With more than 50 000 cases worldwide in since May, 2022, and more than 95% of them in men who have sex with men, the monkeypox outbreak continues to represent a major medical and public health concern. Uncertainties persist regarding the transmission routes; together with epidemiological data, new insights are expected from the virological evaluation of the presence of monkeypox virus (MPXV) in different areas of the human body.
In this issue of The Lancet Infectious Diseases, Romain Palich and colleagues1 report an extended evaluation of MPXV DNA in samples from skin, anus, throat, blood, urine, and semen from 50 French monkeypox cases. MPXV detection was more frequent in skin (44 [88%] of 50), anus (30 [71%] of 42), and throat (36 [77%] of 47) samples than from blood (13 [29%] of 45), urine (nine [22%] of 41), or semen (13 [54%] of 24) samples. Similar studies have been reported in the past months, with largely overlapping findings showing widespread viral detection in different areas of the body (table ). The highest viral DNA loads were consistently found in skin (Cycle threshold [Ct] 19·8) and anogenital swabs (Ct 20·9), suggesting intimate sexual contact as the main route of transmission. This finding is supported by the data on semen, which frequently has shown as DNA-positive in patients with MPXV.1, 2, 3, 6 Nevertheless, several questions regarding the contribution of the different bodily fluids to virus transmission need to be further addressed, also to better define the disease burden and the public health implications.
Table.
Large case series reporting prevalence of MPXV DNA and median Ct of positive samples at PCR in at least two different bodily fluids
| Participants | HIV-positive |
Skin* |
Anogenital |
Nasopharynx |
Plasma |
Urine |
Semen |
Saliva |
Fecal matter |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MPXV DNA prevalence | Median Ct | MPXV DNA prevalence | Median Ct | MPXV DNA prevalence | Median Ct | MPXV DNA prevalence | Median Ct | MPXV DNA prevalence | Median Ct | MPXV DNA prevalence | Median Ct | MPXV DNA prevalence | Median Ct | MPXV DNA prevalence | Median Ct | |||
| France (Palich et al, 2022)1 | 50 | 22/50 (44%) | 44/50 (88%) | 20 | 30/42 (71%) | 21 | 36/47 (77%) | 27 | 13/45 (29%) | 33 | 9/41 (22%) | 31 | 13/24 (54%) | 28 | NA | NA | NA | NA |
| Spain (Peiró-Mestres et al, 2022)2 | 12 | 4/12 (33%) | 12/12 (100%) | 20 | 11/12 (92%) | 23 | 10/12 (83%) | 31 | NA | NA | 9/12 (75%) | 35 | 7/9 (78%) | 32 | 12/12 (100%) | 29 | 8/12 (67%) | 24 |
| 16 countries (Thornhill et al, 2022)†3 | 528 | 218/528 (41%) | 512/528‡ | .. | .. | .. | 138/528 (26%) | NA | 35/528 (7%) | NA | 14/528 (3%) | NA | 29/32 (91%) | NA | NA | NA | NA | NA |
| France (Mailhe et al, 2022)4 | 264 | 73/256 (29%) | 252/258 (98%) | 23 | NA | NA | 150/197 (76%) | 32 | 8/26 (31%) | 36 | NA | NA | NA | NA | NA | NA | NA | NA |
| Spain (Tarín-Vicente et al, 2022)5 | 181 | 72/181 (40%) | 178/180 (99%) | 23 | 43/55 (78%) | 27 | 82/117 (70%) | 32 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Italy (Raccagni et al, 2022)6 | 36 | 15/36 (42%) | 36/36§ (100%) | .. | .. | .. | .. | .. | 24/36 (67%) | 34 | 8/36 (22%) | NA | 22/36 (61%) | 34 | NA | NA | NA | NA |
Data are n/N (%) unless otherwise specified. Ct=cycle threshold. MPXV=monkeypox virus. NA=not available.
Includes perianal skin.
Argentina, Australia, Belgium, Canada, Denmark, France, Germany, Israel, Italy, Mexico, Portugal, Spain, Switzerland, The Netherlands, UK, and USA.
Refers to skin or anogenital samples combined.
Refers to either skin, anogenital, or oropharyngeal samples combined.
First, infectivity is a prerequisite for virus transmission. So far, virus isolation, whether in cell culture or animal models, is recognised as the only laboratory method to prove the presence of infectious viral particles in biological secretions. To date, evidence of replication-competent virus isolation has been reported only from skin (including anal swabs), oropharynx swabs, and semen samples.7, 8 However, this approach is laborious with biosafety and technical limitations. Viral load is commonly used as an estimate of the infectivity potential. MPXV DNA concentrations in clinical samples have recently shown to correlate with viral infectivity, with Ct values lower than 35 found more likely to be infectious by in vitro viral isolation.7 On this assumption, the recent data showed that nasopharyngeal swabs, saliva, and feces mostly contain higher amounts of the virus, thus suggesting the potential for alternative routes of transmission. However, these studies have the intrinsic limitation of collecting samples from different districts at different times. Furthermore, contamination between contiguous matrices (eg, anorectal swabs contaminated by stool, or semen and urine contaminated by blood) might affect the detection. Therefore, further studies on different and larger cohorts, including multi-centre and multi-country cohorts, are required to characterise the factors influencing the MPXV compartmentalisation in the different anatomical sites (ie, exposure and clinical presentation).
Second, clinicians remain unaware of whether the virus can persist within immune-privileged sites, and for how long. Palich and colleagues showed that viral clearance appeared to be relatively rapid, as most tested samples resulted MPXV-negative or weakly positive (below Ct 35) within 14 days after symptom onset. However, data are still scarce and to date MPXV detection and viral shedding kinetics, also in the prodromal stages, are largely unknown. For example, we know that related poxviruses have both primary and secondary viremias, but so far, MPXV viremia has only been assessed in late disease stages. Although poxvirus transmission with transfusion has been documented only once with smallpox,9 these investigations are urgent, with potential implications for public health outside the current transmission chains (ie, in blood and tissue donations).
Finally, to better understand the biology, evolution, and spread of the virus causing the current outbreak, research efforts should be made regarding MPXV genome mapping and phylogenetic characterisation. Viral sequencing has refined phylogeny, with eight B.1 MPXV sub-lineages reported to date. A high number of mutations have been found in the viruses of the current outbreak,10 but whether these variations influenced MPXV transmissibility and virulence remains to be elucidated. Such notable diversification probably arises from long-term asymptomatic circulation leading to host adaptation, but previous smallpox vaccine-elicited immunity and different routes of transmission could also account for some of the phenotypic variations observed.
In conclusion, more extensive investigations are needed to obtain a coherent understanding of transmission factors that have permitted the extraordinary penetration of active MPXV infection into human communities worldwide. Notably, infection of animal hosts, including pets of confirmed cases or rodents infected by human stools in wastewaters, could further drive endemicity outside Africa. If this transmission continues, monkeypox cases are likely to increase in numbers outside of the community of men who have sex with men.
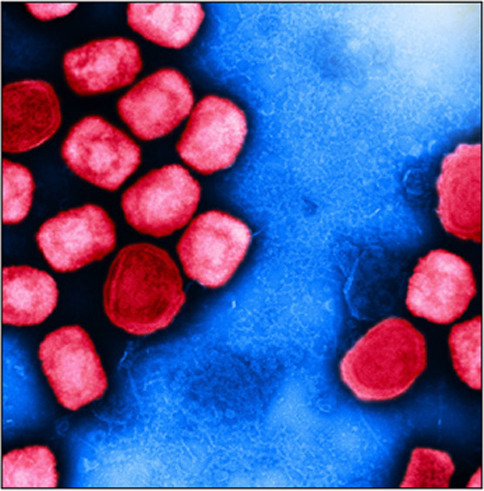
© 2023 Flickr - NIAID
We declare no competing interests.
References
- 1.Palich R, Burrel S, Monsel G, et al. Viral loads in clinical samples of men with monkeypox virus infection: a French case series. Lancet Infect Dis. 2022 doi: 10.1016/S1473-3099(22)00586-2. published online Sept 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peiró-Mestres A, Fuertes I, Camprubí-Ferrer D, et al. Frequent detection of monkeypox virus DNA in saliva, semen, and other clinical samples from 12 patients, Barcelona, Spain, May to June 2022. Euro Surveill. 2022;27:2200503. doi: 10.2807/1560-7917.ES.2022.27.28.2200503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thornhill JP, Barkati S, Walmsley S, et al. Monkeypox virus infection in humans across 16 countries—April–June 2022. N Engl J Med. 2022;387:679–691. doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 4.Mailhe M, Beaumont AL, Thy M, et al. Clinical characteristics of ambulatory and hospitalised patients with monkeypox virus infection: an observational cohort study. Clin Microbiol Infect. 2022 doi: 10.1016/j.cmi.2022.08.012. published online Aug 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tarín-Vicente EJ, Alemany A, Agud-Dios M, et al. Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study. Lancet. 2022;400:661–669. doi: 10.1016/S0140-6736(22)01436-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raccagni AR, Candela C, Mileto D, et al. Monkeypox infection among men who have sex with men: PCR testing on seminal fluids. J Infect. 2022;15:39. doi: 10.1016/j.jinf.2022.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paran N, Yahalom-Ronen Y, Shifman O, et al. Monkeypox DNA levels correlate with virus infectivity in clinical samples, Israel, 2022. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.35.2200636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lapa D, Carletti F, Mazzotta V, et al. Monkeypox virus isolation from a semen sample collected in the early phase of infection in a patient with prolonged seminal viral shedding. Lancet Infect Dis. 2022;22:1267–1269. doi: 10.1016/S1473-3099(22)00513-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cantrell JR, Ravitch MM. Transmission of disease by transfusion of blood and plasma. Am J Med. 1949;6:345–356. doi: 10.1016/0002-9343(49)90172-2. [DOI] [PubMed] [Google Scholar]
- 10.Isidro J, Borges V, Pinto M, et al. Phylogenomic characterization and signs of microevolution in the 2022 multi-country outbreak of monkeypox virus. Nat Med. 2022;28:1569–1572. doi: 10.1038/s41591-022-01907-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


