Abstract
On a global scale, many major rural health issues have persisted for decades despite the introduction of new health interventions and public health policies. Although research efforts have generated valuable new knowledge about the aetiology of health, disease and health inequities in rural communities, rural health systems remain to be some of the most deprived and challenged in both the developing and developed world. While the reasons for this are many, a significant factor contributing to the current state of play is the pressing need for methodological innovation and relevant scientific approaches that have the capacity to support the translation of novel solutions into ‘real world’ rural contexts. Fortunately, complex systems approaches, which have seen an increase in popularity in the wider public health literature, could provide answers to some of the most resilient rural health problems in recent times. The purpose of this article is to promote the value and utility of a complex systems approach in rural health research. We explain the benefits of a complex systems approach and provide a background to the complexity sciences, including the main characteristics of complex systems. Two popular computational methods are described. The next step for rural health research involves exploring how a complex systems approach can help with the identification and evaluation of new and existing solutions to policy-resistant rural health issues. This includes generating awareness around the analytical trade-offs that occur between the use of traditional scientific methods and complex systems approaches.
Keywords: STATISTICS & RESEARCH METHODS, HEALTH SERVICES ADMINISTRATION & MANAGEMENT, PUBLIC HEALTH
Introduction
The field of complexity science engenders its own lexicon, theories and concepts. We have therefore provided the following key definitions and explanations to assist the reader with an understanding of the material forthcoming.
Terms and definitions
Complex systems are found across the micro (eg, biological), meso (eg, individual) and macro (eg, social) levels of the physical and natural world. Complex systems include biological systems, the earth’s atmosphere and climate, ant colonies, diseases, political entities, the stock market, rainforests, organisations and corporations, and pertinent to this article, rural health systems. A complex system is:
…made up of many heterogenous elements; these elements interact with each other; the interactions produce an emergent effect that is different from the effects of the individual elements; and this effect persists over time and adapts to changing circumstances. (Luke and Stamatakis, p.2)1
In attempting to map and understand complex systems, systems modellers and analysts often attempt to identify leverage points. Leverage points are key places within a complex system where a small intervention can produce a large (positive) effect on the system’s outcome. Leverage points are frequently counterintuitive, meaning that change is often required to be enacted in the opposite direction to produce the intended outcome. The points of greatest leverage within a system may not necessarily be obvious at first glance or may even exist beyond initial conceptualisations of a system.
The silver bullet, the miracle cure, the secret passage, the magic password, the single hero who turns the tide of history. We not only want to believe that there are leverage points, but we also want to know where they are and how to get our hands on them. Leverage points are points of power. (Meadows, p.145)2
Background and purpose
The purpose of this article is twofold. First, to encourage new ways of thinking about how rural health issues and health inequalities are created, maintained and prevented through a systems research lens; and second, to promote the value and utility of a complex systems approach in this space. Although the article is written with the rural health researcher in mind, the content may also be interesting to a wider BMJ Open readership, including clinicians, service providers, stakeholders and policy-makers tackling the results of failed and/or troubled healthcare systems.
Why rural health?
Rural health is a multidisciplinary area of study within the field of public health that has largely been neglected from a funding and research perspective.3 While specialist research groups and university departments around the world—Australia, Canada, USA, New Zealand, UK and Europe—are producing excellent (traditional) work in the area of rural health,4 5 the disparities in health outcomes and health inequalities between urban and rural communities continue to persist in the face of new health interventions and policies.6–8 While the reasons for this are many, including factors related to geography, healthcare access, service provision, workforce retention, cultural sensitivities and wider political systems,9 it is these authors’ opinion that the rural health research field is also in drastic need of scientific innovation if it is to seriously tackle the complex global challenges that it faces. The answers we seek, and the change that is desired for rural communities by way of research and advances in knowledge, may lie in the field of systems research and complexity science and its many diverse approaches, methods and models.
Traditional methods in a complex world
Against a backdrop of increasing global interconnectedness, a growing number of researchers have questioned whether clinical and epidemiological methods can alone identify effective solutions to the most resilient public health problems in recent times.10–15 Arguments have centred around the fact that randomised controlled trials (RCTs) and experimental study designs, considered to be the ‘gold standard’ approaches for assessing causality, are only able to quantify the efficacy of a targeted individual-level health intervention.11–13 16 Attempts to ‘scale-up’ evidence-based clinical and behavioural interventions and deliver them into complex, uncontrolled, real-world settings without consideration of the broader sociopolitical context is known to erode their fidelity, adoption, maintenance and effectiveness.17 18
While the traditional Person, Intervention, Comparison, Outcome (PICO) framework has been met with considerable success and should continue to be applied to address well-defined causal research questions, the very act of controlling for background noise; the collapsing down of complexity; the reliance on data at the expense of theory; and desire to increasingly sharpen the effect of individual-level health interventions is not optimal for all health problems, social contexts and circumstances.12 14–16 19 20 The occurrence of health and disease across populations, including rural communities, can also be viewed as a product of the complex interactions that occur among biological, behavioural, societal, environmental and political determinants.10 19 21 This line of thinking encourages debate around what exactly constitutes ‘a cause’ from a scientific perspective, and where within ‘the system’ the most appropriate leverage point may be.10 11
Analytical reductionism can only deliver on so much if the goal of research is to: (1) ask questions about the effectiveness of upstream interventions that exert their effect on downstream factors and health outcomes over an extended timescale; and/or (2) ask questions about how new or existing solutions can be supported or degraded in context of the wider health system and its behaviour.10 12 17 18 22 Complementary research approaches are required to explore the intermediate and distal pathways that shape population health, and by definition rural health, from a broad perspective.
From reductionism to complexity
In response to the need for system-level evaluations of health interventions, there has been a recent groundswell of interest in epidemiology and public health around the use of complex systems approaches from the field of complexity science.16 21–27 Complex systems approaches are used to study discontinuous relations, complex forms of non-linear feedback between factors across multiple levels, networks between people, groups and their environment, and processes of exchange between individual actors in systems that give rise to emergent macro-level system behaviours.1 10 21 23–26 28–32 There is mounting evidence to suggest that a complex systems approach can be of practical assistance in both explaining mechanisms driving adverse health outcomes and system behaviour and also determining where and how to intervene through optimal leverage to achieve positive population health outcomes.18 23–25 27
Despite growing momentum around complex systems approaches, their specific application to issues contained within rural health has received a lack of attention aside from a few notable exceptions, including systems mapping33–35 and dynamic modelling36 studies. Complex systems approaches may help to identify new rural health solutions, identify key leverage points to address workforce issues such as provider maldistribution and shortage,37 support cost-benefit decision-making, and contribute to the evaluation of existing strategies given competing priorities and the balancing of limited resources. While the use of a complex systems approach may not necessarily differ methodologically between urban, semi-urban and rural health contexts, the contribution of systems research in rural health specifically lies in the generation of new evidence and knowledge to complement traditional scientific inquiry.
What is complexity science?
Complexity science is a discipline that attempts to understand and respond to problems that are dynamic and unpredictable, multidimensional and comprise various interrelated actors and components.38 Researchers who study complexity, and by extension complex problems, focus on the interactions among various elements within a complex system, rather than on the role and contribution of those elements in isolation.28 39
Where appropriate, complexity science proponents will advocate for a systems thinking perspective over a reductionist one, as doing so is to consider the whole system, and multiple interacting elements of it, as the primary unit of analysis.28 33 35 39 This affords insight into how the constituent elements of a complex system converge in context of a much greater whole, which is useful when attempting to make sense of resilient, persistent and policy resistant problems.12
Mapping the complexity sciences
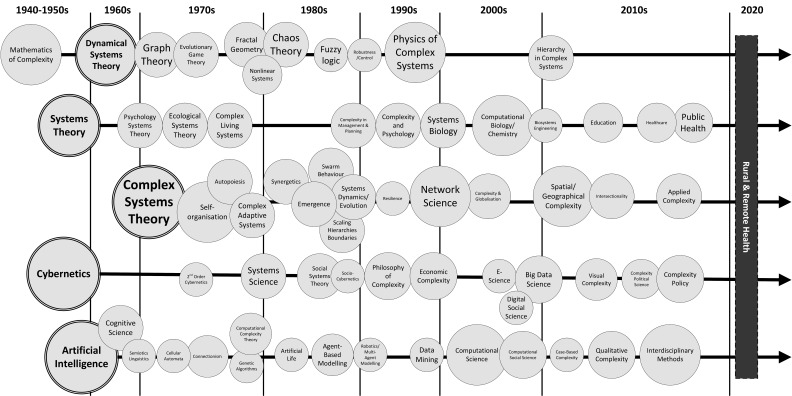
Complexity science incorporates multiple traditions, disciplines, methods, techniques and analytical tools. The Map of the Complexity Sciences40 (figure 1) shows the historical progression of five major intellectual traditions over several decades. The ‘map’ shows that there is no single, unified understanding of what complexity science is when it is subjected to formal investigation and analysis.39 Which complex systems approach to adopt depends on many factors, including available resources, individual expertise and the type of problem to be examined.
Figure 1.
Map of the complexity sciences. Redrawn and modified from Castellani and Gerrits.40 The full colour depiction with associated scholars in the corresponding fields can be viewed at: https://www.art-sciencefactory.com/complexity-map_feb09.html. The five traditions are: (1) dynamical systems theory; (2) systems theory; (3) complex systems theory; (4) cybernetics; and (5) artificial intelligence. Rural health is indicated from ~2022 onwards leaving open the possibility of applying complex systems approaches to contemporary issues in this space.
Characteristics of complex systems
There are discernible characteristics that are universal to all complex systems. Type 2 diabetes mellitus (T2DM), a significant issue in the Australian rural health sector, is selected to elucidate the key concepts (table 1). This section elaborates in greater detail on the definition of a complex system provided at the opening of the Communication.1
Table 1.
Complex systems characteristics
| Characteristic | Description | T2DM example |
| Multiple system levels, scalable | Complex systems vary in type, size and scale, from the micro (eg, molecular, cellular), through to the meso (eg, individual) and macro (eg, socioeconomic, political) levels. |
|
| Diverse range of agents (ie, people and organisations), and factors | Complex systems contain many fundamentally different agents and factors that interact, both within and across multiple system levels. | The occurrence of T2DM is influenced by a multitude of agents and factors:
The above list is by no means comprehensive, and many categories can be further expanded. However, the question remains: if decisions and actions at higher levels of the T2DM system influence and exert their effect on proximate individual behaviours and biology, then is it not reasonable to consider distal determinants as part of the broader set of causes to which T2DM emerges? If new Government legislation increased the number of Continuing Professional Development (CPD) credits that Allied Health Professionals were required to undertake annually, and hypothetically this reduced the occurrence of T2DM in the aggregate, then it can be concluded that the legislation change was indeed a causal factor, and perhaps an important leverage point. Any unintended and counterintuitive effects that result from this decision would need to be examined using a complex systems approach that has the capacity to model, simulate and forecast causal feedback within systems. |
| Open boundaries | Complex systems are ‘open systems’ with permeable boundaries. They continually learn and reconfigure in response to internal perturbation and external influence and intervention. |
|
| Adaptive and self-organising | Complex systems continually shift towards and away from acceptable boundaries of safety and performance. Abrupt transitions without adequate adaptation to maintain equilibrium can result in a tipping point, or system failure. |
|
| Complex behaviours and relationships | Complex systems exhibit non-linear behaviours and feedback among its many agents and factors. This means that small causes can have large effects and vice versa. |
|
| Emergent properties | Complex systems give rise to emergence. Emergence is defined as difficult-to-predict, higher-level patterns, behaviours and/or outputs. |
|
Two complex systems approaches
In the health sciences, two complex systems approaches, agent-based modelling (ABM) and system dynamics (SD) modelling, are gaining popularity due to their capacity to capture and communicate the behaviours and dynamics of complex systems23 41–43 (table 1). Rural health researchers are encouraged to explore how ABM and SD modelling may help with the identification, implementation and evaluation of new and existing strategies within complex rural health systems.
Agent-based modelling (ABM)
ABM is a type of microsimulation whereby interactions between synthetic populations of individual agents (eg, molecules, cells, healthcare professionals, patients) can be observed within a computational environment.31 32 Ideally, these interactions at the individual-level produce various macro-level patterns and complex behaviours that can grow, reflect or explain real-world phenomena.32 Agents can learn, adapt and respond to change based on the programming of demographic, lifestyle and environmental characteristics.29 Empirical data and/or expert theories can be used to instantiate ABMs depending on the modelling purpose (eg, prediction, description, explanation).41 42 44
Methodologically, ABM can be performed hundreds or even thousands of times and the modelled outputs compared under different hypothetical scenarios.1 20 ABM is an in-silico laboratory that has the capacity to evaluate the potential effectiveness of health policies over time.41 42 For example, ABM could be used to estimate the incidence rate of T2DM within a virtual rural community following the implementation of various hypothetical health interventions and policies under changing environmental conditions. The reader is referred to several comprehensive resources covering the origins, purpose and use of ABM,1 20 29–32 41 42 including issues pertaining to the development, verification and validation of simulations.44 45
System dynamics (SD) modelling
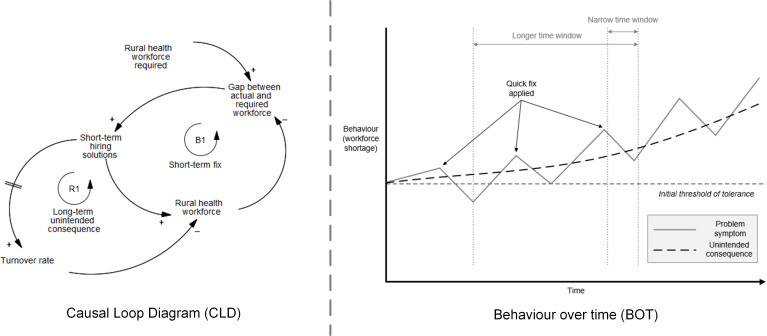
The first phase of SD modelling may involve the development of a causal loop diagram (CLD).33–35 46–48 A CLD is a qualitative model that describes the conceptual, causal relationships between variables that comprise a complex system. There are two types of causal loops in a CLD: reinforcing loops and balancing loops.46–48 Reinforcing loops (labelled ‘R’ in models) produce exponential growth and decay patterns, whereas balancing loops (labelled ‘B’ in models) act to stabilise the system (ie, balancing loops are referred to as ‘goal-seeking’ loops). The combined effect of two or more loops in a CLD can create either stable or unstable equilibrium within a complex system. Time delays between system elements can further trigger oscillation and other unpredictable behaviours. Conceptual behaviour over time (BOT) graphs can visualise such patterns.49 Figure 2 presents a ‘fixes that fails’ system archetype structure50 and the associated BOT graph applied to the rural health workforce shortage problem.
Figure 2.
A causal loop diagram (CLD) (left) that theoretically explains the behaviour of the rural health workforce over time (right) framed through the lens of a ‘fixes that fails’ systems archetype.50 Polarity indicators, positive (+) and negative (−), indicate that variables move in the same direction or move in opposite direction, respectively. Reinforcing loops and balancing loops are represented with the notation (R) and (B), respectively. Time delays are shown by two dashed lines. The fixes that fail system archetype in figure 2 explains that the immediate problem of a rural workforce shortage is giving rise to short-term hiring solutions. For example, under a return of service obligation scheme, health professionals may be required to spend a set numbers of years working in rural locations following government/state supported training. While the short-term intervention appears to improve the situation under a narrow time horizon, over the long run, the solution is equally increasing turnover rate within the rural health service sector, making the shortage worse. Political cycles and/or changes to governments may explain the archetypal fixes that fail system structure. Researchers should consider transforming the CLD into a stock and flow diagram (SFD) as a basis to simulate complex system behaviours using system dynamics (SD) modelling.
A CLD is a useful standalone tool for visualising complexity and conceptualising relatively simple behaviours, including how the various parts of a system (eg, agents, factors, processes) interact to explain or create a problem.48 There are very few examples of CLDs applied specifically in rural contexts,33–35 and further applications are warranted. Despite their holistic point of reference, CLDs are still only static representations and conceptual errors and complex behaviours are often only realised when models are translated into a dynamic format, such as SD modelling.
SD modelling is computational method that can be used to explore the structure and dynamics of both simple and complex systems.43 46 51 The method is capable of simulating non-linear behaviours of complex systems over time, primarily using differential equations and related mathematical formulae.30 31 51 SD modelling incorporates the same features from a CLD, such as variables, feedback loops and time delays; however, stocks and flows are also included in the representation to allow for the accumulation and depletion of key elements over time43 (eg, inventory, money, assets, employees—the rural health workforce). SD modelling has the capacity to reveal the complex processes and pathways that give rise to emergent system behaviours at a macro-level. It is a useful complex systems approach for understanding counterintuitive behaviours within complex systems as a basis to identify potential leverage points for health-related interventions and policies. As with ABM, a range of existing data sources can be used to paramterise and calibrate simulations. For example, in terms of Australian rural health, there is a huge research opportunity around using the readily available and comprehensive National Health Workforce Data Tool,52 along with other data sources, to instantiate models and forecast various rural health system behaviours. The reader is directed to two papers using SD modelling, one examining the implementation of clean cooking interventions in rural India,36 and another that compared the demand and supply of Australian radiologists over 40 years under various scenarios (though not exclusively rural focused).37
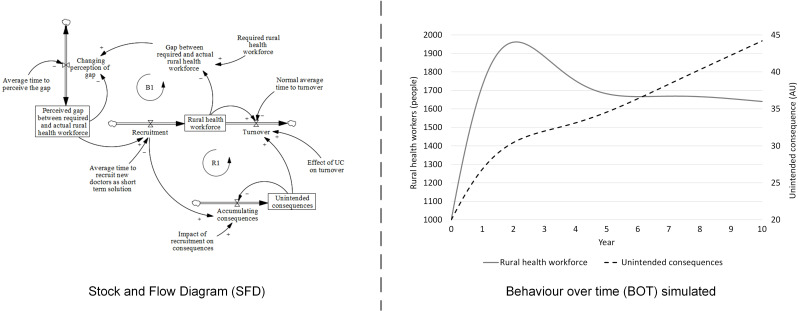
Figure 3 presents a reformulation of the fixes that fail workforce CLD (figure 2), this time as a stock and flow diagram (SFD) to allow for quantitative simulation (Vensim PLE V.9.3.0×64). Figure 3 demonstrates that it is far better to work on identifying and implementing the fundamental solution to the workforce problem than it is to invest in quick fixes to correct the shortage, even if this initially comes at a greater cost to time, expenses and resources. Vensim code provided in online supplemental material 1.
Figure 3.
Stock and flow diagram (SFD) (left) created based on the fixes that fail causal loop diagram (CLD) (figure 2). For the purpose of this article and to demonstrate SFD, the variables ‘Rural health workforce’ and ‘Unintended consequence’ from the initial CLD are hereby represented as ‘stocks’ (square boxes) that can accumulate and drain based on inflows (ie, ‘Recruitment’ and ‘Accumulating consequences’) and outflows (ie, ‘turnover’). To reflect the delay in decision-makers perception of the gap, an additional stock is incorporated, titled ‘Perceived gap between required and actual rural health workforce’. The same balancing and reinforcing loops from the CLD indicate that while the short-term solution is helping to correct the symptomatic problem (ie, balancing loop (B)), it is also part of a greater reinforcing (exponential growth (R)) loop that eventually makes the problem worse due to the effect of the growing unintended consequence. The simulated behaviour over time graph indicates that the short-term hiring solution does indeed initially increase the number of rural health workers. Over time the fix can no longer control the shortage, to the point that the fix actually contributes to it. Loop dominance quickly shifts from the balancing loop to the reinforcing loop. Understanding system behaviour using dynamic systems science approaches is vital for identifying counterintuitive behaviours and identifying optimal system leverage from a cost-benefit standpoint, especially as CLD, SFD and SD models grow in size and complexity.
bmjopen-2022-064646supp001.pdf (44.6KB, pdf)
Methods that are fit for purpose
Complex systems approaches are not intended to act as a replacement for traditional scientific methods well-suited to simpler problems (eg, PICO problems) in the health sciences. The analytical trade-offs associated with both reductionist and complex systems approaches must be acknowledged. To describe these, we refer to the desiderata precision, fit, generality and realism as reported by Ip et al.53
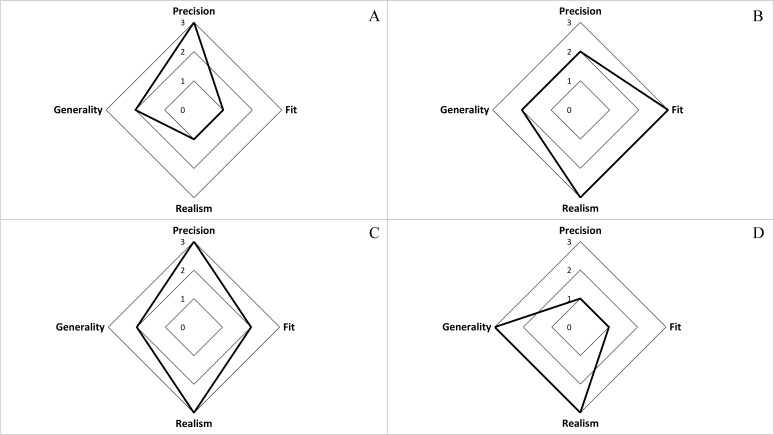
Clinical and epidemiological methods have the advantage of being able to score relatively highly across statistical dimensions of precision and fit, although they equally score lower in measures of generality and realism. The inverse is generally true for complex systems approaches which tend to place a greater reliance on theory relative to data.20 Examples are shown in figure 4.
Figure 4.
The trade-off between the analytical desiderata of precision, fit, realism and generality. The article by Ip et al53 provides an excellent overview of key terms and concepts and enters into greater detail. (A) Simple linear regression analysis; (B) agent-based model (ABM) of estimated disease incidence; (C) system dynamics (SD) model of health service costs to health service utilisation; (D) causal loop diagram (CLD) or a socioecological model of a health system. We note that while four simple examples are shown, there are many different traditional statistical approaches and complex systems approaches, including multiple variations within the approaches themselves, that would produce different results across the four dimensions.
Precision and fit can be thought of as the capacity of a model to produce precise numerical outputs, and to make quantitative predictions based on historical data, respectively.53 Realism on the other hand, explains the accuracy to which a systems model has face validity, describes the world qualitatively, and agrees with expert mental models. Generality is the extent to which a model has external validity across domains.53
An example multi-method complex systems approach
The main point conveyed by figure 4 is that there is a trade-off with respect to all four analytical desiderata.53 Satisfying all four concurrently is not possible via a single application, the outcome of which depends on the research question(s), project goal, use of data and approach. Fortunately, a multi-method complex systems approach could provide a promising way forward in rural health research.
To illustrate, sacrificing precision and fit for generality and realism is not necessarily a detriment if the first phase of a research programme involves mapping all agents and factors from across the ‘rural health system’ that contribute to a health or health system outcome. In this regard, static systems modelling, such as CLDs or socioecological models, could be a useful starting point to conceptualise complexity and generate a rich picture of the problem and the key agents and factors involved as a means to direct subsequent analyses.33–35 The next step in the research programme might involve the use of a ‘top down’ computational method, such as SD modelling, to reveal how non-linear system dynamics and behaviours drive change and shape health outcomes, thereby increasing quantitative precision. The third and final phase may drill down further into key parts of the rural health system via the use of an ABM, to understand the complex processes that give rise to health or health system outcomes, although from a ‘ground up’ perspective that appreciates individual exchanges of information, labour and skill between health professionals and health system managers. This three-step progression from CLD to SD to ABM may act as a simple framework by which rural health researchers can become comfortable and familiar with systems modelling approaches into the future.
The many uses of complex systems approaches
From the above, it is concluded that unlike traditional clinical and epidemiological methods, which are used exclusively to test well-defined and falsifiable a priori causal hypotheses, there are many different reasons to use a complex systems approach.
Static complex systems methods, such as CLDs and socioecological models,2 27 30 33–35 39 47 48 53 can be used to:
Synthesise large amounts of evidence and/or information.
Offer a ‘big picture’ perspective to, for example, support analysis and intervention design.
Illustrate complex causal feedback, theorise system dynamics and identify possible leverage.
Generate new hypotheses and identify gaps in knowledge.
Inform an understanding of the range of factors that contribute to an outcome.
Gain an understanding of the problem ‘envelope’ or system boundary.
Facilitate co-design, participatory and group model-building initiatives.
Computational complex systems methods, such as ABM and SD modelling,1 20 29 32 36 37 41–46 51 53 can be used to:
Explain and forecast the emergence of various patterns and systems phenomena (eg, survival rates, impact of health policies, direction of effect of interventions).
Understand the mechanisms that drive the behaviour of complex systems.
Simulate the dynamics of a problem to observe how factors, structures and systems behave over time.
Conduct multiple in-silico ‘what if’ experiments that otherwise would not be possible in situ (ie, policy comparative analyses).
Towards a complex systems approach in rural health research
Adopting a complex systems approach in rural health research would recognise that real, long-term change within rural communities is only created when systems and processes are redesigned and reconfigured, and not necessarily when a single ‘fix’ or individual-level health intervention is implemented.12 22 The role of subject matter expertise and causal theories explaining health generation in rural settings would play a greater role in complexity science applications relative to a traditional scientific approach.10 20 The triangulation of various sources of data across multiple system levels and from the perspective of various stakeholders would feed into the development of models to enrich understanding of where to intervene in rural health systems.18 25 Involving rural health communities, consumers, service providers, stakeholders and policy-makers in the development of conceptual systems models would provide a sense of ownership and transparency of the model-construction process to ensure that the resulting solutions are endorsed long-term.43
Under a complexity framework, rural health researchers would ask not whether a specific intervention works; but rather, how new or existing solutions could be supported or degraded by the wider system.17 24 When rural health systems are mapped, modelled and understood, it is possible to identify where key leverage points may be and how to best to manipulate them through a multidisciplinary effort.2 18 These points of leverage may be found across all levels of the complex rural health system; however, further interrogation of the outputs would expose optimal targets for interventions and solutions given limited resources and competing priorities. To achieve this, the use of static and computational methods from the complexity sciences, such as CLD,35 48 SD modelling23 43 and ABM32 41 42 can be used to conceptualise and simulate the non-linear behaviours of complex rural health systems. Doing so will offer original data and evidence to complement traditional forms of scientific inquiry to translate effective new rural health interventions and policies. Indeed, a particularly important issue in rural health that systems methods could be applied to includes the widespread maldistribution, dispersion and shortage of medical and allied health professionals.8 9 Understanding the complex interrelationships between various system wide factors that are driving this problem with the aim of identifying optimal systemic leverage given the presence of counterintuitive behaviour is a major future research opportunity for the systems-based (computational) modelling community.
The field of implementation science has become important in marrying the outcomes of complex systems thinking and real-world objectives for better health outcomes.18 24 25 Implementation science, which is increasingly integrating realist evaluation theories,24 has seen a tremendous uptake in the application of complex systems approaches as it allows a better understanding of what works, for whom, when and why.17 18 25 The integration of complexity science, implementation science and realist evaluation frameworks is also an encouraging future direction for rural health research.
Closing remarks
Rural health researchers are encouraged to consider how adopting a complex systems approach could provide a new spark in a field that desperately requires scientific innovation and complementary methods. By taking a systems thinking perspective, rural health researchers can begin to explore, model and understand the myriad of factors and interactions that contribute to health outcomes and health system issues at scale, both within and between different rural communities. The qualitative and quantitative systems modelling methods described in this article will be highly useful should they find their way into the rural health researcher’s methodological and analytical toolkit—though the appropriate training and learning elements are to precede novel applications to ensure best practice principles are adhered to. The present authors welcome this challenge and embrace the possibilities that are derived from adopting new ways of thinking about, and scientifically approaching, rural health issues.
Supplementary Material
Acknowledgments
We thank Bahram Sangelaji, Clara Walker, and Tony Fallon at Southern Queensland Rural Health (SQRH) for their readiness to engage in interesting discussion around how to enhance the quality of life for our rural communities through methodological innovation.
Footnotes
Twitter: @system_complex, @DrJ_Thompson, @ArgusGeoff
Contributors: All authors contributed to the content in accordance with the ICMJE guidelines for authorship. AH contributed to conceptualisation, writing–initial draft; reviewing and editing. JT, AB and GA contributed to writing, reviewing, editing and refining figures and models.
Funding: This research received no external funding or sponsorship. Three memebers of the author team who completed this work (AH, JT, GA) are employed under the Australian government’s Rural Health Multidisciplinary Training (RHMT) program. Award/Grant number is not applicable.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics approval
Not applicable.
References
- 1.Luke DA, Stamatakis KA. Systems science methods in public health: dynamics, networks, and agents. Annu Rev Public Health 2012;33:357–76. 10.1146/annurev-publhealth-031210-101222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meadows DH. Thinking in systems: a primer. London: Earthscan, 2009. [Google Scholar]
- 3.Barclay L, Phillips A, Lyle D. Rural and remote health research: does the investment match the need? Aust J Rural Health 2018;26:74–9. 10.1111/ajr.12429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lyle D, Greenhill J. Two decades of building capacity in rural health education, training and research in Australia: University departments of rural health and rural clinical schools. Aust J Rural Health 2018;26:314–22. 10.1111/ajr.12470 [DOI] [PubMed] [Google Scholar]
- 5.Wilson CR, Rourke J, Oandasan IF, et al. Progress made on access to rural health care in Canada. Canadian Family Physician 2020;66:31. [Google Scholar]
- 6.Schopfer DW. Rural health disparities in chronic heart disease. Prev Med 2021;152:106782. 10.1016/j.ypmed.2021.106782 [DOI] [PubMed] [Google Scholar]
- 7.Harrington RA, Califf RM, Balamurugan A, et al. Call to action: rural health: a presidential advisory from the American heart association and American stroke association. Circulation 2020;141:e615–44. 10.1161/CIR.0000000000000753 [DOI] [PubMed] [Google Scholar]
- 8.Iglehart JK. The challenging quest to improve rural health care. N Engl J Med 2018;378:473–9. 10.1056/NEJMhpr1707176 [DOI] [PubMed] [Google Scholar]
- 9.AIHW . Rural and remote health. Canberra: AIHW, 2020. [Google Scholar]
- 10.Galea S, Riddle M, Kaplan GA. Causal thinking and complex system approaches in epidemiology. Int J Epidemiol 2010;39:97–106. 10.1093/ije/dyp296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vandenbroucke JP, Broadbent A, Pearce N. Causality and causal inference in epidemiology: the need for a pluralistic approach. Int J Epidemiol 2016;45:1776–86. 10.1093/ije/dyv341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rutter H, Savona N, Glonti K, et al. The need for a complex systems model of evidence for public health. Lancet 2017;390:2602–4. 10.1016/S0140-6736(17)31267-9 [DOI] [PubMed] [Google Scholar]
- 13.Glass TA, Goodman SN, Hernán MA, et al. Causal inference in public health. Annu Rev Public Health 2013;34:61–75. 10.1146/annurev-publhealth-031811-124606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keyes K, Galea S. What matters most: quantifying an epidemiology of consequence. Ann Epidemiol 2015;25:305–11. 10.1016/j.annepidem.2015.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galea S, Keyes KM. What matters, when, for whom? Three questions to guide population health scholarship. Inj Prev 2018;24:i3–6. 10.1136/injuryprev-2017-042415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diez Roux AV. Complex systems thinking and current impasses in health disparities research. Am J Public Health 2011;101:1627–34. 10.2105/AJPH.2011.300149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zamboni K, Schellenberg J, Hanson C, et al. Assessing scalability of an intervention: why, how and who? Health Policy Plan 2019;34:544–52. 10.1093/heapol/czz068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koorts H, Rutter H. A systems approach to scale-up for population health improvement. Health Res Policy Syst 2021;19:27. 10.1186/s12961-021-00679-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diez Roux AV. Integrating social and biologic factors in health research: a systems view. Ann Epidemiol 2007;17:569–74. 10.1016/j.annepidem.2007.03.001 [DOI] [PubMed] [Google Scholar]
- 20.Hernán MA. Invited commentary: agent-based models for causal inference—reweighting data and theory in epidemiology. Am J Epidemiol 2015;181:103–5. 10.1093/aje/kwu272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kouser HN, Barnard-Mayers R, Murray E. Complex systems models for causal inference in social epidemiology. J Epidemiol Community Health 2020. doi: 10.1136/jech-2019-213052. [Epub ahead of print: 10 Nov 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crane M, Nathan N, McKay H, et al. Understanding the sustainment of population health programmes from a whole-of-system approach. Health Res Policy Syst 2022;20:37. 10.1186/s12961-022-00843-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carey G, Malbon E, Carey N, et al. Systems science and systems thinking for public health: a systematic review of the field. BMJ Open 2015;5:e009002. 10.1136/bmjopen-2015-009002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGill E, Er V, Penney T, et al. Evaluation of public health interventions from a complex systems perspective: a research methods review. Soc Sci Med 2021;272:113697. 10.1016/j.socscimed.2021.113697 [DOI] [PubMed] [Google Scholar]
- 25.Northridge ME, Metcalf SS. Enhancing implementation science by applying best principles of systems science. Health Res Policy Syst 2016;14:74. 10.1186/s12961-016-0146-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trochim WM, Cabrera DA, Milstein B, et al. Practical challenges of systems thinking and modeling in public health. Am J Public Health 2006;96:538–46. 10.2105/AJPH.2005.066001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kiekens A, Dierckx de Casterlé B, Vandamme A-M. Qualitative systems mapping for complex public health problems: a practical guide. PLoS One 2022;17:e0264463. 10.1371/journal.pone.0264463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ottino JM. Complex systems. AIChE J 2003;49:292–9. 10.1002/aic.690490202 [DOI] [Google Scholar]
- 29.Marshall BDL, Paczkowski MM, Seemann L, et al. A complex systems approach to evaluate HIV prevention in metropolitan areas: preliminary implications for combination intervention strategies. PLoS One 2012;7:e44833. 10.1371/journal.pone.0044833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hulme A, Mclean S, Salmon PM, et al. Computational methods to model complex systems in sports injury research: agent-based modelling (ABM) and systems dynamics (SD) modelling. Br J Sports Med 2019;53:1507. 10.1136/bjsports-2018-100098 [DOI] [PubMed] [Google Scholar]
- 31.Hulme A, Thompson J, Nielsen RO, et al. Using computational modelling for sports injury prevention: Agent-Based modelling and system dynamics modelling. Human Factors and Ergonomics in Sport: CRC Press, 2020: 323–44. [Google Scholar]
- 32.Hulme A, Thompson J, Nielsen RO, et al. Towards a complex systems approach in sports injury research: simulating running-related injury development with agent-based modelling. Br J Sports Med 2019;53:560. 10.1136/bjsports-2017-098871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Allender S, Owen B, Kuhlberg J, et al. A community based systems diagram of obesity causes. PLoS One 2015;10:e0129683. 10.1371/journal.pone.0129683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keane P, Ortega A, Linville J. Healthy kids, healthy Cuba: findings from a group model building process in the rural Southwest. J Public Health Manag Pract 2015;21 Suppl 3:S70–3. 10.1097/PHH.0000000000000250 [DOI] [PubMed] [Google Scholar]
- 35.Bolton KA, Fraser P, Lowe J, et al. Generating change through collective impact and systems science for childhood obesity prevention: the GenR8 change case study. PLoS One 2022;17:e0266654. 10.1371/journal.pone.0266654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chalise N, Kumar P, Priyadarshini P, et al. Dynamics of sustained use and abandonment of clean cooking systems: lessons from rural India. Environ Res Lett 2018;13:035010. 10.1088/1748-9326/aab0af [DOI] [Google Scholar]
- 37.Taba ST, Atkinson SR, Lewis S, et al. A systems life cycle approach to managing the radiology profession: an Australian perspective. Aust Health Rev 2015;39:228–39. 10.1071/AH14113 [DOI] [PubMed] [Google Scholar]
- 38.Salmon PM, McLean S. Complexity in the beautiful game: implications for football research and practice. Sci Med Footb 2020;4:162–7. 10.1080/24733938.2019.1699247 [DOI] [Google Scholar]
- 39.Hulme A, McLean S, Salmon PM. Sport as a complex socio-technical system. Human Factors and Ergonomics in Sport: CRC Press, 2020: 21–40. [Google Scholar]
- 40.Castellani BG L. Map of the complexity sciences: art and science factory, LLC., 2021. Available: https://www.art-sciencefactory.com/complexity-map_feb09.html
- 41.Tracy M, Cerdá M, Keyes KM. Agent-based modeling in public health: current applications and future directions. Annu Rev Public Health 2018;39:77. 10.1146/annurev-publhealth-040617-014317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nianogo RA, Arah OA. Agent-based modeling of noncommunicable diseases: a systematic review. Am J Public Health 2015;105:e20–31. 10.2105/AJPH.2014.302426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Darabi N, Hosseinichimeh N. System dynamics modeling in health and medicine: a systematic literature review. Syst Dyn Rev 2020;36:29–73. 10.1002/sdr.1646 [DOI] [Google Scholar]
- 44.Calder M, Craig C, Culley D, et al. Computational modelling for decision-making: where, why, what, who and how. R Soc Open Sci 2018;5:172096. 10.1098/rsos.172096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rand W, Rust RT. Agent-based modeling in marketing: guidelines for rigor. Int J Res Mark 2011;28:181–93. 10.1016/j.ijresmar.2011.04.002 [DOI] [Google Scholar]
- 46.Forrester JW. Industrial dynamics. J Oper Res Soc 1997;48:1037–41. 10.1057/palgrave.jors.2600946 [DOI] [Google Scholar]
- 47.Senge PM. The fifth discipline: the art and practice of the learning organization: currency, 2006. [Google Scholar]
- 48.Baugh Littlejohns L, Hill C, Neudorf C. Diverse approaches to creating and using causal loop diagrams in public health research: recommendations from a scoping review. Public Health Rev 2021;42:1604352. 10.3389/phrs.2021.1604352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Calancie L, Anderson S, Branscomb J, et al. Using behavior over time graphs to spur systems thinking among public health practitioners. Prev Chronic Dis 2018;15:E16. 10.5888/pcd15.170254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim D. Systems archetypes II: using systems archetypes to take effective action. 2. Waltham, MA: Pegasus Communications, 1994. [Google Scholar]
- 51.Sterman JD. Learning from evidence in a complex world. Am J Public Health 2006;96:505–14. 10.2105/AJPH.2005.066043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.The Department of Health and Aging . Data tool: Australian government, 2022. Available: https://hwd.health.gov.au/datatool/
- 53.Ip EH, Rahmandad H, Shoham DA, et al. Reconciling statistical and systems science approaches to public health. Health Educ Behav 2013;40:123s–31. 10.1177/1090198113493911 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-064646supp001.pdf (44.6KB, pdf)