Dear Editor,
The most recent and extensive non-endemic outbreak of monkeypox virus (MPXV) has just occurred. In contrast to previous outbreaks, this one lacks a clear link between infected people or a common source of viral exposure (such as travel to endemic areas or contact with infected animals). The dynamics of infection transmission are still unknown. The World Health Organization (WHO) has raised the risk of MPXV infection to the highest level for public health. The WHO's delay in releasing a statement regarding the recent spread of MPXV outside of Africa demonstrates a disregard for developing countries, particularly in Africa, and even certain groups of people with specific sexual tendency, because time is important in epidemics. Surprisingly, homosexual males contact (MSM) has been confirmed as the most recent route of infection, although that is not a sexually transmitted disease. The true risk associated with this issue is that as monkeypox virus spread to other countries around the globe, it may ultimately to endemic infect gay and bisexual men on a continuing basis, which in many ways will promote it to spread even further quickly among wild populations (mostly rodents) [1,2]. Therefore, using the knowledge we have acquired about infectious diseases with the potential for epidemics, particularly HIV-gay related immunodeficiency (GRID), we attempted to address the issue of monkeypox virus interference with HIV infection, and to clarify whether or not MPXV through the sexual route can be effective in immunodeficiency conditions. The sexual route is one of the “microbiome exchanges” routes. In actuality, interactions between the pathogen and the host lead to sexually transmitted diseases [3]. Although MPXV should not be regarded as a sexually transmitted infection, it is nevertheless necessary to identify current knowledge gaps by comprehending the interference or competition between pathogens in previous outbreaks to present. As a result, a variety of factors have contributed to the spread of the monkeypox virus that has the potential to become an epidemic, including: 1. the cessation of smallpox vaccination resulting in a susceptible population; 2. a loss of immunization and para immunization; 3. an increase in risky behavior and a shift in human lifestyles; 4. an increase in number of immunocompromised people; 5. changes in virus properties; 6. re-emergence of pathogens with unusual transmission routes; 7. change of paratope-epitope link; 8. waning of cross- and extensive immunity; and 9. increase animal hosts. All have increased the efficiency of transmission of monkeypox from humans to humans which might be a potential public health threat on a large scale [[4], [5], [6]]. Humanity has learned from the COVID-19 era that there is always a chance that red-alert infections will reappear. The simultaneous circulation of infectious agents can result in unusual competitive or cooperative interactions amongst pathogens. It can influence how associated diseases spread through the population and shape the epidemiological patterns of related infections. There has been no simultaneous outbreak of smallpox and monkeypox virus, and host adaptation, alteration ecological, genetic changes, with a significant rise in number of people with immunodeficiency disorders including HIV/AIDS, and the rise in sexually transmitted diseases have all contributed to a higher prevalence of MPXV outside of the African continent. Men who have sex with each other (MSM) are more likely to contract pathogen-based sexually transmitted diseases (STDs) due to a combination of behavioral and biological variables [7,8]. With more than 50 countries now reporting MPXV cases, its 2022 outbreak is just as dangerous as the HIV pandemic or the COVID-19 pandemic. Despite the lab-leak hypothesis of COVID-19, all three of the examples cited are zoonotic infections that have jumped from animal hosts to human populations [9]. This serves as a reminder that these occurrences still take effect. Many members of the MSM group have never heard of atypical clinical manifestations of the monkeypox virus or other STDs. The fact that there is now no credible proof that MPXV can be transferred sexually highlights the scientific gap as to why such cases should continue to arise. On the other hand, little is known about the prevalence of monkeypox worldwide. It is necessary to know what factors have caused the unprecedented spread of MPXV. How concerned should we be about HIV/ADIS and MPXV (Fig. 1 )? For the spread of the monkeypox virus and other infectious diseases, HIV GRID serves as a cautionary tale [[10], [11], [12]]. Awareness and training campaigns should be developed for these situations because we must be aware of the enormous risks of sexual transmission and refrain from stigmatizing certain groups of society, such as the LGBT family [13]. Out of 118 confirmed cases of MPXV in the study by Ogunleye et al. [14], seven patients died 58 from the monkeypox virus, four had HIV and were not receiving antiretroviral therapy (ART). However, it is still unclear how many individuals were HIV and monkeypox virus infected. In the study by Ogoina et al. [15], confirmed cases of MPXV/HIV had skin rashes, vaginal sores, or secondary bacterial infections that lasted noticeably longer. 14 of the 27 MSM cases that were confirmed in Portugal were HIV positive [16]. Although there is currently little information available, factors including high CD4 levels, undetectable viral loads, and ART regimens lower the chance that patients may experience severe infection events. Although there is not a definite biological sign of monkeypox virus risk in gay men, it may still spread through social interactions and interpersonal relationships. In theory, the recent outbreak of monkeypox virus has challenged our earlier hypotheses and established it as a variable virus in both its rate of transmission and mutation [17]. As an animal model of variola infection in humans, monkeypox virus (MPXV) infection of non-human primates (NHPs) is being researched and developed. Identification of inflammatory patterns has always been crucial for predicting progression of MPXV using biomarkers. In the interim, non-specific biomarkers that can estimate the risk of monkeypox infection such as, fluorine-18 fluorodeoxyglucose (FDG), a biomarker of immune activation and inflammation have been used [18]. Dyall et al. [19] revealed that NPHs survived the challenge and demonstrated significant FDG absorption in axillary lymph nodes while having no clinical symptoms of the illness. This suggests a link between activation of pre-existing immunity and survival and better reflects the temporal progression of the disease in humans. Recent outbreaks of monkeypox outside of Africa have led to a more complete clinical description of risk factors for MPXV transmission. The imaging of inflammation patterns in infectious sites and immune system activation can be linked to disease severity with FDG allows for the rapid detection and localization of inflammation foci with a high sensitivity. The use of biomarkers of inflammation/infection helps to develop predictive algorithms for early detection and evaluation of infection which seems to be important for MPXV because, as a consequence of the antigenic affinity of orthopoxviruses, existing vaccinations employed in the smallpox eradication program induce cross immunity against MPXV infection. On the other hand, because smallpox was successfully eradicated, it was not necessary to maintain immunization, which resulted in an unimmunized population that is susceptible to MPXV. Therefore, finding new antiviral drugs that are effective therapeutic targets is imperative [[20], [21], [22]]. The monkeypox virus is a zoonotic infection that has long been neglected. Its recent outbreak has drawn a lot of attention to the development of newer preventative and therapeutic approaches. Applying the lessons learned from the COVID-19 pandemic will help with MPXV management. Although we are only beginning to comprehend these consequences in life, human activities and behavior trigger evolutionary dynamics that facilitate emergence and reemergence of viruses.
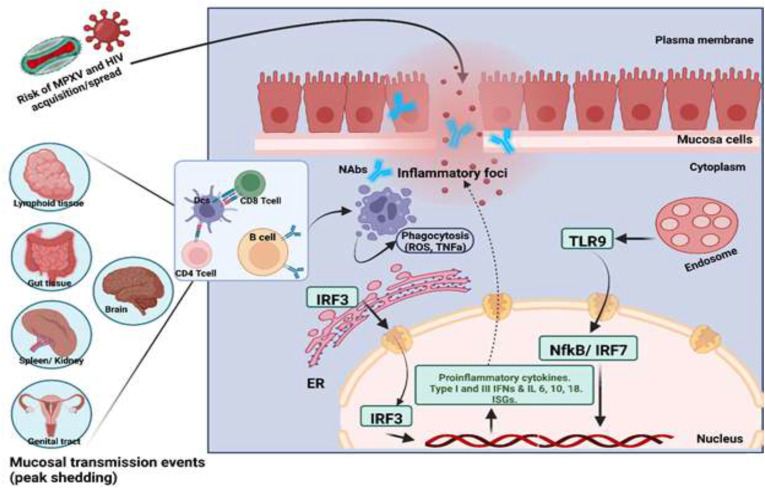
Fig. 1.
HIV infection risk and immune protection against MPXV infection. Antigen presenting cells (APCs) are recruited due to the release of proinflammatory cytokines and chemokines by activated keratinocytes. Monkeypox virus and HIV are both known to be risk factors for inflammation. APCs are activated in local lymph nodes and help activate CD8+, CD4+, and B cells specific to the antigen. Both can spread from APCs to T cells using immune cell trafficking. The inflammatory state also triggers natural killer cells and other innate immune responses. Inflammation causes the invasion of CD4+ T cells, which help clear the virus and serve as HIV target cells, and CD8+ T cells kill virus-infected cells. Neutralizing antibodies (NAbs) are secreted by plasma cells, neutralizing MPXV and preventing the infection from spreading. Dendritic cells (DCs) and macrophages cause apoptosis and phagocytosis, produce anti-inflammatory mediators, and begin the healing process. The monkeypox virus's genome causes several downstream factors to release interferons (IFN I & III), cytokines, and interleukins (IL 1, 6, 10, 18) for an active antiviral immune response during an infection.
Abbreviations: TLR9: toll-like receptor 9, IFN: interferons, CK: cytokines, NF-κB: nuclear factor κB, IRF 3 & 7: interferon regulatory factor 3 & 7, IL: interleukin, ISGs: IFN stimulating genes, ER: endoplasmic reticulum.
Ethical approval
This article does not require any human/animal subjects to acquire such approval.
Sources of funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contribution
Milad Zandi: Conceptualization, Data Curation, Writing -Original Draft, Writing - review & editing. Maryam Shafaati: Writing - Original Draft, Data Curation. Om PrakashChoudhary: Review & editing. All authors critically reviewed and approved the final version of the manuscript.
Research registration Unique Identifying number (UIN)
-
1.
Name of the registry: Not applicable.
-
2.
Unique Identifying number or registration ID: Not applicable.
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): Not applicable.
Guarantor
Milad Zandi, PhD in medical virology, senior researcher in emerging and re-emerging viruses, Department of Virology, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. Tel: +989372876578, Email. Miladzandi416@gmail.com.
Data statement
The data in this correspondence article is not sensitive in nature and is accessible in the public domain. The data is therefore available and not of a confidential nature.
Provenance and peer review
Not commissioned, internally peer-reviewed.
Declaration of competing interest
All authors report no conflicts of interest relevant to this article.
References
- 1.Liu X., Zhu Z., He Y., Lim J.W., Lane B., Wang H., et al. Monkeypox claims new victims: the outbreak in 100 men who have sex with men. Infect Dis. Poverty. 2022;11(1):1–3. doi: 10.1186/s40249-022-01007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kmiec D., Kirchhoff F. Monkeypox: a new threat? Int. J. Mol. Sci. 2022;23(14):7866. doi: 10.3390/ijms23147866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bragazzi N.L., Kong J.D., Wu J. ResearchGate Project; 2022. A Tale of Two (And More) Stories: Smallpox-Monkeypox Viruses (HIV, and Other Sexually Transmitted Disesases) Interaction Dynamics. 2022 Monkeypox Epidemic. [Google Scholar]
- 4.Einav T., Cleary B. Extrapolating missing antibody-virus measurements across serological studies. Cell Syst. 2022:561–573. doi: 10.1016/j.cels.2022.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Okyay R.A., Bayrak E., Kaya E., Şahin A.R., Koçyiğit B.F., Taşdoğan A.M., et al. Another epidemic in the shadow of Covid 19 pandemic: a review of monkeypox. Proteins. 2022;7:10. [Google Scholar]
- 6.Segredo-Otero E, Sanjuán R. Cooperative Virus-Virus Interactions: an Evolutionary Perspective 2. [DOI] [PMC free article] [PubMed]
- 7.Schneider K.A., Eichner M. Does it matter who is spreading monkeypox? Lancet Infect. Dis. 2022 doi: 10.1016/S1473-3099(22)00431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaler J., Hussain A., Flores G., Kheiri S., Desrosiers D. Monkeypox: a comprehensive review of transmission, pathogenesis, and manifestation. Cureus. 2022;14(7) doi: 10.7759/cureus.26531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu F., Li L., Che D. Monkeypox virus under COVID-19: caution for sexual transmission–Correspondence. Int. J. Surg. 2022;104 doi: 10.1016/j.ijsu.2022.106768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Antinori A., Mazzotta V., Vita S., Carletti F., Tacconi D., Lapini L.E., et al. Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy. Euro Surveill. 2022;27(22) doi: 10.2807/1560-7917.ES.2022.27.22.2200421. May 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hammerschlag Y., MacLeod G., Papadakis G., Sanchez A.A., Druce J., Taiaroa G., et al. Monkeypox infection presenting as genital rash, Australia. Euro Surveill. 2022;27(22) doi: 10.2807/1560-7917.ES.2022.27.22.2200411. May 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bížová B., Veselý D., Trojánek M., Rob F. Coinfection of syphilis and monkeypox in HIV positive man in Prague, Czech Republic. Trav. Med. Infect. Dis. 2022 doi: 10.1016/j.tmaid.2022.102368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gonsalves G.S., Mayer K., Beyrer C. Déjà vu all over again? Emergent monkeypox, delayed responses, and stigmatized populations. J. Urban Health. 2022:1–4. doi: 10.1007/s11524-022-00671-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yinka-Ogunleye A., Aruna O., Dalhat M., Ogoina D., McCollum A., Disu Y., et al. Outbreak of human monkeypox in Nigeria in 2017–18: a clinical and epidemiological report. Lancet Infect. Dis. 2019;19(8):872–879. doi: 10.1016/S1473-3099(19)30294-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ogoina D., Iroezindu M., James H.I., Oladokun R., Yinka-Ogunleye A., Wakama P., et al. Clinical course and outcome of human monkeypox in Nigeria. Clin. Infect. Dis. 2020;71(8):e210–e214. doi: 10.1093/cid/ciaa143. [DOI] [PubMed] [Google Scholar]
- 16.Duque M.P., Ribeiro S., Martins J.V., Casaca P., Leite P.P., Tavares M., et al. Ongoing monkeypox virus outbreak, Portugal, 29 April to 23 May 2022. Euro Surveill. 2022;27(22):2200424–2200426. doi: 10.2807/1560-7917.ES.2022.27.22.2200424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shafaati M., Zandi M. Monkeypox virus neurological manifestations in comparison to other orthopoxviruses. Trav. Med. Infect. Dis. 2022 doi: 10.1016/j.tmaid.2022.102414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saijo M., Ami Y., Suzaki Y., Nagata N., Iwata N., Hasegawa H., et al. Virulence and pathophysiology of the Congo Basin and West African strains of monkeypox virus in non-human primates. J. Gen. Virol. 2009;90(9):2266–2271. doi: 10.1099/vir.0.010207-0. [DOI] [PubMed] [Google Scholar]
- 19.Dyall J., Johnson R.F., Chen D.-Y., Huzella L., Ragland D.R., Mollura D.J., et al. Evaluation of monkeypox disease progression by molecular imaging. J. Infect. Dis. 2011;204(12):1902–1911. doi: 10.1093/infdis/jir663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stittelaar K.J., van Amerongen G., Kondova I., Kuiken T., van Lavieren R.F., Pistoor F.H., et al. Modified vaccinia virus Ankara protects macaques against respiratory challenge with monkeypox virus. J. Virol. 2005;79(12):7845–7851. doi: 10.1128/JVI.79.12.7845-7851.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scharko A.M., Perlman S.B., Pw2nd H., Hanson J.M., Uno H., Pauza C.D. Whole body positron emission tomography imaging of simian immunodeficiency virus-infected rhesus macaques. Proc. Natl. Acad. Sci. USA. 1996;93(13):6425–6430. doi: 10.1073/pnas.93.13.6425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reynolds M.G., Yorita K.L., Kuehnert M.J., Davidson W.B., Huhn G.D., Holman R.C., et al. Clinical manifestations of human monkeypox influenced by route of infection. J. Infect. Dis. 2006;194(6):773–780. doi: 10.1086/505880. [DOI] [PubMed] [Google Scholar]