Abstract
Purpose/Objective:
Health care providers’ attitudes of marginalized groups can be key factors that contribute to health care access and outcome disparities because of their influence on patient encounters as well as clinical decision-making. Despite a growing body of knowledge linking disparate health outcomes to providers’ clinical decision making, less research has focused on providers’ attitudes about disability. The aim of this study was to examine providers’ explicit and implicit disability attitudes, interactions between their attitudes, and correlates of explicit and implicit bias.
Research Method/Design:
We analyzed secondary data from 25,006 health care providers about their disability attitudes. In addition to analyzing people’s explicit and implicit attitudes (Disability Attitudes Implicit Association Test), we used Son Hing, Chung-Yan, Hamilton, & Zanna’s (2008) model of two-dimensional prejudice to compare provider’s explicit and implicit attitudes. Finally, we used linear regression models to examine correlates of providers’ explicit and implicit attitudes.
Results:
While on average, provider’s explicit attitudes (M = 4.41) indicated little prejudice, their implicit attitudes (M = 0.54) revealed they moderately preferred nondisabled people—they were aversive ableists. Correlates of providers’ explicit and implicit attitudes also included age, gender, political orientation, and having relationships with disability (friends, family, and being a person with disability).
Conclusions/Implications:
This study revealed that despite a majority of providers self-reporting not being biased against people with disabilities, implicitly, the overwhelming majority were biased. This study’s findings can be used to better understand how provider disability bias can contribute to inequitable health care access and health outcomes for people with disabilities.
Keywords: people with disabilities, explicit attitudes, implicit attitudes, health care, disparities
Introduction
Recognizing, understanding, and, ultimately, eliminating the factors that produce disparate health care service provision and health outcomes is an overarching goal of many governments and health organizations on a global scale (Orgera & Artiga, 2018). Health care disparities are avoidable differences in access, quality, and services between certain groups, often social minorities, that contribute to disparate health outcomes (Nelson, Stith, & Smedley, 2002). Research indicates people with disabilities (PWD) have not only poorer health than nondisabled people but also shorter life expectancies (Altman & Bernstein, 2008; Iezzoni, 2011; Krahn, Walker, & Correa-De-Araujo, 2015). For example, PWD have higher rates of chronic disease compared to their nondisabled peers, which is attributed to factors such as referral to fewer preventive and health promotion services (Reichard, Stolzle, & Fox, 2011). The health disparities faced by PWD are not necessarily due to their impairments or health behaviors; health care providers’ beliefs and attitudes about social minorities and marginalized groups have been identified as key factors that contribute to both health care access and outcome disparities because they influence behaviors in patient encounters, clinical decision making, and referral of care (Carrillo et al., 2011; Nelson et al., 2002). In fact, in addition to social structures and access to care, health care providers’ attitudes as part of the social environment may act as social determinants of health for PWD as they influence equity in care receipt as well as health status (Kirschner & Curry, 2009; Koh, Piotrowski, Kumanyika, & Fielding, 2011).
Stereotypes, negative attitudes and prejudice, and biases develop over time and operate at different levels: consciously (explicit) and unconsciously (implicit; Amodio & Mendoza, 2011; Antonak & Livneh, 2000; Wilson, Lindsey, & Schooler, 2000). Explicit bias represents conscious attitudes that result in deliberate and calculating behaviors; explicit attitudes have traditionally been measured via self-report (e.g., questionnaires; Nosek et al., 2007; Phelan et al., 2015). Implicit bias represents unconscious attitudes that result in spontaneous and unplanned behaviors; one of the most common measures of implicit attitudes is the Implicit Association Test (IAT; Greenwald, McGhee, & Schwartz, 1998). It is important to examine both explicit and implicit attitudes, as these attitudes are expressed in different ways; people may feel social pressure to conceal their biases, or may not be aware they hold biases in the first place (Son Hing et al.’s, 2008).
Because explicit and implicit attitudes operate differently, people’s explicit and implicit attitudes do not always align. Combinations of explicit and implicit bias can be organized into four different categories: symbolic, aversive, principled conservative, and truly low prejudiced (Friedman, 2019; Son Hing et al., 2008). People with high explicit and high implicit prejudice toward PWD are symbolic ableists. Symbolic ableists recognize there is discrimination against PWD and have some empathy toward them, however, they score high in terms of philosophical individualism and are more likely to believe PWD produce excessive burdens on social systems and demand special treatment (Friedman, 2019; Friedman & Awsumb, 2019). People with low explicit prejudice and high implicit prejudice toward PWD are aversive ableists. Aversive ableists tend to be progressive and well-meaning, yet still participate in biased actions or thought, especially in situations where their prejudice is less overtly evident (Friedman, 2018, 2019). People with high explicit prejudice and low implicit prejudice toward PWD are principled conservatives. Principled conservatives truly value abstract conservative ideas; as a result, this causes them to dislike policies that stray from tradition (Son Hing et al., 2008). Since they favor traditional values, these individuals score high on explicit prejudice, however, they score low on implicit prejudice because they tend to discriminate against non-dominant groups equally (Friedman, 2019; Son Hing et al., 2008). People with low explicit and low implicit prejudice scores are considered truly low prejudiced toward PWD.
As implicit biases are more difficult to recognize and measure, the extent of their influence on behaviors, especially behaviors of health care providers, may be underestimated, particularly by those expressing these attitudes (Teal, Gill, Green, & Crandall, 2012). For example, while many providers believe they are not prejudiced against racial/ethnic minority groups, differences have been found in their clinical interactions among racial and ethnic minority groups (Dovidio & Gaertner, 2000). In fact, most systematic reviews exploring implicit and explicit racial/ethnic biases have found that the majority of providers are biased, to an extent similar to the general population (FitzGerald & Hurst, 2017; Hall et al., 2015; Maina, Belton, Ginzberg, Singh, & Johnson, 2018). Further, levels of bias are correlated with differences in provider-patient demographics (FitzGerald & Hurst, 2017). One consequence of providers’ bias is that they not only make inadequate or inappropriate clinical decisions, but may also fail to make appropriate recommendations for preventive care (McKinlay, Lin, Freund, & Moskowitz, 2002). In addition, providers’ bias impacts social minorities’ perceptions of their health care interactions and furthers the cycle of poorer mental and physical health (Borrell, Kiefe, Williams, Diez-Roux, & Gordon-Larsen, 2006; Dressler, Oths, & Gravlee, 2005; Harrell, Hall, & Taliaferro, 2003; Lewis, Cogburn, & Williams, 2015; Williams & Jackson, 2005).
Provider Attitudes Toward PWD
As disability bias is extremely prominent (Friedman, 2019), it is likely that providers not only have biased disability attitudes, but also demonstrate biased interactions with PWD that are impacted by these attitudes. For example, a study by Pruett and Chan (2006) found rehabilitation counseling students were implicitly prejudiced against PWD. Physician assistant students were also implicitly prejudiced against PWD (Archambault, Van Rhee, Marion, & Crandall, 2008). Similarly, research by Kelly and Barnes-Holmes (2013) found that applied behavior analysts held negative implicit attitudes toward children with autism. Research by VanPuymbrouck and Friedman (2019) found occupational therapy students had high levels of implicit bias toward PWD. In addition, Omori et al. (2012) found clinical medical residents in Japan implicitly associated people with schizophrenia with criminals, even after contact with people with schizophrenia. Research by Peris, Teachman, and Nosek (2008) found that mental health professionals who had implicit bias but no explicit bias were more likely to overdiagnose people with psychiatric disabilities.
In addition, research suggests that lack of provider knowledge in working with PWD contributes to inequities in health care access as well as preventable inequities in health outcomes (Krahn et al., 2015; Peacock, Iezzoni, & Harkin, 2015). In fact, Healthy People 2020 (United States Department of Health and Human Services, n.d.) reveals that common provider misperceptions about PWD contribute to under referral and disparities in methods to manage health (Reichard et al., 2011; United States Department of Health and Human Services, n.d.). Evidence also suggests providers make clinical decisions that work to avoid treating PWD (Akhavan & Tillgren, 2015) and that providers’ lack of knowledge about disability, as well as their medicalized attitudes of PWD, negatively impact access to care for PWD (McColl et al., 2008; Sanchez et al., 2000).
There is increasing demand for socially and culturally appropriate behavior by providers in clinical encounters, which includes reduction of both explicitly and implicitly biased care (Byron & Dieppe, 2000; Lie, Lee-Rey, Gomez, Bereknyei, & Braddock, 2011). Understanding both the impact and influence of explicit and implicit biases of providers toward PWD, particularly the interaction between their explicit and implicit attitudes, and if/how demographic factors correlate with their bias is one of the first steps in reducing disability discrimination within clinical encounters (VanPuymbrouck, 2018). Doing so is necessary in order to develop evidence-based interventions targeted at reducing providers’ negative attitudes. For these reasons, the aim of this study was to explore the disability attitudes of health care providers. This study had four research questions:
What are health care providers’ explicit attitudes toward disability?
What are health care providers’ implicit attitudes toward disability?
What is the relationship between health care providers’ explicit and implicit attitudes?
What demographic factors are associated with lower explicit and implicit disability attitudes of health care providers?
To explore these questions, we performed a secondary analysis on disability attitudes IAT (Disability Attitude Implicit Association Test [DA-IAT]) from 25,006 health care providers. In addition to analyzing people’s explicit and implicit attitudes, we used Son Hing et al.’s (2008) model of two-dimensional prejudice to compare combinations of provider’s explicit and implicit attitudes. Finally, we used linear regression models to examine correlates of providers’ explicit and implicit attitudes.
Method
Participants
Secondary data about disability attitudes were obtained from Project Implicit (Xu, Nosek, & Greenwald, 2014) a database where people can test their implicit prejudices, including those held about PWD. Between 2004 and 2017, 728,134 people participated in the DA-IAT. Of those people, 48.4% of the sample (n = 352,722) provided information about their occupation. The remaining participants (n = 375,412) were removed from the sample. Of those participants who identified their occupation, 25,006 were health care providers. As a result, the final sample size was 25,006 participants (Table 1).
Table 1.
Demographics of Sample
| Demographic variable | % | n |
|---|---|---|
| Healthcare occupation | ||
| Occupational and physical therapy assistants | 30.4 | 7,603 |
| Diagnosis and treating practitioners (MD, dentist, etc.) | 25.2 | 6,301 |
| Technologists and technicians | 10.3 | 2,581 |
| Nursing and home health assistants | 5.6 | 1,390 |
| Other healthcare support | 28.5 | 7,131 |
| Disability (n = 24,036) | ||
| Nondisabled | 90.7 | 21,789 |
| Person with a disability | 9.3 | 2,247 |
| Sex (n = 24,882) | ||
| Female | 80.6 | 20,043 |
| Male | 19.4 | 4,839 |
| Race (n = 938) | ||
| White | 74.9 | 18,595 |
| Multiracial | 9.3 | 2,302 |
| Black | 7.2 | 1,791 |
| East Asian | 2.9 | 724 |
| South Asian | 2.7 | 677 |
| Native Hawaiian or other Pacific Islander | 0.5 | 130 |
| Indigenous American | 0.5 | 121 |
| Latinx | 0.2 | 50 |
| Other | 1.8 | 449 |
| Family member have a disability? (n = 24,076) | ||
| No | 60.7 | 14,615 |
| Yes | 39.3 | 9,461 |
| Friend or acquaintance with disability? (n = 23,991) | ||
| No | 54.5 | 13,080 |
| Yes | 45.5 | 10,911 |
| Political orientation (n = 24,645) | ||
| Strongly conservative | 3.5 | 869 |
| Moderately conservative | 11.7 | 2,881 |
| Slightly conservative | 9.4 | 2,322 |
| Neutral | 35.1 | 8,649 |
| Slightly liberal | 11.2 | 2,758 |
| Moderately liberal | 20.4 | 5,033 |
| Strongly liberal | 8.7 | 2,133 |
Note. N = 25,006.
Participants represented the following health care professions: occupational and physical therapy assistants (30.4%), diagnosis and treating practitioners (e.g., MD, dentist, etc.; 25.2%); technologists and technicians (10.3%); nursing and home health assistants (5.6%); and other health care support (28.5%). The mean age of participants was 32.2 years old (SD = 11.7). Most participants were female (80.6%) and White (74.9%). Only a small proportion of participants (9.3%) identified as PWD. Slightly more than one third of participants (39.3%) had a family member with disabilities, and slightly less than half (45.5%) had a friend or acquaintance with disabilities. In terms of political orientation, most people identified as liberal (40.3%) with fewer identifying as “neutral” (35.1%) or conservative (24.6%).
Measure and Procedure
IATs, which are commonly utilized to measure implicit attitudes (Greenwald et al., 1998), measure reaction times (RTs) to examine associations between groups and traits. To do so, IATs present two target-concept discriminations (e.g., disabled persons and abled persons) and two attribute dimensions (e.g., good and bad) and ask them to categorize different stimuli into different categories, both congruent and incongruent with stereotypes. The quicker the RT, the more strongly a person associates the groups and traits together (Karpinski & Hilton, 2001). The disability attitudes version of the IAT was utilized in this study (DA-IAT).
Several studies have shown the DA-IAT’s construct validity (Aaberg, 2012; Pruett, 2004; Pruett & Chan, 2006), discriminant validity (White, Jackson, & Gordon, 2006), and reliability (Pruett, 2004; Pruett & Chan, 2006; Thomas, 2004). Moreover, research has shown that even when participants try to fake an IAT, faking is evident (Cvencek, Greenwald, Brown, Gray, & Snowden, 2010). The IAT has built-in safeguards against participants selecting at random or trying to fake. The updated scoring algorithm includes eliminating any trials with response latencies of greater than 10,000 ms (Greenwald, Nosek, & Banaji, 2003). Moreover, any participants who have 10% or more trials less than 300 ms will be removed (Greenwald et al., 2003). Participants were presented with the DA-IAT instructions, which instructed them to push the “E” key if presented stimuli belonged in categories on the left side of the computer screen and the “I” key for the right. They were told to categorize the stimuli as quickly as possible and with the fewest errors. They were also informed in advanced which stimuli fit into which category (e.g., wheelchair symbol with disabled persons). If participants sorted stimuli incorrectly, a red “X” appeared until they corrected their choice. After the instructions, participants completed seven rounds of categorization tasks, including a few practice sessions. Participants were asked to sort stimuli related to people without disabilities, disabled persons, good, and bad, in ways that were congruent with stereotypes (i.e., disabled persons matched with bad, and abled persons with good) and incongruent with stereotypes (i.e., disabled persons with good, and abled persons with bad). Finally, participants completed a number of demographic questions and an explicit measure of disability attitudes, which asked participants to rate their preferences for people with or without disabilities on a 7-point Likert scale from 1 (strongly prefer PWD) to 7 (strongly prefer nondisabled people).
Analysis
This study asked four research questions as outlined above. To examine our first research question, we used descriptive statistics of the explicit measure. We also utilized a one-way t test to examine the distribution and spread of explicit disability attitudes.
We explored our second research question using the DA-IAT. Implicit attitudes on the DA-IAT were calculated using Greenwald et al.’s (2003) updated IAT scoring protocol. Scores represent response latencies in stereotype-consistent and stereotype-inconsistent sessions of the DA-IAT. Scores, which range from −2.0 to 2.0, report the strength of preference for PWD or nondisabled people. Scores of −0.14 to 0.14 reveal no preference for PWD or nondisabled people, scores of 0.15 to 0.34 a slight preference for nondisabled people, 0.35 to 0.64 a moderate preference, and 0.65 or greater a strong preference (Greenwald et al., 2003). Negative values of the same ranges reveal preferences for PWD (Greenwald et al., 2003). We also utilized a one-way t test to examine the distribution and spread of the implicit disability attitudes of providers.
To understand the relationship between health care providers’ explicit and implicit attitudes, we used an adapted version of Son Hing et al.’s (2008) two-dimensional model of racial prejudice to determine combinations of explicit and implicit attitudes. In Son Hing et al.’s (2008) model, participants’ explicit and implicit scores are categorized as high and low and then grouped into four prejudice styles. People with high explicit and high implicit are symbolic ableists; high explicit and low implicit are principled conservatives; low explicit and high implicit are aversive ableists; and, low explicit and low implicit are truly low prejudiced. Once explicit and implicit scores were calculated we used this information to categorize people as low or high, subsequently grouping them into prejudice styles. Implicit scores were cut-off at the moderate prejudice level (0.35) according to IAT standards (e.g., Greenwald et al., 2003). The explicit score cut-off was the moderate preference for nondisabled people on the explicit scale.
Our final research question was exploratory; we were interested in examining what demographic factors, if any, were associated with lower explicit and implicit disability attitudes of health care providers. To do so, we ran linear regression models to examine the relationships between participants’ demographics (independent variables [IVs]) and their explicit and implicit attitudes (dependent variables [DVs] in separate models).
Results
Explicit Disability Attitudes
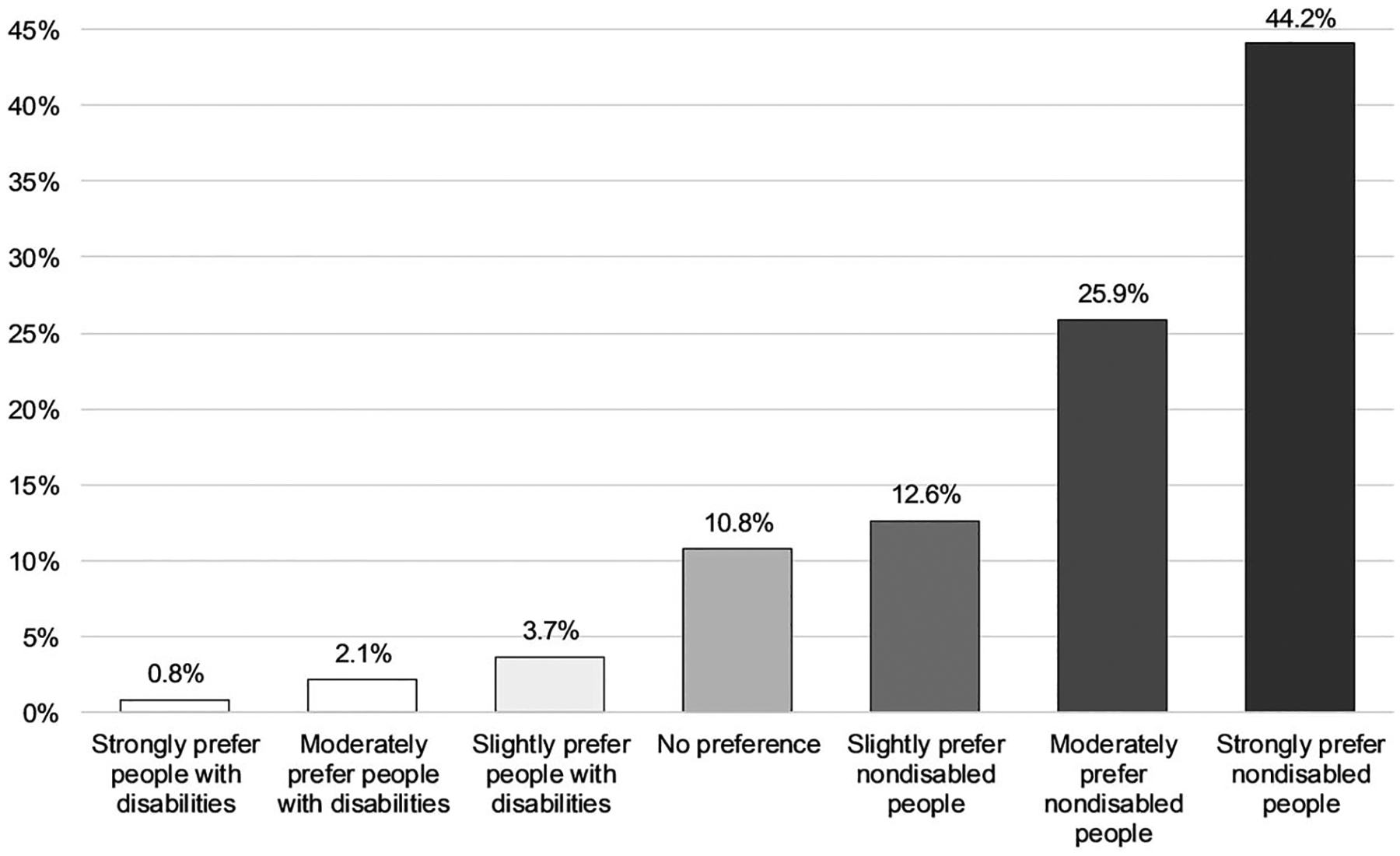
The explicit scores of providers ranged from 1 (strongly prefer PWD) to 7 (strongly prefer nondisabled people). Providers’ average explicit score was 4.41 (SD = 0.90), falling in the no preference for PWD or nondisabled people range. A one-way t test revealed this score was significantly different than a mean score of 4.00 (no preference), t(23,391) = 70.34, p < .001, Cohen’s d = 0.46 (representing a medium effect size). Findings revealed most providers (63.7%) reported having no explicit preference for PWD or nondisabled people, 32.1% reported preferring nondisabled people explicitly, and 4.3% reported preferring PWD explicitly (Figure 1).
Figure 1.

Explicit attitudes of health care providers. The figure shows that the majority of people (64%) have no explicit preferences for people with disabilities or nondisabled people, 32% of people explicitly preferred nondisabled people, and 4.2% of people explicitly preferred people with disabilities.
Implicit Disability Attitudes
The DA-IAT scores of providers ranged from −1.74 (strong preference for PWD) to 1.69 (strong preference for nondisabled people). Providers’ average score on the DA-IAT was 0.54 (SD = 0.43), which falls in the range of moderately preferring nondisabled people. A one-way t test revealed this score was significantly different from a mean score of 0, t(22,749) = 189.84, p < .001, Cohen’s d = 1.26 (large effect size), indicating an implicit bias for nondisabled people among providers. Findings revealed most providers (83.6%) preferred nondisabled people implicitly, 6.6% preferred PWD, and 10.8% had no preference (Figure 2).
Figure 2.
Implicit attitudes of health care providers. This figure shows the majority of people implicitly preferred nondisabled people (83%), whereas 6.6% of people implicitly preferred people with disabilities, and 11% had no preference.
Relationships Between Explicit and Implicit Attitudes
In order to determine types of prejudice present according to Son Hing et al.’s (2008) two-dimensional model of prejudice, providers’ explicit and implicit scores were categorized as high and low. Scores were then grouped into symbolic ableist (high explicit, high implicit), principled conservative (high explicit, low implicit), aversive ableist (low explicit, high implicit), and truly low prejudiced (low explicit, low implicit). Participants with any skipped items (n = 3,071) were excluded from this part of the analysis, thus yielding a lower number of resulting categorizations compared with our overall participant number. The majority of providers were aversive ableists (low explicit, high implicit; n = 12,939), with fewer providers scoring as symbolic ableists (high explicit, high implicit; n = 2,602), or principled conservatives (high explicit, low implicit; n = 504). Approximately one quarter of participants categorized were truly low prejudiced (low explicit, low implicit; n = 5,890; Figure 3).
Figure 3.
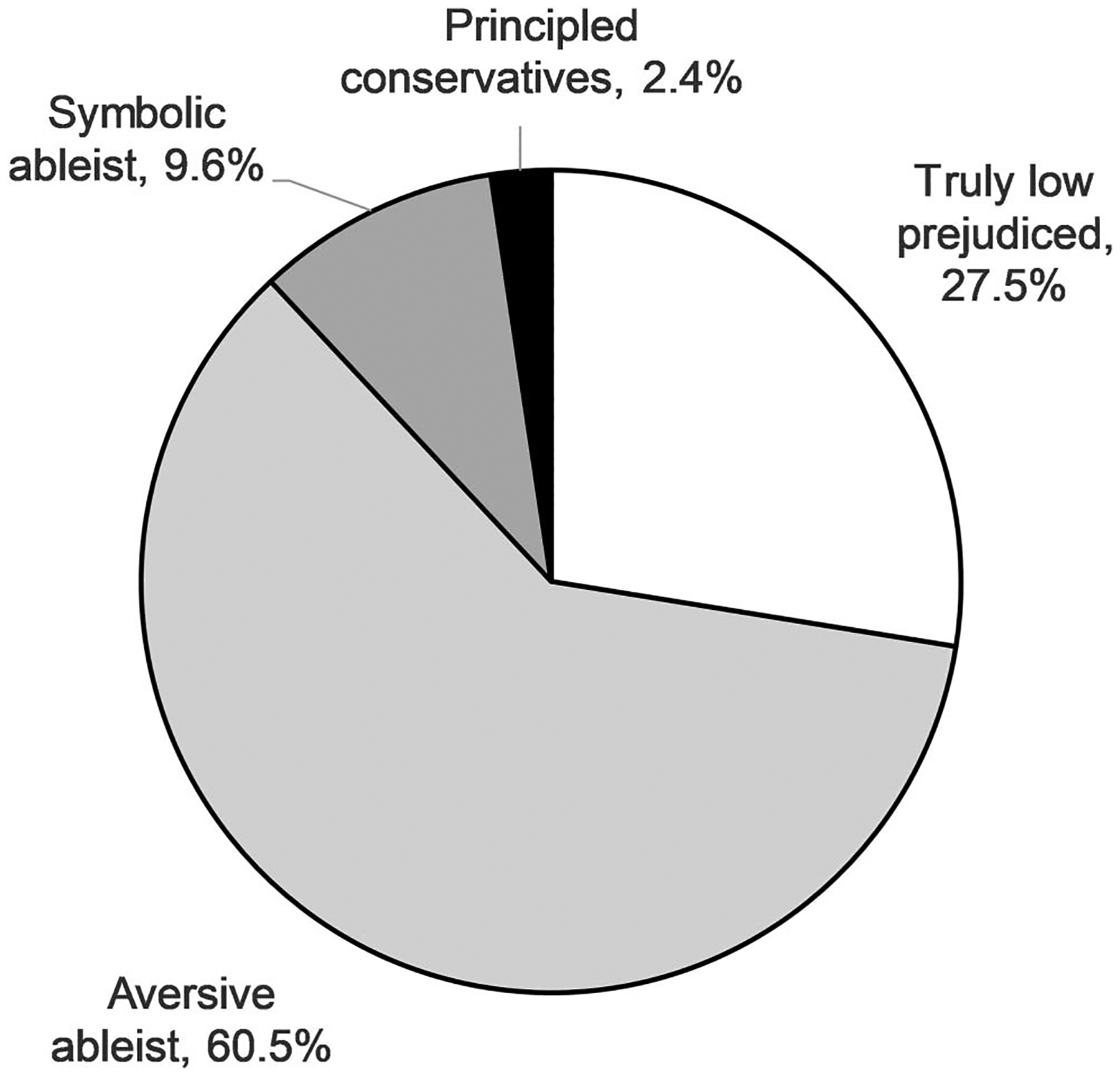
Prejudice styles of health care providers. This figure shows that 61% of people scored as aversive ableists, 10% as symbolic ableists, 2% as principled conservatives, and 28% as truly low prejudiced.
Correlates of Explicit and Implicit Attitudes
To explore correlates of disability attitudes, we ran a linear regression model to explore the relationship between providers’ demographic variables (IVs) and their explicit disability attitudes (DV). The model was significant, F(19, 22,555) = 54.66, p < .001, R2 = 0.044. The model demonstrated that age was correlated to explicit prejudice, with higher prejudice values occurring in older providers. For example, controlling for all other variables, a 25-year-old provider is expected to have an explicit score of 4.62 whereas a 45-year-old provider is expected to have an explicit score of 4.68. Providers with disabilities had lower explicit scores (4.55) than nondisabled providers (4.68). Female providers had lower explicit scores (4.39) than male providers (4.55). White providers had lower explicit scores (4.55) than Black providers (4.62), East Asian providers (4.85), South Asian providers (4.66), and Native Hawaiian or other Pacific Islander providers (4.91). However, White providers had higher explicit scores than Indigenous providers (4.30), and Latinx providers (4.17). Providers who had a family member with a disability had lower explicit scores (4.47) than those without family members with disabilities (4.55). Moreover, providers with friends or acquaintances with disabilities also had lower explicit scores (4.32) than those without friends or acquaintances with disabilities (4.55). Providers who were strongly conservative had higher explicit scores (4.55) than those who identified as neutral (4.38) or strongly liberal (4.43).
We also ran a linear regression model to explore the relationship between providers’ demographic variables (IVs) and their implicit disability attitudes. The model was significant, F(19, 21,799) = 52.08, p < .001, R2 = 0.043. Again, the model demonstrated correlation between age and implicit prejudice, with higher implicit scores occurring in older providers. For example, controlling for all other variables, a 25-year-old provider is expected to have a score of 0.58, whereas a 45-year-old provider is expected to have an implicit score of 0.68. Providers with disabilities are expected to have lower implicit scores (0.39) than nondisabled providers (0.45). Male providers are expected to have higher implicit scores (0.45) than female providers (0.35). Multiracial providers and people from the “other” race category are expected to have lower implicit scores (0.41 and 0.39, respectively) than White providers. East Asian providers are expected to have higher implicit scores (0.49) than White providers (0.45). Providers without a family member with disabilities are expected to have higher implicit scores (0.45) than those with family members with disabilities (0.43). Those providers with friends or acquaintances with disabilities are expected to have lower implicit scores (0.40) than those with no friends or acquaintances with disabilities (0.45). Those providers who identified as strongly conservative had higher implicit scores (0.45) than those who identified as slightly liberal (0.39), moderately liberal (0.39), or strongly liberal (0.33; Table 2).
Table 2.
Linear Regression Model Coefficients
| Model | ||||
|---|---|---|---|---|
| Explicit attitudes | Implicit attitudes | |||
| Variable | Coefficient | β | Coefficient | β |
| Constant | 4.55 | 0.45 | ||
| Age | 0.003*** | 0.03 | 0.005*** | 0.15 |
| Nondisabled (ref: person with disability) | 0.13*** | 0.04 | 0.06*** | 0.04 |
| Female (ref: Male) | −0.16*** | −0.07 | −0.10*** | −0.09 |
| Race (ref: White) | ||||
| Multiracial | 0.03 | 0.01 | −0.04*** | −0.02 |
| Black | 0.07** | 0.02 | 0.05 | 0.03 |
| East Asian | 0.30*** | 0.06 | 0.04* | 0.02 |
| South Asian | 0.11** | 0.02 | −0.03 | −0.01 |
| Native Hawaiian or other Pacific Islander | 0.36*** | 0.03 | 0.03 | 0.004 |
| Indigenous American | −0.25** | −0.02 | 0.006 | 0.0009 |
| Latinx | −0.38** | −0.02 | −0.13 | −0.01 |
| Other | −0.007 | −0.001 | −0.06** | −0.02 |
| Family member with a disability (ref: no family member) | −0.08*** | −0.04 | −0.02*** | −0.03 |
| Friend or acquaintance with disability (ref: no friend/acquaintance) | −0.23*** | −0.13 | −0.05*** | −0.06 |
| Political orientation (ref: strongly conservative) | ||||
| Moderately conservative | −0.009 | −0.003 | 0.001 | 0.001 |
| Slightly conservative | −0.04 | −0.01 | −0.02 | −0.01 |
| Neutral | −0.17*** | −0.09 | −0.02 | −0.02 |
| Slightly liberal | −0.03 | −0.01 | −0.06*** | −0.04 |
| Moderately liberal | −0.06 | −0.03 | −0.06*** | −0.06 |
| Strongly liberal | −0.12** | −0.04 | −0.12*** | −0.08 |
p < .05.
p < .01.
p < .001.
Discussion
As health care providers’ disability attitudes have the potential to not only impact the care PWD receive, but also their health outcomes, the aim of this study was to explore providers’ explicit and implicit attitudes. We were especially interested in exploring how providers’ implicit and explicit attitudes intertwined, as well as factors that impacted their disability attitudes. Our study of more than 25,000 providers revealed the majority of providers self-reported (consciously) not being biased against PWD. Yet, when disability attitudes were explored implicitly, the overwhelming majority of providers were biased against PWD and preferred nondisabled people.
The Relationship Between Health Care Professionals’ Explicit and Implicit Attitudes
Our findings revealed a significant mismatch between providers’ explicit and implicit disability attitudes. In fact, the majority of the providers in our study were aversive ableists, having low explicit prejudice and high implicit prejudice. While providers may believe they view PWD positively due to their low conscious prejudice, due to their implicit biases, they may in actuality see PWD as less capable of achieving. PWD and providers may also have different perceptions of the care providers provide due to aversive ableism. Examples of common microinequities—subtle and often unconscious forms of discrimination—include failure to accommodate a PWD within the health care setting while providing basic health care services. Moreover, another common form of discrimination PWD face in health care is a lack of accessible equipment, which providers frequently justify as being out of their control (Pharr, 2013). The lack of recognition of this discrimination, as well as the tendency of providers to excuse inequitable treatment, is a common reflection of implicit bias (Dovidio, Pagotto, & Hebl, 2011). In fact, when people are prejudiced in an aversive fashion, they also often rationalize their prejudice and justify it as not biased (Gaertner & Dovidio, 1986).
Meanwhile, approximately 10% of providers in our study were symbolic ableists, with high levels of explicit and implicit bias. One core component of explicit bias against PWD is philosophical individualism, which includes an emphasis on a Protestant work ethic, being directly responsible for one’s own outcomes, and belief in a just world, wherein people are rewarded for their actions (Friedman & Awsumb, 2019). When disability is considered in this context, there is an emphasis on framing disability as an individualized problem one “suffers” from, and a need to overcome bodily differences, thus, ignoring the environmental, social, and political barriers PWD face on a daily basis. Reflective of these associations, research suggests a link between individualization of disability and negative disability attitudes and stereotypes (Friedman & Owen, 2017; VanPuymbrouck & Friedman, 2019). Further, PWD have historically been equated with traits that have been viewed as undesirable, such as infirmity, disease, and ill health, with segregation and isolation from society as a result (Baynton, 2001). These deeply ingrained beliefs of providers that disability and health cannot coexist may explain clinical behaviors that systematically fail to provide equitable preventive care and referral to health and wellness programs. Among other marginalized populations, for example, there is evidence that minority clients’ mistrust of providers is based on perceptions of bias unrecognized by the providers, such as nonverbal body language (Penner et al., 2010). Additionally, clients’ experiences with discrimination have been linked to underutilization of necessary care (Burgess, Ding, Hargreaves, van Ryn, & Phelan, 2008; Dovidio et al., 2008).
A very low percentage of participants were categorized as principled conservatives, with high explicit bias, and low implicit bias. It is theorized that principled conservatives truly value abstract conservative ideas (Son Hing et al., 2008). However, principled conservativism is one of the less researched forms of prejudice and less is known about how it operates, especially related to disability. While theories suggest that principled conservativism may relate to fiscal/economic conservatism, work ethic, and individualism—all of which have implications for disability—Berdein (2007) also found inconsistencies across people, noting some conservatives apply and abandon their principles differently, especially when it applies to categories such as race. As such, more research is needed to explore not only principled conservatives’ attitudes toward disability, but also those of providers who may fall into this category.
Finally, approximately one-quarter of providers in our study (28%) were categorized as truly low prejudiced—scoring low in explicit and implicit bias. This percentage is similar, although slightly lower than Friedman’s (2019) study of prejudice styles from 350,000 people in the general population (29% truly low prejudice), suggesting providers have levels of bias similar to the general population. Moreover, we theorize truly low prejudiced providers likely share perspectives of disability that align with social or relational models of disability, which focus less on disability as an issue of the body, and recognize that social structures, such as inaccessible environments and discriminatory attitudes imposed upon people with impairments, are the root cause of disability in society (Campbell, 2014; Linton, 1998).
Factors Associated With Lower Explicit and Implicit Disability Attitudes
Factors that were associated with the lowest explicit and implicit biases among providers were being younger; female; strongly liberal; having friends, acquaintances, or family members with disabilities; or having a disability oneself. For example, female providers in this study had lower explicit and implicit disability prejudice than male providers. This finding is consistent with previous research suggesting women have more favorable views of PWD than men (Friedman & Awsumb, 2019; Hirschberger, Florian, & Mikulincer, 2005). Similarly, research also suggests women have lower explicit bias regarding race/ethnicity, gender, and body habitus (Haider et al., 2015; Sabin, Marini, & Nosek, 2012; Sabin, Nosek, Greenwald, & Rivara, 2009).
Our findings also revealed a number of differences in explicit and implicit attitudes of providers from different races. For example, East Asian providers had higher explicit and implicit attitudes than White providers. A social minority group relations theory that could account for this finding posits that minority groups “might adopt the dominant attitudes of majority groups, including stereotypes of and discrimination against other minorities” (Bratton & Haynie, 1999, p. 661). Although providers that were Black, Native Hawaiian or other Pacific Islander, and Indigenous American had higher explicit attitudes than White providers, they did not significantly differ from White providers when it came to implicit disability attitudes. Similarly, while Latinx providers had lower explicit attitudes than White providers, their implicit attitudes did not significantly differ than White providers. This mismatch in explicit and implicit attitudes of providers of different races may point to different cultural attitudes toward and/or relationships with disability. For example, some cultures have curated views of the importance of family and community, which includes care for those who are ill or have a disability, as well as historical health beliefs that situate disability within spiritual or folk contexts, as a punishment or condition meant to be cared for by families (mostly mothers) equipped to “manage” the disability (Zea, Quezada, & Belgrave, 1994; Braun, Kim, Ka’opua, Mokuau, & Browne, 2015; Salas-Provance, Erickson, & Reed, 2002). There may also be an interaction at play as racial minorities themselves continue to face significant health disparities and inequity of access to care, in part due to social determinants of health, such as socioeconomic status, education, and segregation, as well as a lack of culturally responsive approaches to health intervention (Chung-Do et al., 2016; Kaholokula, Ing, Look, Delafield, & Sinclair, 2018; Magaña, Parish, Morales, Li, & Fujiura, 2016; Zea et al., 1994). Moreover, people of color are also more likely to acquire disabilities themselves because of environmental conditions and social disparities (Mendes de Leon, Barnes, Bienias, Skarupski, & Evans, 2005; Thorpe et al., 2014).
Providers’ relationships to and with disability also impacted their explicit and implicit disability attitudes. Those providers who had disabilities themselves had less prejudicial explicit and implicit attitudes than providers without disabilities. Furthermore, people with friends, acquaintances, and family members with disabilities, also had lower explicit and implicit biases than providers without these relationships to PWD. These findings are consistent with an extensive body of social psychology literature that has found regular contact with groups perceived as having diverse characteristics is one of the most direct ways to combat bias or stereotyping behaviors (Burgess, Van Ryn, Dovidio, & Saha, 2007; Pettigrew & Tropp, 2006). However, it should be noted that research exploring the impact of brief exposure to positive disability exemplars found these as ineffective and, in fact, produced an increase in negative disability attitudes in some people (Kallman, 2017). However, in contrast, a study by Galli, Lenggenhager, Scivoletto, Molinari, and Pazzaglia (2015) found that short-term interactions while participating in the community with a person with disability had an effect on reducing biases of participants. While the long-term effects of the attitudes in the Galli et al. (2015) study were not explored, as a result of both our findings and the conflicting past research, contact related means of intervention is a recommended area of future study.
While much has been written about factors such as the influence of age on bias in general, little literature has specifically focused on how these factors interact with explicit and implicit bias toward PWD, particularly in the context of health care provision. It may be that the longer providers are situated in their respective health care fields, the more entrenched they become in individualized views of disability, which produce more bias. Younger providers are also likely one of the first generations to grow up with the Americans with Disabilities Act, which could have implications regarding how they have interacted with PWD through their development, such as in school and at work. Although more research is needed to explore why older providers may be more biased against PWD, it is important to note that older adults’ prejudice against disability works against their own self-interest since people are more likely to acquire disability as they age (Ory, Kinney Hoffman, Hawkins, Sanner, & Mockenhaupt, 2003; Smeeding, Butler, & Schaber, 1999). However, at the same time, ageism may lead to older adults wanting to disassociate their own experiences of aging from disability.
Finally, our findings revealed a number of differences in providers’ explicit and implicit attitudes based on their political orientation. For example, strongly liberal providers had lower explicit and implicit attitudes than providers that identified as strongly conservative. While previous literature here is sparse regarding the relationship between disability attitudes and political orientation, some researchers have noted that ideologies such as individualism, including an individual’s responsibility for contribution and productivity within capitalist economies, play a central role in politically conservative values, which has tended to devalue PWD as being “unfit” to work and thus less productive members of society and the workforce (Dodd, 2013; Feldman, Huddy, Wronski, & Lown, 2019).
Limitations
When interpreting the findings from this study, a number of limitations should be noted. First, this was not a representative sample—it was a convenience sample—and there is a chance of self-selection bias. As this was secondary data, we did not have the ability to ask additional questions, add additional variables, or clarify definitions (such as political orientation of ‘neutral’). For example, the explicit measure was limited to one item, which could have impacted social desirability, and we were not able to add additional metrics. In addition, our findings for the fourth research question represented low levels of variance; however, the aim of our fourth research question was not to build the strongest model but to explore correlates with disability attitudes. It is also important to recognize that critiques of IATs, including challenges to the proposed psychometric acceptability as well as claims about susceptibility to faking, are also reported in the literature, despite continued widespread use of IAT measures (Blanton et al., 2009; Steffens, 2004). Thus, it is important to interpret findings from the IAT with caution. Finally, it is important to note that correlation does not equal causation. We believe these limitations should also be considered as invitations for future study, perhaps examining how IAT scores correlate with observed provider interactions with PWD.
Implications
This study’s findings can be used to better understand how health care provider bias of PWD might contribute to inequitable health care access and health outcomes for PWD. A growing body of literature acknowledges providers’ implicit bias, attitudes, and beliefs contribute to unequal treatment and referral to services of patients from minority and ethnic groups (Dovidio & Fiske, 2012; Hall et al., 2015). PWD are a disparate health population often overlooked in these studies; however, the findings from our research indicate the majority of providers do hold implicit biases against PWD, and, in many cases, are not cognizant of their own biases. As such, we believe these findings indicate a need for increased study of this phenomenon and the mechanisms that influence it, as well as how providers’ attitudes continue to impact the health care experiences and health outcomes of PWD. Based on the results of our analysis as well as previous literature, it may be theorized that biases toward PWD contribute to unequal clinical treatment, similar to those inequities experienced by other social minority groups. More research is needed to fully understand the impact of bias on PWD in health care contexts, as well as to determine and implement effective means of reducing bias among providers. Specific interventions aimed at prejudice reduction among providers must be tailored not only to individual health care contexts but also to address the four distinct combinations of explicit and implicit bias to better address the mechanisms that can influence clinical decision making and negatively impact health care experiences and health outcomes of PWD.
Research has identified how racial stereotyping informs clinical decision-making of providers when well established standards of care are absent (Dovidio et al., 2008). Currently no standards of care exist for delivery of primary and preventive care for people across disability type. Arguably, tailoring treatment to the individual with disabilities requires extra time and knowledge of the provider to make clinical decisions of appropriate care delivery. However, research also finds increased demands on provider time and lack of provider knowledge of disability are the leading barriers to care for PWD (Kirschner & Curry, 2009; Morrison, George, & Mosqueda, 2008). Thus, the combination of these factors likely contributes to providers making clinical decisions in primary and preventive care based on established stereotypes of PWD (Ravesloot et al., 2007; Shakespeare & Kleine, 2013; Smeltzer, 2007).
Cultural competency training of providers working with ethnic and minority populations has been found to have a positive impact on provider behaviors during clinical encounters (Beach et al., 2005). Accordingly, engaging in culturally responsive care is increasingly recognized and taught as a part of provider educational standards (Butler et al., 2016); however, exploring PWD as a socially marginalized group is frequently not included within the umbrella of cultural competence. This oversight fails to address the many subtle experiences of discrimination and/or microinequities PWD experience as a result of their unique history and “place” within health care. Providers, as a group, are generally dedicated to achieving standards of normalcy to claim health and wellness of their clients. Exploring aversive ableism among providers might provide a foundation to circumvent traditional norms around concepts of health and wellness, and result in a shift in common provider practices which currently result in a failure to refer a PWD to health screenings, preventative interventions, and wellness programs (Nosek & Howland, 1997; Nosek & Simmons, 2007).
How disability is explained and explored within curricula might also examine how biases are reinforced or changed during provider education. For example, beginning in the early part of the 20th century the inclusion of standardized or simulated patients—actors playing the part of a PWD or a person with an illness—were introduced, and over the years increasingly embraced (Barrows, 1993). Yet, the literature critiques doing so as it is a form of relaying stereotypical disability experience, rather than offering the lived experience of PWD (VanPuymbrouck, Heffron, Sheth, & The, 2017). Curricula should closely explore if, and how, these forms of professional education act upon provider biases and prejudices. It should also be noted that the findings of this study provide support for increasing efforts to recruit and include PWD across medical and allied health professions.
Lastly, the disability community and members of some provider groups call for implementing standards of care for working with the disability community into professional competency standards (Alliance for Disability in Health Care Education, 2019; Minihan et al., 2001). Implementing these standards into education as well as practice could potentially remove the ambiguity within clinical contexts that often result in stereotypical assumptions and bias toward PWD by providers.
Conclusion
There is an extensive body of evidence that implicit bias exists and is associated with prejudicial attitudes and behaviors of providers, which negatively impact the health of ethnic and racial communities. This study provides evidence that the majority of providers are also implicitly biased against PWD, and opens dialogue onto how these attitudes may impact PWD’s health care encounters and clinical decision-making. The differences between the participants’ explicit and implicit attitudes also suggest more precarious ramifications might occur when socially unacceptable implicit attitudes are masked by superficial, explicit acceptance, especially by individuals in traditional positions of power who are entrusted with health-related clinical decisions for PWD. Thus, continuing to examine both explicit and implicit attitudes, as well as the relationship between them, is necessary in order to develop approaches for reducing prejudice against PWD within the context of health care. Future research should critically examine how providers’ disability bias informs their health care recommendations, referrals, and other care inequities known to contribute to disparities in health outcomes of PWD. Additionally, this study sought to understand the factors that influence explicit and implicit attitudes of health care providers, and if any are associated with lower biases. Our findings suggest factors do exist that might be harnessed to inform educational curricula and institutional policies to support a culture and context that nurtures attitudes and behaviors of low disability prejudice. Moreover, better understanding these factors and their influences could play a role in lessening the disparities in health care experienced by the disability community. Reducing ableism in broader society is the ultimate objective; within health care, achieving this is a proximate mandate and the only option for providers to attend to their ethical commitments of benevolence and nonmaleficence for all communities they serve.
Impact and Implications.
The findings of this study suggest that health care providers, in many cases, are not cognizant of their own biases related to disability. It is evident that more research is needed to fully understand the impact of bias on people with disabilities in health care contexts, as well as to determine and implement effective means of reducing bias among providers.
Contributor Information
Laura VanPuymbrouck, Rush University.
Carli Friedman, The Council on Quality and Leadership, Towson, Maryland.
Heather Feldner, University of Washington.
References
- Aaberg VA (2012). A path to greater inclusivity through understanding implicit attitudes toward disability. The Journal of Nursing Education, 51, 505–510. 10.3928/01484834-20120706-02 [DOI] [PubMed] [Google Scholar]
- Akhavan S, & Tillgren P (2015). Client/patient perceptions of achieving equity in primary health care: A mixed methods study. International Journal for Equity in Health, 14, 65–77. 10.1186/s12939-015-0196-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alliance for Disability in Health Care Education. (2019). Core competencies on disability for health care education. Peapack, NJ: Alliance for Disability in Health Care Education. Retrieved from http://www.adhce.org/ [Google Scholar]
- Altman B, & Bernstein A (2008). Disability and health in the United States, 2001–2005. Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Amodio DM, & Mendoza SA (2011). Implicit intergroup bias: Cognitive, affective, and motivational underpinnings. In Gawronski B & Payne BK (Eds.), Handbook of implicit social cognition: Measurement, theory, and applications (pp. 353–374). New York, NY: Guilford Press. [Google Scholar]
- Antonak RF, & Livneh H (2000). Measurement of attitudes towards persons with disabilities. Disability and Rehabilitation: An International, Multidisciplinary Journal, 22, 211–224. 10.1080/096382800296782 [DOI] [PubMed] [Google Scholar]
- Archambault M, Van Rhee J, Marion G, & Crandall S (2008). Utilizing implicit association testing to promote awareness of biases regarding age and disability. The Journal of Physician Assistant Education: the Official Journal of the Physician Assistant Education Association, 19, 20–26. 10.1097/01367895-200819040-00003 [DOI] [Google Scholar]
- Barrows HS (1993). An overview of the uses of standardized patients for teaching and evaluating clinical skills. Academic Medicine: Journal of the Association of American Medical Colleges, 68, 443–451. 10.1097/00001888-199306000-00002 [DOI] [PubMed] [Google Scholar]
- Baynton DC (2001). Disability and the justification of inequality in American history. In Longmore P & Umansky L (Eds.), The new disability history: American perspectives (pp. 33–57). New York, NY: University Press. [Google Scholar]
- Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, Palacio A, … Cooper LA (2005). Cultural competence. Medical Care, 43, 356–373. 10.1097/01.mlr.0000156861.58905.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berdein I (2007). Principled conservatives or covert racists: Disentangling racism and ideology through implicit measures (Doctoral dissertation). Stony Brook University, Stony Brook, NY. [Google Scholar]
- Blanton H, Jaccard J, Klick J, Mellers B, Mitchell G, & Tetlock PE (2009). Strong claims and weak evidence: Reassessing the predictive validity of the IAT. Journal of Applied Psychology, 94, 567–582. 10.1037/a0014665 [DOI] [PubMed] [Google Scholar]
- Borrell LN, Kiefe CI, Williams DR, Diez-Roux AV, & Gordon-Larsen P (2006). Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Social Science & Medicine, 63, 1415–1427. 10.1016/j.socscimed.2006.04.008 [DOI] [PubMed] [Google Scholar]
- Bratton K, & Haynie K (1999). Agenda setting and legislative success in state legislatures: The effects of gender and race. The Journal of Politics, 61, 658–679. 10.2307/2647822 [DOI] [Google Scholar]
- Braun KL, Kim BJ, Ka’opua LS, Mokuau N, & Browne CV (2015). Native Hawaiian and Pacific Islander elders: What gerontologists should know. The Gerontologist, 55, 912–919. 10.1093/geront/gnu072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Ding Y, Hargreaves M, van Ryn M, & Phelan S (2008). The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. Journal of Health Care for the Poor and Underserved, 19, 894–911. 10.1353/hpu.0.0063 [DOI] [PubMed] [Google Scholar]
- Burgess D, van Ryn M, Dovidio J, & Saha S (2007). Reducing racial bias among health care providers: Lessons from social-cognitive psychology. Journal of General Internal Medicine, 22, 882–887. 10.1007/s11606-007-0160-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler M, McCreedy E, Schwer N, Burgess D, Call K, Przedworski J, … Kane R (2016). Improving cultural competence to reduce health disparities. comparative effectiveness (AHRQ Publication No. 16- EHC006-EF). Rockville, MD: Agency for Healthcare Research and Quality. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK361126/?report=reader [PubMed] [Google Scholar]
- Byron M, & Dieppe P (2000). Educating health professionals about disability: ‘attitudes, attitudes, attitudes’. Journal of the Royal Society of Medicine, 93, 397–398. 10.1177/014107680009300801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell F (2014). Ableism: A theory of everything? Paper presented at the Ableism, Racism and Conflicts of Participation and Inclusion in Society and the Labour Market, Hamburg, Germany. [Google Scholar]
- Carrillo JE, Carrillo VA, Perez HR, Salas-Lopez D, Natale-Pereira A, & Byron AT (2011). Defining and targeting health care access barriers. Journal of Health Care for the Poor and Underserved, 22, 562–575. 10.1353/hpu.2011.0037 [DOI] [PubMed] [Google Scholar]
- Chung-Do JJ, Look MA, Mabellos T, Trask-Batti M, Burke K, & Mau MK (2016). Engaging Pacific Islanders in research: Community recommendations. Progress in Community Health Partnerships, 10, 63–71. 10.1353/cpr.2016.0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cvencek D, Greenwald AG, Brown AS, Gray NS, & Snowden RJ (2010). Faking of the implicit association test is statistically detectable and partly correctable. Basic and Applied Social Psychology, 32, 302–314. 10.1080/01973533.2010.519236 [DOI] [Google Scholar]
- Dodd S (2013). Personalization, individualism and the politics of disablement. Disability & Society, 28, 260–273. 10.1080/09687599.2012.699283 [DOI] [Google Scholar]
- Dovidio JF, & Fiske ST (2012). Under the radar: How unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. American Journal of Public Health, 102, 945–952. 10.2105/AJPH.2011.300601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio JF, & Gaertner SL (2000). Aversive racism and selection decisions: 1989 and 1999. Psychological Science, 11, 315–319. 10.1111/1467-9280.00262 [DOI] [PubMed] [Google Scholar]
- Dovidio J, Pagotto L, & Hebl M (2011). Implicit attitudes and discrimination against people with physical disabilities. In Wierner R & Willborn S (Eds.), Disability and aging discrimination (pp. 157–183). New York, NY: Springer. 10.1007/978-1-4419-6293-5_9 [DOI] [Google Scholar]
- Dovidio J, Penner LA, Albrecht T, Norton W, Gaertner S, & Shelton J (2008). Disparities and distrust: The implications of psychological processes for understanding racial disparities in health and health care. Social Science & Medicine, 67, 478–486. 10.1016/j.socscimed.2008.03.019 [DOI] [PubMed] [Google Scholar]
- Dressler W, Oths K, & Gravlee C (2005). Race and ethnicity in public health research: Models to explain health disparities. Annual Review of Anthropology, 34, 231–252. 10.1146/annurev.anthro.34.081804.120505 [DOI] [Google Scholar]
- Feldman S, Huddy L, Wronski J, & Lown P (2019). The interplay of empathy and individualism in support for social welfare policies. Political Psychology. Advance online publication. 10.1111/pops.12620 [DOI] [Google Scholar]
- FitzGerald C, & Hurst S (2017). Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics, 18, 19. 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman C (2018). Aversive ableism: Modern prejudice towards disabled people. Review of Disability Studies: An International Journal, 14, 1–21. [Google Scholar]
- Friedman C (2019). Mapping ableism: A two-dimensional model of explicit and implicit disability attitudes. Canadian Journal of Disability Studies, 8, 95–120. [Google Scholar]
- Friedman C, & Awsumb J (2019). Research article: The Symbolic Ableism Scale. Review of Disability Studies: An International Journal, 15, 1–20. [Google Scholar]
- Friedman C, & Owen A (2017). Defining disability: Understandings of and attitudes towards ableism and disability. Disability Studies Quarterly. Advance online publication. 10.18061/dsq.v37i1.5061 [DOI] [Google Scholar]
- Gaertner S, & Dovidio J (1986). The aversive form of racism. In Gaertner S & Dovidio J (Eds.), Prejudice, discrimination, and racism: Theory and research (pp. 61–89). Orlando, FL: Academic Press. [Google Scholar]
- Galli G, Lenggenhager B, Scivoletto G, Molinari M, & Pazzaglia M (2015). Don’t look at my wheelchair! The plasticity of longlasting prejudice. Medical Education, 49, 1239–1247. 10.1111/medu.12834 [DOI] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, & Schwartz JL (1998). Measuring individual differences in implicit cognition: The implicit association test. Journal of Personality and Social Psychology, 74, 1464–1480. 10.1037/0022-3514.74.6.1464 [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, & Banaji MR (2003). Understanding and using the implicit association test: I. An improved scoring algorithm. Journal of Personality and Social Psychology, 85, 197–216. 10.1037/0022-3514.85.2.197 [DOI] [PubMed] [Google Scholar]
- Haider AH, Schneider EB, Sriram N, Dossick DS, Scott VK, Swoboda SM, … Freischlag JA (2015). Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decisions. Journal of the American Medical Association Surgery, 150, 457–464. 10.1001/jamasurg.2014.4038 [DOI] [PubMed] [Google Scholar]
- Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, … Coyne-Beasley T (2015). Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. American Journal of Public Health, 105, e60–e76. 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell JP, Hall S, & Taliaferro J (2003). Physiological responses to racism and discrimination: An assessment of the evidence. American Journal of Public Health, 93, 243–248. 10.2105/AJPH.93.2.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschberger G, Florian V, & Mikulincer M (2005). Fear and compassion: A terror management analysis of emotional reactions to physical disability. Rehabilitation Psychology, 50, 246–257. 10.1037/0090-5550.50.3.246 [DOI] [Google Scholar]
- Iezzoni L (2011). Eliminating health and health care disparities among the growing population of people with disabilities. Health Affairs, 30, 1947–1954. 10.1377/hlthaff.2011.0613 [DOI] [PubMed] [Google Scholar]
- Kaholokula JK, Ing CT, Look MA, Delafield R, & Sinclair K (2018). Culturally responsive approaches to health promotion for Native Hawaiians and Pacific Islanders. Annals of Human Biology, 45, 249–263. 10.1080/03014460.2018.1465593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kallman D (2017). Integrating disability: Boomerang effects when using positive media exemplars to reduce disability prejudice. International Journal of Disability Development and Education, 64, 644–662. 10.1080/1034912X.2017.1316012 [DOI] [Google Scholar]
- Karpinski A, & Hilton JL (2001). Attitudes and the implicit association test. Journal of Personality and Social Psychology, 81, 774–788. 10.1037/0022-3514.81.5.774 [DOI] [PubMed] [Google Scholar]
- Kelly A, & Barnes-Holmes D (2013). Implicit attitudes towards children with autism versus normally developing children as predictors of professional burnout and psychopathology. Research in Developmental Disabilities, 34, 17–28. 10.1016/j.ridd.2012.07.018 [DOI] [PubMed] [Google Scholar]
- Kirschner KL, & Curry RH (2009). Educating health care professionals to care for patients with disabilities. Journal of the American Medical Association, 302, 1334–1335. 10.1001/jama.2009.1398 [DOI] [PubMed] [Google Scholar]
- Koh HK, Piotrowski JJ, Kumanyika S, & Fielding JE (2011). Healthy people: A 2020 vision for the social determinants approach. Health Education & Behavior, 38, 551–557. 10.1177/1090198111428646 [DOI] [PubMed] [Google Scholar]
- Krahn GL, Walker DK, & Correa-De-Araujo R (2015). Persons with disabilities as an unrecognized health disparity population. American Journal of Public Health, 105, S198–S206. 10.2105/AJPH.2014.302182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, & Williams DR (2015). Self-reported experiences of discrimination and health: Scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology, 11, 407–440. 10.1146/annurev-clinpsy-032814-112728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lie DA, Lee-Rey E, Gomez A, Bereknyei S, & Braddock CH III. (2011). Does cultural competency training of health professionals improve patient outcomes? A systematic review and proposed algorithm for future research. Journal of General Internal Medicine, 26, 317–325. 10.1007/s11606-010-1529-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linton S (1998). Reassigning meaning. In Linton S (Ed.), Claiming disability, knowledge and identity (pp. 8–33). New York, NY: New York University Press. [Google Scholar]
- Magaña S, Parish S, Morales MA, Li H, & Fujiura G (2016). Racial and ethnic health disparities among people with intellectual and developmental disabilities. Intellectual and Developmental Disabilities, 54, 161–172. 10.1352/1934-9556-54.3.161 [DOI] [PubMed] [Google Scholar]
- Maina IW, Belton TD, Ginzberg S, Singh A, & Johnson TJ (2018). A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Social Science & Medicine, 199, 219–229. 10.1016/j.socscimed.2017.05.009 [DOI] [PubMed] [Google Scholar]
- McColl MA, Forster D, Shortt SE, Hunter D, Dorland J, Godwin M, & Rosser W (2008). Physician experiences providing primary care to people with disabilities. Healthcare Policy, 4, e129–e147. 10.12927/hcpol.2008.19989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinlay JB, Lin T, Freund K, & Moskowitz M (2002). The unexpected influence of physician attributes on clinical decisions: Results of an experiment. Journal of Health and Social Behavior, 43, 92–106. 10.2307/3090247 [DOI] [PubMed] [Google Scholar]
- Mendes de Leon CF, Barnes LL, Bienias JL, Skarupski KA, & Evans DA (2005). Racial disparities in disability: Recent evidence from self-reported and performance-based disability measures in a population-based study of older adults. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences, 60, S263–S271. 10.1093/geronb/60.5.S263 [DOI] [PubMed] [Google Scholar]
- Minihan P, Robey K, Long-Bellil L, Graham C, Hahn J, Woodard L, & Eddey G (2001). Outcomes of disability-related training for the generalist physician: An exploration of the contributions of knowledge, attitudes and skills. Academic Medicine, 86, 1163–1170. [DOI] [PubMed] [Google Scholar]
- Morrison EH, George V, & Mosqueda L (2008). Primary care for adults with physical disabilities: Perceptions from consumer and provider focus groups. Family Medicine, 40, 645–651. [PubMed] [Google Scholar]
- Nelson A, Stith A, & Smedley B (2002). Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Nosek B, Smyth F, Hansen J, Devos T, Lindner N, Ranganath K, … Banaji M (2007). Pervasiveness and correlates of implicit attitudes and stereotypes. European Review of Social Psychology, 18, 36–88. 10.1080/10463280701489053 [DOI] [Google Scholar]
- Nosek MA, & Howland CA (1997). Breast and cervical cancer screening among women with physical disabilities. Archives of Physical Medicine and Rehabilitation, 78, S39–S44. 10.1016/S0003-9993(97)90220-3 [DOI] [PubMed] [Google Scholar]
- Nosek MA, & Simmons DK (2007). Sexual and reproductive health disparities experienced by people with disabilities. Californian Journal of Health Promotion, 5(special issue), 68–81. 10.32398/cjhp.v5iSI.1201 [DOI] [Google Scholar]
- Omori A, Tateno A, Ideno T, Takahashi H, Kawashima Y, Takemura K, & Okubo Y (2012). Influence of contact with schizophrenia on implicit attitudes towards schizophrenia patients held by clinical residents. BMC Psychiatry, 12, 205. 10.1186/1471-244X-12-205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgera K, & Artiga S (2018). Disparities in health and healthcare: Five key questions and answers. Retrieved from http://files.kff.org/attachment/Issue-Brief-Disparities-in-Health-and-Health-Care-Five-Key-Questions-and-Answers
- Ory M, Kinney Hoffman M, Hawkins M, Sanner B, & Mockenhaupt R (2003). Challenging aging stereotypes: Strategies for creating a more active society. American Journal of Preventive Medicine, 25, 164–171. 10.1016/S0749-3797(03)00181-8 [DOI] [PubMed] [Google Scholar]
- Peacock G, Iezzoni LI, & Harkin TR (2015). Health care for Americans with disabilities—25 years after the ADA. The New England Journal of Medicine, 373, 892–893. 10.1056/NEJMp1508854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, West TV, Gaertner SL, Albrecht TL, Dailey RK, & Markova T (2010). Aversive racism and medical interactions with black patients: A field study. Journal of Experimental Social Psychology, 46, 436–440. 10.1016/j.jesp.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Teachman BA, & Nosek BA (2008). Implicit and explicit stigma of mental illness: Links to clinical care. Journal of Nervous and Mental Disease, 196, 752–760. 10.1097/NMD.0b013e3181879dfd [DOI] [PubMed] [Google Scholar]
- Pettigrew TF, & Tropp LR (2006). A meta-analytic test of intergroup contact theory. Journal of Personality and Social Psychology, 90, 751–783. 10.1037/0022-3514.90.5.751 [DOI] [PubMed] [Google Scholar]
- Pharr J (2013). Accessible medical equipment for patients with disabilities in primary care clinics: Why is it lacking? Disability and Health Journal, 6, 124–132. 10.1016/j.dhjo.2012.11.002 [DOI] [PubMed] [Google Scholar]
- Phelan SM, Puhl RM, Burke SE, Hardeman R, Dovidio JF, Nelson DB, … van Ryn M (2015). The mixed impact of medical school on medical students’ implicit and explicit weight bias. Medical Education, 49, 983–992. 10.1111/medu.12770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruett SR (2004). A psychometric validation of a disability attitude implicit association test (Doctoral dissertation). University of Wisconsin–Madison, Madison, WI. [Google Scholar]
- Pruett SR, & Chan F (2006). The development and psychometric validation of the Disability Attitude Implicit Association Test. Rehabilitation Psychology, 51, 202–213. 10.1037/0090-5550.51.3.202 [DOI] [Google Scholar]
- Ravesloot CH, Seekins T, Cahill T, Lindgren S, Nary DE, & White G (2007). Health promotion for people with disabilities: Development and evaluation of the Living Well with a Disability program. Health Education Research, 22, 522–531. 10.1093/her/cyl114 [DOI] [PubMed] [Google Scholar]
- Reichard A, Stolzle H, & Fox MH (2011). Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disability and Health Journal, 4, 59–67. 10.1016/j.dhjo.2010.05.003 [DOI] [PubMed] [Google Scholar]
- Sabin JA, Marini M, & Nosek BA (2012). Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS ONE, 7, e48448. 10.1371/journal.pone.0048448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin J, Nosek BA, Greenwald A, & Rivara FP (2009). Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. Journal of Health Care for the Poor and Underserved, 20, 896–913. 10.1353/hpu.0.0185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Provance M, Erickson G, & Reed J (2002). Disabilities as viewed by four generations of one Hispanic family. American Journal of Speech-Language Pathology, 11, 151–162. 10.1044/1058-0360(2002/015) [DOI] [Google Scholar]
- Sanchez J, Byfield G, Brown TT, LaFavor K, Murphy D, & Laud P (2000). Perceived accessibility versus actual physical accessibility of healthcare facilities. Rehabilitation Nursing, 25, 6–9. 10.1002/j.2048-7940.2000.tb01849.x [DOI] [PubMed] [Google Scholar]
- Shakespeare T, & Kleine I (2013). Educating health professionals about disability: A review of interventions. Health and Social Care Education, 2, 20–37. 10.11120/hsce.2013.00026 [DOI] [Google Scholar]
- Smeeding T, Butler R, & Schaber G (1999, July). The consequences of population aging for society. Workshop Report. New York, NY: International Longevity Center, LTD. [Google Scholar]
- Smeltzer SC (2007). Improving the health and wellness of persons with disabilities: A call to action too important for nursing to ignore. Nursing Outlook, 55, 189–195. e2. 10.1016/j.outlook.2007.04.001 [DOI] [PubMed] [Google Scholar]
- Son Hing LS, Chung-Yan GA, Hamilton LK, & Zanna MP (2008). A two-dimensional model that employs explicit and implicit attitudes to characterize prejudice. Journal of Personality and Social Psychology, 94, 971–987. 10.1037/0022-3514.94.6.971 [DOI] [PubMed] [Google Scholar]
- Steffens MC (2004). Is the implicit association test immune to faking? Experimental Psychology, 51, 165–179. 10.1027/1618-3169.51.3.165 [DOI] [PubMed] [Google Scholar]
- Teal CR, Gill AC, Green AR, & Crandall S (2012). Helping medical learners recognise and manage unconscious bias toward certain patient groups. Medical Education, 46, 80–88. 10.1111/j.1365-2923.2011.04101.x [DOI] [PubMed] [Google Scholar]
- Thomas C (2004). Rescuing a social relational understanding of disability. Scandinavian Journal of Disability Research, 6, 22–36. 10.1080/15017410409512637 [DOI] [Google Scholar]
- Thorpe RJ Jr., McCleary R, Smolen JR, Whitfield KE, Simonsick EM, & LaVeist T (2014). Racial disparities in disability among older adults: Finding from the exploring health disparities in integrated communities study. Journal of Aging and Health, 26, 1261–1279. 10.1177/0898264314534892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. (n.d.). Healthy People 2020. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/disability-and-health
- VanPuymbrouck L (2018). Rights to accommodation in healthcare: Self-advocacy experiences of people with disabilities (Doctoral dissertation). Rush University, Chicago, IL. [Google Scholar]
- VanPuymbrouck L, & Friedman C (2019). Exploring the understanding of entry-level graduate OT students’ perceptions of disability. Scandinavian Journal of Occupational Therapy. Advance online publication. 10.1080/11038128.2019.1596310 [DOI] [Google Scholar]
- VanPuymbrouck L, Heffron J, Sheth A, & The K (2017). Experiential learning: Critical analysis of standardized patient and disability simulations. Journal of Occupational Therapy Education. Advance online publication. 10.26681/jote.2017.010305 [DOI] [Google Scholar]
- White MJ, Jackson V, & Gordon P (2006). Implicit and explicit attitudes toward athletes with disabilities. Journal of Rehabilitation, 72, 33–40. [Google Scholar]
- Williams DR, & Jackson PB (2005). Social sources of racial disparities in health. Health Affairs, 24, 325–334. 10.1377/hlthaff.24.2.325 [DOI] [PubMed] [Google Scholar]
- Wilson TD, Lindsey S, & Schooler TY (2000). A model of dual attitudes. Psychological Review, 107, 101–126. 10.1037/0033-295X.107.1.101 [DOI] [PubMed] [Google Scholar]
- Xu K, Nosek B, & Greenwald A (2014). Psychology data from the race implicit association test on the project implicit demo website. Journal of Open Psychology Data, 2, e3. 10.5334/jopd.ac [DOI] [Google Scholar]
- Zea MC, Quezada T, & Belgrave FZ (1994). Latino cultural values: Their role in adjustment to disability. Journal of Social Behavior & Personality, 9, 185–200. [Google Scholar]


