Monkeypox was discovered in 1958, but scientists are now looking for answers to new questions raised by its continued global spread. Talha Burki reports.
As of June 13, 2022, 1285 confirmed cases of monkeypox had been reported to WHO from 28 non-endemic countries, predominantly in Europe and North America, since mid-May. It is unclear when the outbreak began. Health workers outside the west and central African nations where monkeypox is endemic were unlikely to be looking out for the disease. Besides, if monkeypox is capable of generating asymptomatic infections, which has yet to be confirmed, it could circulate for some time without being detected. Certainly, most newly identified patients have no history of travel to Africa.
“Monkeypox cases have emerged sporadically in non-monkeypox-endemic countries before, but never on this scale, across continents, and with ongoing human-to-human local transmission”, said Sir Ali Zumla, professor of infectious diseases and international health at University College London (UK). He is not surprised by the recent developments. “For decades, scientists in Africa have witnessed a gradual rise in monkeypox cases. As humans continued to move into animal habitats and cross-protection offered from smallpox immunisation campaigns began to wane, the optimal conditions for an outbreak were in place”, said Zumla. Like smallpox, monkeypox is an orthopoxvirus, although fortunately it is much less virulent. The vaccinia virus vaccine that was used against smallpox is highly effective against monkeypox, but has not been part of routine immunisation programmes for several decades.
© 2022 Smith Collection/Gado/Contributor/GettyImages
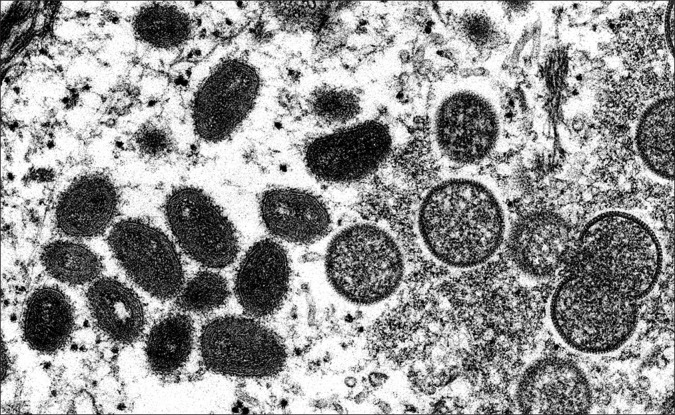
David Evans is a virologist in the department of medical microbiology and immunology at the University of Alberta (Edmonton, AB, Canada). He notes that the clinical presentation of monkeypox does not seem to have changed very much over the past 40 years. But the intervening period has seen the inexorable rise of HIV/AIDS in sub-Saharan Africa. “Monkeypox has done what you would expect it to do. It has taken advantage of immunodeficiencies and declining smallpox vaccination status to expand its numbers”, said Evans. Monkeypox was first discovered in a laboratory monkey in Denmark in 1958. Nonetheless, it is far more common in rodents than in monkeys. The natural reservoir is unknown, as is the range of animals that the virus can infect. Poxviruses contain a large protein complex on their surface, which can attach to almost any kind of cell. “What determines whether an animal can host the monkeypox virus is their ability to block the infection, not whether the virus can enter in the first place”, explained Evans.
The earliest documented human case of monkeypox was in 1970 in Zaire (now DR Congo). The first identified occasion on which the disease broke out from Africa occurred in 2003, after a shipment of monkeypox-infected rodents from Ghana arrived in Texas, USA, where they were kept in close proximity to prairie dogs, which in turn contracted the virus. Several dozen Americans were subsequently diagnosed with monkeypox, starting with a 3-year-old girl who was bitten by her pet prairie dog.
Preliminary genomic sequencing studies have implicated the West African variant of monkeypox in the recent outbreak in non-endemic countries. The variant is associated with an estimated case fatality rate of 1%, as compared with up to 10% for the Congo-basin variant. Cameroon is the only country in which both variants have been found. It is not clear exactly what differentiates the two variants.
No nation outside of Africa has ever reported a death from monkeypox. Symptoms of the disease are typically mild and self-resolving. Once the characteristic lesions have crusted over and fallen off, patients are thought not to be infectious (although there remain questions over whether the virus can linger in bodily fluids such as semen). Still, for some individuals, monkeypox can be serious. Death is a possibility, as is blindness. “If you cannot mount a good cellular immune response to an orthopoxvirus, you will have a terrible time clearing it, and you might not be able to do it”, said Evans. Like smallpox, monkeypox is responsible for fetal mortality. Very young children are also vulnerable. This year alone, DR Congo has seen 1356 suspected cases of monkeypox and 64 deaths.
In a statement to the media on May 31, Hans Kluge, WHO Regional Director for Europe, asserted that “based on the case reports to date, this outbreak is currently being transmitted through social networks connected largely through sexual activity, primarily involving men who have sex with men”. He added that “many, but not all, cases report fleeting and/or multiple sexual partners, sometimes associated with large events or parties”.
Whether or not monkeypox is a sexually transmitted disease has yet to be shown; it is definitely passed on through close contact. Kluge stressed that “the gay and bisexual communities have high awareness and rapid health-seeking behaviour when it comes to their and their communities’ sexual health”. This increased awareness heightens the chances of any disease being diagnosed. Organisations such as the UK Health Security Agency have been collaborating with groups that work with the gay and bisexual communities to alert people to the emergence of monkeypox, and the symptoms of the disease, without stigmatising those at risk. As of June 8, the UK had confirmed 336 cases of monkeypox in the current outbreak, including 320 in England, of which at least 311 were in men.
The spike in cases in Europe and North America could be linked to a mutation that has left the monkeypox virus more transmissible. Set against this possibility is the fact that monkeypox is a DNA virus, which makes it considerably more stable than RNA viruses such as SARS-CoV-2 and influenza. “I think the most probable explanation is that monkeypox simply found its way into the right population at the right time, which has allowed it to spread”, said Anne Rimoin, Professor of Epidemiology at the University of California, Los Angeles Fielding School of Public Health (Los Angeles, CA, USA). “There is no evidence of anything beyond a little bit of random drift, from one host to another”, added Evans.
Zumla believes the outbreak is indicative of a continuing failure to tackle the threat of emerging and re-emerging infectious diseases in a unified way, addressing human, environmental, and animal health. “We are at a pivotal moment in what happens with poxviruses globally”, said Rimoin. “We have given monkeypox an opportunity to spread and spread quickly because we have not been monitoring it in Africa with anything like the kind of intensity that such efforts warrant.” She pointed out that monkeypox researchers have consistently struggled to obtain funding. “This is a virus that, until recently, has been circulating primarily in remote villages in central Africa; it takes a lot of money and organising to do the studies that would allow us to truly understand it”, she said.
Several key questions remain unanswered. “We need to characterise the transmission mechanisms. We need to understand the clinical presentation and disease severity in different risk groups”, Rimoin told The Lancet. “We need to assess the potential for pre-symptomatic transmission, the period of infectivity, and the stability of the virus on surfaces and in the air. We do not even know what the best inactivation protocols are for different settings.”
A central issue concerns the potential for reverse zoonosis. Can human beings transmit monkeypox to animals? If monkeypox does become established in an animal population in Europe or North America, it will be difficult to eradicate. In such circumstances, endemicity would be a distinct possibility. “It is not immediately obvious which European species could host monkeypox, but it would probably be some kind of shrew or vole”, said Evans. “Certainly, in Africa the virus is found in a variety of rodents.” Matters are complicated by the widespread presence of various strains of cowpox in Europe, against which monkeypox would presumably be competing. In which case, monkeypox might struggle to gain traction. North America, on the other hand, does not appear to have much orthopoxvirus in circulation, which might make it more vulnerable to monkeypox.
WHO has suggested that monkeypox will continue spreading in Europe over the summer months. An antiviral has been authorised by the European Medicines Agency, and a vaccine has been approved by the US Food and Drug Administration. The UK has purchased over 20 000 doses of the vaccine, which it is making available to close contacts of those diagnosed with monkeypox. The vaccine is ideally given within 4 days of exposure to the virus, although it is thought to be effective up to 14 days post-exposure.“We should now be able to draw some conclusions on how the therapeutics and vaccines work in real-world circumstances”, said Evans. “Is the vaccine really effective as post-exposure prophylaxis?” These are products that could be deployed against smallpox, in the event of an accidental or deliberate release of the virus. Indeed, monkeypox has long been used by researchers as a surrogate for smallpox. “The silver lining of this new outbreak is that we can assess how the actual performance of the drugs and vaccine compare with the predictive models accepted by the US Food and Drug Administration and Health Canada as evidence of efficacy”, said Evans. “That will help clarify our procedures in terms of dealing with monkeypox, but it will also provide a little reassurance in terms of smallpox.”