difficulties, the study of subclinical psychosis in the general population, that can be defined as psychotic symptoms in subjects who do not meet criteria for psychotic disorders, is convenient (Verdoux and van Os, 2002; McGrath et al., 2015), especially in accordance to the aetiological psychotic continuum hypothesis. According to this hypothesis, subclinical psychosis has a similar origin/aetiology as psychotic disorders (Linscott and van Os, 2013; van Os, 2014; Pignon et al., 2018; Pries et al., 2018). Thus, studying genetic or environmental risk factors associated with subclinical psychosis may provide insights into the aetiology of psychosis and partly reduce the potential interference of reverse causation, i.e. factors are associated with or caused by the clinical disorders themselves [e.g. hospitalisations, stigma, substance use disorders or social drift after onset (Zipursky, 2014; Sariaslan et al., 2016; Pignon et al., 2019a)]. Furthermore, in line with the continuum theory, subclinical psychosis can be characterised by continuous variables, improving statistical power, which is a key issue in GxE interaction studies.
Psychotic disorders are characterised by a polygenic architecture, with thousands of common genetic variants with small effect sizes, and a few rare variants with large effect sizes (Smeland et al., 2020). The genome-wide effects of disease-associated common genetic variants can be summarised in a polygenic risk score (PRS) (Anderson et al., 2019), which offers new opportunities to characterise the complex genetic aetiology of psychotic disorders. In subjects included through the EUropean network of national schizophrenia networks studying Gene-Environment Interactions (EU-GEI), the PRS for schizophrenia (PRS-SZ) explained between 7 and 9% of the variance of the case-control status (Di Forti et al., 2019b; Tripoli et al., 2020), consistently with other studies (Vassos et al., 2017). Of note, among patients with psychotic disorders, the PRS-SZ is also associated with antipsychotic treatment response, the level of quality of life, or, in the general population, to the intelligence quotient (IQ), and the risk of attention-deficit/hyperactivity disorder (ADHD) (Mistry et al., 2018; Legge et al., 2019; Zhang et al., 2019; Pries et al., 2020c).
Studies of associations between subclinical psychosis and the PRS-SZ have produced contradictory results (Zammit et al., 2014; Mistry et al., 2018; Legge et al., 2019; Nenadić et al., 2020), and further studies are needed. Moreover, to date, four studies have investigated the role of GxE interaction on subclinical psychosis using PRS-SZ. Two studies assessed the interaction between PRS-SZ and childhood trauma, but only one reported a significant interaction (Pries et al., 2020b), whereas the other showed an independent (additive) effects of the PRS-SZ and the trauma without significant interaction (Trotta et al., 2016). A recent study assessing the associations between momentary stress and subclinical psychotic symptoms showed that higher levels of PRS-SZ were associated with a higher intensity of symptoms after a momentary stress among controls (Schick et al., 2022). In the fourth study, the authors assessed the interaction between PRS-SZ and smoking status, but did not show significant association (García-González et al., 2020).
In addition to increasing the risk for psychosis by GxE interactions, the PRS-SZ has also been associated with a greater risk of exposure to environmental risk factors for psychosis (Pingault et al., 2018). For instance, several studies have reported associations between the PRS-SZ and cannabis use (Gage et al., 2017; Pasman et al., 2018) or between the PRS-SZ and urbanicity (Colodro-Conde et al., 2018; Paksarian et al., 2018; Maxwell et al., 2021) or the level of neighbourhood deprivation and social fragmentation at birth (Solmi et al., 2020), challenging the traditional gene v. environment dichotomy. However, these observations could not explain the strength of the associations between cannabis use or urbanicity and the risk of psychotic disorders (Vassos et al., 2012; Di Forti et al., 2019a). To the best of our knowledge, the genetic-environment (G-E) associations between PRS-SZ and psychosocial stressors have not been studied to date.
In a former study on population-based controls from the EU-GEI work package 2 (WP2) (Pignon et al., 2021), we showed that psychosocial stressors, i.e. childhood trauma, stressful life-events, self-reported discrimination experiences and low social capital, had independent effects on subclinical psychosis dimensions, without significant environment x environment (ExE) interactions. In the current study, we aimed to study the relationships between these psychosocial stressors, the PRS-SZ, and three dimensions of subclinical psychosis (positive, negative, depressive), looking for GxE interaction. Furthermore, we aimed to study the association between psychosocial stressors and the PRS-SZ, looking for G-E associations.
Methods
EU-GEI WP2 study
Clinical, environmental and genetic data have been collected through the EU-GEI WP2 (named ‘Functional Enviromics’), a multicentre case-sibling-control study of genetic and environmental determinants of the occurrence and severity of psychotic disorders. Population-based controls were recruited across 6 countries: Brazil, France, Italy, the Netherlands, Spain, and the United Kingdom. Inclusion criteria were: age 18–64, living in the catchment areas, no evidence of current or past psychotic disorders. These controls were recruited using a mixture of random and quota sampling to ensure that they were broadly representative of the at-risk populations on predefined variables (age, sex, and migration) (Gayer-Anderson et al., 2020).
Ethical approval was obtained from local research ethics committees in each country. The EU-GEI Project was funded by the European Community's Seventh Framework Program under grant agreement no. HEALTH-F2-2010-241909.
Subclinical psychosis and psychosocial stressors assessment
The Community Assessment of Psychic Experiences (CAPE) is a 42-item self-report questionnaire that has been developed to assess lifetime subclinical psychotic dimensions in the general population (Stefanis et al., 2002). For each item, 4 answers were possible according to the frequency of their occurrences (from never to nearly always). To construct the dimension scores [positive, negative and depressive (Mark and Toulopoulou, 2016)], we dichotomised answers of each CAPE item (never v. sometimes or more) and summed the positive answers. The cross-national invariance of the CAPE score in the EU-GEI WP2 samples was previously demonstrated (Pignon et al., 2019b).
Childhood trauma was assessed with a short version of the Childhood Trauma Questionnaire (CTQ), with 25 items assessing five different domains (emotional and physical neglect, emotional, physical and sexual abuse) (Bernstein et al., 2003). Only the total score was used. Lifetime self-reported discrimination experiences were assessed with a modified version of the 12-item Williams' major experiences of discrimination scale (unfairly fired or not hired because of your ethnicity/sex/weight/etc., unfairly stopped/questioned/physically threatened or abused by the police, etc.) (Williams et al., 1997; Jongsma et al., 2020). Perceived social capital in each participant's immediate neighbourhood was assessed using the Social Environment Assessment Tool (SEAT), a 23-item questionnaire, that was designed to capture four dimensions of social capital: civic disorder (CD), impact of civic disorder (ICD), informal social control (ISC), and social cohesion and trust (SCT) (Sampson et al., 1997; Lochner et al., 1999; McCulloch, 2003; Drukker et al., 2006). Subjects answer according to a five-point Likert-scale (1: unusual, to 5: very common), and a sum of the weighted scores of the 4 subscales were calculated to obtain the total social capital score (SEAT score = zCD + 0.51 × zICD + 1.6 × zISC + zSCT). Finally, stressful life events were assessed using the List of Threatening Experiences (LTE) which comprises 20 binary items of events usually associated with major stress over the course of the previous 6 months (e.g. serious injury, death of a parent, separation from a partner, financial difficulties) (Brugha et al., 1985; Motrico et al., 2013).
Calculation of a polygenic risk score for schizophrenia (PRS-SZ)
Blood samples of the control sample were genotyped by the Medical Research Council Centre for Neuropsychiatric Genetics and Genomics (Cardiff, United Kingdom) using a custom ‘Illumina HumanCoreExome-24 BeadChip’ genotyping array, covering 570 038 genetic variants. As described elsewhere (Di Forti et al., 2019b), the PRS-SZ were generated using PRSice from the summary results of the Psychiatric Genomics Consortium (PGC), wave 2 (Schizophrenia Working Group of the PGC, 2014). Clumping was performed to obtain SNPs in approximate linkage disequilibrium with an r2 < 0.25 within a 250 kb window. PRS-SZ were calculated, at p-value thresholds of 0.05, because this threshold best captures liability to the disorder according to the PGC analysis (Schizophrenia Working Group of the PGC, 2014). The sample was restricted to 706 European descendant subjects (due to over-representation of European descendant subjects in the PGC2 training sample used to calculate the PRS-SZ).
Statistical analyses
The G-E association has been assessed by Spearman correlation tests between the 4 psychosocial stressors and the PRS-SZ. Then, linear regression models were used to assess the relationships between the CAPE dimensions scores (positive, negative, depressive), environmental and genetic variables, and to look for GxE interactions. Of note, we consider multiplicative interactions (Rothman et al., 1980; VanderWeele and Knol, 2014).
The different models were adjusted for age, sex, and the 10 first principal components (PCs) of the genetic analyses of the ethnic variance. For each CAPE dimension, thirteen models were tested:
A ‘Genetic model’, with the sole PRS-SZ;
Four ‘Environmental models’ for each of the 4 psychosocial stressors variables: childhood trauma, stressful life-events, self-reported discrimination experiences and low social capital;
Four ‘Independent models’: one for each of the 4 psychosocial stressors variables and the PRS-SZ, without interaction term;
Four ‘Interaction models’: each of the 4 psychosocial stressors variables and the PRS-SZ, with a GxE interaction term.
To compare the fit of the different models (and particularly the Independent and the Interaction models), we compared the explained variances (R2), and use likelihood ration test (LRT) to assess whether the addition of a factor (E + G v. G, E + G v. E, E + G + E × G v. E + G) improved the fit of the model. To verify that the results were not biased by the imputation of the outcome (CAPE scales), analyses were repeated in a sample without imputation of the CAPE.
Psychosocial variables and PRS-SZ were standardised to Z-scores (i.e. to a mean equal to 0, and a standard-deviation equal to 1). The SEAT (social capital) score was inverted, so that higher scores were associated with lower social capital. Missing data of the CAPE (between 3 and 5.9% according to the different dimensions) and the psychosocial stressors variables (between 0.5 and 20.7%) were imputed with multivariate imputation by chained equations (MICE) in 20 resamples (the country was added to CAPE and psychosocial stressors variables for the imputation). R software version 3.6.0 was used for the statistical analyses.
Results
Description of the data
The 706 European descendant subjects without psychotic disorders included in our study showed a sex ratio close to 1 (53% women) and a mean age of 38.2 (s.d. = 13.4) (% of missing data according to the different countries are available in the online Supplementary Table 3). The scores of subclinical psychosis dimensions and psychosocial stressors scales, and the values of PRS-SZ scores are available in the Table 1 (for non-imputed data, see online Supplementary Table 2).
Table 1.
Description of the data: socio-demographic, subclinical psychosis, psychosocial stressors and polygenic risk scores variables
| Median (IQR), mean (s.d.) or N (%) | |
|---|---|
| Age | 36.00 (22.00), 38.18 (13.35) |
| Sex | |
| Women | 376 (53.3%) |
| Men | 330 (46.7%) |
| CAPE dimensions scales | |
| Positive | 4.00 (4.00), 4.51(2.81) |
| Negative | 6.00 (5.00), 6.24 (3.49) |
| Depressive | 4.00 (3.00), 4.39 (1.82) |
| Psychosocial stressors measures | |
| Childhood trauma | 31.00 (9.75), 33.34 (9.29) |
| Self-reported discrimination experiences | 0.00 (1.00), 0.51 (0.92) |
| Stressful life events | 1.00 (2.00), 1.37 (1.29) |
| Social capital | 0.37 (3.27), 0.37 (2.37) |
| PRS-SZ | −0.00096 (0.00018), −0.00096 (0.00014) |
CAPE, Community Assessment of Psychic Experiences’; IQR, interquartile range; PRS-SZ, polygenic risk score for schizophrenia; s.d., standard-deviation.
Correlation between genetic vulnerability and environmental factors
Spearman correlation tests did not suggest any evidence of associations between psychosocial stressors levels and the PRS-SZ (Table 2).
Table 2.
Spearman tests between Z-scores of genetic and environmental factors among subjects with complete data (N = 456)
| Childhood trauma | Self-reported discrimination experiences | Stressful life events | Social capital | |
|---|---|---|---|---|
| Polygenic risk score for schizophrenia | ρ = 0.063 (p-value = 0.18) | ρ = −0.047 (p-value = 0.32) | ρ = 0.083 (p-value = 0.08) | ρ = 0.032 (p-value = 0.48) |
Legend: ρ: Spearman correlation coefficient.
Influence of genetic vulnerability and environmental factors on subclinical psychosis dimensions
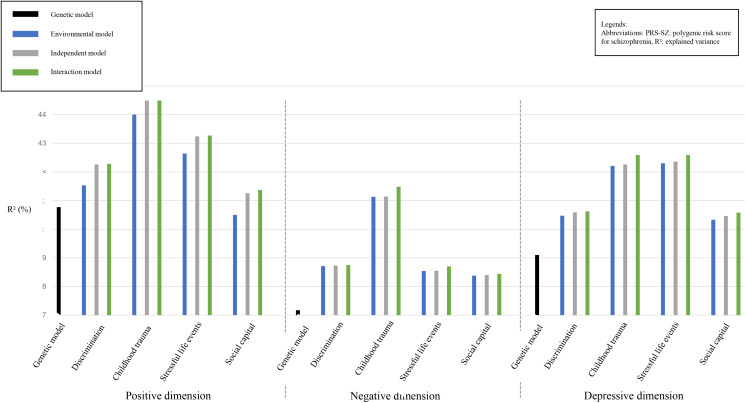
For the three subclinical psychosis dimensions that we studied, we first assessed the variance that might be explained by the PRS-SZ (Genetic models, Fig. 1 and Table 3). Only the positive dimension was associated with the PRS-SZ (β = 0.086, p-value = 0.02, with a R2 = 7.77%).
Fig. 1.
Explained variances of the different models.
Table 3.
Model comparison of the explained variances of the subclinical psychosis dimensions
| Explained variance by the models (R2) (%) | PRS-SZ | LRT: comparison of ‘G’ and ‘E + G’ models (p-values) | Environmental factor | LRT: comparison of ‘E’ and ‘E + G’ models (p-values) | Interaction term between the PRS-SZ and the environmental factor | LRT: comparison of ‘E + G’ and ‘E + G + E × G’ models (p-values) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | s.d. | p-value | β | s.d. | p-value | β | s.d. | p-value | |||||||
| Positive dimension | G | 7.77 | 0.086 | 0.037 | 0.024 | – | – | – | – | – | – | – | – | – | |
| Self-reported discrimination experiences | E | 8.53 | – | – | – | – | 0.122 | 0.037 | 0.001 | – | – | – | – | – | |
| E + G | 9.26 | 0.085 | 0.037 | 0.026 | 0.006 | 0.122 | 0.037 | 0.001 | 0.013 | – | – | – | – | ||
| E + G + E × G | 9.28 | 0.085 | 0.037 | 0.026 | – | 0.127 | 0.038 | 0.001 | – | 0.006 | 0.037 | 0.776 | 0.884 | ||
| Childhood trauma | E | 11.00 | – | – | – | – | 0.199 | 0.036 | <0.001 | – | – | – | – | – | |
| E + G | 11.49 | 0.069 | 0.036 | 0.065 | <0.001 | 0.193 | 0.036 | <0.001 | 0.041 | – | – | – | – | ||
| E + G + E × G | 11.49 | 0.069 | 0.036 | 0.065 | – | 0.192 | 0.037 | <0.001 | – | 0.004 | 0.036 | 0.887 | 0.937 | ||
| Stressful life events | E | 9.64 | – | – | – | – | 0.162 | 0.036 | <0.001 | – | – | – | – | – | |
| E + G | 10.24 | 0.076 | 0.036 | 0.044 | <0.001 | 0.157 | 0.036 | <0.001 | 0.037 | – | – | – | – | ||
| E + G + E × G | 10.27 | 0.076 | 0.037 | 0.045 | – | 0.157 | 0.037 | <0.001 | – | −0.007 | 0.037 | 0.714 | 0.652 | ||
| Low level of social capital | E | 7.50 | – | – | – | – | 0.069 | 0.037 | 0.087 | – | – | – | – | – | |
| E + G | 8.26 | 0.086 | 0.037 | 0.024 | 0.066 | 0.068 | 0.037 | 0.088 | 0.013 | – | – | – | – | ||
| E + G + E × G | 8.37 | 0.085 | 0.037 | 0.026 | – | 0.066 | 0.037 | 0.101 | – | −0.029 | 0.036 | 0.470 | 0.650 | ||
| Negative dimension | G | 4.17 | 0.014 | 0.038 | 0.718 | – | – | – | – | – | – | – | – | – | |
| Self-reported discrimination experiences | E | 5.71 | – | – | – | – | 0.125 | 0.037 | 0.001 | – | – | – | – | – | |
| E + G | 5.73 | 0.012 | 0.037 | 0.748 | <0.001 | 0.125 | 0.037 | 0.001 | 0.910 | – | – | – | – | ||
| E + G + E × G | 5.75 | 0.012 | 0.037 | 0.747 | – | 0.125 | 0.037 | 0.001 | – | −0.012 | 0.038 | 0.740 | 0.777 | ||
| Childhood trauma | E | 8.13 | – | – | – | – | 0.200 | 0.037 | <0.001 | – | – | – | – | – | |
| E + G | 8.14 | −0.004 | 0.037 | 0.854 | <0.001 | 0.200 | 0.037 | <0.001 | 0.723 | – | – | – | – | ||
| E + G + E × G | 8.48 | −0.006 | 0.037 | 0.838 | – | 0.213 | 0.038 | <0.001 | – | −0.057 | 0.036 | 0.125 | 0.188 | ||
| Stressful life events | E | 5.54 | – | – | – | – | 0.117 | 0.037 | 0.007 | – | – | – | – | – | |
| E + G | 5.55 | 0.006 | 0.038 | 0.830 | <0.001 | 0.117 | 0.037 | 0.007 | 0.883 | – | – | – | – | ||
| E + G + E × G | 5.70 | 0.005 | 0.038 | 0.835 | – | 0.118 | 0.037 | 0.006 | – | −0.035 | 0.038 | 0.386 | 0.304 | ||
| Low level of social capital | E | 5.38 | – | – | – | – | 0.110 | 0.037 | 0.008 | – | – | – | – | – | |
| E + G | 5.40 | 0.014 | 0.037 | 0.723 | <0.001 | 0.109 | 0.037 | 0.009 | 0.897 | – | – | – | – | ||
| E + G + E × G | 5.44 | 0.014 | 0.037 | 0.712 | – | 0.111 | 0.037 | 0.008 | – | 0.016 | 0.037 | 0.660 | 0.870 | ||
| Depressive dimension | G | 6.10 | 0.036 | 0.037 | 0.350 | – | – | – | – | – | – | – | – | – | |
| Self-reported discrimination experiences | E | 7.47 | – | – | – | – | 0.122 | 0.037 | 0.001 | – | – | – | – | – | |
| E + G | 7.59 | 0.034 | 0.037 | 0.369 | <0.001 | 0.122 | 0.037 | 0.001 | 0.373 | – | – | – | – | ||
| E + G + E × G | 7.62 | 0.034 | 0.037 | 0.369 | – | 0.123 | 0.037 | 0.001 | – | −0.017 | 0.038 | 0.656 | 0.489 | ||
| Childhood trauma | E | 9.21 | – | – | – | – | 0.180 | 0.037 | <0.001 | – | – | – | – | – | |
| E + G | 9.26 | 0.018 | 0.037 | 0.595 | <0.001 | 0.178 | 0.037 | <0.001 | 0.611 | – | – | – | – | ||
| E + G + E × G | 9.59 | 0.022 | 0.037 | 0.566 | – | 0.165 | 0.038 | <0.001 | – | 0.056 | 0.036 | 0.124 | 0.058 | ||
| Stressful life events | E | 9.30 | – | – | – | – | 0.181 | 0.037 | <0.001 | – | – | – | – | – | |
| E + G | 9.36 | 0.024 | 0.036 | 0.525 | <0.001 | 0.180 | 0.037 | <0.001 | 0.604 | – | – | – | – | ||
| E + G + E × G | 9.59 | 0.022 | 0.037 | 0.559 | – | 0.182 | 0.037 | <0.001 | – | −0.047 | 0.037 | 0.239 | 0.325 | ||
| Low level of social capital | E | 7.33 | – | – | – | – | 0.115 | 0.037 | 0.004 | – | – | – | – | – | |
| E + G | 7.46 | 0.035 | 0.037 | 0.354 | 0.014 | 0.115 | 0.037 | 0.004 | 0.363 | – | – | – | – | ||
| E + G + E × G | 7.58 | 0.036 | 0.037 | 0.338 | – | 0.118 | 0.037 | 0.004 | – | 0.032 | 0.037 | 0.408 | 0.337 | ||
E, Environmental model; E + G, Independent model; E + G + E × G, Interaction model; G, Genetic model; LRT, Likelihood ratio test; PRS-SZ, polygenic risk score for schizophrenia.
The different models were adjusted on age, sex, and the first ten principal components of the ethnicity-based genetic variance.
The significant associations are shown in bold.
We then assessed the variance explained by each of the 4 psychosocial stressors, i.e. discrimination, childhood trauma, stressful events and low social capital (Environmental models). Each psychosocial stressor was associated with the three subclinical psychosis dimensions, except the low level of social capital that was not associated with the positive dimension (Fig. 1 and Table 3). Of note, when associated with subclinical dimensions, the variance explained by Environmental models was always higher than the one explained by Genetic models (except, concerning the positive dimension, for the low level of social capital).
Combination of genetic and environmental factors
In the Independent models, for the 3 dimensions, the explained variances were better than in the Genetic models, which was confirmed by the LRT (p-values < 0001 for almost all models, Fig. 1 and Table 3, except for the low level of social capital in the positive dimension).
However, concerning the negative and depressive dimensions, in comparison to Environmental models, the Independent models did not fit better. In other words, adding the PRS-SZ to the Environmental factors did not improve the explained variances of these models. Concerning the positive dimension, the Independent models fitted better than both Genetic and Environment models (LRT: p-values between 0.013 and 0.041, Table 3).
In the Interaction models, no significant GxE interaction was observed: adding a GxE interaction term in the Independent models was associated with modest increases of the explained variance, and no interaction term was significantly associated with one of the 3 subclinical psychosis dimension scores. The LRT confirmed that the Interaction models did not fit better than Independent models (Table 3). The analyses presented in Table 3 were repeated in a sample without imputation of the CAPE, without significant change (see online Supplementary Table 3).
Discussion
In this population-based subjects without psychotic disorders transnational study on the relationships between subclinical psychosis and genetic and environmental (psychosocial stressors) risk factors, the PRS-SZ was associated with the positive dimension but not with the negative and the depressive dimensions. By contrast, the psychosocial stressors were positively associated with the 3 dimensions, except for the low level of social capital, which was not associated with the positive dimension. Moreover, considering the positive dimension, PRS-SZ and psychosocial stressors were independently associated, without GxE interaction, consistently with independent effects of genetic and environmental risk factors.
A genetic psychotic continuum?
The association between the PRS-SZ and the positive dimension is consistent with the hypothesis of an aetiological psychotic continuum, with subclinical psychosis and psychotic disorders sharing aetiological – genetic and environmental – factors (Linscott and van Os, 2013). This hypothesis could not be verified concerning the other dimensions. A precedent EU-GEI study analysing in controls the relationships between subclinical psychosis and another factor associated with the risk of psychotic disorders, i.e. advanced paternal age, found consistent results: significant association with the positive dimension, but not to negative and depressive dimensions (Schürhoff et al., 2020). The aetiological psychotic continuum could concern particularly the positive dimension. Indeed, in comparison to the negative and depressive dimensions, the positive symptoms are the most specific of psychotic disorders (Hanssen et al., 2003). Furthermore, in a study analysing the associations between the PRS-SZ and clinical dimensions among antipsychotic-naïve patients with first episode of psychotic disorders (FEP), Santoro et al. (2018) found an association with the positive dimension of the positive and negative syndrome scale (PANSS). Moreover, Markota et al. (2018) found higher level PRS-SZ in manic-psychosis among patient with bipolar disorder. In future studies, it would be interesting to analyse the relationships between the negative and the depressive dimensions with other PRS (e.g. for depression, or bipolar disorder).
Several studies have found an association between the PRS-SZ and subclinical psychosis, but not all. Indeed, some of these studies did not find any significant associations (Derks et al., 2012; Nenadić et al., 2020). Methodological differences could be involved, including study population [e.g. some of them were conducted in the paediatric population (Zammit et al., 2014; Pries et al., 2020a)], or the tools used to measure subclinical psychosis [e.g. schizotypy scales do not take account of hallucinations (Seiler et al., 2020)]. In a recent study from EU-GEI WP6 (‘Vulnerability and Severity’) sample, van Os et al. (2020) did not find any associations between PRS-SZ and the 3 dimensions of the CAPE in the controls (without psychotic disorders), although among siblings, a significant association with the negative dimension was found. Among the different studies on association between the PRS-SZ and subclinical psychosis, UK Biobank represents the most closely related to EU-GEI (sample from the general population from United Kingdom), and two of the three studies conducted in UK Biobank found significant associations (Legge et al., 2019; García-González et al., 2020), contrary to the third, that did not find any significant difference (Alloza et al., 2020). Of note, in these 3 UK Biobank studies, the samples were different, especially according to the available data of each subject (e.g. MRI data).
Association between environmental and genetic factors
Several studies found G-E associations. In a transnational study (Australia, Netherlands and United Kingdom), the PRS-SZ was associated with the population density of the residence (Colodro-Conde et al., 2018), i.e. with urbanicity (Vassos et al., 2012). These findings were replicated recently in the United Kingdom (Maxwell et al., 2021). Of note, this last study considered also other PRS (for depression, bipolar disorder, etc.) and found analogous results. Other studies found similar associations with the cannabis use (Gage et al., 2017; Pasman et al., 2018). These studies suggest that the association between these environmental factors and the risk of psychotic disorders could partially be explained by the same genetic factors (Pingault et al., 2018). This hypothesis particularly concerns childhood trauma, that has often be supposed to be associated with vulnerabilities to psychiatric disorders (Etain et al., 2008; Varese et al., 2012; Baudin et al., 2017). Sharing the same genetic risk factors could explain the association between childhood trauma and psychiatric disorders. However, in our study, we did not find any G-E association neither with childhood trauma nor with the other psychosocial stressors.
Gene x environment (psychosocial stressors) interactions
Our study did not show any statistically significant interaction between the psychosocial stressors and the PRS-SZ, but independent effects concerning the positive dimension. Trotta et al. (2016) found similar results: the PRS-SZ and childhood trauma history predicted both psychosis status, without interaction between these factors. To our knowledge, two other studies have looked for such interactions, that found a significant GxE interaction between the PRS-SZ and childhood trauma (Pries et al., 2020b; Schick et al., 2022). Another study using the PRS-SZ and conducted in adults looked for interaction with other environmental factors, i.e. smoking status, without finding any GxE interaction (García-González et al., 2020).
One hypothesis to explain the negative results of this GxE interaction study is that the PRS-SZ is not the appropriate tool for the study of GxE interaction in psychosis (Assary et al., 2018). Indeed, this statistical tool summarises essentially monogenic factors with small effects sizes; and GxE interaction could only involve monogenic factors (Caspi et al., 2005; Stefanis et al., 2007; Alemany et al., 2011). However, other studies used PRS and found GxE interaction, for instance between childhood trauma and the PRS for depression in the risk of major depressive disorder (Peyrot et al., 2014), or between this PRS and stressful life events in the level of depressive symptoms (Domingue et al., 2017), as well as studies on non-psychiatric diseases, e.g. for breast cancer (Meisner et al., 2019; Shi et al., 2020). The problem could concern specifically PRS-SZ, with (i) an insufficient sample of subjects included in the genome-wide association studies (GWAS) used to calculate it, which is a major issue concerning PRSs (Plomin and von Stumm, 2018), and (ii) the fact that the PRS-SZ performed better among European descendants (which has prevented the inclusion of subjects from ethnic minorities) (Vassos et al., 2017). Moreover, the PRS does not take copy number variant (CNVs) or epigenetic factors in account, and they are associated with the risk of schizophrenia (and with childhood trauma concerning epigenetic factors) (St Clair, 2009; Shorter and Miller, 2015; Parade et al., 2021). Another hypothesis states that the genes that increase the sensibility to environmental stressors could be different from the genes that increase the risk of schizophrenia (displayed in the GWAS). Furthermore, GxE interactions could also concern other environmental factors (urbanicity, advanced paternal age, migration, etc.). Finally, the study GxE interactions using exposome scores (Pries et al., 2020a), that takes account of several environmental exposures (including psychosocial stressors), could be instructive.
Limitations
Some limitations should be acknowledged. First, due to the cross-sectional nature of EU-GEI study, the assessment of both subclinical psychosis and psychosocial stressors was retrospective, thus susceptible to be biased (e.g. recall bias) and influenced by clinical variables as depressive or positive symptoms (MacDonald et al., 2015). These potential biases, especially concerning psychosocial stressors assessment (particularly the low level of discrimination experience), have been discussed previously (Pignon et al., 2021). Moreover, regarding the sample size, that could be considered as insufficient to enhance an GxE interaction, Pries et al. (2020a) found an interaction between childhood adversity and PRS-SZ concerning subclinical psychosis (with an ecological momentary assessment) with a lower sample (n = 593). The absence of subjects from ethnic minorities, is a major limitation (Tortelli et al., 2018). Indeed, these minorities are exposed to higher levels of psychosocial stress (Hatch et al., 2016). Contrary to the CAPE (Pignon et al., 2019b), concerning the assessment of these psychosocial stressors, the cross-national invariance of the different tools that were used (CTQ, Williams' major experiences of discrimination scale, LTE, SEAT) has not been studies. Moreover, as the sampling was not fully at random, we cannot assume that our sample was representative of the general population.
Conclusion
This general population-based study revealed an association between PRS-SZ and the subclinical positive dimension of psychosis, as well as independent effects of the PRS-SZ and of the psychosocial stressors (childhood trauma, stressful life events, self-reported discrimination experiences) on the positive dimension, contrary to the negative and depressive dimensions. Moreover, concerning the 3 dimensions, this study did not evidence any GxE interaction, or any G-E association.
Acknowledgements
None.
Supplementary material
For supplementary material accompanying this paper visit http://doi.org/10.1017/S2045796022000464.
click here to view supplementary material
Data
Data is confidential and not available.
Conflict of interest and Financial support
Dr Bernardo has been a consultant for, received grant/research support and honoraria from, and been on the speakers/advisory board of ABBiotics, Adamed, Angelini, Casen Recordati, Janssen-Cilag, Menarini, Rovi and Takeda. Dr Arango has received support by the Spanish Ministry of Science and Innovation. Instituto de Salud Carlos III (SAM16PE07CP1, PI16/02012, PI19/024), co-financed by ERDF Funds from the European Commission, ‘A way of making Europe’, CIBERSAM. Madrid Regional Government (B2017/BMD-3740 AGES-CM-2), European Union Structural Funds. European Union Seventh Framework Program under grant agreements FP7-4-HEALTH-2009-2.2.1-2-241909 (Project EU-GEI) and FP7-HEALTH-2013-2.2.1-2-603196 (Project PSYSCAN); and European Union H2020 Program under the Innovative Medicines Initiative 2 Joint Undertaking (grant agreement No 115916, Project PRISM, and grant agreement No 777394, Project AIMS-2-TRIALS), Fundación Familia Alonso and Fundación Alicia Koplowitz. Dr James B. Kirkbride has received consultancy fees from Roche and the Health Services Executive, Ireland. He is supported by the National Institute of Health Research University College London Hospital Biomedical Research Centre.
Ethical standards
Ethical approval was obtained from local research ethics committees in each country. The EU-GEI Project was funded by the European Community's Seventh Framework Program under grant agreement no. HEALTH-F2-2010-241909.
References
- Alemany S, Arias B, Aguilera M, Villa H, Moya J, Ibáñez MI, Vossen H, Gastó C, Ortet G and Fañanás L (2011) Childhood abuse, the BDNF-Val66Met polymorphism and adult psychotic-like experiences. The British Journal of Psychiatry 199, 38–42. [DOI] [PubMed] [Google Scholar]
- Alloza C, Blesa-Cábez M, Bastin ME, Madole JW, Buchanan CR, Janssen J, Gibson J, Deary IJ, Tucker-Drob EM, Whalley HC, Arango C, McIntosh AM, Cox SR and Lawrie SM (2020) Psychotic-like experiences, polygenic risk scores for schizophrenia, and structural properties of the salience, default mode, and central-executive networks in healthy participants from UK Biobank. Translational Psychiatry 1, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson JS, Shade J, DiBlasi E, Shabalin AA and Docherty AR (2019) Polygenic risk scoring and prediction of mental health outcomes. Current Opinion in Psychology 27, 77–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assary E, Vincent JP, Keers R and Pluess M (2018) Gene-environment interaction and psychiatric disorders: review and future directions. Seminars in Cell & Developmental Biology 77, 133–143. [DOI] [PubMed] [Google Scholar]
- Baudin G, Szöke A, Richard J-R, Pelissolo A, Leboyer M and Schürhoff F (2017) Childhood trauma and psychosis: beyond the association. Child Abuse & Neglect 72, 227–235. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D and Zule W (2003) Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect 27, 169–190. [DOI] [PubMed] [Google Scholar]
- Brugha T, Bebbington P, Tennant C and Hurry J (1985) The List of Threatening Experiences: a subset of 12 life event categories with considerable long-term contextual threat. Psychological Medicine 15, 189–194. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Cannon M, McClay J, Murray R, Harrington H, Taylor A, Arseneault L, Williams B, Braithwaite A, Poulton R and Craig IW (2005) Moderation of the effect of adolescent-onset Cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biological Psychiatry 57, 1117–1127. [DOI] [PubMed] [Google Scholar]
- Collip D, Myin-Germeys I, Wichers M, Jacobs N, Derom C, Thiery E, Lataster T, Simons C, Delespaul P, Marcelis M, van Os J and van Winkel R (2013) FKBP5 as a possible moderator of the psychosis-inducing effects of childhood trauma. The British Journal of Psychiatry: The Journal of Mental Science 202, 261–268. [DOI] [PubMed] [Google Scholar]
- Colodro-Conde L, Couvy-Duchesne B, Whitfield JB, Streit F, Gordon S, Kemper KE, Yengo L, Zheng Z, Trzaskowski M, de Zeeuw EL, Nivard MG, Das M, Neale RE, MacGregor S, Olsen CM, Whiteman DC, Boomsma DI, Yang J, Rietschel M, McGrath JJ, Medland SE and Martin NG (2018) Association between population density and genetic risk for schizophrenia. JAMA Psychiatry 75, 901–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costas J, Sanjuán J, Ramos-Ríos R, Paz E, Agra S, Ivorra JL, Páramo M, Brenlla J and Arrojo M (2011) Heterozygosity at catechol-O-methyltransferase Val158Met and schizophrenia: new data and meta-analysis. Journal of Psychiatric Research 45, 7–14. [DOI] [PubMed] [Google Scholar]
- Derks EM, Vorstman JAS, Ripke S, Kahn RS, Consortium TSPG and Ophoff RA (2012) Investigation of the genetic association between quantitative measures of psychosis and schizophrenia: a polygenic risk score analysis. PLoS One 7, e37852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Forti M, Quattrone D, Freeman TP, Tripoli G, Gayer-Anderson C, Quigley H, Rodriguez V, Jongsma HE, Ferraro L, La Cascia C, La Barbera D, Tarricone I, Berardi D, Szöke A, Arango C, Tortelli A, Velthorst E, Bernardo M, Del-Ben CM, Menezes PR, Selten J-P, Jones PB, Kirkbride JB, Rutten BP, de Haan L, Sham PC, van Os J, Lewis CM, Lynskey M, Morgan C, Murray RM, Amoretti S, Arrojo M, Baudin G, Beards S, Bernardo M, Bobes J, Bonetto C, Cabrera B, Carracedo A, Charpeaud T, Costas J, Cristofalo D, Cuadrado P, Díaz-Caneja CM, Ferchiou A, Franke N, Frijda F, García Bernardo E, Garcia-Portilla P, González E, Hubbard K, Jamain S, Jiménez-López E, Leboyer M, López Montoya G, Lorente-Rovira E, Marcelino Loureiro C, Marrazzo G, Martínez C, Matteis M, Messchaart E, Moltó MD, Nacher J, Olmeda MS, Parellada M, González Peñas J, Pignon B, Rapado M, Richard J-R, Rodríguez Solano JJ, Roldán Díaz L, Ruggeri M, Sáiz PA, Sánchez E, Sanjuán J, Sartorio C, Schürhoff F, Seminerio F, Shuhama R, Sideli L, Stilo SA, Termorshuizen F, Tosato S, Tronche A-M, van Dam D and van der Ven E (2019a) The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. The Lancet Psychiatry 6, 427–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Forti M, Wu-Choi B, Quattrone D, Richards AL, Freeman TP, Tripoli G, Gayer-Anderson C, Rodriguez V, Jongsma H, Ferraro L, Cascia CL, Tosato S, Tarricone I, Berardi D, Szoke A, Arango C, Bobes J, Sanjuan J, Santos JL, Arrojo M, Velthorst E, Bernardo M, Ben CMD, Selten J-P, Jones PB, Kirkbride JB, Rutten BN, de Haan L, van Os J, Lynskey M, Morgan C, Vassos E, O'Donovan M, Lewis C, Sham PC, Murray RM and Group E-GW (2019b) The independent and combined influence of schizophrenia polygenic risk score and heavy cannabis use on risk for psychotic disorder: a case-control analysis from the EUGEI study. Preprint (bioRxiv) 844803. [Google Scholar]
- Domingue BW, Liu H, Okbay A and Belsky DW (2017) Genetic heterogeneity in depressive symptoms following the death of a spouse: polygenic score analysis of the U.S. Health and Retirement Study. The American Journal of Psychiatry 174, 963–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drukker M, Krabbendam L, Driessen G and van Os J (2006) Social disadvantage and schizophrenia. A combined neighbourhood and individual-level analysis. Social Psychiatry and Psychiatric Epidemiology 41, 595–604. [DOI] [PubMed] [Google Scholar]
- Etain B, Henry C, Bellivier F, Mathieu F and Leboyer M (2008) Beyond genetics: childhood affective trauma in bipolar disorder. Bipolar Disorders 10, 867–876. [DOI] [PubMed] [Google Scholar]
- Frydecka D, Kotowicz K, Gawęda Ł, Prochwicz K, Kłosowska J, Rymaszewska J, Samochowiec A, Samochowiec J, Podwalski P, Pawlak-Adamska E, Szmida E, Cechnicki A and Misiak B (2020) Effects of interactions between variation in dopaminergic genes, traumatic life events, and anomalous self-experiences on psychosis proneness: results from a cross-sectional study in a nonclinical sample. European Psychiatry: The Journal of the Association of European Psychiatrists 63, e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gage SH, Jones HJ, Burgess S, Bowden J, Smith GD, Zammit S and Munafò MR (2017) Assessing causality in associations between cannabis use and schizophrenia risk: a two-sample Mendelian randomization study. Psychological Medicine 47, 971–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-González J, Ramírez J, Howard DM, Brennan CH, Munroe PB and Keers R (2020) The effects of polygenic risk for psychiatric disorders and smoking behaviour on psychotic experiences in UK Biobank. Translational Psychiatry 1, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gayer-Anderson C, Jongsma HE, Di Forti M, Quattrone D, Velthorst E, de Haan L, Selten J-P, Szöke A, Llorca P-M, Tortelli A, Arango C, Bobes J, Bernardo M, Sanjuán J, Santos JL, Arrojo M, Parellada M, Tarricone I, Berardi D, Ruggeri M, Lasalvia A, Ferraro L, La Cascia C, La Barbera D, Menezes PR, Del-Ben CM, Hubbard K, Beards S, Reininghaus U, Tripoli G, Stilo SA, Parellada M, Roldán L, López G, Matteis M, Rapado M, González E, Martínez C, Cuadrado P, Solano JJR, Carracedo A, Costas J, Bernardo EG, Sánchez E, Olmeda MS, Cabrera B, Lorente-Rovira E, Garcia-Portilla P, Jiménez-López E, Franke N, van Dam D, Termorshuizen F, van der Ven E, Messchaart E, Leboyer M, Schürhoff F, Baudin G, Ferchiou A, Pignon B, Jamain S, Richard J-R, Charpeaud T, Tronche A-M, Frijda F, Sideli L, Seminerio F, Sartorio C, Marrazzo G, Loureiro CM, Shuhama R, Ruggeri M, Tosato S, Bonetto C, Cristofalo D, Rutten BP, van Os J, Jones PB, Murray RM, Kirkbride JB, Morgan C and EU-GEI WP2 Group (2020) The European network of national schizophrenia networks studying gene–environment interactions (EU-GEI): incidence and first-episode case–control programme. Social Psychiatry and Psychiatric Epidemiology 55, 645–657. [DOI] [PubMed] [Google Scholar]
- Hanssen M, Peeters F, Krabbendam L, Radstake S, Verdoux H and van Os J (2003) How psychotic are individuals with non-psychotic disorders? Social Psychiatry and Psychiatric Epidemiology 38, 149–154. [DOI] [PubMed] [Google Scholar]
- Hatch SL, Gazard B, Williams DR, Frissa S, Goodwin L and Hotopf M (2016) Discrimination and common mental disorder among migrant and ethnic groups: findings from a South East London Community sample. Social Psychiatry and Psychiatric Epidemiology 51, 689–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henquet C, Rosa A, Krabbendam L, Papiol S, Faňanás L, Drukker M, Ramaekers JG and van Os J (2006) An experimental study of catechol-O-methyltransferase Val158Met moderation of Δ-9-tetrahydrocannabinol-induced effects on psychosis and cognition. Neuropsychopharmacology 12, 2748–2757. [DOI] [PubMed] [Google Scholar]
- Jongsma HE, Gayer-Anderson C, Tarricone I, Velthorst E, van der Ven E, Quattrone D, di Forti M, Group E-GW, Menezes PR, Del-Ben CM, Arango C, Lasalvia A, Berardi D, Cascia CL, Bobes J, Bernardo M, Sanjuán J, Santos JL, Arrojo M, de Haan L, Tortelli A, Szöke A, Murray RM, Rutten BP, van Os J, Morgan C, Jones PB and Kirkbride JB (2020) Social disadvantage, linguistic distance, ethnic minority status and first-episode psychosis: results from the EU-GEI case–control study. Psychological Medicine 51, 1536–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS and Eaves LJ (1986) Models for the joint effect of genotype and environment on liability to psychiatric illness. The American Journal of Psychiatry 143, 279–289. [DOI] [PubMed] [Google Scholar]
- Legge SE, Jones HJ, Kendall KM, Pardiñas AF, Menzies G, Bracher-Smith M, Escott-Price V, Rees E, Davis KAS, Hotopf M, Savage JE, Posthuma D, Holmans P, Kirov G, Owen MJ, O'Donovan MC, Zammit S and Walters JTR (2019) Association of genetic liability to psychotic experiences with neuropsychotic disorders and traits. JAMA Psychiatry 76, 1256–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linscott RJ and van Os J (2013) An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychological Medicine 43, 1133–1149. [DOI] [PubMed] [Google Scholar]
- Lochner K, Kawachi I and Kennedy BP (1999) Social capital: a guide to its measurement. Health & Place 5, 259–270. [DOI] [PubMed] [Google Scholar]
- MacDonald K, Thomas ML, MacDonald TM and Sciolla AF (2015) A perfect childhood? Clinical correlates of minimization and denial on the childhood trauma questionnaire. Journal of Interpersonal Violence 30, 988–1009. [DOI] [PubMed] [Google Scholar]
- Mark W and Toulopoulou T (2016) Psychometric properties of ‘community assessment of psychic experiences’: review and meta-analyses. Schizophrenia Bulletin 42, 34–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markota M, Coombes BJ, Larrabee BR, McElroy SL, Bond DJ, Veldic M, Colby CL, Chauhan M, Cuellar-Barboza AB, Fuentes M, Kung S, Prieto ML, Rummans TA, Bobo WV, Frye MA and Biernacka JM (2018) Association of schizophrenia polygenic risk score with manic and depressive psychosis in bipolar disorder. Translational Psychiatry 1, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell JM, Coleman JRI, Breen G and Vassos E (2021) Association between genetic risk for psychiatric disorders and the probability of living in urban settings. JAMA Psychiatry 78, 1355–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCulloch A (2003) An examination of social capital and social disorganisation in neighbourhoods in the British household panel study. Social Science & Medicine (1982) 56, 1425–1438. [DOI] [PubMed] [Google Scholar]
- McGrath JJ, Saha S, Al-Hamzawi A, Alonso J, Bromet EJ, Bruffaerts R, Caldas-de-Almeida JM, Chiu WT, de Jonge P, Fayyad J, Florescu S, Gureje O, Haro JM, Hu C, Kovess-Masfety V, Lepine JP, Lim CCW, Mora MEM, Navarro-Mateu F, Ochoa S, Sampson N, Scott K, Viana MC and Kessler RC (2015) Psychotic experiences in the general population: a cross-national analysis based on 31,261 respondents from 18 countries. JAMA Psychiatry 72, 697–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisner A, Kundu P and Chatterjee N (2019) Case-only analysis of gene-environment interactions using polygenic risk scores. American Journal of Epidemiology 188, 2013–2020. [DOI] [PubMed] [Google Scholar]
- Mistry S, Harrison JR, Smith DJ, Escott-Price V and Zammit S (2018) The use of polygenic risk scores to identify phenotypes associated with genetic risk of schizophrenia: systematic review. Schizophrenia Research 197, 2–8. [DOI] [PubMed] [Google Scholar]
- Motrico E, Moreno-Küstner B, de Dios Luna J, Torres-González F, King M, Nazareth I, Montón-Franco C, Josefa Gilde Gómez-Barragán M, Sánchez-Celaya M, Ángel Díaz-Barreiros M, Vicens C, Moreno-Peral P and Ángel Bellón J (2013) Psychometric properties of the List of Threatening Experiences – LTE and its association with psychosocial factors and mental disorders according to different scoring methods. Journal of Affective Disorders 150, 931–940. [DOI] [PubMed] [Google Scholar]
- Murray RM, Reveley AM and McGuffin P (1986) Genetic vulnerability to schizophrenia. Psychiatric Clinics of North America 9, 3–16. [PubMed] [Google Scholar]
- Nenadić I, Meller T, Schmitt S, Stein F, Brosch K, Mosebach J, Ettinger U, Grant P, Meinert S, Opel N, Lemke H, Fingas S, Förster K, Hahn T, Jansen A, Andlauer TFM, Forstner AJ, Heilmann-Heimbach S, Hall ASM, Awasthi S, Ripke S, Witt SH, Rietschel M, Müller-Myhsok B, Nöthen MM, Dannlowski U, Krug A, Streit F and Kircher T (2020) Polygenic risk for schizophrenia and schizotypal traits in non-clinical subjects. Psychological Medicine, 1–11 (in press). [DOI] [PubMed] [Google Scholar]
- Paksarian D, Trabjerg BB, Merikangas KR, Mors O, Børglum AD, Hougaard DM, McGrath JJ, Pedersen CB, Mortensen PB and Agerbo E (2018) The role of genetic liability in the association of urbanicity at birth and during upbringing with schizophrenia in Denmark. Psychological Medicine 48, 305–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parade SH, Huffhines L, Daniels TE, Stroud LR, Nugent NR and Tyrka AR (2021) A systematic review of childhood maltreatment and DNA methylation: candidate gene and epigenome-wide approaches. Translational Psychiatry 1, 1–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasman JA, Verweij KJH, Gerring Z, Stringer S, Sanchez-Roige S, Treur JL, Abdellaoui A, Nivard MG, Baselmans BML, Ong J-S, Ip HF, van der Zee MD, Bartels M, Day FR, Fontanillas P, Elson SL, 23andMe Research Team, de Wit H, Davis LK, MacKillop J, Substance Use Disorders Working Group of the Psychiatric Genomics Consortium, International Cannabis Consortium, Derringer JL, Branje SJT, Hartman CA, Heath AC, van Lier PAC, Madden PAF, Mägi R, Meeus W, Montgomery GW, Oldehinkel AJ, Pausova Z, Ramos-Quiroga JA, Paus T, Ribases M, Kaprio J, Boks MPM, Bell JT, Spector TD, Gelernter J, Boomsma DI, Martin NG, MacGregor S, Perry JRB, Palmer AA, Posthuma D, Munafò MR, Gillespie NA, Derks EM and Vink JM (2018) GWAS Of lifetime cannabis use reveals new risk loci, genetic overlap with psychiatric traits, and a causal influence of schizophrenia. Nature Neuroscience 21, 1161–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peyrot WJ, Milaneschi Y, Abdellaoui A, Sullivan PF, Hottenga JJ, Boomsma DI and Penninx BWJH (2014) Effect of polygenic risk scores on depression in childhood trauma. The British Journal of Psychiatry 205, 113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignon B, Schürhoff F, Szöke A, Geoffroy PA, Jardri R, Roelandt J-L, Rolland B, Thomas P, Vaiva G and Amad A (2018) Sociodemographic and clinical correlates of psychotic symptoms in the general population: findings from the MHGP survey. Schizophrenia Research 193, 336–342. [DOI] [PubMed] [Google Scholar]
- Pignon B, Eaton S, Schürhoff F, Szöke A, McGorry P and O'Donoghue B (2019a) Residential social drift in the two years following a first episode of psychosis. Schizophrenia Research 210, 323–325. [DOI] [PubMed] [Google Scholar]
- Pignon B, Peyre H, Ferchiou A, van Os J, Rutten BPF, Murray RM, Morgan C, Leboyer M, Schürhoff F, Szöke A and EU-GEI WP2 Group Author (2019b) Assessing cross-national invariance of the Community Assessment of Psychic Experiences (CAPE). Psychological Medicine 49, 2600–2607. [DOI] [PubMed] [Google Scholar]
- Pignon B, Lajnef M, Kirkbride JB, Peyre H, Ferchiou A, Richard J-R, Baudin G, Tosato S, Jongsma HE, de Haan L, Tarricone I, Bernardo M, Velthorst E, Braca M, Arango C, Arrojo M, Bobes J, Del-Ben CM, Di Forti M, Gayer-Anderson C, Jones PB, La Cascia C, Lasalvia A, Menezes PR, Quattrone D, Sanjuán J, Selten J-P, Tortelli A, Llorca PM, van Os J, Rutten BPF, Murray RM, Morgan C, Leboyer M, Szöke A and Schürhoff F (2021) The independent effects of psychosocial stressors on subclinical psychosis: findings from the multinational EU-GEI study. Schizophrenia Bulletin 47, 1674–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pingault J-B, O'Reilly PF, Schoeler T, Ploubidis GB, Rijsdijk F and Dudbridge F (2018) Using genetic data to strengthen causal inference in observational research. Nature Reviews Genetics 9, 566–580. [DOI] [PubMed] [Google Scholar]
- Plomin R and von Stumm S (2018) The new genetics of intelligence. Nature Reviews Genetics 19, 148–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pries L-K, Gülöksüz S, Ten Have M, de Graaf R, van Dorsselaer S, Gunther N, Rauschenberg C, Reininghaus U, Radhakrishnan R, Bak M, Rutten BPF and van Os J (2018) Evidence that environmental and familial risks for psychosis additively impact a multidimensional subthreshold psychosis syndrome. Schizophrenia Bulletin 44, 710–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pries L-K, Ferro GAD, van Os J, Delespaul P, Kenis G, Lin BD, Luykx JJ, Richards AL, Akdede B, Binbay T, Altınyazar V, Yalınçetin B, Gümüş-Akay G, Cihan B, Soygür H, Ulaş H, Cankurtaran EŞ, Kaymak SU, Mihaljevic MM, Petrovic SA, Mirjanic T, Bernardo M, Mezquida G, Amoretti S, Bobes J, Saiz PA, García-Portilla MP, Sanjuan J, Aguilar EJ, Santos JL, Jiménez-López E, Arrojo M, Carracedo A, López G, González-Peñas J, Parellada M, Maric NP, Atbaşoğlu C, Ucok A, Alptekin K, Saka MC, Investigators GR and O of P (GROUP), Arango C, O'Donovan M, Tosato S, Rutten BPF and Gülöksüz S (2020a) Examining the independent and joint effects of genomic and exposomic liabilities for schizophrenia across the psychosis spectrum. Epidemiology and Psychiatric Sciences 29, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pries L-K, Klingenberg B, Menne-Lothmann C, Decoster J, van Winkel R, Collip D, Delespaul P, Hert MD, Derom C, Thiery E, Jacobs N, Wichers M, Cinar O, Lin BD, Luykx JJ, Rutten BPF, van Os J and Gülöksüz S (2020b) Polygenic liability for schizophrenia and childhood adversity influences daily-life emotion dysregulation and psychosis proneness. Acta Psychiatrica Scandinavica 141, 465–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pries L-K, van Os J, Ten Have M, de Graaf R, van Dorsselaer S, Bak M, Lin BD, van Eijk KR, Kenis G, Richards A, O'Donovan MC, Luykx JJ, Rutten BPF and Gülöksüz S (2020c) Association of recent stressful life events with mental and physical health in the context of genomic and exposomic liability for schizophrenia. JAMA Psychiatry 77, 1296–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S and Walker AM (1980) Concepts of interaction. American Journal of Epidemiology 112, 467–470. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW and Earls F (1997) Neighborhoods and violent crime: a multilevel study of collective efficacy. Science (New York, N.Y.) 277, 918–924. [DOI] [PubMed] [Google Scholar]
- Santoro ML, Ota V, de Jong S, Noto C, Spindola LM, Talarico F, Gouvea E, Lee SH, Moretti P, Curtis C, Patel H, Newhouse S, Carvalho CM, Gadelha A, Cordeiro Q, Bressan RA, Belangero SI and Breen G (2018) Polygenic risk score analyses of symptoms and treatment response in an antipsychotic-naive first episode of psychosis cohort. Translational Psychiatry 8, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sariaslan A, Fazel S, D'Onofrio BM, Långström N, Larsson H, Bergen SE, Kuja-Halkola R and Lichtenstein P (2016) Schizophrenia and subsequent neighborhood deprivation: revisiting the social drift hypothesis using population, twin and molecular genetic data. Translational Psychiatry 6, e796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schick A, van Winkel R, Lin BD, Luykx JJ, de Zwarte SMC, van Eijk KR, GROUP Investigators, Myin-Germeys I and Reininghaus U (2022) Polygenic risk, familial liability and stress reactivity in psychosis: an experience sampling study. Psychological Medicine, 1–10 (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schizophrenia Working Group of the Psychiatric Genomics Consortium (2014) Biological insights from 108 schizophrenia-associated genetic loci. Nature 511, 421–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulsinger F, Parnas J, Mednick S, Teasdale TW and Schulsinger H (1987) Heredity-environment interaction and schizophrenia. Journal of Psychiatric Research 21, 431–436. [DOI] [PubMed] [Google Scholar]
- Schürhoff F, Pignon B, Lajnef M, Denis R, Rutten B, Morgan C, Murray RM, Leboyer M, van Os J and Szöke A (2020) Psychotic experiences are associated with paternal age but not with delayed fatherhood in a large, multinational, community sample. Schizophrenia Bulletin 46, 1327–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seiler N, Nguyen T, Yung A and O'Donoghue B (2020) Terminology and assessment tools of psychosis: a systematic narrative review. Psychiatry and Clinical Neurosciences 74, 226–246. [DOI] [PubMed] [Google Scholar]
- Shi M, O'Brien KM and Weinberg CR (2020) Interactions between a polygenic risk score and non-genetic risk factors in young-onset breast cancer. Scientific Reports 10, 3242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorter KR and Miller BH (2015) Epigenetic mechanisms in schizophrenia. Progress in Biophysics and Molecular Biology 118, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeland OB, Frei O, Dale AM and Andreassen OA (2020) The polygenic architecture of schizophrenia – rethinking pathogenesis and nosology. Nature Reviews Neurology 16, 366–379. [DOI] [PubMed] [Google Scholar]
- Solmi F, Lewis G, Zammit S and Kirkbride JB (2020) Neighborhood characteristics at birth and positive and negative psychotic symptoms in adolescence: findings from the ALSPAC birth cohort. Schizophrenia Bulletin 46, 581–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Clair D (2009) Copy number variation and schizophrenia. Schizophrenia Bulletin 35, 9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefanis NC, Hanssen M, Smirnis NK, Avramopoulos DA, Evdokimidis IK, Stefanis CN, Verdoux H and van Os J (2002) Evidence that three dimensions of psychosis have a distribution in the general population. Psychological Medicine 32, 347–358. [DOI] [PubMed] [Google Scholar]
- Stefanis NC, Henquet C, Avramopoulos D, Smyrnis N, Evdokimidis I, Myin-Germeys I, Stefanis CN and van Os J (2007) COMT Val158Met moderation of stress-induced psychosis. Psychological Medicine 37, 1651–1656. [DOI] [PubMed] [Google Scholar]
- Strahilevitz M (1974) Possible interaction of environmental and biological factors in the etiology of schizophrenia: review and integration. Canadian Psychiatric Association Journal 19, 207–217. [DOI] [PubMed] [Google Scholar]
- Tortelli A, Nakamura A, Suprani F, Schürhoff F, Van der Waerden J, Szöke A, Tarricone I and Pignon B (2018) Subclinical psychosis in adult migrants and ethnic minorities: systematic review and meta-analysis. BJPsych Open 4, 510–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripoli G, Quattrone D, Ferraro L, Gayer-Anderson C, Rodriguez V, La Cascia C, La Barbera D, Sartorio C, Seminerio F, Tarricone I, Berardi D, Szöke A, Arango C, Tortelli A, Llorca P-M, de Haan L, Velthorst E, Bobes J, Bernardo M, Sanjuán J, Santos JL, Arrojo M, Del-Ben CM, Menezes PR, Selten J-P, EU-GEI WP2 Group, Jones PB, Jongsma HE, Kirkbride JB, Lasalvia A, Tosato S, Richards A, O'Donovan M, Rutten BP, van Os J, Morgan C, Sham PC, Murray RM, Murray GK and Di Forti M (2020) Jumping to conclusions, general intelligence, and psychosis liability: findings from the multi-centre EU-GEI case-control study. Psychological Medicine 51, 623–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trotta A, Iyegbe C, Forti MD, Sham PC, Campbell DD, Cherny SS, Mondelli V, Aitchison KJ, Murray RM, Vassos E and Fisher HL (2016) Interplay between schizophrenia polygenic risk score and childhood adversity in first-presentation psychotic disorder: a pilot study. PLoS One 11, e0163319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ and Knol MJ (2014) A tutorial on interaction. Epidemiologic Methods 3, 33–72. [Google Scholar]
- van Os J (2014) The many continua of psychosis. JAMA Psychiatry 71, 985–986. [DOI] [PubMed] [Google Scholar]
- van Os J, Kenis G and Rutten BPF (2010) The environment and schizophrenia. Nature 468, 203–212. [DOI] [PubMed] [Google Scholar]
- van Os J, Pries L-K, Delespaul P, Kenis G, Luykx JJ, Lin BD, Richards AL, Akdede B, Binbay T, Altınyazar V, Yalınçetin B, Gümüş-Akay G, Cihan B, Soygür H, Ulaş H, Cankurtaran EŞ, Kaymak SU, Mihaljevic MM, Petrovic SA, Mirjanic T, Bernardo M, Cabrera B, Bobes J, Saiz PA, García-Portilla MP, Sanjuan J, Aguilar EJ, Santos JL, Jiménez-López E, Arrojo M, Carracedo A, López G, González-Peñas J, Parellada M, Maric NP, Atbaşoğlu C, Ucok A, Alptekin K, Saka MC, Genetic Risk and Outcome Investigators (GROUP), Arango C, O'Donovan M, Rutten BPF and Gülöksüz S (2020) Replicated evidence that endophenotypic expression of schizophrenia polygenic risk is greater in healthy siblings of patients compared to controls, suggesting gene-environment interaction. The EUGEI study. Psychological Medicine 50, 1884–1897. [DOI] [PubMed] [Google Scholar]
- Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Read J, van Os J and Bentall RP (2012) Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin 38, 661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vassos E, Pedersen CB, Murray RM, Collier DA and Lewis CM (2012) Meta-analysis of the association of urbanicity with schizophrenia. Schizophrenia Bulletin 38, 1118–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vassos E, Di Forti M, Coleman J, Iyegbe C, Prata D, Euesden J, O'Reilly P, Curtis C, Kolliakou A, Patel H, Newhouse S, Traylor M, Ajnakina O, Mondelli V, Marques TR, Gardner-Sood P, Aitchison KJ, Powell J, Atakan Z, Greenwood KE, Smith S, Ismail K, Pariante C, Gaughran F, Dazzan P, Markus HS, David AS, Lewis CM, Murray RM and Breen G (2017) An examination of polygenic score risk prediction in individuals with first-episode psychosis. Biological Psychiatry 81, 470–477. [DOI] [PubMed] [Google Scholar]
- Verdoux H and van Os J (2002) Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophrenia Research 54, 59–65. [DOI] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS and Anderson NB (1997) Racial differences in physical and mental health socio-economic status, stress and discrimination. Journal of Health Psychology 2, 335–351. [DOI] [PubMed] [Google Scholar]
- Zammit S, Spurlock G, Williams H, Norton N, Williams N, O'Donovan MC and Owen MJ (2007) Genotype effects of CHRNA7, CNR1 and COMT in schizophrenia: interactions with tobacco and cannabis use. The British Journal of Psychiatry 191, 402–407. [DOI] [PubMed] [Google Scholar]
- Zammit S, Hamshere M, Dwyer S, Georgiva L, Timpson N, Moskvina V, Richards A, Evans DM, Lewis G, Jones P, Owen MJ and O'Donovan MC (2014) A population-based study of genetic variation and psychotic experiences in adolescents. Schizophrenia Bulletin 40, 1254–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J-P, Robinson D, Yu J, Gallego J, Fleischhacker WW, Kahn RS, Crespo-Facorro B, Vazquez-Bourgon J, Kane JM, Malhotra AK and Lencz T (2019) Schizophrenia polygenic risk score as a predictor of antipsychotic efficacy in first-episode psychosis. American Journal of Psychiatry 176, 21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zipursky RB (2014) Why are the outcomes in patients with schizophrenia so poor? The Journal of Clinical Psychiatry 75(suppl. 2), 20–24. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://doi.org/10.1017/S2045796022000464.
click here to view supplementary material
Data Availability Statement
Data is confidential and not available.