A 31-year-old HIV-positive man presented to the hospital on June 30, 2022, with a vesicular rash (figure A ), perianal lesions, swollen inguinal lymph nodes, and arthralgia of the right knee. Under antiretroviral therapy, the HIV viral load was below the limit of detection, and his CD4+ T-cell count was 802 cells per μL. Given the rising number of monkeypox cases in Europe at that time and the patient's history of unprotected sexual contact with a man 1 week before symptom onset, an infection with monkeypox virus was suspected. Specimens from two different skin lesions yielded a positive PCR result (cycle threshold values of 20 and 21) for monkeypox virus. The patient was discharged and self-isolated.
Figure.
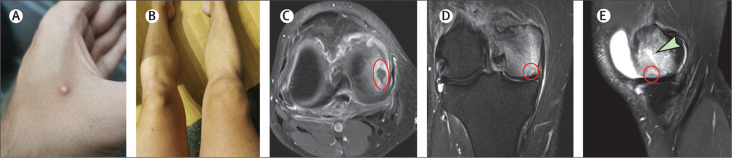
Skin lesion on the left hand (A), swelling of the right knee (B), MRI* of synovitis with subchondral demarcation zone (red circle; C), MRI† with marked oedema of the medial femoral condyle with subchondral demarcation zone (red circle; D), and MRI‡ of joint effusion, marked oedema (green arrow) and subchodral demarcation zone (red circle; E)
* T1-weighted (longitudinal relaxation time) turbo-spin-echo with fat saturation. †T1-weighted (longitudinal relaxation time) turbo inversion recovery magnitude. ‡Proton-density weighted fat suppression fast spin echo sequence.
11 days later a follow-up examination was scheduled, the rash and lymphadenopathy had completely resolved, but a marked swelling of the right knee was noted (figure B). Arthrocentesis was performed, resulting in aspiration of 60 mL of cloudy synovial fluid. Analysis of the synovial fluid showed a cell count of 16 127 cells per μL with 88·5% mononuclear cells (lymphocytes) and 11·5% neutrophil granulocytes. The synovial fluid PCR yielded a positive result for monkeypox virus (cycle threshold value of 27). Laboratory test results were unremarkable apart from a slightly elevated C-reactive protein of 18 mg/L.
Bacterial cultures and broad-range PCR of synovial fluid, serological testing for rheumatoid factor, anti-citrullinated protein antibodies and antinuclear antibodies, human leukocyte antigen B27, and PCR for Lyme disease were all negative. A second arthrocentesis was needed 8 days later due to reoccurrence of effusion. PCR of synovial fluid was again positive for monkeypox virus (cycle threshold value of 33), whereas PCR of whole-blood was negative for monkeypox virus. MRI showed synovitis, joint effusion, and a marked oedema of the medial femoral condyle with a subchondral demarcation zone of 1 cm, compatible with the diagnosis of arthritis and osteomyelitis (figure C–E). Treatment with non-steroidal-anti-inflammatory drugs led to improvement of arthralgia and swelling within 3 weeks.
Viruses are common triggers of arthritis, but viral bone infection has only rarely been reported. However, viral osteomyelitis was a typical complication of smallpox. Referred to as osteomyelitis variolosa, it affected 2–5% of children and 0·25–0·50% of all patients infected with smallpox. No cases of monkeypox-related arthritis or osteomyelitis have been described in the literature so far. Considering that variola virus and monkeypox virus are closely related, we believe that monkeypox virus might lead to arthritis and potentially osteomyelitis.
Declaration of interests
We declare no competing interests.
Contributors
MF was involved in writing and revision of the manuscript, case managing, contact to patient, knee punction, data collection, data curation, and editing of the manuscript. TM wrote the first draft of the manuscript and was involved in revision and data interpretation. JB-K was involved in data analysis, review of the manuscript, and clinical management of the patient (outpatient clinic rheumatology). WH participated in writing the first draft of the manuscript, manuscript revision, data analysis, formal analysis and review of the text, and clinical management of the patient (outpatient clinic infectious diseases). BH-M lead the radiological data interpretation. MT participated in reviewing, modifying, and amending the manuscript. AZ took care of clinical management of the patient (outpatient clinic infectious diseases), took skin samples, reviewed the text, and had professional input in case management. SWA was involved in the virological diagnostic, and review, modification, and amendments to the manuscript. HL and CW reviewed the case report and were involved in the modification and amendments to the manuscript. LE gave clinical input in patient management and was involved in the review, modification, and amendments to the manuscript. The patient provided written informed consent for publication of the case and images.