Abstract
Background
As life expectancy rises, percutaneous coronary intervention (PCI) is being performed more frequently, even in elderly patients with acute myocardial infarction (AMI). This study evaluated outcomes of elderly patients with AMI complicated by heart failure (AMIHF), as defined by Killip Class ≥2 at admission, who undergo PCI.
Methods and Results
We retrospectively analyzed 185 patients with AMIHF aged ≥80 years (median age 85 years) who underwent PCI between 2009 and 2019. The median follow-up period was 572 days. The rates of in-hospital major bleeding (Bleeding Academic Research Consortium Type 3 or 5) and in-hospital all-cause mortality were 20.5% and 25.9%, respectively. The proportion of frail patients increased during hospitalization, from 40.6% at admission to 59.2% at discharge (P<0.01). The cumulative incidence of all-cause mortality was 36.3% at 1 year and 44.1% at 2 years. After adjusting for confounders, advanced age, Killip Class 4, final Thrombolysis in Myocardial Infarction flow grade <3, and longer door-to-balloon time were associated with higher mortality, whereas higher left ventricular ejection fraction and cardiac rehabilitation were associated with lower mortality (all P<0.05). Progression of frailty during hospitalization was an independent risk factor for long-term mortality in hospital survivors (P<0.01).
Conclusions
The management of patients with AMIHF aged ≥80 years who undergo PCI remains challenging, with high rates of in-hospital major bleeding, frailty progression, and mortality.
Key Words: Acute myocardial infarction, Elderly, Frailty, Heart failure, Percutaneous coronary intervention
Heart failure (HF) is a major complication of acute myocardial infarction (AMI) and AMI complicated by HF (AMIHF) is associated with worse outcomes.1–3 Percutaneous coronary intervention (PCI), which is beneficial for achieving rapid reperfusion, is an effective treatment for this serious condition.3,4 With increasing life expectancy, PCI is being performed more frequently in elderly patients with AMI.3–6 Previous studies have shown that AMIHF is more common in elderly than younger patients.2,5,6 However, there are limited data on the clinical outcomes of elderly patients with AMIHF who undergo PCI because many cardiovascular studies either exclude elderly patients altogether or only include those at lower risk.
Frailty is a biological syndrome that reflects a state of decreased physiological reserve and vulnerability to stressors. It is common in older adults.7,8 Like age, frailty has been reported to be associated with mortality and bleeding events in patients with cardiovascular disease.6–11 In recent years, both prognosis and quality of life have become more important, and frailty has been attracting attention. The stress of AMI itself, pulmonary congestion, end-organ hypoperfusion, and bed rest during hospitalization may increase frailty and decrease the ability to perform activities of daily living (ADLs) in elderly patients with AMIHF.
Therefore, this study evaluated the clinical characteristics, changes in frailty status during hospitalization, in-hospital outcomes, including bleeding complications and death, and long-term mortality in patients with AMIHF aged ≥80 years who underwent PCI.
Methods
Study Design and Population
This study was a retrospective single-center observational study. Initially, 2,873 consecutive patients with Type 1 myocardial infarction (MI) who were admitted within 24 h after symptom onset to Miyazaki Medical Association Hospital between January 2009 and December 2019 were eligible for inclusion. AMI was diagnosed based on the universal definition of MI proposed by the European Society of Cardiology and the American Heart Association.3,12,13 Emergency PCI was defined as procedures performed within 24 h after symptom onset. In the present analysis, 2,147 patients aged <80 years, 129 patients aged ≥80 years who did not undergo emergency PCI, and 412 patients with Killip Class 1 disease at admission were excluded. Thus, the study population consisted of 185 patients (Figure 1). The therapeutic strategy and the decision to perform PCI were at the discretion of the attending cardiologist according to the guidelines at that time. Follow-up information was obtained from hospital charts or by contacting patients, relatives, or referring physicians. The median duration of follow-up was 572 days (interquartile range [IQR] 36–1,159 days). Complete 1- and 2-year follow-up information was available for 95.1% and 85.4% of patients, respectively.
Figure 1.
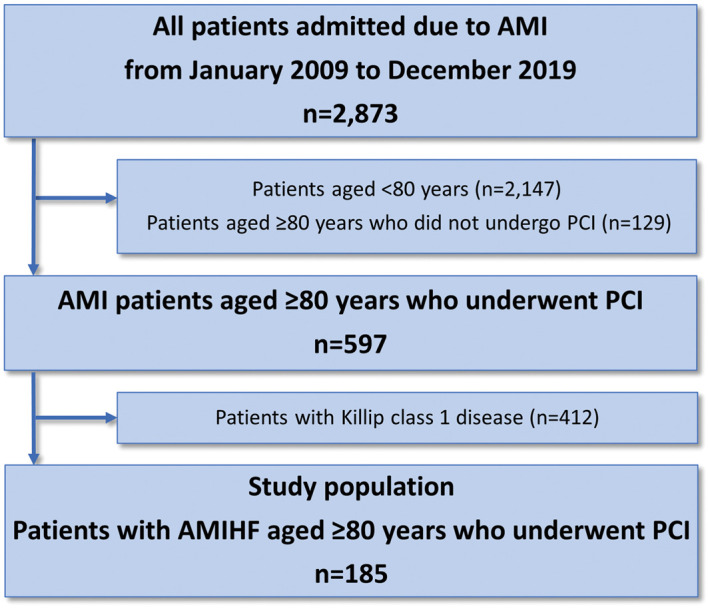
Study flowchart. AMI, acute myocardial infarction; AMIHF, acute myocardial infarction complicated by heart failure; PCI, percutaneous coronary intervention.
All patients provided written informed consent. The study protocol complied with the Declaration of Helsinki and the study was approved by the Institutional Review Board of Miyazaki Medical Association Hospital (2019-6, 2020-16).
Definitions and Endpoints
The severity of HF was assessed at admission based on the Killip classification. HF was defined as Killip Class ≥2 disease.1,4
The primary outcome of this study was all-cause mortality. The incidence of in-hospital major bleeding and in-hospital cardiac death, as well as changes in frailty status during hospitalization, were also assessed. Major bleeding during hospitalization was defined as Bleeding Academic Research Consortium (BARC) Type 3 or 5 bleeding, involving a decrease in hemoglobin of >3 g/dL, need for blood transfusion, cardiac tamponade, surgical intervention, intracranial hemorrhage, or fatal bleeding.9,14,15 Frailty was classified at admission and discharge according to the definition proposed by Dodson et al.9,10,15 Three domains of the frailty phenotype were assessed: walking (0=unassisted; 1=assisted; 2=wheelchair use or non-ambulatory); cognition (0=normal; 1=mildly impaired; 2=moderately to severely impaired); and basic ADLs, such as eating, dressing, bathing, and toileting (0=independent in all ADLs; 1=needs partial assistance; 2=needs full assistance). If patients could not answer questions about these domains by themselves due to high-flow oxygen or intubation, this information was obtained from family members. Patients were classified into the following 3 groups based on the total score: no frailty (score 0), mild frailty (score 1–2), or moderate-to-severe frailty (score ≥3). Patients with mild or moderate-to-severe frailty were defined as having frailty. In this registry, information about these 3 domains was recorded routinely at the time of admission and discharge to help prevent falls and decline in ADLs. Two or more trained physicians and nurses conducted these assessments independently. Any discrepancies were resolved in face-to-face meetings.
Statistical Analysis
Continuous variables are presented as the mean±SD or as the median and IQR, depending on the distribution of the variable. The significance of differences was analyzed using t-tests or the Mann-Whitney U test, as appropriate. Categorical variables are presented as numbers and percentages and were compared using the Chi-squared test or Fisher’s exact test, as appropriate. The Kaplan-Meier method was used to estimate the cumulative incidence of all-cause mortality and differences between groups were assessed using the log-rank test. In addition, a multivariate Cox proportional hazards model was constructed to evaluate predictors of all-cause mortality with adjustment for variables with P<0.1 in univariate analyses. Results are presented as hazard ratios (HRs) with 95% confidence intervals (CIs). A multivariate logistic regression model was also constructed to identify risk factors for frailty progression during hospitalization with adjustment for variables with P<0.1 in univariate analyses. Results are presented as odds ratios (ORs) with 95% CIs. All analyses were performed using JMP version 12.0.1 (SAS Institute, Cary, NC, USA). All tests were 2-sided, and P<0.05 was considered statistically significant.
Results
Baseline Characteristics
The baseline clinical characteristics of the 185 patients with AMIHF aged ≥80 years who underwent PCI are presented in Table 1. The median age was 85 years (IQR 82–88 years), 100 (54.1%) patients were female, and 156 (84.3%) patients had ST-segment elevation MI (STEMI). There were 67 (36.2%), 48 (25.9%), and 70 (37.8%) patients with Killip Class 2, Class 3, and Class 4 disease, respectively. The median left ventricular ejection fraction (LVEF) was 41% (IQR 32–49%), and 67 (36.2%) patients received mechanical support. Regarding medications, 182 (98.4%) patients were treated with dual antiplatelet therapy and 33 (17.8%) were treated with oral anticoagulants; 129 (69.7%) patients underwent cardiac rehabilitation during hospitalization. The PCI success rate, defined as final Thrombolysis in Myocardial Infarction (TIMI) flow grade 3, was 81.1%.
Table 1.
Characteristics of the Study Patients (n=185)
| Baseline characteristics | |
| Age (years) | 85 [82–88] |
| Female sex | 100 (54.1) |
| Hypertension | 146 (78.9) |
| Dyslipidemia | 61 (33.0) |
| Diabetes | 59 (31.9) |
| Previous MI | 25 (13.5) |
| Previous PCI | 25 (13.5) |
| Hemodialysis | 2 (1.1) |
| eGFR (mL/min/1.73 m2) | 45.6±20.6 |
| Peak CPK (IU/L) | 1,943 [576–4,181] |
| Peak CK-MB (IU/L; n=178) | 175 [54–383] |
| Characteristics at admission | |
| Killip class 2/3/4 | 67 (36.2)/48 (25.9)/70 (37.8) |
| Heart rate (beats/min) | 90 [70–104] |
| SBP (mmHg) | 121 [99–146] |
| STEMI | 156 (84.3) |
| LVEF (%) | 41 [32–49] |
| Angiographic and procedural characteristics | |
| Radial access | 102 (55.1) |
| Infarct-related artery | |
| Left main coronary artery | 16 (8.6) |
| Left anterior descending artery | 103 (55.7) |
| Left circumflex artery | 19 (10.3) |
| Right coronary artery | 47 (25.4) |
| Multivessel disease | 110 (59.5) |
| Mechanical (IABP, ECMO, or Impella) support | 67 (36.2) |
| IABP | 66 (35.7) |
| ECMO | 8 (4.3) |
| Impella | 1 (0.5) |
| Final TIMI grade 3 flow | 150 (81.1) |
| Onset-to-balloon time (min; n=172) | 322 [200–637] |
| Door-to-balloon time (min) | 92 [70–121] |
| Treatment during hospitalization | |
| Dual antiplatelet therapy | 182 (98.4) |
| Oral anticoagulation | 33 (17.8) |
| Cardiac rehabilitation | 129 (69.7) |
| Drugs at discharge in hospital survivors (n=137) | |
| ACE inhibitor or ARB | 81 (59.1) |
| β-blocker | 85 (62.0) |
| Mineralocorticoid receptor antagonist | 61 (44.5) |
| Sodium-glucose cotransporter 2 inhibitor | 2 (1.5) |
Data are expressed as the mean±SD, n (%), or median [interquartile range]. ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; CK-MB, creatine kinase-myocardial band; CPK, creatine phosphokinase; ECMO, extracorporeal membrane oxygenation; eGFR, estimated glomerular filtration rate; IABP, intra-aortic balloon pump; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; STEMI, ST-segment elevation myocardial infarction; TIMI, Thrombolysis in Myocardial Infarction.
Clinical characteristics according to access site and cardiac rehabilitation status are presented in Supplementary Table 1. In this study, 102 (55.1%) patients underwent transradial access. Compared with patients with transradial access, those with transfemoral access were more likely to be female and had a lower body weight and a higher rate of Killip Class 4 disease. Patients in the non-rehabilitation group were more likely to be frail at admission, had higher rates of Killip Class 4 disease and renal dysfunction, and had a lower LVEF than those in the rehabilitation group.
In-Hospital Outcomes
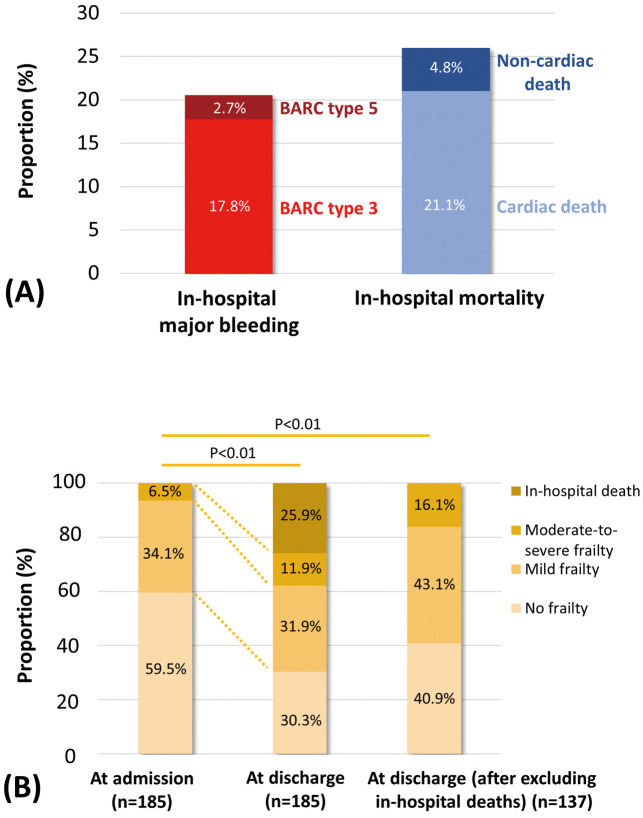
In-hospital major bleeding rate, in-hospital mortality, and changes in frailty status during hospitalization are shown in Figure 2. Overall, in-hospital major bleeding occurred in 20.5% of patients (BARC Type 3, 17.8%; BARC Type 5, 2.7%) and in-hospital death occurred in 25.9% of patients (cardiac death, 21.1%; non-cardiac death, 4.8%; Figure 2A). The proportion of non-frail patients decreased significantly during hospitalization, from 59.5% at admission (no frailty, 59.5%; mild frailty, 34.1%; moderate-to-severe frailty, 6.5%) to 30.3% at discharge (no frailty, 30.3%; mild frailty, 31.9%; moderate-to-severe frailty, 11.9%; in-hospital death, 25.9%; P<0.01). After excluding patients who died in hospital, 59.2% of patients (mild frailty, 43.1%; moderate-to-severe frailty, 16.1%) were classified as frail and 40.9% were classified as non-frail at discharge (Figure 2B).
Figure 2.
(A) In-hospital major bleeding rate and in-hospital mortality. (B) Change in frailty status during hospitalization. BARC, Bleeding Academic Research Consortium.
All-Cause Mortality
The cumulative incidence of all-cause mortality was 36.3% at 1 year and 44.1% at 2 years among all study patients (Figure 3). The incidence of all-cause mortality increased as Killip class worsened (log-rank, P<0.01; Supplementary Figure). Multivariate Cox proportional hazards analysis showed that advanced age (HR 1.07; 95% CI 1.01–1.13), Killip Class 4 disease (HR 1.88; 95% CI 1.13–3.09), final TIMI flow grade <3 (HR 2.04; 95% CI 1.20–3.36), and door-to-balloon time >90 min (HR 2.17; 95% CI 1.29–3.75) were independently associated with higher long-term mortality, whereas higher LVEF (HR 0.79; 95% CI 0.63–0.997) and cardiac rehabilitation (HR 0.30; 95% CI 0.18–0.49) were associated with lower long-term mortality in elderly patients with AMIHF (Table 2).
Figure 3.
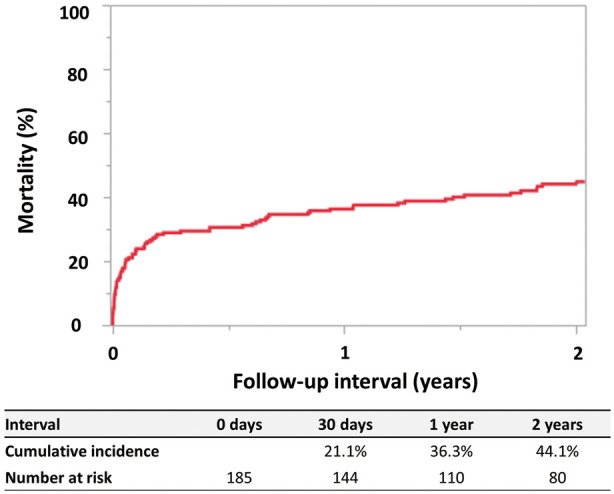
Kaplan-Meier curve for all-cause mortality in patients with acute myocardial infarction complicated by heart failure aged ≥80 years.
Table 2.
Cox Proportional Hazards Analysis of All-Cause Mortality in Elderly Patients With Acute MI Complicated by Heart Failure Undergoing PCI
| Unadjusted | AdjustedA | |||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Age, per 1-year increase | 1.07 (1.02–1.12) | <0.01 | 1.07 (1.01–1.13) | 0.01 |
| Female sex | 0.94 (0.62–1.42) | 0.76 | – | – |
| Frailty at admission | 1.87 (1.25–2.82) | <0.01 | 1.10 (0.66–1.83) | 0.72 |
| Diabetes | 1.39 (0.90–2.12) | 0.14 | – | – |
| eGFR <30 mL/min/1.73 m2 | 1.75 (1.09–2.74) | 0.02 | 0.89 (0.51–1.47) | 0.65 |
| Large infarct size, estimated based on peak CPKB | 1.28 (0.85–1.92) | 0.24 | – | – |
| Heart rate, per 1-beat/min increase | 1.00 (0.99–1.01) | 0.92 | – | – |
| Systolic blood pressure, per 1-mmHg increase | 0.99 (0.99–0.999) | 0.02 | 0.99 (0.98–1.00) | 0.06 |
| STEMI | 1.29 (0.74–2.43) | 0.40 | – | – |
| LVEF, per 10% increase | 0.65 (0.53–0.80) | <0.01 | 0.79 (0.63–0.997) | 0.047 |
| Anterior wall infarction | 1.09 (0.71–1.68) | 0.71 | – | – |
| Killip Class 4 disease | 2.20 (1.46–3.31) | <0.01 | 1.88 (1.13–3.09) | 0.02 |
| Multivessel disease | 0.93 (0.62–1.42) | 0.74 | – | – |
| Stent use | 0.93 (0.46–2.20) | 0.84 | – | – |
| Final TIMI grade <3 flow | 3.48 (2.19–5.39) | <0.01 | 2.04 (1.20–3.36) | <0.01 |
| Onset-to-balloon time >300 min (n=172) | 1.41 (0.92–2.20) | 0.12 | – | – |
| Door-to-balloon time >90 min | 2.13 (1.38–3.36) | <0.01 | 2.17 (1.29–3.75) | <0.01 |
| BARC Type 3 or 5 bleeding | 2.24 (1.38–3.51) | <0.01 | 1.06 (0.58–1.88) | 0.84 |
| Cardiac rehabilitation | 0.20 (0.13–0.30) | <0.01 | 0.30 (0.18–0.49) | <0.01 |
AAdjusted for variables with P<0.1 in univariate analyses. BLarge infarct size estimated using peak CPK was defined as peak CPK higher than the median peak CPK (1,943 IU/L). BARC, Bleeding Academic Research Consortium; CI, confidence interval; HR, hazard ratio. Other abbreviations as in Table 1.
Progression of Frailty During Hospitalization and Mortality
We focused on patients whose frailty scores worsened during hospitalization. After excluding patients with moderate-to-severe frailty at admission and those who died in hospital (n=56), 41 (31.8%) patients experienced frailty progression during hospitalization and 88 (68.2%) did not (Table 3). Compared with patients without frailty progression, a higher proportion of patients with frailty progression had diabetes. They also had a lower estimated glomerular filtration rate. Radial artery access for PCI was less common in patients with frailty progression. There were no significant differences in the rate of cardiac rehabilitation between the 2 groups. In multivariate logistic regression analysis, diabetes (OR 4.44; 95% CI 1.90–10.83) was associated with frailty progression, whereas radial artery access for PCI (OR 0.30; 95% CI 0.13–0.68) was inversely associated with frailty progression (Table 4). The results were consistent even after adjustment by the addition of Killip Class 4 disease to the variables listed in Table 4 (diabetes, OR 4.57 [95% CI 1.94–11.23]; radial artery access, OR 0.32 [95% CI 0.14–0.74]). Kaplan-Meier analysis and multivariate Cox proportional hazards analysis showed that all-cause mortality was much higher among patients with than without frailty progression (log-rank, P<0.01; adjusted HR 2.61; 95% CI 1.38–4.95; Figure 4; Supplementary Table 2).
Table 3.
Comparison of Characteristics Between Patients With and Without Frailty Progression During Hospitalization
| Frailty progression (n=41) |
No frailty progression (n=88) |
P value | |
|---|---|---|---|
| Age (years) | 85 [82–88] | 84 [82–88] | 0.93 |
| Female sex | 25 (61.0) | 44 (50.0) | 0.24 |
| Hypertension | 34 (82.9) | 72 (81.8) | 0.88 |
| Diabetes | 20 (48.8) | 17 (19.3) | <0.01 |
| History of stroke | 8 (19.5) | 11 (12.5) | 0.30 |
| Hemodialysis | 1 (1.4) | 1 (2.4) | 0.54 |
| eGFR (mL/min/1.73 m2) | 45.3±19.1 | 51.7±20.5 | 0.04 |
| Peak CPK (IU/L) | 906 [431–3,534] | 1,634 [739–3,994] | 0.18 |
| Peak CK-MB (IU/L; n=126) | 73 [38–299] | 149 [61–377] | 0.17 |
| Killip Class 4 disease | 14 (34.2) | 19 (21.6) | 0.13 |
| STEMI | 33 (80.5) | 72 (81.8) | 0.86 |
| LVEF (%) | 42.0 [37.0–49.0] | 44.1 [35.8–51.5] | 0.42 |
| Anterior wall infarction | 28 (68.3) | 59 (67.1) | 0.89 |
| Multivessel disease | 23 (56.1) | 52 (59.1) | 0.75 |
| Radial access | 18 (43.9) | 61 (69.3) | <0.01 |
| Mechanical support | 14 (34.1) | 22 (25.0) | 0.28 |
| Final TIMI flow grade 3 | 34 (82.9) | 81 (92.1) | 0.12 |
| BARC Type 3 or 5 bleeding | 4 (9.8) | 9 (10.2) | 1.00 |
| Cardiac rehabilitation | 35 (85.4) | 80 (90.9) | 0.35 |
| Duration of hospitalization (days) | 22 [16–40] | 23 [16–30] | 0.45 |
Data are expressed as n (%) or as the median (interquartile range). Abbreviations as in Tables 1,2.
Table 4.
Risk Factors for Frailty Progression During Hospitalization in Elderly Patients With Acute MI Complicated by Heart Failure Who Underwent PCI
| OR (95% CI) | P value | |
|---|---|---|
| Diabetes | 4.44 (1.90–10.83) | <0.01 |
| eGFR <30 mL/min/1.73 m2 | 2.07 (0.69–6.18) | 0.19 |
| Radial access | 0.30 (0.13–0.68) | <0.01 |
The multivariate logistic regression model adjusted for variables with P<0.1 in univariate analyses (Table 3). OR, odds ratio. Other abbreviations as in Tables 1,2.
Figure 4.
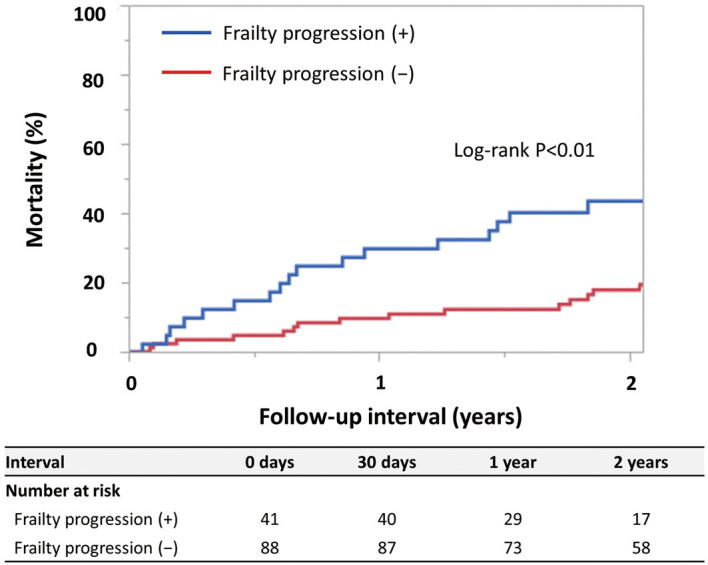
Kaplan-Meier curves for all-cause mortality in patients with acute myocardial infarction complicated by heart failure aged ≥80 years according to frailty progression status during hospitalization.
Discussion
The main findings of this study are as follows: (1) among 597 consecutive patients with AMI aged ≥80 years who underwent emergency PCI, 185 (31.0%) had HF; (2) among these elderly patients, the rates for in-hospital major bleeding, in-hospital mortality, and 1- and 2-year mortality were 20.5%, 25.9%, 36.3%, and 44.1%, respectively; (3) advanced age, Killip Class 4 disease, final TIMI flow grade <3, and longer door-to-balloon time are associated with higher all-cause mortality, whereas higher LVEF and cardiac rehabilitation are associated with lower all-cause mortality; (4) the proportion of frail patients increased during hospitalization; and (5) frailty progression during hospitalization is an independent risk factor for all-cause mortality in hospital survivors of AMIHF.
Acute HF is a frequent complication of AMI. The combination is associated with a particularly poor prognosis.1,2,5,16,17 Several observational studies have reported that HF is more frequently observed in elderly than younger patients.2,5,6,17 As the global population ages, the development of better therapeutic strategies for elderly patients with AMIHF is essential. The current guidelines on STEMI, non-STEMI, and HF recommend immediate implementation of an invasive strategy in patients with AMIHF.3,16,18 However, elderly patients, especially those with HF, have often been excluded from major clinical trials of cardiovascular interventions because of concerns about the increased risk of adverse events, comorbidities, and limited life expectancy. Consequently, optimal management of elderly patients with AMIHF is less clear. Among developed countries, Japan has the largest number of elderly patients with cardiovascular disease in a rapidly aging society.5,19 Comprehensive data from Japan will be crucial for developing perspectives in other countries. In the present study, the proportion of elderly patients aged ≥80 years among all patients with AMI was as high as 25.3%, and 82.2% of patients in this age group underwent emergency PCI. These proportions are consistent with those of the largest nationwide Japanese AMI registry, in which 23.6% of patients were aged ≥80 years and the PCI rate in this age group was 79.9%.5 Our data closely reflect the current status of patients with AMI in Japan.
In the present study, in-hospital and 1- and 2-year mortality were as high as 25.9%, 36.3%, and 44.1%, respectively, among patients with AMIHF aged ≥80 years who underwent PCI. In addition, door-to-balloon time >90 min was associated with higher all-cause mortality, whereas cardiac rehabilitation was associated with lower all-cause mortality in this population. Our results indicate that the management of elderly patients with AMIHF remains challenging, even in the primary PCI era. The American Heart Association’s Mission: Lifeline® program includes door-to-balloon time ≤90 min and cardiac rehabilitation referral for inpatients as important performance measures for STEMI treatment.20 Given our results, these 2 performance indicators may be effective in elderly patients with AMIHF, who are considered to be at very high risk for all-cause mortality.
The unique features of this study are that it showed changes in frailty status during hospitalization and that it explored the effect of frailty progression during hospitalization on all-cause mortality in elderly patients with AMIHF who underwent PCI. Recent studies have reported that frailty is a strong predictor of mortality in patients with AMI and patients with HF.7,9,11,21,22 Significant decreases in mortality among elderly patients with cardiovascular disease have led to a greater focus on functional outcomes and quality of life, and frailty has become a high-priority theme. Immobility, bed rest, acquired muscle weakness, and pressure ulcers during hospitalization, including intensive care unit stay, often exacerbate pre-existing geriatric conditions in elderly patients with acute cardiovascular disease.23 In addition, chronic kidney disease, a common comorbidity in patients with cardiovascular disease, has been reported to be associated with frailty progression.24,25 Although there were few dialysis patients in the present study, a clinical study has shown progression of mobility impairment in this population.25 We previously demonstrated that, among nonagenarians with AMI who underwent PCI, the proportion of patients with frailty increased during hospitalization, from 43.8% at admission to 60.7% at discharge.15 We also reported that although not significant in a multivariate analysis, frailty progression was more frequently observed in patients with AMIHF than in those with Killip Class 1 disease.9 The present study clearly showed that frailty status often worsened during hospitalization in elderly patients with AMIHF and that frailty progression is an independent risk factor for all-cause mortality in hospital survivors of AMIHF. Furthermore, diabetes was associated with frailty progression, whereas radial artery access for PCI was inversely associated with frailty progression. Radial artery access is associated with favorable outcomes in patients with AMI.3,26,27 Radial artery access may decrease the risk of bleeding, shorten the duration of bed rest, and consequently prevent frailty progression. In the present retrospective observational study, patients with transfemoral access were more likely to be female and had a lower body weight and a higher rate of Killip Class 4 disease. Body size, disease severity, and other factors may have influenced the decision regarding access site. Therefore, future large-scale studies are needed to determine whether radial artery access affects frailty status in elderly patients with AMIHF.
Bleeding complications are significant risk factors for subsequent adverse outcomes in patients with AMI who undergo PCI, such as MI, stent thrombosis, stroke, and death.9,14,28–30 Therefore, the identification and management of patients at high bleeding risk are of major importance. Recently, in East Asian populations, frailty and HF have been highlighted as strong risk factors for bleeding in addition to the Academic Research Consortium High Bleeding Risk criterion of older age (≥75 years).28,29 However, limited data are available on bleeding in elderly patients with AMIHF. The present study showed that the in-hospital major bleeding rate of elderly patients with AMIHF undergoing PCI can be as high as 20.5%. Impaired liver and renal function and frailty progression due to serious hypoperfusion and hypoxia affect drug metabolism, which increases bleeding risk. In addition, mechanical support during HF treatment results in an increased risk of bleeding.6,7,23,28–30 Our results, together with those of previous studies, suggest that efforts are needed to reduce bleeding complications, for example by employing radial artery access during PCI and reconsidering the dose and duration of dual antiplatelet therapy, in elderly patients with AMIHF.
Study Limitations
This study has several limitations. First, this was a retrospective single-center observational study with a relatively small sample size, not a randomized controlled trial. Therefore, there may have been selection bias and unmeasured confounders. In addition, the median follow-up duration was 572 days, which may be relatively short for the evaluation of long-term prognosis. Second, HF at admission was assessed based on the Killip classification, which has limitations in the acute setting, because symptoms and signs may be non-specific. However, this classification is widely used in clinical practice, and physical findings of pulmonary rales indicate an unfavorable hemodynamic state and are highly predictive of worse outcomes.1,2,4,17 Third, referral to cardiac rehabilitation and the decision to perform PCI were left to the discretion of each attending physician. Especially regarding cardiac rehabilitation, some patients may not have received it because their condition or frailty was too advanced. In fact, in this study, patients without cardiac rehabilitation were more likely to be frail at admission, had higher rates of Killip Class 4 disease and renal dysfunction, and had a lower LVEF than those with cardiac rehabilitation. However, even after adjusting for these confounders, cardiac rehabilitation was significantly associated with lower long-term mortality. Further randomized controlled trials are needed to examine the effects of cardiac rehabilitation in elderly patients with AMIHF. Finally, the definition of frailty used in the present study may be less objective compared with conventional definitions based on cognitive tests, grip strength, and gait speed.7,21 Meanwhile, this novel definition enabled frailty to be assessed more easily and safely, even in the acute phase of AMIHF.
Conclusions
This study demonstrated that the management of patients with AMIHF aged ≥80 years who undergo PCI remains challenging, with high rates of in-hospital major bleeding, frailty progression, and mortality.
Sources of Funding
No funds were received for this study.
Disclosures
The authors declare that there are no conflicts of interest.
IRB Information
This study was approved by the Institutional Review Board of Miyazaki Medical Association Hospital (2019-6, 2020-16).
Supplementary Files
Supplementary Table 1. Characteristics According to Access Site and Cardiac Rehabilitation Status Supplementary Table 2. Cox Proportional Hazards Analysis of All-Cause Mortality in Hospital Survivors Supplementary Figure.
Data Availability
The deidentified participant data will not be shared.
References
- 1. Desta L, Jernberg T, Löfman I, Hofman-Bang C, Hagerman I, Spaak J, et al.. Incidence, temporal trends, and prognostic impact of heart failure complicating acute myocardial infarction. The SWEDEHEART Registry (Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies): A study of 199,851 patients admitted with index acute myocardial infarctions, 1996 to 2008. JACC Heart Fail 2015; 3: 234–242. [DOI] [PubMed] [Google Scholar]
- 2. Bahit MC, Lopes RD, Clare RM, Newby LK, Pieper KS, Van de Werf F, et al.. Heart failure complicating non-ST-segment elevation acute coronary syndrome: Timing, predictors, and clinical outcomes. JACC Heart Fail 2013; 1: 223–229. [DOI] [PubMed] [Google Scholar]
- 3. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al.. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018; 39: 119–177. [DOI] [PubMed] [Google Scholar]
- 4. Fukutomi M, Nishihira K, Honda S, Kojima S, Takegami M, Takahashi J, et al.. Difference in the in-hospital prognosis between ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction with high Killip class: Data from the Japan Acute Myocardial Infarction Registry. Eur Heart J Acute Cardiovasc Care 2021; 10: 503–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kojima S, Nishihira K, Takegami M, Nakao YM, Honda S, Takahashi J, et al.. Nationwide real-world database of 20,462 patients enrolled in the Japanese Acute Myocardial Infarction Registry (JAMIR): Impact of emergency coronary intervention in a super-aging population. Int J Cardiol Heart Vasc 2018; 20: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Madhavan MV, Gersh BJ, Alexander KP, Granger CB, Stone GW.. Coronary artery disease in patients ≥80 years of age. J Am Coll Cardiol 2018; 71: 2015–2040. [DOI] [PubMed] [Google Scholar]
- 7. Singh M, Stewart R, White H.. Importance of frailty in patients with cardiovascular disease. Eur Heart J 2014; 35: 1726–1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Morici N, De Servi S, De Luca L, Crimi G, Montalto C, De Rosa R, et al.. Management of acute coronary syndromes in older adults. Eur Heart J 2022; 43: 1542–1553. [DOI] [PubMed] [Google Scholar]
- 9. Nishihira K, Yoshioka G, Kuriyama N, Ogata K, Kimura T, Matsuura H, et al.. Impact of frailty on outcomes in elderly patients with acute myocardial infarction who undergo percutaneous coronary intervention. Eur Heart J Qual Care Clin Outcomes 2021; 7: 189–197. [DOI] [PubMed] [Google Scholar]
- 10. Dodson JA, Hochman JS, Roe MT, Chen AY, Chaudhry SI, Katz S, et al.. The association of frailty with in-hospital bleeding among older adults with acute myocardial infarction: Insights from the ACTION Registry. JACC Cardiovasc Interv 2018; 11: 2287–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Uchikado Y, Ikeda Y, Ohishi M.. Current understanding of the role of frailty in cardiovascular disease. Circ J 2020; 84: 1903–1908. [DOI] [PubMed] [Google Scholar]
- 12. Thygesen K, Alpert JS, White HD; Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction.. Universal definition of myocardial infarction. Eur Heart J 2007; 28: 2525–2538. [DOI] [PubMed] [Google Scholar]
- 13. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al.. Third universal definition of myocardial infarction. Eur Heart J 2012; 33: 2551–2567. [DOI] [PubMed] [Google Scholar]
- 14. Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al.. Standardized bleeding definitions for cardiovascular clinical trials: A consensus report from the Bleeding Academic Research Consortium. Circulation 2011; 123: 2736–2747. [DOI] [PubMed] [Google Scholar]
- 15. Nishihira K, Watanabe N, Kuriyama N, Shibata Y.. Clinical outcomes of nonagenarians with acute myocardial infarction who undergo percutaneous coronary intervention. Eur Heart J Acute Cardiovasc Care 2020; 9: 488–495. [DOI] [PubMed] [Google Scholar]
- 16. Harjola VP, Parissis J, Bauersachs J, Brunner-La Rocca HP, Bueno H, Čelutkienė J, et al.. Acute coronary syndromes and acute heart failure: A diagnostic dilemma and high-risk combination. A statement from the Acute Heart Failure Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2020; 22: 1298–1314. [DOI] [PubMed] [Google Scholar]
- 17. Steg PG, Dabbous OH, Feldman LJ, Cohen-Solal A, Aumont MC, López-Sendón J, et al.. Determinants and prognostic impact of heart failure complicating acute coronary syndromes: Observations from the Global Registry of Acute Coronary Events (GRACE). Circulation 2004; 109: 494–499. [DOI] [PubMed] [Google Scholar]
- 18. Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, et al.. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021; 42: 1289–1367. [DOI] [PubMed] [Google Scholar]
- 19. Yasuda S, Miyamoto Y, Ogawa H.. Current status of cardiovascular medicine in the aging society of Japan. Circulation 2018; 138: 965–967. [DOI] [PubMed] [Google Scholar]
- 20. American Heart Association.. Mission: Lifeline STEMI receiving center. https://www.heart.org/-/media/Files/Professional/Quality-Improvement/Mission-Lifeline/MLSTEMIReceivingRecognition2022.pdf (accessed December 31, 2021).
- 21. Afilalo J, Alexander KP, Mack MJ, Maurer MS, Green P, Allen LA, et al.. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol 2014; 63: 747–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pandey A, Kitzman D, Reeves G.. Frailty is intertwined with heart failure: Mechanisms, prevalence, prognosis, assessment, and management. JACC Heart Fail 2019; 7: 1001–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Damluji AA, Forman DE, van Diepen S, Alexander KP, Page RL 2nd, Hummel SL, et al.. Older adults in the cardiac intensive care unit: Factoring geriatric syndromes in the management, prognosis, and process of care: A scientific statement from the American Heart Association. Circulation 2020; 141: e6–e32. [DOI] [PubMed] [Google Scholar]
- 24. Guerville F, de Souto Barreto P, Taton B, Bourdel-Marchasson I, Rolland Y, Vellas B, et al.. Estimated glomerular filtration rate decline and incident frailty in older adults. Clin J Am Soc Nephrol 2019; 14: 1597–1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Moorthi RN, Fadel WF, Cranor A, Hindi J, Avin KG, Lane KA, et al.. Mobility impairment in patients new to dialysis. Am J Nephrol 2020; 51: 705–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Karrowni W, Vyas A, Giacomino B, Schweizer M, Blevins A, Girotra S, et al.. Radial versus femoral access for primary percutaneous interventions in ST-segment elevation myocardial infarction patients: A meta-analysis of randomized controlled trials. JACC Cardiovasc Interv 2013; 6: 814–823. [DOI] [PubMed] [Google Scholar]
- 27. Dworeck C, Redfors B, Völz S, Haraldsson I, Angerås O, Råmunddal T, et al.. Radial artery access is associated with lower mortality in patients undergoing primary PCI: A report from the SWEDEHEART registry. Eur Heart J Acute Cardiovasc Care 2020; 9: 323–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Urban P, Mehran R, Colleran R, Angiolillo DJ, Byrne RA, Capodanno D, et al.. Defining high bleeding risk in patients undergoing percutaneous coronary intervention. Circulation 2019; 140: 240–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nakamura M, Kimura K, Kimura T, Ishihara M, Otsuka F, Kozuma K, et al.. JCS 2020 guideline focused update on antithrombotic therapy in patients with coronary artery disease. Circ J 2020; 84: 831–865. [DOI] [PubMed] [Google Scholar]
- 30. Nishihira K, Honda S, Takegami M, Kojima S, Asaumi Y, Suzuki M, et al.. Impact of bleeding on mortality in patients with acute myocardial infarction complicated by cardiogenic shock. Eur Heart J Acute Cardiovasc Care 2021; 10: 388–396. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Characteristics According to Access Site and Cardiac Rehabilitation Status Supplementary Table 2. Cox Proportional Hazards Analysis of All-Cause Mortality in Hospital Survivors Supplementary Figure.
Data Availability Statement
The deidentified participant data will not be shared.