Abstract
Long noncoding RNAs are involved in epigenetic gene modification, including binding to the chromatin rearrangement complex in pre-transcriptional regulation and to gene promoters in gene expression regulation, as well as acting as microRNA sponges to control messenger RNA levels in post-transcriptional regulation. An increasing number of studies have found that long noncoding RNA plasmacytoma variant translocation 1 (PVT1) plays an important role in cancer development. In this review of a large number of studies on PVT1, we found that PVT1 is closely related to tumor onset, proliferation, invasion, epithelial–mesenchymal transformation, and apoptosis, as well as poor prognosis and radiotherapy and chemotherapy resistance in some cancers. This review comprehensively describes PVT1 expression in various cancers and presents novel approaches to the diagnosis and treatment of cancer.
Keywords: Long noncoding RNA, PVT1, Oncogene, Cancer
Introduction
Cancer death rate has continuously declined in the past 2 years, although it remains the second leading cause of death worldwide according to the latest cancer statistics from the USA [1]. Changes at the gene level include gene mutations, amplification, deletion, DNA methylation, and insertion mutations. Abnormal oncogene activation and tumor suppressor gene inactivation are important factors that lead to the occurrence of cancer. Advances in genetic research have revealed the pathogenesis of many cancers, which has led to the development of effective treatments. For example, leukemia caused by breakpoint cluster region–Abelson mutations can be effectively cured using imatinib [2]. Protein-coding genes account for < 2% of the total genome. The remaining genome consists of noncoding genes that are responsible for the vast majority of tumorigenesis.
Long noncoding RNAs (lncRNAs) are RNAs that are longer than 200 nucleotides. lncRNAs are located in the nucleus or cytoplasm of eukaryotic cells and have a variety of functions, including regulating gene expression in both a cis and a trans manner, acting as a sponge for microRNA (miRNA), and directly affecting proteins and other RNAs [3]. In the early twentieth century, the lncRNA X-inactive specific transcript was first discovered, wrapping the X chromosome in a cis-like manner, resulting in silencing of the entire chromosome. lncRNAs have been discovered and have been proven to play important roles in many diseases and cell development and as biomarkers. For example, abnormal MALAT1 expression promotes the development of bladder cancer [4]. lncRNAs in kinase activation are associated with poor prognosis in patients with breast or lung cancer [5]. However, the mechanism by which lncRNAs regulate tumor development remains unclear, and further studies are needed to explore and summarize the potential mechanisms of action of lncRNAs.
The lncRNA plasmacytoma variant translocation 1 (PVT1), which is located on the telomeres of chromosome 8 in the c-Myc gene, was first reported by Guan et al. [5]. Recently, abnormal PVT1 expression was found in a variety of human malignancies, including non-small cell lung cancer (NSCLC) [6], nasopharyngeal carcinoma (NPC) [7], gastric cancer (GC) [8], oral squamous cell carcinoma (OSCC) [9], esophageal cancer (EC) [10], colorectal cancer (CRC) [11], hepatocellular carcinoma (HCC) [12], gallbladder cancer (GBC) [13], cholangiocarcinoma (CCA) [14], pancreatic cancer (PC) [15], breast cancer (BC) [16], cervical cancer (CC) [17], endometrial cancer [18], ovarian cancer (OC) [19], renal cell carcinoma (RCC) [20], bladder cancer [21], prostate cancer (PCa) [22], glioma [23], osteosarcoma (OS) [24], multiple myeloma (MM) [25], thyroid cancer (TC) [26], lymphoma [27], and leukemia [28]. Identifying the mechanisms of action of various cancers has helped researchers discover new biomarkers and therapeutic targets. Here, we aimed to identify new biomarkers and therapeutic targets by summarizing the mechanisms of PVT1 in various cancers.
Functions of lncRNA
Many studies have shown that lncRNAs play vital roles as biomarkers in cancer diagnosis, therapeutic targets, prognosis, drug sensitizers, stratification, and other aspects [6–11].
lncRNAs can regulate chromatin topology by binding to H3K4me3 and H3K36me3 and through histone acetylation and other activated histone modifications to promote gene transcription [29]. Conversely, lncRNAs induce chromatin closure by binding to H3K9me3, H3K27me3, and H4K20me3 and through DNA methylation and other suppressive histone modification factors [30]. lncRNAs can serve as a central platform for assembling relevant molecular components, binding to nucleic acids through sequence complementation, and binding to proteins through RNA structural elements [31–33]. A variety of signaling pathways rely on scaffolds to deliver precise signals. lncRNAs can bind to multiple effector elements in the same space at the same time and integrate the information of the depression effector elements or activity effector elements. lncRNAs act as decoys and can directly bind to proteins, messenger RNAs (mRNAs), and miRNAs [34–36]. Accumulating evidence suggests that the decoy function of lncRNAs plays an irreplaceable role in tumor initiation, progression, and metastasis.
Role of PVT1 in various human tumors
PVT1 is abnormally overexpressed in a variety of cancers and often promotes the occurrence, progression, invasion, metastasis, and chemoradiotherapy resistance in tumors by interacting with c-Myc [37–40]. The most common mechanism of PVT1 in various cancers is regulation of the relevant signaling pathways by competitive endogenous RNA (ceRNA), which promotes the occurrence and development of cancer. PVT1 can also directly regulate RNA, DNA, and protein expression. For example, in NPC, PVT1 stabilizes the structure of c-Myc by preventing its phosphorylation, promoting DNA repair in NPC cells, and increasing radiotherapy resistance [7]. In addition, PVT1 acts as a scaffold to regulate downstream genes and pathways. For example, in NPC, PVT1 promotes H3K9 acetylation by recruiting KAT2A [41]. PVT1 can recruit EZH2 to the promoter region of LAST2 and inhibit LAST2 expression in patients with NSCLC [42]. Similarly, PVT1 regulates P15/P16 and vascular endothelial growth factor (VEGF)A expression by recruiting EZH2 and signal transducer and activator of transcription (STAT)3 in GC cells [43]. In addition, PVT1 recruits EZH2 to downregulate miR-214 and P53 expression in HCC cells [44]. PVT1 regulates EZH2 binding to ANGPTL4 in CCA cells to inactivate its promoter region and reduce its expression [45]. In CC cells, PVT1 reduces the miR-200b expression by recruiting EZH2 to the promoter region of miR-200b [46]. In androgen-independent castration-resistant PCa, the promoter region of NOV is bound by EZH2 recruited by PVT1, which ultimately inhibits NOV expression [47]. In TC, PVT1 also promotes the proliferation of TC cells by recruiting EZH2, thereby affecting its expression of TSHR [26]. In general, PVT1 overexpression is associated with poor prognosis [48–51]. However, in the early stages of some cancers, such as OC, it predicts a good prognosis [52]. Recently, several studies have shown that PVT1 is involved in the clinical and pathological development of various cancers. The functions and mechanisms of action of PVT1 in human tumors are listed in Tables 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11 and 12.
Table 1.
Functional characterization of PVT1 in respiratory system tumors
| Tumor type | Expression | Role | Function role | miRNAs | Related genes | References |
|---|---|---|---|---|---|---|
| Nasopharyngeal carcinoma | Upregulation | Oncogene | Proliferation | miR-1207 | PI3K/AKT | [54] |
| Nasopharyngeal carcinoma | Upregulation | Oncogene | Proliferation and radioresistance | miR-515-5p | PIK3CA | [55] |
| Lung cancer | Upregulation | Oncogene | Proliferation | / | P15/P21 | [6] |
| Lung cancer | Upregulation | Oncogene | Invasion and proliferation | miR-497 | / | [56] |
| Lung cancer | Upregulation | Oncogene | Proliferation | / | LATS2 | [42] |
| Lung cancer | Upregulation | Oncogene | Proliferation, migration, invasion, and EMT | miR-497 | YAP1 | [57] |
| Lung cancer | Upregulation | Oncogene | Proliferation and migration | miR-526b | EZH2 | [58] |
| Lung cancer | Upregulation | Oncogene | Invasion | miR-200a/200b | MMP9 | [59] |
| Lung cancer | Upregulation | Oncogene | Proliferation | miR-199a-5p | HIF-1α | [60] |
| Lung cancer | Upregulation | Oncogene | Angiogenesis | miR-29c | VEGF | [61] |
| Lung cancer | Upregulation | Oncogene | Proliferation and metastasis | miR-128 | VEGFC | [62] |
| Lung cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-361-3p | SOX9 | [63] |
| Lung cancer | Upregulation | Oncogene | Migration and invasion | miR-760 | IL-6 | [64] |
| Lung cancer | Upregulation | Oncogene | Proliferation | miR-17-5p | BAMBI | [65] |
| Lung cancer | Upregulation | Oncogene | Proliferation and migration | miR-148 | RAB34 | [66] |
| Lung cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-551b | FGFR1 | [67] |
| Lung cancer | Upregulation | Oncogene | Invasion and growth | miR-378c | SLC2A1 | [68] |
| Lung cancer | Upregulation | Oncogene | Radioresistance | miR-195 | / | [69] |
| Lung cancer | Upregulation | Oncogene | Radioresistance | miR-424-5p | CARM1 | [70] |
| Lung cancer | Upregulation | Oncogene | Cisplatin-resistance | miR-181a-5p | SP1 | [71] |
| Lung cancer | Upregulation | Oncogene | Cisplatin-resistance | miR-216b | Beclin-1 | [72] |
Table 2.
Main characteristics of the studies included in the review of respiratory system tumors
| Study | Tumor type | Sample size (normal: tumor) | Detection method | P value | TNM (P value) | LNM (P value) | DM (P value) | OS (P value) | DFS (P value) | References |
|---|---|---|---|---|---|---|---|---|---|---|
| Cui | Nasopharyngeal carcinoma | 15:15 | qRT-PCR | < 0.001 | / | / | / | 0.0385 | 0.0261 | [54] |
| Cui | Lung cancer | 108:108 | qRT-PCR | < 0.05 | 0.003 | < 0.001 | 0.571 | 0.014 | 0.036 | [6] |
| Wan | Lung cancer | 105:105 | qRT-PCR | < 0.05 | 0.001 | 0.011 | / | / | / | [42] |
| Chen | Lung cancer | 80:80 | qRT-PCR | < 0.0001 | / | / | / | / | / | [59] |
| Qi | Lung cancer | 30:30 | qRT-PCR | < 0.05 | / | / | / | / | / | [63] |
| Wu | Lung cancer | 31:31 | qRT-PCR | < 0.05 | 0.017 | 0.018 | / | / | / | [69] |
| Chen | Lung cancer | 40:40 | qRT-PCR | < 0.05 | 0.01 | 0.0146 | / | / | / | [72] |
Table 3.
Functional characterization of PVT1 in digestive system tumors
| Tumor type | Expression | Role | Function role | miRNAs | Related genes | References |
|---|---|---|---|---|---|---|
| Oral squamous cell carcinoma | Upregulation | Oncogene | Proliferation, invasion, and migration | miR-150-5p | GLUT-1 | [9] |
| Oral squamous cell carcinoma | Upregulation | Oncogene | Proliferation and chemoresistance | miR-194-5p | HIF1a | [75] |
| Esophageal cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-186-5p | PTTG1 | [10] |
| Esophageal cancer | Upregulation | Oncogene | Growth and invasion | miR-203 | LASP1 | [78] |
| Esophageal cancer | Upregulation | Oncogene | Migration and invasion | miR-145 | FSCN1 | [79] |
| Gastric cancer | Upregulation | Oncogene | Growth and invasion | / | FOXM1 | [84] |
| Gastric cancer | Upregulation | Oncogene | Angiogenesis | / | Slug/VEGFA | [43] |
| Gastric cancer | Upregulation | Oncogene | Growth and invasion | miR-186 | HIF-1α | [85] |
| Gastric cancer | Upregulation | Oncogene | Growth and invasion | miR-152 | FGF2/CD151 | [86] |
| Gastric cancer | Upregulation | Oncogene | EMT | miR-30a | Snail | [87] |
| Liver cancer | Upregulation | Oncogene | Proliferation | / | NOP2 | [92] |
| Liver cancer | Upregulation | Oncogene | Growth and invasion | miR-214 | / | [44] |
| Liver cancer | Upregulation | Oncogene | Proliferation | / | P53 | [95] |
| Liver cancer | Upregulation | Oncogene | Migration and invasion | miR-3619-5p | MKL1 | [97] |
| Liver cancer | Upregulation | Oncogene | Invasion and migration | miR-186-5p | YAP1 | [98] |
| Liver cancer | Upregulation | Oncogene | Growth and invasion | miR-150 | HIG2 | [99] |
| Liver cancer | Upregulation | Oncogene | Proliferation | miR-424-5p | INCENP | [100] |
| Liver cancer | Upregulation | Oncogene | Autophagy | miR-365 | ATG3 | [101] |
| Cholangiocarcinoma | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-186 | SEMA4D | [14] |
| Cholangiocarcinoma | Upregulation | Oncogene | Migration and invasion | / | ANGPTL4 | [45] |
| Gallbladder cancer | Upregulation | Oncogene | Proliferation | miR-18b-5p | HIF1A | [13] |
| Gallbladder cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-143 | HK2 | [105] |
| Gallbladder cancer | Upregulation | Oncogene | Growth and invasion | miR-30d-5p | / | [106] |
| Pancreatic cancer | Upregulation | Oncogene | EMT | / | TGF-β/Smad | [108] |
| Pancreatic cancer | Upregulation | Oncogene | EMT | / | P21 | [109] |
| Pancreatic cancer | Upregulation | Oncogene | Proliferation and migration | miR-448 | SERBP1 | [110] |
| Pancreatic cancer | Upregulation | Oncogene | Progression and glycolysis | miR-519d-3p | HIF-1A | [111] |
| Pancreatic cancer | Upregulation | Oncogene | Autophagy | miR-20a-5p | ULK1 | [113] |
| Pancreatic cancer | Upregulation | Oncogene | Chemoresistance | / | EZH2 | [115] |
| Pancreatic cancer | Upregulation | Oncogene | Proliferation | miR-1207 | / | [116] |
| Pancreatic cancer | Upregulation | Oncogene | Chemoresistance | miR-409 | SHH/GLI/MGMT | [117] |
| Pancreatic cancer | Upregulation | Oncogene | Chemoresistance | miR-619-5p | Pygo2 | [118] |
| Pancreatic cancer | Upregulation | Oncogene | Autophagy and chemoresistance | miR-143 | HIF-1α/VMP1 | [119] |
| Colorectal cancer | Upregulation | Oncogene | Proliferation and metastasis | miR-26b | / | [11] |
| Colorectal cancer | Upregulation | Oncogene | Metastasis | miR-152-3p | VEGFA, EGFR | [125] |
| Colorectal cancer | Upregulation | Oncogene | EMT | miR-216a-5p | YBX1 | [126] |
| Colorectal cancer | Upregulation | Oncogene | EMT | miR-16-5p | VEGFA | [127] |
| Colorectal cancer | Upregulation | Oncogene | EMT | miR-186 | Twist1 | [128] |
| Colorectal cancer | Upregulation | Oncogene | Proliferation, invasion, and migration | miR-455 | RAF-1 | [129] |
| Colorectal cancer | Upregulation | Oncogene | Growth and invasion | miR-30d-5p | RUNX2 | [130] |
| Colorectal cancer | Upregulation | Oncogene | Invasion and growth | miR-214-3p | IRS1 | [131] |
| Colorectal cancer | Upregulation | Oncogene | Apoptosis | miR-146a | COX2 | [132] |
| Colorectal cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-106b-5p | FJX1 | [133] |
| Colorectal cancer | Upregulation | Oncogene | Proliferation | miR-761 | MAPK1 | [134] |
Table 4.
Main characteristics of the studies included in the review of digestive system tumors
| Study | Tumor type | Sample size (normal: tumor) | Detection method | P value | TNM (P value) | LNM (P value) | DM (P value) | OS (P value) | DFS (P value) | References |
|---|---|---|---|---|---|---|---|---|---|---|
| Li | Oral squamous cell carcinoma | 70:70 | qRT-PCR | < 0.01 | < 0.05 | / | < 0.01 | / | / | [9] |
| Zheng | Esophageal cancer | 77:77 | qRT-PCR | 0.002 | 0.009 | / | / | / | / | [77] |
| Li | Esophageal cancer | 104:104 | qRT-PCR | 0.024 | 0.001 | 0.597 | / | 0.005 | 0.011 | [78] |
| Xu | Gastric cancer | 190:190 | qRT-PCR | < 0.001 | / | / | / | / | / | [84] |
| Huang | Gastric cancer | 68:68 | qRT-PCR | < 0.05 | 0.022 | 0.005 | / | / | / | [85] |
| Li | Gastric cancer | 20:20 | qRT-PCR | 0.0004 | / | / | / | / | / | [86] |
| Wang | Gastric cancer | 42:42 | qRT-PCR | < 0.01 | < 0.05 | < 0.01 | / | / | / | [87] |
| Ding | Liver cancer | 58:58 | qRT-PCR | 0.042 | < 0.05 | / | / | / | 0.021 | [12] |
| Wang | Liver cancer | 89:89 | qRT-PCR | < 0.05 | 0.007 | / | / | 0.0104 | 0.0043 | [92] |
| Gou | Liver cancer | 92:92 | qRT-PCR | < 0.05 | < 0.05 | / | / | / | / | [44] |
| Guo | Liver cancer | 121:121 | qRT-PCR | < 0.05 | 0.010 | / | / | / | / | [95] |
| Lan | Liver cancer | 48:48 | qRT-PCR | < 0.001 | < 0.05 | / | / | 0.035 | / | [98] |
| Yang | Liver cancer | 80:80 | qRT-PCR | < 0.05 | 0.041 | / | / | / | / | [101] |
| Jin | Gallbladder cancer | 55:55 | qRT-PCR | < 0.001 | < 0.011 | < 0.032 | / | < 0.001 | / | [13] |
| Chen | Gallbladder cancer | 20:20 | qRT-PCR | < 0.05 | < 0.001 | / | 0.047 | < 0.05 | / | [105] |
| Wu | Pancreatic cancer | 30:20 | qRT-PCR | < 0.01 | < 0.05 | < 0.05 | / | / | / | [109] |
| Zhao | Pancreatic cancer | 34:34 | qRT-PCR | < 0.05 | 0.038 | / | 0.000 | / | / | [110] |
| Sun | Pancreatic cancer | 30:30 | qRT-PCR | < 0.001 | 0.05 | 0.004 | / | / | / | [111] |
| Huang | Pancreatic cancer | 68:68 | qRT-PCR | < 0.001 | < 0.05 | / | / | < 0.05 | / | [113] |
| Zeng | Colorectal cancer | 70:70 | qRT-PCR | < 0.001 | 0.029 | 0.014 | / | / | / | [126] |
| Wu | Colorectal cancer | 72:72 | qRT-PCR | < 0.05 | < 0.05 | < 0.01 | < 0.05 | / | / | [127] |
| Chai | Colorectal cancer | 20:20 | qRT-PCR | < 0.001 | / | / | / | / | / | [129] |
| Yu | Colorectal cancer | 60:60 | qRT-PCR | < 0.05 | 0.040 | 0.006 | / | / | < 0.05 | [130] |
| Liu | Colorectal cancer | 62:62 | qRT-PCR | < 0.05 | 0.0001 | 0.005 | 0.002 | / | / | [133] |
| Ping | Colorectal cancer | 112:112 | qRT-PCR | < 0.05 | 0.001 | 0.015 | 0.007 | / | / | [136] |
Table 5.
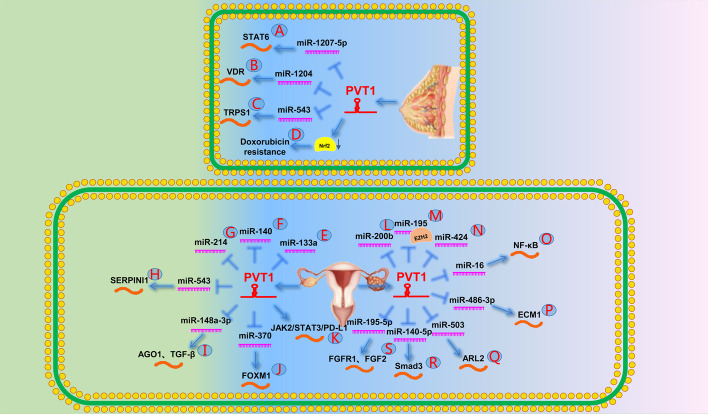
Functional characterization of PVT1 in endocrine reproductive system tumors
| Tumor type | Expression | Role | Function role | miRNAs | Related genes | References |
|---|---|---|---|---|---|---|
| Breast cancer | Upregulation | Oncogene | Proliferation | / | P21 | [140] |
| Breast cancer | Upregulation | Oncogene | EMT | / | SOX2 | [142] |
| Breast cancer | Upregulation | Oncogene | Migration | / | Claudin 4 | [145] |
| Breast cancer | Upregulation | Oncogene | Proliferation | miR-1207-5p | STAT6 | [146] |
| Breast cancer | Upregulation | Oncogene | EMT and proliferation | miR-1204 | VDR | [147] |
| Breast cancer | Upregulation | Oncogene | Proliferation | miR-543 | TRPS1 | [148] |
| Breast cancer | Upregulation | Oncogene | Chemoresistance | / | Nrf2 | [149] |
| Ovarian cancer | Upregulation | Oncogene | Growth and invasion | miR-133a | / | [151] |
| Ovarian cancer | Upregulation | Oncogene | Proliferation | miR-140 | / | [152] |
| Ovarian cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-214 | / | [153] |
| Ovarian cancer | Upregulation | Oncogene | Growth | / | P57 | [154] |
| Ovarian cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-543 | SERPINI1 | [155] |
| Ovarian cancer | Upregulation | Oncogene | Chemoresistance | / | TGF-β, p-Smad4, Caspase-3 | [19] |
| Ovarian cancer | Upregulation | Oncogene | Proliferation, migration, invasion, viability, and EMT | miR-148a-3p | AGO1 | [156] |
| Ovarian cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-370 | FOXM1 | [158] |
| Ovarian cancer | Upregulation | Oncogene | Proliferation and invasion | / | JAK2/STAT3/PD-L1 | [159] |
| Cervical cancer | Upregulation | Oncogene | Proliferation and migration | miR-200b | / | [46] |
| Cervical cancer | Upregulation | Oncogene | EMT and chemoresistance | miR-195 | / | [163] |
| Cervical cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-424 | / | [164] |
| Cervical cancer | Upregulation | Oncogene | Growth | / | TGF-β1 | [165] |
| Cervical cancer | Upregulation | Oncogene | Growth and apoptosis | miR-16 | NF-κB | [166] |
| Cervical cancer | Upregulation | Oncogene | Growth and invasion | miR-486-3p | ECM1 | [167] |
| Cervical cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-503 | ARL2 | [168] |
| Cervical cancer | Upregulation | Oncogene | Growth and invasion | miR-140-5p | Smad3 | [169] |
| Endometrial carcinoma | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-195-5p | FGFR1/FGF2 | [18] |
Table 6.
Main characteristics of the studies included in the review of endocrine reproductive system tumors
| Study | Tumor type | Sample size (normal: tumor) | Detection method | P value | TNM (P value) | LNM (P value) | DM (P value) | OS (P value) | DFS (P value) | References |
|---|---|---|---|---|---|---|---|---|---|---|
| Li | Breast cancer | 84:84 | qRT-PCR | < 0.01 | 0.061 | 0.117 | / | 0.034 | 0.045 | [140] |
| Wang | Breast cancer | 38:38 | qRT-PCR | < 0.0001 | 0.002 | 0.023 | 0.009 | 0.003 | / | [142] |
| Wang | Breast cancer | 30:30 | qRT-PCR | < 0.05 | / | / | / | / | / | [148] |
| Yang | Ovarian cancer | 42:42 | qRT-PCR | < 0.01 | / | / | / | < 0.05 | / | [151] |
| Ding | Ovarian cancer | / | qRT-PCR | < 0.05 | < 0.05 | / | / | 0.0230 | / | [152] |
| Chen | Ovarian cancer | 58:231 | qRT-PCR | < 0.05 | < 0.05 | 0.436 | / | 0.020 | 0.016 | [153] |
| Qu | Ovarian cancer | 42:42 | qRT-PCR | < 0.01 | / | / | / | 0.012 | / | [155] |
| El-Khazragy | Ovarian cancer | 30:100 | qRT-PCR | < 0.001 | 0.001 | / | 0.001 | 0.001 | 0.01 | [157] |
| Chen | Ovarian cancer | 38:91 | qRT-PCR | < 0.001 | < 0.05 | < 0.05 | / | < 0.001 | 0.002 | [159] |
| Iden | Cervical cancer | 30:127 | qRT-PCR | < 0.001 | / | / | / | 0.03 | / | [17] |
| Zhang | Cervical cancer | 90:90 | qRT-PCR | < 0.001 | / | / | / | 0.015 | / | [46] |
| Wang | Cervical cancer | 39:156 | qRT-PCR | < 0.05 | / | / | / | < 0.05 | / | [165] |
Table 7.
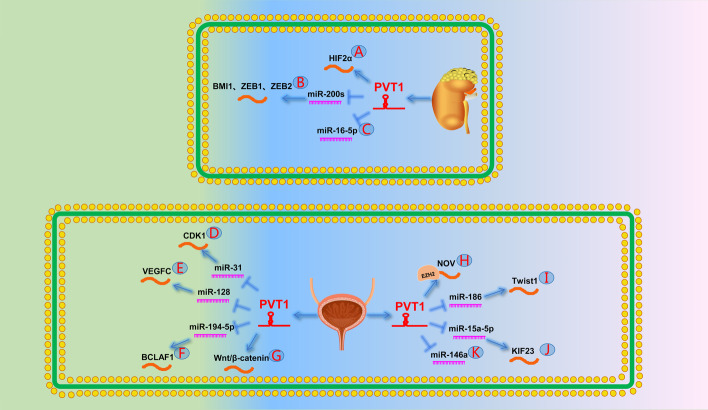
Functional characterization of PVT1 in urinary system tumors
| Tumor type | Expression | Role | Function role | miRNAs | Related genes | References |
|---|---|---|---|---|---|---|
| Renal cell carcinoma | Upregulation | Oncogene | Apoptosis | / | EGFR/AKT/MYC | [173] |
| Renal cell carcinoma | Upregulation | Oncogene | Apoptosis | / | Mcl-1 | [174] |
| Renal cell carcinoma | Upregulation | Oncogene | Proliferation, migration, invasion, and angiogenesis | / | HIF2α | [175] |
| Renal cell carcinoma | Upregulation | Oncogene | Proliferation and invasion | miR-200s | BMI1, ZEB1 and ZEB2 | [179] |
| Renal cell carcinoma | Upregulation | Oncogene | Proliferation, invasion, and EMT | miR-16-5p | / | [180] |
| Bladder cancer | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-31 | CDK1 | [184] |
| Bladder cancer | Upregulation | Oncogene | Proliferation and migration | miR-128 | VEGFC | [185] |
| Bladder cancer | Upregulation | Oncogene | Proliferation,migration, and apoptosis | miR-194-5p | BCLAF1 | [186] |
| Bladder cancer | Upregulation | Oncogene | Proliferation,invasion, apoptosis, and chemoresistance | / | Wnt/β-catenin | [187] |
| Prostate cancer | Upregulation | Oncogene | Growth | / | c-Myc | [189] |
| Prostate cancer | Upregulation | Oncogene | EMT | miR-186 | Twist1 | [190] |
| Prostate cancer | Upregulation | Oncogene | Proliferation and migration | / | P38 | [191] |
| Prostate cancer | Upregulation | Oncogene | Metastasis | / | NOP2 | [192] |
| Prostate cancer | Upregulation | Oncogene | Migration and invasion | miR-15a-5p | KIF23 | [193] |
| Prostate cancer | Upregulation | Oncogene | Growth | miR-146a | / | [194] |
Table 8.
Main characteristics of the studies included in the review of urinary system tumors
| Study | Tumor type | Sample size (normal: tumor) | Detection method | P value | TNM (P value) | LNM (P value) | DM (P value) | OS (P value) | DFS (P value) | References |
|---|---|---|---|---|---|---|---|---|---|---|
| Li | Renal cancer | 40:40 | qRT-PCR | < 0.001 | < 0.05 | / | / | < 0.01 | / | [173] |
| Zhuang | Bladder cancer | 32:32 | qRT-PCR | < 0.01 | 0.002 | / | / | / | / | [21] |
| Li | Bladder cancer | 98:98 | qRT-PCR | < 0.001 | 0.02 | < 0.001 | / | 0.004 | / | [183] |
| Tian | Bladder cancer | 35:35 | qRT-PCR | < 0.01 | / | / | / | / | / | [184] |
| Chen | Bladder cancer | 27:43 | qRT-PCR | < 0.01 | < 0.001 | 0.394 | / | / | / | [186] |
| Yang | Prostate cancer | 30:152 | qRT-PCR | < 0.0001 | < 0.01 | > 0.05 | / | 0.0127 | 0.0097 | [189] |
| Chang | Prostate cancer | 52:499 | qRT-PCR | < 0.05 | / | / | / | 0.046 | / | [190] |
| Wu | Prostate cancer | 25:25 | qRT-PCR | < 0.01 | / | / | / | / | / | [193] |
Table 9.
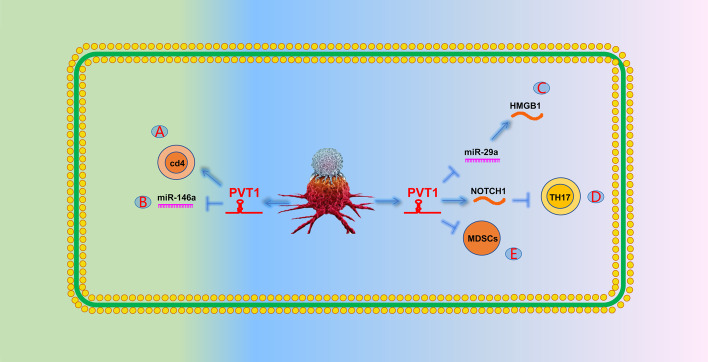
Functional characterization of PVT1 in immune system
| Disease type | Expression | Role | Function role | miRNAs | Related genes | References |
|---|---|---|---|---|---|---|
| Sjogren’s syndrome | Upregulation | Pathogenic factor | Activate CD4+ T cells | / | / | [196] |
| Heart transplant rejection | Downregulation | Protection factor | Regulation of autophagy in regulatory T cells | miR-146a | / | [197] |
| Infectious myocardial injury | Upregulation | Pathogenic factor | Promote macrophage polarization | miR-29a | HMGB1 | [198] |
| Immune thrombocytopenia | Downregulation | Protection factor | Downregulation of Th17 cell differentiation | / | NOTCH1 | [199] |
| Tumor immune suppression | Upregulation | Pathogenic factor | Enhancing the function of MDSCs | / | / | [200] |
Table 10.
Main characteristics of the studies included on the immune system
| Study | Disease type | Sample size (normal: tumor) | Detection method | P value | TNM (P value) | LNM (P value) | DM (P value) | OS (P value) | DFS (P value) | References |
|---|---|---|---|---|---|---|---|---|---|---|
| Fu | Sjogren’s syndrome | 4:4 | qRT-PCR | < 0.05 | / | / | / | / | / | [196] |
| Lu | Transplant rejection | 6:6 | qRT-PCR | < 0.01 | / | / | / | / | / | [197] |
| Yu | Immune thrombocytopenia | 12:12 | qRT-PCR | < 0.01 | / | / | / | / | / | [199] |
Table 11.
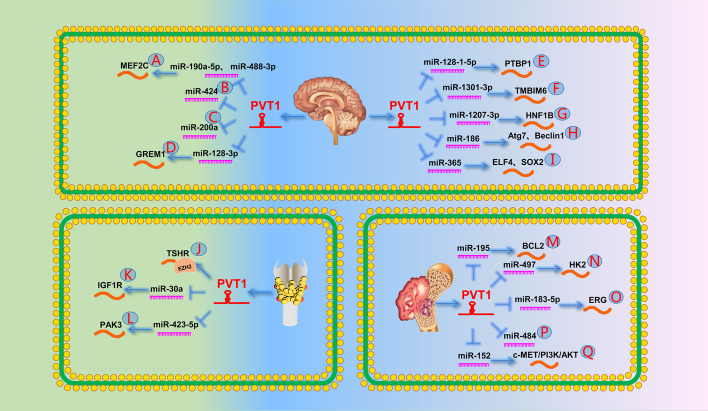
Functional characterization of PVT1 in tumors of other systems
| Tumor type | Expression | Role | Function role | miRNAs | Related genes | References |
|---|---|---|---|---|---|---|
| Glioma | Upregulation | Oncogene | Growth | miR-190a-5p/miR-488-3p | MEF2C | [202] |
| Glioma | Upregulation | Oncogene | Cell activity, migration, and invasion | miR-424 | / | [203] |
| Glioma | Upregulation | Oncogene | Growth and invasion | miR-200a | / | [204] |
| Glioma | Upregulation | Oncogene | Proliferation and migration | / | UPF1 | [205] |
| Glioma | Upregulation | Oncogene | Cell activity, growth, and invasion | miR-128-3p | GREM1 | [23] |
| Glioma | Upregulation | Oncogene | Proliferation | miR-128-1-5p | PTBP1 | [206] |
| Glioma | Upregulation | Oncogene | Proliferation, invasion, and apoptosis | miR-1301-3p | TMBIM6 | [207] |
| Glioma | Upregulation | Oncogene | EMT | miR-1207-3p | HNF1B | [208] |
| Glioma | Upregulation | Oncogene | Proliferation and migration | miR-186 | Atg7/Beclin1 | [209] |
| Glioma | Upregulation | Oncogene | Proliferation, migration, invasion, stemness, and chemoresistance | miR-365 | ELF4/SOX2 | [210] |
| Osteosarcoma | Upregulation | Oncogene | Proliferation, migration, and invasion | miR-195 | BCL2 | [24] |
| Thyroid cancer | Upregulation | Oncogene | Proliferation | / | TSHR | [26] |
| Thyroid cancer | Upregulation | Oncogene | Viability and invasion | miR-30a | IGF1R | [212] |
| Thyroid cancer | Upregulation | Oncogene | Proliferating, invasion, and apoptosis | miR-423-5p | PAK3 | [213] |
| Osteosarcoma | Upregulation | Oncogene | Growth and invasion | miR-497 | HK2 | [217] |
| Osteosarcoma | Upregulation | Oncogene | Growth and metastasis | miR-183-5p | ERG | [218] |
| Osteosarcoma | Upregulation | Oncogene | Metastasis | miR-484 | / | [219] |
| Osteosarcoma | Upregulation | Oncogene | Chemoresistance | miR-152 | c-MET/PI3K/AKT | [222] |
| Multiple myeloma | Upregulation | oncogene | Proliferation | miR-203a | / | [25] |
| Leukemia | Upregulation | Oncogene | Growth, migration, invasion, and apoptosis | miR-29 family | WAVE1 | [231] |
Table 12.
Main characteristics of the studies included in the review of other system tumors
| Study | Tumor type | Sample size (normal: tumor) | Detection method | P value | TNM (P value) | LNM (P value) | DM (P value) | OS (P value) | DFS (P value) | References |
|---|---|---|---|---|---|---|---|---|---|---|
| Gong | Glioma | 28:30 | qRT-PCR | < 0.01 | < 0.01 | / | / | 0.0240 | / | [210] |
| Zhou | Osteosarcoma | 26:26 | qRT-PCR | < 0.05 | / | / | / | < 0.05 | / | [24] |
| Song | Osteosarcoma | 46:46 | qRT-PCR | 0.0009 | < 0.001 | / | / | 0.011 | / | [217] |
| Yan | Osteosarcoma | 48:48 | qRT-PCR | < 0.0001 | 0.008 | / | 0.001 | 0.0001 | / | [219] |
| Xun | Osteosarcoma | 78:78 | qRT-PCR | < 0.001 | 0.000 | 0.017 | 0.017 | / | / | [220] |
| Zhou | Thyroid cancer | 84:84 | qRT-PCR | < 0.0001 | / | / | / | / | / | [26] |
| Feng | Thyroid cancer | 72:72 | qRT-PCR | < 0.05 | < 0.01 | < 0.01 | / | / | / | [212] |
| Lin | Thyroid cancer | 47:47 | qRT-PCR | < 0.001 | / | / | / | / | / | [213] |
| Yang | Multiple myeloma | 33:14 | qRT-PCR | < 0.05 | / | / | / | / | / | [25] |
| Yang | Leukemia | 62:286 | qRT-PCR | < 0.001 | / | / | / | < 0.001 | / | [27] |
| Izadifard | AML | 40:22 | qRT-PCR | 0.017 | / | / | / | / | / | [227] |
| El-Khazragy | AML | 70:20 | qRT-PCR | < 0.01 | / | / | / | / | / | [228] |
| Cheng | AML | 30:30 | qRT-PCR | < 0.01 | / | / | / | / | / | [231] |
Role of PVT1 in the respiratory system
PVT1 in nasopharyngeal carcinoma
NPC originates from nasopharyngeal epithelial cells and is particularly common in Southeast Asia, North Africa, and southern China. New cases accounted for only 0.7% of the total cancer incidence, and the mortality rate has decreased significantly with advancements in medical treatments. However, the treatment of NPC is difficult owing to radiotherapy and chemotherapy resistance, postoperative recurrence, diffusion, and metastasis, which require further exploration to better diagnose and treat patients with NPC [53].
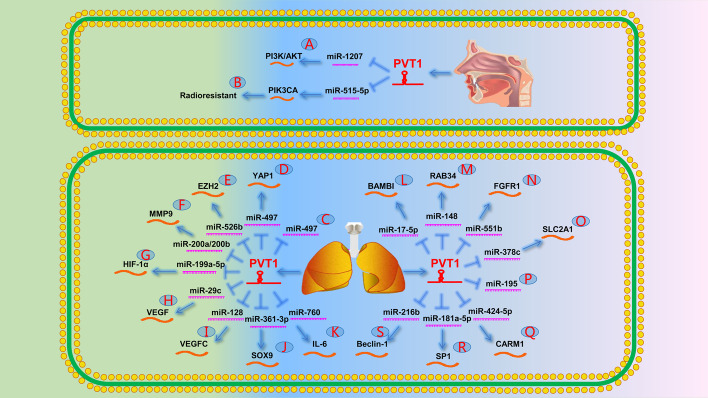
In a study by Cui et al. [54] on the formation, metastasis, and recurrence of NPC, the authors reported that PVT1 promoted tumor stem cell growth by inhibiting miR-1207 and activating the phosphatidylinositol 3-kinase/protein kinase B (PI3K/AKT) signaling pathway (Fig. 1A). In addition, He et al. [7] demonstrated that PVT1 acted as a radioresistant factor, thereby promoting DNA repair and inhibiting apoptosis in NPC cells by activating ATM/Chk2/p53 phosphorylation. Han et al. [55] revealed that PVT1 controls NPC cell radioresistance and proliferation through the miR-515-5p/PIK3CA axis (Fig. 1B). Wang et al. [41] discovered another mechanism by which PVT1 reduces radiotherapy sensitivity in NPC cells. They validated that PVT1 acts as a scaffold to promote H3K9 acetylation by the chromatin modifier KAT2A, thereby activating the downstream expression of nuclear factor 90 through H3K9ac binding to TIF1β. Furthermore, the stability of hypoxia-inducible factor (HIF)-1α mRNA was further strengthened to achieve tumor resistance to radiotherapy.
Fig. 1.
The role of PVT1 in the respiratory system. A PVT1 promotes the expression of PI3K/AKT by targeting miR-1207. B PVT1 promotes the expression of PIK3CA by targeting miR-515-5p, which in turn causes radioresistance. C PVT1 directly targets miR-497. D PVT1 promotes the expression of YAP1 by targeting miR-497. E PVT1 promotes the expression of EZH2 by targeting miR-526b. F PVT1 promotes the expression of MMP9 by targeting miR-200a/200b. G PVT1 promotes the expression of HIF-1α by targeting miR-199a-5p. H PVT1 promotes the expression of VEGF by targeting miR-29c. I PVT1 promotes the expression of VEGFC by targeting miR-128. J PVT1 promotes the expression of SOX9 by targeting miR-361-3p. K PVT1 promotes the expression of IL-6 by targeting miR-760. L PVT1 promotes the expression of BAMBI by targeting miR-17-5p. M PVT1 promotes the expression of RAB34 by targeting miR-148. N PVT1 promotes the expression of FGFR1 by targeting miR-551b. O PVT1 promotes the expression of SLC2A1 by targeting miR-378c. P PVT1 directly targets miR-195. Q PVT1 promotes the expression of CARM1 by targeting miR-424-5p. R PVT1 promotes the expression of SP1 by targeting miR-181a-5p. S PVT1 promotes the expression of Beclin-1 by targeting miR-216b
In conclusion, PVT1 plays an important role in the tumorigenesis and radioresistance of NPC.
PVT1 in non-small cell lung cancer
As of 2022, lung cancer accounted for 12% and 13% of all cancers in men and women, respectively [1]. Advanced NSCLC remains the leading cause of cancer-related deaths. However, little progress has been made in understanding its molecular mechanisms. Therefore, a study elucidating the underlying mechanisms of NSCLC is urgently needed.
A previous study showed that PVT1 promotes NSCLC cell proliferation by inhibiting P15 and P21 expression [6]. Another study reported that PVT1 regulates miR-497 to promote tumor formation in patients with NPC (Fig. 1C) [56]. Wan et al. [42] demonstrated that PVT1 repressed the expression of LAST2 by recruiting EZH2 to the promoter region of LAST2. LAST2 is an upstream phosphokinase of the Hippo signaling pathway that can phosphorylate YAP1 to reduce its expression and activate the Hippo signaling pathway. Subsequently, Zeng et al. [57] further confirmed that PVT1 promoted YAP1 expression by downregulating miR-497 by mediating EZH2, leading to the inhibition of the Hippo signaling pathway. Ultimately, the neurogenic locus notch homolog protein 1 (NOTCH1) signaling pathway was activated to promote NSCLC cell proliferation, migration, and epithelial–mesenchymal transition (EMT) (Fig. 1D). Another study emphasized that PVT1 upregulated EZH2 by acting as a sponge for miR-526b (Fig. 1E) [58].
PVT1 can also promote NSCLC progression as a ceRNA. Chen et al. [59] showed that PVT1 overexpression promoted NSCLC invasion by competitively binding miR-200a/200b to upregulate MMP9 expression (Fig. 1F). Additionally, Wang et al. [60] indicated that PVT1 was overexpressed in patients with hypoxic NSCLC and upregulated HIF-1α expression by acting as a sponge for miR-199a-5p. These findings suggest that PVT1 may serve as a potential therapeutic target for the treatment of hypoxic NSCLC (Fig. 1G). Several studies have indicated an important role of the lncRNA–miRNA–mRNA axis in patients with NSCLC. Specifically, PVT1 reportedly contributed to the proliferation, migration, invasion, and apoptosis of NSCLC cells by upregulating VEGF, VEGFC, SOX9, interleukin-6, BAMBI, RAB34, fibroblast growth factor receptor 1 (FGFR1), and SLC2A1 via miR-29c, miR-128, miR-361-3p, miR-760, miR-17-5p, miR-148, miR-551b, and miR-378c regulation (Fig. 1H−O) [61–68], respectively.
PVT1 also plays an important role in radiotherapy and chemotherapy in patients with advanced NSCLC. Wu et al. [69] found that miR-195 release after PVT1 knockdown increased NSCLC cell apoptosis during radiotherapy (Fig. 1P). Subsequently, Wang et al. [70] revealed that PVT1 and CARM1 downregulation led to miR-424-5p overexpression, which may improve radiosensitivity in patients with NSCLC (Fig. 1Q). Interestingly, the Chinese herbal prescription Xiaoji decoction enhanced the efficacy of cisplatin in patients with NSCLC by decreasing the expression of the PVT1/miR-181a-5p/SP1 axis (Fig. 1R) [71]. Similarly, Chen et al. [72] reported that PVT1 enhances cisplatin resistance in patients with NSCLC by regulating the miR-216b/Beclin-1 axis (Fig. 1S).
These results suggest that lncRNA PVT1 plays a vital role in the invasion, proliferation, migration, drug resistance, and radiosensitivity of NSCLC cells.
Role of PVT1 in the digestive system
PVT1 in oral squamous cell carcinoma
OSCC is a malignant tumor derived from oral epithelial cells with a high incidence in Southeast Asia and southern China that may be related to dietary habits, such as betel nut consumption. In 2021, there were 377,713 new cases, accounting for 2% of all cancers, and 177,757 new deaths accounting for 1.8% of all cancers [73]. The number of patients with OSCC is expected to increase by 30% within the next 10 years, with a 5-year survival rate of only 50% [53]. Therefore, further studies on the pathogenesis of OSCC are required to improve its diagnosis, treatment, and prognosis.
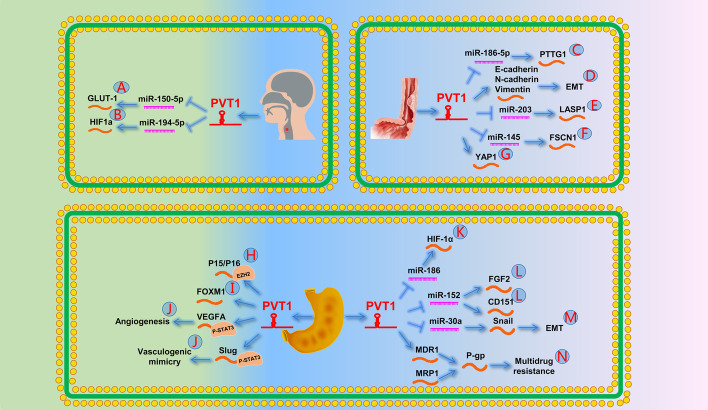
Li et al. [9] verified that PVT1 downregulation inhibits glucose transporter protein type 1 through miR-150-5p, regulates glucose metabolism in tumor cells, promotes invasion and migration of OSCC cells, and inhibits cell apoptosis (Fig. 2A). Wang et al. [74] found that PVT1 accelerated the development of EMT and led to tumor progression in patients with OSCC.
Fig. 2.
The role of PVT1 in the digestive system [1]. A PVT1 promotes the expression of GLUT-1 by targeting miR-150-5p. B PVT1 promotes HIF1a by targeting miR-194-5p and leads to cisplatin resistance in OSCC. C PVT1 promotes the expression of PTTG1 by targeting miR-186-5p. D PVT1 can promote the expression of EMT markers (E-cadherin, N-cadherin, and vimentin) in EC cells, indicating that it can promote the occurrence of EMT. E PVT1 promotes the expression of LASP1 by targeting miR-203. F PVT1 promotes the expression of FSCN1 by targeting miR-145. G PVT1 prevents the inactivation of Hippo’s downstream effector YAP1 by reducing its phosphorylation. H PVT1 downregulates P15/P16 expression by recruiting EZH2. I A positive feedback loop between PVT1 and FOXM1 promotes GC growth and invasion. J PVT1 can promote the expression of VEGFA and Slug by binding to STAT3 and ultimately promote angiogenesis and VM. K PVT1 promotes the expression of HIF-1α by targeting miR-186. L PVT1 promotes the expression of FGF2 and CD151 by targeting miR-152. M PVT1 promotes the expression of Snail by targeting miR-30a. N PVT1 promotes GC multidrug resistance by upregulating the ATP-dependent efflux pump P-gp by promoting the expression of MDR1 and MRP1
Cisplatin is a chemotherapeutic agent commonly used for the treatment of OSCC. Most patients with OSCC with poor prognosis have multiple drug resistance; however, the underlying mechanism remains unclear. Wang et al. [75] reported that PVT1 regulates cisplatin resistance in patients with OSCC through the miR-194-5p/HIF-1α signaling pathway (Fig. 2B).
These studies confirm that PVT1 is responsible for the occurrence, invasion, and drug resistance of OSCC cells.
PVT1 in esophageal cancer
EC causes 500,000 deaths annually, accounting for 5.5% of all cancer-related deaths worldwide. Esophageal squamous cell carcinoma (ESCC) is the most common type [76]. The latest data show that the incidence of EC is only 3.1% among all cancers, although its mortality rate is 5.5% [53]. ESCC is mainly associated with a poor prognosis because early detection is difficult. Most patients present with extensive metastases at the time of diagnosis [76]. Therefore, its pathogenesis should be further explored to improve the diagnosis and treatment of EC.
Yang et al. [10] reported that PVT1 might function as a ceRNA by targeting miR-186-5p to upregulate the oncogene PTTG1 (Fig. 2C). Zheng et al. [77] revealed that lncRNA PVT1 induces EMT by regulating the expression of EMT markers (E-cadherin, N-cadherin, and vimentin) (Fig. 2D). Li et al. [78] found that PVT1 upregulates LASP1 expression by targeting miR-203, thereby promoting ESCC progression (Fig. 2E). Shen et al. [79] demonstrated upregulated miR-145 and downregulated FSCN1 expression after PVT1 knockout, which inhibited ESCC cell invasion, migration, and survival (Fig. 2F). Xu et al. [80] discovered that silencing PVT1 might lead to decreased YAP1 expression through phosphorylated LATS1, thereby inhibiting tumor growth (Fig. 2G).
In summary, these studies indicate that PVT1 is involved in ESCC progression and acts as a diagnostic biomarker and therapeutic target.
PVT1 in gastric cancer
GC is the fourth most common cancer and the second most lethal malignant tumor worldwide. With the development of gastrointestinal endoscopy technology and GC drugs, GC death rates have decreased in recent years. However, advanced GC remains difficult to cure [1]. Identifying new biomarkers and therapeutic methods is an effective method for determining the pathogenesis of GC.
Recent studies have shown that PVT1 promotes GC migration, invasion, and lymph node metastasis (LNM) [81–83]. Kong et al. [8] reported that PVT1 negatively regulates P15/P16 through the epigenetic recruitment of EZH2, thereby promoting GC proliferation (Fig. 2H). Subsequently, Xu et al. [84] revealed that PVT1 promotes GC growth and invasion through a positive feedback loop with FOXM1 (Fig. 2I). In addition, Zhao et al. [43] found that PVT1 binds to STAT3, resulting in the recruitment of STAT3 to VEGFA and Slug promoters, whereas increased VEGFA led to angiogenesis and increased Slug-mediated GC vasculogenic mimicry network formation (Fig. 2J).
PVT1 can also regulate tumor progression through the lncRNA–miRNA–mRNA axis in patients with GC. Huang et al. [85] reported that PVT1 plays a key role in GC pathogenesis and may be a potential therapeutic target via miR-186/HIF-1α signaling (Fig. 2K). Similarly, Li et al. [86] indicated that PVT1 promotes GC growth and invasion by competitively binding to miR-152 to regulate CD151 and FGF2 (Fig. 2L). Furthermore, Wang et al. [87] demonstrated that PVT1 controls the EMT of GC via the miR-30a/Snail axis (Fig. 2M).
PVT1 is also involved in multidrug resistance in patients with GC. Zhang et al. [88] reported that PVT1 promotes the expression of adenosine triphosphate-dependent efflux pump P-glycoprotein protein by upregulating multidrug resistance 1 (MDR1) and multidrug resistance-related protein 1 (MRP1) expression, thereby leading to the occurrence of multidrug resistance (Fig. 2N).
Thus, PVT1 can be used as a biomarker for the diagnosis and prognosis of GC. High expression often represents deep infiltration; advanced tumor, node, metastasis (TNM) stages; and poor prognosis.
PVT1 in hepatocellular carcinoma
Although the incidence of HCC has gradually stabilized after rapid growth in recent decades, the HCC survival rate is only 20% [1]. Approximately one-quarter of patients with HCC have genetic mutations [89]. Therefore, the pathogenesis of HCC should be studied to identify novel targets and treatments.
Ding et al. [12] found that increased PVT1 often indicated poor prognosis and a high recurrence rate, which was closely related to alpha-fetoprotein levels. Yu et al. [90, 91] suggested that PVT1 can be combined with several other lncRNAs as a complementary diagnostic tool for HCC. Wang et al. [92] revealed that hepatitis B virus (HBV) infection promotes proliferation, development, and stem cell characteristics in HCC cells by enhancing the transforming growth factor beta (TGF-β)1/lncRNA-hPVT1/NOP2 signaling pathway, thereby accelerating the cell cycle. Similarly, Yan et al. [93] found that PVT1 upregulation was more common in early-onset than late-onset HCC after HBV infection. Subsequently, Jiang et al. [94] confirmed that PVT1 expression in HCC cells caused by HBV infection was significantly higher than that in HCC cells without HBV infection. Gou et al. [44] found that PVT1 interacts with EZH2 to downregulate miR-214 and promote the proliferation and invasion of HCC cells. Another research group revealed that PVT1 increases the stability of the MDM2 protein by enhancing EZH2 and inhibiting P53 protein expression to promote HCC cell proliferation [95]. Furthermore, Zhang et al. [96] speculated that PVT1 may play an important role in the occurrence and development of HCC by affecting the DLC1 and Hippo signaling pathways.
Increasing evidence shows that PVT1 functions as a ceRNA through lncRNA–miRNA–mRNA signaling. A previous study demonstrated that PVT1 upregulates the MKL1 expression by binding to miR-3619-5p in a positive feedback pathway. MKL1 in turn promotes PVT1 expression by binding to the CArG box, which is located in the PVT1 promoter region (Fig. 3A) [97]. Subsequently, several studies have shown that PVT1 promotes the invasion, migration, and proliferation of HCC cells by upregulating YAP1, HIG2, INCENP, and ATG3 by modulating miR-186-5p, miR-150, miR-424-5p, and miR-365 (Fig. 3B−E) [98–101], respectively.
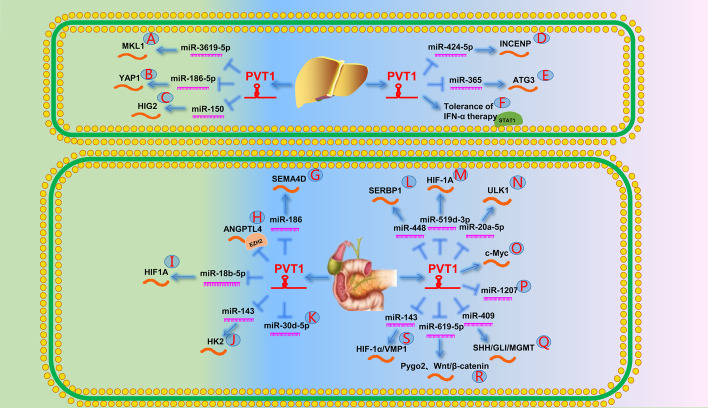
Fig. 3.
The role of PVT1 in the digestive system [2]. A PVT1 promotes the expression of MKL1 by targeting miR-3619-5p. B PVT1 promotes the expression of YAP1 by targeting miR-186-5p. C PVT1 promotes the expression of HIG2 by targeting miR-150. D PVT1 promotes the expression of INCENP by targeting miR-424-5p. E PVT1 promotes the expression of ATG3 by targeting miR-365. F PVT1 can decrease the phosphorylation of STAT1 and finally leads to the tolerance of IFN-α therapy. G PVT1 promotes the expression of SEMA4D by targeting miR-186. H PVT1 downregulates its expression by recruiting EZH2 to the ANGPTL4 promoter region. I PVT1 downregulates miR-18b-5p expression by binding to EZH2 and promotes HIF1A expression. J PVT1 promotes the expression of HK2 by targeting miR-143. K PVT1 directly binds to miR-30d-5p. (L) PVT1 promotes the expression of SERBP1 by targeting miR-448. M PVT1 promotes the expression of HIF-1A by targeting miR-519d-3p. N PVT1 promotes the expression of ULK1 by targeting miR-20a-5p. O PVT1 enhances gemcitabine resistance of PDAC by increasing c-Myc expression. P PVT1 enhances gemcitabine resistance of PC by inhibiting miR-1207 expression. Q PVT1 promotes the SHH/GLI/MGMT signal pathway by targeting miR-409. R PVT1 upregulates Pygo2 by targeting miR-619-5p and ultimately activates Wnt/β-catenin signaling pathway, resulting in PC resistance to gemcitabine chemotherapy. S PVT1 promotes the HIF-1α/VMP1 signaling pathway by targeting miR-143, resulting in PC resistance to gemcitabine chemotherapy
Interferon alpha (IFN-α) has a significant effect on prolonging the postoperative disease-free survival and prognosis of patients with HCC, although patients’ tolerance to IFN-α remains an unsolved problem. A recent study suggests that IFN-α decreases PVT1 methylation by regulating H3K4me3 in the PVT1 promoter region, thereby increasing PVT1 expression. PVT1 subsequently reduces STAT1 phosphorylation, thereby blocking the IFN-α signaling pathway (Fig. 3F) [102].
The above evidence suggests that PVT1 plays an important role in the invasion, migration, proliferation, and drug resistance of HCC.
PVT1 in gallbladder cancer and cholangiocarcinoma
GBC is a rare disease that is caused by long-term gallstones and cholecystitis. The prognosis of GBC is usually poor because of early metastasis [103]. CCA is mainly derived from bile duct epithelial cells and peribiliary glands or hepatocytes. CCA is a fatal epithelial malignancy, and most patients have no identifiable risk factors [104]. Therefore, early detection of the related biomarkers can facilitate the early diagnosis of GBC and CCA, which is crucial for improving patient prognosis.
Yu et al. [14] showed that SRY-box transcription factor 2 (SOX2) activates the PVT1/miR-186/SEMA4D axis by promoting PVT1 expression, thereby enhancing CCA cell viability (Fig. 3G). Another study showed that PVT1 inactivated the ANGPTL4 promoter region by binding to EZH2, thereby regulating CCA vascular endothelial cell apoptosis (Fig. 3H) [45]. Similarly, Jin et al. [13] demonstrated that PVT1 recruits DNA methyltransferase through EZH2 and inhibits miR-18b-5p, thereby upregulating HIF-1α and promoting GBC cell proliferation (Fig. 3I). Moreover, Chen et al. [105] found that PVT1 controls aerobic glucose metabolism in GBC cells through the PVT1/miR-143/HK2 axis, thereby promoting tumor proliferation and metastasis (Fig. 3J). Liu et al. [106] reported that PVT1 promotes GBC progression by acting as a ceRNA of miR-30d-5p (Fig. 3K).
In conclusion, PVT1 shows strong carcinogenicity and can be used as a potential biomarker and therapeutic target in CBC and CCA.
PVT1 in pancreatic cancer
PC is the leading cause of cancer-related deaths worldwide, and is one of the top five causes of cancer-related deaths in the USA. According to the latest cancer statistics, PC has a 5-year survival rate of only 11%. Therefore, further exploration of the molecular markers is crucial for the early diagnosis and treatment of PC [1, 107].
Xie et al. [15] found that PVT1 and HOTAIR may serve as biomarkers for predicting early-stage PC. Two years later, Zhang et al. [108] demonstrated that PVT1 regulates PC cell survival, metastasis, and EMT by affecting the TGF-β/Smad signaling pathway. Similarly, Wu et al. [109] reported that silencing PVT1 increased tumor suppressor P21 and downregulated the EMT transcription factors Snail and ZEB1, suggesting that PVT1 affects EMT through P21 in PC cells. Moreover, Zhao et al. [110] showed that PVT1 promotes PC cell proliferation and migration by functioning as a ceRNA to regulate SERBP1 by sequestering miR-448 (Fig. 3L). Another study reported that PVT1 acts as a sponge for miR-519d-3p to modulate HIF-1α, which in turn activates angiogenesis, glucose metabolism, cell proliferation, migration, and metastasis (Fig. 3M) [111]. Subsequently, Zhu et al. [112] reported a positive feedback regulatory loop between PVT1 and HIF-1α, indicating that HIF-1α promotes PVT1 expression in hypoxia, whereas PVT1 promotes HIF-1α expression in normoxic environments. In addition, Huang et al. [113] revealed that PVT1 promotes the development of PC by regulating miR-20a-5p/ULK1 to increase cellular protective autophagy (Fig. 3N).
Chemotherapeutic drugs, such as gemcitabine (GEM), are important in the treatment of patients with advanced PC. Therefore, predicting the efficacy of chemotherapy and exploring the causes of chemotherapy resistance are important for improving patient prognosis and making correct treatment decisions. Wang et al. [114] pointed out that the combination of PVT1, HOTTIP, and MALAT1 may be a new noninvasive biomarker for predicting GEM efficacy in patients with PC. Another study showed that PVT1 and EZH2 combine to form a complex that promotes c-Myc expression and enhances PC resistance to GEM (Fig. 3O) [40]. Another study by Sun et al. [115] showed that HAT1 improves the resistance of PC to chemotherapy by promoting PVT1 expression and inhibiting EZH2 degradation. Moreover, You et al. [116] confirmed that the chemotherapy resistance of PC can be inhibited by silencing PVT1 or overexpressing miR-1207 (Fig. 3P). Furthermore, Shi et al. [117] showed that PVT1 can directly target miR-409 to promote the SHH/GLI/MGMT signaling pathway and enhance chemoresistance to GEM (Fig. 3Q). Similarly, Zhou et al. [118] found that PVT1 activates the Wnt/β-catenin signaling pathway via the miR-619-5p/Pygo2 axis to influence the chemotherapeutic sensitivity of GEM (Fig. 3R). A year later, Liu et al. [119] revealed that PVT1 knockdown inhibited autophagy by regulating the miR-143/HIF-1α/VMP1 axis, thereby improving PC cell sensitivity to chemotherapy (Fig. 3S).
Overall, PVT1 is strongly correlated with drug resistance in patients with PC and can be used as a new biomarker for PC.
PVT1 in colorectal cancer
CRC is the third most common cancer worldwide, with 151,030 new cases estimated to occur by 2022 [1]. CRC occurs at a younger age and is expected to become one of the leading causes of cancer-related deaths among people aged 20–49 years by 2030 [120, 121]. Developing more sensitive screening methods, enriching treatment options, and further exploring the role of PVT1 in CRC is urgently needed.
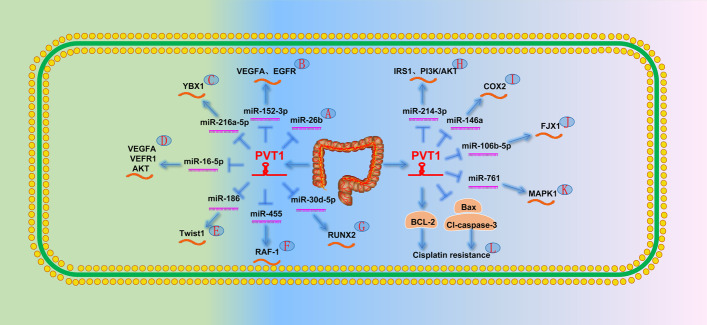
PVT1 upregulation promotes the proliferation, invasion, and metastasis of CRC and suggests poor prognosis [48–51]. PVT1 is a highly effective biomarker for early CRC screening and has greater diagnostic and prognostic value than that of carcinoembryonic antigen [122, 123]. Zhang et al. [11] confirmed that PVT1 promotes CRC cell proliferation and metastasis by inhibiting miR-26b as an endogenous sponge (Fig. 4A). In addition, Guo et al. [124] reported that PVT1 in extracellular vesicles promotes CRC cell progression. Four years later, Lai et al. [125] demonstrated that PVT1 in exosomes upregulates VEGFA and EGFR by regulating miR-152-3p expression, thereby promoting the distant metastasis of CRC cells (Fig. 4B). In addition, Ansari and Shigeyasu et al. [37, 38] found that PVT1 extensively affects CRC signaling pathways, including the TGFβ/Smad and Wnt/β-catenin signaling pathways, and promotes CRC cell metastasis by regulating MYC, which may lead to a poor prognosis by promoting the ability of CRC stem cells.
Fig. 4.
The role of PVT1 in the digestive system [3]. A PVT1 directly targets miR-26b. B PVT1 promotes the expression of VEGFA and EGFR by targeting miR-152-3p. C PVT1 promotes YBX1 expression by targeting miR-216a-5p and ultimately leads to EMT in CRC cells. D By targeting miR-16-5p, PVT1 leads to increased VEGFA, VEGFR1, and AKT expression and ultimately leads to EMT in CRC cells. E PVT1 ultimately promotes EMT in CRC cells by targeting miR-186 and leading to increased Twist1 expression. F PVT1 promotes RAF-1 by targeting miR-455. G PVT1 promotes the expression of RUNX2 by targeting miR-30d-5p. H PVT1 upregulates IRS1 by targeting miR-214-3p and ultimately activates PI3K/AKT signaling pathway. I PVT1 promotes the expression of COX2 by targeting miR-146a. J PVT1 promotes the expression of FJX1 by targeting miR-106b-5p. K PVT1 promotes the expression of MAPK1 by targeting miR-761. L PVT1 promotes the occurrence of EMT in CRC cells by downregulating the pro-apoptotic proteins Bax and Cl-caspase-3 and upregulating the expression of the anti-apoptotic protein BCL-2
Transformation of the cell phenotype from epithelial cells to mesenchymal cells is an important factor leading to tumor invasion and metastasis. YBX1 is a multifunctional tumor protein that promotes EMT by increasing the expression of angiogenesis factors. Zeng et al. [126] found that PVT1 promotes YBX1 expression by downregulating miR-216a-5p, thereby promoting EMT, invasion, and CRC cell metastasis (Fig. 4C). Recently, Wu et al. [127] found that PVT1 promotes angiogenesis and EMT through the miR-16-5p/VEGFA/VEGFR1/AKT signaling pathway (Fig. 4D). Radwan et al. [128] discovered a new signaling pathway that induces EMT. PVT1 increased the expression of the related transcription factor TWIST1 during EMT by downregulating miR-186 (Fig. 4E).
Chai et al. [129] reported that PVT1, as a key component of the RUNX2/PVT1/miR-455/RAF-1 axis, affects the growth and invasion of CRC (Fig. 4F). Subsequently, Yu et al. [130] confirmed that PVT1 promotes CRC cell proliferation through the miR-30d-5p/RUNX2 axis (Fig. 4G). Moreover, Shang et al. [131] reported that PVT1 upregulates IRS1 by targeting miR-214-3p and ultimately activates the PI3K/AKT signaling pathway to promote CRC proliferation and invasion (Fig. 4H). Several studies have reported on the lncRNA–miRNA–mRNA signaling in CRC and demonstrated that PVT1 promotes CRC cell proliferation, migration, and invasion by upregulating COX2, FJX1, and MAPK1 via the modulation of miR-146a, miR-106b-5p, and miR-761 (Fig. 4I−K) [132–134], respectively.
Chemotherapy is crucial in the treatment of CRC; however, the emergence of drug resistance often indicates a low survival rate and poor prognosis. Fan et al. [135] showed that PVT1 enhances cisplatin resistance in patients with CRC by inhibiting the endogenous apoptosis signaling pathway. Another research group discovered that PVT1 downregulated pro-apoptotic proteins [B-cell lymphoma 2 (Bcl-2) associated X protein and cleaved caspase-3] and upregulated the expression of anti-apoptotic protein BCL-2 (Fig. 4L) [136].
These findings indicate that PVT1 can be used as a new biomarker for the diagnosis and treatment of CRC, providing a novel target for future treatments.
Role of PVT1 in the endocrine reproductive system
PVT1 in breast cancer
According to the 2022 Cancer Statistics, BC is the most common cancer among women, accounting for approximately 30% of all cancers. BC accounts for 15% of all cancer-related deaths and ranks second among the top ten causes of cancer-related deaths. Advances in BC diagnosis and treatment have greatly improved 5-year survival rates. However, recurrence, metastasis, and chemotherapy resistance remain urgent and unsolved problems [1]. Therefore, in-depth exploration of the molecular mechanisms can improve BC diagnosis in the future.
Guan et al. [16] showed that inhibition of PVT1 may inhibit BC proliferation. Zhang et al. [137] suggested that the GG genotype of the single nucleotide polymorphism rs13281615 may influence the development of BC through PVT1 and is associated with estrogen receptor positivity, higher tumor grades, and higher proliferative indices. Another study showed that activated PVT1-KLF5-CTNNB1 (β-catenin) promotes the proliferation of triple-negative BC [138]. RSPO1 is a key regulator of the β-catenin signaling pathway required for female development. A study showed that MYC-PVT1 overexpression causes RSPO1 upregulation, which ultimately leads to the development of cancer [139]. Another study showed that PVT1 promoted BC cell proliferation through the negative regulation of P21 [140]. A year later, Wang et al. [141] also demonstrated that PVT1 influenced EMT through P21, resulting in the proliferation and migration of triple-negative BC. The transcription factor SOX2 plays an important role in various cancers by controlling stem cell activity. Wang et al. [142] showed that PVT1 promotes EMT through SOX2 upregulation, thereby regulating BC invasion and growth. Zhu et al. [143] conducted a bioinformatics analysis and reported that a prediction model composed of four lncRNAs, PVT1, MAPT-AS1, LINC00667, and LINC00938, had good sensitivity and specificity for predicting BC prognosis. Subsequently, El-Fattah et al. [144] revealed the efficacy of PVT1, HOTAIR, NEAT1, PAI-1, and OPN as diagnostic biomarkers in BC. A year later, Levine et al. [145] suggested that PVT1 exon 9 may regulate BC cell migration by reducing claudin 4 expression.
Moreover, Yan et al. [146] showed that PVT1 promotes BC cell proliferation and colony formation by downregulating STAT6 cell cycle regulators through miR-1207-5p (Fig. 5A). Similarly, Liu et al. [147] found that PVT1 promoted BC cell EMT and proliferation by increasing VDR by antagonizing miR-1204 (Fig. 5B). In addition, Wang et al. [148] reported that PVT1 affects cell proliferation by promoting TRPS1 expression by sponging miR-543 in BC cells (Fig. 5C).
Fig. 5.
The role of PVT1 in the endocrine reproductive system. A PVT1 downregulates STAT6 by generating miR-1207-5p. B PVT1 targets VDR by generating miR-1204. C PVT1 promotes the expression of TRPS1 by targeting miR-543. D PVT1 caused Nrf2 degradation, eventually leading to doxorubicin resistance in TNBC. E PVT1 directly targets miR-133a. F PVT1 directly targets miR-140. G PVT1 directly targets miR-214. H PVT1 promotes SERPINI1 expression by targeting miR-543. I PVT1 upregulates AGO1 by targeting miR-148a-3p to promote the expression of TGF-β and ultimately leads to cisplatin resistance in OC. J PVT1 promotes FOXM1 expression by targeting miR-370. K PVT1 promotes OC cisplatin resistance by affecting the JAK2/STAT3/PD-L1 signaling pathway. L PVT1 directly targets miR-200b. M PVT1 directly targets miR-195. N PVT1 directly targets miR-424. O PVT1 promotes NF-κB signaling by targeting miR-16. P PVT1 promotes ECM1 expression by targeting miR-486-3p. Q PVT1 promotes ARL2 expression by targeting miR-503. R PVT1 promotes Smad3 expression by targeting miR-140-5p. S PVT1 promotes the expression of FGF2 and FGFR1 by targeting miR-195-5p
In addition, PVT1 promoted chemotherapy resistance to adriamycin in triple-negative BC cells by competitively binding Keap1 to degrade the nuclear factor erythroid 2-related factor 2 protein (Fig. 5D) [149].
Taken together, these studies suggest that PVT1 plays an important role in the proliferation, invasion, and metastasis of BC, and is related to the drug resistance mechanism of triple-negative BC.
PVT1 in ovarian cancer
OC originates from the germinal epithelium of the ovary and can be divided into serous, endometrioid, clear cell, and mucous types. OC is the seventh most common cancer among women worldwide, with a survival rate of 46%. Therefore, the development of new detection methods and treatments is urgently needed [150].
Several studies have demonstrated that PVT1 regulates OC cell proliferation and invasion by acting as a ceRNA of miR-133a, miR-140, and miR-214 (Fig. 5E−G) [151–153]. Li et al. [154] demonstrated that PVT1 can inactivate EZH2 by recruiting it to the promoter region of tumor suppressor gene P57. Ketamine can reduce this recruitment, which in turn increases P57 expression. Another study showed that PVT1 knockdown may induce apoptosis through the miR-543/SERPINI1 axis in OC cells (Fig. 5H) [155].
PVT1 can regulate the resistance of OC to cisplatin by regulating the expression of apoptosis-related proteins such as TGF-β1, p-Smad4, and caspase-3 [19]. Wu et al. [156] demonstrated that PVT1 upregulates AGO1 by sponging miR-148a-3p, thereby downregulating TGF-β and promoting OC progression (Fig. 5I). Subsequent studies have also demonstrated that PVT1, TUG1, and MEG3 can lead to cisplatin resistance by inhibiting OC cell apoptosis [157]. Yi et al. [158] reported that PVT1 could directly bind to FOXM1 to stabilize its expression or promote FOXM1 expression by binding to miR-370 through a sponging effect, ultimately leading to OC progression and chemotherapy resistance (Fig. 5J). Another study reported that PVT1 silencing inhibits OC cell growth, metastasis, and cisplatin resistance by downregulating the JAK2/STAT3/programmed death-ligand (PD-L1) pathway. The authors suggested that combination therapy targeting PVT1 and the PD-L1 immune checkpoint blockade may have a synergistic effect on the clinical treatment of patients with OC (Fig. 5K) [159].
Martini et al. [160] analyzed the expression of multiple lncRNAs in 202 cases of early-onset OC and found that lncRNA PVT1 predicted a poor prognosis in patients with early-onset OC. Conversely, Yamamoto et al. [52] argued that high PVT1 and MYC expression predicted a good prognosis in patients with early-onset OC. High PVT1 and MYC expression may predict a good prognosis because of cell senescence induced by oncogenes and DNA damage caused by excessive replication stress in oncogenes. ATM-Chk1 and ATR-Chk2 pathway activation leads to p53 and retinoblastoma protein upregulation, which has a synergistic effect on cell growth arrest.
In conclusion, PVT1 may provide new insights for future treatment strategies and cisplatin resistance in OC. PVT1 may be a powerful biomarker for OC diagnosis and prognosis.
PVT1 in cervical cancer
CC is the second leading cause of cancer-related deaths among women aged 20–39 years [1]. Therefore, identifying the molecular markers and therapeutic targets is important.
Sun et al. [161, 162] showed that PVT1 could be used as a new non-invasive biomarker for the early diagnosis of CC. Iden et al. [17] showed that PVT1 may promote cell proliferation, migration, and invasion through interaction with nucleolar proteins, and is associated with poor prognosis of CC. Zhang et al. [46] revealed that PVT1 downregulates miR-200b by recruiting EZH2 to the miR-200b promoter region, thereby promoting CC cell cycle progression and migration (Fig. 5L). Subsequently, Shen et al. [163] confirmed that PVT1 attenuates miR-195 by binding EZH2 to increase the H3K27me3 level in the promoter region (Fig. 5M). They also found that PVT1 acts as a sponge to attract miR-195 and that PVT1 inhibition reduced paclitaxel-induced EMT and chemotherapy resistance. Moreover, Gao et al. [164] reported that PVT1 promotes the progression and invasion of CC by targeting miR-424 (Fig. 5N). Another study demonstrated that PVT1 promotes CC cell growth and invasion by downregulating TGF-β1 expression [165]. Further studies demonstrated that PVT1 regulated CC cell growth, invasion, and apoptosis by upregulating the nuclear factor-κB, ECM1, ARL2, and Smad3 pathways by modulating miR-16, miR-486-3p, miR-503, and miR-140-5p (Fig. 5O−R) [166–169], respectively.
These data demonstrate that PVT1 is an important molecular marker and significant therapeutic target for CC.
PVT1 in endometrial cancer
Endometrial cancer is the most common metastatic malignant tumor among women, and originates from endometrial epithelial cells [170]. Therefore, there is an urgent need to elucidate the underlying molecular mechanisms.
Kong et al. [18] demonstrated that the PVT1-miR-195-5p-FGFR1/FGF2 axis plays an important role in endometrial cancer (Fig. 5S). They found that cell proliferation, migration, and invasion were inhibited by PVT1 knockdown.
In conclusion, PVT1 plays a key role in endometrial cancer and is expected to become a new therapeutic target and be included in diagnostic screening methods in the future.
Role of PVT1 in the urinary system
PVT1 in renal cell carcinoma
By 2022, 79,000 new cases of kidney and pelvic cancer will be diagnosed in the USA, and 13,920 people will die from the disease [1]. Approximately 85% of kidney tumors are RCC [171]. RCC is classified into three subtypes: clear cell RCC (ccRCC), papillary carcinoma, and chromophobe RCC. RCC is associated with late detection and poor prognosis; therefore, new and effective detection methods must be explored [172].
One study pointed out that hypomethylation of the PVT1 promoter leads to its upregulation in patients with RCC. PVT1 upregulation stabilizes MYC expression, promotes tumor occurrence, and predicts a poor prognosis [20]. Subsequently, Li et al. [173] further demonstrated that PVT1 regulates the RCC cell cycle as well as apoptosis, and proliferation by upregulating EGFR expression and affecting its downstream proteins, AKT and MYC. Another study showed that PVT1 promotes RCC cell growth and inhibits RCC cell apoptosis by upregulating Mcl-1 [174]. Recently, Zhang et al. [175] found that HIF-2α promotes PVT1 expression by binding to the PVT1 enhancer; similarly, PVT1 can protect HIF-2α from ubiquitin-dependent degradation. This PVT1/HIF-2α loop promotes tumorigenesis and metastasis in RCC (Fig. 6A). Wang et al. [176] showed that PVT1 is significantly associated with a poor prognosis in patients with ccRCC. Furthermore, Wu et al. [177] found a 5-lncRNA signature, including lncRNA PANDAR, PVT1, LET, PTENP1, and linc00963, which was used to differentiate benign and malignant renal masses. Similarly, Liu et al. [178] proved that PVT1 combined with TCL6, mIR-155HG, and HAR1B could be used as biomarkers to evaluate the prognosis of ccRCC. Yang et al. [179] reported that PVT1 promotes the proliferation and metastasis of RCC by competitively binding miR-200s to upregulate BMI1, ZEB1, and ZEB2 (Fig. 6B). Another study showed that PVT1 acts as a sponge for miR-16-5p to regulate apoptosis and EMT in RCC cells (Fig. 6C) [180].
Fig. 6.
The role of PVT1 in the urinary system. A PVT1 forms a positive feedback loop with HIF2α protein. B PVT1 promotes BMI1, ZEB1, and ZEB2 by targeting miR-200s. C PVT1 can directly target miR-16-5p. D PVT1 promotes the expression of CDK1 by targeting miR-31. E PVT1 promotes the expression of VEGFC by targeting miR-128. F PVT1 promotes the expression of BCLAF1 by targeting miR-194-5p. G PVT1 leads to chemoresistance in BCa by activating the Wnt/β-catenin signaling pathway. H PVT1 represses NOV expression by recruiting EZH2 to the promoter region of NOV. I PVT1 promotes Twist1 expression by targeting miR-186 and ultimately leads to EMT. J PVT1 promotes the expression of KIF23 by targeting miR-15a-5p. K PVT1 can directly target miR-146a
In summary, PVT1 was specifically upregulated in RCC, especially ccRCC. Many studies have shown that PVT1 combined with other lncRNAs is an efficient and accurate method for RCC diagnosis and prognosis prediction.
PVT1 in bladder cancer
Bladder cancer is the sixth most common cancer in men, with approximately 500,000 new cases and 200,000 deaths worldwide each year [181]. Current diagnostic markers, such as bladder tumor antigen and nuclear matrix protein, are not suitable for early bladder cancer owing to their lack of specificity and sensitivity [182]. Therefore, identifying new biomarkers is necessary for early diagnosis.
Zhuang et al. [21] reported that downregulation of PVT1 inhibits bladder cancer growth and induces apoptosis. Another study showed that elevated PVT1 was significantly associated with poor prognosis in muscle-invasive bladder cancer [183]. Tian et al. [184] demonstrated that the PVT1/miR-31/CDK1 pathway is responsible for the invasion, metastasis, and occurrence of bladder cancer (Fig. 6D). VEGFC is a lymphatic vasculature growth factor involved in lymphangiogenesis, angiogenesis, and regional lymphatic metastasis. Subsequently, Yu et al. [185] reported that PVT1 promotes the growth and metastasis of bladder cancer cells by upregulating VEGFC expression by acting as a ceRNA of miR-128 (Fig. 6E). Recently, Chen et al. [186] reported that PVT1 expression was significantly increased in bladder cancer. The PVT1/miR-194-5p/BCLAF1 axis was reportedly involved in the malignant progression and development of bladder cancer (Fig. 6F).
Another study indicated that PVT1 promotes the expression of MDR1 and MRP1 in bladder cancer by activating the Wnt/β-catenin pathway, ultimately reducing the response of bladder cancer cells to doxorubicin and cisplatin (Fig. 6G) [187].
In conclusion, PVT1 plays an important role in bladder cancer and is a new biomolecular marker that may be used as a new therapeutic target and diagnostic tool.
PVT1 in prostate cancer
According to the analysis of the 2022 Cancer Statistics, the incidence of PCa in American men ranked first among all cancers, accounting for 27% of all cases [1]. Although prostate-specific antigen can detect PCa early, recurrence in patients with advanced PCa is still an important factor that affects prognosis. Therefore, the underlying mechanisms of PCa need to be further explored.
A study suggested that exon 9 of PVT1 may be closely associated with invasive PCa in men of African descent [22]. Four years later, Pal et al. [188] demonstrated that exon 9 of PVT1 induced the proliferation and migration of prostate epithelial cells and was correlated with castration resistance after androgen deprivation therapy. A year later, Videira et al. [47] pointed out that PVT1 upregulation downregulated the expression of the androgen suppressor gene NOV through epigenetic modifications that recruited EZH2 to its promoter. This eventually led to the progression of androgen-independent castration-resistant PCa (Fig. 6H). Moreover, Yang et al. [189] reported that the knockdown of PVT1 significantly inhibited PCa cell growth, promoted apoptosis, and reduced c-Myc expression in cells. Subsequently, Chang et al. [190] found that PVT1 acts as a sponge of miR-186 to promote the expression of the EMT-related transcription factor TWIST1 (Fig. 6I). Wan et al. [191] showed that PVT1 downregulation inhibited PCa cell proliferation by reducing the phosphorylation of mitosis-related molecule P38. Another study discovered that PVT1 upregulated the expression of tumor metastasis-related protein NOP2 and promoted the invasion and metastasis of PCa [192]. Recently, Wu et al. [193] demonstrated that PVT1 promotes PCa progression by mediating the miR-15a-5p/KIF23 pathway (Fig. 6J). In addition, another study pointed out that PVT1 promotes tumor growth by regulating miR-146a methylation (Fig. 6K) [194].
In conclusion, high PVT1 expression plays an important role in promoting tumorigenesis in castrate-resistant prostate cancer and PCa.
Role of PVT1 in the immune system
The immune system is important as it regulates the body’s immune responses and functions. It is composed of immune organs, cells, and molecules. Changes in the immune system may affect the occurrence and development of various diseases, including cancer. Therefore, studying the effect of PVT1 on the immune system is of considerable significance for the future treatment of tumors through immune regulation [195].
Sjogren’s syndrome is a chronic autoimmune disease characterized by highly activated CD4+ T cells in the salivary glands. Fu et al. [196] found that PVT1 overexpression in patients with Sjogren’s syndrome promoted CD4+ T-cell activation (Fig. 7A). Lu et al. [197] showed that PVT1 promotes regulatory T-cell autophagy and ultimately inhibits allograft rejection by acting as a sponge for miR-146a (Fig. 7B). Luo et al. [198] reported that PVT1 promotes M1 macrophage polarization and aggravates myocardial injury through the miR-29a/HMGB1 axis in sepsis-induced myocardial injury. Immune thrombocytopenia (ITP) is an acquired autoimmune disease characterized by a significant increase in T helper 17 (Th17) cells in peripheral blood (Fig. 7C). Yu et al. [199] found that PVT1 overexpression reduced Th17 differentiation by downregulating NOTCH1 levels, thereby alleviating the occurrence of ITP. Myeloid-derived suppressor cells (MDSCs) can impair the antitumor response induced by T cells, thereby achieving tumor immunosuppression (Fig. 7D). Zheng et al. [200] found that the knockdown of PVT1 significantly inhibited the immunosuppressive ability of MDSCs (Fig. 7E).
Fig. 7.
The role of PVT1 in the immune system. A PVT1 can activate CD4+ T cells. B PVT1 can promote autophagy of regulatory T cells by targeting miR-146a. C PVT1 can promote the expression of HMGB1 and promote the polarization of M1 macrophages by targeting miR-29a. D PVT1 can reduce TH17 differentiation by attenuating NOTCH1 expression. E PVT1 can promote the effect of MDSCs to achieve tumor immune suppression
Role of PVT1 in tumors of other systems
PVT1 in glioma
Glioma is the most aggressive malignant tumor of the central nervous system and occurs mainly in the brain and glial tissues. The 5-year survival rate of glioma is only 0.05–4.7%. Therefore, exploring the pathogenesis of glioma is of great significance for improving its therapeutic effect in the future [201].
One study showed that PVT1, as a ceRNA, binds to miR-190a-5p and miR-488-3p to upregulate myocyte enhancer factor 2C expression. It then promotes the expression of JAGGED1, which ultimately leads to increased malignant behavior in glioma cells (Fig. 8A) [202]. A year later, Han et al. [203] showed that PVT1 promotes glioma progression as a ceRNA of miR-424 (Fig. 8B). Another study came to a similar conclusion that PVT1 acted as a sponge of miR-200a and promoted glioma proliferation and invasion (Fig. 8C) [204]. A study by Lv et al. [205] indicated that PVT1 promotes glioma progression by downregulating UPF1 expression.
Fig. 8.
The role of PVT1 in the other systems. A PVT1 promotes the expression of MEF2C by targeting miR-190a-5p and miR-488-3p. B PVT1 can directly target miR-424. C PVT1 can directly target miR-200a. D PVT1 promotes the expression of GREM1 by targeting miR-128-3p. E PVT1 promotes PTBP1 by targeting miR-128-1-5p. F PVT1 promotes TMBIM6 by targeting miR-1301-3p. G PVT1 promotes HNF1B by targeting miR-1207-3p. H PVT1 promotes Atg7 and Beclin1 by targeting miR-186. I PVT1 promotes the expression of ELF4 by targeting miR-365 to regulate the expression of SOX2. J PVT1 represses its expression by recruiting EZH2 to the promoter region of TSHR. K PVT1 can directly target miR-30a. L PVT1 promotes the expression of PAK3 by targeting miR-423-5p. M PVT1 promotes the expression BCL2 by targeting miR-195. N PVT1 promotes the expression of HK2 by targeting miR-497. O PVT1 promotes the expression of ERG by targeting miR-183-5p. P PVT1 can directly target miR-484. Q PVT1 promotes the expression of the c-MET/PI3K/AKT signaling pathway by targeting miR-152, which leads to chemoresistance
Many studies have revealed the important role of the lncRNA–miRNA–mRNA pathway in gliomas. Specifically, PVT1 reportedly promotes glioma cell proliferation, invasion, metastasis, and EMT by upregulating GREM1, PTBP1, TMBIM6, HNF1B, and Atg7/Beclin1 by modulating miR-128-3p, miR-128-1-5p, miR-1301-3p, miR-1207-3p, and miR-186, respectively (Fig. 8D–H) [23, 206–209].
PVT1 is also involved in chemotherapy resistance in glioma. Gong et al. [210] found that PVT1 upregulated ELF4 expression by acting as a ceRNA of miR-365, which then directly activated stem cell-related protein SOX2 expression, ultimately promoting stem cell characteristics and temozolomide resistance in gliomas (Fig. 8I).
Taken together, these studies demonstrate that PVT1 is an oncogene in glioma and may be a target for future therapy.
PVT1 in thyroid cancer
TC is the most common malignant tumor of the endocrine glands. According to the latest cancer statistics, an estimated 43,800 new cases were reported in 2022 [1]. Primary TCs include papillary TC (PTC), follicular TC, medullary TC, and anaplastic TC. PTC accounts for 85–90% of all TCs and has a good prognosis. Anaplastic TC is the most aggressive TC and has a poor prognosis and low survival rate [211]. Exploring the molecular mechanism of TC is of great significance for discovering new therapeutic targets in the future.
One study showed that PVT1 promotes TC cell proliferation by recruiting EZH2 and affecting TSHR expression (Fig. 8J) [26]. Another study showed that high PVT1 levels promoted TC cell growth and invasion by targeting the miR-30a/IGF1R axis and was associated with higher TNM and LNM stages (Fig. 8K) [212]. Two years later, Lin et al. [213] showed that PVT1 promoted malignant proliferation and migration of TC through the miR-423-5p/PAK3 pathway (Fig. 8L). In addition, Possieri et al. [214] showed that co-expression of MALAT1, PVT1, and HOTAIR could be used to distinguish benign and malignant thyroid nodules.
In conclusion, these results suggest that PVT1 plays a significant role in promoting TC, which is related to TNM and LNM stages, and TC tumor invasion, and can be used in the diagnosis of thyroid nodules.
PVT1 in osteosarcoma
OS is a rare tumor that often occurs in children and adolescents. Approximately 400 children and adolescents are diagnosed with OS in the USA every year, and as many as 25% of patients have metastasis by the time they are diagnosed. Therefore, exploring the mechanism of metastasis of OS is important for the development of future treatments [215, 216].
Zhou et al. [24] showed that PVT1 upregulates the expression of BCL2 by inhibiting miR-195, thereby inducing OS cell cycle arrest, inhibiting apoptosis, and promoting cell migration and invasion (Fig. 8M). Another study indicated that PVT1 upregulated HK2 by binding miR-497 and increasing glucose uptake and lactate production in OS cells, which ultimately accelerated cell proliferation and invasion (Fig. 8N) [217]. Similarly, Zhao et al. [218] showed that PVT1, as a ceRNA, inhibits its degradation and ubiquitination by binding to miR-183-5p, thereby upregulating ERG and ultimately promoting OS progression and metastasis (Fig. 8O). A year later, Yan et al. [219] found that PVT1 promoted metastasis in OS by targeting miR-484 (Fig. 8P). Xun et al. [220] demonstrated that PVT1 promotes EMT in OS cells and is highly correlated with TNM stage and distant metastases, which may be used as an independent prognostic risk marker of OS. In addition, Chen et al. [221] reported that the expression of PVT1 was upregulated in OS. Functionally, ALKBH5-mediated upregulation of PVT1 promotes OS cell growth in vitro and in vivo. Sun et al. [222] demonstrated that PVT1 enhanced the chemoresistance of OS by targeting miR-152 to activate the c-MET/PI3K/AKT signaling pathway (Fig. 8Q).
Taken together, these studies show that PVT1 is a significant factor in promoting OS progression and chemoresistance.
PVT1 in multiple myeloma
MM is a malignant tumor that originates from mutations in the bone marrow plasma cells and is characterized by abnormal proliferation and production of monoclonal immunoglobulins or light chains. Although current treatments can greatly improve remission rates, patients have a high risk of relapse or progression. Therefore, exploration of its pathogenesis is urgently needed to develop further treatments for this disease [223].
Yang et al. [25] demonstrated that PVT1 promotes MM cell proliferation by competitively binding to miR-203a. Handa et al. [224] showed that MYC and PVT1 synergistically promote MM progression.
Overall, these data suggest that PVT1 may serve as a future therapeutic target in patients with MM.
PVT1 in lymphoma
Lymphoma is a malignant tumor originating from lymphatic tissue and is mainly divided into Hodgkin’s and non-Hodgkin’s lymphoma (NHL). Hodgkin’s lymphoma is nearly twice as common as NHL, whereas the opposite is true for children with Hodgkin’s lymphoma [1]. Diffuse large B-cell lymphoma (DLBCL) is the most common and aggressive NHL subtype, accounting for 40% of NHL cases. Owing to the lack of effective treatments, survival rates remain very low [225].
Yang et al. [27] showed that overexpression of PVT1 promoted the proliferation of DLBCL cells and predicted poor prognosis.
This evidence suggests that PVT1 acts as an oncogene to promote lymphoma growth.
PVT1 in leukemia
Leukemia is a malignant tumor of the hematopoietic system. Leukemia can be classified as acute or chronic leukemia. Acute leukemia can be further classified as acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). Chronic leukemia can be classified as chronic myeloid leukemia and chronic lymphocyte leukemia (CLL). The 5-year survival rates are 27.4% and 84.2% for AML and CLL, respectively. Identifying new gene targets is important for improving leukemia cure rates [226].
Houshmand et al. [28] showed that PVT1 knockout in hematologic malignancies results in c-Myc degradation, decreased proliferation, increased apoptosis, and cell cycle arrest. PVT1 expression was higher in patients with AML than in healthy controls. In addition, PVT1 expression levels in the high-risk AML group were higher than in the medium- and low-risk AML groups. Similarly, Izadifard et al. [227] reported that PVT1 expression was higher in patients with AML than in healthy controls. PVT1 expression levels in the high-risk AML group were higher than in the medium- and low-risk AML groups. A subsequent study also confirmed that PVT1 and CCAT1 were highly expressed in patients with AML and were associated with poor prognosis [228]. Salehi et al. [229] showed that the inhibition of PVT1 significantly induced AML cell apoptosis and necrosis and reduced proliferation and C-MYC expression in AML cells. A year later, another study confirmed the relationship between PVT1 and c-Myc and suggested that the PVT1 blockade might be a potential treatment for AML [230]. In addition, Cheng et al. [231] found that PVT1 promotes the malignant progression of AML through the miR-29 family/WAVE1 axis, suggesting that PVT1 may be a potential therapeutic target for AML. Another study showed that PVT1 knockout significantly promoted apoptosis of ALL cells, blocked the cell cycle at G0/G1, reduced the proliferation rate, and downregulated the expression of oncogene c-Myc [232].
In conclusion, PVT1, as an oncogene, plays an important role in the development of leukemia and may be a therapeutic target in the future.
Circular RNA PVT1 in various human tumors
The PVT1 gene located on chromosome 8 encodes lncRNA PVT1 as well as circular RNA PVT1 (circPVT1), obtained by circularization of its exon 2. circPVT1 is also a noncoding RNA that is widely present in the occurrence and development of various tumors [233].
In the respiratory system, circPVT1 has oncogenic effects in patients with NSCLC, lung adenocarcinoma, and lung squamous cell carcinoma (LSCC). Qin et al. [234] reported that circPVT1, as a ceRNA of miR-497, indirectly regulates Bcl-2 expression to promote the proliferation of NSCLC and inhibit cell apoptosis. Zheng et al. [235] demonstrated that circPVT1 regulates cisplatin and pemetrexed resistance in lung adenocarcinoma by acting as a sponge for miR-145-5p. Gao et al. [236] reported similar results, showing that circPVT1 enhances cisplatin resistance in lung adenocarcinoma cells by regulating miR-429/forkhead box K1 expression. Finally, Shi et al. [237] revealed that circPVT1 was significantly upregulated in the tissues, serum, and cell lines of patients with LSCC and promoted LSCC progression by increasing cyclin F expression, acting as a sponge for miR-30d and miR-30e.
In the digestive system, circPVT1 is closely related to the occurrence, development, and drug resistance of various tumors. He et al. [238] showed that circPVT1 regulates STAT3 levels by acting as a sponge for miR-125b and ultimately increases OSCC cell proliferation. Wang et al. [239] revealed that circPVT1 promotes OSCC progression by regulating the miR-143-3p/SLC7A11 axis and affecting the MAPK signaling pathway. Zhong et al. [240] found that circPVT1 regulated the progression of EC by influencing miR-4663 levels to modulate Paxs and peroxisome proliferator-activated receptor levels. Yao et al. [241] revealed that circPVT1 increased EC cell resistance to 5-fluorouracil by inhibiting ferroptosis through miR-30a-5p/Frizzled3. Chen et al. [242] found that circPVT1 was significantly upregulated in patients with GC and modulated the proliferation of GC cells by acting as a sponge for miR-125. These results suggested that circPVT1 expression is an independent prognostic marker. Liu et al. [243] showed that circPVT1 enhanced the resistance of GC cells to paclitaxel through the miR-124-3p/ZEB1 axis. Similarly, Wang et al. [244] showed that circPVT1 regulates the expression of HCC-derived growth factors by targeting miR-152-3p, leading to cisplatin resistance in GC cells. Zhu et al. [245] found that upregulation of circPVT1 regulates the proliferation and invasion ability of HCC cells by affecting the miR-203/homeobox D3 axis. Bu et al. [246] found that circPVT1 regulated HCC cell proliferation and glycolysis through sponging of miR-377. Wang et al. [247] found that circPVT1 regulated CRC cell metastasis by acting as a sponge for miR-145.
CircPVT1 also plays an important role in the endocrine and urinary systems [248]. Bian et al. [249] reported that circPVT1 regulated BC cell invasion and EMT by acting as a ceRNA of miR-204-5p. Wang et al. [250] revealed that circPVT1 promotes the ARG2/HIF-1α axis by regulating miR-29a-3p, thereby enhancing BC cell proliferation, invasion, and metastasis. In addition, Sun et al. [251] found that circPVT1 inhibited apoptosis and promoted OC cell proliferation by sponging miR-149. Zheng et al. [252] showed that circPVT1 affects ccRCC cell growth and metastasis by targeting the miR-145-5p/TX15 axis.
Leukemia is a disease that occurs mainly in the region of chromosome 8q24. Therefore, studying circPVT1, which is also located on chromosome 8, is of great significance for further exploration of the pathogenesis of leukemia [253]. Hu et al. [254] found that circPVT1 was significantly upregulated in patients with ALL and promoted cell proliferation by promoting the expression of c-Myc and Bcl-2. Gaffo et al. [255] showed that circPVT1 was significantly upregulated in children with B-precursor ALL. Moreover, a study by Chen et al. [256] revealed that circPVT1 was significantly upregulated in 68 patients with AML, and patients with high circPVT1 expression had significantly shortened overall and shortened event-free survival rates, suggesting that circPVT1 may be used as a biomarker to assess prognosis.
Osteosarcoma (OS) is a common primary bone malignancy. Noncoding RNA, as an oncogenic factor, also plays an important role in OS [257]. Wan et al. [258] demonstrated that circPVT1 inhibited miR-423-5p, thereby promoting the Wnt5a/Ror2 signaling pathway and affecting OS cell glycolysis, proliferation, migration, and metastasis. Huang et al. [259] found that circPVT1 inhibition significantly inhibited proliferation and induced apoptosis of OS cells through the miR-26b-5p/CCNB1 axis. Li et al. [260] validated that circPVT1 enhances the resistance of OS cells to doxorubicin by regulating the miR-137/TRIAP1 axis.
The abnormal expression of circPVT1 in patients with TC also warrants further investigation. Tao et al. [261] confirmed that circPVT1 inhibited PTC progression by sponging miR-126. Subsequently, Zeng et al. [262] showed that circPVT1 acted as a sponge for miR-195 to regulate VEGFA expression. circPVT1 promotes the Wnt/β-catenin signaling pathway and proliferation, migration, and invasion of PTC. In addition, Zheng et al. [261] reported that circPVT1 regulates EMT by targeting the miR-455-5p/CXCL12/CXCR4 signaling pathway and promotes thyroid medullary cancer cell proliferation, invasion, and migration.
Conclusions
Cancer is one of the greatest risks to human health. By 2022, 1,918,030 new cases and 609,360 cancer-related deaths are estimated to occur in the USA [1]. Owing to delayed diagnosis, recurrence, metastasis, chemotherapy resistance, and other problems, patients tend to have poor prognosis and low survival rates. Therefore, the discovery of new biomarkers for early diagnosis and new targets in the treatment of cancer is vital for improving the survival rates of patients with cancer.
With the development of second-generation sequencing and bioinformatics, lncRNAs have gradually emerged in our field of vision, and have been found to play important roles in tumor progression. Previously, lncRNAs were reported to directly regulate chromatin topology or act as scaffolds for RNA and protein expression. Many studies have found that lncRNAs, including PVT1, are differentially expressed in tumor tissues compared with non-tumor tissues. However, the upstream and downstream regulatory mechanisms and how they affect the occurrence and development of tumors remain unclear. This study provides a new perspective for understanding the mechanisms underlying tumorigenesis and its development.
This review describes the mechanisms of action of PVT1 in various cancers. We found that PVT1 acts as a ceRNA to bind miRNAs and regulate downstream gene expression. PVT1 can also bind directly to the promoter region of the target gene, thereby promoting its methylation to regulate its expression. PVT1 also promotes the proliferation, invasion, and EMT of various tumor cells. For example, Wang et al. [87] pointed out that PVT1 promotes EMT in GC cells through the miR-30a/Snail axis. PVT1 is a biomarker that can be detected in serum. Wu et al. [177] constructed a model based on five lncRNAs (LET, PVT1, PANDAR, PTENP1, and linc00963), which are highly valuable in the diagnosis of ccRCC. In addition, PVT1 plays an important role in chemotherapy resistance. For example, tumor tissues with high PVT1 expression are resistant to GEM, cisplatin, adriamycin, and other chemotherapy drugs [40, 72, 149]. Some studies have also shown that PVT1 is a critical regulatory molecule in radiotherapy resistance. For instance, Wang et al. [70] showed that PVT1 significantly improved the radioresistance of NSCLC cells.
In summary, PVT1 plays an oncogenic role in many cancers. PVT1 is closely associated with the onset, development, invasion, migration, and treatment of cancer. PVT1 is an emerging biomarker for the diagnosis and treatment of cancer.
Acknowledgements
Not applicable.
Abbreviations
- ALL
Acute lymphoblastic leukemia
- AML
Acute myeloid leukemia
- BC
Breast cancer
- Bcl-2
B-cell lymphoma
- CC
Cervical cancer
- CCA
Cholangiocarcinoma
- ccRCC
Clear cell renal cell carcinoma
- ceRNA
Competitive endogenous RNA
- circPVT1
Circular RNA PVT1
- CLL
Chronic lymphocyte leukemia
- CRC
Colorectal cancer
- DLBCL
Diffuse large B-cell lymphoma
- EC
Esophageal cancer
- EMT
Epithelial–mesenchymal transition
- ESCC
Esophageal squamous cell carcinoma
- FGFR1
Fibroblast growth factor receptor 1
- GBC
Gallbladder cancer
- GC
Gastric cancer
- GEM
Gemcitabine
- HBV
Hepatitis B virus
- HCC
Hepatocellular carcinoma
- HIF
Hypoxia-inducible facto
- IFN-α
Interferon alpha
- ITP
Immune thrombocytopenia
- lncRNAs
Long noncoding RNAs
- LNM
Lymph node metastasis
- LSCC
Lung squamous cell carcinoma
- MDSCs
Myeloid-derived suppressor cells
- miRNA
MicroRNA
- MM
Multiple myeloma
- MDR1
Multidrug resistance 1
- MRP1
Multidrug resistance-related protein 1
- mRNA
Messenger RNA
- NHL
Non-Hodgkin’s lymphoma
- NOTCH1
Neurogenic locus notch homolog protein 1
- NPC
Nasopharyngeal carcinoma
- NSCLC
Non-small cell lung cancer
- OC
Ovarian cancer
- OS
Osteosarcoma
- OSCC
Oral squamous cell carcinoma
- PI3K/AKT
Phosphatidylinositol 3-kinase/protein kinase B
- PC
Pancreatic cancer
- PCa
Prostate cancer
- PTC
Papillary thyroid cancer
- PVT1
Plasmacytoma variant translocation 1
- RCC
Renal cell carcinoma
- SOX2
SRY-box transcription factor 2
- STAT
Signal transducer and activator of transcription
- TC
Thyroid cancer
- TGF-β
Transforming growth factor beta
- Th17
T helper 17
- TNM
Tumor, node, metastasis
- VEGF
Vascular endothelial growth factor
Author contributions
K.W., R.L., and X.W. conceived the review; K.W., R.L., and C.Z. wrote the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by National Natural Science Foundation of China (grant no. 82072835) to K. Wang, Key Research and Development Joint Program of Liaoning Province (grant no. 2020JH 2/10300139) to K. Wang, Natural Science Foundation of Liaoning Province (grant no. 2019-MS-360) to K. Wang, Shenyang Science and Technology Bureau Plan Projects (grant no. 20-205-4-076) to K. Wang, 345 Talent Project of Shengjing Hospital of China Medical University (grant no. M0366) to K. Wang, and Outstanding Scientific Fund of Shengjing Hospital to K. Wang.
Availability of data and materials
Not applicable.
Declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Chunming Zhu, Email: chunmzhu@126.com.
Kefeng Wang, Email: wang.kefeng@hotmail.com.
References
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. Cancer J Clin. 2022;72(1):234. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 2.Ransohoff JD, Wei Y, Khavari PA. The functions and unique features of long intergenic non-coding RNA. Nat Rev Mol Cell Biol. 2018;19(3):143–157. doi: 10.1038/nrm.2017.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brockdorff N, Ashworth A, Kay GF, McCabe VM, Norris DP, Cooper PJ, et al. The product of the mouse Xist gene is a 15 kb inactive X-specific transcript containing no conserved ORF and located in the nucleus. Cell. 1992;71(3):515–526. doi: 10.1016/0092-8674(92)90519-I. [DOI] [PubMed] [Google Scholar]
- 4.Kandoth C, McLellan MD, Vandin F, Ye K, Niu B, Lu C, et al. Mutational landscape and significance across 12 major cancer types. Nature. 2013;502(7471):333–339. doi: 10.1038/nature12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin A, Hu Q, Li C, Xing Z, Ma G, Wang C, et al. The LINK-A lncRNA interacts with PtdIns(3,4,5)P3 to hyperactivate AKT and confer resistance to AKT inhibitors. Nat Cell Biol. 2017;19(3):238–251. doi: 10.1038/ncb3473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cui D, Yu CH, Liu M, Xia QQ, Zhang YF, Jiang WL. Long non-coding RNA PVT1 as a novel biomarker for diagnosis and prognosis of non-small cell lung cancer. Tumour Biol. 2016;37(3):4127–4134. doi: 10.1007/s13277-015-4261-x. [DOI] [PubMed] [Google Scholar]
- 7.He Y, Jing Y, Wei F, Tang Y, Yang L, Luo J, et al. Long non-coding RNA PVT1 predicts poor prognosis and induces radioresistance by regulating DNA repair and cell apoptosis in nasopharyngeal carcinoma. Cell Death Dis. 2018;9(2):235. doi: 10.1038/s41419-018-0265-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kong R, Zhang EB, Yin DD, You LH, Xu TP, Chen WM, et al. Long noncoding RNA PVT1 indicates a poor prognosis of gastric cancer and promotes cell proliferation through epigenetically regulating p15 and p16. Mol Cancer. 2015;14:82. doi: 10.1186/s12943-015-0355-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li X, Ren H. Long noncoding RNA PVT1 promotes tumor cell proliferation, invasion, migration and inhibits apoptosis in oral squamous cell carcinoma by regulating miR-150-5p/GLUT-1. Oncol Rep. 2020;44(4):1524–1538. doi: 10.3892/or.2020.7706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang S, Ning Q, Zhang G, Sun H, Wang Z, Li Y. Construction of differential mRNA–lncRNA crosstalk networks based on ceRNA hypothesis uncover key roles of lncRNAs implicated in esophageal squamous cell carcinoma. Oncotarget. 2016;7(52):85728–85740. doi: 10.18632/oncotarget.13828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang R, Li J, Yan X, Jin K, Li W, Liu X, et al. Long noncoding RNA plasmacytoma variant translocation 1 (PVT1) promotes colon cancer progression via endogenous sponging miR-26b. Med Sci Monit. 2018;24:8685–8692. doi: 10.12659/MSM.910955. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 12.Ding C, Yang Z, Lv Z, Du C, Xiao H, Peng C, et al. Long non-coding RNA PVT1 is associated with tumor progression and predicts recurrence in hepatocellular carcinoma patients. Oncol Lett. 2015;9(2):955–963. doi: 10.3892/ol.2014.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jin L, Cai Q, Wang S, Wang S, Wang J, Quan Z. Long noncoding RNA PVT1 promoted gallbladder cancer proliferation by epigenetically suppressing miR-18b-5p via DNA methylation. Cell Death Dis. 2020;11(10):871. doi: 10.1038/s41419-020-03080-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yu A, Zhao L, Kang Q, Li J, Chen K, Fu H. SOX2 knockdown slows cholangiocarcinoma progression through inhibition of transcriptional activation of lncRNA PVT1. Biochem J. 2020;477(18):3527–3540. doi: 10.1042/BCJ20200219. [DOI] [PubMed] [Google Scholar]
- 15.Xie Z, Chen X, Li J, Guo Y, Li H, Pan X, et al. Salivary HOTAIR and PVT1 as novel biomarkers for early pancreatic cancer. Oncotarget. 2016;7(18):25408–25419. doi: 10.18632/oncotarget.8323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guan Y, Kuo W-L, Stilwell JL, Takano H, Lapuk AV, Fridlyand J, et al. Amplification of PVT1 contributes to the pathophysiology of ovarian and breast cancer. Clin Cancer Res. 2007;13(19):5745–5755. doi: 10.1158/1078-0432.CCR-06-2882. [DOI] [PubMed] [Google Scholar]
- 17.Iden M, Fye S, Li K, Chowdhury T, Ramchandran R, Rader JS. The lncRNA PVT1 contributes to the cervical cancer phenotype and associates with poor patient prognosis. PLoS ONE. 2016;11(5):e0156274. doi: 10.1371/journal.pone.0156274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kong F, Ma J, Yang H, Yang D, Wang C, Ma X. Long non-coding RNA PVT1 promotes malignancy in human endometrial carcinoma cells through negative regulation of miR-195–5p. Mol Cell Res. 2018;56:78. doi: 10.1016/j.bbamcr.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Liu E, Liu Z, Zhou Y, Mi R, Wang D. Overexpression of long non-coding RNA PVT1 in ovarian cancer cells promotes cisplatin resistance by regulating apoptotic pathways. Int J Clin Exp Med. 2015;8(11):20565–20572. [PMC free article] [PubMed] [Google Scholar]
- 20.Posa I, Carvalho S, Tavares J, Grosso AR. A pan-cancer analysis of MYC-PVT1 reveals CNV-unmediated deregulation and poor prognosis in renal carcinoma. Oncotarget. 2016;7(30):47033–47041. doi: 10.18632/oncotarget.9487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhuang C, Li J, Liu Y, Chen M, Yuan J, Fu X, et al. Tetracycline-inducible shRNA targeting long non-coding RNA PVT1 inhibits cell growth and induces apoptosis in bladder cancer cells. Oncotarget. 2015;6(38):41194–41203. doi: 10.18632/oncotarget.5880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ilboudo A, Chouhan J, McNeil BK, Osborne JR, Ogunwobi OO. PVT1 exon 9: a potential biomarker of aggressive prostate cancer? Int J Environ Res Public Health. 2015;13(1):0012. doi: 10.3390/ijerph13010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fu C, Li D, Zhang X, Liu N, Chi G, Jin X. LncRNA PVT1 facilitates tumorigenesis and progression of glioma via regulation of MiR-128-3p/GREM1 axis and BMP signaling pathway. Neurotherapeutics. 2018;15(4):1139–1157. doi: 10.1007/s13311-018-0649-9. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Zhou Q, Chen F, Zhao J, Li B, Liang Y, Pan W, et al. Long non-coding RNA PVT1 promotes osteosarcoma development by acting as a molecular sponge to regulate miR-195. Oncotarget. 2016;7(50):82620–82633. doi: 10.18632/oncotarget.13012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang M, Zhang L, Wang X, Zhou Y, Wu S. Down-regulation of miR-203a by lncRNA PVT1 in multiple myeloma promotes cell proliferation. Arch Med Sci. 2018;14(6):1333–1339. doi: 10.5114/aoms.2018.73975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou Q, Chen J, Feng J, Wang J. Long noncoding RNA PVT1 modulates thyroid cancer cell proliferation by recruiting EZH2 and regulating thyroid-stimulating hormone receptor (TSHR) Tumour Biol. 2016;37(3):3105–3113. doi: 10.1007/s13277-015-4149-9. [DOI] [PubMed] [Google Scholar]
- 27.Yang R, Shao T, Long M, Shi Y, Liu Q, Yang L, et al. Long noncoding RNA PVT1 promotes tumor growth and predicts poor prognosis in patients with diffuse large B-cell lymphoma. Cancer Commun. 2020;40(10):551–555. doi: 10.1002/cac2.12073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Houshmand M, Yazdi N, Kazemi A, Atashi A, Hamidieh AA, Anjam Najemdini A, et al. Long non-coding RNA PVT1 as a novel candidate for targeted therapy in hematologic malignancies. Int J Biochem Cell Biol. 2018;98:54–64. doi: 10.1016/j.biocel.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Wang KC, Yang YW, Liu B, Sanyal A, Corces-Zimmerman R, Chen Y, et al. A long noncoding RNA maintains active chromatin to coordinate homeotic gene expression. Nature. 2011;472(7341):120–124. doi: 10.1038/nature09819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scarola M, Comisso E, Pascolo R, Chiaradia R, Marion RM, Schneider C, et al. Epigenetic silencing of Oct4 by a complex containing SUV39H1 and Oct4 pseudogene lncRNA. Nat Commun. 2015;6:7631. doi: 10.1038/ncomms8631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao J, Sun BK, Erwin JA, Song JJ, Lee JT. Polycomb proteins targeted by a short repeat RNA to the mouse X chromosome. Science. 2008;322(5902):750–756. doi: 10.1126/science.1163045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kretz M, Siprashvili Z, Chu C, Webster DE, Zehnder A, Qu K, et al. Control of somatic tissue differentiation by the long non-coding RNA TINCR. Nature. 2013;493(7431):231–235. doi: 10.1038/nature11661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yoon J-H, Abdelmohsen K, Srikantan S, Yang X, Martindale JL, De S, et al. LincRNA-p21 suppresses target mRNA translation. Mol Cell. 2012;47(4):648–655. doi: 10.1016/j.molcel.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee S, Kopp F, Chang T-C, Sataluri A, Chen B, Sivakumar S, et al. Noncoding RNA NORAD regulates genomic stability by sequestering PUMILIO Proteins. Cell. 2016;164(1–2):69–80. doi: 10.1016/j.cell.2015.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang J, Lou J, Liu X, Xie Y. LncRNA PCGsEM1 contributes to the proliferation, migration and invasion of non-small cell lung cancer cells via acting as a sponge for miR-152–3p. Curr Pharm Des. 2021;27:4663. doi: 10.2174/1381612827666210827104828. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Y, Pitchiaya S, Cieslik M, Niknafs YS, Tien JC, Hosono Y, et al. Analysis of the androgen receptor-regulated lncRNA landscape identifies a role for ARLNC1 in prostate cancer progression. Nat Genet. 2018;50(6):814–824. doi: 10.1038/s41588-018-0120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shigeyasu K, Toden S, Ozawa T, Matsuyama T, Nagasaka T, Ishikawa T, et al. The PVT1 lncRNA is a novel epigenetic enhancer of MYC, and a promising risk-stratification biomarker in colorectal cancer. Mol Cancer. 2020;19(1):155. doi: 10.1186/s12943-020-01277-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ansari H, Shahrisa A, Birgani YT, Birgani MT, Hajjari M, Asl JM. Long noncoding RNAs in colorectal adenocarcinoma; an in silico analysis. Pathol Oncol Res. 2019;25(4):1387–1394. doi: 10.1007/s12253-018-0428-2. [DOI] [PubMed] [Google Scholar]
- 39.Xiong X, Yuan J, Zhang N, Zheng Y, Liu J, Yang M. Silencing of lncRNA PVT1 by miR-214 inhibits the oncogenic GDF15 signaling and suppresses hepatocarcinogenesis. Biochem Biophys Res Commun. 2020;521(2):478–484. doi: 10.1016/j.bbrc.2019.10.137. [DOI] [PubMed] [Google Scholar]
- 40.Yoshida K, Toden S, Ravindranathan P, Han H, Goel A. Curcumin sensitizes pancreatic cancer cells to gemcitabine by attenuating PRC2 subunit EZH2, and the lncRNA PVT1 expression. Carcinogenesis. 2017;38(10):1036–1046. doi: 10.1093/carcin/bgx065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Y, Chen W, Lian J, Zhang H, Yu B, Zhang M, et al. The lncRNA PVT1 regulates nasopharyngeal carcinoma cell proliferation via activating the KAT2A acetyltransferase and stabilizing HIF-1α. Cell Death Differ. 2020;27(2):695–710. doi: 10.1038/s41418-019-0381-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wan L, Sun M, Liu GJ, Wei CC, Zhang EB, Kong R, et al. Long noncoding RNA PVT1 promotes non-small cell lung cancer cell proliferation through epigenetically regulating LATS2 expression. Mol Cancer Ther. 2016;15(5):1082–1094. doi: 10.1158/1535-7163.MCT-15-0707. [DOI] [PubMed] [Google Scholar]
- 43.Zhao J, Wu J, Qin Y, Zhang W, Huang G, Qin L. LncRNA PVT1 induces aggressive vasculogenic mimicry formation through activating the STAT3/Slug axis and epithelial-to-mesenchymal transition in gastric cancer. Cell Oncol (Dordr) 2020;43(5):863–876. doi: 10.1007/s13402-020-00532-6. [DOI] [PubMed] [Google Scholar]
- 44.Gou X, Zhao X, Wang Z. Long noncoding RNA PVT1 promotes hepatocellular carcinoma progression through regulating miR-214. Cancer Biomark. 2017;20(4):511–519. doi: 10.3233/CBM-170331. [DOI] [PubMed] [Google Scholar]
- 45.Yu Y, Zhang M, Liu J, Xu B, Yang J, Wang N, et al. Long non-coding RNA PVT1 promotes cell proliferation and migration by silencing ANGPTL4 expression in cholangiocarcinoma. Mol Ther Nucleic Acids. 2018;13:503–513. doi: 10.1016/j.omtn.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang S, Zhang G, Liu J. Long noncoding RNA PVT1 promotes cervical cancer progression through epigenetically silencing miR-200b. APMIS. 2016;124(8):649–658. doi: 10.1111/apm.12555. [DOI] [PubMed] [Google Scholar]
- 47.Videira A, Beckedorff FC, daSilva LF, Verjovski-Almeida S. PVT1 signals an androgen-dependent transcriptional repression program in prostate cancer cells and a set of the repressed genes predicts high-risk tumors. Cell Commun Signal. 2021;19(1):5. doi: 10.1186/s12964-020-00691-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Takahashi Y, Sawada G, Kurashige J, Uchi R, Matsumura T, Ueo H, et al. Amplification of PVT-1 is involved in poor prognosis via apoptosis inhibition in colorectal cancers. Br J Cancer. 2014;110(1):164–171. doi: 10.1038/bjc.2013.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li Q, Dai Y, Wang F, Hou S. Differentially expressed long non-coding RNAs and the prognostic potential in colorectal cancer. Neoplasma. 2016;63(6):977–983. doi: 10.4149/neo_2016_617. [DOI] [PubMed] [Google Scholar]
- 50.Fan H, Zhu J-H, Yao X-Q. Long non-coding RNA PVT1 as a novel potential biomarker for predicting the prognosis of colorectal cancer. Int J Biol Markers. 2018;33(4):415–422. doi: 10.1177/1724600818777242. [DOI] [PubMed] [Google Scholar]
- 51.Wang C, Zhu X, Pu C, Song X. Upregulated plasmacytoma variant translocation 1 promotes cell proliferation, invasion and metastasis in colorectal cancer. Mol Med Rep. 2018;17(5):6598–6604. doi: 10.3892/mmr.2015.4303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yamamoto A, Kurata M, Yamamoto K, Nogawa D, Inoue M, Ishibashi S, et al. High amplification of PVT1 and MYC predict favorable prognosis in early ovarian carcinoma. Pathol Res Pract. 2020;216(11):153175. doi: 10.1016/j.prp.2020.153175. [DOI] [PubMed] [Google Scholar]
- 53.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 54.Cui M, Chang Y, Fang Q-G, Du W, Wu J-F, Wang J-H, et al. Non-coding RNA Pvt1 promotes cancer stem cell-like traits in nasopharyngeal cancer via inhibiting miR-1207. Pathol Oncol Res. 2019;25(4):1411–1422. doi: 10.1007/s12253-018-0453-1. [DOI] [PubMed] [Google Scholar]
- 55.Han Y, Li F, Xie J, Wang Y, Zhang H. PVT1 mediates cell proliferation, apoptosis and radioresistance in nasopharyngeal carcinoma through regulating miR-515-5p/PIK3CA axis. Cancer Manag Res. 2020;12:10077–10090. doi: 10.2147/CMAR.S257583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guo D, Wang Y, Ren K, Han X. Knockdown of lncRNA PVT1 inhibits tumorigenesis in non-small-cell lung cancer by regulating miR-497 expression. Exp Cell Res. 2018;362(1):172–179. doi: 10.1016/j.yexcr.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 57.Zeng SHG, Xie JH, Zeng QY, Dai SHH, Wang Y, Wan XM, et al. lncRNA PVT1 promotes metastasis of non-small cell lung cancer through EZH2-mediated activation of Hippo/NOTCH1 signaling pathways. Cell J. 2021;23(1):21–31. doi: 10.22074/cellj.2021.7010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Qiu C, Li S, Sun D, Yang S. lncRNA PVT1 accelerates progression of non-small cell lung cancer via targeting miRNA-526b/EZH2 regulatory loop. Oncol Lett. 2020;19(2):1267–1272. doi: 10.3892/ol.2019.11237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen W, Zhu H, Yin L, Wang T, Wu J, Xu J, et al. lncRNA-PVT1 facilitates invasion through upregulation of MMP9 in nonsmall cell lung cancer cell. DNA Cell Biol. 2017;36(9):787–793. doi: 10.1089/dna.2017.3725. [DOI] [PubMed] [Google Scholar]
- 60.Wang C, Han C, Zhang Y, Liu F. LncRNA PVT1 regulate expression of HIF1alpha via functioning as ceRNA for miR199a5p in nonsmall cell lung cancer under hypoxia. Mol Med Rep. 2018;17(1):1105–1110. doi: 10.3892/mmr.2017.7962. [DOI] [PubMed] [Google Scholar]
- 61.Mao Z, Xu B, He L, Zhang G. PVT1 promotes angiogenesis by regulating miR-29c/vascular endothelial growth factor (VEGF) signaling pathway in non-small-cell lung cancer (NSCLC) Med Sci Monit. 2019;25:5418–5425. doi: 10.12659/MSM.917601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pan Y, Liu L, Cheng Y, Yu J, Feng Y. Amplified lncRNA PVT1 promotes lung cancer proliferation and metastasis by facilitating VEGFC expression. Biochem Cell Biol. 2020;98(6):676–682. doi: 10.1139/bcb-2019-0435. [DOI] [PubMed] [Google Scholar]
- 63.Qi G, Li L. Long non-coding RNA PVT1 contributes to cell growth and metastasis in non-small-cell lung cancer by regulating miR-361-3p/SOX9 axis and activating Wnt/beta-catenin signaling pathway. Biomed Pharmacother. 2020;126:110100. doi: 10.1016/j.biopha.2020.110100. [DOI] [PubMed] [Google Scholar]
- 64.Su XH, Zhu YR, Hou YJ, Li K, Dong NH. PVT1 induces NSCLC cell migration and invasion by regulating IL-6 via sponging miR-760. Mol Cell Probes. 2020;54:101652. doi: 10.1016/j.mcp.2020.101652. [DOI] [PubMed] [Google Scholar]
- 65.Wang Z, Zhang Q, Sun Y, Shao F. Long non-coding RNA PVT1 regulates BAMBI to promote tumor progression in non-small cell lung cancer by sponging miR-17-5p. Onco Targets Ther. 2020;13:131–142. doi: 10.2147/OTT.S217335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xi Y, Shen W, Jin C, Wang L, Yu B. PVT1 promotes the proliferation and migration of non-small cell lung cancer via regulating miR-148/RAB34 signal axis. Onco Targets Ther. 2020;13:1819–1832. doi: 10.2147/OTT.S222898. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 67.Wang X, Cheng Z, Dai L, Jiang T, Li P, Jia L, et al. LncRNA PVT1 facilitates proliferation, migration and invasion of NSCLC cells via miR-551b/FGFR1 axis. Onco Targets Ther. 2021;14:3555–3565. doi: 10.2147/OTT.S273794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xia H, Zhang Z, Yuan J, Niu Q. The lncRNA PVT1 promotes invasive growth of lung adenocarcinoma cells by targeting miR-378c to regulate SLC2A1 expression. Hum Cell. 2021;34(1):201–210. doi: 10.1007/s13577-020-00434-7. [DOI] [PubMed] [Google Scholar]
- 69.Wu D, Li Y, Zhang H, Hu X. Knockdown of lncRNA PVT1 enhances radiosensitivity in non-small cell lung cancer by sponging Mir-195. Cell Physiol Biochem. 2017;42(6):2453–2466. doi: 10.1159/000480209. [DOI] [PubMed] [Google Scholar]
- 70.Wang D, Hu Y. Long non-coding RNA PVT1 competitively binds microRNA-424-5p to regulate CARM1 in radiosensitivity of non-small-cell lung cancer. Mol Ther Nucleic Acids. 2019;16:130–140. doi: 10.1016/j.omtn.2018.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 71.Wu J, Ma C, Tang X, Shi Y, Liu Z, Chai X, et al. The regulation and interaction of PVT1 and miR181a-5p contributes to the repression of SP1 expression by the combination of XJD decoction and cisplatin in human lung cancer cells. Biomed Pharmacother. 2020;121:109632. doi: 10.1016/j.biopha.2019.109632. [DOI] [PubMed] [Google Scholar]
- 72.Chen L, Han X, Hu Z, Chen L. The PVT1/miR-216b/Beclin-1 regulates cisplatin sensitivity of NSCLC cells via modulating autophagy and apoptosis. Cancer Chemother Pharmacol. 2019;83(5):921–931. doi: 10.1007/s00280-019-03808-3. [DOI] [PubMed] [Google Scholar]
- 73.Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR. Head and neck squamous cell carcinoma. Nat Rev Dis Primers. 2020;6(1):92. doi: 10.1038/s41572-020-00224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang Q, Zhang W. LncRNA PVT1 participates in the development of oral squamous cell carcinomas through accelerating EMT and serves as a diagnostic biomarker. Panminerva Med. 2019;8:67. doi: 10.23736/S0031-0808.19.03703-0. [DOI] [PubMed] [Google Scholar]
- 75.Wang F, Ji X, Wang J, Ma X, Yang Y, Zuo J, et al. LncRNA PVT1 enhances proliferation and cisplatin resistance via regulating miR-194-5p/HIF1a axis in oral squamous cell carcinoma. Onco Targets Ther. 2020;13:243–252. doi: 10.2147/OTT.S232405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13(6):1010–1021. doi: 10.1007/s12328-020-01237-x. [DOI] [PubMed] [Google Scholar]
- 77.Zheng X, Hu H, Li S. High expression of lncRNA PVT1 promotes invasion by inducing epithelial-to-mesenchymal transition in esophageal cancer. Oncol Lett. 2016;12(4):2357–2362. doi: 10.3892/ol.2016.5026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Li P-D, Hu J-L, Ma C, Ma H, Yao J, Chen L-L, et al. Upregulation of the long non-coding RNA PVT1 promotes esophageal squamous cell carcinoma progression by acting as a molecular sponge of miR-203 and LASP1. Oncotarget. 2017;8(21):34164–34176. doi: 10.18632/oncotarget.15878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shen S-N, Li K, Liu Y, Yang C-L, He C-Y, Wang H-R. Down-regulation of long noncoding RNA PVT1 inhibits esophageal carcinoma cell migration and invasion and promotes cell apoptosis via microRNA-145-mediated inhibition of FSCN1. Mol Oncol. 2019;13(12):2554–2573. doi: 10.1002/1878-0261.12555. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 80.Xu Y, Li Y, Jin J, Han G, Sun C, Pizzi MP, et al. LncRNA PVT1 up-regulation is a poor prognosticator and serves as a therapeutic target in esophageal adenocarcinoma. Mol Cancer. 2019;18(1):141. doi: 10.1186/s12943-019-1064-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li Y, Song S, Pizzi MP, Han G, Scott AW, Jin J, et al. LncRNA PVT1 Is a Poor Prognosticator and Can Be Targeted by PVT1 Antisense Oligos in Gastric Adenocarcinoma. Cancers (Basel). 2020;12:10. doi: 10.3390/cancers12102995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ren X, Cao D, Yang L, Li X, Zhang W, Xiao Y, et al. High Expression of long non-coding RNA PVT1 predicts metastasis in Han and Uygur patients with gastric cancer in Xinjiang, China. Sci Rep. 2019;9(1):548. doi: 10.1038/s41598-018-36985-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yuan CL, Li H, Zhu L, Liu Z, Zhou J, Shu Y. Aberrant expression of long noncoding RNA PVT1 and its diagnostic and prognostic significance in patients with gastric cancer. Neoplasma. 2016;63(3):442–449. doi: 10.4149/314_150825N45. [DOI] [PubMed] [Google Scholar]
- 84.Xu MD, Wang Y, Weng W, Wei P, Qi P, Zhang Q, et al. A positive feedback loop of lncRNA-PVT1 and FOXM1 facilitates gastric cancer growth and invasion. Clin Cancer Res. 2017;23(8):2071–2080. doi: 10.1158/1078-0432.CCR-16-0742. [DOI] [PubMed] [Google Scholar]
- 85.Huang T, Liu HW, Chen JQ, Wang SH, Hao LQ, Liu M, et al. The long noncoding RNA PVT1 functions as a competing endogenous RNA by sponging miR-186 in gastric cancer. Biomed Pharmacother. 2017;88:302–308. doi: 10.1016/j.biopha.2017.01.049. [DOI] [PubMed] [Google Scholar]
- 86.Li T, Meng XL, Yang WQ. Long noncoding RNA PVT1 acts as a "sponge" to inhibit microRNA-152 in gastric cancer cells. Dig Dis Sci. 2017;62(11):3021–3028. doi: 10.1007/s10620-017-4508-z. [DOI] [PubMed] [Google Scholar]
- 87.Wang L, Xiao B, Yu T, Gong L, Wang Y, Zhang X, et al. lncRNA PVT1 promotes the migration of gastric cancer by functioning as ceRNA of miR-30a and regulating Snail. J Cell Physiol. 2021;236(1):536–548. doi: 10.1002/jcp.29881. [DOI] [PubMed] [Google Scholar]
- 88.Zhang XW, Bu P, Liu L, Zhang XZ, Li J. Overexpression of long non-coding RNA PVT1 in gastric cancer cells promotes the development of multidrug resistance. Biochem Biophys Res Commun. 2015;462(3):227–232. doi: 10.1016/j.bbrc.2015.04.121. [DOI] [PubMed] [Google Scholar]
- 89.Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7(1):6. doi: 10.1038/s41572-020-00240-3. [DOI] [PubMed] [Google Scholar]
- 90.Yu J, Han J, Zhang J, Li G, Liu H, Cui X, et al. The long noncoding RNAs PVT1 and uc002mbe2 in sera provide a new supplementary method for hepatocellular carcinoma diagnosis. Medicine (Baltimore) 2016;95(31):e4436. doi: 10.1097/MD.0000000000004436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhao K, Zhao Y, Zhu J-Y, Dong H, Cong W-M, Yu Y, et al. A panel of genes identified as targets for 8q2413–243 gain contributing to unfavorable overall survival in patients with hepatocellular carcinoma. Curr Med Sci. 2018;38(4):590–596. doi: 10.1007/s11596-018-1918-x. [DOI] [PubMed] [Google Scholar]
- 92.Wang F, Yuan JH, Wang SB, Yang F, Yuan SX, Ye C, et al. Oncofetal long noncoding RNA PVT1 promotes proliferation and stem cell-like property of hepatocellular carcinoma cells by stabilizing NOP2. Hepatology. 2014;60(4):1278–1290. doi: 10.1002/hep.27239. [DOI] [PubMed] [Google Scholar]
- 93.Yan H, Yang Y, Zhang L, Tang G, Wang Y, Xue G, et al. Characterization of the genotype and integration patterns of hepatitis B virus in early- and late-onset hepatocellular carcinoma. Hepatology (Baltimore, MD) 2015;61(6):1821–1831. doi: 10.1002/hep.27722. [DOI] [PubMed] [Google Scholar]
- 94.Jiang B, Yang B, Wang Q, Zheng X, Guo Y, Lu W. lncRNA PVT1 promotes hepatitis B virus-positive liver cancer progression by disturbing histone methylation on the c-Myc promoter. Oncol Rep. 2020;43(2):718–726. doi: 10.3892/or.2019.7444. [DOI] [PubMed] [Google Scholar]
- 95.Guo J, Hao C, Wang C, Li L. Long noncoding RNA PVT1 modulates hepatocellular carcinoma cell proliferation and apoptosis by recruiting EZH2. Cancer Cell Int. 2018;18:98. doi: 10.1186/s12935-018-0582-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhang Y, Dang YW, Wang X, Yang X, Zhang R, Lv ZL, et al. Comprehensive analysis of long non-coding RNA PVT1 gene interaction regulatory network in hepatocellular carcinoma using gene microarray and bioinformatics. Am J Transl Res. 2017;9(9):3904–3917. [PMC free article] [PubMed] [Google Scholar]
- 97.Liu H, Yin Y, Liu T, Gao Y, Ye Q, Yan J, et al. Long non-coding RNA PVT1 regulates the migration of hepatocellular carcinoma HepG2 cells via miR-3619-5p/MKL1 axis. Bosn J Basic Med Sci. 2021;21(2):187–197. doi: 10.17305/bjbms.2020.4641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lan T, Yan X, Li Z, Xu X, Mao Q, Ma W, et al. Long non-coding RNA PVT1 serves as a competing endogenous RNA for miR-186-5p to promote the tumorigenesis and metastasis of hepatocellular carcinoma. Tumour Biol. 2017;39(6):1010428317705338. doi: 10.1177/1010428317705338. [DOI] [PubMed] [Google Scholar]
- 99.Xu Y, Luo X, He W, Chen G, Li Y, Li W, et al. Long non-coding RNA PVT1/miR-150/HIG2 axis regulates the proliferation, invasion and the balance of iron metabolism of hepatocellular carcinoma. Cell Physiol Biochem. 2018;49(4):1403–1419. doi: 10.1159/000493445. [DOI] [PubMed] [Google Scholar]
- 100.Zhang Y, Wen DY, Zhang R, Huang JC, Lin P, Ren FH, et al. A preliminary investigation of PVT1 on the effect and mechanisms of hepatocellular carcinoma: evidence from clinical data, a meta-analysis of 840 cases, and in vivo validation. Cell Physiol Biochem. 2018;47(6):2216–2232. doi: 10.1159/000491534. [DOI] [PubMed] [Google Scholar]
- 101.Yang L, Peng X, Jin H, Liu J. Long non-coding RNA PVT1 promotes autophagy as ceRNA to target ATG3 by sponging microRNA-365 in hepatocellular carcinoma. Gene. 2019;697:94–102. doi: 10.1016/j.gene.2019.02.036. [DOI] [PubMed] [Google Scholar]
- 102.Ding H, Liu J, Liu B, Zeng Y, Chen P, Su Y. Long noncoding RNA PVT1 inhibits interferon-alpha mediated therapy for hepatocellular carcinoma cells by interacting with signal transducer and activator of transcription 1. Biochem Biophys Res Commun. 2018;500(4):973–980. doi: 10.1016/j.bbrc.2018.04.219. [DOI] [PubMed] [Google Scholar]
- 103.Baiu I, Visser B. Gallbladder cancer. JAMA. 2018;320(12):1294. doi: 10.1001/jama.2018.11815. [DOI] [PubMed] [Google Scholar]
- 104.Brindley PJ, Bachini M, Ilyas SI, Khan SA, Loukas A, Sirica AE, et al. Cholangiocarcinoma. Nat Rev Dis Primers. 2021;7(1):65. doi: 10.1038/s41572-021-00300-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chen J, Yu Y, Li H, Hu Q, Chen X, He Y, et al. Long non-coding RNA PVT1 promotes tumor progression by regulating the miR-143/HK2 axis in gallbladder cancer. Mol Cancer. 2019;18(1):33. doi: 10.1186/s12943-019-0947-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Liu K, Xu Q. LncRNA PVT1 regulates gallbladder cancer progression through miR-30d-5p. J Biol Regul Homeost Agents. 2020;34(3):875–883. doi: 10.23812/20-180-A-32. [DOI] [PubMed] [Google Scholar]
- 107.Ilic M, Ilic I. Epidemiology of pancreatic cancer. World J Gastroenterol. 2016;22(44):9694–9705. doi: 10.3748/wjg.v22.i44.9694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhang X, Feng W, Zhang J, Ge L, Zhang Y, Jiang X, et al. Long non-coding RNA PVT1 promotes epithelial–mesenchymal transition via the TGF-β/Smad pathway in pancreatic cancer cells. Oncol Rep. 2018;40(2):1093–1102. doi: 10.3892/or.2018.6462. [DOI] [PubMed] [Google Scholar]
- 109.Wu B-Q, Jiang Y, Zhu F, Sun D-L, He X-Z. Long noncoding RNA PVT1 promotes EMT and cell proliferation and migration through downregulating p21 in pancreatic cancer cells. Technol Cancer Res Treat. 2017;16(6):819–827. doi: 10.1177/1533034617700559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhao L, Kong H, Sun H, Chen Z, Chen B, Zhou M. LncRNA-PVT1 promotes pancreatic cancer cells proliferation and migration through acting as a molecular sponge to regulate miR-448. J Cell Physiol. 2018;233(5):4044–4055. doi: 10.1002/jcp.26072. [DOI] [PubMed] [Google Scholar]
- 111.Sun J, Zhang P, Yin T, Zhang F, Wang W. Upregulation of lncRNA PVT1 facilitates pancreatic ductal adenocarcinoma cell progression and glycolysis by regulating MiR-519d-3p and HIF-1A. J Cancer. 2020;11(9):2572–2579. doi: 10.7150/jca.37959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhu Y, Wu F, Gui W, Zhang N, Matro E, Zhu L, et al. A positive feedback regulatory loop involving the lncRNA PVT1 and HIF-1α in pancreatic cancer. J Mol Cell Biol. 2021;78:4658. doi: 10.1093/jmcb/mjab042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Huang F, Chen W, Peng J, Li Y, Zhuang Y, Zhu Z, et al. LncRNA PVT1 triggers cyto-protective autophagy and promotes pancreatic ductal adenocarcinoma development via the miR-20a-5p/ULK1 axis. Mol Cancer. 2018;17(1):98. doi: 10.1186/s12943-018-0845-6. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 114.Wang C-J, Shi S-B, Tian J, Xu J, Niu Z-X. lncRNA MALAT1, HOTTIP and PVT1 as predictors for predicting the efficacy of GEM based chemotherapy in first-line treatment of pancreatic cancer patients. Oncotarget. 2017;8(56):95108–95115. doi: 10.18632/oncotarget.19345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sun Y, Ren D, Zhou Y, Shen J, Wu H, Jin X. Histone acetyltransferase 1 promotes gemcitabine resistance by regulating the PVT1/EZH2 complex in pancreatic cancer. Cell Death Dis. 2021;12(10):878. doi: 10.1038/s41419-021-04118-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.You L, Wang H, Yang G, Zhao F, Zhang J, Liu Z, et al. Gemcitabine exhibits a suppressive effect on pancreatic cancer cell growth by regulating processing of PVT1 to miR1207. Mol Oncol. 2018;12(12):2147–2164. doi: 10.1002/1878-0261.12393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Shi Y, Wang Y, Qian J, Yan X, Han Y, Yao N, et al. MGMT expression affects the gemcitabine resistance of pancreatic cancer cells. Life Sci. 2020;259:118148. doi: 10.1016/j.lfs.2020.118148. [DOI] [PubMed] [Google Scholar]
- 118.Zhou C, Yi C, Yi Y, Qin W, Yan Y, Dong X, et al. LncRNA PVT1 promotes gemcitabine resistance of pancreatic cancer via activating Wnt/β-catenin and autophagy pathway through modulating the miR-619-5p/Pygo2 and miR-619-5p/ATG14 axes. Mol Cancer. 2020;19(1):118. doi: 10.1186/s12943-020-01237-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Liu Y-F, Luo D, Li X, Li Z-Q, Yu X, Zhu H-W. PVT1 knockdown inhibits autophagy and improves gemcitabine sensitivity by regulating the MiR-143/HIF-1α/VMP1 axis in pancreatic cancer. Pancreas. 2021;50(2):227–234. doi: 10.1097/MPA.0000000000001747. [DOI] [PubMed] [Google Scholar]
- 120.Rahib L, Wehner MR, Matrisian LM, Nead KT. Estimated projection of US cancer incidence and death to 2040. JAMA Netw Open. 2021;4(4):e214708. doi: 10.1001/jamanetworkopen.2021.4708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chang SH, Patel N, Du M, Liang PS. Trends in early-onset vs late-onset colorectal cancer incidence by race/ethnicity in the United States Cancer Statistics Database. Clin Gastroenterol Hepatol. 2021;89:3572. doi: 10.1016/j.cgh.2021.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Pan X, Cheng R, Zhu X, Cai F, Zheng G, Li J, et al. Prognostic significance and diagnostic value of overexpressed lncRNA PVT1 in colorectal cancer. Clin Lab. 2019;65:12. doi: 10.7754/Clin.Lab.2019.190412. [DOI] [PubMed] [Google Scholar]
- 123.Liu H, Ye D, Chen A, Tan D, Zhang W, Jiang W, et al. A pilot study of new promising non-coding RNA diagnostic biomarkers for early-stage colorectal cancers. Clin Chem Lab Med. 2019;57(7):1073–1083. doi: 10.1515/cclm-2019-0052. [DOI] [PubMed] [Google Scholar]
- 124.Guo K, Yao J, Yu Q, Li Z, Huang H, Cheng J, et al. The expression pattern of long non-coding RNA PVT1 in tumor tissues and in extracellular vesicles of colorectal cancer correlates with cancer progression. Tumour Biol. 2017;39(4):1010428317699122. doi: 10.1177/1010428317699122. [DOI] [PubMed] [Google Scholar]
- 125.Lai S-W, Chen M-Y, Bamodu OA, Hsieh M-S, Huang T-Y, Yeh C-T, et al. Exosomal lncRNA PVT1/VEGFA axis promotes colon cancer metastasis and stemness by downregulation of tumor suppressor miR-152-3p. Oxid Med Cell Longev. 2021;2021:9959807. doi: 10.1155/2021/9959807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Zeng X, Liu Y, Zhu H, Chen D, Hu W. Downregulation of miR-216a-5p by long noncoding RNA PVT1 suppresses colorectal cancer progression via modulation of YBX1 expression. Cancer Manag Res. 2019;11:6981–6993. doi: 10.2147/CMAR.S208983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wu H, Wei M, Jiang X, Tan J, Xu W, Fan X, et al. lncRNA PVT1 promotes tumorigenesis of colorectal cancer by stabilizing miR-16-5p and interacting with the VEGFA/VEGFR1/AKT axis. Mol Ther Nucleic Acids. 2020;20:438–450. doi: 10.1016/j.omtn.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Radwan AF, Shaker OG, El-Boghdady NA, Senousy MA. Association of MALAT1 and PVT1 variants, expression profiles and target miRNA-101 and miRNA-186 with colorectal cancer: correlation with epithelial–mesenchymal transition. Int J Mol Sci. 2021;22:11. doi: 10.3390/ijms22116147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chai J, Guo D, Ma W, Han D, Dong W, Guo H, et al. A feedback loop consisting of RUNX2/lncRNA-PVT1/miR-455 is involved in the progression of colorectal cancer. Am J Cancer Res. 2018;8(3):538–550. [PMC free article] [PubMed] [Google Scholar]
- 130.Yu X, Zhao J, He Y. Long non-coding RNA PVT1 functions as an oncogene in human colon cancer through miR-30d-5p/RUNX2 axis. J BUON. 2018;23(1):48–54. [PubMed] [Google Scholar]
- 131.Shang A-Q, Wang W-W, Yang Y-B, Gu C-Z, Ji P, Chen C, et al. Knockdown of long noncoding RNA PVT1 suppresses cell proliferation and invasion of colorectal cancer via upregulation of microRNA-214-3p. Am J Physiol Gastrointest Liver Physiol. 2019;317(2):G222–G232. doi: 10.1152/ajpgi.00357.2018. [DOI] [PubMed] [Google Scholar]
- 132.Zhang W, Xiao J, Lu X, Liu T, Jin X, Xiao Y, et al. PVT1 (rs13281615) and miR-146a (rs2910164) polymorphisms affect the prognosis of colon cancer by regulating COX2 expression and cell apoptosis. J Cell Physiol. 2019;234(10):17538–17548. doi: 10.1002/jcp.28377. [DOI] [PubMed] [Google Scholar]
- 133.Liu F, Wu R, Guan L, Tang X. Knockdown of PVT1 suppresses colorectal cancer progression by regulating MiR-106b-5p/FJX1 axis. Cancer Manag Res. 2020;12:8773–8785. doi: 10.2147/CMAR.S260537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Liu Y, Wu Y, Zhu Z, Gong J, Dou W. Knockdown of lncRNA PVT1 inhibits the proliferation and accelerates the apoptosis of colorectal cancer cells via the miR‑761/MAPK1 axis. Mol Med Rep. 2021;24:5 [DOI] [PubMed]
- 135.Fan H, Zhu J-H, Yao X-Q. Knockdown of long non-coding RNA PVT1 reverses multidrug resistance in colorectal cancer cells. Mol Med Rep. 2018;17(6):8309–8315. doi: 10.3892/mmr.2018.8907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ping G, Xiong W, Zhang L, Li Y, Zhang Y, Zhao Y. Silencing long noncoding RNA PVT1 inhibits tumorigenesis and cisplatin resistance of colorectal cancer. Am Transl Res. 2018;10(1):138–149. [PMC free article] [PubMed] [Google Scholar]
- 137.Zhang Z, Zhu Z, Zhang B, Li W, Li X, Wu X, et al. Frequent mutation of rs13281615 and its association with PVT1 expression and cell proliferation in breast cancer. J Genetics Genom. 2014;41(4):187–195. doi: 10.1016/j.jgg.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 138.Tang J, Li Y, Sang Y, Yu B, Lv D, Zhang W, et al. LncRNA PVT1 regulates triple-negative breast cancer through KLF5/beta-catenin signaling. Oncogene. 2018;37(34):4723–4734. doi: 10.1038/s41388-018-0310-4. [DOI] [PubMed] [Google Scholar]
- 139.Sarver AL, Murray CD, Temiz NA, Tseng Y-Y, Bagchi A. MYC and PVT1 synergize to regulate RSPO1 levels in breast cancer. Cell Cycle (Georgetown, Tex) 2016;15(7):881–885. doi: 10.1080/15384101.2016.1149660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Li X, Chen W, Wang H, Wei Q, Ding X, Li W. Amplification and the clinical significance of circulating cell-free DNA of PVT1 in breast cancer. Oncol Rep. 2017;38(1):465–471. doi: 10.3892/or.2017.5650. [DOI] [PubMed] [Google Scholar]
- 141.Wang L, Wang R, Ye Z, Wang Y, Li X, Chen W, et al. PVT1 affects EMT and cell proliferation and migration via regulating p21 in triple-negative breast cancer cells cultured with mature adipogenic medium. Acta Biochim Biophys Sin. 2018;50(12):1211–1218. doi: 10.1093/abbs/gmy129. [DOI] [PubMed] [Google Scholar]
- 142.Wang Y, Zhou J, Wang Z, Wang P, Li S. Upregulation of SOX2 activated lncRNA PVT1 expression promotes breast cancer cell growth and invasion. Biochem Biophys Res Commun. 2017;493(1):429–436. doi: 10.1016/j.bbrc.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 143.Zhu M, Lv Q, Huang H, Sun C, Pang D, Wu J. Identification of a four-long non-coding RNA signature in predicting breast cancer survival. Oncol Lett. 2020;19(1):221–228. doi: 10.3892/ol.2019.11063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.El-Fattah AAA, Sadik NAH, Shaker OG, Mohamed Kamal A, Shahin NN. Serum long non-coding RNAs PVT1, HOTAIR, and NEAT1 as potential biomarkers in Egyptian women with breast cancer. Biomolecules. 2021;11:2. doi: 10.3390/biom11020301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Levine F, Ogunwobi OO. Targeting PVT1 exon 9 re-expresses claudin 4 protein and inhibits migration by claudin-low triple negative breast cancer cells. Cancers. 2021;13:5. doi: 10.3390/cancers13051046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Yan C, Chen Y, Kong W, Fu L, Liu Y, Yao Q, et al. PVT1-derived miR-1207-5p promotes breast cancer cell growth by targeting STAT6. Cancer Sci. 2017;108(5):868–876. doi: 10.1111/cas.13212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Liu X, Bi L, Wang Q, Wen M, Li C, Ren Y, et al. miR-1204 targets VDR to promotes epithelial-mesenchymal transition and metastasis in breast cancer. Oncogene. 2018;37(25):3426–3439. doi: 10.1038/s41388-018-0215-2. [DOI] [PubMed] [Google Scholar]
- 148.Wang H, Huang Y, Yang Y. LncRNA PVT1 regulates TRPS1 expression in breast cancer by sponging miR-543. Cancer Manag Res. 2020;12:7993–8004. doi: 10.2147/CMAR.S263383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Luo Y, Zhang W, Xu L, Chen Y, Xu Y, Yuan L. Long non-coding RNA PVT1 regulates the resistance of the breast cancer cell line MDA-MB-231 to doxorubicin via Nrf2. Technol Cancer Res Treat. 2020;19:1533033820980763. doi: 10.1177/1533033820980763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lheureux S, Gourley C, Vergote I, Oza AM. Epithelial ovarian cancer. Lancet (London, England) 2019;393(10177):1240–1253. doi: 10.1016/S0140-6736(18)32552-2. [DOI] [PubMed] [Google Scholar]
- 151.Yang Q, Yu Y, Sun Z, Pan Y. Long non-coding RNA PVT1 promotes cell proliferation and invasion through regulating miR-133a in ovarian cancer. Biomed Pharmacother. 2018;106:61–67. doi: 10.1016/j.biopha.2018.06.112. [DOI] [PubMed] [Google Scholar]
- 152.Ding Y, Fang Q, Li Y, Wang Y. Amplification of lncRNA PVT1 promotes ovarian cancer proliferation by binding to miR-140. Mamm Genome. 2019;30(7–8):217–225. doi: 10.1007/s00335-019-09808-1. [DOI] [PubMed] [Google Scholar]
- 153.Chen Y, Du H, Bao L, Liu W. LncRNA PVT1 promotes ovarian cancer progression by silencing miR-214. Cancer Biol Med. 2018;15(3):238–250. doi: 10.20892/j.issn.2095-3941.2017.0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Li T, Yang J, Yang B, Zhao G, Lin H, Liu Q, et al. Ketamine inhibits ovarian cancer cell growth by regulating the lncRNA-PVT1/EZH2/p57 axis. Front Genet. 2020;11:597467. doi: 10.3389/fgene.2020.597467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Qu C, Dai C, Guo Y, Qin R, Liu J. Long non-coding RNA PVT1-mediated miR-543/SERPINI1 axis plays a key role in the regulatory mechanism of ovarian cancer. Bioscience Rep. 2020;40:6. doi: 10.1042/BSR20200800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wu Y, Gu W, Han X, Jin Z. LncRNA PVT1 promotes the progression of ovarian cancer by activating TGF-β pathway via miR-148a-3p/AGO1 axis. J Cell Mol Med. 2021;25(17):8229–8243. doi: 10.1111/jcmm.16700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.El-Khazragy N, Mohammed HF, Yassin M, Elghoneimy KK, Bayoumy W, Hewety A, et al. Tissue-based long non-coding RNAs "PVT1, TUG1 and MEG3" signature predicts cisplatin resistance in ovarian cancer. Genomics. 2020;112(6):4640–4646. doi: 10.1016/j.ygeno.2020.08.005. [DOI] [PubMed] [Google Scholar]
- 158.Yi K, Hou M, Yuan J, Yang L, Zeng X, Xi M, et al. LncRNA PVT1 epigenetically stabilizes and post-transcriptionally regulates FOXM1 by acting as a microRNA sponge and thus promotes malignant behaviors of ovarian cancer cells. Am J Transl Res. 2020;12(6):2860–2874. [PMC free article] [PubMed] [Google Scholar]
- 159.Chen Y, Li F, Li D, Liu W, Zhang L. Atezolizumab and blockade of lncRNA PVT1 attenuate cisplatin resistant ovarian cancer cells progression synergistically via JAK2/STAT3/PD-L1 pathway. Clin Immunol (Orlando, Fla) 2021;227:108728. doi: 10.1016/j.clim.2021.108728. [DOI] [PubMed] [Google Scholar]
- 160.Martini P, Paracchini L, Caratti G, Mello-Grand M, Fruscio R, Beltrame L, et al. lncRNAs as novel indicators of patients' prognosis in stage I epithelial ovarian cancer: a retrospective and multicentric study. Clin Cancer Res. 2017;23(9):2356–2366. doi: 10.1158/1078-0432.CCR-16-1402. [DOI] [PubMed] [Google Scholar]
- 161.Yang JP, Yang XJ, Xiao L, Wang Y. Long noncoding RNA PVT1 as a novel serum biomarker for detection of cervical cancer. Eur Rev Med Pharmacol Sci. 2016;20(19):3980–3986. [PubMed] [Google Scholar]
- 162.Sun W, Wang L, Zhao D, Wang P, Li Y, Wang S. Four circulating long non-coding RNAs act as biomarkers for predicting cervical cancer. Gynecol Obstet Invest. 2018;83(6):533–539. doi: 10.1159/000487595. [DOI] [PubMed] [Google Scholar]
- 163.Shen C-J, Cheng Y-M, Wang C-L. LncRNA PVT1 epigenetically silences miR-195 and modulates EMT and chemoresistance in cervical cancer cells. J Drug Target. 2017;25(7):637–644. doi: 10.1080/1061186X.2017.1307379. [DOI] [PubMed] [Google Scholar]
- 164.Gao Y-L, Zhao Z-S, Zhang M-Y, Han L-J, Dong Y-J, Xu B. Long noncoding RNA PVT1 facilitates cervical cancer progression via negative regulating of miR-424. Oncol Res. 2017;25(8):1391–1398. doi: 10.3727/096504017X14881559833562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wang X, Wang G, Zhang L, Cong J, Hou J, Liu C. LncRNA PVT1 promotes the growth of HPV positive and negative cervical squamous cell carcinoma by inhibiting TGF-beta1. Cancer Cell Int. 2018;18:70. doi: 10.1186/s12935-018-0567-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wang C, Zou H, Yang H, Wang L, Chu H, Jiao J, et al. Long non-coding RNA plasmacytoma variant translocation 1 gene promotes the development of cervical cancer via the NF-κB pathway. Mol Med Rep. 2019;20(3):2433–2440. doi: 10.3892/mmr.2019.10479. [DOI] [PubMed] [Google Scholar]
- 167.Wang C, Zou H, Chen A, Yang H, Yu X, Yu X, et al. C-Myc-activated long non-coding RNA PVT1 enhances the proliferation of cervical cancer cells by sponging miR-486-3p. J Biochem. 2020;167(6):565–575. doi: 10.1093/jb/mvaa005. [DOI] [PubMed] [Google Scholar]
- 168.Liu W, Yao D, Huang B. LncRNA PVT1 promotes cervical cancer progression by sponging miR-503 to upregulate ARL2 expression. Open Life Sci. 2021;16(1):1–13. doi: 10.1515/biol-2021-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Chang Q-Q, Chen C-Y, Chen Z, Chang S. LncRNA PVT1 promotes proliferation and invasion through enhancing Smad3 expression by sponging miR-140-5p in cervical cancer. Radiol Oncol. 2019;53(4):443–452. doi: 10.2478/raon-2019-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E. Endometrial cancer. Lancet (London, England) 2016;387(10023):1094–1108. doi: 10.1016/S0140-6736(15)00130-0. [DOI] [PubMed] [Google Scholar]
- 171.Motzer RJ, Jonasch E, Boyle S, Carlo MI, Manley B, Agarwal N, et al. NCCN Guidelines Insights: Kidney Cancer, Version 12021. J Natl Compr Cancer Netw. 2020;18(9):1160–1170. doi: 10.6004/jnccn.2020.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Gray RE, Harris GT. Renal cell carcinoma: diagnosis and management. Am Fam Physician. 2019;99(3):179–184. [PubMed] [Google Scholar]
- 173.Li W, Zheng Z, Chen H, Cai Y, Xie W. Knockdown of long non-coding RNA PVT1 induces apoptosis and cell cycle arrest in clear cell renal cell carcinoma through the epidermal growth factor receptor pathway. Oncol Lett. 2018;15(5):7855–7863. doi: 10.3892/ol.2018.8315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wu Q, Yang F, Yang Z, Fang Z, Fu W, Chen W, et al. Long noncoding RNA PVT1 inhibits renal cancer cell apoptosis by up-regulating Mcl-1. Oncotarget. 2017;8(60):101865–101875. doi: 10.18632/oncotarget.21706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Zhang M-X, Zhang L-Z, Fu L-M, Yao H-H, Tan L, Feng Z-H, et al. Positive feedback regulation of lncRNA PVT1 and HIF2α contributes to clear cell renal cell carcinoma tumorigenesis and metastasis. Oncogene. 2021;40(37):5639–5650. doi: 10.1038/s41388-021-01971-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wang Y, Li Z, Li W, Zhou L, Jiang Y. Prognostic significance of long non-coding RNAs in clear cell renal cell carcinoma: a meta-analysis. Medicine. 2019;98(40):e17276. doi: 10.1097/MD.0000000000017276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Wu Y, Wang YQ, Weng WW, Zhang QY, Yang XQ, Gan HL, et al. A serum-circulating long noncoding RNA signature can discriminate between patients with clear cell renal cell carcinoma and healthy controls. Oncogenesis. 2016;5:e192. doi: 10.1038/oncsis.2015.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Liu H, Ye T, Yang X, Lv P, Wu X, Zhou H, et al. A panel of four-lncRNA signature as a potential biomarker for predicting survival in clear cell renal cell carcinoma. J Cancer. 2020;11(14):4274–4283. doi: 10.7150/jca.40421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Yang T, Zhou H, Liu P, Yan L, Yao W, Chen K, et al. lncRNA PVT1 and its splicing variant function as competing endogenous RNA to regulate clear cell renal cell carcinoma progression. Oncotarget. 2017;8(49):85353–85367. doi: 10.18632/oncotarget.19743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.LncRNA PVT1 promotes proliferation, invasion and epithelial–mesenchymal transition of renal cell carcinoma cells through downregulation of miR-16–5p [Corrigendum]. OncoTargets Therapy. 2019;12:5649. [DOI] [PMC free article] [PubMed]
- 181.Lenis AT, Lec PM, Chamie K, Mshs MD. Bladder cancer: a review. JAMA. 2020;324(19):1980–1991. doi: 10.1001/jama.2020.17598. [DOI] [PubMed] [Google Scholar]
- 182.Bhat A, Ritch CR. Urinary biomarkers in bladder cancer: where do we stand? Curr Opin Urol. 2019;29(3):203–209. doi: 10.1097/MOU.0000000000000605. [DOI] [PubMed] [Google Scholar]
- 183.Li B, Guo L-H, Ban Z-Q, Liu L, Luo L, Cui T-Y. Upregulation of lncRNA plasmacytoma variant translocation 1 predicts poor prognosis in patients with muscle-invasive bladder cancer. Medicine. 2020;99(28):e21059. doi: 10.1097/MD.0000000000021059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Tian Z, Cao S, Li C, Xu M, Wei H, Yang H, et al. LncRNA PVT1 regulates growth, migration, and invasion of bladder cancer by miR-31/CDK1. J Cell Physiol. 2019;234(4):4799–4811. doi: 10.1002/jcp.27279. [DOI] [PubMed] [Google Scholar]
- 185.Yu C, Longfei L, Long W, Feng Z, Chen J, Chao L, et al. LncRNA PVT1 regulates VEGFC through inhibiting miR-128 in bladder cancer cells. J Cell Physiol. 2019;234(2):1346–1353. doi: 10.1002/jcp.26929. [DOI] [PubMed] [Google Scholar]
- 186.Chen M, Zhang R, Lu L, Du J, Chen C, Ding K, et al. LncRNA PVT1 accelerates malignant phenotypes of bladder cancer cells by modulating miR-194-5p/BCLAF1 axis as a ceRNA. Aging. 2020;12(21):22291–22312. doi: 10.18632/aging.202203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Liu Z, Zhang H. LncRNA plasmacytoma variant translocation 1 is an oncogene in bladder urothelial carcinoma. Oncotarget. 2017;8(38):64273–64282. doi: 10.18632/oncotarget.19604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Pal G, Huaman J, Levine F, Orunmuyi A, Olapade-Olaopa EO, Onagoruwa OT, et al. Long noncoding RNA from PVT1 exon 9 is overexpressed in prostate cancer and induces malignant transformation and castration resistance in prostate epithelial cells. Genes. 2019;10:12. doi: 10.3390/genes10120964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Yang J, Li C, Mudd A, Gu X. LncRNA PVT1 predicts prognosis and regulates tumor growth in prostate cancer. Biosci Biotechnol Biochem. 2017;81(12):2301–2306. doi: 10.1080/09168451.2017.1387048. [DOI] [PubMed] [Google Scholar]
- 190.Chang Z, Cui J, Song Y. Long noncoding RNA PVT1 promotes EMT via mediating microRNA-186 targeting of Twist1 in prostate cancer. Gene. 2018;654:36–42. doi: 10.1016/j.gene.2018.02.036. [DOI] [PubMed] [Google Scholar]
- 191.Wan B, Wu H-Y, Lv D-J, Zhou X-M, Zhong L-R, Lei B, et al. Downregulation of lncRNA PVT1 expression inhibits proliferation and migration by regulating p38 expression in prostate cancer. Oncol Lett. 2018;16(4):5160–5166. doi: 10.3892/ol.2018.9305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Sun F, Wu K, Yao Z, Mu X, Zheng Z, Sun M, et al. Long noncoding RNA PVT1 promotes prostate cancer metastasis by increasing NOP2 expression via targeting tumor suppressor microRNAs. Onco Targets Ther. 2020;13:6755–6765. doi: 10.2147/OTT.S242441. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 193.Wu H, Tian X, Zhu C. Knockdown of lncRNA PVT1 inhibits prostate cancer progression in vitro and in vivo by the suppression of KIF23 through stimulating miR-15a-5p. Cancer Cell Int. 2020;20:283. doi: 10.1186/s12935-020-01363-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Liu H-T, Fang L, Cheng Y-X, Sun Q. LncRNA PVT1 regulates prostate cancer cell growth by inducing the methylation of miR-146a. Cancer Med. 2016;5(12):3512–3519. doi: 10.1002/cam4.900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Atianand MK, Caffrey DR, Fitzgerald KA. Immunobiology of long noncoding RNAs. Annu Rev Immunol. 2017;35:177–198. doi: 10.1146/annurev-immunol-041015-055459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Fu J, Shi H, Wang B, Zhan T, Shao Y, Ye L, et al. LncRNA PVT1 links Myc to glycolytic metabolism upon CD4 T cell activation and Sjögren's syndrome-like autoimmune response. J Autoimmun. 2020;107:102358. doi: 10.1016/j.jaut.2019.102358. [DOI] [PubMed] [Google Scholar]
- 197.Lu J, Wang X, Zhang B, Li P, Du X, Qi F. The lncRNA PVT1 regulates autophagy in regulatory T cells to suppress heart transplant rejection in mice by targeting miR-146a. Cell Immunol. 2021;367:104400. doi: 10.1016/j.cellimm.2021.104400. [DOI] [PubMed] [Google Scholar]
- 198.Luo Y-Y, Yang Z-Q, Lin X-F, Zhao F-L, Tu H-T, Wang L-J, et al. Knockdown of lncRNA PVT1 attenuated macrophage M1 polarization and relieved sepsis induced myocardial injury via miR-29a/HMGB1 axis. Cytokine. 2021;143:155509. doi: 10.1016/j.cyto.2021.155509. [DOI] [PubMed] [Google Scholar]
- 199.Yu L, Zhang L, Jiang Z, Yu B. Decreasing lncRNA PVT1 causes Treg/Th17 imbalance via NOTCH signaling in immune thrombocytopenia. Hematology (Amsterdam, Netherlands) 2021;26(1):734–740. doi: 10.1080/16078454.2021.1974200. [DOI] [PubMed] [Google Scholar]
- 200.Zheng Y, Tian X, Wang T, Xia X, Cao F, Tian J, et al. Long noncoding RNA Pvt1 regulates the immunosuppression activity of granulocytic myeloid-derived suppressor cells in tumor-bearing mice. Mol Cancer. 2019;18(1):61. doi: 10.1186/s12943-019-0978-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ostrom QT, Bauchet L, Davis FG, Deltour I, Fisher JL, Langer CE, et al. The epidemiology of glioma in adults: a "state of the science" review. Neuro Oncol. 2014;16(7):896–913. doi: 10.1093/neuonc/nou087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Xue W, Chen J, Liu X, Gong W, Zheng J, Guo X, et al. PVT1 regulates the malignant behaviors of human glioma cells by targeting miR-190a-5p and miR-488–3p. Biochim Biophys Acta. 2018;1864(5 Pt A):1783–94. [DOI] [PubMed]
- 203.Han Y, Li X, He F, Yan J, Ma C, Zheng X, et al. Knockdown of lncRNA PVT1 inhibits glioma progression by regulating miR-424 expression. Oncol Res. 2019;27(6):681–690. doi: 10.3727/096504018X15424939990246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Zhang Y, Yang G, Luo Y. Long non-coding RNA PVT1 promotes glioma cell proliferation and invasion by targeting miR-200a. Exp Ther Med. 2019;17(2):1337–1345. doi: 10.3892/etm.2018.7083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Lv ZH, Wang ZY, Li ZY. LncRNA PVT1 aggravates the progression of glioma via downregulating UPF1. Eur Rev Med Pharmacol Sci. 2019;23(20):8956–8963. doi: 10.26355/eurrev_201910_19294. [DOI] [PubMed] [Google Scholar]
- 206.Dahai Z, Daliang C, Famu L, Xiang W, Lenian L, Jianmin C, et al. Lowly expressed lncRNA PVT1 suppresses proliferation and advances apoptosis of glioma cells through up-regulating microRNA-128–1–5p and inhibiting PTBP1. Brain research bulletin. 2020;163. [DOI] [PubMed]
- 207.Jin Z, Piao LH, Sun GC, Lv CX, Jing Y, Jin RH. Long non-coding RNA plasmacytoma variant translocation 1 (PVT1) promotes glioblastoma multiforme progression via regulating miR-1301-3p/TMBIM6 axis. Eur Rev Med Pharmacol Sci. 2020;24(22):11658–11665. doi: 10.26355/eurrev_202011_23810. [DOI] [PubMed] [Google Scholar]
- 208.Bi Y, Ji J, Zhou Y. LncRNA-PVT1 indicates a poor prognosis and promotes angiogenesis via activating the HNF1B/EMT axis in glioma. J Cancer. 2021;12(19):5732–5744. doi: 10.7150/jca.60257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Ma Y, Wang P, Xue Y, Qu C, Zheng J, Liu X, et al. PVT1 affects growth of glioma microvascular endothelial cells by negatively regulating miR-186. Tumour Biol. 2017;39(3):1010428317694326. doi: 10.1177/1010428317694326. [DOI] [PubMed] [Google Scholar]
- 210.Gong R, Li Z-Q, Fu K, Ma C, Wang W, Chen J-C. Long noncoding RNA PVT1 promotes stemness and temozolomide resistance through miR-365/ELF4/SOX2 axis in glioma. Exp Neurobiol. 2021;30(3):244–255. doi: 10.5607/en20060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Cabanillas ME, McFadden DG, Durante C. Thyroid cancer. Lancet (London, England) 2016;388(10061):2783–2795. doi: 10.1016/S0140-6736(16)30172-6. [DOI] [PubMed] [Google Scholar]
- 212.Feng K, Liu Y, Xu L-J, Zhao L-F, Jia C-W, Xu M-Y. Long noncoding RNA PVT1 enhances the viability and invasion of papillary thyroid carcinoma cells by functioning as ceRNA of microRNA-30a through mediating expression of insulin like growth factor 1 receptor. Biomed Pharmacother. 2018;104:686–698. doi: 10.1016/j.biopha.2018.05.078. [DOI] [PubMed] [Google Scholar]
- 213.Lin Q-Y, Qi Q-L, Hou S, Chen Z, Zhang L, Zhao H-G, et al. LncRNA PVT1 acts as a tumor promoter in thyroid cancer and promotes tumor progression by mediating miR-423-5p-PAK3. Cancer Manag Res. 2020;12:13403–13413. doi: 10.2147/CMAR.S283443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Possieri C, Locantore P, Salis C, Bacci L, Aiello A, Fadda G, et al. Combined molecular and mathematical analysis of long noncoding RNAs expression in fine needle aspiration biopsies as novel tool for early diagnosis of thyroid cancer. Endocrine. 2021;72(3):711–720. doi: 10.1007/s12020-020-02508-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Eaton BR, Schwarz R, Vatner R, Yeh B, Claude L, Indelicato DJ, et al. Osteosarcoma. Pediatr Blood Cancer. 2021;68(Suppl 2):e28352. doi: 10.1002/pbc.28352. [DOI] [PubMed] [Google Scholar]
- 216.Gill J, Gorlick R. Advancing therapy for osteosarcoma. Nat Rev Clin Oncol. 2021;18(10):609–624. doi: 10.1038/s41571-021-00519-8. [DOI] [PubMed] [Google Scholar]
- 217.Song J, Wu X, Liu F, Li M, Sun Y, Wang Y, et al. Long non-coding RNA PVT1 promotes glycolysis and tumor progression by regulating miR-497/HK2 axis in osteosarcoma. Biochem Biophys Res Commun. 2017;490(2):217–224. doi: 10.1016/j.bbrc.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 218.Zhao W, Qin P, Zhang D, Cui X, Gao J, Yu Z, et al. Long non-coding RNA PVT1 encapsulated in bone marrow mesenchymal stem cell-derived exosomes promotes osteosarcoma growth and metastasis by stabilizing ERG and sponging miR-183-5p. Aging. 2019;11(21):9581–9596. doi: 10.18632/aging.102406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Yan M, Pan XF, Liu Y, Zhao S, Gong WQ, Liu W. Long noncoding RNA PVT1 promotes metastasis via miR-484 sponging in osteosarcoma cells. Eur Rev Med Pharmacol Sci. 2020;24(5):2229–2238. doi: 10.26355/eurrev_202003_20488. [DOI] [PubMed] [Google Scholar]
- 220.Xun C, Jiang D, Tian Z, Yunus A, Chen J. Long noncoding RNA plasmacytoma variant translocation gene 1 promotes epithelial-mesenchymal transition in osteosarcoma. J Clin Lab Anal. 2021;35(1):e23587. doi: 10.1002/jcla.23587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Chen S, Zhou L, Wang Y. ALKBH5-mediated mA demethylation of lncRNA PVT1 plays an oncogenic role in osteosarcoma. Cancer Cell Int. 2020;20:34. doi: 10.1186/s12935-020-1105-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Sun Z-Y, Jian Y-K, Zhu H-Y, Li B. lncRNAPVT1 targets miR-152 to enhance chemoresistance of osteosarcoma to gemcitabine through activating c-MET/PI3K/AKT pathway. Pathol Res Pract. 2019;215(3):555–563. doi: 10.1016/j.prp.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 223.Marinac CR, Ghobrial IM, Birmann BM, Soiffer J, Rebbeck TR. Dissecting racial disparities in multiple myeloma. Blood Cancer J. 2020;10(2):19. doi: 10.1038/s41408-020-0284-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Handa H, Honma K, Oda T, Kobayashi N, Kuroda Y, Kimura-Masuda K, et al. Long noncoding RNA is regulated by bromodomain protein BRD4 in multiple myeloma and is associated with disease progression. Int J Mol Sci. 2020;21:19. doi: 10.3390/ijms21197121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Li S, Young KH, Medeiros LJ. Diffuse large B-cell lymphoma. Pathology. 2018;50(1):74–87. doi: 10.1016/j.pathol.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 226.Bispo JAB, Pinheiro PS, Kobetz EK. Epidemiology and etiology of leukemia and lymphoma. Cold Spring Harb Perspect Med. 2020;10(6). [DOI] [PMC free article] [PubMed]
- 227.Izadifard M, Pashaiefar H, Yaghmaie M, Montazeri M, Sadraie M, Momeny M, et al. Expression analysis of PVT1, CCDC26, and CCAT1 long noncoding RNAs in acute myeloid leukemia patients. Genet Test Mol Biomarkers. 2018;22(10):593–598. doi: 10.1089/gtmb.2018.0143. [DOI] [PubMed] [Google Scholar]
- 228.El-Khazragy N, Elayat W, Matbouly S, Seliman S, Sami A, Safwat G, et al. The prognostic significance of the long non-coding RNAs "CCAT1, PVT1" in t(8;21) associated acute myeloid leukemia. Gene. 2019;707:172–177. doi: 10.1016/j.gene.2019.03.055. [DOI] [PubMed] [Google Scholar]
- 229.Salehi M, Sharifi M, Bagheri M. Knockdown of long noncoding RNA plasmacytoma variant translocation 1 with antisense locked nucleic acid gapmers exerts tumor-suppressive functions in human acute erythroleukemia cells through downregulation of expression. Cancer Biother Radiopharm. 2019;34(6):371–379. doi: 10.1089/cbr.2018.2510. [DOI] [PubMed] [Google Scholar]
- 230.Ghadiri A, Sharifi M, Mehrzad V, Bagheri P. Reduce proliferation of human bone marrow cells from acute myeloblastic leukemia with minimally differentiation by blocking lncRNA PVT1. Clin Translat Oncol. 2020;22(11):2103–2110. doi: 10.1007/s12094-020-02360-4. [DOI] [PubMed] [Google Scholar]
- 231.Cheng J, Song Y, Xu J, Li H-H, Zheng J-F. LncRNA PVT1 promotes the malignant progression of acute myeloid leukaemia via sponging miR-29 family to increase WAVE1 expression. Pathology. 2021;53(5):613–622. doi: 10.1016/j.pathol.2020.11.003. [DOI] [PubMed] [Google Scholar]
- 232.Yazdi N, Houshmand M, Atashi A, Kazemi A, Najmedini AA, Zarif MN. Long noncoding RNA PVT1: potential oncogene in the development of acute lymphoblastic leukemia. Turk J Biol. 2018;42(5):405–413. doi: 10.3906/biy-1801-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Palcau AC, Canu V, Donzelli S, Strano S, Pulito C, Blandino G. CircPVT1: a pivotal circular node intersecting long non-coding-PVT1 and c-MYC oncogenic signals. Mol Cancer. 2022;21(1):33. doi: 10.1186/s12943-022-01514-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Qin S, Zhao Y, Lim G, Lin H, Zhang X, Zhang X. Circular RNA PVT1 acts as a competing endogenous RNA for miR-497 in promoting non-small cell lung cancer progression. Biomed Pharmacother. 2019;111:244–250. doi: 10.1016/j.biopha.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 235.Zheng F, Xu R. CircPVT1 contributes to chemotherapy resistance of lung adenocarcinoma through miR-145–5p/ABCC1 axis. Biomed Pharmacother. 2020;124:109828. doi: 10.1016/j.biopha.2020.109828. [DOI] [PubMed] [Google Scholar]
- 236.Cao L, Zhou X, Ding X, Gao D. Knockdown of circ-PVT1 inhibits the progression of lung adenocarcinoma and enhances the sensitivity to cisplatin via the miR-429/FOXK1 signaling axis. Mol Med Rep. 2021;24:4. doi: 10.3892/mmr.2021.12323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Shi J, Lv X, Zeng L, Li W, Zhong Y, Yuan J, et al. CircPVT1 promotes proliferation of lung squamous cell carcinoma by binding to miR-30d/e. J Exp Clin Cancer Res. 2021;40(1):193. doi: 10.1186/s13046-021-01976-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.He T, Li X, Xie D, Tian L. Overexpressed circPVT1 in oral squamous cell carcinoma promotes proliferation by serving as a miRNA sponge. Mol Med Rep. 2019;20(4):3509–3518. doi: 10.3892/mmr.2019.10615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Wang S, Li W, Yang L, Yuan J, Wang L, Li N, et al. CircPVT1 facilitates the progression of oral squamous cell carcinoma by regulating miR-143–3p/SLC7A11 axis through MAPK signaling pathway. Funct Integr Genomics. 2022;78:9. doi: 10.1007/s10142-022-00865-5. [DOI] [PubMed] [Google Scholar]
- 240.Zhong R, Chen Z, Mo T, Li Z, Zhang P. Potential role of circPVT1 as a proliferative factor and treatment target in esophageal carcinoma. Cancer Cell Int. 2019;19:267. doi: 10.1186/s12935-019-0985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Yao W, Wang J, Meng F, Zhu Z, Jia X, Xu L, et al. Circular RNA CircPVT1 Inhibits 5-fluorouracil chemosensitivity by regulating ferroptosis through MiR-30a-5p/FZD3 axis in esophageal cancer cells. Front Oncol. 2021;11:780938. doi: 10.3389/fonc.2021.780938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Chen J, Li Y, Zheng Q, Bao C, He J, Chen B, et al. Circular RNA profile identifies circPVT1 as a proliferative factor and prognostic marker in gastric cancer. Cancer Lett. 2017;388:208–219. doi: 10.1016/j.canlet.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 243.Liu Y-Y, Zhang L-Y, Du W-Z. Circular RNA circ-PVT1 contributes to paclitaxel resistance of gastric cancer cells through the regulation of ZEB1 expression by sponging miR-124–3p. Biosci Rep. 2019;39:12. doi: 10.1042/BSR20193045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Wang X, Zhang Y, Li W, Liu X. Knockdown of cir_RNA PVT1 elevates gastric cancer cisplatin sensitivity via sponging miR-152-3p. J Surg Res. 2021;261:185–195. doi: 10.1016/j.jss.2020.12.013. [DOI] [PubMed] [Google Scholar]
- 245.Zhu Y, Liu Y, Xiao B, Cai H, Liu M, Ma L, et al. The circular RNA PVT1/miR-203/HOXD3 pathway promotes the progression of human hepatocellular carcinoma. Biology Open. 2019;8:9. doi: 10.1242/bio.043687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Bu N, Dong Z, Zhang L, Zhu W, Wei F, Zheng S. CircPVT1 regulates cell proliferation, apoptosis and glycolysis in hepatocellular carcinoma via miR-377/TRIM23 axis. Cancer Manag Res. 2020;12:12945–12956. doi: 10.2147/CMAR.S280478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Wang Z, Su M, Xiang B, Zhao K, Qin B. Circular RNA PVT1 promotes metastasis via miR-145 sponging in CRC. Biochem Biophys Res Commun. 2019;512(4):716–722. doi: 10.1016/j.bbrc.2019.03.121. [DOI] [PubMed] [Google Scholar]
- 248.Foruzandeh Z, Zeinali-Sehrig F, Nejati K, Rahmanpour D, Pashazadeh F, Seif F, et al. CircRNAs as potent biomarkers in ovarian cancer: a systematic scoping review. Cell Mol Biol Lett. 2021;26(1):41. doi: 10.1186/s11658-021-00284-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Bian Q, Circular RNA. PVT1 promotes the invasion and epithelial-mesenchymal transition of breast cancer cells through serving as a competing endogenous RNA for miR-204-5p. Onco Targets Ther. 2019;12:11817–11826. doi: 10.2147/OTT.S180850. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 250.Wang J, Huang K, Shi L, Zhang Q, Zhang S. CircPVT1 promoted the progression of breast cancer by regulating MiR-29a-3p-mediated AGR2-HIF-1α pathway. Cancer Manag Res. 2020;12:11477–11490. doi: 10.2147/CMAR.S265579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Sun X, Luo L, Gao Y. Circular RNA PVT1 enhances cell proliferation but inhibits apoptosis through sponging microRNA-149 in epithelial ovarian cancer. J Obstet Gynaecol Res. 2020;46(4):625–635. doi: 10.1111/jog.14190. [DOI] [PubMed] [Google Scholar]
- 252.Zheng Z, Chen Z, Zhong Q, Zhu D, Xie Y, Shangguan W, et al. CircPVT1 promotes progression in clear cell renal cell carcinoma by sponging miR-145-5p and regulating TBX15 expression. Cancer Sci. 2021;112(4):1443–1456. doi: 10.1111/cas.14814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Chinen Y, Sakamoto N, Nagoshi H, Taki T, Maegawa S, Tatekawa S, et al. 8q24 amplified segments involve novel fusion genes between NSMCE2 and long noncoding RNAs in acute myelogenous leukemia. J Hematol Oncol. 2014;7:68. doi: 10.1186/s13045-014-0068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Hu J, Han Q, Gu Y, Ma J, McGrath M, Qiao F, et al. Circular RNA PVT1 expression and its roles in acute lymphoblastic leukemia. Epigenomics. 2018;10(6):723–732. doi: 10.2217/epi-2017-0142. [DOI] [PubMed] [Google Scholar]
- 255.Gaffo E, Boldrin E, Dal Molin A, Bresolin S, Bonizzato A, Trentin L, et al. Circular RNA differential expression in blood cell populations and exploration of circRNA deregulation in pediatric acute lymphoblastic leukemia. Sci Rep. 2019;9(1):14670. doi: 10.1038/s41598-019-50864-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Chen T, Chen F. The role of circular RNA plasmacytoma variant translocation 1 as a biomarker for prognostication of acute myeloid leukemia. Hematology (Amsterdam, Netherlands) 2021;26(1):1018–1024. doi: 10.1080/16078454.2021.1987649. [DOI] [PubMed] [Google Scholar]
- 257.Pan X, Guo J, Liu C, Pan Z, Yang Z, Yao X, et al. LncRNA HCG18 promotes osteosarcoma growth by enhanced aerobic glycolysis via the miR-365a-3p/PGK1 axis. Cell Mol Biol Lett. 2022;27(1):5. doi: 10.1186/s11658-021-00304-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Wan J, Liu Y, Long F, Tian J, Zhang C. circPVT1 promotes osteosarcoma glycolysis and metastasis by sponging miR-423-5p to activate Wnt5a/Ror2 signaling. Cancer Sci. 2021;112(5):1707–1722. doi: 10.1111/cas.14787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Huang S-X, Mei H-B, Liu K, Tang J, Wu J-Y, Zhu G-H, et al. CircPVT1 promotes the tumorigenesis and metastasis of osteosarcoma via mediation of miR-26b-5p/CCNB1 axis. J Bone Miner Metab. 2022;40(4):581–593. doi: 10.1007/s00774-022-01326-6. [DOI] [PubMed] [Google Scholar]
- 260.Li D, Huang Y, Wang G. Circular RNA circPVT1 contributes to doxorubicin (DXR) resistance of osteosarcoma cells by regulating TRIAP1 via miR-137. Biomed Res Int. 2021;2021:7463867. doi: 10.1155/2021/7463867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Tao L, Yang L, Tian P, Guo X, Chen Y. Knockdown of circPVT1 inhibits progression of papillary thyroid carcinoma by sponging miR-126. RSC Adv. 2019;9(23):13316–13324. doi: 10.1039/C9RA01820D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Zeng L, Yuan S, Zhou P, Gong J, Kong X, Wu M. Circular RNA Pvt1 oncogene (CircPVT1) promotes the progression of papillary thyroid carcinoma by activating the Wnt/β-catenin signaling pathway and modulating the ratio of microRNA-195 (miR-195) to vascular endothelial growth factor A (VEGFA) expression. Bioengineered. 2021;12(2):11795–11810. doi: 10.1080/21655979.2021.2008639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Zheng X, Rui S, Wang X-F, Zou X-H, Gong Y-P, Li Z-H. circPVT1 regulates medullary thyroid cancer growth and metastasis by targeting miR-455-5p to activate CXCL12/CXCR4 signaling. J Exp Clin Cancer Res. 2021;40(1):157. doi: 10.1186/s13046-021-01964-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.