Abstract
A real-time, multiplexed polymerase chain reaction (PCR) assay based on dried PCR reagents was developed. Only variola virus could be specifically detected by a FAM (6-carboxyfluorescein)-labeled probe while camelpox, cowpox, monkeypox and vaccinia viruses could be detected by a TET (6-carboxytetramethylrhodamine)-labeled probe in a single PCR reaction. Approximately 25 copies of cloned variola virus DNA and 50 copies of genomic orthopoxviruses DNA could be detected with high reproducibility. The assay exhibited a dynamic range of seven orders of magnitude with a correlation coefficient value greater than 0.97. The sensitivity and specificity of the assay, as determined from 100 samples that contained nucleic acids from a multitude of bacterial and viral species were 96% and 98%, respectively. The limit of detection, sensitivity and specificity of the assay were comparable to standard real-time PCR assays with wet reagents. Employing a multiplexed format in this assay allows simultaneous discrimination of the variola virus from other closely related orthopoxviruses. Furthermore, the implementation of dried reagents in real-time PCR assays is an important step towards simplifying such assays and allowing their use in areas where cold storage is not easily accessible.
Keywords: Orthopox virus, Smallpox, Variola, Monkeypox, Cowpox, Vaccinia, Taqman, PCR, Real-time PCR, Multiplex PCR, Dried PCR reagents
1. Introduction
There are at least nine recognized Orthopoxvirus species, four of which (cowpox, monkeypox, vaccinia, and variola viruses) are known to cause human disease with varied severity depending on the viral species or strain, and the host's immune status. The most serious disease is smallpox. During the 20th century alone, smallpox is estimated to have caused over 300 million human deaths (Flint et al., 2004). The last naturally occurring case of smallpox was observed in Somalia in 1977 (Fenner, 1977). However, stocks of its causative agent, the variola virus, still exist in two World Health Organization repositories (the Centers for Disease Control and Prevention [CDC] in Atlanta, Georgia, USA, and the State Research Center of Virology and Biotechnology/Vector in Koltsovo, Russia).
Monkeypox virus can naturally produce disease in humans that closely resembles smallpox, with up to 15% mortality rates (Heymann et al., 1998). This virus was introduced into the United States in 2003 through importation of infected rodents from Ghana demonstrating the public health importance of this agent, and its potential as an emerging biological threat agent (Charatan, 2003, Reed et al., 2004, Ligon, 2004, Sale et al., 2006, Stephenson, 2003).
Natural infection with cowpox virus usually produces localized, self-limiting cutaneous disease in humans (Esposito and Fenner, 2001), however, severe cases involving atopic dermatitis have also been reported, including one fatality (Baxby et al., 1994, Pelkonen et al., 2003). The unusual manifestation in these cases suggests vulnerabilities of certain patients, perhaps similar to those observed with vaccinia virus.
While no significant disease has been attributed to camelpox virus, some concern exists over its deliberate use as a biological agent, mainly because of its close phylogenetic relationship to variola virus (Gubser and Smith, 2002). Four additional insertions, elongated inverted terminal repeats, and a small area of gene rearrangement present in camelpox virus are the major differences between camelpox and variola strain Bangladesh-1975 (Gubser and Smith, 2002).
Concerns have been raised that undeclared variola virus stocks may exist elsewhere, or other orthopoxviruses may be rendered more pathogenic by genetic engineering. Studies have shown in mouse models, that incorporation of cloned host cytokine genes into the genomes of mousepox and vaccinia viruses increased their virulence (Jackson et al., 2001, Robbins et al., 2005). Re-emergence of variola or genetically altered Orthopoxvirus chimeras would pose serious public health threats.
As a result of those concerns, efforts are mounting to replenish the vaccine supply for variola, and develop new drugs and diagnostic methods for the early detection of variola or related infections. Many phenotypic and genotypic methods involving virological, immunological, and molecular approaches have been used to identify orthopoxviruses. The molecular approaches, including DNA sequencing, polymerase chain reaction (PCR), restriction fragment-length polymorphism (RFLP), real-time PCR, and microarrays, are more sensitive and specific than the virological and immunological approaches. Of the molecular approaches, sequencing provides the highest level of specificity for species or strain identification but current sequencing techniques are not yet practical as rapid diagnostic tools, in most laboratories. Real-time PCR was utilized in the investigation of the 2003 US monkeypox outbreak (Sejvar et al., 2004). Because of its sensitivity, rapidity, and ease, real-time PCR is increasingly becoming the method of choice for preliminary detection of Orthopoxvirus infection, with isolation and growth in a high-level containment laboratory utilized for confirmation. Previously, the development of real-time PCR for detection of Orthopoxvirus infections was reported (Ibrahim et al., 1997, Ibrahim et al., 1998, Ibrahim et al., 2003, Aitichou et al., 2005). Other reports have demonstrated the utility of real-time PCR in detecting variola and other Orthopoxvirus species (Espy et al., 2002, Kulesh et al., 2004a, Kulesh et al., 2004b, Li et al., 2006, Nitsche et al., 2004, Olson et al., 2004, Scaramozzino et al., 2007). These previous reports describing the use of real-time PCR for detecting orthopoxviruses are based on liquid-dispensed reagents that require freezing or refrigeration. In this study, a multiplexed Taqman real-time PCR assay using dried PCR reagents is described. The assay detects specifically variola virus and differentiates this virus from other Orthopoxvirus species simultaneously. The dried reagents for this assay can be stored at ambient temperature for up to 1 year, thus obviating the need for cold chain storage. If combined with a portable, analytical, real-time PCR platform, dried reagents can bring field testing by real-time PCR a step closer.
2. Materials and methods
2.1. PCR primers and probes
The forward primer OPXJ7R3U (5′-TCATCTGGAGAATCCACAACA-3′), reverse primer OPXJ7R3L (5′-CATCATTGGCGGTTGATTTA-3′) and the probes VARJ7R3P-F (5′-FAM-CAAGACGTCGGGACCAATTACTAATA-TAMRA-3′), were described previously (Ibrahim et al., 2003). The OPXJ7R3P (5′-TET-CTGTAGTGTATGAGACAGTGTCTGTGAC-TAMRA-3′) was designed from a highly conserved region of the hemagglutinin gene to detect camelpox, cowpox, monkeypox, vaccinia in addition to variola viruses. The primers were synthesized by Invitrogen (Carlsbad, CA). Taqman probes were synthesized by Applied Biosystems (Foster City, CA). The variola Taqman probe contained 6-carboxyfluorescein (FAM) and the Orthopoxvirus Taqman probe contained 6-carboxytetramethylrhodamine (TET) at the 5′ end. Both probes utilized TAMRA as a quencher at the 3′ end.
2.2. Nucleic acid preparation
All viral and bacterial samples used in this study were from and the United States Army Medical Research Institute of Infectious Diseases (USAMRIID), Fort Detrick, MD and the Centers for Disease Control and Prevention (CDC), Atlanta, GA. They are listed in Table 1 . Nucleic acids from threat agents were pre-prepared and rendered noninfectious at biosafety level 4. The origins, propagation, and harvesting procedures for orthopoxviruses have been previously reported (Ropp et al., 1995). Poxvirus DNAs were extracted from virus-infected cells utilizing the Aquapure DNA kit (Bio-Rad, Hercules, CA). Prior experiments demonstrated that the material was noninfectious after 60 min of incubation at 55 °C in Aquapure lysis buffer. Bacterial DNA was extracted by the QIAamp DNA mini Kit (Qiagen, Valencia, CA). Total RNA was extracted from virus-infected cell cultures by the Trizol LS reagent (Invitrogen, Carlasbald, CA) according to the manufacturer's directions, and RNA pellets were dissolved in 10 μL of molecular biology-grade water and stored at −70 °C prior to use.
Table 1.
Cross-reactivity results of the multiplexed Taqman PCR assays for detecting variola and other orthopoxviruses
| Species/sample | Isolate | Conc. [Fg] | Dry Ct FAM | Dry Ct TET | Liquid Ct FAM | Liquid Ct TET |
|---|---|---|---|---|---|---|
| Orthopoxvirus samples | ||||||
| Camelpox virus | Somalia | 1000 | 0/2 | 2/2 | 0/2 | 2/2 |
| Cowpox virus | Brighton | 1000 | 0/2 | 2/2 | 0/2 | 2/2 |
| J7R Cloned DNA | BHS | 100 | 5/5 | 5/5 | 5/5 | 5/5 |
| J7R Cloned DNA | BHS | 10 | 8/8 | 8/8 | 8/8 | 8/8 |
| J7R Cloned DNA | BHS | 0.1 | 11/12a | 12/12 | 12/12 | 11/12a |
| Monkeypx virus | Zaire 96(I-16) | 1000 | 0/4 | 0/4 | 0/4 | 0/4 |
| Monkeypx virus | Zaire 96(I-16) | 100 | 0/5 | 0/5 | 0/5 | 0/5 |
| Monkeypx virus | Zaire 96(I-16) | 10 | 0/6 | 5/6a | 0/6 | 5/6a |
| Myxoma virus | CDC | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Racconpox virus | CDC | 1000 | 0/2 | 2/2 | 0/2 | 2/2 |
| Rabbitpox virus | CDC | 1000 | 0/2 | 2/2 | 0/2 | 2/2 |
| Skunkpox virus | CDC | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Tanapox virus | CDC | 1000 | 0/2 | 2/2 | 0/2 | 2/2 |
| Vaccinia virus | CPN | 1000 | 0/2 | 2/2 | 0/2 | 2/2 |
| Bacterial samples | ||||||
| Bacillus anthracis | 4728 | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Francisella tularensis | NA | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Yersinia pseudotuberculosis | 690 | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Stpahylococcus hominis | 27844 | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Neisseria lactamica | 23970 | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Haemophlius influenzae | 10211 | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Staphylococcus aureus | 25923 | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Listeia monocytogenes | 15313 | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Streptococcus pyogenes | 19615 | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Clostridium perfringens | 13124 | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
| Viral samples | ||||||
| Black Creek Canal virus | 39179 | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| Ebola Sudan virus | Boniface | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| Ebola Zaire virus | Zaire95 | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| Hantaan virus | 76-118 | 100 | 1/2b | 0/2 | 0/2 | 0/2 |
| Lassa virus | Josiah | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| Dengue 3 | CH3489 | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| Eastern Equine Encephalitis | FL-4679 | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| Rift Valley fever virus | ZH 548 | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| Venezuelan e. encephalitis | PE-4.0904 | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| West Nile | Crow397-99 | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| Yellow Fever | Assibe | 100 | 0/2 | 0/2 | 0/2 | 0/2 |
| Other samples | ||||||
| Human genome DNA | N/A | 1000 | 0/2 | 0/2 | 0/2 | 0/2 |
Comparison of the performance of the assay with dried (Dry FAM and Dry TET) and liquid (Liquid FAM and Liquid TET) reagents showing the number of positive samples over the total number of samples tested. The sensitivity and specificity were determined as described in Section 2. The results indicate that the sensitivity and specificity of the assay with dried PCR reagents, were 96% and 98%, respectively, and the sensitivity and specificity of the liquid reagents were 100%.
One sample has a Ct value below the threshold.
False positive.
2.3. Taqman assays
Standard real-time PCR reactions with liquid reagents were carried out in 30 μL volume utilizing the SmartCycler platform (Cepheid, Sunnyvale, CA). Each reaction contained 0.5 μM of each primer, 200 nM of each probe, 5 mM MgCl2, 200 μM dATP, dGTP, dCTP, and 0.4 μM dUTP in Platinum Quantitative PCR Supermix-UDG (Invitrogen, Carlasbald, CA) and 5 μL of DNA template.
Real-time PCRs with dried reagents were carried out using formulations that contained 0.625 μM of each primers, 240 nM of each probe, 5 mM MgCl2, 200 μM dATP, dGTP, dCTP, and 400 μM dUTP, and optimized Platinum Quantitative PCR SuperMix-UDG. The formulations were mixed with proprietary cryoprotectants, aliquoted in vials, flash frozen and lyophilized under vacuum (Invitrogen). Dried real-time PCR mix was dissolved in 25 μL of molecular grade biology water and 5 μL of template DNA was added after complete dissolution within 5 min.
For both types of PCR reagents, cycling conditions were performed as follows: 1 cycle at 50 °C for 2 min, 1 cycle at 95 °C for 2 min, followed by 45 cycles of 95 °C for 10 s, and 60 °C for 45 s.
2.4. Data analysis
Calculations of sensitivity and specificity were determined as follows: percent sensitivity = [TP/(TP + FN)] × 100 and percent specificity = [TN/(TN + FP)] × 100, where TP is the number of true-positive samples, FN is the number of false-negative samples, TN is the number of true-negative samples, and FP is the number of false-positive samples. Regression analysis was performed with Microsoft Excel to evaluate assay linearity and determine the quantitative performance of each assay. A cutoff value to determine the positive calls was established by using the mean threshold cycle (C t) value obtained from 20 replicates, each containing 50 genome copies, plus three times the standard deviation. The C t value for the SmartCycler device is defined as the first cycle in which there is a significant increase in fluorescence above the background.
3. Results
The use of dried real-time PCR reagents for diagnostic purposes has not been well established. The performance of multiplexed Taqman PCR assays using dried and liquid reagents were compared. Each method was evaluated by determining the lowest concentration of DNA that could be detected. The ability of each method to identify specifically variola virus and other orthopoxviruses in a panel of unrelated bacterial and viral nucleic acids samples was also assessed.
Limits of detection (LOD) for each assay were determined. Serial 10-fold dilutions from variola J7R cloned DNA and monkeypox virus DNA were subjected to amplification by the dried and liquid real-time PCR reagents. The amplification curves of variola J7R and monkeypox genomic DNA with dried and liquid reagents are presented in Fig. 1, Fig. 2, Fig. 3, Fig. 4 . From these results, both methods detected 0.1 fg of J7R cloned DNA (25 copies) and 10 fg (50 copies) of monkeypox genomic DNA.
Fig. 1.
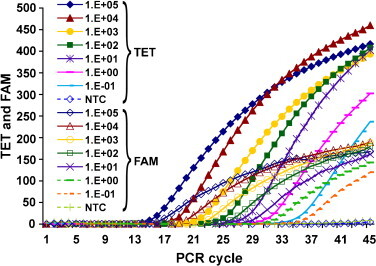
Detection limit of multiplexed real-time PCR with liquid reagents. Variola J7R clone DNA was serially diluted from 105 to 0.1 fg per reaction. Each curve represents the average fluorescence value of three replicates. Both FAM and TET probes signals were detected as expected in the presence of variola DNA. The assay has a detection limit of 0.1 fg per reaction (approximately 25 copies).
Fig. 2.
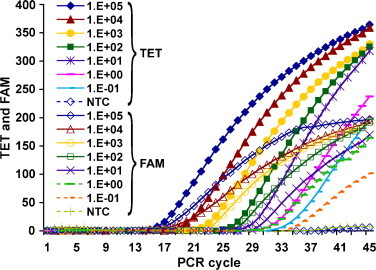
Detection limit of multiplex real-time PCR with dried reagents. Variola J7R DNA clone was serially diluted from 105 to 0.1 fg per reaction. Each curve represents the average fluorescence value of three replicates. Both FAM and TET probes signals were detected as expected in the presence of variola DNA fragment. The assay has a detection limit of 0.1 fg per reaction (25 copies).
Fig. 3.
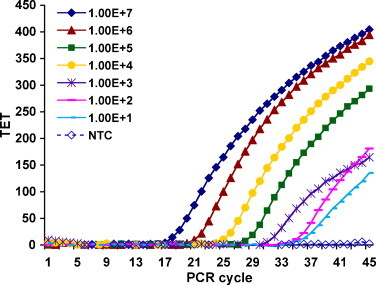
Detection limit of multiplex real-time PCR with liquid reagents. Monkeypox virus genomic DNA was diluted from 106 to 10 fg per reaction. Each curve represents the average fluorescence value of two to three replicates. Only TET signal was detected in the presence of monkeypox DNA. FAM signal was absent because it is specific for variola. The assay has a detection limit of 10 fg per reaction (approximately 50 copies).
Fig. 4.
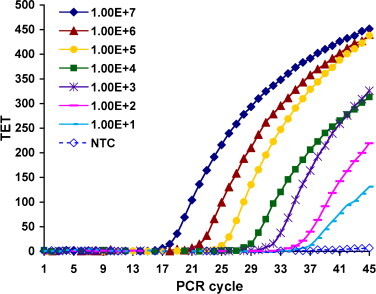
Detection limit of multiplex real-time PCR with dried reagents. Monkeypox virus genomic DNA was diluted from 106 to 10 fg per reaction. Each curve represents the average fluorescence value of two to three replicates. Only TET signal was detected in the presence of monkeypox DNA. FAM signal was absent because it is specific for Variola. The assay has a detection limit of 10 fg per reaction (approximately 50 copies).
Regression analysis was performed using the Microsoft Excel software. Both real-time PCR methods utilizing dried and liquid reagents had a strong linear correlation (R 2 > 0.97) between the C t values and J7R DNA concentrations over seven orders of magnitude (Fig. 5a and b). The correlation between the C t values and genomic DNA concentrations was also linear with both methods over seven orders of magnitude where R 2 = 0.99 (Fig. 5c).
Fig. 5.
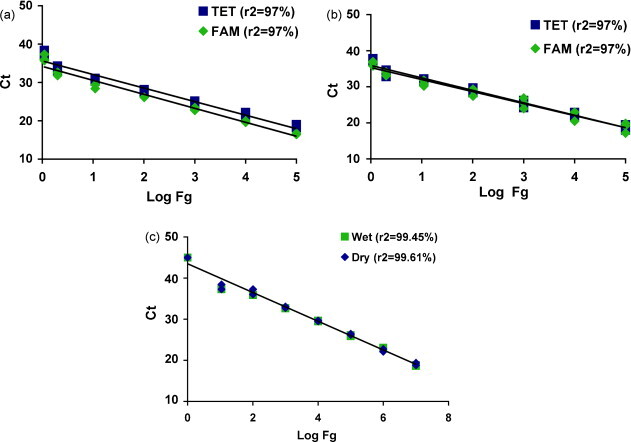
Standard curves were generated by plotting PCR threshold cycles (Ct) against log concentration of J7R cloned DNA. Regression analysis showed a broad dynamic range that with seven orders of magnitude for both FAM and TET reporters. (a) Dried PCR reagents; (b) wet PCR reagents; (c) regression analysis curves generated by plotting PCR threshold cycles (Ct) against log fg of monkeypox virus genomic DNA obtained with wet and dried PCR reagents. The coefficients of correlation are indicated.
The LOD of each assay was tested for reproducibility. All 20 test repetitions with 0.1 fg of the variola virus J7R clone were detected with dried and liquid PCR reagents. The calculated threshold value of dry reagents was slightly higher (39.2) than that of the liquid reagents (37.8). When monkeypox virus genomic DNA was tested at the LOD of 10 fg, 19 of 20 replicates were detected with dried reagents whereas 20 of 20 replicates were detected with the liquid reagents. The calculated threshold Ct values for monkeypox were 40.2 and 37.7 for the dried and liquid reagents, respectively (data not shown).
The results of the sensitivity and specificity experiments for the dried and liquid real-time PCR assays are shown in Table 1. Since these assays were multiplexed with dual probes, the data are shown for two probes: one probe (FAM) specific for only variola virus, and the other probe (TET) for camelpox, cowpox, monkeypox, rabbitpox, vaccinia, or variola viruses. Of 25 samples containing cloned variola J7R DNA, 25 were detected by both probes as expected. All 25 samples containing Orthopoxvirus genomic DNAs were correctly detected with liquid reagents, and 24 of the 25 samples were detected with dried reagents. Therefore, the sensitivity of the assay was 96% and 100% for dried reagents and liquid reagents, respectively. The false negative was obtained from one of the six replicates of monkeypox DNA at 10 fg. Since five of six of these samples were correctly detected, it is possible that the missed sample was due to a technical error, e.g., pipetting. When the missed sample was retested it was positive, but it is more appropriate to report the results of the original test here as it is part of the experimental design.
A total of 50 negative samples were tested. All of the 50 negative samples were negative with liquid real-time PCR reagents. Therefore, the specificity was 100%. However, one false positive was obtained with dried real-time PCR reagents resulting in 98% specificity. The false positive was obtained from one of two hantavirus samples that are clearly unrelated to orthopoxviruses, suggesting that the false positive was most likely due to inadvertent contamination of the samples.
4. Discussion
The objective of this study was to develop a simplified, multiplexed real-time PCR assay based on dried reagents for simultaneously detecting variola virus and other orthopoxviruses in the same reaction. The genomes of Orthopoxvirus species are highly conserved and proper detection requires a technology that enables species differentiation. Primers and probes were chosen to hybridize with the hemagglutinin (HA) gene sequence because this gene is unique to orthopoxviruses, including human pathogenic species.
The multiplexed assays described in this study here use dried PCR reagents incorporating all primers, probes, enzyme, buffers, and Mg+2 at optimized concentrations as described in Section 2. At least 25 copies of the variola virus J7R cloned DNA (0.1 fg) and 50 copies of monkeypox virus genomic DNA (10 fg) were detected per assay. These LOD were similar to those obtained using standard liquid PCR reagents. These LOD were well below the range of viral load expected in clinical samples. For example, up to 106 pock-forming units or 200 pg of variola DNA were obtained from skin lesions of the smallpox rash by day 2 of the rash (Nitsche et al., 2004, Damon and Esposito, 2003). The assay also exhibited high sensitivity (96%) and specificity (98%) that was comparable with assays based on liquid reagents.
The detection limits of real-time PCR assays reported previously for orthopoxviruses ranged from 2 to 25 genome copies per PCR reaction (Espy et al., 2002, Ibrahim et al., 2003, Nitsche et al., 2004, Kulesh et al., 2004a, Kulesh et al., 2004b, Olson et al., 2004, Li et al., 2006, Scaramozzino et al., 2007). In this study, the LOD of dried reagent based PCR assays was 25 and 50 copies for plasmid and genomic DNA, respectively. This LOD was determined utilizing 20 PCR reactions containing DNA at concentrations of 25 and 50 copies. A minimum of 95% reproducibility was set as a standard before choosing this LOD. Less than 25 copies can be detected although the reproducibility is significantly lower. The differences in sensitivity between assays described previously and dried reagent based PCR assays can be explained by the usage of different DNA extraction methods, PCR reagents, and PCR platforms.
With regards to the dried reagents stability, the components of the PCR reagents were lyophilized and stored at room temperature. The process of lyophilizing and storing PCR reagents seems to have no deleterious effect on the probes, primers, enzyme, or buffer after storage for up to 1 year at ambient temperatures because the assay with dried PCR reagents has the same sensitivity and specificity as those obtained when using liquid reagents based PCR.
The main advantages of dried PCR reagents are that they eliminate the requirement for cold storage and multiple pipetting, thus reducing logistical burden and errors due to the repetitive steps of reagent handing. Thus, by using dried real-time PCR reagents, a technician with basic skills can perform real-time PCR by simply adding molecular biology-grade water and template DNA to the dried PCR components. These advantages allow performing real-time PCR in remote areas where there is a growing need to monitor these viral strains, and in situations where transporting and shipping clinical samples between areas require stabilizers to preserve the integrity of specimens.
Although the cost benefit from implementing dried reagents for real-time PCR assays has not been formally evaluated in this study, it is anticipated that the elimination of cold chain requirement would clearly reduce the cost of storage, transportation and enhance the applicability of the technique for a broader suite of human pathogens, e.g., aiding public health in developing countries.
Acknowledgements
This work was supported by research program funds managed by the Defense Threat Reduction Agency grant #02-4-4I-091. We thank Katheryn Kenyon for reviewing the manuscript. The mention of materials or products in this article does not constitute endorsement by the Department of Defense or the United States government.
References
- Aitichou M., Javorschi S., Ibrahim M.S. Two-color multiplex assay for the identification of orthopox viruses with real-time LUX-PCR. Mol. Cell. Probes. 2005;19:323–328. doi: 10.1016/j.mcp.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Baxby D., Bennett M., Getty B. Human cowpox 1969–93: a review based on 54 cases. Br. J. Dermatol. 1994;131:598–607. doi: 10.1111/j.1365-2133.1994.tb04969.x. [DOI] [PubMed] [Google Scholar]
- Charatan F. US doctors investigate more than 50 possible cases of monkeypox. Br. Med. J. 2003;326:1350. doi: 10.1136/bmj.326.7403.1350-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damon I.K., Esposito J.J. In: Manual of Clinical Microbiology. 8th ed. Murray P.R., Baron E.J., Pfaller M.A., Tenover F.C., Yolken R.H., editors. American Society for Microbiology Press; Washington, D.C.: 2003. Poxvirus infections; pp. 1583–1591. [Google Scholar]
- Esposito, J.J., Fenner, F., 2001. Poxviruses. In: Knipe, D.M., Howley, P.M., Griffin, D.E., et al. (Eds.), Fields Virology, 4th ed. Lippincott Williams & Wilkins, Philadelphia, PA, pp. 2885–2921.
- Espy M.J., Cockerill F.R., III, Meyer R.F., Bowen M.D., Poland G.A., Hadfield T.L., Smith T.F. Detection of smallpox virus DNA by LightCycler PCR. J. Clin. Microbiol. 2002;40:1985–1988. doi: 10.1128/JCM.40.6.1985-1988.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenner F. The eradication of smallpox. Prog. Med. Virol. 1977;23:1–21. [PubMed] [Google Scholar]
- Flint S.J., Enquist L.W., Rancaniello V.R., Skalka A.M. 2nd ed. ASM press; Washington, D.C.: 2004. Principles of Virology: Molecular Biology, Pathogenesis and Control of Animal Viruses. p. 918. [Google Scholar]
- Gubser C., Smith G.L. The sequence of camelpox virus shows it is most closely related to variola virus, the cause of smallpox. J. Gen. Virol. 2002;83:855–872. doi: 10.1099/0022-1317-83-4-855. [DOI] [PubMed] [Google Scholar]
- Heymann D.L., Szczeniowski M., Esteves K. Re-emergence of monkeypox in Africa: a review of the past six years. Br. Med. Bull. 1998;54:693–702. doi: 10.1093/oxfordjournals.bmb.a011720. [DOI] [PubMed] [Google Scholar]
- Ibrahim M.S., Esposito J.J., Jahrling P.B., Lofts R.S. The potential of 5′ nuclease PCR for detecting a single-base polymorphism in orthopoxvirus. Mol. Cell. Probes. 1997;11:143–147. doi: 10.1006/mcpr.1996.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim M.S., Kulesh D.A., Saleh S.S., Damon I.K., Esposito J.J., Schmaljohn A.L., Jahrling P.B. Real-time PCR assay to detect smallpox virus. J. Clin. Microbiol. 2003;41:3835–3839. doi: 10.1128/JCM.41.8.3835-3839.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim M.S., Lofts R.S., Jahrling P.B., Henchal E.A., Weedn V.W., Northrup M.A., Belgrader P. Real-time microchip PCR for detecting single-base differences in viral and human DNA. Anal. Chem. 1998;70:2013–2017. doi: 10.1021/ac971091u. [DOI] [PubMed] [Google Scholar]
- Jackson R.J., Ramsay A.J., Christensen C.D., Beaton S., Hall D.F., Ramshaw I.A. Expression of mouse interleukin-4 by a recombinant ectromelia virus suppresses cytolytic lymphocyte responses and overcomes genetic resistance to mousepox. J. Virol. 2001;75:1205–1210. doi: 10.1128/JVI.75.3.1205-1210.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulesh D.A., Baker R.O., Loveless B.M., Norwood D., Zwiers S.H., Mucker E., Hartmann C., Herrera R., Miller D., Christensen D., Wasieloski L.P., Jr., Huggins J., Jahrling P.B. Smallpox and pan-orthopox virus detection by real-time 3′-minor groove binder TaqMan assays on the Roche LightCycler and the Cepheid SmartCycler platforms. J. Clin. Microbiol. 2004;42:601–609. doi: 10.1128/JCM.42.2.601-609.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulesh D.A., Loveless B.M., Norwood D., Garrison J., Whitehouse C.A., Hartmann C., Mucker E., Miller D., Wasieloski L.P., Jr., Huggins J., Huhn G., Miser L.L., Imig C., Martinez M., Larsen T., Rossi C.A., Ludwig G.V. Monkeypox virus detection in rodents using real-time 3′-minor groove binder TaqMan assays on the Roche LightCycler. Lab. Invest. 2004;84:1200–1208. doi: 10.1038/labinvest.3700143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Olson V.A., Laue T., Laker M.T., Damon I.K. Detection of monkeypox virus with real-time PCR assays. J. Clin. Virol. 2006;36:194–203. doi: 10.1016/j.jcv.2006.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ligon B.L. Monkeypox: a review of the history and emergence in the Western hemisphere. Semin. Pediatr. Infect. Dis. 2004;15:280–287. doi: 10.1053/j.spid.2004.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitsche A., Ellerbrok H., Pauli G. Detection of orthopoxvirus DNA by real-time PCR and identification of variola virus DNA by melting analysis. J. Clin. Microbiol. 2004;42:1207–1213. doi: 10.1128/JCM.42.3.1207-1213.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson V.A., Laue T., Laker M.T., Babkin I.V., Drosten C., Shchelkunov S.N., Niedrig M., Damon I.K., Meyer H. Real-time PCR system for detection of orthopoxviruses and simultaneous identification of smallpox virus. J. Clin. Microbiol. 2004;42:1940–1946. doi: 10.1128/JCM.42.5.1940-1946.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelkonen P.M., Tarvainen K., Hynninen A., Kallio E.R., Henttonen K., Palva A., Vaheri A., Vapalahti O. Cowpox with severe generalized eruption in Finland. Emerg. Infect. Dis. 2003;9:1458–1461. doi: 10.3201/eid0911.020814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed K.D., Melski J.W., Graham M.B., Regnery R.L., Sotir M.J., Wegner M.V., Kazmierczak J.J., Stratman E.J., Li Y., Fairley J.A., Swain G.R., Olson V.A., Sargent E.K., Kehl S.C., Frace M.A., Kline R., Foldy S.L., Davis J.P., Damon I.K. The detection of monkeypox in humans in the Western Hemisphere. N. Engl. J. Med. 2004;350:342–350. doi: 10.1056/NEJMoa032299. [DOI] [PubMed] [Google Scholar]
- Robbins S.J., Jackson R.J., Fenner F., Beaton S., Medveczky J., Ramshaw I.A., Ramsay A.J. The efficacy of cidofovir treatment of mice infected with ectromelia (mousepox) virus encoding interleukin-4. Antiviral Res. 2005;66:1–7. doi: 10.1016/j.antiviral.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Ropp S.L., Jin Q., Knight J.C., Massung R.F., Esposito J.J. PCR strategy for identification and differentiation of smallpox and other orthopoxviruses. J. Clin. Microbiol. 1995;33:2069–2076. doi: 10.1128/jcm.33.8.2069-2076.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sale T.A., Melski J.W., Stratman E.J. Monkeypox: an epidemiologic and clinical comparison of African and US disease. J. Am. Acad. Dermatol. 2006;55:478–481. doi: 10.1016/j.jaad.2006.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scaramozzino N., Ferrier-Rembert A., Favier A.L., Rothlisberger C., Richard S., Crance J.M., Meyer H., Garin D. Real-time PCR to identify variola virus or other human pathogenic orthopox viruses. Clin. Chem. 2007;53(4):606–613. doi: 10.1373/clinchem.2006.068635. [DOI] [PubMed] [Google Scholar]
- Sejvar J.J., Chowdary Y., Schomogyi M., Stevens J., Patel J., Karem K., Fischer M., Kuehnert M.J., Zaki S.R., Paddock C.D., Guarner J., Shieh W.J., Patton J.L., Bernard N., Li Y., Olson V.A., Kline R.L., Loparev V.N., Schmid D.S., Beard B., Regnery R.R., Damon I.K. Human monkeypox infection: a family cluster in the midwestern United States. J. Infect. Dis. 2004;190:1833–1840. doi: 10.1086/425039. [DOI] [PubMed] [Google Scholar]
- Stephenson J. Monkeypox outbreak a reminder of emerging infections vulnerabilities. J. A. M. A. 2003;290:23–24. doi: 10.1001/jama.290.1.23. [DOI] [PubMed] [Google Scholar]


