FOR RELATED ARTICLE, SEE PAGE 782
Prone positioning has been recommended for patients with moderate-to-severe ARDS who receive mechanical ventilation well before the appearance of the novel COVID-19.1 It improves survival, possibly by reopening or “recruiting” the dorsal nonaerated lung tissue and diminishing ventral hyperinflation. As a result, aeration becomes distributed more evenly, alveolar deformation (strain) and tension (stress) are smaller, and mechanical ventilation is safer than in the supine position.2 Reducing the harms of mechanical ventilation is the strongest rationale for prone positioning in ARDS; increasing arterial oxygenation is less important, except for the unusual case of life-threatening hypoxemia.2 Prone positioning of patients who receive mechanical ventilation carries some risks, including endotracheal tube obstruction or displacement (up to accidental extubation), reduced venous return, need for more sedation, vomiting, loss of venous access, and pressure sores.2 The advantages of prone positioning are more likely to outweigh these dangers in moderate-to-severe ARDS when pulmonary edema is severe enough to increase the risk of secondary lung damage.3 In a study on 100 healthy subjects, the lung weight was 929 ± 188 g; the amount of nonaerated tissue was 7% ± 4%, and the lung gas volume was 4,066 ± 1,190 mL.4 By contrast, in 94 patients with moderate-to-severe ARDS who were studied with 5 cm H2O of positive end-expiratory pressure, the median (quartile 1 to quartile 3) lung weight was 1,567 g (1,363 to 1,991 g), the amount of nonaerated tissue was 50% (38% to 62%), and the lung gas volume was 859 mL (537 to 1,257 mL).5 If changes in lung weight and aeration are less pronounced, as in mild ARDS, then the rationale for prone positioning will be weaker, and the benefit smaller or nil.3
Soon after the appearance of COVID-19, prone positioning started to be used widely in patients with related moderate-to-severe ARDS who required invasive mechanical ventilation.6 We are now beginning to understand that prone positioning decreases alveolar collapse and hyperinflation, making lung aeration distribution more homogeneous, even in these patients.7 Therefore, prone positioning may also be beneficial in moderate-to-severe ARDS that is related to COVID-19, but the quality of evidence remains very low.
Moreover, (awake) prone positioning was used in patients with different degrees of hypoxemia who were not intubated. A collaborative meta-analysis of six randomized controlled trials on 1,126 patients who were treated with high-flow nasal cannula found a lower risk of endotracheal intubation but a similar risk of death with awake-prone positioning.8 Diversely, six other randomized controlled trials on 432 patients on conventional respiratory support (ie, oxygen delivered via the nasal cannula or a face mask) were all negative.9
In this issue of the CHEST, Rampon et al10 present the results of a multicenter trial that randomly assigned adults with non-severe COVID-19 in the ED or medical ward to receive a recommendation on their smartphone to lie in bed in a prone position or their preferred position. The primary outcome was worsening of respiratory failure, defined as a need for more oxygen or transfer to the ICU.
The trial was stopped early for slow enrollment. A total of 3,128 patients were screened; 305 patients were assigned randomly, and 293 patients received a recommendation on their smartphone to lie prone (n = 159) or in their preferred position (n = 134) until hospital discharge. Results can be summarized in the following manner: (1) 99 of 159 patients (62%) and 83 of 134 patients (62%) accessed the recommendation on their smartphone; (2) 50 of 159 patients (31%) and 41 of 134 patients (31%) reported lying in the prone position at least once, usually for a few hours; and (3) 32 of 159 patients (20%) and 31 of 134 patients (23%) experienced the primary outcome. None of these results significantly differed between the two groups. Therefore, encouraging patients to lie prone did not improve outcome.
Patients enrolled in the trial had non-severe COVID-19. According to inclusion criteria, they required no oxygen (140 of 293 patients; 48%) or < 6 L/min of oxygen (the others). Oxygen saturation to Fio 2 was 396 (306 to 378). Respiratory rate was 18 beats/min (18 to 20 beats/min). Seventy-nine of 293 patients (27%) had neither opacities nor infiltrates on their chest radiogram. Six of 293 patients (2%) were admitted to the ICU. Hospital stay was, on average, 3 to 4 days. Hospital mortality rate was 1% (four of 293 patients).
The authors must be applauded for running such a complex study during the pandemic. Using a smartphone is appealing because it facilitates rapid enrollment and intervention delivery while allowing social distancing and conserving personal protective equipment. Even so, it failed to improve adherence to prone positioning. Repeated encouragement by bedside physicians may be more effective.9 However, one key question remains: should we encourage prone positioning in patients with non-severe COVID-19? How strong is the rationale for doing it?
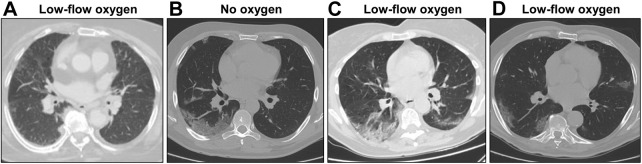
If the requisites for a positive response are always the same, then prone positioning will benefit patients who are not intubated provided their lung weight and aeration are markedly altered. To address this issue, we reviewed the chest CT examinations of 112 patients with COVID-19 who had been treated with no or < 6 L/min of oxygen, as in the study by Rampon et al,10 and who had been included originally in another study conducted at our institution.11 With the use of quantitative analysis,12 their total lung weight was 1,037 g (866 to 1,143 g); the amount of the non-aerated tissue was 8% (6 to 10%), and the lung gas volume was 3,470 mL (2,304 to 4,214 mL). These values are much more similar to those of healthy subjects4 than those of patients who receive mechanical ventilation with moderate-to-severe ARDS.5 In line with these findings, the chest CT scans of patients with non-severe COVID-19 can look quite normal (Fig 1 ). Therefore, patients with non-severe COVID-19 may lack the requisites for a positive response to prone positioning.
Figure 1.
A-D, Lung morphologic images in patients with non-severe COVID-19. Representative CT scans of four patients with COVID-19 who were treated with no oxygen or < 6 L/min of oxygen. All images were obtained at full inspiration. A, Low-flow oxygen (lung weight: 1,079 g); B, no oxygen (lung weight: 1,204 g); C, low-flow oxygen (lung weight: 1,024 g); D, low-flow oxygen (lung weight: 1,109 g).
In conclusion, encouraging patients with non-severe COVID-19 to lie prone while in bed did not improve outcome. This result may reflect low adherence to the recommended intervention. Alternatively, it may indicate that patients with non-severe COVID-19 are bad candidates for prone positioning: their lung injury may be too mild for a positive response. If so, interventions aimed at increasing adherence to prone positioning in this population may prove less beneficial than expected, even when effective.
Acknowledgments
Financial/nonfinancial disclosures: None declared.
References
- 1.Fan E., Del Sorbo L., Goligher E.C., et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 2.Guérin C., Albert R.K., Beitler J., et al. Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med. 2020;46(12):2385–2396. doi: 10.1007/s00134-020-06306-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gattinoni L., Protti A. Ventilation in the prone position: for some but not for all? CMAJ. 2008;178(9):1174–1176. doi: 10.1503/cmaj.080359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cressoni M., Gallazzi E., Chiurazzi C., et al. Limits of normality of quantitative thoracic CT analysis. Crit Care. 2013;17(3):R93. doi: 10.1186/cc12738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coppola S., Froio S., Marino A., et al. Respiratory mechanics, lung recruitability, and gas exchange in pulmonary and extrapulmonary acute respiratory distress syndrome. Crit Care Med. 2019;47(6):792–799. doi: 10.1097/CCM.0000000000003715. [DOI] [PubMed] [Google Scholar]
- 6.Langer T., Brioni M., Guzzardella A., et al. Prone position in intubated, mechanically ventilated patients with COVID-19: a multi-centric study of more than 1000 patients. Crit Care. 2021;25(1):128. doi: 10.1186/s13054-021-03552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Protti A., Santini A., Pennati F., et al. Lung response to prone positioning in mechanically-ventilated patients with COVID-19. Crit Care. 2022;26(1):127. doi: 10.1186/s13054-022-03996-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ehrmann S., Li J., Ibarra-Estrada M., et al. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med. 2021;9(12):1387–1395. doi: 10.1016/S2213-2600(21)00356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li J., Luo J., Pavlov I., et al. Awake prone positioning for non-intubated patients with COVID-19-related acute hypoxaemic respiratory failure: a systematic review and meta-analysis. Lancet Respir Med. 2022;10(6):573–583. doi: 10.1016/S2213-2600(22)00043-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rampon G., Jia S., Agrawal R., et al. Smartphone-guided self-prone positioning vs usual care in nonintubated hospital ward patients with COVID-19: a pragmatic randomized clinical trial. Chest. 2022;162(4):782–791. doi: 10.1016/j.chest.2022.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lanza E., Muglia R., Bolengo I., et al. Quantitative chest CT analysis in COVID-19 to predict the need for oxygenation support and intubation. Eur Radiol. 2020;30(12):6770–6778. doi: 10.1007/s00330-020-07013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Protti A., Santini A., Pennati F., et al. Lung response to a higher positive end-expiratory pressure in mechanically ventilated patients with COVID-19. Chest. 2022;161(4):979–988. doi: 10.1016/j.chest.2021.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]