Abstract
Virus purification in a high-containment setting provides unique challenges due to barrier precautions and operational safety approaches that are not necessary in lower biosafety level (BSL) 2 environments. The need for high risk group pathogen diagnostic assay development, anti-viral research, pathogenesis and vaccine efficacy research necessitates work in BSL-3 and BSL-4 labs with infectious agents. When this work is performed in accordance with BSL-4 practices, modifications are often required in standard protocols. Classical virus purification techniques are difficult to execute in a BSL-3 or BSL-4 laboratory because of the work practices used in these environments. Orthopoxviruses are a family of viruses that, in some cases, requires work in a high-containment laboratory and due to size do not lend themselves to simpler purification methods. Current CDC purification techniques of orthopoxviruses uses 1,1,2-trichlorotrifluoroethane, commonly known as Genetron®. Genetron® is a chlorofluorocarbon (CFC) that has been shown to be detrimental to the ozone and has been phased out and the limited amount of product makes it no longer a feasible option for poxvirus purification purposes. Here we demonstrate a new Orthopoxvirus purification method that is suitable for high-containment laboratories and produces virus that is not only comparable to previous purification methods, but improves on purity and yield.
Keywords: Orthopoxvirus, Variola, Monkeypox, Purification, High-containment
1. Introduction
Virus purification in a high-containment setting provides unique challenges due to barrier precautions and operational safety approaches that are not necessary in lower biosafety level (BSL) 2 environments. The need for high risk group pathogen diagnostic assay development, anti-viral research, pathogenesis and vaccine efficacy research necessitates work in BSL-4 labs with infectious agents. When this work is performed in accordance with BSL-4 practices, modifications are often required in standard protocols. Classical virus purification techniques are difficult to execute in a BSL-3 or BSL-4 laboratory because of the work practices used in these environments. The minimal use of sharp objects in the BSL-4 labs restricts the use of glass items, such as a dounce homogenizer, or needles as would be needed for certain gradient extractions. The visibility and dexterity in either a full-body, air-supplied, positive pressure suit, or a class III biosafety cabinet also make procedures like visual identification of gradient layers containing virions in gradient centrifugations more difficult. Under some instances, methods employed to purify small virus particles by filtration of culture media might not be suitable for larger pathogens (Berting et al., 2005, Ver et al., 1968). Hence, there is a need for pathogen specific protocols to produce purified preparation of viruses. In this study, we have addressed an alternate protocol for simple and efficient purification of Variola virus (VARV), a BSL-4 pathogen.
VARV, the causative agent of smallpox, belongs to the Orthopoxvirus genus of the family Poxviridae. The poxviruses includes large double stranded DNA (dsDNA) viruses, approximately 360 × 270 × 250 nm, with a wide host range of infectivity, from insects to mammals. One of the unique features of poxviruses is the ability to replicate and assemble into the fully infectious form in the cytoplasm of infected cells (Cyrklaff et al., 2005, Moss, 2012). The majority of mature infectious virions (MVs) accumulate in the cytoplasm with only a small portion, <1%, secreted in the form of extracellular virus (Payne, 1979, Payne, 1986). Hence, the purification of poxviruses are primarily of the MV form from cell lysates. Infected cells are sheared using dounce homogenizers suspended in hypotonic lysis buffer or through the use of repeated freeze/thaw cycles, followed by separation using density gradient centrifugations (Broder and Earl, 1999, Huang and Chang, 2012, Kremer et al., 2012). Although, this method is widely employed in BSL-2 laboratories for purification of most orthopoxviruses such as Vaccinia virus (VACV) and Cowpox virus (CPXV), safety precautions prevent use of this procedure in high-containment laboratories, while working with Monkeypox virus (MPXV) (BSL-2 with BSL-3 practices and BSL-3 if working with infected animals) or VARV (BSL-4) (Canada, 2011, Services et al., 2009).
Current CDC purification techniques of orthopoxviruses uses 1,1,2-trichlorotrifluoroethane, commonly known as Genetron®. Genetron®, aids in the disassociation of virus particles from cellular membranes and has been used in poxvirus purification, hepatitis A vaccine investigation studies, purification of previously unknown viruses such as fowl poxviruses and epizootic hemorrhagic disease virus among other virus purifications (Al Falluji et al., 1979, Bogaerts and Durville-van der, 1972, Epstein, 1958, Heinricy et al., 1987, Kontor and Welch, 1976, Welch, 1971). Genetron® is a chlorofluorocarbon (CFC) that has been shown to be detrimental to the ozone and the Montreal protocol called for the phase out of Genetron® use by 2010. Though there are exceptions in the United States for the use of Genetron®, the limited amount of product makes it no longer a feasible option for poxvirus purification purposes. Due to the need for purified MPXV and VARV in diagnostic assay and animal model development, a new purification protocol lacking Genetron® and employing a deoxyribonuclease (Benzonase®) was utilized for purification. Initial experiments were performed and optimized using VACV in a BSL-2 laboratory and followed up with VARV and MPXV purification in BSL-4 or BSL-3 labs respectively. In this study, we present the efficacy of the new Benzonase® protocol compared to Genetron® purification for high-containment laboratories.
2. Materials and methods
2.1. Viruses
MPXV strain USA 2003_44 (accession #DQ011153),VACV strain Wyeth, and VARV strain Bangladesh 1975 (accession #L22579) were used in this study. VARV is a Tier-1 select agent and subject to the select agent regulations 42 CFR Part 73. Per Biosafety in Microbiological and Biomedical Laboratories recommendations, all of the staff who participated in this work were vaccinated (U.S.D.o.H.a.H Services, 2009). MPXV and VACV were grown at 37 °C and VARV was grown at 35.5 °C. Initial experiments with MPXV and VACV were conducted in a BSL-2 laboratory using BSL-3 precautions and experiments with live VARV were performed in a BSL-4 laboratory. BSC-40 cells (African green monkey kidney cells) from eight T150 flasks, infected at a multiplicity of infection (MOI) of 0.1, were harvested at optimal observable cytopathic effects (CPE), approximately 48 h post-inoculation (hpi).
2.2. Virus purification
2.2.1. Benzonase®-positive and Benzonase®-negative purifications
The infected cells were scraped from the flasks and combined, then centrifuged at 15,300 × g in a Beckman J14 rotor for 1 h. The pellet was resuspended in 60 ml total volume of 1 mM Tris–HCL (pH 9.0) (sample 1) and divided in half placing 30 ml into each of two, 50 ml conical tube. Both suspensions were sonicated three times in a cup horn sonicator (Branson Digital Sonifier® 450) containing water maintained at 4 °C with ice for 1 min at 160 W, vortexing and placing the tubes on ice for 20 s between each sonication and replacing the ice water between sonications. Five μl of Benzonase® (≥250 units/uL; Sigma-Aldrich #E1014-25KU CAS#9025-65-4), St. Louis, MO) was added to one sample (sample B+) and incubated at room temperature for 30 min while the other sample was left on ice (B-). Samples were centrifuged for 10 min at 1174 × g in a Sorval ST 16R and the resulting supernatants (approximately 25–30 ml) were laid over a 5 ml 36% sucrose cushion in a 50 ml polycarbonate Oak Ridge centrifuge tube (Beckman #3118-0050, Brea, CA) and centrifuged for 80 min at 22,600 × g in a Beckman JS13.1 rotor. The supernatants were removed and each pellet resuspended in 5 ml 1 mM Tris–HCL (pH 9.0) and sonicated as described above. One milliliter was removed for analysis. The remaining 4 ml of suspension was placed over a 1 ml 36% sucrose (w/v in 1 mM Tris–HCl pH 9.0 buffer) cushion in a 5 ml sterile polyallomer centrifuge tube (Beckman #326819) and centrifuged for 80 min at 30,000 × g in a Beckman SW55Ti swinging bucket rotor. Again the supernatant was removed and the final pellet was resuspended in a total volume of 1 ml 1 mM Tris–HCL (pH 9.0) and sonicated as described previously. A diagram of the experimental outline demonstrates the steps (Supplementary Fig. 1). Samples were taken at each step for analysis.
2.2.2. Genetron® purification
The Genetron® purification was modified from the original protocol (Epstein, 1958) and performed as described previously (Hughes et al., 2014). The infected cells were scraped from the flasks and combined, then centrifuged at 15,300 × g in a Beckman J14 rotor for 1 h at 4 °C. The pellet was resuspended in 20 ml total volume of Tris–HCL (pH 9.0). The suspension was sonicated three times at 160 W for 1 min, vortexed and placed on ice for 20 s between each cycle. The ice water was replaced between sonications. Samples were then centrifuged at 4 °C for 10 min at 1174 × g in a Sorval ST 16R and the supernatants were collected, combined, and placed on ice. The pellets were resuspended in 10 ml total volume of 1 mM Tris–HCL pH 9.0. Samples were sonicated as described above. The suspensions were centrifuged at 1174 × g in a Sorval ST 16R for 10 min at 4 °C, supernatants were collected and combined with preparations from the previous spin for a total volume of 30 ml. This volume was then divided into two 50 ml conical tubes containing 15 ml each. Twenty ml of Genetron® was added to each tube, vortexed twice for 30 s, to achieve a homogeneous viscous mixture, and then centrifuged at 1174 × g for 5 min at 4 °C. The upper aqueous phase was collected and placed into a new tube. An equivalent volume of Genetron® was added to each tube and the samples were centrifuged again at 1174 × g for 5 min at 4 °C. The resulting supernatants (approximately 25–30 ml) were overlaid onto a 5 ml 36% sucrose cushion in a 50 ml polycarbonate Oak Ridge centrifuge tube (Beckman #3118-0050) and centrifuged for 80 min at 22,600 × g in a Beckman JS13.1 rotor. The supernatants were discarded and pellet was resuspended in 5 ml of Tris–HCL and sonicated three times. The suspensions (4 ml) were placed over a 1 ml 36% sucrose cushion in a 5 ml sterile polyallomer centrifuge tube (Beckman #326819) and centrifuged for 80 min at 30,000 × g in a Beckman SW55Ti swinging bucket rotor. The supernatants were discarded and the final pellets were resuspended in a total volume of 1 ml 1 mM Tris–HCL (pH 9.0) and sonicated as described previously. An aliquot of all samples were taken at each step for analysis.
2.3. Real-time PCR
2.3.1. Generic orthopoxvirus PCR
Orthopoxvirus DNA was extracted using the QIAamp DNA Blood Mini Kit per manufacturer’s instructions (Qiagen, Valencia, CA). The Orthopoxvirus generic PCR was performed as previously described (Reynolds et al., 2010). In short, primers and probes targeting the Orthopoxvirus DNA polymerase gene E9L (GenBank accession no. L22579) were synthesized in the Biotechnology Core Facility (CDC). Reactions contained 1 μl of viral DNA diluted 1:500 in water, 0.5 μl of each primer, 0.5 μl of probe added to the Taqman Fast Advanced Master Mix (ABI; cat.#4444964, Applied Biosystems, Foster City, CA). Cycling conditions were 95 °C for 20 s followed by 40 cycles of 95 °C for 3 s, 60 °C for 30 s.
2.3.2. Cellular DNA PCR
The cellular DNA PCR was performed as described previously (Kondas et al., 2015). In short, primers and probes targeting a cellular gene were synthesized in the Biotechnology Core Facility (CDC). Reactions contained 1 μl of viral DNA diluted 1:500 in water, 0.5 μl of each primer and 0.5 μl of probe added to the Taqman Fast Advanced Master Mix (ABI; cat.#4444964). Cycling conditions were 95 °C for 20 s followed by 40 cycles of 95 °C for 3 s, 60 °C for 30 s.
2.4. Western blot for cellular contamination
Virus samples were separated on a 4–20% gradient gel (Bio-Rad mini-PROTEAN TGX ® precast gels, Bio-Rad, Hercules, CA) and transferred to 0.45 μM nitrocellulose membrane. The membrane was probed with an organelle detection antibody cocktail (Abcam #133989, Cambridge, MA) at manufacturer’s recommended dilution. After 1 h incubation, the membrane was washed two times with PBS containing 0.05% Tween 20 and once with PBS. The membrane was incubated with 1:3000 dilution of secondary antibody (KPL #074-18-061) for 1 h, washed and developed using Clarity Western ECL Substrate (Bio-Rad).
2.5. Inactivation of VARV for western blot analysis and microscopy
The standard one kill dose (KD) for inactivation of OPXVs by gamma-irradiation is 4.4 × 106 rads. VARV was inactivated with WHO approved 3 KD radiation. MPXV and VACV were inactivated using UV irradiation for 10 min. UV inactivation was validated by plaque assay.
2.6. Electron microscopy of samples
Negative staining of purified virus was performed after inactivation with either gamma- or UV-irradiation. Briefly, inactivated virus was sonicated three times as described previously and allowed to adsorb to a formvar/carbon-coated electron microscopy grid and stained with 5% ammonium molybdate, pH 6.9, and 0.1% trehalose. Grids were examined in an FEI Spirit electron microscope.
2.7. Determination of viral titer
Viral titer was determined by standard plaque assay on BSC-40 cells in a 6-well plate format as described previously (Hutson et al., 2015). Essentially, cells were infected with 10-fold virus dilutions for 1 h at 37 °C (MPXV and VACV) or 35.5 °C (VARV). Virus inoculum was removed after 1 h, replaced with 2% RPMI and were incubated for 2 (MPXV and VACV) at 37 °C or 3 days (VARV) at 35.5 °C in 5% CO2. The plaques were visualized by crystal violet staining (in 10% formalin).
3. Results
3.1. Comparison of a spin-only purification method with purification containing the addition of Benzonase®
Deoxyribonucleases (DNAse) have been previously demonstrated to be effective in virus purification methods (Kleiner et al., 2015, Sun et al., 2014). In this study, we investigated advantages of a strong DNAse, such as Benzonase®, to the purity of the final virus preparation without compromising virus yield.
3.1.1. Comparison of viral genome copy number
As shown in Supplementary Table 1, both the Benzonase® treated and the untreated sample showed similar vaccinia viral genome copy numbers (GCN). The Benzonase® positive sample showed no cellular DNA contamination after the Benzonase® was added. The Benzonase® negative sample, however, still contained detectable levels of cellular DNA (CT values <40) with a slight decrease with each purification step as indicated by the increasing CT values. Therefore, the use of Benzonase® increased purity of viral preparation by degradation of cellular DNA contamination that co-precipitated with the virus particles.
3.1.2. Electron microscopy of Benzonase®-positive and Benzonase®-negative purification samples
All of the samples were imaged using an electron microscope as shown in Supplementary Fig. 2. The negative stain of purified virus particles from both Benzonase®-treated and untreated samples appeared similar in overall morphology and size. Since, the staining intensity was different in the two methods, we performed additional experiments to determine levels of purity from contaminating cellular organelles and membrane proteins.
3.2. Comparison of Benzonase® purification technique with Genetron® purification technique
To determine if the Benzonase® protocol was viable for a high-containment laboratory and could provide comparable results to the standard purification technique, this was performed along with the Genetron® protocol. Both protocols were performed by two different individuals to assess for any variability across users. Viable virus was calculated as plaque forming units per ml (pfu/ml).
3.2.1. Production of viable virus
Pre- and post-procedure viral titers were calculated to assess for loss. As shown in Table 1 , both protocols started with very similar numbers of viable viral particles as determined by plaque assay. The final purified virus preparation using Genetron® yielded more than a log lower total pfu compared to the starting viral titer. However, Benzonase® treatment did not exhibit appreciable loss in virus titer as determined by plaque assay pre- and post- purification samples. This demonstrates more efficient retrieval of virus particles by Benzonase® during the purification process.
Table 1.
Comparison of virus titers, GCN, and particle to PFU ratios from Genetron® and Benzonase® purification methods.
| Average Titer (pfu/ml) | Total pfu | GCN/ml | Total GCN | GCN/pfu ratio | Cellular DNA CT | |
|---|---|---|---|---|---|---|
| Pre-Genetron® | 2.8E + 09 | 2.75E + 10 | 4.00E + 10 | 4.00E + 11 | 14.6 | 18.4 |
| Final Genetron® | 1.1E + 10 | 3.31E + 09 | 4.18E + 10 | 4.18E + 10 | 12.6 | 18.4 |
| Pre-Benzonase® | 2.4E + 09 | 2.44E + 10 | 3.17E + 10 | 1.79E + 11 | 7.34 | 18.8 |
| Final Benzonase® | 1.6E + 10 | 1.61E + 10 | 1.74E + 11 | 1.74E + 11 | 10.8 | Undetermined |
3.2.2. Determination of viral GCN
Viral genome copy number as determined by quantitative Real Time-PCR was to determine viral load in the samples. Both purification methods had similar levels of viral genome copies as shown in Table 1. Based on these results, the Genetron® purification method appears to have a greater overall loss in virus than the Benzonase® purification method. As seen with virus titers, the Genetron® purification method exhibited a greater loss in viral genomes than seen with the use of Benzonase®. The determination of viral titer and viral GCN are both methods that can provide valuable information, but each have different limitations so that viral GCN is not directly comparable to viral titer. To try and address this, the GCN to viable virus ratio or genome to pfu ratio was calculated. Both purification methods resulted in similar genome/pfu ratios with the Genetron® purification method showing a slight increase in the genome/pfu ratio.
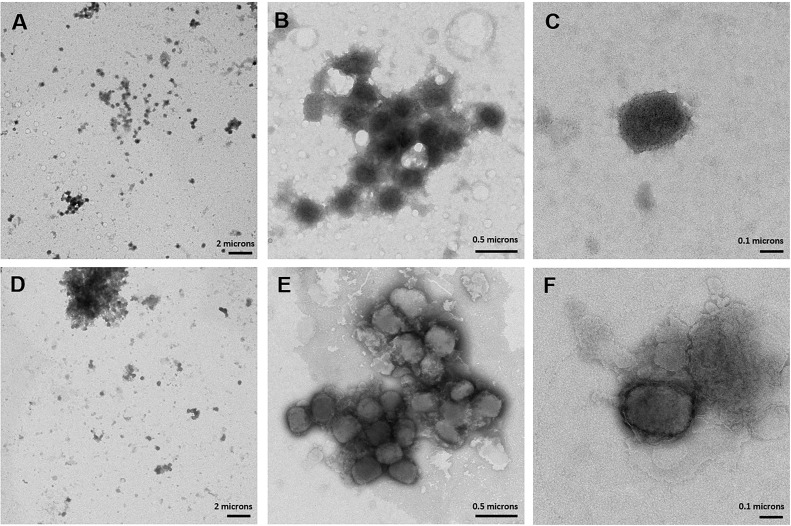
3.2.3. Investigation of viral aggregation
Previous reports have indicated that virus particle density can affect aggregation properties (Planterose et al., 1962). To investigate viral aggregation, electron microscopy images were compared. Fig. 1 shows images of the overall samples, aggregates, and individual particles. Both samples appear to have similar purity levels, but the Benzonase®-treated samples are more prone to aggregation, which can be reduced with sonication.
Fig. 1.
Electron Microscopy images of (A–C) Genetron® purified samples and (D–F) Benzonase® purified samples. Figures shown representative images of (A and D) the purity of the preparations, (B and E) image of aggregates, and (C and F) an individual Variola virus particle.
To determine if variation in purity and aggregation occurs routinely between virus preparations, Genetron® purification of three different orthopoxviruses were compared via electron microscopy (Supplementary Fig. 3). Under these conditions, MPXV appears to aggregate the most. Interestingly, it also appears to contain the least amount of contamination. As the MPXV appears to contain the least amount of contaminants, it is possible that the differing aggregation properties of the viruses are due to the cleanliness of the virus. Previous reports have indicated that virus particle density can affect aggregation properties (Planterose et al., 1962); while this might be a factor, it is unlikely that it is the only factor in this investigation as all of these preparations are of similar high titer leading to the assumption that they are of similar concentration density.
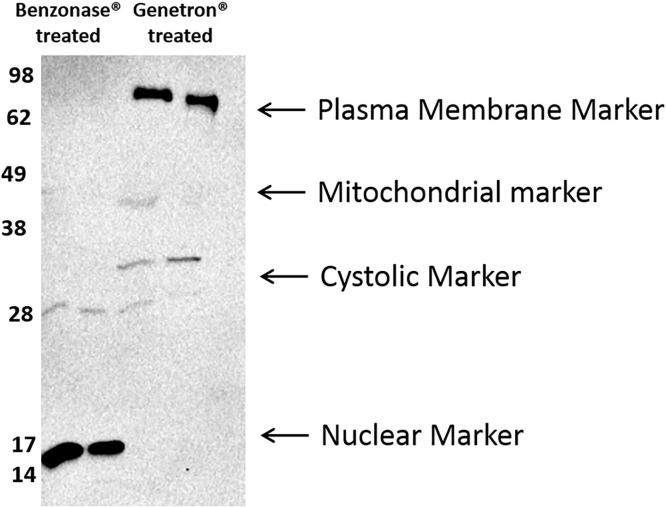
3.2.4. Examination of cellular contaminants
To determine the type of protein contaminations present, samples were analyzed by western blot and by PCR specific to cellular DNA. An antibody cocktail that identifies a plasma membrane protein, a mitochondrial membrane protein, a cytosolic membrane protein, and a nuclear membrane protein was used for analysis (Fig. 2 ). Though both methods of purification produced similar levels of cellular contaminants, the nature of the contaminants are markedly different. The Benzonase® purification method consists primarily of nuclear membrane proteins with a very slight amount of mitochondrial contamination, while the Genetron® purification method contaminants are comprised primarily of plasma membrane proteins with some cytosolic contaminants and varying mitochondrial contaminants. As would be expected, in Table 1, the Benzonase ® treated samples have no detectable cellular DNA contamination, while the Genetron® samples show no change in the amount of cellular DNA levels, even though both samples started with similar levels of cellular DNA contamination. It is possible that these difference in cellular contaminants are a contributing factor to the variation in aggregation properties.
Fig. 2.
Western blot of cellular membrane protein contaminants: Though both methods of purification appear to produce similar levels of cellular contaminants, the nature of the contaminants are markedly different. The Benzonase® purification method consists primarily of nuclear membrane proteins with a very slight amount of mitochondrial contamination, while the Genetron® purification method contaminants are comprised primarily of plasma membrane proteins with some cystolic contaminants and varying mitochondrial contaminants.
3.2.5. Assessment of Benzonase® activity after purification
To assess whether any active Benzonase® was detectable at the end of the purification process that could potentially affect later assays, the virus sample was spiked with human DNA. The change in cellular DNA CT values was assessed after 1 h. Table 2 shows that there was no significant change in the levels of human DNA after incubation with the virus sample indicating that there is no active Benzonase® left after the purification. It was determined that downstream steps of the purification method either inactivate or remove the Benzonase®. Therefore, the use of a DNAse in this protocol should have no effect when these virus preps are utilized for in vitro or in vivo based assays.
Table 2.
Determination of active Benzonase® left in purified sample: After samples were spiked with human DNA for one hour, changes in cellular DNA CT values were determined.
| 0 h (CT value) | 1 h (CT value) | |
|---|---|---|
| Virus Sample from Benzonase® prep + human DNA | 35.04 | 34.89 |
| Virus sample from Benzonase® prep + no DNA | Undetermined | Undetermined |
| Positive Control (human DNA spiked into the PCR reaction alone) | 29.68 | 29.46 |
| Negative Control (nothing added to the PCR reaction) | Undetermined | Undetermined |
4. Discussion
Genetron®’s detrimental effects on the ozone made development of an alternate virus purification method that was appropriate for use in high-containment laboratories a necessity. The size of orthopoxviruses makes the use of traditional purification methods, such as filtration, a poor alternative to the use of Genetron®. In establishing this protocol, we determined that while the removal of Genetron® from the original protocol was sufficient to produce semi-pure virus, the addition of Benzonase® significantly decreased contamination with cellular DNA and altered the types of membrane contaminants found in the concentrated virus preps. It also appears that the use of Benzonase® results in a slightly greater retention of viable virus at the end of the purification protocol though there are no significant differences in the genome/pfu ratios. Whilst the Benzonase® treatment was shown to remove cellular DNA, viral genomic DNA did not seem to be affected. This explains the lack of change in GCN from the pre- and post-Benzonase® treatments. The aggregation of Benzonase® treated samples are probably due to greater particle concentration within the samples and can be overcome by more stringent sonication methods. Finally, decreased time for manipulations to purify the virus within the high containment laboratories was an additional benefit.
In conclusion, Benzonase® purification resulted in a higher yield of virus and was less time and labor intensive than the standard Genetron® purification method. The use of Benzonase® leads to less cellular DNA contamination and though the protein contamination for the two methods is different, this appears to have no effect on assays requiring live virus. The use of Benzonase® in place of Genetron® is a viable alternative for purification of viruses in a high-containment setting.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention. Use of trade, product of firm names does not imply endorsement by the U.S Government.
Acknowledgements and funding
This research was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and CDC. This work was conducted with ACVVR/WHO approval.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jviromet.2017.01.018.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Al Falluji M.M., Tantawi H.H., Al-Bana A., Al-Sheikhly S. Pox infection among captive peacocks. J. Wildl. Dis. 1979;15:597–600. doi: 10.7589/0090-3558-15.4.597. [DOI] [PubMed] [Google Scholar]
- Berting A., Goerner W., Spruth M., Kistner O., Kreil T.R. Effective poxvirus removal by sterile filtration during manufacture of plasma derivatives. J. Med. Virol. 2005;75:603–607. doi: 10.1002/jmv.20299. [DOI] [PubMed] [Google Scholar]
- Bogaerts W.J., Durville-van der O. Immunization of mice against encephalomyocarditis virus. I. Purification concentration, and inactivation of encephalomyocarditis virus. Infect. Immun. 1972;6:508–512. doi: 10.1128/iai.6.4.508-512.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broder C., Earl P. Recombinant vaccinia viruses. Mol. Biotechnol. 1999;13:223–245. doi: 10.1385/MB:13:3:223. [DOI] [PubMed] [Google Scholar]
- Canada, P.H.A.o., 2011. Monkeypox Virus.
- Cyrklaff M., Risco C., Fernandez J.J., Jimenez M.V., Esteban M., Baumeister W., Carrascosa J.L. Cryo-electron tomography of vaccinia virus. Proc. Natl. Acad. Sci. U. S. A. 2005;102:2772–2777. doi: 10.1073/pnas.0409825102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein M.A. An investigation into the purifying effect of a fluorocarbon on vaccinia virus. Br. J. Exp. Pathol. 1958;39:436–446. [PMC free article] [PubMed] [Google Scholar]
- Heinricy U., Stierhof Y.D., Pfisterer M., Flehmig B. Properties of a hepatitis A virus candidate vaccine strain. J. Gen. Virol. 1987;68(Pt. 9):2487–2493. doi: 10.1099/0022-1317-68-9-2487. [DOI] [PubMed] [Google Scholar]
- Huang C.-Y., Chang W. In: Vaccinia Virus and Poxvirology. Isaacs S.N., editor. Humana Press; 2012. Imaging of vaccinia virus entry into HeLa cells; pp. 123–133. [DOI] [PubMed] [Google Scholar]
- Hughes L.J., Goldstein J., Pohl J., Hooper J.W., Lee Pitts R., Townsend M.B., Bagarozzi D., Damon I.K., Karem K.L. A highly specific monoclonal antibody against monkeypox virus detects the heparin binding domain of A27. Virology. 2014;464–465:264–273. doi: 10.1016/j.virol.2014.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutson C.L., Nakazawa Y.J., Self J., Olson V.A., Regnery R.L., Braden Z., Weiss S., Malekani J., Jackson E., Tate M., Karem K.L., Rocke T.E., Osorio J.E., Damon I.K., Carroll D.S. Laboratory investigations of African pouched rats (Cricetomys gambianus) as a potential reservoir host species for monkeypox virus. PLoS Negl. Trop. Dis. 2015;9:e0004013. doi: 10.1371/journal.pntd.0004013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiner M., Hooper L.V., Duerkop B.A. Evaluation of methods to purify virus-like particles for metagenomic sequencing of intestinal viromes. BMC Genom. 2015;16 doi: 10.1186/s12864-014-1207-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondas A.V., Olson V.A., Li Y., Abel J., Laker M., Rose L., Wilkins K., Turner J., Kline R., Damon I.K. Variola virus-specific diagnostic assays: characterization, sensitivity, and specificity. J. Clin. Microbiol. 2015;53:1406–1410. doi: 10.1128/JCM.03613-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kontor E.J., Welch A.B. Characterisation of an epizootic haemorrhagic disease virus. Res. Vet. Sci. 1976;21:190–196. [PubMed] [Google Scholar]
- Kremer M., Volz A., Kreijtz J.C.M., Fux R., Lehmann M., Sutter G. In: Vaccinia Virus and Poxvirology. Isaacs S.N., editor. Humana Press; 2012. Easy and efficient protocols for working with recombinant vaccinia virus MVA; pp. 59–92. [DOI] [PubMed] [Google Scholar]
- Moss B. Poxvirus cell entry: how many proteins does it take? Viruses. 2012;4:688–707. doi: 10.3390/v4050688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne L.G. Identification of the vaccinia hemagglutinin polypeptide from a cell system yielding large amounts of extracellular enveloped virus. J. Virol. 1979;31:147–155. doi: 10.1128/jvi.31.1.147-155.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne L.G. The existence of an envelope on extracellular cowpox virus and its antigenic relationship to the vaccinia envelope. Arch. Virol. 1986;90:125–133. doi: 10.1007/BF01314150. [DOI] [PubMed] [Google Scholar]
- Planterose D.N., Nishimura C., Salzman N.P. The purification of vaccinia virus from cell cultures. Virology. 1962;18:294–301. doi: 10.1016/0042-6822(62)90016-8. [DOI] [PubMed] [Google Scholar]
- Reynolds M.G., Carroll D.S., Olson V.A., Hughes C., Galley J., Likos A., Montgomery J.M., Suu-Ire R., Kwasi M.O., Jeffrey Root J., Braden Z., Abel J., Clemmons C., Regnery R., Karem K., Damon I.K. A silent enzootic of an Orthopoxvirus in Ghana, West Africa: evidence for multi-species involvement in the absence of widespread human disease. Am. J. Trop. Med. Hyg. 2010;82:746–754. doi: 10.4269/ajtmh.2010.09-0716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Services U.S.D.o.H.a.H., Service P.H., Prevention C.f.D.C.a., Health N.I.o. 5 ed. 2009. Biosafety in Microbiological and Biomedical Laboratories. (p. 415) [Google Scholar]
- Sun G., Xiao J., Wang H., Gong C., Pan Y., Yan S., Wang Y. Efficient purification and concentration of viruses from a large body of high turbidity seawater. MethodsX. 2014;1:197–206. doi: 10.1016/j.mex.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ver B.A., Melnick J.L., Wallis C. Efficient filtration and sizing of viruses with membrane filters. J. Virol. 1968;2:21–25. doi: 10.1128/jvi.2.1.21-25.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch A.B. Purification, morphology and partial characterization of a reovirus-like agent associated with neonatal calf diarrhea. Can. J. Comp. Med.: Rev. Can. Med. Comp. 1971;35:195–202. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.