Abstract
Aims
Due to the recent rapid expansion of scooter sharing companies, there has been a dramatic increase in the number of electric scooter (e-scooter) injuries. Our purpose was to conduct a systematic review to characterize the demographic characteristics, most common injuries, and management of patients injured from electric scooters.
Methods
We searched PubMed, EMBASE, Scopus, and Web of Science databases using variations of the term “electric scooter”. We excluded studies conducted prior to 2015, studies with a population of less than 50, case reports, and studies not focused on electric scooters. Data were analyzed using t-tests and p-values < 0.05 were considered significant.
Results
We studied 5,705 patients from 34 studies. The mean age was 33.3 years (SD 3.5), and 58.3% (n = 3,325) were male. The leading mechanism of injury was falling (n = 3,595, 74.4%). Injured patients were more likely to not wear a helmet (n = 2,114; 68.1%; p < 0.001). The most common type of injury incurred was bony injuries (n = 2,761, 39.2%), of which upper limb fractures dominated (n = 1,236, 44.8%). Head and neck injuries composed 22.2% (n = 1,565) of the reported injuries, including traumatic brain injuries (n = 455; 2.5%), lacerations/abrasions/contusions (n = 500; 7.1%), intracerebral brain haemorrhages (n = 131; 1.9%), and concussions (n = 255; 3.2%). Standard radiographs comprised most images (n = 2,153; 57.7%). Most patients were treated and released without admission (n = 2,895; 54.5%), and 17.2% (n = 911) of injured patients required surgery. Qualitative analyses of the cost of injury revealed that any intoxication was associated with higher billing costs.
Conclusion
The leading injuries from e-scooters are upper limb fractures. Falling was the leading mechanism of injury, and most patients did not wear a helmet. Future research should focus on injury characterization, treatment, and cost.
Cite this article: Bone Jt Open 2022;3(9):674–683.
Keywords: Electric scooters, Systematic review, Fractures, Public health, haemorrhages, t-tests, traumatic brain injuries, upper limb fractures, bony injuries, contusions, neck injuries, concussions, radiographs, brain
Introduction
Electric scooters (e-scooters) have heavily increased in popularity over the past decade due to being an efficient, novel, environmentally conscious, and economically friendly mode of transportation. 1 Originally common in Europe and Asia, e-scooters recently became more plentiful in USA cities. 1,2 E-scooters can reduce vehicle traffic, 3 which in turn can reduce total emissions from combustion engines. 1 While e-scooters have proven to be a convenient and cost-effective solution to transportation gaps found in many cities, they have also introduced a novel public safety concern that clinicians and city officials must address.
Although e-scooter companies have released recommendations that scooter riders wear helmets and ride only on roadways rather than sidewalks, these recommendations are often not followed. 4 This may account for significant trauma incurred by riders, particularly head and bony injuries. 5,6 Additionally, dockless e-scooters are often parked in public areas and on sidewalks, creating pedestrian hazards. 4 Although the number of injuries attributed to motorized scooters continues to be a public health concern, adequate legislative changes have not yet been introduced in the USA to address the dangers of e-scooter use including falls, collision injuries, and motor vehicle accidents. 1
As e-scooter use continues to increase, it is important to better understand the medical and economic implications of injuries sustained from these devices. While it is known that there has been an increase in injuries secondary to e-scooter use, less is known about the most common circumstances leading to injury, injury patterns, and the injuries’ cost to society. Although there have been several studies on this topic, they have predominately focused on one or two hospitals in a particular city. 5-10 Therefore, there is a need to consolidate those studies and their data to draw conclusions about the broader effects of e-scooter injuries. The primary goal of this study is to conduct a systematic review to assess user demographic characteristics, overall injury locations and types, and orthopaedic fracture locations associated with e-scooters, with secondary goals of analyzing the management of these injuries and their cost to society. By providing a comprehensive overview of the literature, we hope to provide insight that can inform future legislation to improve e-scooter safety. Additionally, we hope to identify gaps in the current study and data collection of e-scooters to help guide future research.
Methods
Literature search and study selection
Following PRISMA guidelines, we searched PubMed, Embase, Scopus, and Web of Science databases using variations of the terms “motorized scooter”, “electric scooter”, “e-scooter”, “electric kick scooter”, and/or the popular scooter brands: Lime, Uber, Bird, Spin, Lyft, Scoot, Voi, Wind, Razor, Gotrax, Xiaomi, Segway, Apollo, Kaabo, Emove, Dualtron, Inokin, and Rion. To narrow the search to meet the objectives of the study, we added the terms “fractures”, “bones”, “trauma”, “wounds”, and “injuries”. A total of 390 references were found using these search criteria, out of which 208 were duplicates, leaving 182 to be reviewed (Supplementary Figure a). Two researchers independently screened the trials to ensure compatible screening criteria on COVIDENCE (Veritas Health Innovation, Australia).
Exclusion criteria included: studies conducted before 2015; case reports, presentations, or posters only; studies with a population of less than 50; and studies focusing on non e-scooter devices (e.g. personal mobility scooters, sitting scooters, ATVs, motorcycles, motorized bicycles). A total of 67 studies were initially excluded, and an additional 32 were excluded based upon full text review, leaving a total of 34 studies ultimately included.
Data extraction
Demographic data, injury location and type, and treatment and cost data were extracted from included articles by two independent reviewers (PS, MJ). If discordant data were extracted, both reviewers reviewed the study together to reach a consensus. Studies with good or fair quality of data, graded using the Newcastle Ottawa scale quality assessment form for cohort studies, were included in this analysis. 11
Statistical analysis
Pooled analyses were conducted to determine demographics and injury characteristics. Continuous variables were analyzed using t-tests with Welch’s correction, not assuming equal standard deviations (SDs) between the comparison groups. Categorical variables were analyzed using chi-squared tests. The p-value for statistical significance was set to 0.05.
To address possible causes of heterogeneity of the results, subgroup analyses were also performed, comparing USA-based studies with those conducted abroad. These were performed when each subgroup had data from five or more studies. The mean percentages for different variables were compared using independent-samples t-tests with Welch’s correction between subgroups and paired t-tests within subgroups. Analyses were conducted using GraphPad Prism v. 8.4.3 (GraphPad Software, USA).
Results
Study characteristics
Data on a total of 5,702 participants were collected from 34 studies. 5-9,12-40 The mean study duration was 390 days (95% confidence interval (CI) 282.9 to 496.7). On average, a person was injured every 3.08 days (95% CI 2.19 to 3.97). The majority of studies (n = 18; 53%) were conducted in the USA, followed by Europe (n = 9; 24%), and New Zealand/Australia (n = 5; 15%). More than half of studies (n = 18; 53%) reported data from one hospital, and 44% (n = 15) collected data from multiple hospitals. Six (17.6%) were prospective cohort studies and the rest were retrospective (Supplementary Table i).
Participants
The most common characteristics of those injured were white race (48.5%; n = 447), male sex (58.3%; n = 3,325), and mean age of 33.3 years (SD 3.5) (Table I). Nearly 25% of people injured were under the influence of alcohol (n = 815), and 20.0% (n = 236) were under the influence of other drugs (marijuana, cocaine, heroin, benzodiazepines). Overall, 68% of people injured were not wearing helmets (n = 2,114), and 5.6% were under the age of 18 (n = 139), the legal age to use e-scooters for most e-scooter companies. Nearly 30% of people were injured on their first time riding an e-scooter (n = 178).
Table I.
Participant and injury characteristics.
| Study characteristics | Total | p-value* |
|---|---|---|
| Mean age, yrs (SD) (n = 22) | 33.3 (3.5) | |
| Sex, n (%) (n = 34) | 5,702 | |
| Male | 3,325 (58.3) | < 0.001 |
| Female | 2,377 (41.7) | |
| Race, n (%) (n = 10) | ||
| White | 477 (48.5) | |
| Black | 16 (1.6) | |
| Asian | 113 (11.5) | |
| Hispanic | 117 (11.9) | |
| Native Hawaiian or Pacific Islander | 9 (0.9) | |
| European | 250 (25.4) | |
| Māori | 38 (3.9) | |
| Middle Eastern | 5 (0.5) | |
| Other | 76 (7.7) | |
| Alcohol, n (%) (n = 24) | < 0.001 | |
| Alcohol use | 815 (25.1) | |
| No use | 2,310 (71.0) | |
| Unknown | 128 (3.9) | |
| Utox, n (%) (n = 8) | < 0.001 | |
| Positive | 236 (20.3) | |
| Negative | 929 (79.7) | |
| Helmet, n (%) (n = 23) | < 0.001 | |
| Yes | 151 (4.9) | |
| No | 2,114 (68.1) | |
| Unknown | 839 (27.0) | |
| < 18 yrs, n (%) (n = 15) | 139/2,468 (5.6) | |
| First time rider, n (%) | 178/604 (29.4) | |
| Presentation, n (%) (n = 12) | < 0.001 | |
| Ambulance | 849 (39.3) | |
| Walk in | 1,312 (60.7) | |
| Day of week, n (%) (n = 7) | < 0.001 | |
| Weekday | 464 (54.6) | |
| Weekend | 386 (45.4) | |
| Time of day, n (%) (n = 14) | < 0.001 | |
| Night | 1,094 (42.1) | |
| Day | 1,509 (57.9) | |
| Mechanism of injury, n (%) (n = 20) | ||
| Fall | 2,419 (74.4) | |
| Struck object | 269 (8.3) | |
| Vehicle | 332 (10.2) | |
| Pedestrian | 100 (3.1) | |
| Malfunction | 13 (0.4) | |
| Other | 119 (3.7) | |
| Location, n (%) (n = 5) | ||
| Street | 361 (48.5) | |
| Sidewalk | 195 (26.2) | |
| Other | 41 (5.5) | |
| Unknown | 148 (19.9) |
Chi-squared test.
SD, standard deviation; utox, urine toxicology test.
Regarding presentation to the emergency department (ED), the majority of patients self-presented (60.7%, n = 1,312), whereas 39.3% presented via ambulance (n = 849). There was a significant difference between the proportion of riders injured during the week versus the weekend (p = < 0.001, chi-squared test) and those injured during the day versus at night, as defined between 6 pm and 6 am (p = < 0.001, chi-squared test). The most common mechanism of injury was falling (74.4%), followed by collision with a vehicle (10.2%) or another inanimate object (8.3%). Nearly one-third of people were injured on the street (48.5%), and 26.2% were injured on the sidewalk.
Injury characteristics
A total of 5,702 injuries were reported from the 34 included studies. The most common injury types were orthopaedic in nature (n = 2,761; 39,2%) (Table II). Soft-tissue injuries comprised 28.5% (n = 2,010) of total injuries and were further subcategorized into lacerations, abrasions, and contusions (19.1%, n = 1,347) or sprains, strains, and dislocations (5.1%; n = 357). Internal organ injuries were rare (0.3%; n = 24) and only reported in nine of the 34 studies. Dental injuries were slightly more common, comprising 1.3% of total injuries (n = 95). Overall, 17 studies reported head and neck injuries, the most frequent being lacerations, abrasions, and contusions (7.1%; n = 500), followed by concussions comprising 3.2% of injuries (n = 255). Traumatic brain injuries were reported in 2.5% of cases (n = 455), with 1.9% being some form of intracranial haemorrhage (n = 131). There was only one reported death.
Table II.
Types of injuries.
| Type of injury | n (%) | Studies, n |
|---|---|---|
| Total | 7,052 | |
| Bone | 2,761 (39.2) | 30 |
| Soft-tissue injury | 2,010 (28.5) | 21 |
| Lacerations/abrasions/contusions | 1,347 (19.1) | 20 |
| Sprain/strain/dislocation | 357 (5.1) | 15 |
| Internal organ | 24 (0.3) | 9 |
| Dental | 95 (1.3) | 10 |
| Head and neck | 1,565 (22.2) | 17 |
| Lacerations/abrasion/contusions | 500 (7.1) | 15 |
| TBI | 455 (2.5) | 9 |
| ICH | 131 (1.9) | 23 |
| Concussion | 255 (3.2) | 17 |
ICH, intracranial haemorrhage; TBI, traumatic brain injury.
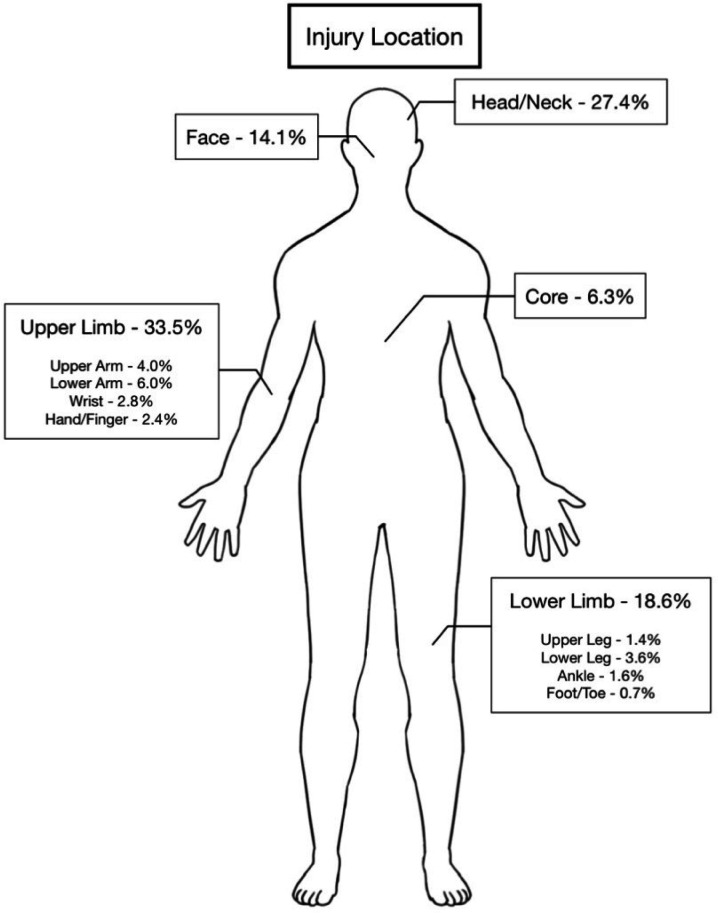
Of the total 7,502 injuries reported, 4,228 (56.4%) specified anatomical location. The most frequent location was the upper limb (n = 1,418; 33.5%), followed by head/neck (n = 1,157; 27.4%), lower limb (n = 787; 18.6%), and face (n = 598; 14.1%) (Figure 1).
Fig. 1.
Injury location.
Fracture characteristics
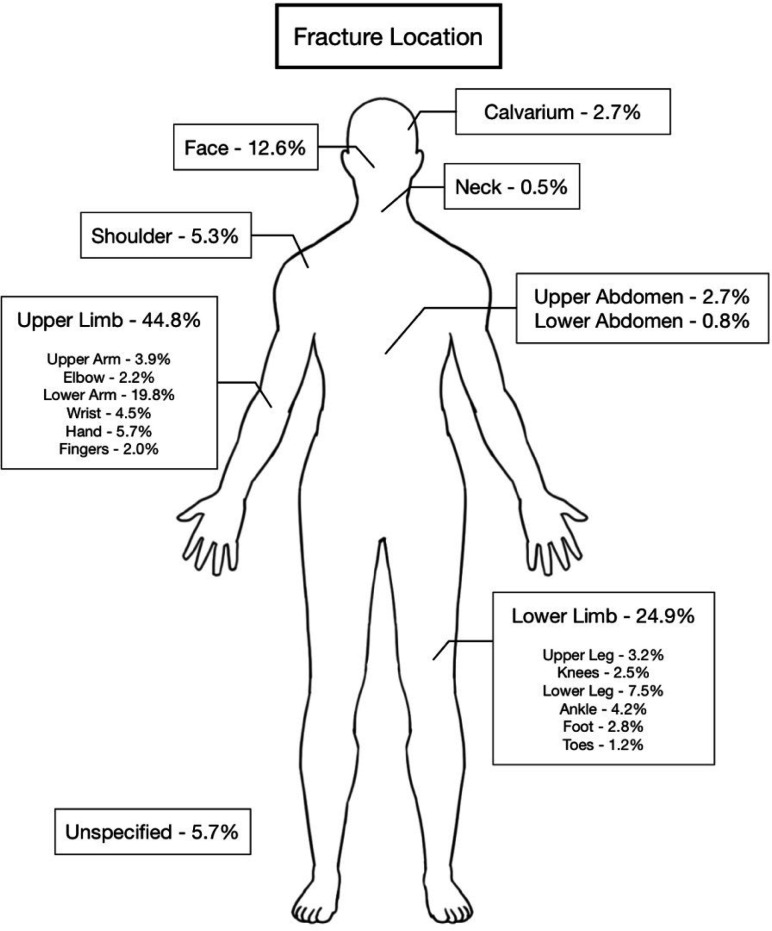
Upper limb fractures were most commonly sustained (n = 1,236; 44%), consisting of ulnar and radial fractures (n = 546; 19.8%) (Figure 2). Approximately one-quarter of fractures involved the lower limb, specifically the tibia and fibula (n = 208; 7.5%). Fractures involving the chest and pelvis occurred in 2.7% (n = 74) and 0.8% (n = 23) of cases, respectively. Five studies subcategorized facial fractures (12.6%). 5,7,8,27,39 The most documented of these were maxillary (27.6%; n = 96), orbit (17.8%; n = 62), nasal (15.2%; n = 53), and mandibular (11.8%; n = 41) fractures (Supplementary Table ii).
Fig. 2.
Fracture location.
Imaging and treatment
Of the total of 3,734 imaging studies performed, 57.7% (n = 2,153) were standard radiographs, 34.3% (n = 1,281) were CT scans, 0.9% (n = 33) were MRI studies, and 7.2% (n = 267) were ultrasounds or unspecified methods. Most patients were treated in the ED and released (54.5%), although 22.2% were admitted to an inpatient service (Table III). Over 900 patients (17.2%) required some form of surgery during their initial ED visit.
Table III.
Treatment disposition.
| Disposition | n (%) | Studies, n |
|---|---|---|
| Total | 5,308 | |
| Treated and released | 2,895 (54.5) | 26 |
| Admitted to inpatient | 1,178 (22.2) | 26 |
| Treated and transferred | 39 (0.7) | 5 |
| Left without treatment | 27 (0.5) | 3 |
| Held for observation | 23 (0.4) | 2 |
| ICU | 65 (1.2) | 11 |
| Outpatient | 170 (3.2) | 3 |
| Surgery | 911 (17.2) | 24 |
ICU, intensive care unit.
Cost analysis
Four of the included studies performed a cost analysis of e-scooter injuries; 7,12,15,23 two were conducted in the USA and two in New Zealand. 7,12,15,23 The two New Zealand studies were excluded from the qualitative analysis due to the differences in medical billing systems. Of the two studies based in the USA, Bloom et al 12 included all patients that incurred e-scooter injuries at their urban level I trauma centre, affiliated community hospital, urgent care clinics, and outpatient clinics, while Lavoie-Gagne et al 7 focused on e-scooter injury encounters just in their ED or trauma bay. Bloom et al 12 reported that the median facilities cost for these encounters was $1,213 (interquartile range (IQR) $499 to $3,312), although the facilities’ costs were greater for people under the influence of alcohol $2,674 (IQR $1,033 to $15,727) and marijuana $42,132 (IQR $9,695 to $110,095). Lavoie-Gagne et al 7 reported that the median total billing for these encounters was $50,432 (IQR $42,194 to $83,046). Their multivariable regression of total billing cost also revealed that any intoxication was associated with higher costs (p = 0.02).
Subgroup analysis
Due to the heterogeneity of data coming from several countries, subgroups stratified by country were analyzed. The mean age was comparable among all groups (overall 33.3 years (SD 3.5); USA 34.6 years (SD 3.1); non-USA 31.9 years (SD 3.7)). Even when stratified by sub-group the differences in sex, presentation to the hospital, helmet use, and alcohol use were all preserved (Table IV). Sub-group analysis was unable to be performed for other categories as there were less than five studies within each sub-group, limiting statistical power. Sub-group analysis was unable to be performed for other categories as there were less than five studies within each sub-group, limiting statistical power. Table IV
Table IV.
Subgroup analysis by demographic characteristics.
| Characteristic | Overall | USA | Non-USA | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Studies, n | p-value* | Mean (SD) | Studies, n | p-value* | Mean (SD) | Studies, n | p-value* | |
| Mean age, yrs (SD) | 33.3 (3.5) | 21 | 34.6 (3.1) | 11 | 31.9 (3.7) | 10 | |||
| Sex, n (%) | 34 | 18 | 16 | ||||||
| Male | 59.6 (8.1) | < 0.001 | 60.5 (7.4) | < 0.001 | 58.7 (9.0) | < 0.001 | |||
| Female | 41.2 (9.3) | 39.5 (7.4) | 43.0 (11.1) | ||||||
| Alcohol, n (%) | 23 | 14 | 9 | ||||||
| Alcohol use | 27.0 (19.9) | < 0.001 | 27.6 (17.8) | < 0.001 | 26.2 (23.8) | < 0.001 | |||
| No use | 69.9 (24.3) | 72.4 (17.8) | 66.0 (32.8) | ||||||
| Utox, n (%) (n = 8) | 8 | 4 | 4 | ||||||
| Positive | 25.5 (20.4) | < | < 0.001 | N/R | N/R | ||||
| Negative | 74.5 (20.4) | N/R | N/R | ||||||
| Helmet, n (%) (n = 23) | 23 | 11 | 12 | ||||||
| Yes | 5.2 (10.1) | < 0.001 | 3.0 (5.3) | < 0.001 | 7.3 (12.9) | < 0.001 | |||
| No | 69.4 (35.5) | 76.3 (29.8) | 63.1 (40.3) | ||||||
| < 18 yrs, % | 139/2522 (5.5) | 16 | 85/1591 (5.3) | 8 | 54/931 (5.8) | 8 | |||
| Presentation, n % | 12 | 6 | 6 | ||||||
| Ambulance | 36.9 (14.9) | < 0.001 | 42.0 (15.8) | < 0.001 | 31.8 (13.2) | < 0.001 | |||
| Walk in | 62.0 (14.8) | 58.0 (15.8) | 65.9 (14.0) | ||||||
| Time of day, n % | 14 | 5 | 9 | ||||||
| Night | 48.6 (42.7) | < 0.001 | 31.3 (19.9) | < 0.001 | 58.2 (49.8) | < 0.001 | |||
| Day | 67.7 (29.0) | 65.6 (18.2) | 68.9 (34.6) | ||||||
hi-squared test.
SD, standard deviation.
Even when comparing the mean percentages of injuries sustained in each subgroup, bony injuries remained the most common injury (47.4% (SD 29.0%)) in the USA. Although not statistically significant, there are differences between the USA and non-USA group; soft-tissue injuries (39.1% (SD 29.2%)), consisting of sprain and laceration/abrasions/contusions were more common in the non-US group than bony injuries (33.7% (SD 20.9%)). The upper limbs remained the foremost location injured (Table V).
Table V.
Subgroup analysis by injury characteristics.
| Characteristic | Overall analysis | USA | Non-USA | ||||
|---|---|---|---|---|---|---|---|
| Mean, % (SD)* | Studies, n | Mean, % (SD)* | Studies, n | Mean, % (SD)* | Studies, n | p-value† | |
| Mechanism of injury | |||||||
| Fall | 70.6 (26.2) | 17 | 56.5 (30.1) | 8 | 84.7 (10.4) | 9 | 0.024 |
| Struck object | 10.5 (21.2) | 17 | 18.6 (29.2) | 8 | 3.4 (5.4) | 9 | 0.187 |
| Vehicle | 11.0 (12.8) | 17 | 16.7 (16.0) | 8 | 5.3 (4.6) | 9 | 0.069 |
| Pedestrian | 2.2 (3.7) | 17 | 2.8 (5.1) | 8 | 1.7 (2.4) | 9 | 0.531 |
| Types of injuries | |||||||
| Bone | 40.6 (25.8) | 30 | 47.4 (29.0) | 15 | 33.7 (20.9) | 15 | 0.151 |
| Soft-tissue | 37.7 (23.3) | 26 | 35.9 (21.5) | 11 | 39.1 (29.2) | 15 | 0.727 |
| Lacerations | 35.7 (21.6) | 20 | 31.4 (19.6) | 7 | 38.0 (23.1) | 13 | 0.511 |
| Sprains | 13.5 (9.3) | 15 | 18.4 (9.7) | 6 | 10.2 (8.0) | 9 | 0.119 |
| Head and neck | 27.5 (15.1) | 26 | 23.2 (14.2) | 11 | 30.6 (15.3) | 15 | 0.218 |
| TBI | 11.0 (8.5) | 24 | 10.2 (9.0) | 14 | 12.2 (8.0) | 10 | 0.570 |
| ICH | 3.6 (4.0) | 22 | 4.9 (5.3) | 11 | 2.2 (1.6) | 11 | 0.127 |
| Concussion | 8.6 (6.7) | 16 | 7.6 (5.2) | 7 | 9.3 (7.9) | 9 | 0.604 |
| Injury location | |||||||
| Head and neck | 32.7 (20.7) | 24 | 28.4 (19.1) | 10 | 35.8 (22.0) | 14 | 0.391 |
| Face | 23.1 (16.2) | 17 | 27.4 (13.5) | 9 | 18.3 (18.5) | 8 | 0.276 |
| Core | 7.2 (4.6) | 21 | 7.7 (5.9) | 10 | 6.8 (3.2) | 11 | 0.660 |
| Upper limb | 40.7 (18.2) | 21 | 40.1 (18.6) | 13 | 41.7 (18.7) | 8 | 0.849 |
| Lower limb | 26.8 (18.1) | 20 | 28.0 (19.6) | 12 | 25.0 (16.7) | 8 | 0.723 |
| Fracture location | |||||||
| Skull/head | 5.1 (9.9) | 16 | 9.9 (13.9) | 7 | 1.3 (0.7) | 9 | 0.151 |
| Face | 10.3 (6.8) | 21 | 11.5 (8.7) | 9 | 9.4 (5.1) | 12 | 0.546 |
| Upper limb | 34.8 (31.0) | 27 | 37.3 (31.9) | 13 | 32.4 (31.1) | 14 | 0.691 |
| Lower limb | 21.6 (21.3) | 25 | 27.5 (23.4) | 12 | 16.3 (18.4) | 13 | 0.201 |
| Disposition | |||||||
| Treated and released | 70.7 (18.9) | 26 | 73.7 (19.2) | 14 | 67.2 (18.7) | 12 | 0.394 |
| Admitted to inpatient | 23.3 (12.0) | 26 | 18.9 (12.54) | 14 | 26.3 (10.7) | 12 | 0.119 |
| Surgery | 20.8 (13.8) | 24 | 14.4 (7.7) | 12 | 27.2 (15.8) | 12 | 0.023 |
Mean of the percentages reported by each study in the subgroup.
Independent-samples t-test with Welch’s correction between USA and non-USA subgroups.
ICH, intracranial haemorrhage; SD, standard deviation; TBI, traumatic brain injury.
There were only two variables that had a statistically significant difference between the subgroups: fall as the mechanism of injury and those that underwent a surgical procedure. More people were injured outside of the USA (84.7% (SD 10.4%)) by falling than in the USA (56.5% (SD 30.1%); p = 0.024, paired t-test) as well as underwent a surgical procedure (non-USA 27.2% (SD 15.8%), USA 14.4% (SD 7.7%); p = 0.023, paired t-test).
Discussion
Although several retrospective studies have analyzed the impact of motorized scooters on society, this is the first systematic review of the field and consolidates the findings of 34 studies worldwide. E-scooter use has greatly increased since 2017, when Lyft and Uber first introduced their ride-sharing services. 41 Unfortunately, the studies included in our review found that injuries and hospitalizations have also increased secondary to e-scooter use. Despite the numerous published studies analyzing e-scooters, our systematic review has shown that most provide only descriptive statistics, with an average of approximately 160 (mean 163 (SD 133)) included subjects. This pooling of data allowed us to collectively analyze 5,702 patients with a total of 7,502 injuries. We found that the most common injury was fractures of the upper limbs, and that more injuries occurred to first-time riders and riders not wearing helmets. Although data on the management of fractures and cost analyses were limited, the majority of patients were treated and released, with 20.8% undergoing an unspecified surgical procedure. With regard to cost, intoxication by alcohol or other drugs was associated with higher billing costs, perhaps because intoxicated riders have less control of their scooters and are more likely to sustain more complex or high-energy injuries, or perhaps their intoxicated status leads to longer hospital stays to reach baseline, resulting in increased hospital costs.
Trivedi et al 42 first analyzed e-scooter trauma in the USA. Since then, our systematic review found six more studies meeting our inclusion criteria were published in 2019, 12 more in 2020, and 15 more as of September 2021 (Supplementary Table ii). Most studies were retrospective in nature, and few analyzed risk factors associated with injury type, location, or severity. All USA-based studies similarly found that the most common characteristics of injured riders were white ethnicity, male sex, and mean age between 30 and 40 years. The reported use of alcohol varied drastically from 3% to 4%, 6,13 to as high as 85%. 14 The lack of helmet use was consistent across all the studies, with most reporting < 2% and one outlier reporting 46% helmet usage. 15
Interestingly, but not surprisingly, the most common injury reported was fracture, followed by soft-tissue injury and injury involving the head and neck. The most common fracture location was the distal limbs, mainly radial and ulnar fractures. Unfortunately, limited data were published regarding surgical details for the treatment of these fractures; however, roughly 16% of all injured riders required surgical intervention. Subgroup analyses revealed that those injured outside the USA were more likely to undergo a surgical procedure than those injured in the USA. Future research should further explore this difference.
While the current state of e-scooters poses public health safety concerns, legislative efforts both nationally and internationally have been slow in implementation, varying heavily based on country, state, and city. 43 In the USA, only nine states have a minimum age required for e-scooter riding, two of which have a minimum age as low as 12 years old. 44 Additionally, ten states require helmets for riders under the age of 18, and while no e-scooter company prohibits the use of helmets, they often state that riders are trusted to make responsible decisions regarding their health while riding. 44 Other studies also call for bolstering e-scooter regulations, particularly for children, since they experience a greater rate of fractures and polytrauma when compared to adults. 45 Sidewalk riding is not legal in 11 states, and only five states have declared a mandatory speed limit, ranging from 15 to 20 mph. 44 Although studies did not report the speed at the time of injury, it could be a useful variable to collect in the future, as it may aid in making evidence-based policy decisions to standardize a mandatory speed limit. Like the USA, Europe has variable laws regulating e-scooters, dependent by country. Minimum age requirements are as low as 12 years in some countries, and there is a wide range of speed limits that varies by country. 10,44
In our study, we found that 5.6% of riders injured were under the age of 18. Additionally, sidewalk accidents were a common location of injury, which indicates that legislature still needs to expand to prevent sidewalk riding. However, the presence of e-scooters on roads may be associated with an increase in motor vehicle accidents. Therefore, cities should consider the benefit of designated roadway spaces for e-scooters when renovating old or developing new infrastructure. Finally, upper limb injuries and head and neck injuries were the most common locations of injury mentioned in our study, which could potentially be reduced by increased mandating of protective gear such as helmets as well as elbow and wrist pads.
This systematic review shares the same limitations as the studies from which it pulls data. The patient population is predominantly composed of people presenting to the ED of local hospitals. This excludes patients who presented to outpatient care clinics or their primary care physicians, which may cause our data to both underestimate the total number of patients and injuries of lower severity, i.e. sprains, strains, lacerations, abrasions etc. This also potentially skews our data when considering patient access to care and insurance status. The inclusion of orthopaedic search terms could have skewed the injuries found, leading to more of an orthopaedic emphasis, excluding those more related to plastics or otolaryngology. The retrospective nature of the studies reflected their limited ability to assess certain data endpoints. This is compounded by the fact that several of the studies failed to assess certain variables such as injury location, urine toxicology reports, specific surgical treatment, or weekday of injury occurrence. Not all studies screened for helmet, alcohol use, or intoxication in all their patients, leading to an inaccurate representation of the total number of people injured affected by these conditions. Some variables were not clearly defined either, specifically “fall” as a mechanism of injury. This encompasses both falling from a stationary and moving scooter, which have different injury biomechanics. Additionally, most studies provided minimal descriptions on how they characterized mechanisms of injury, making it difficult for readers to understand the difference between similar sounding mechanisms. Aside from one study that analyzed data from a USA national database, 3 all other included studies focused on a small number of sites and are therefore limited by sampling bias from various geographical and urban planning factors. Another limitation is that some studies were conducted throughout the initial quarantine period associated with the COVID-19 pandemic, during which there was a universal decline in e-scooter usage. Along similar lines, the variable duration of these studies may skew data, as usage will change depending upon seasonal weather.
Despite these limitations, this multivariable systematic review of e-scooter implications is the most comprehensive of its kind in the literature with respect to the metrics that are evaluated. Further study is necessary to understand the orthopaedic impacts such as fracture types and the specific treatments and costs associated with them. Additionally, overall injury prevention and injury mitigation should be studied, such as encouraging helmet and elbow/wrist guard use and improving training, especially given the prevalence of injury with first-time use.
Upper limb fractures were the most common injury type incurred from e-scooter use, and the most common demographic characteristics were white males in their early 30s. There should be more emphasis on wearing protective gear like wrist and elbow guards in addition to helmets. Future prospective studies with larger cohorts across multiple regions and hospitals are necessary to truly characterize the nature and cost of e-scooter injuries.
Take home message
- There should be increased emphasis on e-scooter riders wearing protective gear, especially on their upper limbs, as this is the most common location for injury.
- Orthopaedic injuries are the most common e-scooter injuries, and the most common mechanism of injury is falling.
- Further state and national policy implementations are needed to reduce the increasing prevalence of e-scooter injuries.
Acknowledgements
We would like to acknowledge Katie Lobner, MLIS, for assisting with the creation of search terms and for conducting the intial literature search for this study.
Footnotes
Author contributions: P. Singh: Conceptualization, Methodology, Investigation, Data curation, Formal analysis, Writing – original draft, Writing – review & editing.
M. Jami: Methodology, Data curation, Writing – original draft, Writing – review & editing.
J. Geller: Conceptualization, Writing – review & editing.
C. Granger: Conceptualization, Writing – review & editing.
L. Geaney: Conceptualization, Writing – review & editing.
A. Aiyer: Conceptualization, Project administration, Writing – original draft, Writing – review & editing.
Funding statement: The authors received no financial or material support for the research, authorship, and/or publication of this article. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
ICMJE COI statement: Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
Open access funding: Funding for open access was provided for by the authors’ personal academic funds.
Twitter: Follow A. Aiyer @orthomentor and @momentummed
Supplementary material: Tables containing information regarding the PRISMA outline used for this systematic review, characteristics of the 34 studies included, and the location of facial fractures incurred in the e-scooter injured population.
Contributor Information
Priya Singh, Email: psingh34@jh.edu.
Meghana Jami, Email: mjami2@jh.edu.
Joseph Geller, Email: joseph.s.geller@gmail.com.
Caroline Granger, Email: c.granger@wustl.edu.
Lauren Geaney, Email: lageaney@uchc.edu.
Amiethab Aiyer, Email: tabsaiyer@gmail.com.
References
- 1. Bresler AY, Hanba C, Svider P, Carron MA, Hsueh WD, Paskhover B. Craniofacial injuries related to motorized scooter use: a rising epidemic. Am J Otolaryngol. 2019;40(5):662–666. 10.1016/j.amjoto.2019.05.023 [DOI] [PubMed] [Google Scholar]
- 2. Dickey MR. Electric scooters are going worldwide. TechCrunch. 2018. https://techcrunch.com/2018/08/12/electric-scooters-all-over-the-world/ (date last accessed 3 August 2022).
- 3. Namiri NK, Lui H, Tangney T, Allen IE, Cohen AJ, Breyer BN. Electric scooter injuries and hospital admissions in the United States, 2014-2018. JAMA Surg. 2020;155(4):357–359. 10.1001/jamasurg.2019.5423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Choron RL, Sakran JV. The integration of electric scooters: useful technology or public health problem? Am J Public Health. 2019;109(4):555–556. 10.2105/AJPH.2019.304955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Puzio TJ, Murphy PB, Gazzetta J, et al. The electric scooter: a surging new mode of transportation that comes with risk to riders. Traffic Inj Prev. 2020;21(2):175–178. 10.1080/15389588.2019.1709176 [DOI] [PubMed] [Google Scholar]
- 6. Trivedi TK, Liu C, Antonio ALM, et al. Injuries associated with standing electric scooter use. JAMA Netw Open. 2019;2(1):e187381. 10.1001/jamanetworkopen.2018.7381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lavoie-Gagne O, Siow M, Harkin WE, et al. Financial impact of electric scooters: a review of injuries over 27 months at an urban level 1 trauma center (cost of e-scooter injuries at an urban level 1 trauma center). Trauma Surg Acute Care Open. 2021;6(1):e000634. 10.1136/tsaco-2020-000634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mukhtar M, Ashraf A, Frank MS, Steenburg SD. Injury incidence and patterns associated with electric scooter accidents in a major metropolitan city. Clin Imaging. 2021;74:163–168. 10.1016/j.clinimag.2021.02.005 [DOI] [PubMed] [Google Scholar]
- 9. Brownson AB, Fagan PV, Dickson S, Civil ID. Electric scooter injuries at Auckland City Hospital. N Z Med J. 2019;132(1505):62–72. [PubMed] [Google Scholar]
- 10. Franks J. E-scooter rules still varied – and changing – across Europe. Fleet Europe. 2021. https://www.fleeteurope.com/en/last-mile/europe/features/e-scooter-rules-still-varied-and-changing-across-europe (date last accessed 17 August 2022).
- 11. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses Ottawa Hospital research Institute. 2021. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (date last accessed 17 August 2022).
- 12. Bloom MB, Noorzad A, Lin C, et al. Standing electric scooter injuries: impact on a community. Am J Surg. 2021;221(1):227–232. 10.1016/j.amjsurg.2020.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Genc Yavuz B, Zengin Temel T, Satilmis D, Güven R, Çolak Ş. Analysis of electric scooter injuries admitted to the emergency service. Ir J Med Sci. 2022;191(2):915–918. 10.1007/s11845-021-02628-w [DOI] [PubMed] [Google Scholar]
- 14. Kleinertz H, Ntalos D, Hennes F, Nüchtern JV, Frosch K-H, Thiesen DM. Accident mechanisms and injury patterns in e-scooter users. Dtsch Ärztebl Int. 2021;118:117–121. 10.3238/arztebl.m2021.0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mitchell G, Tsao H, Randell T, Marks J, Mackay P. Impact of electric scooters to a tertiary emergency department: 8-week review after implementation of a scooter share scheme. Emerg Med Australas. 2019;31(6):930–934. 10.1111/1742-6723.13356 [DOI] [PubMed] [Google Scholar]
- 16. No authors listed . Dockless electric scooter-related injuries study. Austin Public Health. 2019. APH_Dockless_Electric_Scooter_Study_5-2-19.pdf (date last accessed 3 August 2022).
- 17. Badeau A, Carman C, Newman M, Steenblik J, Carlson M, Madsen T. Emergency department visits for electric scooter-related injuries after introduction of an urban rental program. Am J Emerg Med. 2019;37(8):1531–1533. 10.1016/j.ajem.2019.05.003 [DOI] [PubMed] [Google Scholar]
- 18. Kobayashi LM, Williams E, Brown CV, et al. The e-merging e-pidemic of e-scooters. Trauma Surg Acute Care Open. 2019;4(1):e000337. 10.1136/tsaco-2019-000337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mayhew LJ, Bergin C. Impact of e-scooter injuries on Emergency Department imaging. J Med Imaging Radiat Oncol. 2019;63(4):461–466. 10.1111/1754-9485.12889 [DOI] [PubMed] [Google Scholar]
- 20. Alwani M, Jones AJ, Sandelski M, et al. Facing facts: facial injuries from stand-up electric scooters. Cureus. 2020;12(1):e6663. 10.7759/cureus.6663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bauer F, Riley JD, Lewandowski K, Najafi K, Kepros J. Traumatic injuries associated with standing motorized scooters. JAMA Netw Open. 2020;3(3):e201925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Beck S, Barker L, Chan A, Stanbridge S. Emergency department impact following the introduction of an electric scooter sharing service. Emerg Med Australas. 2020;32(3):409–415. 10.1111/1742-6723.13419 [DOI] [PubMed] [Google Scholar]
- 23. Bekhit MNZ, Le Fevre J, Bergin CJ. Regional healthcare costs and burden of injury associated with electric scooters. Injury. 2020;51(2):271–277. 10.1016/j.injury.2019.10.026 [DOI] [PubMed] [Google Scholar]
- 24. Dhillon NK, Juillard C, Barmparas G, et al. Electric scooter injury in Southern California trauma centers. J Am Coll Surg. 2020;231(1):133–138. 10.1016/j.jamcollsurg.2020.02.047 [DOI] [PubMed] [Google Scholar]
- 25. English KC, Allen JR, Rix K, et al. The characteristics of dockless electric rental scooter-related injuries in a large U.S. city. Traffic Inj Prev. 2020;21(7):476–481. 10.1080/15389588.2020.1804059 [DOI] [PubMed] [Google Scholar]
- 26. Faraji F, Lee JH, Faraji F, et al. Electric scooter craniofacial trauma. Laryngoscope Investig Otolaryngol. 2020;5(3):390–395. 10.1002/lio2.380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ishmael CR, Hsiue PP, Zoller SD, et al. An early look at operative orthopaedic injuries associated with electric scooter accidents: bringing high-energy trauma to a wider audience. J Bone Joint Surg Am. 2020;102-A(5):e18. 10.2106/JBJS.19.00390 [DOI] [PubMed] [Google Scholar]
- 28. Nellamattathil M, Amber I. An evaluation of scooter injury and injury patterns following widespread adoption of E-scooters in a major metropolitan area. Clin Imaging. 2020;60(2):200–203. 10.1016/j.clinimag.2019.12.012 [DOI] [PubMed] [Google Scholar]
- 29. Siow MY, Lavoie-Gagne O, Politzer CS, et al. Electric scooter orthopaedic injury demographics at an urban Level I trauma center. J Orthop Trauma. 2020;34(11):e424–e429. 10.1097/BOT.0000000000001803 [DOI] [PubMed] [Google Scholar]
- 30. Störmann P, Klug A, Nau C, et al. Characteristics and injury patterns in electric-scooter related accidents-a prospective two-center report from Germany. J Clin Med. 2020;9(5):1569. 10.3390/jcm9051569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cicchino JB, Kulie PE, McCarthy ML. Severity of e-scooter rider injuries associated with trip characteristics. J Safety Res. 2021;76:256–261. 10.1016/j.jsr.2020.12.016 [DOI] [PubMed] [Google Scholar]
- 32. Coelho A, Feito P, Corominas L, et al. Electric scooter-related injuries: A new epidemic in orthopedics. J Clin Med. 2021;10(15):3283. 10.3390/jcm10153283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Harbrecht A, Hackl M, Leschinger T, et al. What to expect? Injury patterns of electric-scooter accidents over a period of one year - a prospective monocentric study at a Level 1 trauma center. Eur J Orthop Surg Traumatol. 2022;32(4):641–647. 10.1007/s00590-021-03014-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Heuer S, Landschoof S, Kornherr P, Grospietsch B, Kühne CA. Epidemiology and injury pattern of e-scooter injuries - initial results. Z Orthop Unfall. 2021. 10.1055/a-1419-0584 [DOI] [PubMed] [Google Scholar]
- 35. Kim M, Lee S, Ko DR, Kim D-H, Huh J-K, Kim J-Y. Craniofacial and dental injuries associated with stand-up electric scooters. Dent Traumatol. 2021;37(2):229–233. 10.1111/edt.12620 [DOI] [PubMed] [Google Scholar]
- 36. Moftakhar T, Wanzel M, Vojcsik A, et al. Incidence and severity of electric scooter related injuries after introduction of an urban rental programme in Vienna: a retrospective multicentre study. Arch Orthop Trauma Surg. 2021;141(7):1207–1213. 10.1007/s00402-020-03589-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nielsen KI, Nielsen FE, Rasmussen SW. Injuries following accidents with electric scooters. Dan Med J. 2021;68(2):A09200697. [PubMed] [Google Scholar]
- 38. Shichman I, Shaked O, Factor S, Elbaz E, Khoury A. Epidemiology of fractures sustained during electric scooter accidents: a retrospective review of 563 cases. J Bone Joint Surg Am. 2021;103-A(12):1125–1131. 10.2106/JBJS.20.01746 [DOI] [PubMed] [Google Scholar]
- 39. Shiffler K, Mancini K, Wilson M, Huang A, Mejia E, Yip FK. Intoxication is a significant risk factor for severe craniomaxillofacial injuries in standing electric scooter accidents. J Oral Maxillofac Surg. 2021;79(5):1084–1090. 10.1016/j.joms.2020.09.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Uluk D, Lindner T, Dahne M, et al. E-scooter incidents in Berlin: an evaluation of risk factors and injury patterns. Emerg Med J. 2022;39(4):295–300. 10.1136/emermed-2020-210268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kaufman SM, Buttenwieser L. The State of Scooter Sharing in United States Cities. Rudin Center for Transportation New York University Robert F. Wagner School for Public Service. 2018. https://wagner.nyu.edu/files/faculty/publications/Rudin_ScooterShare_Aug2018_0.pdf (date last accessed 17 August 2022).
- 42. Trivedi B, Kesterke MJ, Bhattacharjee R, Weber W, Mynar K, Reddy LV. Craniofacial injuries seen with the introduction of bicycle-share electric scooters in an urban setting. J Oral Maxillofac Surg. 2019;77(11):2292–2297. 10.1016/j.joms.2019.07.014 [DOI] [PubMed] [Google Scholar]
- 43. Lee KC, Naik K, Wu BW, Karlis V, Chuang S-K, Eisig SB. Are motorized scooters associated with more severe craniomaxillofacial injuries? J Oral Maxillofac Surg. 2020;78(9):1583–1589. 10.1016/j.joms.2020.04.035 [DOI] [PubMed] [Google Scholar]
- 44. No authors listed . The Comprehensive Guide to Electric Scooter Laws. UNAGI. 2021. https://unagiscooters.com/articles/the-2021-comprehensive-guide-to-electric-scooter-laws/?_gl=1%2ajb0aqo%2a_ga%2aNzM0MDgzOTQ2LjE2MzY2Njg0NTY.%2a_ga_8C7B7DM578%2aMTYzNjY2ODQ1Ni4xLjEuMTYzNjY2ODc0Ni4w (date last accessed 17 August 2022).
- 45. Cohen LL, Geller JS, Yang BW, Allegra PR, Dodds SD. Pediatric injuries related to electric scooter use: a national database review. J Pediatr Orthop B. 2022;31(2):e241–e245. 10.1097/BPB.0000000000000879 [DOI] [PubMed] [Google Scholar]