Abstract
Obesity is a multifactorial disease with a variable and underwhelming weight loss response to current treatment approaches. Precision medicine proposes a new paradigm to improve disease classification based on the premise of human heterogeneity, with the ultimate goal of maximizing treatment effectiveness, tolerability, and safety. Recent advances in high-throughput biochemical assays have contributed to the partial characterization of obesity’s pathophysiology, as well as to the understanding of the role that intrinsic and environmental factors, and their interaction, play in its development and progression. These data have led to the development of biological markers that either are being or will be incorporated into strategies to develop personalized lines of treatment for obesity. There are currently many ongoing initiatives aimed at this; however, much needs to be resolved before precision obesity medicine becomes common practice. This review aims to provide a perspective on the currently available data of high-throughput technologies to treat obesity.
Keywords: phenotypes, ADOPT, genetics, microbiome
Obesity is a complex and chronic multifactorial disease affecting 39% of the adult population in the United States and contributing to 280,000 deaths annually.1 Obesity is not only associated with a high incidence of several major noncommunicable diseases including cardiovascular conditions and type 2 diabetes2, but also with the loss of up to one in four potential disease-free years of life during middle and later adulthood.3 The high prevalence of obesity and its associated comorbidities results in nearly $480 billion in direct healthcare costs annually.4 It is estimated that by 2030 up to 49% of all adults in the United States will have obesity.5 These alarming projections and accompanying economic burden demand the development of effective therapeutic strategies that can complement obesity’s current standard of care approach.
The variability in weight loss response to the current obesity treatment approach is the result of the heterogeneity of this disease’s etiology, clinical presentation, and development of associated comorbidities. Current obesity guidelines suggest escalation therapy starting with lifestyle modifications supported by pharmacologic agents, endoscopic devices, and/or bariatric surgery based on the body mass index (BMI) and comorbidities of an individual, and his/her response to these different therapies.6–8 Each of these treatment strategies has been shown to have wide variability in terms of weight loss outcomes, suggesting that this current approach does not address the comprehensive and individualized care that patients with obesity need.
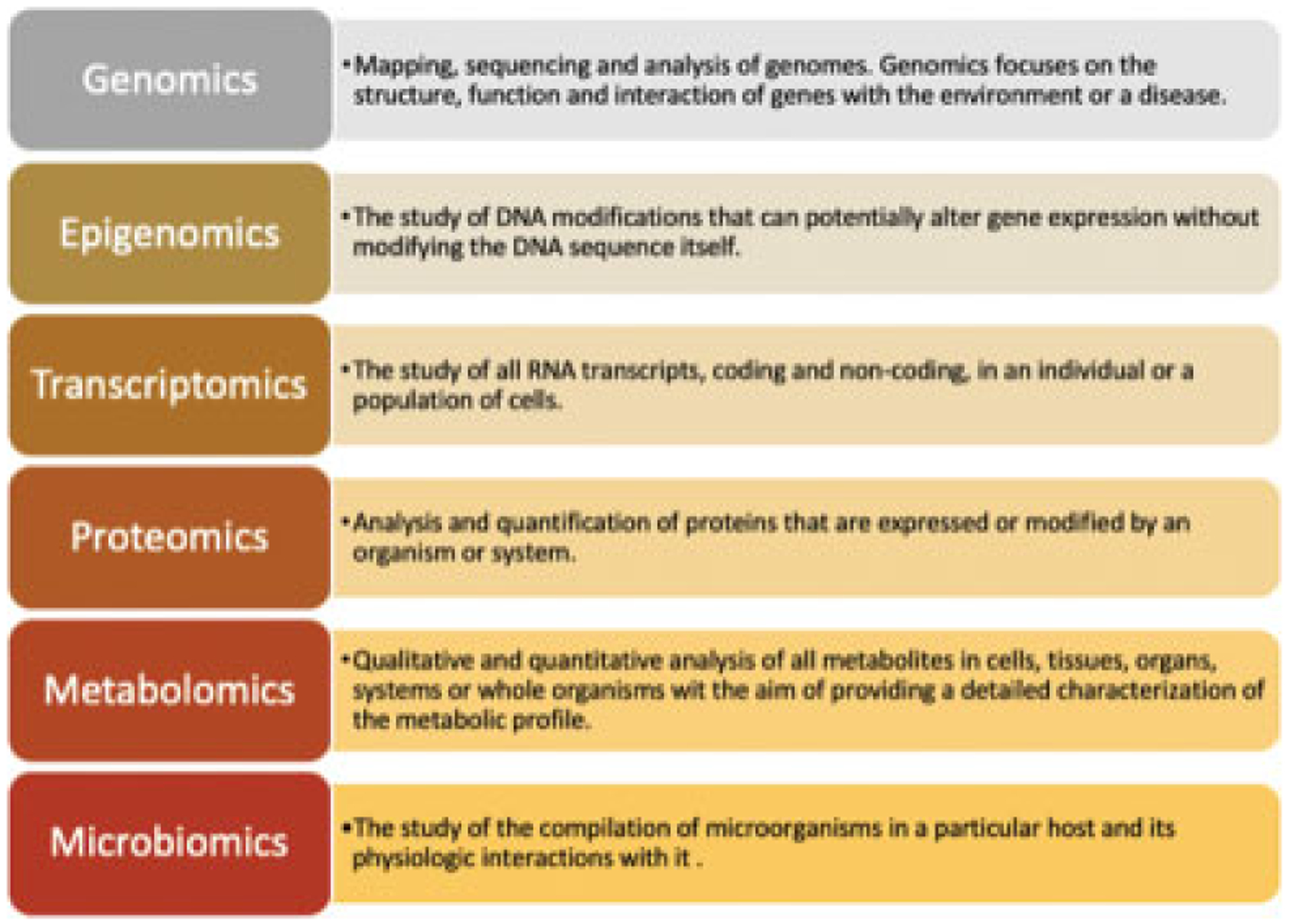
Precision medicine for obesity proposes a new paradigm in which the disease is stratified based on specific biological markers gathered predominantly from high-throughput or ‘omics assays (e.g., genomics, epigenomics, transcriptomics, and microbiomics among others), as well as from other clinical, physiological, and behavioral characteristics. These biological markers cannot only predict the risk of progression into developing other comorbidities, but can potentially be used to predict the response to specific therapies as well. This review aims to provide a perspective on the currently available data that can potentially pave the pathway toward identifying obesity phenotypes and the development of obesity precision medicine. First, we describe the traditional approach to treat obesity; second, we will summarize the currently available data on ‘omics and obesity; and third, we will describe how these data have been and can potentially be incorporated into precision medicine for obesity.
The Traditional Approach to Obesity Treatment
Obesity is typically defined as excessive body fat accumulation that can be categorized based on anthropometric measures. The most common tool to assess body fat is the BMI, which is weight (kg) divided by height squared (m2).9 BMI allows classifying individuals according to standardized ranges established from population studies. A BMI ≥30 kg/m2 defines obesity.2,10 In addition to total body excess fat, the location of fat distribution plays a major role in the risk of developing metabolic comorbidities, with central obesity and a consequential higher waist circumference (WC) posing a much higher comorbidity risk compared with lower-body adiposity distribution.11
Because these standard classifications based on anthropometric measures do not necessarily predict the risk of developing metabolic complications, other risk stratification systems have been developed to differentiate individuals at increased mortality risk who will benefit the most from weight-management interventions. One of such systems is the Edmonton Obesity Staging System (EOSS). The EOSS comprises a five-stage risk-stratification system that classifies obesity considering physical, psychological, and metabolic parameters.12 In longitudinal studies, EOSS has been a better indicator of mortality than BMI. In spite of the current evidence, the traditional approach to obesity treatment is still based on obesity severity defined by BMI.13
The current guidelines recognize that transitioning from a pro-obesogenic lifestyle to a healthy lifestyle is the cornerstone of obesity management. A multidisciplinary team, led by professionals with obesity medicine and/or nutrition training, facilitates this transition by helping patients navigate through a therapeutic algorithm. This therapeutic algorithm begins with lifestyle and behavior modifications that are recommended for anyone with a BMI greater than 25 kg/m2 with or without comorbidities, and escalates to add medications, bariatric endoscopic procedures, and/or bariatric surgery. The escalation through the algorithm depends on the individual’s initial BMI, weight loss goal, and response to treatment.6–8,14
The fundamental recommendations of a weight loss program include changes in diet to achieve a significant caloric restriction, increased activity to promote higher energy expenditure, and behavior therapy to modify habits related to eating and physical activity that contribute to excess weight. Although lifestyle and behavior modification are the basis of any weight loss program, weight loss outcomes are modest, a many patients do not respond to these changes, and maintaining weight loss remains a critical challenge.15–20
If lifestyle interventions fail or are not sufficient to achieve the weight loss goal, medical therapy is the next step in this obesity therapeutic algorithm. Antiobesity medications are generally indicated for individuals with a BMI ≥30 kg/m2 or those with a BMI ≥27 kg/m2 with weight-related comorbidities.6,8,21 Medications should not be used independently, but rather in combination with an intensive lifestyle intervention plan. Medications approved to treat obesity, combined with a lifestyle intervention plan, have resulted in a higher mean weight loss than placebo. However, there is high variability in the response to each medication with inconsistent predictors of treatment response being reported in the literature to a given drug.22,23 The current recommendations suggest a trial-and-error approach, in which medications should be prescribed for 12 to 16 weeks and then continue only in those with a body weight loss of greater than 5%.24,25
Bariatric endoscopy procedures are contemplated if patients cannot lose weight or maintain weight loss over time with diet, physical activity, behavioral modification with or without medications, that is, patients who have failed lifestyle interventions and medical attempts at weight loss.26 Bariatric surgery is a safe, efficacious, and durable treatment option for patients with severe obesity, defined by a BMI ≥40 kg/m2, or for patients with a BMI ≥35 kg/m2 with at least one obesity-associated comorbidity.27,28 Nevertheless, although overall highly successful, postoperative outcomes have high individual variability as well.29,30
Precision Medicine for Obesity
Precision medicine encompasses the concept of personalized preventive, diagnostic, and therapeutic measures that seek to improve disease stratification and maximize treatment effectiveness by considering individual variability.31 Precision medicine has five goals: to personalize care, to predict disease progression, to predict therapeutic success, to prevent disease progression, and to achieve an adequate therapy adherence32 (►Fig. 1). To accomplish these goals, we must integrate the current knowledge on obesity pathophysiology with data from ‘omics assays, accounting for the variability in lifestyle, psychosocial, and environmental factors that play a role in obesity development. This integration will allow bridging current evidence-based medical practice and precision medicine.33
Fig. 1.
Precision medicine integrates the biomarker data from -omics, lifestyle, psychosocial, and environmental factors.
In 2015, the White House launched the Precision Medicine Initiative to promote cooperative efforts by researchers, medical providers, and patients.34 The paradigm of precision medicine is not new, but the revolution of ‘omics profiling technologies, data available from electronic medical records and implementation of alternative classification systems, may allow more precise models to reach the ultimate goal. The National Institutes of Health initiative entitled Accumulating Data to Optimally Predict Obesity Treatment (ADOPT) Core Measures Project aims to develop an integrated model for biological, environmental, behavioral, and psychosocial domains to understand individual variability in obesity treatment.35
Omics and Obesity
A variety of high-throughput profiling technologies across biological tissues and fluids have identified genetic and epigenetic variations that translate into transcriptome, proteome, and metabolome changes. These changes may potentially participate in a disease’s pathophysiology and have led to the discovery of biomarkers that could be therapeutically targeted to discover novel mechanisms involved in the development and progression of a specific disease.36,37 In obesity, ‘omics biomarkers can provide information regarding the etiology of obesity and its pathophysiological connections with chronic disorders that eventually may help target obesity more efficiently and in an individualized manner.38 Although genes, epigenetic factors, transcripts, proteins, and metabolites are individually identified as a first step to understand pathways and mechanisms, the overall goal is to use multi-omics data for health assessment and prediction (►Fig. 2).
Fig. 2.

Multi-omics.
Genetics and Obesity
The sequencing of the human genome and the understanding of the regulation of energy homeostasis mediated by the leptin-melanocortin pathway led to the first well-recognized genes associated with obesity.39 These genes account for less than 1% of fully penetrant nonsyndromic obesity cases40,41 and 2 to 3% of syndromic monogenic obesity cases.42 The majority of obesity cases are polygenic. Polygenic obesity is attributed to the interplay between multiple loci. For instance, genetic studies have led to the discovering of heritable traits linked to obesity with heritability estimates ranging from 40 to 70% for BMI, 40 to 80% for WC, and 30 to 60% for waist-to-hip ratio (WHR).43–46
Sequencing of the human genome has been pivotal in identifying hundreds of gene variants or single nucleotide polymorphisms (SNPs) associated with obesity and its related traits through genome-wide linkage studies and genome-wide association studies. However, their contribution to obesity development is modest. For instance, although BMI’s heritability has been estimated to be up to 70%, the better-characterized SNPs and their effects do not account for more than 15% of the BMI’s variance. This gap suggests that there are many more gene variants that remain to be discovered.
Gene–environment interactions complement the heritability of obesity traits. Available data suggest that unfavorable dietary, activity, and environmental factors can amplify the genetic predisposition to obesity in individuals with certain SNPs. Because of the modest effect of SNPs on obesity traits, researchers have aggregated multiple SNPs into genetic risk scores. Genetic risk scores take into account estimated variations in multiple anthropometric traits based on demographic and environmental characteristics to increase the detection of gene–environment interactions.47 For instance, factors that can amplify the association of genetic risk scores with BMI include increased consumption of sugar-containing beverages, increased fried food intake, decreased physical activity, sleep deprivation, and low socioeconomic status.48–51
Epigenetics
Epigenetics is the study of reversible DNA modifications that can alter gene expression independently of changes in the nucleotide sequence. These modifications, influenced by genetic variants and environmental exposures, provide an additional layer of complexity in understanding obesity’s pathophysiology.52 DNA methylation is the best-studied epigenetic mark associated with pathways involved in obesity such as eating behavior, circadian rhythm, hunger, satiety, and lipid metabolism.53,54 Epigenome-wide association studies showed the correlation between methylation changes and clinical variables related to obesity like BMI, WC, WHR, and body fat percentage.55,56
DNA methylation profiles offer information about the pathophysiology of obesity and the predisposition to comorbidities. Weight loss intervention studies involving dietary factors, physical activity, and/or surgical treatments demonstrated the reversibility of cell-type–specific obesity-associated epigenetic changes.57–59 Presence of these changes can improve the metabolic outcome to certain therapies and may allow predicting who is going to respond better to a certain therapy. These observed methylation variations, without demonstrated clinical significance, are unlikely to result in the generation of precision obesity therapies.60,61 However, baseline methylation patterns may serve as a diagnostic biomarker or prognostic tool.
Transcriptomics
Transcriptomics is the study of all RNA transcripts in an individual or a population of cells, including coding and noncoding mRNA. Noncoding regions include a rich diversity of functional units critical for protein regulation and other cellular processes.62 The role of transcriptomics on obesity is slowly advancing. For instance, multiple associations and validation studies have demonstrated that small nucleolar RNAs are associated with food intake and body weight in patients with Prader–Willi syndrome.63 Similarly, microRNAs have been associated with metabolic pathways involved in adipogenesis and adipocyte differentiation.64
RNA sequencing allows the quantification of gene expression and provides a better understanding of cellular functions. For instance, sequencing technology advances have allowed researchers to measure gene expression and comprehensively classify adipose tissue.65 The transcriptomics profiling of subcutaneous adipose tissue for patients undergoing surgical treatment has corroborated the role of adipose tissue on inflammation and subsequent effect on obesity development.66 However, the transcriptome-wide changes from adipose tissue after weight loss interventions may not be enough to use a therapeutic target or predict response to treatment.67
Metabolomics
Metabolomics is the qualitative and quantitative analysis of all metabolites at the cellular level, tissues, organs, systems, or whole organisms. Metabolomics studies provide a detailed characterization of the metabolic profile in response to genetic variations, and physiological or pathological conditions. Metabolites are small molecules that act as substrates, intermediates, or products of cellular functions. Each cell type has a distinctive and fluctuating metabolite collection that reflects the host’s genome-controlled physiological state and its relationship with the environment.68 In obesity, metabolomics studies aim to evaluate the changes in metabolites at the cellular level, with the goal of understanding the biochemical pathways and obtaining recognizable chemical patterns. Once these chemical patterns are identified, they become potential therapeutic targets.
Studies in children with obesity have found metabolomics profiles characterized by increased steroid derivatives such as dehydroepiandrosterone sulfate, highlighting the possible role of steroids in disease development.69 In adults, obesity is associated with profiles containing higher levels of aromatic amino acids (phenylalanine and tyrosine), branched-chained amino acids (BCAAs; leucine, isoleucine, and valine), and products of nucleotide metabolism (uric acid and urate).70 Among adult patients with obesity, subjects with associated metabolic comorbidities presented increased levels in BCAAs, α-aminoadipic acid, and acylcarnitines.71 Based on these associations, researchers have been able to identify metabolic signatures related to obesity traits (e.g., BMI) and metabolic comorbidities associated with the disease. For instance, patients with obesity can present specific metabolomics patterns indicative of impaired glucose and lipid metabolism.69
Dietary interventions indicate that long-term weight loss can improve pathologic metabolomics profiles and decrease the risk of metabolic comorbidities.72 Furthermore, acute intervention studies have addressed the effect of diet on the metabolic profile with the potential to predict the risk of metabolic comorbidities and an individual’s response to dietary interventions.73
Microbiota
The microbiota comprises various interactive coexisting bacteria, archaea, bacteriophages, viruses, and fungi that have coevolved with a particular host.74 The human gut microbiota possesses a genomic repertoire much greater than the human genome and has physiologic roles in food digestion, drug metabolism, intestinal endocrine function, neurological signaling, gut epithelial cells renewal, and immune system training.75 The gut microbiota and its physiologic interactions with the host can be influenced by internal factors (e.g., genetics and anatomy, among others) and external elements (e.g., diet, exercise, and medications, among others).76–78
Animal studies have demonstrated the ability of intestinal microbiota to regulate energy metabolism and food intake. For instance, after a high-fat diet, there is an increase in Firmicutes: Bacteroidetes ratio, which can contribute to metabolic endotoxemia.79 The metabolic endotoxemia alters the gut–brain axis, mainly by affecting satiety signals.80 The gut microbiota also has the ability to modulate bile acid metabolism by changing the bile acid pool size and composition.81 The bile acid pathway participates in food intake regulation, food absorption, and glucose metabolism.82
Despite the absence of a standardized definition of a healthy gut microbiome, metagenome-wide association studies comparing individuals with obesity and lean individuals have shown differences in bacteria quantification and diversity, and microbial pathways. For instance, obesity is associated with an increase in short-chain fatty acid–producing bacteria, such as Roseburia intestinalis and Eubacterium ventriosum, and a decrease in glutamate-fermenting bacteria, such as Bacteroides thetaiotaomicron.83,84 On the other hand, intestinal microbiota from lean individuals to recipients with metabolic syndrome showed improvements in glucose metabolism.85 Dietary interventions in patients with obesity and microbiota analysis after Roux-en-Y gastric bypass validated that both interventions increased microbiome diversity, resulting in increased microbial utilization of macro- and micronutrients.86
Pharmacogenomics
Pharmacogenomics studies the association between gene variants and drug-metabolizing enzymes, transporters and receptors, and its impact on a specific medication response.87 Pharmacogenomics could partially explain the heterogeneous response to weight loss medications observed in clinical trials, or, conversely, the weight gain associated with certain prescription drugs. For instance, variants of the insulin receptor gene INSR and the glucagon-like peptide receptor gene GLP-1R targeted by topiramate and liraglutide, respectively, have been associated with a differential treatment response.88–90 Three silent SNPs in the gene encoding the pancreatic lipase were shown to influence the efficacy of orlistat.91 In the same way, 13 SNPs have been strongly associated with weight or BMI changes secondary to antipsychotic medications use.92
Nutrigenetics and Nutrigenomics
Diet interacts with genes to affect metabolic pathways and homeostatic control. The effect of diet on these systems varies widely among individuals. The development of nutrigenetics and nutrigenomics aims to understand the interaction between diet and disease. Nutrigenetics, on the one hand, is the science studying the impact of genetic variation on dietary response. Nutrigenomics, on the other hand, attempts to explain the effect of diet on gene expression.93 Available evidence has led to the understanding of how SNPs interact with diet and how dietary components affect a specific gene variant–associated phenotype. Additionally, high-resolution biotechnologies have made possible assessing the effect of nutrition on histone methylation, RNA transcription, protein synthesis, and metabolite synthesis. Population studies have analyzed candidate genes, their SNPs, and the relation with obesity traits. These SNPs–diet associations regulate food intake energy balance, insulin signaling, inflammatory response, and pathways of lipid, lipoprotein, and glucose metabolism.94,95 The goal of these two sciences is to develop personalized dietary interventions to prevent or treat diseases.
Toward Precision Medicine for Obesity: Major Obesity Precision Medicine Initiatives
High-resolution biotechnologies have so far delivered information about a myriad of biological variants that contribute to obesity development. In some instances, these variants have helped with the identification of pathophysiologic processes involved in obesity and therefore have become potential therapeutic targets to individualize obesity treatment. Although there is a significant amount of relevant information about these variants, its applicability to develop individualized therapeutic strategies for obesity remains limited.
Based on a deeper understanding on how some of these biological variants contribute to obesity, researchers have been able to develop therapeutic approaches that can potentially have a greater impact on obesity treatment outcomes compared with current standard of care. Most of these approaches remain investigational at the moment. We summarize this information below:
Genetics: The recognition of the genes associated with the leptin-melanocortin pathway has led to the development of the first gene-directed obesity treatments. The use of recombinant leptin in children with leptin deficiency proves the relevance and efficacy of this targeted therapy.96 More recently, the MC4R agonist (setmelanotide) has become a promising drug to treat hyperphagia caused by POMC or LEPR deficiency.97,98 In spite of such important advances, pharmacologic treatment options for other genetic defects associated with obesity are still lacking. Current data pave the way for future therapeutic possibilities for precision medicine, especially for monogenic and syndromic obesity.
Nutrigenetics/Nutrigenomics: The aim of these sciences is to identify patients who will benefit from genotype-based tailored dietary approaches. In this context, researchers have developed customized weight loss strategies focused on calorie-restricted diets based on gene–diet interactions. To date, most studies incorporating genetic testing into dietary interventions have failed to demonstrate a beneficial weight loss effect.99–102 In spite of this, there is currently an increased availability of direct-to-consumer genetic testing offering suggestions for personalized lifestyle intervention based on the presence of gene variants that have been linked to obesity, its traits, and its interactions with diet. Although attractive for individualized care, the clinical efficacy of these tests has not been validated in the clinical trials that have been conducted to date.
Pharmacogenetics: The ultimate goal of pharmacogenomics is to maximize the efficiency and safety of an individual’s response to pharmacologic agents. Within this field, as described earlier, few genetic variants that affect the individual’s susceptibility for antiobesity medications’ adverse effects and/or weight loss response have been identified and could be used to maximize response to treatment in clinical practice.88–91,103 Furthermore, in spite of the available evidence on the effect of certain genetic variants on the predisposition to gain weight with some medications, more research is needed to develop specific guidelines.92
- Microbiomics: The gut microbiota plays a crucial role in energy homeostasis and feeding behavior. There is an association between obesity and specific changes within its composition76,78,81,104 Microbiota’s shifts between health and disease could potentially be used to identify specific microbiome signatures. These signatures can in turn be used to build statistical models to identify who is at risk of a disease, who is at risk of disease progression and complications, and could also be used to distinguish therapy responders from nonresponders.105 Consequently, microbiota manipulation to foster the growth of “healthy” bacteria has been proposed as a potentially valuable therapeutic approach to combat obesity. Currently, possible clinical applications for microbiota manipulation include diet, prebiotics, probiotics, and fecal matter transplant.
- Microbiota-based personalized nutrition may be designed by identifying particular microbiota signatures and their associated metabolic properties. Dietary macronutrient changes and/or supplements lead to significant changes in the human gut microbiota.106 A low-carbohydrate diet, for example, results in reduced levels of fecal butyrate-producing bacteria.107 Butyrate can contribute to food intake and energy expenditure regulation by inducing GLP-1 and PYY secretion.75 Microbiota’s changes through an optimal diet could provide a practical approach for the treatment and prevention of obesity. One limitation of this approach, however, is that in addition to food, the gut microbiota’s composition is influenced by several other factors that render it more complicated to assess its collective responsiveness and clinical consequences.
- Prebiotics are nondigestible foods used by intestinal bacteria and have the potential of beneficially affecting the host’s physiology. Studies have shown promising clinical applications. For instance, supplementation with oligofructose, an energy substrate for bacteria, has been associated with increased satiety and decreased body weight in the pediatric population.108–110
- Probiotics are living microorganisms that give a health advantage to the host when delivered in appropriate quantities.111 Currently, there is little information available on the efficacy and safety of probiotic formulations. There are some data suggesting that a probiotic mixture containing Lactobacillus, Lactococcus and Bifidobacterium, reduced body weight, BMI, WC, and WHR.112
- Fecal matter transplant has been used to treat patients with chronic gastrointestinal and inflammatory bowel disorders.113 Despite the absence of a healthy microbiome signature, interventions using lean donor fecal matter transplant to recipients with metabolic syndrome demonstrated short-term improvements in metabolic disorders.114 Nevertheless, few human studies have shown a definite beneficial long-term effect on metabolic disorders.115
The applicability of other omics (i.e., epigenomics, transcriptomics, and metabolomics) for individualizing obesity therapy relies on identifying signatures that can predict disease progression, weight loss in response to specific therapies, or improvement in comorbidities. Studies suggest that the baseline epigenetic methylation patterns and metabolic parameters can predict a significant proportion of weight loss variability after weight loss interventions (diet modification and sleeve gastrectomy).57,116–118 Researchers have also used subcutaneous adipose tissue to define a transcriptomics profile that may predict glycemic outcomes after dietary interventions.67 Overall, the data from these high-resolution biotechnologies could potentially provide a more in-depth view of the disease’s course. However, additional validation studies will be needed to consider any of these profiles’ specific biomarkers for obesity or use them as part of predicting models.
Phenotypes: The term “phenotype” refers to the observable characteristics of an organism determined by gene expression and environmental influences upon these genes.119 Ideally, phenotyping would lead to disease classification based on genetic and molecular alterations, pathophysiologic changes, and clinical features. This characterization would potentially enhance the predictability of treatment response and overall improve clinical outcomes in the form of precision medicine.120 Given the heterogeneity of obesity, current strategies have mostly focused on clinical phenotyping. Clinical phenotyping aims to identify unique patient quantitative traits based on pathophysiological and behavioral changes associated with obesity. These quantitative traits can lead to the discovery of clinical and molecular biomarkers that can, in turn, be used to individualize obesity treatment and predict the response to treatment. From our current understanding of food intake regulation121 and the availability of validated tests to measure biological biomarkers involved in energy balance, researchers have so far identified the following quantitative traits: satiety and satiation, gastric motility, behavioral factors, and gastric sensorimotor features.122–124 Targeting therapy to reverse abnormalities in these quantitative traits could potentially enhance the response to treatment. For instance, patients with obesity and accelerated gastric emptying would benefit the most from GLP-1 agonists as they slow down gastric emptying125–128; and patients with obesity and abnormal satiation would benefit the most from phentermine topiramate.123 Proof-of-concept trials on pharmacotherapy and endoscopic interventions suggest that this strategy could increase treatment success.129
Conclusions
The traditional approach to treat obesity focuses on the assumption that “one size fits all.” This current standard of care involves escalation of therapy from lifestyle interventions to bariatric surgery based on BMI, and does not take into consideration the major heterogeneity associated with this condition. As a result, we have observed underwhelming responses to current antiobesity therapies. The lack of established therapeutic options for obesity, paired with its rising prevalence, justifies the search for treatment approaches to complement current strategies. Ideally, these new strategies would be best suited to individual patients for enhanced effectiveness and tolerability via precision medicine.
Precision medicine incorporates the idea of tailored care allowing a better classification of a disease with the overall goal of improving the efficiency of care by recognizing individual variability. The principle of precision medicine is not new, but high-resolution technologies based on “omics profiling,” has revolutionized its use. ‘Omics profiling has generated an increasingly comprehensive knowledge of obesity’s etiology, development, and progression, which can ultimately enable us to treat obesity, and any other disease, more effectively.
Precision medicine–based studies are paving the way for personalized treatment of obesity. A better understanding of biological variants has facilitated the development of therapeutic approaches that can potentially have a more significant impact on obesity treatment outcomes. Nowadays, several of these methods remain investigational and their therapeutic effectiveness is yet to be determined. While the use of multi-omics evidence has given a more in-depth understanding of obesity progression, further confirmation trials are required to consider or use some of these biomarkers for obesity as part of predictive models. The overall goal is to fuse multi-omics data into precision medicine for obesity to optimize therapeutic success.
Funding
National Institute of Diabetes and Digestive and Kidney Diseases http://dx.doi.org/10.13039/100000062 DK114460 Mayo Foundation for Medical Education and Research http://dx.doi.org/10.13039/100007048 CIM
Conflict of Interest
A.A. reports grants from NIH-NIDDK, NIH-NIDDK, NIH-NIDDK, ANMS, Mayo Clinic Center for Individualized Medicine, and Mayo Clinic, during the conduct of the study; other from Gila Therapeutics and Phenomix Sciences; personal fees from Rhythm Pharmaceuticals, General Mills, and Gila Therapeutics, outside the submitted work. In addition, A.A. has a Patent Cooperation Treaty (US 62/589,915) licensed to Phenomix Sciences.
Footnotes
Disclosures
A.A. is a stockholder in Gila Therapeutics, Phenomix Sciences; he serves as a consultant for Rhythm Pharmaceuticals and General Mills.
References
- 1.Afshin A, Forouzanfar MH, Reitsma MB, et al. ; GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017;377(01):13–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 2009;9:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nyberg ST, Batty GD, Pentti J, et al. Obesity and loss of disease-free years owing to major non-communicable diseases: a multi-cohort study. Lancet Public Health 2018;3(10):e490–e497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Waters H, Graf M. America’s Obesity Crisis:The Health and Economic Costs of Excess Weight. The Milken Institute; October 26, 2018 [Google Scholar]
- 5.Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med 2019;381(25):2440–2450 [DOI] [PubMed] [Google Scholar]
- 6.Jensen MD, Ryan DH, Apovian CM, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2014;129(25, Suppl 2):S102–S138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fitzpatrick SL, Wischenka D, Appelhans BM, et al. ; Society of Behavioral Medicine. An evidence-based guide for obesity treatment in primary care. Am J Med 2016;129(01):115.e1–115.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Acosta A, Streett S, Kroh MD, et al. White Paper AGA: POWER - Practice Guide on Obesity and Weight Management, Education, and Resources. Clin Gastroenterol Hepatol 2017;15(05): 631–649.e10 [DOI] [PubMed] [Google Scholar]
- 9.Deurenberg P, Weststrate JA, Seidell JC. Body mass index as a measure of body fatness: age- and sex-specific prediction formulas. Br J Nutr 1991;65(02):105–114 [DOI] [PubMed] [Google Scholar]
- 10.WHO. Obesity: Preventing and Managing the Global Epidemic. World Health Organization; 2000 [PubMed] [Google Scholar]
- 11.Ross R, Neeland IJ, Yamashita S, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol 2020;16(03):177–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma AM, Kushner RF. A proposed clinical staging system for obesity. Int J Obes 2009;33(03):289–295 [DOI] [PubMed] [Google Scholar]
- 13.Padwal RS, Pajewski NM, Allison DB, Sharma AM. Using the Edmonton obesity staging system to predict mortality in a population-representative cohort of people with overweight and obesity. CMAJ 2011;183(14):E1059–E1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garvey WT, Mechanick JI, Brett EM, et al. ; Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract 2016;22 (Suppl 3):1–203 [DOI] [PubMed] [Google Scholar]
- 15.Knowler WC, Barrett-Connor E, Fowler SE, et al. ; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346(06):393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring) 2014;22(01):5–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med 2009;360(09):859–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McMillan-Price J, Petocz P, Atkinson F, et al. Comparison of 4 diets of varying glycemic load on weight loss and cardiovascular risk reduction in overweight and obese young adults: a randomized controlled trial. Arch Intern Med 2006;166(14):1466–1475 [DOI] [PubMed] [Google Scholar]
- 19.Das SK, Gilhooly CH, Golden JK, et al. Long-term effects of 2 energy-restricted diets differing in glycemic load on dietary adherence, body composition, and metabolism in CALERIE: a 1-y randomized controlled trial. Am J Clin Nutr 2007;85(04): 1023–1030 [DOI] [PubMed] [Google Scholar]
- 20.Slentz CA, Duscha BD, Johnson JL, et al. Effects of the amount of exercise on body weight, body composition, and measures of central obesity: STRRIDE–a randomized controlled study. Arch Intern Med 2004;164(01):31–39 [DOI] [PubMed] [Google Scholar]
- 21.Apovian CM, Aronne LJ, Bessesen DH, et al. ; Endocrine Society. Pharmacological management of obesity: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2015;100 (02):342–362 [DOI] [PubMed] [Google Scholar]
- 22.Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA 2014;311(01):74–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dong Z, Xu L, Liu H, Lv Y, Zheng Q, Li L. Comparative efficacy of five long-term weight loss drugs: quantitative information for medication guidelines. Obes Rev 2017;18(12):1377–1385 [DOI] [PubMed] [Google Scholar]
- 24.Fujioka K, O’Neil PM, Davies M, et al. Early weight loss with Liraglutide 3.0 mg predicts 1-year weight loss and is associated with improvements in clinical markers. Obesity (Silver Spring) 2016;24(11):2278–2288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fujioka K, Plodkowski R, O’Neil PM, Gilder K, Walsh B, Greenway FL. The relationship between early weight loss and weight loss at 1 year with naltrexone ER/bupropion ER combination therapy. Int J Obes 2016;40(09):1369–1375 [DOI] [PubMed] [Google Scholar]
- 26.Abu Dayyeh BK, Kumar N, Edmundowicz SA, et al. ; ASGE Bariatric Endoscopy Task Force and ASGE Technology Committee. ASGE Bariatric Endoscopy Task Force systematic review and meta-analysis assessing the ASGE PIVI thresholds for adopting endoscopic bariatric therapies. Gastrointest Endosc 2015;82(03): 425–38.e5 [DOI] [PubMed] [Google Scholar]
- 27.Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 2009;122(03):248–256.e5 [DOI] [PubMed] [Google Scholar]
- 28.Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg 2014;149 (03):275–287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Christou NV, Look D, Maclean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg 2006;244(05):734–740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sjöström L Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med 2013;273(03):219–234 [DOI] [PubMed] [Google Scholar]
- 31.Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med 2015;372(09):793–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gameiro GR, Sinkunas V, Liguori GR, Auler-Júnior JOC. Precision medicine: changing the way we think about healthcare. Clinics (São Paulo) 2018;73:e723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beckmann JS, Lew D. Reconciling evidence-based medicine and precision medicine in the era of big data: challenges and opportunities. Genome Med 2016;8(01):134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hudson K, Lifton R, Patrick-Lake B. The Precision Medicine Initiative Cohort Program—Building a Research Foundation for 21st Century Medicine. Precision Medicine Initiative (PMI) Working Group Report to the Advisory Committee to the Director 2015 [Google Scholar]
- 35.MacLean PS, Rothman AJ, Nicastro HL, et al. The Accumulating Data to Optimally Predict Obesity Treatment (ADOPT) Core Measures Project: rationale and approach. Obesity (Silver Spring) 2018;26(Suppl 2):S6–S15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen R, Mias GI, Li-Pook-Than J, et al. Personal omics profiling reveals dynamic molecular and medical phenotypes. Cell 2012; 148(06):1293–1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hasin Y, Seldin M, Lusis A. Multi-omics approaches to disease. Genome Biol 2017;18(01):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aleksandrova K, Egea Rodrigues C, Floegel A, Ahrens W. Omics biomarkers in obesity: novel etiological insights and targets for precision prevention. Curr Obes Rep 2020;9(03):219–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature 1994;372(6505):425–432 [DOI] [PubMed] [Google Scholar]
- 40.Naggert J, Harris T, North M. The genetics of obesity. Curr Opin Genet Dev 1997;7(03):398–404 [DOI] [PubMed] [Google Scholar]
- 41.Chen D, Garg A. Monogenic disorders of obesity and body fat distribution. J Lipid Res 1999;40(10):1735–1746 [PubMed] [Google Scholar]
- 42.Kaur Y, de Souza RJ, Gibson WT, Meyre D. A systematic review of genetic syndromes with obesity. Obes Rev 2017;18(06):603–634 [DOI] [PubMed] [Google Scholar]
- 43.Schousboe K, Visscher PM, Erbas B, et al. Twin study of genetic and environmental influences on adult body size, shape, and composition. Int J Obes Relat Metab Disord 2004;28(01):39–48 [DOI] [PubMed] [Google Scholar]
- 44.Farooqi IS, O’Rahilly S. Genetic factors in human obesity. Obes Rev 2007;8(Suppl 1):37–40 [DOI] [PubMed] [Google Scholar]
- 45.Qi L, Kang K, Zhang C, et al. Fat mass-and obesity-associated (FTO) gene variant is associated with obesity: longitudinal analyses in two cohort studies and functional test. Diabetes 2008;57(11):3145–3151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diels S, Vanden Berghe W, Van Hul W. Insights into the multifactorial causation of obesity by integrated genetic and epigenetic analysis. Obes Rev 2020;21(07):e13019. [DOI] [PubMed] [Google Scholar]
- 47.Wray NR, Goddard ME, Visscher PM. Prediction of individual genetic risk to disease from genome-wide association studies. Genome Res 2007;17(10):1520–1528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brunkwall L, Chen Y, Hindy G, et al. Sugar-sweetened beverage consumption and genetic predisposition to obesity in 2 Swedish cohorts. Am J Clin Nutr 2016;104(03):809–815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Qi Q, Chu AY, Kang JH, et al. Fried food consumption, genetic risk, and body mass index: gene-diet interaction analysis in three US cohort studies. BMJ 2014;348:g1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ahmad S, Rukh G, Varga TV, et al. ; InterAct Consortium DIRECT Consortium. Gene × physical activity interactions in obesity: combined analysis of 111,421 individuals of European ancestry. PLoS Genet 2013;9(07):e1003607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Celis-Morales C, Lyall DM, Guo Y, et al. Sleep characteristics modify the association of genetic predisposition with obesity and anthropometric measurements in 119,679 UK Biobank participants. Am J Clin Nutr 2017;105(04):980–990 [DOI] [PubMed] [Google Scholar]
- 52.Milagro FI, Mansego ML, De Miguel C, Martínez JA. Dietary factors, epigenetic modifications and obesity outcomes: progresses and perspectives. Mol Aspects Med 2013;34(04): 782–812 [DOI] [PubMed] [Google Scholar]
- 53.Rohde K, Keller M, la Cour Poulsen L, Blüher M, Kovacs P, Böttcher Y. Genetics and epigenetics in obesity. Metabolism 2019; 92:37–50 [DOI] [PubMed] [Google Scholar]
- 54.Bell CG. The epigenomic analysis of human obesity. Obesity (Silver Spring) 2017;25(09):1471–1481 [DOI] [PubMed] [Google Scholar]
- 55.Wahl S, Drong A, Lehne B, et al. Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature 2017;541(7635):81–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dick KJ, Nelson CP, Tsaprouni L, et al. DNA methylation and body-mass index: a genome-wide analysis. Lancet 2014;383 (9933):1990–1998 [DOI] [PubMed] [Google Scholar]
- 57.Barres R, Kirchner H, Rasmussen M, et al. Weight loss after gastric bypass surgery in human obesity remodels promoter methylation. Cell Rep 2013;3(04):1020–1027 [DOI] [PubMed] [Google Scholar]
- 58.Rönn T, Volkov P, Davegårdh C, et al. A six months exercise intervention influences the genome-wide DNA methylation pattern in human adipose tissue. PLoS Genet 2013;9(06): e1003572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Milagro FI, Campión J, Cordero P, et al. A dual epigenomic approach for the search of obesity biomarkers: DNA methylation in relation to diet-induced weight loss. FASEB J 2011;25(04): 1378–1389 [DOI] [PubMed] [Google Scholar]
- 60.Cordero P, Campion J, Milagro FI, et al. Leptin and TNF-alpha promoter methylation levels measured by MSP could predict the response to a low-calorie diet. J Physiol Biochem 2011;67(03): 463–470 [DOI] [PubMed] [Google Scholar]
- 61.Nicoletti CF, Nonino CB, de Oliveira BAP, et al. DNA methylation and hydroxymethylation levels in relation to two weight loss strategies: energy-restricted diet or bariatric surgery. Obes Surg 2016;26(03):603–611 [DOI] [PubMed] [Google Scholar]
- 62.Wang Z, Gerstein M, Snyder M. RNA-Seq: a revolutionary tool for transcriptomics. Nat Rev Genet 2009;10(01):57–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Amri EZ, Scheideler M. Small non coding RNAs in adipocyte biology and obesity. Mol Cell Endocrinol 2017;456:87–94 [DOI] [PubMed] [Google Scholar]
- 64.Ortiz-Dosal A, Rodil-García P, Salazar-Olivo LA. Circulating microRNAs in human obesity: a systematic review. Biomarkers 2019;24(06):499–509 [DOI] [PubMed] [Google Scholar]
- 65.Deutsch A, Feng D, Pessin JE, Shinoda K. The impact of single-cell genomics on adipose tissue research. Int J Mol Sci 2020;21(13): 4773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.González-Plaza JJ, Gutiérrez-Repiso C, García-Serrano S, et al. Effect of Roux-en-Y gastric bypass-induced weight loss on the transcriptomic profiling of subcutaneous adipose tissue. Surg Obes Relat Dis 2016;12(02):257–263 [DOI] [PubMed] [Google Scholar]
- 67.Armenise C, Lefebvre G, Carayol J, et al. Transcriptome profiling from adipose tissue during a low-calorie diet reveals predictors of weight and glycemic outcomes in obese, nondiabetic subjects. Am J Clin Nutr 2017;106(03):736–746 [DOI] [PubMed] [Google Scholar]
- 68.Holmes E, Wilson ID, Nicholson JK. Metabolic phenotyping in health and disease. Cell 2008;134(05):714–717 [DOI] [PubMed] [Google Scholar]
- 69.Rangel-Huerta OD, Pastor-Villaescusa B, Gil A. Are we close to defining a metabolomic signature of human obesity? A systematic review of metabolomics studies. Metabolomics 2019;15 (06):93–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Baker PR II, Boyle KE, Koves TR, et al. Metabolomic analysis reveals altered skeletal muscle amino acid and fatty acid handling in obese humans. Obesity (Silver Spring) 2015;23(05):981–988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gao X, Zhang W, Wang Y, et al. Serum metabolic biomarkers distinguish metabolically healthy peripherally obese from unhealthy centrally obese individuals. Nutr Metab (Lond) 2016;13 (01):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cirulli ET, Guo L, Leon Swisher C, et al. Profound perturbation of the metabolome in obesity is associated with health risk. Cell Metab 2019;29(02):488–500.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Badoud F, Lam KP, Perreault M, Zulyniak MA, Britz-McKibbin P, Mutch DM. Metabolomics reveals metabolically healthy and unhealthy obese individuals differ in their response to a caloric challenge. PLoS One 2015;10(08):e0134613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The human microbiome project. Nature 2007;449 (7164):804–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fan Y, Pedersen O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol 2020;19(01):55–71 [DOI] [PubMed] [Google Scholar]
- 76.Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature 2009;457(7228):480–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dethlefsen L, Relman DA. Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci U S A 2011;108 (Suppl 1):4554–4561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Santacruz A, Marcos A, Wärnberg J, et al. ; EVASYON Study Group. Interplay between weight loss and gut microbiota composition in overweight adolescents. Obesity (Silver Spring) 2009;17(10): 1906–1915 [DOI] [PubMed] [Google Scholar]
- 79.Ding S, Chi MM, Scull BP, et al. High-fat diet: bacteria interactions promote intestinal inflammation which precedes and correlates with obesity and insulin resistance in mouse. PLoS One 2010;5 (08):e12191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vaughn AC, Cooper EM, DiLorenzo PM, et al. Energy-dense diet triggers changes in gut microbiota, reorganization of gut-brain vagal communication and increases body fat accumulation. Acta Neurobiol Exp (Warsz) 2017;77(01):18–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sayin SI, Wahlström A, Felin J, et al. Gut microbiota regulates bile acid metabolism by reducing the levels of tauro-beta-muricholic acid, a naturally occurring FXR antagonist. Cell Metab 2013;17 (02):225–235 [DOI] [PubMed] [Google Scholar]
- 82.Calderon G, McRae A, Rievaj J, et al. Ileo-colonic delivery of conjugated bile acids improves glucose homeostasis via colonic GLP-1-producing enteroendocrine cells in human obesity and diabetes. EBioMedicine 2020;55:102759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tims S, Derom C, Jonkers DM, et al. Microbiota conservation and BMI signatures in adult monozygotic twins. ISME J 2013;7(04):707–717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Liu R, Hong J, Xu X, et al. Gut microbiome and serum metabolome alterations in obesity and after weight-loss intervention. Nat Med 2017;23(07):859–868 [DOI] [PubMed] [Google Scholar]
- 85.Vrieze A, Van Nood E, Holleman F, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 2012; 143(04):913–6.e7 [DOI] [PubMed] [Google Scholar]
- 86.Palleja A, Kashani A, Allin KH, et al. Roux-en-Y gastric bypass surgery of morbidly obese patients induces swift and persistent changes of the individual gut microbiota. Genome Med 2016;8 (01):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Relling MV, Evans WE. Pharmacogenomics in the clinic. Nature 2015;526(7573):343–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Li QS, Lenhard JM, Zhan Y, et al. A candidate-gene association study of topiramate-induced weight loss in obese patients with and without type 2 diabetes mellitus. Pharmacogenet Genomics 2016;26(02):53–65 [DOI] [PubMed] [Google Scholar]
- 89.de Luis DA, Diaz Soto G, Izaola O, Romero E. Evaluation of weight loss and metabolic changes in diabetic patients treated with liraglutide, effect of RS 6923761 gene variant of glucagon-like peptide 1 receptor. J Diabetes Complications 2015;29(04):595–598 [DOI] [PubMed] [Google Scholar]
- 90.Chedid V, Vijayvargiya P, Carlson P, et al. Allelic variant in the glucagon-like peptide 1 receptor gene associated with greater effect of liraglutide and exenatide on gastric emptying: a pilot pharmacogenetics study. Neurogastroenterol Motil 2018;30(07):e13313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.O’Connor A, Swick AG. Interface between pharmacotherapy and genes in human obesity. Hum Hered 2013;75(2–4):116–126 [DOI] [PubMed] [Google Scholar]
- 92.Zhang JP, Lencz T, Zhang RX, et al. Pharmacogenetic associations of antipsychotic drug-related weight gain: a systematic review and meta-analysis. Schizophr Bull 2016;42(06):1418–1437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fenech M, El-Sohemy A, Cahill L, et al. Nutrigenetics and nutrigenomics: viewpoints on the current status and applications in nutrition research and practice. J Nutrigenet Nutrigenomics 2011;4(02):69–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ramos-Lopez O, Milagro FI, Allayee H, et al. Guide for current nutrigenetic, nutrigenomic, and nutriepigenetic approaches for precision nutrition involving the prevention and management of chronic diseases associated with obesity. J Nutrigenet Nutrigenomics 2017;10(1–2):43–62 [DOI] [PubMed] [Google Scholar]
- 95.Heianza Y, Qi L. Gene-diet interaction and precision nutrition in obesity. Int J Mol Sci 2017;18(04):787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Farooqi IS, Jebb SA, Langmack G, et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N Engl J Med 1999;341(12):879–884 [DOI] [PubMed] [Google Scholar]
- 97.Clément K, van den Akker E, Argente J, et al. ; Setmelanotide POMC and LEPR Phase 3 Trial Investigators. Efficacy and safety of setmelanotide, an MC4R agonist, in individuals with severe obesity due to LEPR or POMC deficiency: single-arm, open-label, multicentre, phase 3 trials. Lancet Diabetes Endocrinol 2020;8 (12):960–970 [DOI] [PubMed] [Google Scholar]
- 98.Collet TH, Dubern B, Mokrosinski J, et al. Evaluation of a melanocortin-4 receptor (MC4R) agonist (Setmelanotide) in MC4R deficiency. Mol Metab 2017;6(10):1321–1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Celis-Morales C, Marsaux CF, Livingstone KM, et al. Can genetic-based advice help you lose weight? Findings from the Food4Me European randomized controlled trial. Am J Clin Nutr 2017;105 (05):1204–1213 [DOI] [PubMed] [Google Scholar]
- 100.Frankwich KA, Egnatios J, Kenyon ML, et al. Differences in weight loss between persons on standard balanced vs nutrigenetic diets in a randomized controlled trial. Clin Gastroenterol Hepatol 2015;13(09):1625–1632.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gardner CD, Trepanowski JF, Del Gobbo LC, et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS Randomized Clinical Trial. JAMA 2018; 319(07):667–679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Horne JR, Gilliland JA, O’Connor CP, Seabrook JA, Madill J. Change in weight, BMI, and body composition in a population-based intervention versus genetic-based intervention: the NOW Trial. Obesity (Silver Spring) 2020;28(08):1419–1427 [DOI] [PubMed] [Google Scholar]
- 103.Kranzler HR, Feinn R, Gelernter J, Pond T, Covault J. Topiramate’s reduction of body mass index in heavy drinkers: lack of moderation by a GRIK1 polymorphism. Exp Clin Psychopharmacol 2014;22(05):419–423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006;444(7122):1027–1031 [DOI] [PubMed] [Google Scholar]
- 105.Zeevi D, Korem T, Zmora N, et al. Personalized nutrition by prediction of glycemic responses. Cell 2015;163(05):1079–1094 [DOI] [PubMed] [Google Scholar]
- 106.Kolodziejczyk AA, Zheng D, Elinav E. Diet-microbiota interactions and personalized nutrition. Nat Rev Microbiol 2019;17 (12):742–753 [DOI] [PubMed] [Google Scholar]
- 107.Duncan SH, Belenguer A, Holtrop G, Johnstone AM, Flint HJ, Lobley GE. Reduced dietary intake of carbohydrates by obese subjects results in decreased concentrations of butyrate and butyrate-producing bacteria in feces. Appl Environ Microbiol 2007;73(04):1073–1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cani PD, Lecourt E, Dewulf EM, et al. Gut microbiota fermentation of prebiotics increases satietogenic and incretin gut peptide production with consequences for appetite sensation and glucose response after a meal. Am J Clin Nutr 2009;90(05): 1236–1243 [DOI] [PubMed] [Google Scholar]
- 109.Cani PD, Joly E, Horsmans Y, Delzenne NM. Oligofructose promotes satiety in healthy human: a pilot study. Eur J Clin Nutr 2006;60(05):567–572 [DOI] [PubMed] [Google Scholar]
- 110.Nicolucci AC, Hume MP, Martínez I, Mayengbam S, Walter J, Reimer RA. Prebiotics reduce body fat and alter intestinal microbiota in children who are overweight or with obesity. Gastroenterology 2017;153(03):711–722 [DOI] [PubMed] [Google Scholar]
- 111.FAO WHO. Probiotics in Food: Health and Nutritional Properties and Guidelines for Evaluation. FAO; 2006 [Google Scholar]
- 112.Michael DR, Jack AA, Masetti G, et al. A randomised controlled study shows supplementation of overweight and obese adults with lactobacilli and bifidobacteria reduces bodyweight and improves well-being. Sci Rep 2020;10(01):4183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Smits LP, Bouter KE, de Vos WM, Borody TJ, Nieuwdorp M. Therapeutic potential of fecal microbiota transplantation. Gastroenterology 2013;145(05):946–953 [DOI] [PubMed] [Google Scholar]
- 114.Kootte RS, Levin E, Salojärvi J, et al. Improvement of insulin sensitivity after lean donor feces in metabolic syndrome is driven by baseline intestinal microbiota composition. Cell Metab 2017;26(04):611–619.e6 [DOI] [PubMed] [Google Scholar]
- 115.Lee P, Yacyshyn BR, Yacyshyn MB. Gut microbiota and obesity: an opportunity to alter obesity through faecal microbiota transplant (FMT). Diabetes Obes Metab 2019;21(03):479–490 [DOI] [PubMed] [Google Scholar]
- 116.Huang YT, Maccani JZJ, Hawley NL, Wing RR, Kelsey KT, McCaffery JM. Epigenetic patterns in successful weight loss maintainers: a pilot study. Int J Obes 2015;39(05):865–868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Benton MC, Johnstone A, Eccles D, et al. An analysis of DNA methylation in human adipose tissue reveals differential modification of obesity genes before and after gastric bypass and weight loss. Genome Biol 2015;16(01):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kwon Y, Jang M, Lee Y, Ha J, Park S. Amino acid metabolites and slow weight loss in the early postoperative period after sleeve gastrectomy. J Clin Med 2020;9(08):E2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rice JP, Saccone NL, Rasmussen E. Definition of the phenotype. Adv Genet 2001;42:69–76 [DOI] [PubMed] [Google Scholar]
- 120.Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med 2012;18(05):716–725 [DOI] [PubMed] [Google Scholar]
- 121.Camilleri M Peripheral mechanisms in appetite regulation. Gastroenterology 2015;148(06):1219–1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Camilleri M, Acosta A. Gastrointestinal traits: individualizing therapy for obesity with drugs and devices. Gastrointest Endosc 2016;83(01):48–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Acosta A, Camilleri M, Shin A, et al. Quantitative gastrointestinal and psychological traits associated with obesity and response to weight-loss therapy. Gastroenterology 2015;148(03):537–546.e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Pajot G, Camilleri M, Calderon G, et al. Association between gastrointestinal phenotypes and weight gain in younger adults: a prospective 4-year cohort study. Int J Obes 2020;44(12): 2472–2478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Delgado-Aros S, Kim DY, Burton DD, et al. Effect of GLP-1 on gastric volume, emptying, maximum volume ingested, and postprandial symptoms in humans. Am J Physiol Gastrointest Liver Physiol 2002;282(03):G424–G431 [DOI] [PubMed] [Google Scholar]
- 126.Halawi H, Khemani D, Eckert D, et al. Effects of liraglutide on weight, satiation, and gastric functions in obesity: a randomised, placebo-controlled pilot trial. Lancet Gastroenterol Hepatol 2017;2(12):890–899 [DOI] [PubMed] [Google Scholar]
- 127.Hjerpsted JB, Flint A, Brooks A, Axelsen MB, Kvist T, Blundell J. Semaglutide improves postprandial glucose and lipid metabolism, and delays first-hour gastric emptying in subjects with obesity. Diabetes Obes Metab 2018;20(03):610–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Acosta A, Camilleri M, Burton D, et al. Exenatide in obesity with accelerated gastric emptying: a randomized, pharmacodynamics study. Physiol Rep 2015;3(11):e12610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lopez-Nava G, Jaruvongvanich V, Storm AC, et al. Personalization of endoscopic bariatric and metabolic therapies based on physiology: a prospective feasibility study with a single fluid-filled intragastric balloon. Obes Surg 2020;30(09):3347–3353 [DOI] [PubMed] [Google Scholar]


