Abstract
Human monkeypox (MPX) is an endemic zoonotic disease in regions of Africa caused by the monkeypox virus, with recent outbreaks in several non-African countries. In this study, we present two cases of patients with MPX infection complicated by a deep skin infection. Both patients presented to our dermatology clinic with a clinical syndrome characteristic of MPX. The diagnosis was confirmed based on swabs of skin lesions. Both patients later returned to our clinic with erythema, pain, and edema at the site of previous papules and were diagnosed with deep skin bacterial infection. In this study we provide information on what we believe was an underreported MPX infection complication and give some advice on preventing cases of cellulitis in these patients.
Keywords: Monkeypox, Disease outbreak, Cellulitis, Infectious skin diseases
Introduction
Human monkeypox (MPX) is a zoonosis caused by monkeypox virus (MPXV), an orthopoxvirus endemic in some African countries, with few reported outbreaks in non-African countries until 2022 (Di Giulio and Eckburg, 2004; Petersen et al., 2019). The clinical syndrome is characterized by fever, rash, and lymphadenopathy (Huhn et al., 2005; Thornhill et al., 2022). Most patients have a moderate form of the disease with no need for hospitalization or antiviral treatment; however, described MPX complications include pneumonitis, encephalitis, keratitis, secondary bacterial infections, deep tissue MPX abscess, myocarditis, and epiglottitis (Adler et al., 2022; Huhn et al., 2005; Thornhill et al., 2022). Since early May 2022, more than 16,000 MPX cases and five deaths have been reported in more than 75 countries worldwide, leading the World Health Organization to declare MPX a “Public Health Emergency of International Concern” (World Health Organization, 2022a, 2022b). Since 3 May 2022, Portugal has reported cases of MPX with sustained local human-to-human transmission, with 588 cases of confirmed MPX up to 25 July 2022 (World Health Organization, 2022a), with a suspected sexual transmitted infection (STI) pattern of transmission (Alpalhão et al., 2022; Perez Duque et al., 2022). This report aims to describe cellulitis as an MPX complication, describing the clinical and laboratory characteristics of two patients, as well as potential preventive measures.
Case report
Our first report is of a 34-year-old, Fitzpatrick phototype III, male patient. Past medical history included HIV infection under antiretroviral treatment with good immune-virologic control and type 1 diabetes mellitus with adequate metabolic control. There was no pre-exposure smallpox vaccination. There was no history of international travel in the past 3 months. The patient presented with a painful skin lesion, fatigue, and sore throat for 2 days. He reported 18 casual unprotected sexual contacts with men in the last 30 days, all asymptomatic to his knowledge.
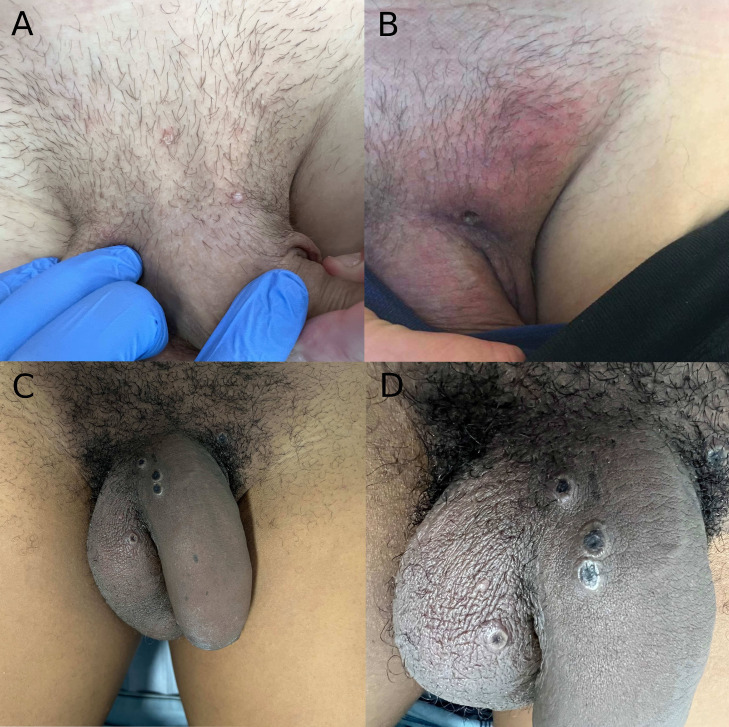
On observation, the patient had one umbilicated painful papule on the suprapubic region (Figure 1 a). Inguinal centimetric lymphadenopathy was also present. No other skin or oral lesions were present at that time.
Figure 1.
(a) Whitish papule on the first patient observation; (b) Ulcerated lesion with concurrent erythema and edema of the inguinal fold on day 11 of disease onset; (c) Penile edema and erythema; (d) Umbilicated pustules with necrotic center detailed.
After suspicion of MPX, swab samples were collected from the lesion surface genital area and the oropharynx. STI screening was negative for hepatitis C, hepatitis B, hepatitis A, and syphilis, as well as for urethral Neisseria gonorrhoeae or Chlamydia trachomatis infection, and genital Herpes Simplex Virus 1 and 2. Diagnosis with polymerase chain reaction (PCR) in real time was based on detecting the orthopoxvirus genus gene rpo18, followed by Sanger sequencing of PCR products. On day 11 after disease onset, the patient was admitted for observation with inguinal erythema, edema, and local pain at the previous site of lymphadenopathy, compatible with pubic and inguinal cellulitis (Figure 1b). Laboratory workups revealed elevated C-reactive protein (CRP) levels (6.24 mg/dl), with no changes in white cell count. Treatment with oral flucloxacillin was initiated, with clinical and symptomatic improvement, and cellulitis resolution was observed after 6 days.
Our second case was a 35-year-old, Fitzpatrick phototype IV, male patient. Past medical history included HIV under antiretroviral treatment with good immune-virologic control. There was no pre-exposure smallpox vaccination or history of international travel in the past 3 months. The patient presented to our walk-in Emergency Care Dermatology Clinic with skin lesions, fatigue, and headache for 3 days. He reported three sexual contacts with men in the last 30 days, all asymptomatic to his knowledge.
On observation, disseminated papules and pustules were present, some umbilicated with a hemorrhagic center, on the trunk, face, genital and perianal areas, with a total count under 20. Samples were collected as previously described, with MPX diagnosis. STI screening was negative for hepatitis C, hepatitis B, syphilis, and genital Herpes Simplex Virus 1/2. On day 6 after disease onset, the patient was admitted for observation with penile erythema, edema, and pain compatible with cellulitis (Figure 1c-d). Laboratory workups revealed elevated CRP levels (8.08 mg/dl), with no white cell count changes. Treatment with oral flucloxacillin was also initiated, with clinical and symptomatic improvement and cellulitis resolution 7 days after treatment was initiated.
Discussion
MPX treatment is recommended in cases of severe disease, patients at risk of severe disease, such as immunocompromised persons, pediatric populations, pregnant and breastfeeding women, and in people with one or more complications (Centers for Disease Control and Prevention (CDC), 2022). Given the low severity of MPX in our patients, we opted for a conservative approach by closely monitoring disease progression and complications. Although deep skin infections, where there is the involvement of the dermis and subcutaneous tissues, such as cellulitis, are not commonly associated with MPX, the natural progression of the skin lesions with ulceration might create a portal of entry for bacterial skin infections. There are deep tissue MPX abscess descriptions in the literature, one in an adult patient with confirmed high levels of MPXV DNA in the abscess fluid (Adler et al., 2022), and the other on a child with MPX and a radiologically confirmed retropharyngeal abscess (Anderson et al., 2003). Recently published literature has highlighted the need for clinical follow-up of patients with MPX to allow early detection and treatment of bacterial superinfected lesions; however, large patient series to estimate this complication risk are missing (Ortiz-Martínez et al., 2022).
The effect of HIV on the severity of MPX is unknown. Although HIV positivity has not been associated with higher symptom severity in patients with good immune-virologic control, an exuberant cutaneous presentation has been described in an acute HIV setting (Català et al., 2022; de Sousa et al., 2022).
The suspected route of transmission was through close contact during sexual intercourse, following the previously described pattern of STI transmission. (Alpalhão et al., 2022; Thornhill et al., 2022) All close contacts of our patients were followed-up by the public health authorities to establish if there is a possible chain of transmission or if close contacts were eligible for MPX vaccination.
We postulate that bacterial skin infections are an underreported entity in patients with MPX that lead to more patient morbidity and require further resource allocation in a time where responsiveness must be drawn to early diagnosis and management to avoid further MPX spreading. In our study, oral flucloxacillin was used empirically, based on the most common causative agents. Although our patients had risk factors (HIV and men who have sex with men) for resistant pathogens such as methicillin-resistant S. aureus, treatment was initiated with a good response without the need for broader spectrum antibiotics. From our center's empiric experience, the use of topical antibiotics as prophylaxis, particularly in lesions on the genital and anal region, might reduce MPX complications and patients with low hazard potential.
Conclusion
MPX is a known entity with limited published data available on the outcomes and complications of patients. We draw attention to the need for wound care and advice for the use of topical antibiotics on ulcerations of patients with a higher risk of skin infections, such as immunocompromised patients or when lesions on the genital and anal area are present.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Informed consent and permission for publication of medical images were taken from the patients.
CRediT authorship contribution statement
Diogo de Sousa: Conceptualization, Investigation, Writing – original draft. Joana Frade: Investigation. João Patrocínio: Investigation. João Borges-Costa: Writing – review & editing, Supervision. Paulo Filipe: Writing – review & editing, Project administration.
Declaration of competing interests
The authors have no competing interests to declare.
Acknowledgments
The patients in this manuscript have given written informed consent to the publication of their case details. The authors would like to thank Instituto Nacional de Saúde Doutor Ricardo Jorge (INSA) for the help provided in diagnosing Monkeypox Virus cases.
References
- Adler H, Gould S, Hine P, Snell LB, Wong W, Houlihan CF, et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022;22:1153–1162. doi: 10.1016/S1473-3099(22)00228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alpalhão M, Frade JV, Sousa D, Patrocínio J, Garrido PM, Correia C, et al. Monkeypox: a new (sexually transmissible) epidemic? J Eur Acad Dermatol Venereol Forthcoming. 2022 doi: 10.1111/jdv.18424. [DOI] [PubMed] [Google Scholar]
- Anderson MG, Frenkel LD, Homann S, Guffey J. A case of severe monkeypox virus disease in an American child: emerging infections and changing professional values. Pediatr Infect Dis J. 2003;22:1093–1096. doi: 10.1097/01.inf.0000101821.61387.a5. [DOI] [PubMed] [Google Scholar]
- Català A, Clavo Escribano P, Riera J, Martín-Ezquerra G, Fernandez-Gonzalez P, Revelles Peñas L, et al. Monkeypox outbreak in Spain: clinical and epidemiological findings in a prospective cross-sectional study of 185 cases. Br J Dermatol Forthcoming. 2022 doi: 10.1111/bjd.21790. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Treatment information for healthcare professionals | Monkeypox | Poxvirus. CDC. https://www.cdc.gov/poxvirus/monkeypox/clinicians/treatment.html, 2022 (accessed 27 July 2022).
- de Sousa D, Patrocínio J, Frade J, Correia C, Borges-Costa J, Filipe P. Human monkeypox coinfection with acute HIV: an exuberant presentation. Int J STD AIDS Forthcoming. 2022 doi: 10.1177/09564624221114998. [DOI] [PubMed] [Google Scholar]
- Di Giulio DB, Eckburg PB. Human monkeypox: an emerging zoonosis. Lancet Infect Dis. 2004;4:15–25. doi: 10.1016/S1473-3099(03)00856-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huhn GD, Bauer AM, Yorita K, Graham MB, Sejvar J, Likos A, et al. Clinical characteristics of human monkeypox, and risk factors for severe disease. Clin Infect Dis. 2005;41:1742–1751. doi: 10.1086/498115. [DOI] [PubMed] [Google Scholar]
- Ortiz-Martínez Y, Rodríguez-Morales AJ, Franco-Paredes C, Chastain DB, Gharamti AA, Barahona LV, et al. Monkeypox – a description of the clinical progression of skin lesions: a case report from Colorado, USA. Ther Adv Infect Dis. 2022;9 doi: 10.1177/20499361221117726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez Duque M, Ribeiro S, Martins JV, Casaca P, Leite PP, Tavares M, et al. Ongoing monkeypox virus outbreak, Portugal, 29 April to 23 May 2022. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.22.2200424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen E, Kantele A, Koopmans M, Asogun D, Yinka-Ogunleye A, Ihekweazu C, et al. Human monkeypox: epidemiologic and clinical characteristics, diagnosis, and prevention. Infect Dis Clin North Am. 2019;33:1027–1043. doi: 10.1016/j.idc.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornhill JP, Barkati S, Walmsley S, Rockstroh J, Antinori A, Harrison LB, et al. Monkeypox virus infection in humans across 16 countries - April–June 2022. N Engl J Med. 2022;387:679–691. doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Multi-country outbreak of monkeypox, External situation Report #2. https://www.who.int/publications/m/item/multi-country-outbreak-of-monkeypox–external-situation-report–2—25-july-2022, 2022a (accessed July 27, 2022).
- World Health Organization. (IHR) Emergency Committee regarding the multi-country outbreak of monkeypox. Second meeting of the International Health Regulations, 2005. https://www.who.int/news/item/23-07-2022-second-meeting-of-the-international-health-regulations-(2005)-(ihr)-emergency-committee-regarding-the-multi-country-outbreak-of-monkeypox, 2022b (accessed 24 July 2022).