Abstract
Since the eradication of Smallpox, researchers have attempted to study Orthopoxvirus pathogenesis and immunity in animal models in order to correlate results human smallpox. A solely human pathogen, Orthopoxvirus variola fails to produce authentic smallpox illness in any other animal species tested to date. In 2003, an outbreak in the USA of Orthopoxvirus monkeypox, revealed the susceptibility of the North American black-tailed prairie dog (Cynomys ludovicianus) to infection and fulminate disease. Prairie dogs infected with Orthopoxvirus monkeypox present with a clinical scenario similar to ordinary smallpox, including prodrome, rash, and high mortality. This study examines if Black-tailed prairie dogs can become infected with O. variola and serve as a surrogate model for the study of human smallpox disease. Substantive evidence of infection is found in immunological seroconversion of animals to either intranasal or intradermal challenges with O. variola, but in the absence of overt illness.
Keywords: Variola, Smallpox, Immunity, Infection, Orthopoxvirus, Prairie dog, Animal model
Introduction
Homo sapiens are the only known natural or permissive host for smallpox (Orthopoxvirus variola). Heroic efforts in the 20th century eradicated smallpox from the human population and led to the eventual consolidation of O. variola stocks into two WHO sanctioned smallpox research collaborating programs in the US and Russia. Historically, although suckling mice succumb to infections with O. variola, no adult rodent or small mammal models using O. variola have been successfully developed (Mayr and Herrlich, 1960, Murti and Shrivastav, 1957). O. variola challenges of various non-human primate species were conducted in the 20th century (Hahon and Wilson, 1960, Brinckerhoff and Tyzzer, 1906, Noble and Rich, 1969), and some cause generalized rash, but rarely was mortality observed. In recent years, efforts to develop new therapeutics and vaccines for smallpox have relied on surrogate, non-O. variola Orthopoxvirus animal infection models and one O. variola model in non-human primates. Despite significant animal models of Orthopoxvirus infection (Chapman et al., 2010) to date the only lethal animal model using O. variola infection is a high dose intravenous, or intravenous/aerosol challenge of non-human primates (Cynomolgus macaques) (Jahrling et al., 2004). At highest challenge dose (109 pfu), disease onset is rapid, within 3–4 days post-infection, with some attributes of hemorrhagic disease and is often lethal by 7 days post infection. A lower dose (108 pfu), results in a more typical rash illness with rash onset occuring at 3–4 days post exposure and rash progression similar to smallpox. Studies based on this latter challenge model have used small number of animals, and overall mortality and disease progression has been variable (Jahrling et al., 2004). An O. monkeypox respiratory challenge model in non-human primates may provide a surrogate model for O. variola since clinical disease progression in this model is more similar to human smallpox than an intravenous challenge (Dyall et al., 2011, Goff et al., 2011, Nalca et al., 2010). However, human smallpox was not commonly associated with extensive pulmonary manifestations, as seen in the intrabronchial respiratory O. monkeypox challenges. Additional surrogate models have been researched using non-O. variola orthopoxviruses to mimic smallpox like disease in various animal models (reviewed in (Chapman et al., 2010)).
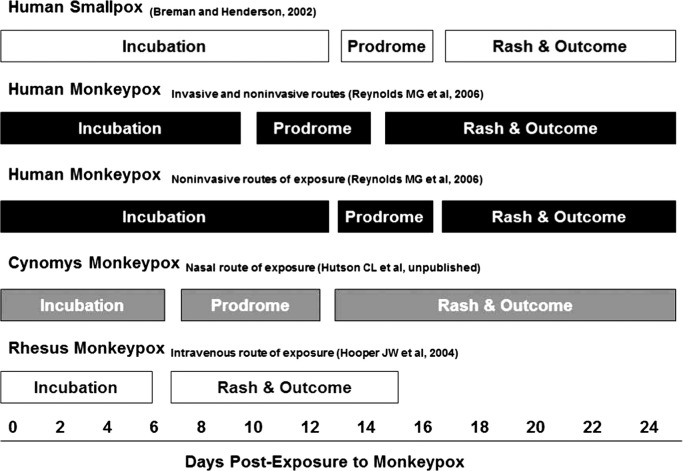
In 2003 a US outbreak of O. monkeypox resulted in the inadvertent infection of a North American species, Cynomys ludovicianus (Black-tailed prairie dog) as well as a substantial human outbreak (Reed et al. 2004). Subsequent research studies identified the susceptibility of this species to O. monkeypox and revealed a clinical course similar to ordinary (human) smallpox (Hutson et al., 2009; Reynolds et al. 2006). Evidence stemming from the 2003 US outbreak of monkeypox and subsequent laboratory challenge studies of O. monkeypox in Cynomys confirm this susceptibility and lethality through intranasal O. Monkeypox challenge with relatively low viral doses (103 pfu). Similar clinical features, and timecourse of illness, to that previously observed in ordinary human smallpox and in human monkeypox was observed in cynomys infected with O. monkeypox ( Fig. 1). High susceptibility of this new world mammal species with an old world virus (O. monkeypox) promoted the question of whether or not Cynomys is susceptible to O. variola. In an effort to test this hypothesis, Black-tailed prairie dogs were obtained and subjected to infection with O. variola via two routes, intranasal and intradermal scarification.
Fig. 1.
Summary of clinical pathogenesis and stages of illness of smallpox in humans, and monkeypox in humans, prairie dogs and rhesus maquaces.
Results
Pathogenesis
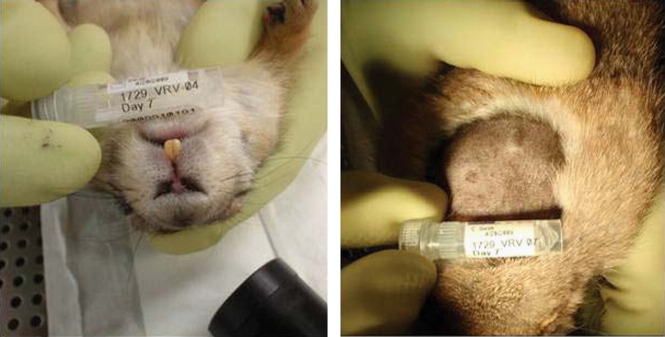
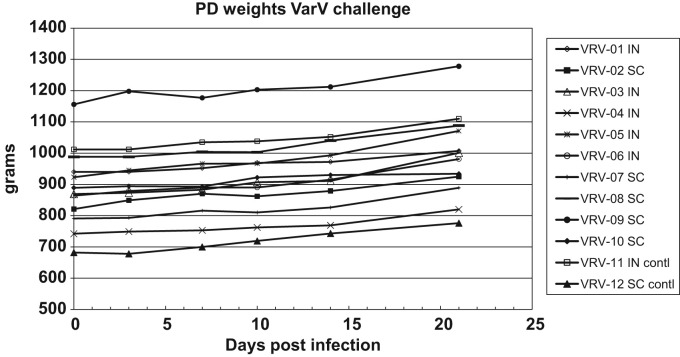
To determine if prairie dogs are susceptible to O. variola, animals were infected by intranasal or intradermal routes with 6.6×106 pfu O. variola as described in materials and methods and monitored daily for signs of illness. Slight erythema was noted in all intradermally challenged animals at days 2–4 at the inoculation site but no observed lesion could be identified at day 7 ( Fig. 2). In animals challenged intranasally, slight redness was noted at day 3 post challenge around the nares, but by day 7 no signs of infection could be identified (Fig. 2). Otherwise no signs of illness or infection were detectable upon gross physical examination. Body weight was taken every three days and indicates no significant weight loss post challenge for any animals ( Fig. 3).
Fig. 2.
Photos of inoculation sites day 7 post inoculation (a) intranasally and (b) intradermally.
Fig. 3.
Weights of animals (in grams) post challenge, measured every 3 days.
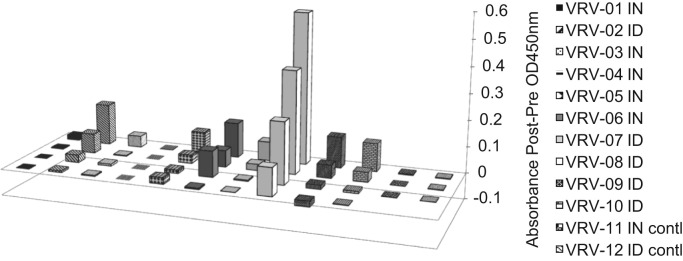
Immunology
ELISA testing for Orthopoxvirus specific antibody indicates seroconversion to O. variola in 9 out of 10 challenged animals at day 21. Of these 9, four were challenged intranasally, and five intradermally ( Fig. 4). Control animals were negative by ELISA. Serum viral neutralization titers were observed in 5 of the challenge animals; two intranasally and 3 challenged intradermally. The highest 50% neutralizing titer (1:154) was observed in two intradermal challenge animals. Positive control (VIG) resulted in a 50% neutralizing titer of 1:6103 ( Table 1).
Fig. 4.
ELISA of anti-Orthopoxvirus antibody in animal sera. Values are reported as post challenge (day 21) minus pre challenge (day 0) absorbance at 450 nm.
Table 1.
Neutralization capacity of sera at day 21 post challenge. Sera collected at day 21 was analyzed for virus neutralization capacity using the array scan system. Titers reported are that which neutralized 50% of the virus titer.
| Sample |
50% neutralizing titer |
|---|---|
| day 21 | |
| VRV-01 IN | <1:40 |
| VRV-02 ID | <1:40 |
| VRV-03 IN | 50.45⁎ |
| VRV-04 IN | <1:40 |
| VRV-05 IN | <1:40 |
| VRV-06 IN | 106 |
| VRV-07 ID | <1:40 |
| VRV-08 ID | 153.6 |
| VRV-09 ID | 48.07 |
| VRV-10 ID | 154 |
| VRV-11 IN contl | <1:40 |
| VRV-12 ID contl | <1:40 |
| Naïve/Prebleeds | <1:40⁎ |
| VIG | 6103a |
Naïve sera and prebleeds from all animals tested <1:40 dilution for 50% viral neutralization.
VIG titer giving 50% viral neutralization; R²=0.9699.
Viral DNA detection
Real time PCR was performed for O. variola specific sequences (A36R), and each sample was tested in triplicate. CT values above 40 are considered negative (see methods). As such, all samples tested were considered negative. A description of the analysis is as follows. PCR results from control animals were negative in all oral swab and tissue samples although certain necropsy samples at day 21 did have PCR results which crossed the threshold after cycle 40 (intranasal control: CT>42 for both lung and spleen; and intradermal control: CT>42 in liver and gonad). Three inoculated animals also showed PCR results which crossed the threshold after cycle 40 in oral swabs. At day 3, oral swabs from two intranasally challenged animals (VRV-04 female, VRV-05 male) and one intradermally challenged animal (VRV-07 female) exhibited CT values ≥42, yet they were not reproducibly seen (<3 of triplicate reactions crossing the threshold). Day 7 oral swab from the intradermal challenged animal (VRV 07) had two of triplicate PCR assays cross the threshold (CT values of 43.53, and 43.77). All other oral swab samples remained negative throughout the study. Tissues collected on day 21 post challenge were also tested for the presence of viral DNA. All tissues did not have PCR assays which crossed the threshold with the exception of three (VRV-07 female, VRV-08 male, VRV-09 male) intradermally challenged animals in lung, spleen, and gonad samples (CT values ≥42 in one of three runs per sample in all tests). The intradermal challenge site (skin) of one animal (VRV-07) exhibited a CT≥42 in all three replicate reactions from day 21 post challenge. No viable virus was cultured from oral swabs or tissue samples (including inoculation site) following two weeks of incubation on cell culture. Although CT levels above 40 are considered negative, the analyses of the results are discussed (below).
Discussion
Historically, laboratory research efforts have tested several animal species for susceptibility to O. variola. To date, using adult animals, only non-human primate models have exhibited overt illness in a manner comparable to smallpox (Hahon and Wilson, 1960, Jahrling et al., 2004, Noble and Rich, 1969). However, the recent studies showing the most significant clinical disease require the intravenous injection of a high infectious dose, (1×108−1×109 pfu). The discovery of a novel, more permissive/representative animal model system may facilitate the development of next-generation smallpox vaccines and therapeutics.
The absence of overt illness in Black-tailed prairie dogs suggests that this host is not permissive for clinical infection by O. variola. However, seroconversion of 9 out of 10 challenged animals to O. variola indicates recognition of the virus by the host immune system and perhaps some level of viral replication. The highest serologic response was observed in an intradermally challenged animal (VRV-08), with all intradermally challenged animals serocoverting, while 4 of 5 intranasally challenged animals seroconverted (Fig. 4). PCR results are negative for all samples tested and all samples were negative for viral growth in tissue culture. PCR values above the threshold (CT>40) in control animals suggests that these are not reflective of viral DNA, but perhaps some other factor causing low signals. In fact, 9/10 challenged animals seroconverted while unchallenged controls did not, suggesting that cross contamination of controls is unlikely and supports CT values above 40 as being negative. Attempts to correlate seroconversion to sex of animals, challenge route or evidence of viral replication (PCR or culture) lack support. Immune induction in 9/10 challenged animals may be considered a measure of viral replication, or viral gene expression to some degree, but the ability to establish viral replication in this host remains speculative since viral DNA was not detected and cultures from animals were negative. And while cynomys species are extremely susceptible to some Orthoxpoxviruses, under the challenge conditions presented here they do not appear to be permissive for overt illness when challenged with O. variola.
Multiple immortalized cell lines are permissive to in vitro infection with O. variola but in vivo host restriction indicates some biological barrier to productive infection (Pirsch et al., 1963). In C. ludivicanus, an increase in challenge dose and/or altered challenge route may facilitate a more robust infection, as observed in non-human primate models. However, our attempt was to develop a model with natural routes of infection and moderate dosing to mimic human smallpox disease onset and sequelae. Additional testing of O. variola in this species to develop a model of human smallpox is not currently being considered. However, understanding the different host responses to O. variola or O. monkeypox infection may enable our understanding of virus host interactions. The results of this study suggest that Black-tailed prairie dogs are not readily susceptible to clinically relevant O. variola infection through traditional and natural routes of infection.
Materials and methods
Laboratory
All work with live O. variola was conducted within the maximum containment laboratory (biosafety level 4) under the Terms of Reference of the WHO Collaborating Center for Smallpox and Other Poxvirus Infections at the World Health Organization (WHO) collaborating center in Atlanta, GA USA. The facility is reviewed for safety and biosecurity practices by independent U.S. and WHO teams on a frequent basis. The work was pre-approved by, and presented to, the WHO Advisory Committee on Variola Virus Research.
Animals
Twelve wild-caught (Colorado) black-tailed prairie dogs (6 females (VRV-02, VRV-04, VRV-06, VRV-07, VRV-10, and VRV-12), 6 males (VRV-01, VRV-03, VRV-05, VRV-08, VRV-09, and VRV-11) were used in this study. The animals were approximately one year old. The animals were topically treated with permethrin prior to transport to the CDC, and were cared for in accordance with the CDC Institutional Animal Care and Use Committee (IACUC) under an IACUC approved protocol (♯ 1729KARPRAC-A2). Animal handling and husbandry was performed by properly trained personnel using biosafety level 4 personal protective equipment (PPE).
Pathogen screening
Animals were screened for Yersinia pestis, Francisella tularensis, Bartonella spp. and Rickettsia spp. by polymerase chain reaction (PCR) as previously described (Stevenson et al., 2003, Kugeler et al., 2006, Sackal et al., 2008). Briefly, these assays use primer sets to target the Bartonella and rickettsial citrate synthase gene (gltA), the F. tularensis pdpD gene, and the Y. pestis pla gene. In addition, serum from these animals taken prior to study start was tested by Enzyme-Linked Immunosorbant Assay (ELISA) to detect IgG antibodies to Orthopoxvirus species.
Diet
The prairie dogs were provided with a commercially available diet (Exotic Nutrition, Newport News VA) and water; both ad libitum. The food is a high fiber formula developed within GMP guidelines to replicate the prairie dogs natural high fiber intake in the wild and contains vitamin D-3, A and E supplements. One or more of the following was provided approximately three times a week for dietary enrichment: either Sugar Beet Treats (Exotic Nutrition), Fruit Kabobs (Exotic Nutrition) containing, fresh sweet potatoes, alfalfa or Timothy Hay (Exotic Nutrition). In addition, the animals were provided with Monkey Biscuits (Exotic Nutrition) as treats on a daily basis as they are an easily measured indicator of inappetance if refused by the animals.
Animal infections and sampling
All animal manipulations were performed on animals, which were sedated using 5% inhalant isoflurane. Control animals (n=2) were sham infected for each route of infection and observed for possible non-specific signs (e.g., inoculation site trauma). Intranasal infection was performed in (n=4) animals with approximately 6.6×106 pfu of purified O. variola strain Solamain (BSH-74-Sol) in total volume of 10 ul (5 ul per nostril) administered with a pipette. Intradermal infection was performed via scarification in (n=4) animals by administration of 6.6×106 pfu in total volume of 10 ul to the skin on the back between the shoulder blades followed by ten intradermal sticks with a tuberculin syringe needle. The animals were observed daily for 21 days for inappetance and general health. For sample collection, animals were anesthetized using 5% isoflurane gas anesthetic in a chamber with maintenance of anesthesia via nosecone and kept on heating blanket to maintain core temperature in accordance with IACUC-approved protocol. The hind limb/groin area was sprayed with 70% isopropanol. A 28-gauge needle was used to collect 1 ml of blood from the saphenous vein. The femoral vein was used only when blood could not be obtained from saphenous vein. Blood was distributed to a serum separation tube (Fisher Scientific) for serum collection. Sera was gamma irradiated at 4.4×106 rads (1 kill dose for Orthopoxvirus) prior to being tested by ELISA and neutralization testing. Animals were bled for serum pre infection and again at day 21. Oral swab and weight of animals were taken pre infection and post challenge on day 3, day 7, day 10, day 14, and day 21. At the conclusion of the study (day 21), all animals were euthanized and necropsy performed to collect lung, liver, gonads and spleen tissues for immunopathology analysis. Animal carcasses were autoclaved and incinerated for disposal.
Real time-PCR and tissue infectivity culture of virus
Samples were assayed by RT-PCR using forward primers, reverse primers and probe complementary to the conserved O. variolaA36R (a viral envelope protein) gene. The primer/probe sequences were selected from a conserved region of A36R (O. variola BSH75_banu, GenBank L22579) with Primer Express (version 1.5; Applied Biosystems). These included A36R forward primer (5′–TTC AGA CTA CCA GTT ATT CTC GGA-3′), A36R reverse primer (5′–AGC CAG GTA GTC AAG ACA TCA GA-3′), and A36R probe (5′FAM-CA AAT TGC GCC ACA GAA TCA TCA AC-BHQ13′). The target sequence is identical in all sequenced strains of O. variola with the exception of a single nucleotide polymorphism within the forward primer sequence of the O. variola CHN48_horn strain. Primers and probe were synthesized in the Biotechnology Core Facility (CDC, Atlanta GA), utilizing standard phosphoramidite chemistry. The detection probe contained 5′ reporter molecule (FAM) and 3′ aminomodifier (Glen Research, Sterling, VA). A 3′ quencher molecule, BHQ1 (Molecular Probes, Eugene, OR), was conjugated to the 3′ amino group after synthesis. PCR assay conditions were optimized according to standard protocols (protocol 04304449, Applied Biosystems, Foster City, CA) by adjusting primer and probe concentrations, and thermal cycling temperatures/duration. Each reaction (30 μL) contained 1× TaqMan Universal PCR Master Mix (Applied Biosystems, Foster City, CA), 1 μl of 25 μmol/μL each primer, 1 μl of 25 μmol/μL TaqMan probe, and 1 μL of template DNA. Thermal cycling conditions for the ABI7900 (Applied Biosystems, Foster City, CA): one cycle of 95 °C for 6 min; followed by 45 cycles of 95 °C for 5 s, and 60 °C for 25 s. PCR amplification is based on fluorescent emission after annealing/elongation (60 °C). O. variola BSH75_banu was used as a positive control. Based on positive controls, CT values were correlated to genome copies with a CT value of 39.3 being equivalent to 20 genome copies and CT value of 42.6 equivalent to 2 genome copies. For this assay, CT values above 40 are considered negative based on reproducibility (among triplicate testing and in duplicate testing) and absence of viral growth in tissue culture (BSC40 cells with 10% RPMI media). Any sample which caused the fluorescent signal to cross the threshold (even if it was after cycle 40) was evaluated for viability by growth in tissue culture.
Enzyme-linked immunosorbant assays (ELISA)
ELISA was used to screen animal sera for the presence of orthopoxvirus specific antibodies as previously described (Hutson et al., 2009). Briefly, microtiter plates (Immulon II) were coated with 100 μl of O. vaccinia (Dryvax purified) at 0.01 μg/well in carbonate buffer overnight at 4 °C followed by formalin inactivation on the plate. Blocking buffer was used (PBS 0.01 M, pH 7.4 (GibcoBRL cat. ♯93-0223 DK)+0.05% tween-20, 5% dried skim milk (DIFCO, ♯232100), 2% normal goat serum (CDC ID♯ CP0523), and 2% bovine serum albumin (Sigma, A-7030)) and test samples were tested using 2 fold dilutions of 1:100, 1:200, 1:400 and 1:800 in assay diluent and incubated for 1 h at 37 °C. A 1:30,000 dilution of Immunopure A/G conjugate (Pierce ImmunoPure® Protein A/G/ Peroxidase conjugated, ♯ 32490) in assay diluent was added for 1 h at 37 °C. Detection was performed with TMB microwell peroxidase substrate (KPL ♯50-76-05) 1-component substrate was added followed by addition of stop solution (KPL ♯50-85-05) Raw absorbance was determined at OD 450 nm. Values reported represent the average of duplicate wells of each dilution run with paired prebleed sample dilution values subtracted. Standard deviation in raw absorbance values between dublicate wells in all samples was <0.035. Positive and negative control sera were used as assay controls.
High content screening-green fluorescent protein (HCS-GFP) neutralization assay
Neutralizing antibody titers against O. vaccinia were measured using a previously validated and described GFP-based assay (Johnson et al., 2008). In brief, Vero E6 Cells were diluted with 10% DMEM from a stock suspension to 1.7×105 cells/mL, seeded into a 96 well flat bottom plate and overnight in a 37 °C CO2 incubator to form a cell monolayer. Serial dilutions of the prairie dog serum samples were made with 2% DMEM. Tubes containing 180 μL of virus (virus only, no serum), and 12 tubes containing 360 μL of media only (no virus or serum) were used as assay controls. WR-GFP O. vaccinia was thawed on ice for 1 h followed by three rounds of sonication and dilution in 2% DMEM. This viral was added (180 μL) to samples and used as plate viral only control. Samples were briefly rocked and placed in a 37 °C CO2 incubator for 2 h, and rocked once every 30 min. The media was carefully removed from the cell monolayer (96 well plate) and replaced with test samples and controls in triplicate (3 wells per sample). After a 2 h incubation, the inoculum was aspirated and replaced with 100 μl of 2% DMEM +46 μg/mL cytosine arabinoside (Ara-C) and then placed in a 37 °C CO2 incubator for 18 h. The cells were formalin fixed and stained with DAPI (3 mM). Two channel analysis was performed for DAPI and GFP signals. The plate was analyzed on the Array Scan HCS Reader with the target acquisition software from Cellomics (Thermo Scientific: Cellomics, Pennsylvania). Prism 5.0 (GraphPad) was used to confirm the Gaussian distribution of our data. Because the data passed the D'Agostino-Pearson omnibus test, which measures the deviation from a predicted Gaussian distribution by skewness (asymmetry) and kurtosis (shape), further statistics were performed assuming a Gaussian “normal” distribution. The column statistics option was used to determine means, medians, standard deviations, and standard error from the mean measurements of our data. Additional statistics utilized in this paper include one-tailed t-tests.
Acknowledgments
The authors would like to acknowledge the assistance of the following individuals in accomplishing this project: Allison Williams DVM and Eddie Jackson of the Roybal ARB staff for animal husbandry. This work was funded through program funds at the poxvirus program in the Centers for Disease Control and Prevention. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
- Brinckerhoff W.R., Tyzzer E.E. Studies upon the Immunity Reactions of the Monkey after Inoculation with Vaccine or with Variola Virus: Part III. J. Med. Res. 1906;14:321–339. [PMC free article] [PubMed] [Google Scholar]
- Chapman J.L., Nichols D.K., Martinez M.J., Raymond J.W. Animal models of orthopoxvirus infection. Vet. Pathol. 2010;47:852–870. doi: 10.1177/0300985810378649. [DOI] [PubMed] [Google Scholar]
- Dyall J., Johnson R.F., Chen D.Y., Huzella L., Ragland D.R., Mollura D.J., Byrum R., Reba R.C., Jennings G., Jahrling P.B., Blaney J.E., Paragas J. Evaluation of monkeypox disease progression by molecular imaging. J. Infect. Dis. 2011;204:1902–1911. doi: 10.1093/infdis/jir663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff A.J., Chapman J., Foster C., Wlazlowski C., Shamblin J., Lin K., Kreiselmeier N., Mucker E., Paragas J., Lawler J., Hensley L. A novel respiratory model of infection with monkeypox virus in Cynomolgus macaques. J. Virol. 2011;85:4898–4909. doi: 10.1128/JVI.02525-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahon N., Wilson B.J. Pathogenesis of variola in Macaca irus monkeys. Am. J. Hyg. 1960;71:69–80. doi: 10.1093/oxfordjournals.aje.a120091. [DOI] [PubMed] [Google Scholar]
- Hutson C.L., Olson V.A., Carroll D.S., Abel J.A., Hughes C.M., Braden Z.H., Weiss S., Self J., Osorio J.E., Hudson P.N., Dillon M., Karem K.L., Damon I.K., Regnery R.L. A prairie dog animal model of systemic orthopoxvirus disease using West African and Congo Basin strains of monkeypox virus. J. Gen. Virol. 2009;90:323–333. doi: 10.1099/vir.0.005108-0. [DOI] [PubMed] [Google Scholar]
- Jahrling P.B., Hensley L.E., Martinez M.J., Leduc J.W., Rubins K.H., Relman D.A., Huggins J.W. Exploring the potential of variola virus infection of Cynomolgus macaques as a model for human smallpox. Proc. Natl. Acad. Sci. USA. 2004;101:15196–15200. doi: 10.1073/pnas.0405954101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.C., Damon I.K., Karem K.L. A rapid, high-throughput vaccinia virus neutralization assay for testing smallpox vaccine efficacy based on detection of green fluorescent protein. J. Virol. Methods. 2008;150:14–20. doi: 10.1016/j.jviromet.2008.02.009. [DOI] [PubMed] [Google Scholar]
- Kugeler K.J., Pappert R., Zhou Y., Petersen J.M. Real-time PCR for Francisella tularensis types A and B. Emerg. Infect. Dis. 2006;12:1799–1801. doi: 10.3201/eid1211.060629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayr A., Herrlich A. Cultivation of the variola virus in the infantile mouse. Arch. Gesamte. Virusforsch. 1960;10:226–235. [PubMed] [Google Scholar]
- Murti B.R., Shrivastav J.B. A study of biological behaviour of variola virus. II. Experimental inoculation of laboratory animals. Indian J. Med. Sci. 1957;11:580–587. [PubMed] [Google Scholar]
- Nalca A., Livingston V.A., Garza N.L., Zumbrun E.E., Frick O.M., Chapman J.L., Hartings J.M. Experimental infection of Cynomolgus macaques (Macaca fascicularis) with aerosolized monkeypox virus. PloS One. 2010;5 doi: 10.1371/journal.pone.0012880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble, J., Jr., Rich J.A. Transmission of smallpox by contact and by aerosol routes in Macaca irus. Bull. WHO. 1969;40:279–286. [PMC free article] [PubMed] [Google Scholar]
- Pirsch J.B., Mika L.A., Purlson E.H. Growth characteristics of variola virus in tissue culture. J. Infect. Dis. 1963;113:170–178. doi: 10.1093/infdis/113.3.170. [DOI] [PubMed] [Google Scholar]
- Reed K.D., Melski J.W., Graham M.B., Regnery R.L., Sotir M.J., Wegner M.V., Kazmierczak J.J., Stratman E.J., Li Y., Fairley J.A., Swain G.R., Olson V.A., Sargent E.K., Kehl S.C., Frace M.A., Kline R., Foldy S.L., Davis J.P., Damon I.K. The detection of monkeypox in humans in the Western Hemisphere. N. Engl. J. Med. 2004;350:342–350. doi: 10.1056/NEJMoa032299. [DOI] [PubMed] [Google Scholar]
- Reynolds M.G., Yorita K.L., Kuehnert M.J., Davidson W.B., Huhn G.D., Holman R.C., Damon I.K. Clinical manifestations of human monkeypox influenced by route of infection. J. Infect. Dis. 2006;194:773–780. doi: 10.1086/505880. [DOI] [PubMed] [Google Scholar]
- Sackal C., Laudisoit A., Kosoy M., Massung R., Eremeeva M.E., Karpathy S.E., Van Wyk K., Gabitzsch E., Zeidner N.S. Bartonella spp. and Rickettsia felis in fleas, Democratic Republic of Congo. Emerg. Infect. Dis. 2008;14:1972–1974. doi: 10.3201/eid1412.080610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson H.L., Bai Y., Kosoy M.Y., Montenieri J.A., Lowell J.L., Chu M.C., Gage K.L. Detection of novel Bartonella strains and Yersinia pestis in prairie dogs and their fleas (Siphonaptera: Ceratophyllidae and Pulicidae) using multiplex polymerase chain reaction. J. Med. Entomol. 2003;40:329–337. doi: 10.1603/0022-2585-40.3.329. [DOI] [PubMed] [Google Scholar]