Abstract
Background
Monkeypox is a zoonosis caused by an Orthopoxvirus of the Poxviridae family. Human infections are often severe and are a public health problem.
Patients and method
We conducted a monkeypox outbreak investigation of suspected case patients in five villages of the Alindao-Mingala Health District following blood sample confirmation of the virus by the Institut Pasteur in Bangui. We aimed to determine disease characteristics, to describe the context and the risk factors, and to measure the incidence and case fatality. Patients were reported in the villages of Rehou 4, 5, Dalakere 1, Kongbo, and Pavika from August to October 2016. Data was collected on individual records when interviewing patients or parents.
Results
A total of 26 patients were identified. The ˂ 10 years and 21–30 years age groups were the most affected. The overall attack rate was 5 per 1000 inhabitants and the case fatality was 7.7%. Young age and the absence of smallpox vaccination were associated with severe presentations in 87.5% of cases.
Conclusion
The annual number of monkeypox outbreaks increases in the Central African Republic with severe presentations and a high case fatality especially in children. Reinforcing the surveillance and characterization of circulating strains will provide information on the need for vaccine production.
Keywords: Monkeypox, Outbreak, Zoonoses
Résumé
Contexte
Le monkeypox est une zoonose due à un Orthopoxvirus de la famille des Poxviridae. L’infection humaine est souvent grave et constitue un problème de santé publique.
Patients et méthodes
Une investigation d’épidémie de monkeypox a été réalisée dans le district sanitaire d’Alindao-Mingala, République centre Africaine, autour des cas suspects de cinq villages suite à la confirmation du virus par l’institut Pasteur de Bangui sur prélèvements sanguins. L’objectif était de déterminer les caractéristiques de la maladie, décrire le contexte et les facteurs favorisants et déterminer l’incidence et la létalité. Les cas ont été recensés dans les villages de Rehou 4, 5, Dalakere 1, Kongbo et Pavika d’août à octobre 2016. Les données ont été collectées sur une fiche individuelle par interview des patients et parents.
Résultats
Au total, 26 patients ont été recensés. Les tranches d’âge de moins de 10 ans et de 21–30 ans étaient les plus touchées. Le taux d’attaque global était de 5 pour 1000 habitants et la létalité de 7,7 %. Le jeune âge et l’absence de vaccination contre la variole étaient associés aux formes graves de la maladie dans 87,5 % des cas.
Conclusion
Le nombre annuel de flambée épidémique de monkeypox augmente en République centrafricaine avec des formes graves et une forte létalité en particulier chez les enfants. Le renforcement de la surveillance et la caractérisation des souches circulantes pourront donner des informations sur la nécessité d’une production de vaccin.
Mots clés: Monkeypox, Épidémie, Zoonose
1. Introduction
Monkeypox has the same clinical presentations as smallpox [1]. Its case fatality reaches 17% and is well below that of smallpox (25%–40%) [2].
Monkeypox is a zoonosis caused by Orthopoxvirus. The monkeypox virus was fortuitously isolated in 1958 from Asian macaques exported to Denmark [3]. Human infections were first reported in Central Africa in 1970 [3], [4]. The monkeypox virus was first isolated from humans in 1970 in the Democratic Republic of the Congo (DRC) [3]. Monkeypox is an endemic disease in the Congo River basin and in West Africa. From 1970 to 1996, human cases of monkeypox were reported in the DRC, Nigeria, Ivory Coast, Liberia, and Sierra Leone, followed by the Central African Republic (CAR) and Gabon [5].
The first human cases of monkeypox observed outside the African continent were reported in 2003 in the Midwestern United States [1], [6], [7]. American patients had been infected through direct contact with pets, especially prairie dogs (Cynomys species) which had been infected through contact with various rodents imported from Ghana [5], [8].
The geographical distribution of monkeypox expanded to South Sudan, East Africa, in 2005.
The known reservoir of the monkeypox virus includes rodents (tree-dwelling squirrels, Gambian pouched rat, and elephant shrew; these animals are actively hunted in Central Africa as they represent a significant source of food) as well as great apes.
An outbreak of monkeypox occurred in the South-East of CAR in the Haute-Kotto prefecture, i.e. in the district of Bangassou between December 2015 and February 2016.
We report a second monkeypox outbreak which simultaneously occurred from August to October 2016 in three villages of the Health District of Alindao-Mingala, which is occupied by armed groups.
2. The outbreak
A health warning issued on September 6, 2016 by the healthcare facility of Irrabanda (Haute-Kotto prefecture) notified several cases of eruptive fever associated with deaths in the villages of Rehou 4 and Dalakere 1 (Health District of Alindao-Mingala). A first exploratory investigation was conducted on September 7 and 8, 2016 in the area of Irrabanda by a team made of members of the non-governmental organization (NGO) International Medical Corps (IMC) and members of the Ministry of Health. Team members identified six hospitalized patients and three blood samples were collected and sent to the Institut Pasteur in Bangui (IPB).
Another investigation was carried out by the Cordaid NGO, which is based in Alindao, from September 11 to 13, 2016 in the villages of Rehou 4 and 5 and Dalakere 1. The investigation team collected blood samples from four of the six suspected case patients of the village of Rehou 4. Following confirmation of monkeypox diagnosis by the IPB laboratory for these four tested patients, the Ministry of Health officially declared the monkeypox outbreak on September 23, 2016. Three additional suspected case patients were at that same time isolated in the hospital of the Alindao district; these patients were from Kongbo and Pavika villages.
From October 2 to 4, 2016, a team made of epidemiologists, public health physicians, clinicians, communication and epidemiological surveillance experts, and logisticians investigated the outbreak in the villages of Rehou 4, Rehou 5, Dalakere 1, Ngbanda (Kongbo), and Pavika.
3. Materials and method
Cases were identified using the consultation and hospitalization registers of healthcare facilities. An active investigation to detect any new case patient was carried out in the villages of Rehou 4, 5, Dalakere 1, Kongbo, and Pavika.
A suspected case of monkeypox was defined as any individual living in the district of Alindao as of July 15, 2016 and presenting with fever and vesicular or pustular skin rash.
A confirmed case of monkeypox was defined as any suspected case patient whose laboratory samples analysis by the IPB confirmed the presence of the monkeypox virus by PCR or virus isolation on baby mouse brain cell culture [9].
A severe case was defined by non-specific skin rash associated with other signs and symptoms such as dysphagia, myalgia, headaches (etc.), requiring hospitalization.
A primary case of monkeypox was defined as any patient without any prior contact with an infected patient (confirmed case) in the 21 days preceding the infection onset.
A secondary case of monkeypox was defined as any patient who had been in contact with another patient during the period running from the 7th to the 21st day preceding the infection onset.
Data was collected through interviews and using a form including the following sections: patient identification, clinical signs, risk factors (contact with a patient, no vaccination against smallpox), outcome, date of infection onset, and primary or secondary status. The form was used with all suspected case patients. The interview was carried out with patients and with parents of children. Data was analyzed using the EpiInfo7 and Excel 2007 software.
4. Results
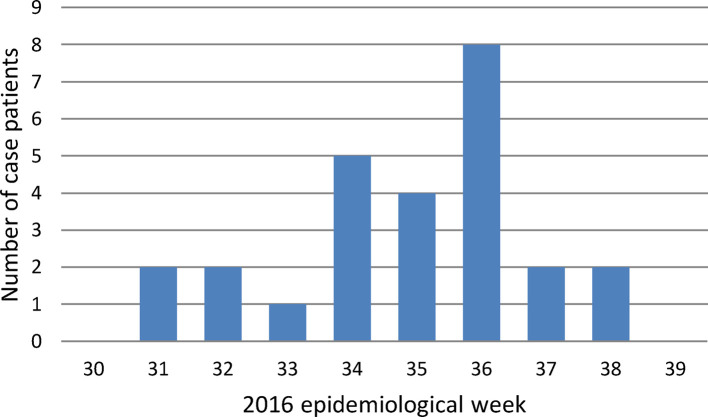
The outbreak took place between August and October 2016, i.e. over the epidemiological weeks 31–38 (Fig. 1 ). The epicenter of the outbreak was the village of Rehou 4, where the index case patient was from. This patient was a hunter and farmer, just like many other inhabitants of the village. He had consumed meat which came from the Xerus erythropus species of squirrels, found dead in the forest. The infection spread among the village as well as to nearby villages (Dalakere 1 and Rehou 5) following this patient's burial. A total of 458 inhabitants lived in the village of Rehou 4. The three cases observed in the villages of Pavika and Ngbanda were sporadic cases without any link with those of Rehou 4. A total of 23 case patients (88.5%) were secondary cases, i.e. all cases observed in Rehou 4, Rehou 5, and Dalakere 1.
Fig. 1.
Number of monkeypox case patients per week in the district of Alindao-Mingala, August–September 2016. The outbreak peaked on Week 36 (8 patients). The curve indicates the human-to-human transmission of the infection. The incubation period was about two weeks.
Le pic de l’épidémie se situait à la 36e semaine (8 cas). La courbe indique une transmission interhumaine de la maladie. La période d’incubation était d’environ 2 semaines.
Overall, 26 case patients were reported. The blood samples of seven of these patients were sent to the IPB: the first three were positive by PCR. More than half of patients (61.5%) had been hospitalized. Five of the 26 patients (19.2%) had the smallpox vaccination scar. The others were too young for having received the smallpox vaccine. Male patients accounted for 53.8% of all 26 patients.
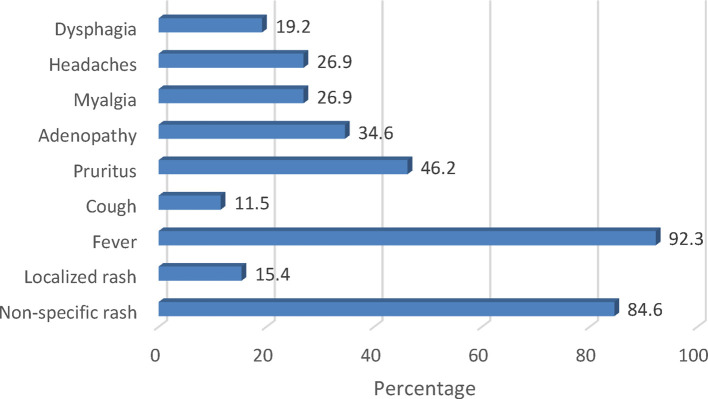
The median age was 24 years (range: 12 months–58 years). The ˂ 10 years and 21–30 years age groups were the most affected (Table 1 ). Apart from fever and skin rash observed in all case patients (as per the case definition), pruritus and cervical and/or inguinal adenopathy were observed in 46.2% and 34.6% of patients, respectively (Fig. 2, Fig. 3 ).
Table 1.
Distribution of monkeypox case patients by age groups in the district of Alindao-Mingala between August and September 2016.
Répartition des patients atteints de monkeypox par tranches d’âge dans le district d’Alindao-Mingala entre août et septembre 2016.
| Age | Number | % |
|---|---|---|
| 0–10 | 8 | 30.80% |
| 11–20 | 4 | 15.40% |
| 21–30 | 6 | 23.10% |
| 31–40 | 3 | 11.50% |
| 41–50 | 2 | 7.70% |
| 51 et + | 3 | 11.50% |
| Total | 26 | 100 |
Fig. 2.
Symptoms of monkeypox in the district of Alindao-Mingala, August to September 2016. Fever and non-specific skin rash were the predominant signs observed.
La fièvre et l’éruption généralisée étaient les signes cliniques dominants. ADP : adénopathie.
Fig. 3.
Features of monkeypox skin rash in a woman and an infant living in Rehou 4 in 2016.
Caractéristiques des éruptions du monkeypox chez une femme et un nourrisson habitant Rehou 4 en 2016.
The index case patient (36 years old) and a 12-month-old infant died.
The overall attack rate (AR) was 5 per 1000 inhabitants. The highest attack rate was observed in Rehou 4 (epicenter of the outbreak) (37.1 per 1000 inhabitants) and in the nearby village of Rehou 5. Unvaccinated patients had a higher AR (3.6%) than vaccinated patients (0.95 per 1000 inhabitants) (Table 2 ).
Table 2.
Determination of the attack rate of monkeypox by village in the district of Alindao-Mingala, August–September 2016.
Détermination du taux d’attaque (pour 1000 habitants) de monkeypox par village dans le district d’Alindao-Mingala, août–septembre 2016.
| Villages | Population | Overall attack rate |
Attack rate by vaccination status |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Case patient | Attack rate | Vaccinated | Attack rate | Non-vaccinated | Attack rate | Unknown | Attack rate | ||
| Rehou 4 | 458 | 17 | 37.1 | 4 | 8.7 | 11 | 24 | 2 | 4.6 |
| Rehou 5 | 133 | 4 | 30.1 | 1 | 7.5 | 3 | 22.6 | 0 | 0 |
| Dalakere 1 | 330 | 2 | 6.1 | 0 | 0 | 2 | 6 | 0 | 0 |
| Pavica 3 | 827 | 1 | 1.2 | 0 | 0 | 1 | 1.2 | 0 | 0 |
| Ngbada | 1483 | 2 | 1.3 | 0 | 0 | 2 | 1.3 | 0 | 0 |
| Total | 5246 | 26 | 5 | 5 | 0.95 | 19 | 3.6 | 2 | 0.4 |
The highest number of cases was observed in the epicenter of the outbreak, i.e. Rehou 4 (65.4%). The overall case fatality was 7.7%. A 50% case fatality was observed in the village of Dalakere 1 (Table 3 ). Severe presentations accounted for 61.5% of cases, including 87.5% of unvaccinated patients against smallpox (Table 4 ).
Table 3.
Distribution of monkeypox case patients by village in the district of Alindao-Mingala, August–September 2016.
Répartition des cas de monkeypox par village dans le district d’Alindao-Mingala, août–septembre 2016.
| Villages | Case patients |
|
|---|---|---|
| Number | % | |
| Rehou 4 | 17 | 65.40% |
| Rehou 5 | 4 | 15.40% |
| Dalakere 1 | 2 | 7.70% |
| Ngbanda | 2 | 7.70% |
| Pavika 3 | 1 | 3.80% |
| Total | 26 | 100% |
Table 4.
Clinical presentations of the disease by vaccination status.
Formes cliniques de la maladie selon le statut vaccinal.
| Status | Severe presentation |
Mild presentation |
||
|---|---|---|---|---|
| Case patient | % | Case patient | % | |
| Vaccinated | 0 | 0 | 5 | 50 |
| Non-vaccinated | 14 | 87.5 | 5 | 50 |
| Unknown | 2 | 12.5 | 0 | 0 |
| Total | 16 | 61.5 | 10 | 38.5 |
5. Discussion
Unlike previous outbreaks of monkeypox in CAR, the outbreak observed in Bangassou and Alindao in 2016 affected many more individuals [10]. Most cases reported in the literature involve children [3], [11]. This well-known risk factor may be due to the lower resistance of infants to infections. However, it also reveals that the only people still likely to have smallpox antibodies–which are partly effective against monkeypox–are now adults aged over 40 years [12].
The symptoms observed in our patients were common and similar to those reported in the literature: skin lesions, headaches, fever, sweats, chills, persistent cough, adenopathy, and sore throat [7]. However, monkeypox lesions may look like chicken-pox skin rash which is quite common in children worldwide. Recent studies of monkeypox in Central Africa suggest that the varicella zoster virus is frequently mistaken for monkeypox. More than 50% of suspected cases of monkeypox reported in these studies were actually chicken-pox cases [13], [14]. An accurate diagnosis is therefore difficult based on the sole clinical symptoms. Laboratory testing is therefore fundamental in confirming the diagnosis of eruptive diseases.
Monkeypox outbreaks observed in CAR occur in geographical areas close to one another. The 2015 and 2016 outbreaks were observed within the same Health Prefecture and two neighboring districts (Bangassou and Alindao-Mingala). These districts are located in a forest with a high reservoir prevalence which is ideal for monkeypox virus circulation [15]. The monkeypox outbreak area is located at the border with the DRC, where the epicenter of the outbreak was located. The trade between CAR and the DRC, as well as population movements following the various armed conflicts in these countries, increase the likelihood of outbreaks.
The increasing number of identified human cases of monkeypox may be due to several factors such as the continuous effort to improve surveillance, the pressure on the environment, and the urbanization of reservoir areas for monkeypox [11]. The most likely risk factor in CAR is hunting and deforestation for pastoral purposes. All monkeypox outbreaks observed in CAR occurred in families of hunters. Investigations always indicated monkey or rodent meat consumption by family members of the index case patient.
Although first reported in CAR a while ago, the population and healthcare professionals are still poorly aware of monkeypox. It is believed to be a mysterious disease, sometimes still associated with smallpox. Monkeypox is a source of worries and stigmatization by communities. Conflicts were observed between the village where the outbreaks discussed here sparked and neighboring villages to the extent that a separation barrier was set up.
The monkeypox outbreak is mainly characterized by a high secondary attack rate among close contacts. All but four patients identified during this outbreak were secondary cases. This is an important factor as physical contact is frequent in most Sub-Saharan countries, when caring for patients and handling the deceased. In 2007, one of the new factors observed during the monkeypox outbreak in the DRC was the high proportion of secondary cases (78%) [16].
The disease attack rate in the district of Bangassou (0.2 per 1000 inhabitants) was lower than that of Alindao (5 per 1000 inhabitants) [10]. Our results are well below those reported by Jezek in 1984 in the DRC. They indeed reported a 7.2% attack rate among case contacts without smallpox vaccination scar and 0.9% among previously vaccinated individuals [17].
Monkeypox is a severe infectious disease in humans and is associated with a high case fatality. All outbreaks observed in CAR over the past years led to deaths, partly because of healthcare facilities plundering and of the arrival of displaced populations due to armed conflicts. Patient management is therefore difficult. The inhabitants of the village of Rehou 4 faced drug shortage in their healthcare facility and procurement difficulty due to racketeering. Patients’ families had to use traditional medicines made of plants and barks, although not always effective.
Considering the increased number of case patients, the growing geographical area of monkeypox virus activity, and the high number of strains stored in laboratories, the development of a vaccine against Orthopoxvirus should be considered. Such vaccine could be useful if these viruses were to be used for bioterrorism purposes. Above all, antiviral investigation against Poxviridae is needed considering the clinical severity and increased incidence of these infections.
As the outbreak sparked in a difficult-to-access area, investigators had to obtain written authorization from the commandant in charge of the area following a thorough interrogation on the mission's objective. The investigators were then authorized to access this occupied area as well as the affected villages. The difficult circulation in this area is due to the numerous racketeering barriers set up by armed groups and to the substantial degradation of roads. Access difficulties and the edginess of members of the armed groups, due to language difficulties, made it difficult to the investigators to carry out their mission and isolated vulnerable populations which could only turn to humanitarian aid.
6. Conclusion
Monkeypox is responsible for severe infections, with a high case fatality. The disease severity is even more important in CAR because of the destruction of healthcare facilities following the military and political crisis. Access to care by the population has become a real issue. Deforestation and hunting partly contribute to the emergence of this human infection. As monkeypox outbreaks are now more common, neighboring districts of monkeypox-infected areas must be closely monitored. The disease severity among young infants and the high case fatality reinforce the need for a vaccine or an antiviral to fight this emerging infection. Communication strategies and awareness campaigns must also be reinforced to avoid confusion and stigmatization.
Funding
The authors did not receive any external funding.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgment
We would like to thank the following NGOs, organizations, and individuals for helping with the outbreak and for contributing to the article:
-
•
Ernest Kalthan funded the research, contributed to the investigation and to data collection. He performed data capture and analysis;
-
•
Joaquim Tenguere contributed to the investigation, to data collection, and to reporting and confirming the case patients;
-
•
Séverin Gervais Ndjapou contributed to the investigation, to data collection, and to reviewing the article;
-
•
Thomas d’Aquin Koyazengbe transmitted information on the outbreak and reviewed the article;
-
•
Justin Mbomba contributed to the investigation and to reviewing the article;
-
•
Régis-Martial Marada contributed to the 2nd investigation and transmitted information on the first case patients;
-
•
Patrice Rombebe was a member of the investigation team and collected data;
-
•
Pépin Yangueme contributed to the investigation and to data collection;
-
•
Michel Babamingui contributed to the investigation and to data collection;
-
•
Arsène Sambella contributed to the 1st investigation, took photos, and performed sample collection;
-
•
Emmanuel Rivelyn Nakoune performed the laboratory diagnosis and contributed to writing the article;
-
•
International Medical Corps;
-
•
Cordaid Alindao;
-
•
Fifth Regional Health Directorate, WHO, Institut Pasteur in Bangui;
-
•
Mrs. Kalthan Marina, and;
-
•
Mr. Gonda François for localizing the case patients on the map.
References
- 1.Huhn G.D., Bauer A.M., Yorita K., Graham M.B., Sejvar J., Likos A., et al. Clinical characteristics of human monkeypox, and risk factors for severe disease. Clin Infect Dis. 2005;41(12):1742–1751. doi: 10.1086/498115. [DOI] [PubMed] [Google Scholar]
- 2.Chastel C. Le monkeypox humain. Pathol Biol. 2009;57:175–183. doi: 10.1016/j.patbio.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jezek Z., Fenner F. In: Melnick J.L., editor. Vol. 17. Karger; Basel, Switzerland: 1988. Human monkeypox. (Monographs in virology). [Google Scholar]
- 4.Marennikova S.S., Seluhina E.M., Mal’ceva N.N., Cimiskjan K.L., Macevic G.R. Isolation and properties of the causal agent of a new variola-like disease (monkeypox) in man. Bull World Health Organ. 1972;46:599–611. [PMC free article] [PubMed] [Google Scholar]
- 5.Boumandouki P., Bileckot R., Ibara J.R.C., et al. Orthopoxvirose simienne (ou variole du singe) : étude de 8 cas observés à l’hôpital d’Impfondo de la République du Congo. Bull Soc Pathol Exot. 2007;100(1):17–21. [PubMed] [Google Scholar]
- 6.Centers for Disease Control, Prevention Multistate outbreak of monkeypox — Illinois, Indiana, and Wisconsin, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:537–540. [PubMed] [Google Scholar]
- 7.Reed K.D., Melski J.W., Graham M.B., et al. The detection of monkeypox in humans in the western hemisphere. N Engl J Med. 2004;350:342–350. doi: 10.1056/NEJMoa032299. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control Prevention Update: multistate outbreak of monkeypox-Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:561–564. [PubMed] [Google Scholar]
- 9.Yu L., et al. Real-time PCR, assays for the specific detection of monkeypox virus West African and Congo basin strain DNA. J Virol Methods. 2010;169:223–227. doi: 10.1016/j.jviromet.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalthan E., Dondo-Fongbia J.P., Yambele S., Dieu-Creer L.R., Zepio R., Pamatika C.M. Épidémie de 12 cas de maladie à virus monkeypox dans le district de Bangassou en République Centrafricaine en décembre 2015. Bull Soc Pathol Exot. 2016;109:358–363. doi: 10.1007/s13149-016-0516-z. [DOI] [PubMed] [Google Scholar]
- 11.Learned L.A., Reynolds M.G., Wassa D.W., Yu L., Olson V.A., Karem K., et al. Extended interhuman transmission of monkeypox in a hospital community in the Republic of the Congo, 2003. Am J Trop Med Hyg. 2005;73:428–434. [PubMed] [Google Scholar]
- 12.Likos A.M., Sammons S.A., Victoria A., Olson A., Frace A.M., Yu L., et al. A tale of two clades: monkeypox viruses. J Gen Virol. 2005;86:2661–2672. doi: 10.1099/vir.0.81215-0. [DOI] [PubMed] [Google Scholar]
- 13.Meyer H., Perrichot M., Stemmler M., Emmerich P., Schmitz H., Varaine F., et al. Outbreaks of disease suspected of being due to human monkeypox virus infection in the Democratic Republic of Congo in 2001. J Clin Microbiol. 2002;40(8):2919–2921. doi: 10.1128/JCM.40.8.2919-2921.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rimoin A.W., Kisalu N., Kebela-Ilunga B., Mukaba T., Wright L.L., Formenty P., et al. Endemic human monkeypox, Democratic Republic of Congo, 2001–2004. Emerg Infect Dis. 2007;13:934–937. doi: 10.3201/eid1306.061540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levine R.S., Peterson A.T., Yorita K.L., Carroll D., Damon I.K., Reynolds M.G. Ecological niche and geographic distribution of human monkeypox in Africa. PLoS One. 2007;2 doi: 10.1371/journal.pone.0000176. [e176] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parker S., Nuara A., Mark R., Buller L., Schultz D.A. Human monkeypox: an emerging zoonotic disease. Future Microbiol. 2007;2(1):17–34. doi: 10.2217/17460913.2.1.17. [DOI] [PubMed] [Google Scholar]
- 17.Jezek Z., Marennikova S.S., Mutumbo M., et al. Human monkeypox: a study of 2,510 contacts of 214 patients. J Infect Dis. 1986;154(4):551–555. doi: 10.1093/infdis/154.4.551. [DOI] [PubMed] [Google Scholar]