Abstract
Closed rhinoplasty is currently losing favour as a method of rhinoplasty reshaping procedure. Open rhinoplasties are usually performed by surgeons because of the greater degree of visualisation of the cartilages and bones within the nose that need to be reshaped. Because of the criticisms of closed rhinoplasty the senior author performed an audit of his outcomes to determine whether closed rhinoplasty still has a role to play in the armamentarium of the plastic surgeon. We conducted this study as a retrospective review of all closed rhinoplasty operations performed by a single surgeon over a two-year period (from 1st January 2016 to 31st December 2017). The operative technique is provided. An independent panel of 3 assessors (2 board certified consultant plastic surgeons and one lay member of the public) rated outcomes of the closed technique based on photographic series. Statistical analysis was performed using Cohen’s Kappa and Friedman test. Additionally, the length of follow up period, revision rates, and post-operative complications (general and aesthetic) were examined. A total of 242 cases of rhinoplasty were performed (8 open and 234 closed rhinoplasty; 225 primary and 17 revision operations). The first consultant surgeon gave a score in a range from 4.2/5 to 4.9/5 with a mode of 4.8 and a mean score of 4.7/5. The second consultant surgeon gave a range of 4.1/5 to 4.9/5 with a mode of 4.4 and mean score of 4.3/5. The lay panel member scored the cases in a range from 4.4/5 to 5/5 with a mode of 4.8 and a mean score of 4.9/5. Cohen’s coefficient was 0.72 showing substantial agreement across the panel. The complication rate for the recorded data was 0.8% with two cases of soft tissue infection treated with oral antibiotics. The results of this paper advocates the benefits of the closed approach in aesthetic rhinoplasty. Surgeons should appreciate that both open and closed approaches are complimentary. The favouring of a single approach is indicated in the scenarios discussed. The remaining cases seem to produce equivocal results and the choice of procedure should be based on patient anatomy, outcome aims, and the ability of a surgeon to perform their preferred technique.
Keywords: Rhinoplasty, Aesthetic, Transcartilaginous, Transcolumellar, Closed approach, External approach
Introduction
Closed rhinoplasty is currently losing favour as a method of rhinoplasty reshaping procedure. Open rhinoplasties are usually performed by surgeons because of the greater degree of visualisation of the cartilages and bones within the nose that need to be reshaped. In addition, adding grafts to the nose is thought to be easier when using an open rhinoplasty approach. The senior author (TS) was initially trained in closed rhinoplasty, and subsequently started performing open rhinoplasty before reverting back to closed rhinoplasty for the majority of his patients. Using the closed rhinoplasty approach, the senior author performs reduction rhinoplasty, augmentation rhinoplasty, rhinoplasty to straighten the nose, and rhinoplasty for breathing difficulties. Because of the criticisms of closed rhinoplasty, and because of the large numbers of cases performed in his practice, the senior author performed an audit of his outcomes to determine whether closed rhinoplasty still has a role to play in the armamentarium of the plastic surgeon.
Methods
We conducted this study as a retrospective review of all closed rhinoplasty operations performed by a single surgeon over a two-year period (from 1st January 2016 to 31st December 2017). We identified the closed rhinoplasty cases from the senior author’s logbook. We then cross-referenced these with the hospital data and patient records for the same period. We used Microsoft Excel to both collect and store the data, and to review the case notes of this consecutive series of patients.
The data collected included the standard patients’ demographics, and their past medical and surgical history. From these medical records we accessed the standardized pre and postoperative rhinoplasty photograph series. We also identified the operative technique and steps in the procedure; complications during follow up period; the length of the follow up period; and revision rates. Post-operative complications were categorized as general and aesthetic complications.
We selected an independent panel of 3 assessors to rate the outcomes of the closed technique rhinoplasty based on the photographic series. The panel included two board certified consultant plastic surgeons and one lay member. The senior author’s identity remained anonymous to the panel. Likewise, the senior author was not involved in the panel’s selection and was unaware of their identities. The panel was asked to review the final post-operative photos by providing an independent star rating score for each case. We selected the Likert scale for scoring, using a five point visual analogue scale.
We performed the statistical analysis using Cohen’s Kappa in order to measure the level of agreement, as we found the data could be grouped into separate categories. We also selected Friedman test, as this study compared matched groups on a score from a non-Gaussian population. Statistical significance was taken at the level of p < 0.05.
Surgical Procedure
The surgical procedure of the rhinoplasty proceeded in the following order. The procedure was modified to include or exclude some or all of these steps, depending on what was required during the rhinoplasty. The magnitude of change was modified for each patient individually depending on what was required in the rhinoplasty.
Patients were placed in a head up position, with the neck slightly extended, under general anaesthesia. Patients were given 1 g IV of tranexamic acid, topical Xylometazoline Hydrochloride 0.1%, and 15.4 ml of 2% lidocaine with 1:80,000 adrenaline (seven syringes of dental local anaesthetic). The local anaesthetic was placed in the following areas: alar (hydrodissection), nasal spine, columella, tip, supra tip, dorsum, sidewall, cartilaginous septum, bony septum, facial artery, infraorbital nerve, and around the inferior turbinates.
The surgical steps performed included:
An intracartilaginous incision through the nasal lining, cutting the alar cartilage but leaving at least 4 mm of alar cartilage caudally
A cephalic trim of the alar cartilage, followed by a wide soft tissue sub-SMAS elevation of the soft tissues of the nose
A complete transfixion incision in the membranous septum that joined both sides, allowing for a delivery approach
A double ended hook was placed in the columella allowing visualisation of the doral skeletal structures of the nose
Caudal septal reduction
Maxillary spine reduction
The upper lateral cartilage was separated from anterior septum
Anterior septal reduction
Dorsal rasping with progressively finer rasps of the bony dorsum
External stab incision to allow entry of an ostetome
In fraar groove
Closure was performed with 4.0 vicryl rapide to the lining, 5.0 prolene to the stab incisions at the sidewall of the nose, and the nose was packed with a trouser leg jelonet d cture of the maxilla at the nasal region, out fractures of the inferior turbinates, fracture of the vomer to straighten the bony septum if required
Tip sutures 3.0 vicryl, through the lining, to pinch tip
Supratip sutures from dermis to dermis at the tip/supratip junction to better define the al ressing
A Denver splint was applied.
Patients discharged when fit to leave, which was either within a few hours of surgery or the following day. The jelonet pack was removed shortly prior to discharge. Patients were reviewed for suture removal and splint removal 1 week post operatively and attended for follow up 1–3 months later and 6–12 months later.
Results
During a 2 year period between 1st of January 2016 and 31st of December 2017 a total of 242 cases of rhinoplasty were performed. 173 were females and 69 were males (F:M ratio 2.5:1). The average age was 30 years old. The age range was 17–62 years old. 8 cases (3.3%) were done via the open approach and 234 (96.6%) were done by a closed rhinoplasty approach (Fig. 1).
Fig. 1.
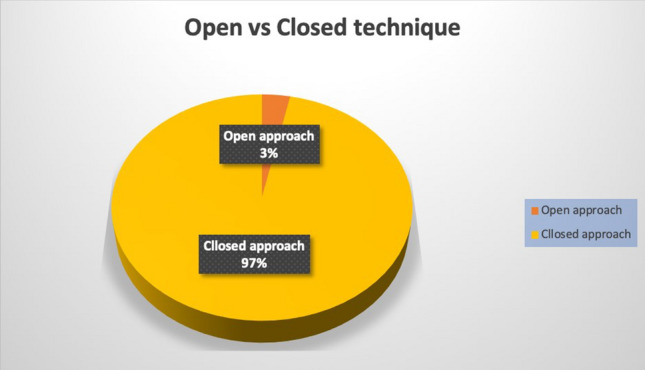
Open vs close technique numbers
Of all cases, 225 were primary operations and there were 17 revision operations, all revisions were carried out using the closed approach (Fig. 2).
Fig. 2.
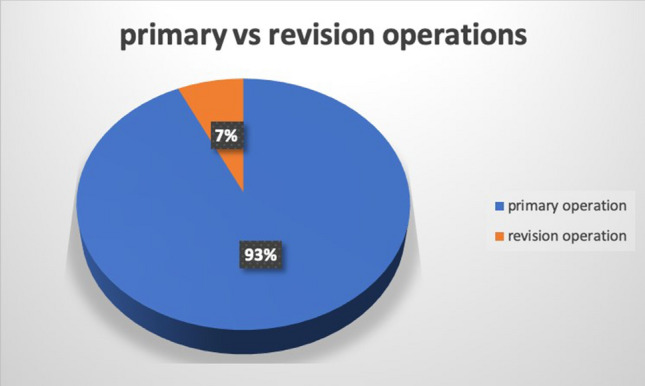
Primary vs revision operation numbers
Panel Scores
Results were assessed by the panel by utilising the visual analogue scale. The first consultant surgeon gave a score in a range from 4.2/5 to 4.9/5 with a mode of 4.8 and a mean score of 4.7/5. The second consultant surgeon gave a range of 4.1/5 to 4.9/5 with a mode of 4.4 and mean score of 4.3/5. The lay panel member scored the cases in a range from 4.4/5 to 5/5 with a mode of 4.8 and a mean score of 4.9/5. Overall the average score for all panel members was 4.6/5 (Fig. 3).
Fig. 3.
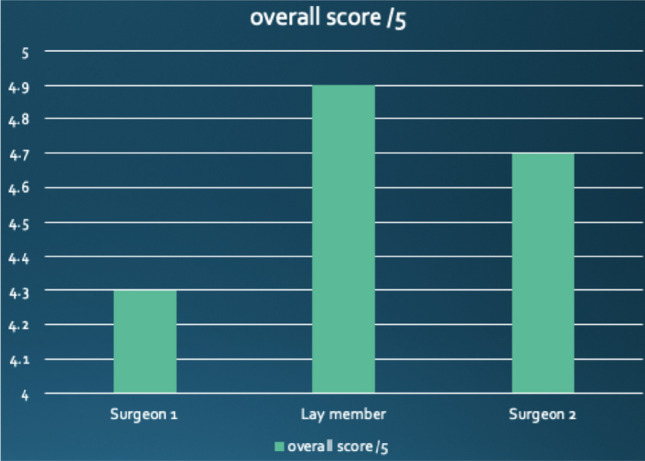
Average score of panel members
Measurement of Agreement
We used Cohen’s Kappa test to measure the agreement between the average scores given by the consultant surgeons and the lay panel member for each individual patient. As this test only compares two sets of categorical data we have taken the average score for the two surgeons and tested it against the lay member’s score. Cohen’s coefficient was 0.72 suggesting a substantial agreement.
| Kappa agreement values—range | |
|---|---|
| Kappa < 0 | Poor |
| Kappa 0–0.20 | Slight |
| Kappa 0.21–0.40 | Fair |
| Kappa 0.41–0.60 | Moderate |
| Kappa 0.61–0.80 | Substantial |
| Kappa > 0.80 | Almost perfect |
Complication Rates
The complication rate for the recorded data was 0.8%, there were two cases of soft tissue infection treated with oral antibiotics.
Discussion
Rhinoplasty is one of the most common procedures performed by a cosmetic surgeon. It is also considered a highly challenging procedure, largely due to its dual role and central importance for both facial aesthetics and bodily function. Modern rhinoplasty can be approached by two distinct techniques: open or closed (endonasal) [1–3]. The preferred method has been subject to controversial and often contentious debate. Emerging evidence suggests a trend towards the open technique. The following discussion aims to address the benefits and drawbacks of each approach, highlight current recommendations, and, importantly, advocate the role of the endonasal approach in modern day rhinoplasty.
Firstly, it is important to address the results of this study. The majority of patients received a primary rhinoplasty via the closed approach (97% closed and 93% primary). All operations were performed by an experienced single surgeon (TS). The results demonstrate overwhelming positivity when operative outcomes were subjected to post-operative grading by the double-blinded independent panel. The author accepts the limitations of a small independent panel size. However, the results still reveal a significant agreement of positive post-operative visual outcomes of the closed rhinoplasty technique. Furthermore, there was a minimal (0.8%) complication rate amongst the cohort. There were only two cases of soft tissue infections and both were amenable to oral antibiotics. In summary, the author has successfully utilised the endonasal approach in reduction, augmentation, nose-straightening, and functional-correction rhinoplasty. This study alone should therefore support its continuing use in modern day rhinoplasty.
A transcolumellar incision and elevation of these soft tissues from the medial and middle crura distinguish open from closed rhinoplasty [4].The main advantages of the open technique is therefore the increased exposure to the surrounding anatomy [5]. There is full visualisation of the medial, middle, and lateral crura bilaterally in their adjacent and undistorted anatomical resting positions [4, 6]. Certainly, an inexperienced surgeon obtains better appreciation of the optimal plane and can better control bleeding points utilising an open approach. The exposure also allows for more precise manipulation, suturing, and grafting potential. Modern advancements have allowed skilled endonasal surgeons to adopt grafting techniques through the closed approach. However, literature clearly illustrates that the open approach is the superior grafting method, especially in more complex cases [2]. The author appreciates the benefits of utilising the open technique in selected cases such as: asymmetric nasal tip; crooked nose deformity (lower two-thirds of nose); saddle nose deformity; cleft-lip nasal deformity; secondary rhinoplasty requiring complex structural grafting; and septal perforation repair [7]. Furthermore, compared to the endonasal approach, the exposure of external rhinoplasty also allows for greater visibility and teaching potential for observers.
Despite the above, the benefits of the endonasal technique must not be dismissed. Firstly, the open approach, by its very nature, causes extensive skeletonisation. The disruption of the tissues risks greater iatrogenic damage to the nose and increases the scarring effect. Secondly, more surgical dissection predisposes to more postoperative oedema, nerve dysfunction, and a prolonged recovery. The endonasal approach does not preclude to these problems and can even be said to give more immediate and predictable results [6, 8, 9]. Thirdly, the open approach risks visible scarring to the columella. The author understands that this argument has been a contentious issue with skeptics labelling this concern as unwarranted [2]. However, compared to endonasal technique, the risk of postoperative residual scarring remains an important differentiating issue. At a very minimum, there remains preferred indications for the closed approach. These include: upper-two thirds in standard cases; subtle supra-tip area surgery; isolated corrections in columella/rim/tip through pocket surgery; and revisions in nasal dorsum limited augmentations [2, 10]. The failure to catagorise and provide details of the endonasal operations performed represents another limitation of this study. This issue will be addressed in future research from the authors.
Finally, there needs to be a continued culture shift in the open vs closed rhinoplasty debate. Both procedures have inherit strengths and weaknesses and should be seen as complimentary. Although there is a modern trend to the open procedure, this study supports available evidence that warrants the continued use of the endonasal approach in selected cases. Many surgeons now recognise situations were a given approach offers advantages and may be considered preferable. Most also agree that a ‘grey area’ exists, where either approach would be appropriate and the results equivocal if well-performed [7]. Moreover, in these indifferent cases, the ultimate selection of approach should be governed by: patient anatomy; the aim of the procedure; and the comfort of a surgeon in performing a particular technique [1, 11].
It should be noted that, due to the extensive number of variables, there exists no valid single-surgeon study that compares results and reoperation rates of open and closed rhinoplasty. As a result, like this article, the literature is based on personal clinical experience and preferences. However, this substantial cohort, single surgeon approach, and significant results means that this author can advocate the use of the endonasal approach in the armamentarium of a skilled and experienced plastic surgeon.
Conclusion
The open vs closed approach to rhinoplasty surgery has been a contentious issue in recent years. It appears that the endonasal approach is losing popularity within the repertoire of a modern day plastic surgeon. The results of this paper support existing literature which advocates the benefits of the closed approach. Surgeons should appreciate that both open and closed approaches are complimentary. The favouring of a single approach is indicated in the scenarios discussed. The remaining cases seem to produce equivocal results and the choice of procedure should be based on patient anatomy, outcome aims, and the ability of a surgeon to perform their preferred technique.
Acknowledgements
The authors would like to acknowledge the help of Maliha Shoaib in preparing this manuscript.
Funding
The author can confirm of no funding interests.
Compliance with Ethical Standards
Conflict of interest
Authors can confirm no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Saif Al Azzawi, Email: saifazzawi8@gmail.com.
Thomas Kidd, Email: thomas.kidd1@nhs.net.
Taimur Shoaib, Email: taimur@shoaib.co.uk.
References
- 1.Alexander R. Fundamental terms, considerations, and approaches in rhinoplasty. Atlas Oral Maxillofac Surg Clin N Am. 1995;3:15–25. doi: 10.1016/S1061-3315(18)30113-6. [DOI] [PubMed] [Google Scholar]
- 2.Berghaus A. Modern rhinoplasty: is there a place for the closed approach? JAMA Facial Plast Surg. 2016;32:402–408. doi: 10.1055/s-0036-1585422. [DOI] [PubMed] [Google Scholar]
- 3.Tasman A. Rhinoplasty-indications and techniques. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2007;6:Doc09. [PMC free article] [PubMed] [Google Scholar]
- 4.Tebbetts JB. Open and closed rhinoplasty (minus the “versus”): analyzing processes. Aesthet Surg J. 2006;26:456–459. doi: 10.1016/j.asj.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Foda H. External rhinoplasty: a critical analysis of 500 cases. J Laryngol Otol. 2003;117:473–477. doi: 10.1258/002221503321892325. [DOI] [PubMed] [Google Scholar]
- 6.Burke A, Cook T. Open versus closed rhinoplasty: what have we learned? Curr Opin Otolaryngol Head Neck Surg. 2000;8:332–336. doi: 10.1097/00020840-200008000-00011. [DOI] [Google Scholar]
- 7.Cafferty A, Becker DG. Open and closed rhinoplasty. Clin Plast Surg. 2016;43:17–27. doi: 10.1016/j.cps.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Bagheri S, Khan H, Jahangirnia A, Rad S. An analysis of 101 primary cosmetic rhinoplasties. J Oral Maxillofac Surg. 2012;70:902–909. doi: 10.1016/j.joms.2011.02.075. [DOI] [PubMed] [Google Scholar]
- 9.Rettinger G. Risks and complications in rhinoplasty. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2008;6:Doc08. [PMC free article] [PubMed] [Google Scholar]
- 10.Perkins S, Patel A. Endonasal suture techniques in tip rhinoplasty. Facial Plast Surg Clin N Am. 2009;17:41–54. doi: 10.1016/j.fsc.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Nguyen P, et al. Surgical approaches in rhinoplasty. Annales de Chirurgie Plastique Esthétique. 2014;59:406–419. doi: 10.1016/j.anplas.2014.08.002. [DOI] [PubMed] [Google Scholar]


