Abstract
To review complications including mortality after transoral robotic surgery (TORS) for both benign and malignant pathologies. This is a prospective observational study. Postoperative haemorrhage (8.7%) was the most common complication and 2 (1.7%) mortality were seen in this study. Airway complications and tracheostomy (1.7%), aspiration pneumonia (1.7%), swallowing problems and nasogastric feeding (7%), intra-operative pharyngocutaneous fistula (0.9%) and transient nasal regurgitation (3.5%) were also seen. The more tissue is removed the more is the risk of complication. Complications were mainly seen in the first year of starting the service of TORS and it is a reflection of the learning curve. However, secondary haemorrhage did not follow any pattern in our series. The postoperative haemorrhage was more common in patients with T2 oropharyngeal carcinoma. The mortality was seen in 2 patients (1.7%) with T2 oropharyngeal carcinoma due to postoperative haemorrhage. Higher T stage of oropharyngeal squamous cell carcinoma (OPSCC) needs bigger resection with resultant increase in morbidity.
Keywords: TORS, Oropharyngeal carcinoma, TORS complication
Introduction
Transoral robotic surgery (TORS) has been used for both benign and malignant conditions in the U.K and the rest of the world. It has been commonly reported from South East Asia, North America and Australia [1–3]. As a technique, it is relatively new in the U.K and the Freeman hospital at Newcastle-upon-Tyne was the first to introduce this service in the U.K IN 2013 [4].
This service started at the Royal Derby hospital in 2015. We are using Da Vinci X robot, manufactured by Intuitive (Intuitive Surgical Inc, Sunnyvale, CA, USA). Melder [5] first used Trans oral robot surgery in 2005 for a vallecular cyst. Weinstein and O’Malley [1] first reported the use of Da Vinci Robot for tongue base neoplasm in 2006. The US Food and drug administration (FDA) approved it in 2009 [6].
The robotic surgery offers advantages over conventional open approach surgery and avoids external scar and preserves oral and oropharyngeal functions like swallow. It also has advantages over trans oral laser surgery because of improved visualisation, instruments that do not require working in straight line of vision and reduced operative time. If available, it is now considered as treatment of choice at least for early (T1&T2) oropharyngeal squamous cell carcinoma (OPSCC) and patients can potentially avoid radiotherapy and chemotherapy and its associated long-term complications.
There are only a few studies that have reported detailed complications following TORS.
Material and Methods
This is a prospective observational study and the data collection started in 2015 since the service began.
The inclusion criteria for this study are.
TORS procedure performed for both benign and malignant pathologies (T1-T3). Only 1 patient had T3 oropharyngeal carcinoma.
Only complications that could directly be attributed to TORS
Any patient who had complication or mortality within 30 days was included in this study.
Two-surgeon team who had received adequate training performed these surgeries.
Results
We carried out 114 procedures between February 2015 and September 2021. The average age of patients in this cohort was 58 years and the majority were males (78), more than twice the number of females (36).
Ninety-two procedures were done for malignancies including revision procedures.
Amongst the malignancies, the most common sites are shown below in Fig. 1
Fig. 1.
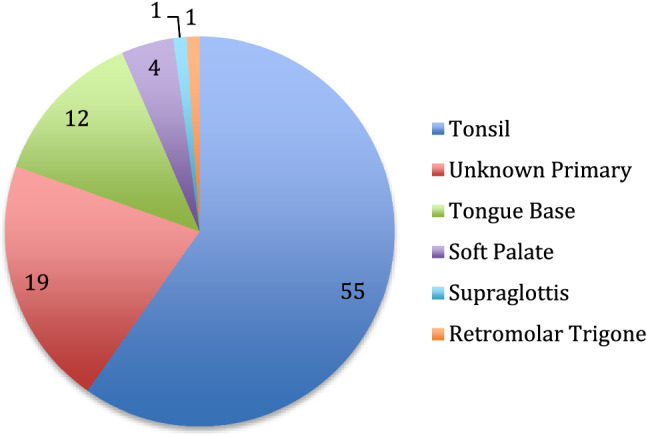
Malignant pathology distribution
The OPSCC accounted for over 57% of the total number of TORS procedures performed in this study. Tonsil cancer was the most common pathology, more than 4 times as common as tongue base cancer. One patient with tonsil cancer had salvage surgery and free flap repair following post chemo-radiotherapy residual disease while all other patients were treated with surgery as primary modality of treatment.
Twenty-two patients had non- malignant lesions as shown below in the Fig. 2. The postoperative histology identified 18 benign pathologies and 4 pre-malignant lesions.
Fig. 2.
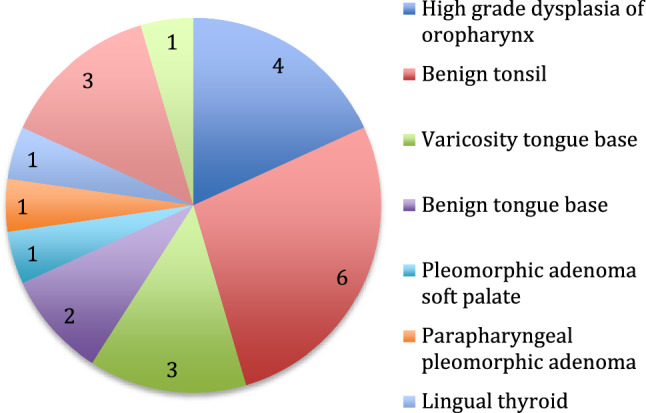
Non- malignant pathology distribution
We will focus on morbidity and mortality directly attributed to TORS. We have divided these into following:
Airway Complications
Two patients (1.7%) needed postoperative tracheostomy. These patients developed either floor of mouth oedema or laryngeal oedema postoperatively.
Bleeding
There were 10 episodes of postoperative bleeding in 10 patients (8.7%). Out of these, 1(0.8%) had primary haemorrhage. There were 9 episodes (7.9%) of secondary haemorrhage in total. Out of these, 6 patients with minor secondary haemorrhages were managed conservatively, 1 patient returned to theatre for arrest of haemorrhage and 2 patients died during resuscitation.
Aspiration Pneumonia
Aspiration pneumonia was treated in 2 patients (1.7%) and both patients required nasogastric tube for feeding and treated with antibiotic. One of these patient had partial oropharyngectomy and the other had supraglottic laryngectomy.
Swallowing Problem and Nasogastric Feeding
A total of 8 patients (7%) had swallowing problem and/or aspiration that required nasogastric tube insertion for feeding.
Nasal Regurgitation
Four patients (3.5%) reported minor transient nasal regurgitation.
Pharyngocutaneous Fistula
One patient (0.9%) had intraoperative fistula that was closed with local flap and it did not manifest post-operatively.
The trend in significant complications like postoperative haemorrhage, airway problems and fistula has been shown below in Fig 3.
Fig. 3.
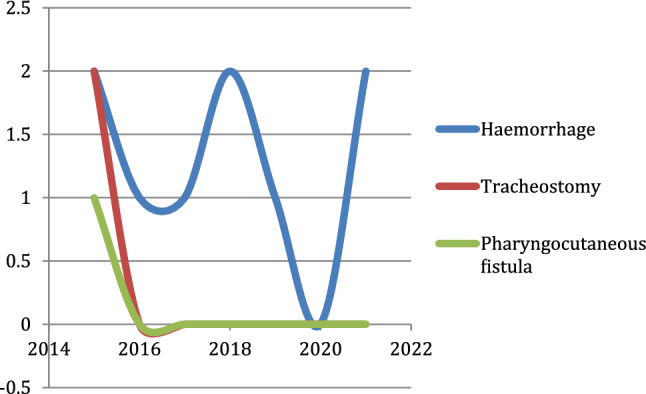
Trend in complications
The X-axis represents the year of complication and Y-axis represents the number of episodes of complications. It clearly shows that airway complications, fistula did not occur after the first year of starting the robotic surgery. The postoperative secondary haemorrhage does not follow any pattern and minor episodes happened intermittently despite increase in the experience of surgeon.
Prolonged Hospital Stay due to Pain and Re-admission due to Pain
Three patients (2.6%) needed longer in-patient hospital stay between 9 and 14 days for pain management. Two patients (1.7%) were readmitted for pain management. Five patients (4.3%) developed first bite syndrome as a medium to long-term complication.
Mortality
Two patients (1.7%) died in this series due to secondary haemorrhage.
Discussion
Trans oral robotic surgery is a relatively new technique particularly in the U.K and is gradually being introduced across various NHS trusts and hospitals. It has shown positive impact particularly on management of oropharyngeal cancers. In centres where facility for robotic surgery is available, it has become an alternative treatment for the early T stage OPSCC. Weinstein et al. [7] have also reported its role in advanced OPSCC. With improvement in the understanding of the causation and prognosis of Human papilloma virus induced oropharyngeal carcinoma, the role of robotic surgery has become more relevant.
The post TORS complication has been reported by various centres particularly in North America and some centres in Europe.
Hay et al. [8] reported 102 complications in 122 TORS procedures. They also reported reducing trend in the complications with increased exposure. In a retrospective survey conducted by Chia et al. [9] there was a significant decrease in complication rate in surgeons with experience of more than 50 TORS procedure.
The most commonly reported complication in post TORS patient is haemorrhage. In our series the overall haemorrhage rate was 8.7% and the majority presented with minor secondary haemorrhage that did not need resuscitation. One of these patients had benign pathology (squamous papilloma) while 6 patients had T2 and 3 patients had T1 OPSCC. Only one patient had primary haemorrhage (within 24 h) that needed return to theatre for arrest of haemorrhage. The secondary haemorrhages happened between day 3-day 8 after surgery. A recent meta-analysis by Stokes et al. [10] reported a post TORS incidence of 5.74% and they equated it to haemorrhage rate following adult tonsillectomy. Chia et al. [9] reported that surgeons with experience of more than 50 cases had haemorrhage rate of 2.8% and those with less than 25 had 4.5% post operative bleeding rate. Their study was a survey of 45 surgeons and included 2015 collective TORS procedures reported overall haemorrhage rate of 3.1% but we feel that their result was skewed because more than half of the procedures were performed by 2 surgeon with less complication rate. Kim et al. [11] did a detailed retrospective review of 222 patients from a single centre and reported a haemorrhage rate of 9.8%. They also studied the effect of selective ligation of arteries in the neck and reported that it did not reduce the rate of bleeding but probably reduced the severity of bleeding. Kubik [12] & Pollei [13] also drew the same conclusion. It is our standard practice to do selective arterial ligation during neck dissection for patients undergoing TORS. Kim [11] et al. also concluded that there was no significant decrease in the haemorrhage rate despite increase in the experience of the surgeon.
The study by Chia [9] also reported 0.3% mortality rate and all the patients died due to postoperative haemorrhage. A multi-institutional study from France [14] reported a mortality rate of 2.3%, two patients died due to massive postoperative haemorrhage and third died due to pulmonary embolism. There are two mortalities in our series (1.7%) and both of them due to catastrophic postoperative secondary haemorrhage. First patient died on postoperative day 8. The post mortem study revealed that he had developed collateral retrograde circulation to the branches of tonsillar arteries via the internal carotid artery. The second patient died on day 3 after surgery due to secondary haemorrhage and aspiration. The post mortem study did not reveal any arterial vessel disruption to explain the haemorrhage but definite surgical site bleed, therefore likely from muscle/wound bed itself. Both patients were staged as p16 positive T2 squamous cell carcinoma of tonsil and none of these were on anticoagulant preoperatively. The mean age of these patients was 61 years and both were male.
Only 2 patients (1.7%) needed tracheostomy following the surgery. Both patients were decannulated in 2 weeks following tracheostomy. One of them had parapharyngeal pleomorphic adenoma that developed acute airway obstruction in the immediate postoperative period while the other had T2 oropharyngeal squamous cell carcinoma and needed tracheostomy to wean off the ventilator in intensive care after 4 days. Van Abel et al. [15] reported 11% tracheostomy is their retrospective series. This study also reported that patients with higher T stage, base of tongue tumour and those undergoing bilateral neck dissection were more likely to need tracheostomy. Hay et al. [8] reported 1 tracheostomy in their series of 122 patients. Williams et al. [16] reported almost 100% tracheostomy in resection via open approach lip split mandibulotomy. Tracheostomy was done in 50% of their patients treated with transoral laser surgery in a case match study. In our series, tracheostomy was only performed in the first year of the start of the service. This indicates that it depends on the extent and duration of surgery. As our experience grew, it would take less time to perform a procedure resulting in lesser postoperative floor of mouth or laryngeal oedema.
None of our patients had long term swallowing problem and needed a gastrostomy tube for feeding. Nasogastric tube was inserted in 8 (7%) patients. These patients remained in the hospital for a maximum of 14 days and were able to be discharged home on oral diet. One of these patients had surgery for parapharyngeal pleomorphic adenoma while others had surgery for malignancies (5 T2, 1 T1 Oropharynx and 1 T1 Supraglottis). Hay [8] reported that 11 patients (9%) needed gastrostomy tube in their series of 122 patients. The swallow problem can be attributed to bigger resection resulting in more tissue loss, pain and impaired swallow.
Two patients had aspiration pneumonia treated with antibiotic. One of them was T2 tonsillar carcinoma, had aspiration following primary haemorrhage. The other patient had T1 supraglottic carcinoma and had aspiration pneumonia after 48 h and needed nasogastric tube for 7 weeks before it could be removed.
Pain management is an important patient concern postoperatively and one of the reasons for delay in discharge to home. Most of our patients were discharged in 72–96 h following surgery. However, 3 patients (2.6%) stayed for between 9 and 14 days for pain control. Ganti et al. [17] have shown that TORS patients on enhanced recovery after surgery (ERAS) protocol needed lesser postoperative morphine equivalent as an inpatient as well as on discharge. 2 patients (1.7%) were re-admitted for pain control. 5 patients (4.3%) developed complication of first bite syndrome. In 4 patients it self resolved in 3 months but in 1 patient it remained a persistent problem after 12 months of follow up. This patient was treated with anticonvulsant like Gabapentin and subsequently referred for Botox injection to parotid gland/pterygoid muscle. Topf et al. [18] reported 7% incidence in their series of 84 patients who had ligation of multiple branches of external carotid artery particularly the lingual artery during neck dissection. This has been attributed to disruption of sympathetic fibres on the carotid artery resulting in unopposed parasympathetic innervation of parotid gland.
Transient nasal regurgitation was seen in 4 (3.5%) patients. Two patients had regurgitation after primary surgery for T1 SCC soft palate and T2 SCC tonsil. The other two were patients (T2) who had revision TORS for tonsillar carcinoma to remove an involved margin. The symptoms resolved in all the patients after 3 months with completion of healing process and also with input from speech and language therapist. Again this can be attributed to bigger the resection, the more tissue loss resulting in temporary velopharyngeal insufficiency.
Conclusion
Our experience reveals that airway complications, primary haemorrhage, feeding problems with nasogastric tube insertion, pharyngocutaneous fistula took place within first year of starting the service of transoral robotic surgery. This suggests that there is a learning curve for any new surgical technique and complications are more likely to happen in the beginning. In our series, morbidity was more common in patients with T2 cancers. This means bigger resection increases the risk of complication. Death following TORS is uncommon but other centre has reported similar result to our study. TORS is a very useful tool and spares the morbidity associated with open approach procedures for oropharyngeal cancers and helps to avoid long term side effects of radiotherapy in carefully selected cohort of early oropharyngeal cancers.
Data Availability
Data collection and analysis were done in accordance with information governance practice of University hospitals of Derby and Burton NHS trust.
Declarations
Conflict of interest
There is no conflict of interest and external funding was not needed to support this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.O'Malley BW, Jr, Weinstein GS. Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope. 2006;116(8):1465–1472. doi: 10.1097/01.mlg.0000227184.90514.1a. [DOI] [PubMed] [Google Scholar]
- 2.Krishnan G, Mintz J, Foreman A, Hodge JC, Krishnan S. The acceptance and adoption of transoral robotic surgery in Australia and New Zealand. J Robot Surg. 2019;13(2):301–307. doi: 10.1007/s11701-018-0856-8. [DOI] [PubMed] [Google Scholar]
- 3.Park YM, Kim WS, De Virgilio A, Lee SY, Seol JH, Kim SH. Transoral robotic surgery for hypopharyngeal squamous cell carcinoma: 3-year oncologic and functional analysis. Oral Oncol. 2012;48(6):560–566. doi: 10.1016/j.oraloncology.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 4.O’Hara J, Warner L, Fox H, Hamilton D, Meikle D, Counter P, Robson A, Goranova R, Shahid I, Kelly C, Robinson M, Paleri V. Primary transoral robotic surgery +/- adjuvant therapy for oropharyngeal squamous cell carcinoma—a large observational single-centre series from the United Kingdom. Clin Otolaryngol. 2021;46(5):1005–1012. doi: 10.1111/coa.13769. [DOI] [PubMed] [Google Scholar]
- 5.McLeod IK, Melder PC. Da Vinci robot assisted excision of vallecular cyst: a case report. Ear Nose Throat J. 2005;84(3):170–172. doi: 10.1177/014556130508400315. [DOI] [PubMed] [Google Scholar]
- 6.US Food and Drug Administration (2009) 501(k) Summary: indications for use for intuitive surgical endoscopic instrument control system for transoral otolaryngology procedures. US Food and Drug Administration, Silver Spring, MD
- 7.Weinstein GS, O’Malley B, Jr, Cohen MA, Quon H. Transoral robotic surgery for advanced oropharyngeal carcinoma. Arch Otolaryngol Head Neck Surg. 2010;136(11):1079–1085. doi: 10.1001/archoto.2010.191. [DOI] [PubMed] [Google Scholar]
- 8.Hay A, Migliacci J, KarassawaZanoni D, Boyle JO, Singh B, Wong RJ, Patel SG, Ganly I. Complications following transoral robotic surgery (TORS): a detailed institutional review of complications. Oral Oncol. 2017;67:160–166. doi: 10.1016/j.oraloncology.2017.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chia SH, Gross ND, Richmon JD. Surgeon experience and complications with transoral robotic surgery (TORS) Otolaryngol Head Neck Surg. 2013;149(6):885–892. doi: 10.1177/0194599813503446. [DOI] [PubMed] [Google Scholar]
- 10.Stokes W, Ramadan J, Lawson G, Ferris FRL, Holsinger FC, Turner MT. Bleeding complications after transoral robotic surgery: a meta-analysis and systematic review. Laryngoscope. 2021;131(1):95–105. doi: 10.1002/lary.28580. [DOI] [PubMed] [Google Scholar]
- 11.Mandal R, Duvvuri U, Ferris RL, Kaffenberger TM, Choby GW. Kim S Analysis of post-transoral robotic-assisted surgery hemorrhage: frequency, outcomes, and prevention. Head Neck. 2016;38(Suppl 1):E776–E782. doi: 10.1002/hed.24101. [DOI] [PubMed] [Google Scholar]
- 12.Kubik M, Mandal R, Albergotti W, Duvvuri U, Ferris RL, Kim S. Effect of transcervical arterial ligation on the severity of postoperative hemorrhage after transoral robotic surgery. Head Neck. 2017;39(8):1510–1515. doi: 10.1002/hed.24677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pollei TR, Hinni ML, Moore EJ, Hayden RE, Olsen KD. Analysis of postoperative bleeding and risk factors in transoral surgery of the oropharynx. JAMA Otolaryngol Head Neck Surg. 2013;139(11):1212–1218. doi: 10.1001/jamaoto.2013.5097. [DOI] [PubMed] [Google Scholar]
- 14.Vergez S, Lallemant B, Ceruse P, Moriniere S, Aubry K, De Mones E, Benlyazid A, Mallet Y. Initial multiinstitutional experience with transoral robotic surgery. Otolaryngol Head Neck Surg. 2012;147(3):475–481. doi: 10.1177/0194599812443221. [DOI] [PubMed] [Google Scholar]
- 15.Van Abel KM, Quick MH, Graner DE, Lohse CM, Price DL, Price KAR, Ma DJ, Moore EJ. Outcomes following TORS for HPV-positive oropharyngeal carcinoma: PEGs, tracheostomies and beyond. Am J Otolaryngol. 2019;40(5):729–734. doi: 10.1016/j.amjoto.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 16.Williams CE, Kinshuck AJ, Derbyshire SG, Upile N, Tandon S, Roland NJ, Jackson SR, Rodrigues J, Husband DJ, Lancaster J, Jones TM. Transoral laser resection versus lip split mandibulotomy in the management of oropharyngeal squamous cell carcinoma (OPSCC]: a case match study. Eur Arch Otorhinolaryngol. 2014;271(2):367–372. doi: 10.1007/s00405-013-2501-5. [DOI] [PubMed] [Google Scholar]
- 17.Ganti A, Eggerstedt M, Grudzinski K, Ramirez EA, Vaughan D, Revenaugh PC, Stenson K, Al-Khudari S. Enhanced recovery protocol for transoral robotic surgery demonstrates improved analgesia and narcotic use reduction. Am J Otolaryngol. 2020;41(6):102649. doi: 10.1016/j.amjoto.2020.102649. [DOI] [PubMed] [Google Scholar]
- 18.Topf MC, Moritz E, Gleysteen J, Curry JM, Cognetti DM, Luginbuhl AJ. First bite syndrome following transcervival arterial ligation after transoral robotic surgery. Laryngoscope. 2018;128(7):1589–1593. doi: 10.1002/lary.27005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data collection and analysis were done in accordance with information governance practice of University hospitals of Derby and Burton NHS trust.


