Although various monkeypox (MPX) outbreaks have been reported, reports indicate that the current one has different epidemiological and clinical characteristics. Investigating these characteristics can remarkably enhance the surveillance measures and the management of affected patients to curb the spread of the outbreak. A meta-analysis was recently published in this regard [1]. However, they generally included studies from different outbreaks, and the reported outcomes were not confined to the current one. Besides, many of their included reports were of limited sample sizes, and various observational investigations have been conducted since then. Therefore, we aimed to conduct an updated meta-analysis to estimate the clinical characteristics and severity of the current MPX outbreak based on evidence from larger studies.
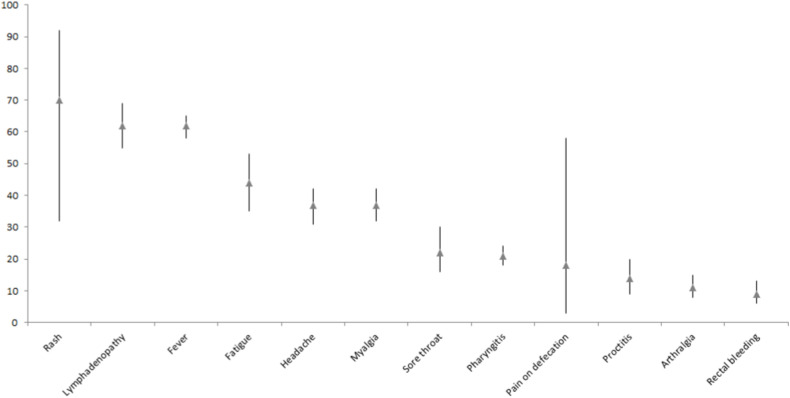
We conducted a rigorous systematic review by following the PRISMA guidelines. We included studies that recruited >10 MPX patients (to minimize the risk of statistical heterogeneity and obtain a better representative sample for the prevalence rates) and reported any of our outcomes. The definition of MPX cases was conducted like previous relevant systematic reviews [[1], [2], [3]]. On Septmeber 2, 2022, we searched five databases by the search term "(“MPV” OR “monkeypox” OR “monkeypox virus” OR “monkey pox")" to recruit all the relevant papers. All the resulting records were screened by at least three authors together with the senior author when disagreement occurred. Our outcomes were: the clinical features of MPX, hospitalization, intensive care unit admission (ICU), and mortality rates. Quality assessment was done using the New-Castle Ottawa scale. The prevalence and the 95% confidence interval (CI) were used as the statistical estimate through the comprehensive meta-analysis software. Out of 4231 citations, we found 14 papers that recruited 4080 MPV cases (Fig. S1). Eleven studies (N = 3488) reported the prevalence of HIV in their MPX populations to be 11.6% (405/3488). Other characteristics of the included studies and their cohorts are presented in Table S1, and the quality assessment results are shown in Table S2. The most common clinical features of MPX were rash 70% (95%CI: 32–92), lymphadenopathy 62% (95%CI: 55–69), and fever 62% (95%CI: 58–65) (Fig. 1 ). Moreover, arthralgia 11% (95%CI: 8–15) and rectal bleeding 9 (95%CI: 6–13) were the least reported symptoms. Only 7% (95%CI: 5–9) of MPX cases required hospitalization. However, all studies recorded no mortality or ICU admission events regarding all the included MPV cases (Figs. S2–14).
Fig. 1.
The prevalence rates (▲) and 95%CI of the clinical manifestations of monkeypox cases.
The current study presents the most extensive evidence of the clinical features and severity of the recent MPX outbreak. Our findings show that rash, lymphadenopathy, and fever are the commonest clinical manifestations reported by MPX patients. Furthermore, arthralgia and rectal bleeding were the least common manifestations. Accordingly, a proper differential diagnosis should be established for MPX to exclude other similar conditions [1]. However, the high prevalence of lymphadenopathy might differentiate MPX from other diseases, like varicella and smallpox [4]. Moreover, the distribution of lesions (more frequent on the genitalia) and the history of presenting patients (more frequent among MSM) in the current outbreak are also other important factors to consider when establishing a differential diagnosis of MPX [1]. Moreover, we found that only 7% of our cohort required hospitalization, with no ICU admissions or mortality events. The reported hospitalization rate in the current study is remarkably lower than that reported by Benites-Zapata et al. [1], 35% in the different MPX outbreaks. However, the authors demonstrated that the hospitalization rate is 1:6 between European and African patients.
When reviewing the literature, we found some reports of MPX deaths. In this context, Sah et al. [5] estimated a case fatality rate of 0.01% in non-endemic areas, compared to 1.81% in endemic regions in 2022. These rates are remarkably lower than the previously estimated ones from previous outbreaks, 4.6% (95%CI: 2.1–8.6%) for the West African clade (Clade II) and 10.6% (95%CI: 8.4–13.3%) for the Central African or Congo basin one (Clade I) [6]. These findings indicate that the current outbreak is significantly milder than previous outbreaks, which might be attributed to the quality of care offered to MPX cases as most patients in the current outbreak were located in high-income countries and were young (Table S1). According to some case reports, the reported mortality rates in some patients might be attributed to the atypical presentation of MPX. For instance, encephalitis, sepsis, and myopericarditis might complicate the infection, inducing a severe disease [5]. Besides, HIV co-infection might be another reason for inducing a severe disease in some patients. However, the exact cause-effect of the different morbidities on the severity of MPX still needs further evidence, particularly from case-control studies.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.tmaid.2022.102456.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Benites-Zapata V.A., Ulloque-Badaracco J.R., Alarcon-Braga E.A., et al. Clinical features, hospitalisation and deaths associated with monkeypox: a systematic review and meta-analysis. Ann Clin Microbiol Antimicrob. 2022;21(1):36. doi: 10.1186/s12941-022-00527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaheen N., Diab R.A., Meshref M., Shaheen A., Ramadan A., Shoib S. Is there a need to be worried about the new monkeypox virus outbreak? A brief review on the monkeypox outbreak. Ann Med Surg. 2022;81 doi: 10.1016/j.amsu.2022.104396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bragazzi NL, Kong JD, Mahroum N, et al. Epidemiological trends and clinical features of the ongoing monkeypox epidemic: a preliminary pooled data analysis and literature review. J Med Virol.n/a(n/a). [DOI] [PubMed]
- 4.McCollum A.M., Damon I.K. Human monkeypox. Clin Infect Dis. 2013;58(2):260–267. doi: 10.1093/cid/cit703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sah R., Mohanty A., Abdelaal A., Reda A., Rodriguez-Morales A.J., Henao-Martinez A.F. First Monkeypox deaths outside Africa: no room for complacency. Therapeut Adv Infect Dis. 2022;9 doi: 10.1177/20499361221124027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bunge E.M., Hoet B., Chen L., et al. The changing epidemiology of human monkeypox—a potential threat? A systematic review. PLoS Neglected Trop Dis. 2022;16(2) doi: 10.1371/journal.pntd.0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.