ABSTRACT
Background
Economic evaluations of nutrition-sensitive agriculture (NSA) interventions are scarce, limiting assessment of their potential affordability and scalability.
Objectives
We conducted cost–consequence analyses of 3 participatory video-based interventions of fortnightly women's group meetings using the following platforms: 1) NSA videos; 2) NSA and nutrition-specific videos; or 3) NSA videos with a nutrition-specific participatory learning and action (PLA) cycle.
Methods
Interventions were tested in a 32-mo, 4-arm cluster-randomized controlled trial, Upscaling Participatory Action and Videos for Agriculture and Nutrition (UPAVAN) in the Keonjhar district, Odisha, India. Impacts were evaluated in children aged 0–23 mo and their mothers. We estimated program costs using data collected prospectively from expenditure records of implementing and technical partners and societal costs using expenditure assessment data collected from households with a child aged 0–23 mo and key informant interviews. Costs were adjusted for inflation, discounted, and converted to 2019 US$.
Results
Total program costs of each intervention ranged from US$272,121 to US$386,907. Program costs per pregnant woman or mother of a child aged 0–23 mo were US$62 for NSA videos, US$84 for NSA and nutrition-specific videos, and US$78 for NSA videos with PLA (societal costs: US$125, US$143, and US$122, respectively). Substantial shares of total costs were attributable to development and delivery of the videos and PLA (52–69%) and quality assurance (25–41%). Relative to control, minimum dietary diversity was higher in the children who underwent the interventions incorporating nutrition-specific videos and PLA (adjusted RRs: 1.19 and 1.27; 95% CIs: 1.03–1.37 and 1.11, 1.46, respectively). Relative to control, minimum dietary diversity in mothers was higher in those who underwent NSA video (1.21 [1.01, 1.45]) and NSA with PLA (1.30 [1.10, 1.53]) interventions.
Conclusion
NSA videos with PLA can increase both maternal and child dietary diversity and have the lowest cost per unit increase in diet diversity. Building on investments made in developing UPAVAN, cost-efficiency at scale could be increased with less intensive monitoring, reduced startup costs, and integration within existing government programs. This trial was registered at clinicaltrials.gov as ISRCTN65922679.
Keywords: Nutrition-sensitive agriculture, Cost–consequence analysis, Participatory learning and action, Women's groups, Dietary diversity, Maternal and child nutrition, India
Background
There is strong evidence on the impacts and cost-effectiveness of nutrition-specific interventions (1–4), particularly in settings with high undernutrition burdens, such as India. However, to achieve the Sustainable Development Goal (SDG) targets (5) to end hunger and undernutrition (SDG 2), multisectoral approaches are needed to address the underlying causes of undernutrition (6). In rural areas of low- and middle-income countries, where the burden of undernutrition is highest and smallholder farming provides a major source of nutrition and income (7), the agriculture sector could provide “nutrition-sensitive” interventions that improve both nutrition and agriculture outcomes simultaneously..
Trials of nutrition-sensitive agriculture (NSA) interventions have shown that these interventions may improve dietary outcomes, with results suggesting that the implementation of these interventions at scale may be a policy option. Of the 8 trials that tested the effects of NSA interventions on minimum dietary diversity of children, 4 trials showed a significant increase, although neither of the 2 NSA trials measuring impacts on maternal dietary diversity showed an effect (8). However, our ability to recommend upscaling of NSA interventions is constrained by a lack of data on their costs, and therefore a lack of evidence regarding their value for money (6, 9, 10). So far, the few economic evaluations (the family of evaluation types that relate costs and impacts) of NSA interventions that do exist come from sub-Saharan Africa (10–12)—none come from South Asia (13, 14). Policymakers need this evidence to prioritize and justify their investments, particularly in resource-constrained settings in South Asia. Additionally, economic evaluations may be more needed for multisectoral interventions such as NSA, to garner support from the multiple (traditionally separate) sectors involved and justify the efforts required to enable collaboration (15).
One reason for the lack of NSA economic evaluations is that traditional methods developed for single-sector interventions are unsuitable for multisectoral interventions. Cost–benefit analyses (which give cost per economic value of aggregate benefits) rely on too many assumptions to compute the economic value of dietary and agricultural outcomes. Cost-effectiveness analyses (which estimate costs per natural unit of an outcome or a composite health measure) give misleadingly high estimates (16). For interventions designed to affect a range of health and non-health outcomes, assigning all intervention costs to a single outcome creates an erroneous impression that the cost per unit of improvement is prohibitively high. Cost–consequence analyses (where outcomes are reported alongside disaggregated costs) offer a transparent approach that allows policymakers to weigh the evidence for themselves. Cost–consequence analyses are recommended for multisectoral interventions with multiple health and nonhealth effects (17, 18), ideally alongside cost-effectiveness analysis.
Here, we present the economic evaluation results of the UPAVAN trial, conducted in Odisha state, India, between 2016 and 2020 (8, 19). The trial aimed to test the nutritional and agricultural impacts of 3 video-based participatory NSA interventions, each compared with a control arm. The specific objectives of the economic evaluations of the UPAVAN study were the following: 1) describe intervention coverage and participation; 2) estimate the program cost and cost efficiency (cost per participant) of implementing the interventions; 3) estimate societal costs of the interventions; 4) conduct a cost–consequence analysis to present the costs alongside the effects of the interventions and estimate cost per unit increase in outcome per intervention; 5) examine effects of uncertain parameters, assumptions, and potential scenarios on intervention costs;, and 6) estimate the cost of delivering the interventions at scale and affordability of scale-up across rural Odisha.
Methods
Overview of the UPAVAN trial study design
Detailed descriptions of the UPAVAN interventions, study design, and impacts are reported elsewhere (8, 19, 20). In brief, the UPAVAN trial was a 4-arm, cluster randomized controlled trial, implemented in 4 administrative blocks (Patna, Keonjhar Sadar, Harichandanpur, and Ghatgaon) in the Keonjhar district, Odisha, India. One or 2 villages and surrounding hamlets were defined as a cluster, to ensure a minimum population of 800 per cluster. Stratified block random assignment was used to allocate 148 clusters to 4 trial arms (3 intervention arms and 1 control arm), giving 37 clusters per arm. Allocation of the clusters was stratified by distance to the nearest town (<10 km or ≥10 km) and the proportion of Scheduled Tribe or Scheduled Caste [historically disadvantaged households: low: 30%, medium: 30–70%; high : >70%] (8, 19), giving 6 strata in total.
Both cluster and individual-level informed consent were obtained for participation in the trial and surveys. Ethics approval for the trial was obtained from the Odisha government's Institutional Review Board, Research and Ethics Committee, Department of Health and Family Welfare, Government of Odisha, and the LSHTM Interventions Research Ethics Committee.
Study setting
The Keonjhar district has an estimated population of 1.8 million residents, 86% of whom reside in a rural setting (21). Of this population, 44% belonged to the Scheduled Tribes and 12% to Scheduled Castes (21)—historically the most disadvantaged socioeconomic groups in India. The prevalence of maternal and child undernutrition in Keonjhar is among the highest in India. In Keonjhar during 2015–2016, 30% of women (age 15–49 y) were underweight and 40% were anemic (13), and of children aged <5 y, >40% were stunted and 19% were wasted (13).
UPAVAN interventions
Interventions were implemented by the Voluntary Association for Rural Reconstruction and Appropriate Technology (VARRAT), a nongovernmental organization in Odisha, with technical support from Digital Green, Ekjut, John Snow Inc. Research and Training Institute (JSI RTI), London School of Hygiene & Tropical Medicine (LSHTM), and University College London (UCL). The trial was evaluated by LSHTM, UCL, and DCOR Consulting Pvt. Ltd.
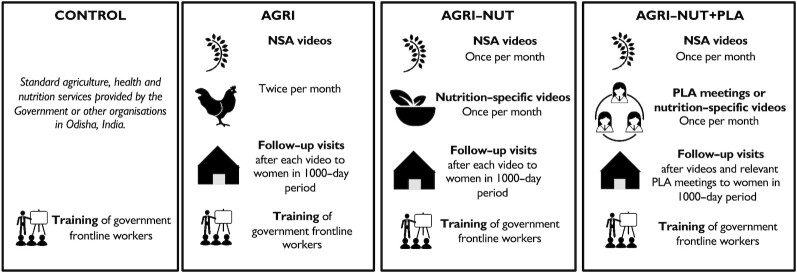
The 3 UPAVAN interventions have been described in detail elsewhere (19, 20) and are briefly described here, with an overview in Figure 1. Each intervention included 2 main components: a fortnightly women's group meeting (the content of which varied between interventions) and a follow-up home visit to each group member after each meeting. The interventions worked with women's self-help groups (SHGs)—an existing platform involved in savings and credit activities. The interventions were implemented for 32 mo, from March 2017 to October 2019.
FIGURE 1.
Overview of components delivered across UPAVAN interventions and control arms, adapted with permission from Kadiyala et al. (2018) (19). AGRI, Nutrition-sensitive agriculture intervention; AGRI-NUT, Nutrition-sensitive and nutrition-specific agriculture intervention; AGRI-NUT + PLA, Nutrition-sensitive and nutrition-specific agriculture intervention using the Participatory Learning and Action approach; PLA, Participatory Learning and Action; UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition.
Nutrition-sensitive agriculture intervention (AGRI)
In this arm, fortnightly women's groups viewed and discussed NSA videos, following a participatory video approach designed by Digital Green (22). The participatory video approach had 4 steps: 1) local implementers identified relevant NSA practices to include in videos, 2) local videographers filmed farmers and other community members demonstrating or discussing the practices, 3) local facilitators screened the videos in group meetings and facilitated discussions, and 4) facilitators conducted follow-up home visits to pregnant women and mothers of children aged 0–23 mo who participated in the group meetings. NSA videos covered the main themes, following UPAVAN's theory of change (5, 19), of increasing production and diversity of nutritious or income-generating foods, increasing women's decision-making power in agricultural activities, and reducing workloads for pregnant and breastfeeding women.
Quality assurance and monitoring were embedded in the participatory video process. Facilitators kept registers to track attendance, whether participants were pregnant or had a child aged 0–23 mo, and whether a government frontline health and nutrition care provider attended the meeting. During home visits, facilitators completed forms to record participants adoption and/or recall of practices promoted in the previous meeting.
Nutrition-sensitive and nutrition-specific agriculture intervention (AGRIAGRI-NUT)
This arm used the same participatory video approach as in the AGRI arm, but videos covered both NSA and nutrition-specific topics. The AGRI-NUT group videos received were half NSA videos shown in the AGRI arm and half nutrition-specific videos covering topics on infant and young-child feeding practices and maternal diets.
AGRI-NUT + Participatory Learning and Action
This arm used the same participatory video approach as in the AGRI arm but integrated nutrition-specific meetings that followed a Participatory Learning and Action (PLA) approach (using half the NSA videos shown in the AGRI arm and half PLA meetings). In the PLA meetings, the groups followed a 4-phase PLA cycle in which they performed the following tasks: 1) learned about and prioritized nutrition problems; 2) discussed and prioritized the causes, effects, and locally feasible strategies to address these problems within their groups and the wider community; 3) implemented the identified strategies; and 4) informally evaluated the results of their actions and made future plans. The PLA meetings were either interactive discussions without videos (using participatory techniques such as voting, storytelling, and games), or participatory videos on nutrition-specific topics that were developed as part of the PLA process. Therefore, the nutrition-specific videos in the PLA arm were different from those in the AGRI-NUT arm.
Control
Those in the control arm (and intervention arms) received standard government services. In addition, the government frontline health and nutrition workers in all 4 arms received 2 d of training on maternal, infant, and young child nutrition.
Evaluating coverage and participation
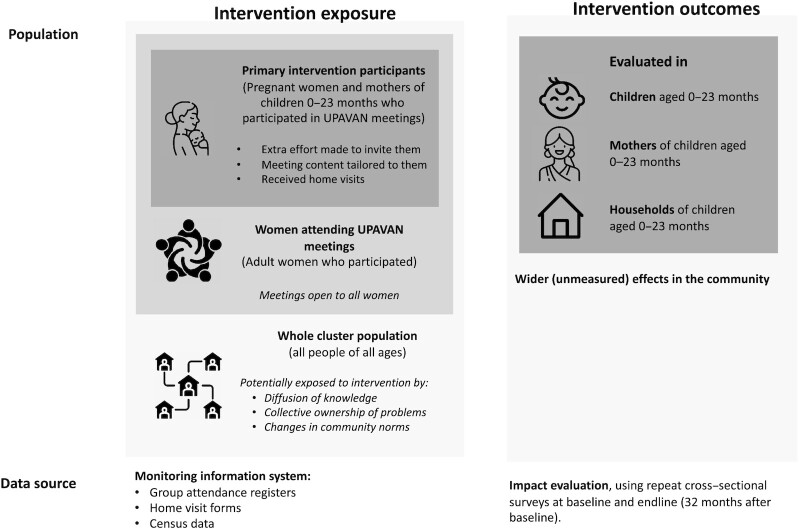
Figure 2 describes the populations aimed for inclusion according to the interventions (intervention exposure) and benefit (intervention outcomes).
FIGURE 2.
Target populations of UPAVAN interventions. UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition.
The UPAVAN interventions were primarily designed to include pregnant women and mothers of children aged 0–23 mo (primary intervention participants) and to benefit children aged 0–23 mo, their mothers, and their households. Therefore, we primarily report coverage and cost-efficiency in terms of the former, and impacts (described in the next section) on the latter.
Coverage was assessed as whether or not primary intervention participants attended ≥1 group meeting and received ≥1 home visit, based on monitoring data recorded by group facilitators (registered with records on 46,327 meetings and forms on 149,585 home visits). We also assessed coverage in terms of all participating women, defined as women of any age who attended ≥1 group meeting according to group registers, because all women of all ages in the intervention clusters were eligible to participate in UPAVAN interventions, and the SHG platform that UPAVAN worked with includes women of all ages.
Participation is given as: total group meetings and home visits attended by primary intervention participants; group meetings attended by all women; and total “points of contact,” the sum of group meeting attendance (all women) and home visits.
Evaluating consequences (trial impacts)
We had 2 primary outcomes. The first outcome was child dietary diversity, measured as the percentage of children aged 6–23 mo consuming ≥4 of 7 food groups in the previous 24 h, using the WHO-defined food groups (23). The second primary outcome was BMI (measured as kg/m2) of nonpregnant, nonpostpartum (gave birth >42 d previously) mothers of these children. Secondary outcomes were maternal dietary diversity, measured as percentage of mothers consuming ≥5 of 10 food groups in the previous 24 h using FAO-defined food groups (24), and percentage of children with a weight-for-height -score <–2 SD of the WHO growth standards median (25). The trial was powered for the 2 primary outcomes to give a target sample size of 4736 mother–child pairs (1184 per arm) at baseline and again at endline. Other outcomes on health, women's empowerment, food security, and agricultural production were prespecified and are given in Supplemental Material Table S1.
The impact of the interventions was evaluated on children aged 0–23 mo and their mothers (and their households for household-level indicators). The impact evaluation used randomly selected samples of eligible households from each cluster at baseline and endline. Households were eligible if they contained a child aged 0–23 mo with no disability affecting anthropometric measurements, and the child's primary caregiver had no disability impairing their participation in the surveys and had been resident in the household for at least half a year before data collection.
Impacts were analyzed using intention-to-treat analysis. The analyses were cross-sectional, assessing outcomes in each intervention arm compared with the control arm at endline. The analyses adjusted for baseline measures by including all individuals at each timepoint linked by cluster, and outcomes were analyzed using separate generalized estimating equations to account for clustering. Adjusted analyses also included distance to the nearest town and proportion of Scheduled Tribe or Scheduled Caste households as covariates.
Results of the UPAVAN impact evaluation are reported elsewhere (8). In this paper, we have presented adjusted effects on all prespecified outcomes that were statistically significant from control; these comprise the “consequences” in our cost–consequence analysis.
Evaluating costs
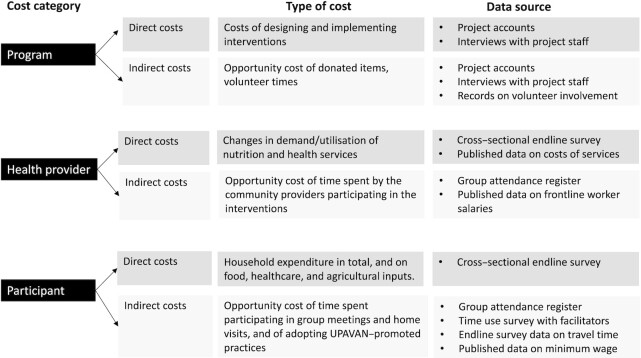
The full cost methodology is presented in the economic evaluation protocol (26) and is summarized in this section and Figure 3.
FIGURE 3.
Conceptual framework for cost analysis of UPAVAN interventions, adapted with permission from Haghparast-Bidgoli et al. (2019) (26).
Economic costs of the interventions were estimated from a program perspective (i.e., costs incurred by the implementing agencies) and a societal perspective (i.e., costs to program implementers, the government health system, and program participants). Economic costs refer to direct financial costs plus indirect costs such as value of donated items or time (opportunity) costs of participating. All direct and indirect cost types, including program and societal costs, as well as the data sources and assumptions used for calculating costs, are given in Supplemental Material Table S2.
The time horizon for cost analysis was 41 mo, including a 9-mo startup period and 32-mo intervention implementation. Activities during the startup period included recruitment and training of group facilitators and their supervisors, community sensitization activities, and development of video content and PLA meeting plans.
Program costs
A combination of activity-based costing (27), expenditure approach, and ingredient approaches (28) were used to estimate program costs. First, the intervention components and associated main activities were identified and defined as cost centers. Then, data on quantity and costs (or estimated value of resources, in case of donated items) were collected and allocated to these cost centers. To estimate the direct costs of designing and implementing the interventions, we collected financial cost data from all UPAVAN partner expenditure records or project accounts. For indirect costs, we identified donated items and volunteered time through interviews with all project staff and estimated their opportunity cost (value) using the current market value for donated items (28–30) and staff monthly salaries for volunteered time. Donated items were mainly video making and editing equipment used by the implementing partner. Volunteered time mainly included unpaid time contributed to the design and adaptation of intervention materials, as well as quality assurance by technical partners.
Cost data were collected using data capture tools (Supplemental Material–data collection tools) designed for the project. All data collected were entered into a customized excel-based costing tool, adapted from the costing tool developed by the UCL Centre for Global Health Economics (http://www.ighe.org) for analysis. The tool categorizes the costs based on the following line items: staff, materials, capital, joint costs (shared by several activities such as field travel and partner meetings), and overheads. the tool also categorizes costs based on the intervention component: AGRI, NUT, PLA, training of government frontline health and nutrition care providers, quality assurance and monitoring, or partner coordination, and implementation stage (startup or implementation). Staff costs were allocated to intervention components using data from staff time–use surveys collected through interviews with all project staff (full descriptions of line items, intervention components, and implementation phases are given in Supplemental Material Table S3). The same allocation rule was applied to allocate nonstaff joint costs to intervention components. Capital costs were annualized based on the estimated lifetime of each item, using a discount rate of 3%. We included contributions of the international technical (JSI RTI) and research partners (LSHTM and UCL) in developing and supporting interventions, but not research costs.
Costs to government health system
We measured direct financial costs and indirect opportunity costs incurred by primary health centers and government frontline health and nutrition care providers [i.e., Anganwadi workers (AWWs), accredited social health activists (ASHAs), and auxiliary nurse midwives (ANMs)].
Direct costs were based on any increase in the use of health and nutrition services (in the past 6 mo), as determined by comparing percentages of households using any health or nutrition services in each intervention relative to control in the endline survey, and published data on unit cost to health centers for providing those services (31–36).
We estimated the indirect costs as the opportunity costs of government frontline health and nutrition care providers participating in the interventions. This calculation was based on group attendance by government frontline health and nutrition workers (assessed from facilitator registers), mean durations of meetings and travel times to meeting locations (from the endline survey), and published monthly salaries of the government frontline health and nutrition care providers (Supplemental Material Table S2).
Costs to participants and their households
We estimated opportunity costs to participants of attending dissemination meetings and follow-up home visits by using data on the total number of group attendants and follow-up home visits per intervention arm (from facilitator registers and home visit forms); mean durations of group meetings and home visits, and mean travel time to the meeting location (collected in the UPAVAN endline survey); and the minimum daily wage of an agricultural worker in Odisha state (303 Indian Rupees or US$4.31) (37) (Supplemental Material Table S2).
We estimated cost to households of adopting practices promoted in UPAVAN as any differences in the following expenditures: seeking healthcare (out-of-pocket fees and transport costs paid for child and maternal healthcare from public, private, or informal healthcare providers), agricultural inputs, food costs, and nonfood costs. These costs were estimated as the mean differences between each intervention and the control arm, using the expenditure survey in the UPAVAN endline survey.
Analysis
Our results are presented in the form of cost–consequence analysis, by tabulating disaggregated costs and outcomes of the interventions compared with the control arm. We selected a program perspective as the base case to reflect the potential budget impact of adopting the intervention. The societal perspective presents the full costs of implementing the interventions.
All costs, including unit costs obtained from published studies, were adjusted for inflation using the Indian Consumer Price Index (38) and converted to 2019 US$, using the exchange rate of 70.42 (39) for the costs to Indian partners (in Indian Rupees), and 0.78 (39) for costs to the UK partners (in British Pounds Sterling, GBP). In addition, costs were discounted at 3% per y, as recommended by WHO-CHOICE (World Health Organization CHOosing Interventions that are Cost-Effective) (40) and the Gates/iDSI Reference Case for Economic Evaluation (41). Our study follows the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) (42).
We calculated total costs and mean annual costs of the interventions. Mean annual costs enable comparisons with other interventions that run for different durations. Mean annual costs were calculated as the sum of startup and implementation costs, divided by 41 mo (the costing time horizon), and multiplied by 12, so they divide startup costs equally across each year. We decomposed the total costs of the interventions and presented these as a share of line-item (i.e., staff, materials, capital, other), intervention component (i.e., NSA videos, nutrition-specific videos, PLA, quality assurance, coordination, frontline worker training), and implementation phase (i.e., startup and implementation).
To estimate the cost-efficiency of the interventions, we calculated the total or annual costs of each intervention per primary intervention participant. We also estimated cost per total point of contact (sum of group attendees and total home visits). We also estimated cost per unit increase in maternal and child dietary diversity scores (i.e., 2 statistically significant primary and secondary outcomes) for each intervention arm, compared with the control arm. They were calculated as mean increase in outcome divided by cost per primary intervention participant.
We conducted a number of univariate sensitivity analyses that vary 1 parameter at a time, and scenarios for potential intervention costs at scale. In sensitivity analysis, we examined the impact of 2 uncertain assumptions: we altered the allocation rule for dividing the costs of the nutrition-specific component between the AGRI-NUT and AGRI-NUT + PLA arms (from a 75:25 rule to a 90:10 rule), and we varied the discount rate from 0% to 6% (40, 41). In scenario analyses, we tested impacts of 3 scenarios that we believe will be relevant when interventions are implemented at scale: reducing startup costs by 50%, reducing costs of monitoring by 25% and 50%, and replacing international staff costs with local staff costs. A detailed description of sensitivity and scenario analyses are presented in the Supplemental Material - Sensitivity and scenario analyses.
Finally, we estimated the potential cost of delivering the AGRI-NUT + PLA intervention to all rural populations in Odisha state, by dividing the total intervention cost by the total population in the intervention clusters (based on census data) and multiplying by the total rural population of Odisha.
Results
Trial coverage and participation
UPAVAN's coverage and participation are described in Table 1. Throughout the 32-mo implementation period, the UPAVAN interventions covered a mean of 4567 primary intervention participants, and 9367 women of any age, per intervention arm. So, approximately one-half of participants were pregnant women and mothers of children aged 0–23 mo, and 17% of the total population directly participated in UPAVAN intervention activities, per arm. Assuming an average of 5 members per household (and 1 participant per household, and that household members discussed the interventions), the interventions reached a mean of 87% of the total population per arm.
TABLE 1.
Population coverage and participation in the UPAVAN interventions1
| Population | AGRI | AGRI-NUT | AGRI-NUT + PLA | Mean |
|---|---|---|---|---|
| Clusters | 37 | 37 | 37 | |
| Pregnant women and mothers of children age < 2 y in intervention clusters | ||||
| Total population (all ages) in intervention clusters | 51,220 | 50,094 | 60,681 | 53,998 |
| Coverage | ||||
| Primary intervention participants2 | 4389 | 4347 | 4965 | 4567 |
| Number of women (any age) who participated | 9202 | 9272 | 9626 | 9367 |
| Participation | ||||
| Average number of participants per video dissemination group | 20 (14–25) | 19 (13–25) | 18 (13–25) | 19 (13–25) |
| Total group meetings attended by primary participants | 61,446 | 60,858 | 44,685 | 55,663 |
| Total home visits to primary intervention participants | 59,482 | 57,051 | 33,0523 | 49,862 |
| Total group meetings attended by all people | 368,080 | 343,064 | 298,406 | 336,517 |
| Total points of contact with all people4 | 427,562 | 400,115 | 331,458 | 386,378 |
Values are n or n (range). AGRI, nutrition-sensitive agriculture intervention; AGRI-NUT, nutrition-sensitive and nutrition-specific agriculture intervention; AGRI-NUT + PLA, nutrition-sensitive and nutrition-specific agriculture intervention using the participatory learning and action approach; PLA, participatory learning and action; UPAVAN: Upscaling Participatory Action and Videos for Agriculture and Nutrition. 2Primary intervention participants were pregnant women and mothers of children 0–23 mo of age who attended ≥1 dissemination group meeting and received a follow-up home visit.
Facilitators aimed to conduct home visits after every video dissemination group meeting but only after some PLA meetings, when appropriate, so fewer home visits were planned in the AGRI-NUT + PLA arm.
Total points of contact is sum of total dissemination meeting attendance by all people and total home visit.
Program costs and program cost efficiency
Program costs are described in Table 2 and presented by year in Supplemental Material Table S4. Total program costs of the AGRI, AGRI-NUT, and AGRI-NUT + PLA intervention arms were estimated as US$272,121, US$366,686, and US$386,907, respectively, and the mean annual costs of the intervention arms were estimated as US$79,645, US$107,323, and US$113,241, respectively. Start-up costs accounted for ∼26% of total costs, with the AGRI-NUT arm having the highest proportion of startup costs (30%) and the AGRI-NUT + PLA arm having the lowest (23%). The main reason for higher startup costs for the AGRI-NUT arm is that more staff time was spent preparing nutrition-specific videos and training, mainly driven by inputs from international staff.
TABLE 2.
Cost description of the UPAVAN interventions from program perspective1
| AGRI | AGRI–NUT | AGRI–NUT + PLA | ||||
|---|---|---|---|---|---|---|
| Description | US$2 | % | US$2 | % | US$2 | % |
| Total economic cost of program | 272,121 | 366,686 | 386,907 | |||
| Startup costs | 71,176 | 26% | 108,978 | 30% | 89,905 | 23% |
| Implementation costs | 200,945 | 74% | 257,708 | 70% | 297,002 | 77% |
| Annual total economic costs3 | 79,645 | 107,323 | 113,241 | |||
| Annual implementation costs4 | 75,354 | 95% | 96,641 | 90% | 111,376 | 98% |
| Economic costs of main intervention components | ||||||
| Developing and delivering NSA videos | 186,912 | 69% | 93,456 | 25% | 93,456 | 24% |
| Developing and delivering nutrition-specific videos | 0 | 0% | 142,007 | 39% | 47,336 | 12% |
| Running PLA sessions and developing nutrition-specific videos through PLA | 0 | 0% | 0 | 0% | 61,557 | 16% |
| Quality assurance and monitoring activities | 69,041 | 25% | 101,976 | 28% | 160,139 | 41% |
| Partner coordination | 16,167 | 6% | 29,247 | 8% | 24,419 | 6% |
| Training government frontline workers5 | 4750 | NA | 4750 | NA | 4750 | NA |
AGRI, nutrition-sensitive agriculture intervention; AGRI-NUT, nutrition-sensitive and nutrition-specific agriculture intervention; AGRI-NUT + PLA, nutrition-sensitive and nutrition-specific agriculture intervention using the participatory learning and action approach; NA, not applicable; NSA, nutrition-sensitive agriculture; PLA, participatory learning and action; UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition.
2019 US$.
Mean annual total intervention costs over a time horizon of 41 mo.
Mean annual total costs during implementation period over implementation period of 32 mo
These costs are not included in total program costs as they were implemented in all arms including the control arm.
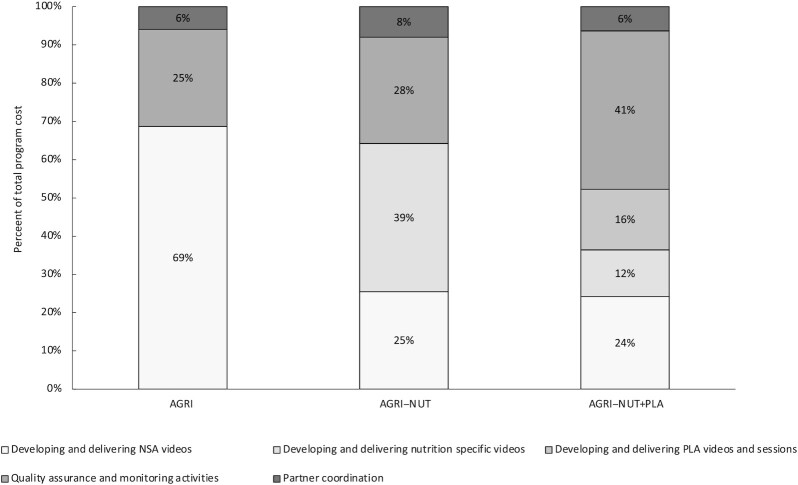
The main intervention activities of video production, group meetings, and follow-up home visits constituted the largest share of total costs (ranging from 52% in AGRI-NUT + PLA to 69% in AGRI). These activities were followed by the quality assurance and monitoring activities (ranging from 25% in the AGRI arm to 41% in the AGRI-NUT + PLA arm) (Figure 4). In the AGRI-NUT + PLA arm, more staff time was spent on the quality assurance of the PLA component from 1 partner (Ekjut).
FIGURE 4.
Composition of total program costs by UPAVAN intervention arm. AGRI, nutrition-sensitive agriculture intervention; AGRI-NUT, nutrition-sensitive and nutrition-specific agriculture intervention; AGRI-NUT + PLA, nutrition-sensitive and nutrition-specific agriculture intervention using the participatory learning and action approach; NSA, nutrition-sensitive agriculture; PLA, participatory learning and action; UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition.
Decomposing the total program costs to line items or inputs (as given in Table 3) shows that staff costs constituted the most costs, at ∼60% in each intervention arm, ranging from 56% in the AGRI-NUT arm to 65% in the AGRI-NUT + PLA arm. The staff costs were followed by other recurrent costs (travel costs and office overheads), varying from 29% in the AGRI-NUT + PLA arm to 39% in the AGRI-NUT arm, mainly due to the large portion of international travel by international staff (JSI RTI) in the AGRI-NUT arm. Most staff costs related to the delivery of interventions, i.e., salary for 24–26 facilitators per arm and 2–3 supervisors per arm, followed by support provided by technical assistance and research partners (Supplemental Figure 1). International staff costs were ∼33% of total staff costs, and mostly contributed to intervention development and technical support during implementation, particularly in the AGRI-NUT arm (Supplemental Figure 1).
TABLE 3.
Total economic program costs from program perspective, by line item and UPAVAN intervention arm1
| AGRI | AGRI-NUT | AGRI-NUT + PLA | ||||
|---|---|---|---|---|---|---|
| Expenses | US$2 | % | US$2 | % | 2019 US$2 | % |
| Staff | 162,153 | 60% | 203,805 | 56% | 249,794 | 65% |
| Materials | 2848 | 1% | 3445 | 1% | 3159 | 1% |
| Capital | 10,836 | 4% | 16,539 | 5% | 23,438 | 6% |
| Other recurrent | 96,284 | 35% | 142,897 | 39% | 110,516 | 29% |
| Total | 272,121 | 366,686 | 386,907 | |||
AGRI, nutrition-sensitive agriculture intervention; AGRI-NUT, nutrition-sensitive and nutrition-specific agriculture intervention; AGRI-NUT + PLA, nutrition sensitive and nutrition-specific agriculture intervention using participatory learning and action approach; PLA, participatory learning and action; UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition
2019 US$. An annual discount rate of 3% has been applied.
Table 4 gives the cost per intervention from both program and societal perspectives, followed by the cost-efficiency estimates per primary participant and per point of contact. Program costs per primary intervention participant were US$62 in the AGRI arm, US$84 in the AGRI-NUT arm, and US$78 in the AGRI-NUT + PLA arm. Program costs per point of contact were US$0.64 in AGRI, US$0.92 in AGRI-NUT, and US$1.17 in AGRI-NUT + PLA.
TABLE 4.
UPAVAN intervention costs and cost-efficiency by intervention arm1
| Description | AGRI | AGRI-NUT | AGRI-NUT + PLA |
|---|---|---|---|
| Program costs and program cost-efficiency (US$)2 | |||
| Total cost | 272,121 | 366,686 | 386,907 |
| Total cost per primary intervention participant3 | 62 | 84 | 78 |
| Annual cost per primary intervention participant4 | 18 | 25 | 23 |
| Total cost per point of contact5 | 0.64 | 0.92 | 1.17 |
| Societal costs, US$ | |||
| Total costs to the public healthcare providers | 6125 | 4735 | 5025 |
| Costs of increase in use of services | 7793 | 1680 | 5096 |
| Opportunity costs of involvement of frontline workers in interventions | 3527 | 4174 | 3326 |
| Total opportunity costs to the participants of attending the dissemination group meetings and home visits6 | 266,228 | 248,814 | 209,433 |
| Total societal costs and cost efficiency, US$ | |||
| Program + provider costs | 283,441 | 372,541 | 395,329 |
| Societal costs (program + provider + participant) | 549,668 | 621,355 | 604,762 |
| Total societal cost per primary intervention participant | 125 | 143 | 122 |
| Total societal cost per points of contact | 1.29 | 1.55 | 1.82 |
AGRI, nutrition-sensitive agriculture intervention; AGRI-NUT, nutrition-sensitive and nutrition-specific agriculture intervention; AGRI-NUT + PLA, nutrition sensitive and nutrition-specific agriculture intervention using participatory learning and action approach; PLA, participatory learning and action; UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition
2019 US$.
Primary intervention participants were pregnant women and mothers of children 0–23 mo of age who attended ≥1 dissemination group meeting and received a follow-up home visit.
Mean annual total costs over a time horizon of 41 mo.
Total points of contact is sum of total dissemination meeting attendance and total home visits.
Included costs incurred by primary intervention participants and all other women who attended ≥1 dissemination group meeting.
Societal costs of the interventions
Interventions slightly increased the use of maternal care services (such as delivery care, on-site feeding, and malaria testing) delivered by government frontline nutrition and health care providers, but participants did not incur significantly higher out-of-pocket expenditures. Based on the unit cost of these services, the total cost to the health system of this increased demand for health services ranged from US$1680 in the AGRI-NUT arm to US$7793 in the AGRI arm (Table 4).
Overall, government frontline nutrition and healthcare workers attended 9388 (in AGRI), 9509 (in AGRI-NUT), and 8012 (in AGRI-NUT + PLA) group meetings. Estimated total opportunity costs of their involvement ranged from US$3326 in the AGRI-NUT + PLA arm to US$4174 in the AGRI-NUT arm (Table 4).
Analyses of the endline survey data showed no evidence that the interventions increased participant household expenditures in total or on healthcare, agricultural inputs, food, or nonfood items (8). The estimated opportunity costs to the intervention participants from time spent participating ranged from US$209,433 in the AGRI-NUT + PLA arm to US$266,228 in the AGRI arm.
Taken together, total societal costs of the AGRI, AGRI-NUT, and AGRI-NUT + PLA interventions were US$549,668; US$621,355; and US$604,762; respectively. Total cost efficiency (program and societal costs per pregnant woman or mother of children aged 0–23 mo) was US$125 in AGRI, US$143 in AGR-NUT, and US$122 in AGRI-NUT + PLA. Total societal costs per point of contact were US$1.29, US$1.55, and US$1.82, respectively, (Table 4).
Intervention consequences and cost–outcome results
Results in Table 5 show that the AGRI-NUT and AGRI-NUT + PLA interventions increased the minimum dietary diversity of children, each compared with the control (adjusted RRs: 1.19 and 1.27; 95% CIs: 1.03, 1.37 and 1.11, 1.46, respectively. Both AGRI and AGRI-NUT + PLA increased minimum dietary diversity in mothers, each compared with the control [adjusted RR (95% CI): AGRI, 1.21 (1.01, 1.45); AGRI-NUT + PLA, 1.30 (1.10, 1.53)]. Furthermore, the AGRI intervention increased decision-making by women and the total and net annual value of agricultural production compared with the control arm. There was no statistically significant effect of the interventions on the other outcomes (8).
TABLE 5.
UPAVAN intervention consequences, measured as effects on trial outcomes among trial participants included in the endline survey1
| Control | AGRI vs. control | AGRI-NUT vs. control | AGRI-NUT + PLA vs. control | ||||
|---|---|---|---|---|---|---|---|
| n | n | aRR (95% CI) | n | aRR (95% CI) | n | aRR (95% CI) | |
| Child minimum diet diversity (ate ≥4 food groups) | 757 | 822 | 1.06 (0.91, 1.23), | 812 | 1.19 (1.03, 1.37)2 | 863 | 1.27 (1.11, 1.46)2 |
| Maternal minimum diet diversity (ate ≥5 food groups) | 997 | 1100 | 1.21 (1.01, 1.45)2 | 1055 | 1.16 (0.98, 1.38) | 1139 | 1.30 (1.10, 1.53)2 |
| Child minimum acceptable diet | 790 | 862 | 1.01 (0.86, 1.19) | 829 | 1.19 (1.02, 1.41)2 | 895 | 1.30 (1.12, 1.52) |
| Women made ≥2 decisions in agriculture or health | 997 | 1100 | 1.05 (1.00, 1.11)2 | 1055 | 1.05 (0.99, 1.1) | 1139 | 1.02 (0.96, 1.07) |
| Total value of agricultural production over 1 y, US$ | 996 | 1100 | 108 (31, 231)1 | 1053 | −5 (−134, 118) | 1138 | 70 (−2, 190) |
| Net value (total value minus input costs) of agriculture production over 1 y, US$ | 996 | 1100 | 97 (25, 219)2 | 1053 | −3 (−131, 112) | 1138 | 76 (12, 196) |
AGRI, nutrition-sensitive agriculture intervention; AGRI-NUT, nutrition-sensitive and nutrition-specific agriculture intervention; AGRI-NUT + PLA, nutrition-sensitive and nutrition-specific agriculture intervention using participatory learning and action approach; aRR, adjusted RR, only reported for the statistically significant outcomes of the trial; PLA, participatory learning and action; UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition; vs., versus.
Significantly different from the control arm, P < 0.05.
Table 6 presents results from our estimates for cost per mean change in maternal and child dietary diversity scores. The results show that, with US$287, the AGRI-NUT + PLA arm has the lowest cost per unit of improvement, reflecting the larger improvements in both maternal and child dietary diversity in the AGRI-NUT + PLA arm than in the AGRI and AGRI-NUT arms, both compared with the control arm.
TABLE 6.
Cost outcome results from UPAVAN interventions, by intervention arm1
| AGRI | AGRI–NUT | AGRI–NUT + PLA | |
|---|---|---|---|
| Total program cost, US$ | 272,121 | 366,686 | 386,907 |
| Primary intervention participants covered,2n | 4389 | 4347 | 4965 |
| Mean child DDS3 | 0.0 (−0.15, 0.16) | 0.13 (−0.04, 0.30) | 0.28 (0.13, 0.44)5 |
| Mean maternal DDS4 | 0.12 (−0.06, 0.30) | 0.14 (−0.03, 0.31) | 0.24 (0.08, 0.41)5 |
| Cost per primary intervention participants, US$ | 62 | 84 | 78 |
| Cost outcome, child DDS | — | 603 | 278 |
| Cost outcome, maternal DDS | 517 | 603 | 325 |
AGRI, nutrition-sensitive agriculture intervention; AGRI-NUT, nutrition-sensitive and nutrition-specific agriculture intervention; AGRI-NUT + PLA, nutrition-sensitive and nutrition-specific agriculture intervention using participatory learning and action approach; DDS, dietary diversity score; PLA, participatory learning and action; UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition.
Primary intervention participants (pregnant women and mothers of children <2 y of age who attended ≥1 women's group meeting). 3DDS: Dietary diversity score
One result from baseline missing due to implausible value.
Significantly different from the control arm, P < 0.05.
Sensitivity and scenario analysis
Table 7 shows that replacing international staff costs with local staff costs and reducing monitoring and startup costs had a large impact on the results. Replacing international staff costs with local staff costs reduced total costs by between 24% in the AGRI-NUT + PLA arm to 40% in the AGRI-NUT arm. Reducing costs of the monitoring information system by 50% (25%) reduced the total costs by between 13% (6%) in the AGRI arm to 21% (10%) in the AGRI-NUT + PLA arm. Reducing startup costs by 50% reduced the total costs and cost per primary intervention participant (pregnant women and mothers of children 0–23 mo of age) between 12% in the AGRI-NUT + PLA arm to 15% in the AGRI-NUT arm. Varying the discount rate or changing the allocation rule for the nutrition-specific component had a modest effect on the results, ranging from −10 to +10%.
TABLE 7.
Results from sensitivity and scenario analyses by UPAVAN intervention arm1.
| Intervention arms | ||||||
|---|---|---|---|---|---|---|
| AGRI | AGRI–NUT | AGRI–NUT + PLA | ||||
| Scenarios/parameters | Total costs | Cost per primary intervention participant3 | Total costs | Cost per primary intervention participant | Total costs | Cost per primary intervention participant |
| Base-case scenario | 272,121 | 62 | 366,686 | 84 | 386,907 | 78 |
| Allocation rule for nutrition-specific component between arms 2 and 3 (base-case 75% vs. 25%) | ||||||
| Alternative allocation rule: 90% vs. 10% | 272,121 | 62 | 403,726 | 93 | 349,867 | 70 |
| Discount rate (base-case 3%) | 0 | |||||
| Discount rate 0% | 284,880 | 65 | 382,748 | 88 | 405,884 | 82 |
| Discount rate 6% | 260,470 | 59 | 352,000 | 81 | 369,612 | 74 |
| Startup costs (base-case 100%) | ||||||
| Reduce startup costs by 50% | 236,533 | 54 | 312,197 | 72 | 341,955 | 69 |
| MIS costs (base-case 100%) | ||||||
| Reducing MIS costs by 25% | 254,860 | 58 | 341,192 | 78 | 346,872 | 70 |
| Reducing MIS costs by 50% | 237,600 | 54 | 315,698 | 73 | 306,837 | 62 |
| Replacing international costs with local staff | 182,849 | 42 | 219,025 | 50 | 294,963 | 59 |
All values in 2019 US$. AGRI, nutrition-sensitive agriculture intervention; AGRI-NUT, nutrition-sensitive and nutrition-specific agriculture intervention; AGRI-NUT + PLA, nutrition-sensitive and nutrition-specific agriculture intervention using participatory learning and action approach; MIS, monitoring information system; PLA, participatory learning and action; UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition; vs., versus.
Program costs
Primary intervention participants were pregnant women and mothers of children aged 0–23 mo who attended ≥1 dissemination group meeting.
Cost and affordability of scaleup
Given that AGRI-NUT + PLA was the only intervention to increase both maternal and child dietary diversity, we modeled the potential cost of scaling up the AGRI-NUT + PLA intervention to all rural districts in Odisha. The cost would be ∼US$65 million per y, based on a cost of US$1.9 per person (total population in the AGRI-NUT + PLA intervention clusters). This is ∼5% of the proposed state health budget for 2021–2022 (∼US$1.3 billion per y) or 1.7% of the combined health and agriculture budget (43). However, unit costs might be lower due to potential economies of scale. In addition, given the investments already made in developing the UPAVAN interventions, it is expected that monitoring and evaluation, startup, and coordination activities will be less intensive at scale, reducing implementation costs significantly, as shown in the sensitivity and scenario analyses.
Discussion
This study contributes to the limited economic evaluation evidence on multisectoral nutrition interventions and is to our knowledge the first economic evaluation of a nutrition-sensitive agriculture intervention in South Asia. We found that participatory NSA interventions, with different combinations of nutrition-specific behavior change or PLA components, can increase child and maternal minimum dietary diversity. The total costs of designing and implementing the UPAVAN interventions ranged from US$271,121 to US$386,907, and annual costs ranged from US$79,645 to US$113,241. Throughout the 32 mo of implementation, the interventions covered a mean of 4567 pregnant women and mothers of children 0–23 mo of age per intervention, and the cost per pregnant woman or mother (the primary intervention participant) ranged from US$62 in the AGRI arm to US$84 in the AGRI-NUT arm.
Making comparison between UPAVAN and other NSA interventions is challenging due to differences in intervention components, delivery platforms, scales, outcomes assessed, and costing approaches. However, 2 interventions share some similarities with the UPAVAN interventions: NEEP-IE (Nutrition Embedded Evaluation Programme Impact Evaluation) in Malawi (11, 12, 44), and Mama SASHA (Sweetpotato Action for Security and Health in Africa) in Kenya (10). NEEP-IE integrated NSA with nutrition-specific training and used community-based early childhood development centers and parenting group platforms (44, 45). Mama SASHA promoted production and consumption of orange-fleshed sweet potato and integrated nutrition-specific and health components, delivered through health facilities, community health workers, and extension officers (46). UPAVAN, NEEP-IE, and Mama Sasha had similar cost efficiency, at US$62 to US$84 per participant in UPAVAN, US$160 per preschool child covered in NEEP-IE (11), and US$110 per woman and child covered in Mama SASHA (10). In all 3 programs, staff and travel costs constituted major shares (UPAVAN: 56–60%; NEEP-IE: 40%; Mama SASHA: 25%). Comparing point estimates, we found that, for child dietary diversity, AGRI and AGRI-NUT were less cost-effective than NEEP-IE and Mama SASHA, but AGRI-NUT + PLA was more cost-effective (AGRI had no effect; cost per food group increase for AGRI-NUT: US$603; NEEP-IE: US$444; Mama SASHA: US$305; and AGRI-NUT + PLA US$278). Similarly, AGRI and AGRI-NUT were less cost-effective than Mama SASHA at improving maternal diet diversity, but AGRI-NUT + PLA was more cost-effective (cost per food group increase for: AGRI US$517; AGRI-NUT US$603; Mama SASHA US$324; AGRI-NUT + PLA US$325) (47). For NEEP-IE, effects on maternal diet diversity were not reported.
Taken together, our findings show broadly similar cost profiles, cost-efficiency, and cost-effectiveness for UPAVAN, NEEP-IE, and Mama SASHA. Although the UPAVAN trial was not designed to detect differences between intervention arms, we note that the higher cost-effectiveness in the AGRI-NUT + PLA intervention compared with that in the control arm suggests that the AGRI-NUT + PLA intervention is a better value for the money than the AGRI or AGRI-NUT interventions. Therefore, the Participatory Learning and Action component may help to increase cost-effectiveness of NSA interventions. The choice of which intervention to scale up will depend on transferability of intervention models across contexts, and policymaker priorities for other outcomes. For example, NEEP-IE had additional effects on stunting [with cost-effectiveness ratios of US$595 per case of stunting averted, and US$516 per disability-adjusted life years (DALYs)averted (12)], and both NEEP-IE and AGRI interventions increased agricultural production, whereas Mama SASHA specifically increased production of orange-flesh sweet potatoes and nutrition knowledge.
We consider how NSA interventions compare to other nutrition-specific interventions, beyond the 10 nutrition-specific interventions already recommended at scale (at a cost of US$125 to US$571 per life-year saved). Nutrition-specific women's groups using a PLA approach (48) and SHG (49) have shown similar cost efficiency (US$62 to US$140 per participant), and similar magnitude of effects on dietary diversity of mothers [adjusted OR >5/10 food groups: 1.4 (48)], and children [mean difference: 0.17 food groups (49)]. Biofortification with nutrition education is less expensive, at US$65 and US$49 per beneficiary household in Mozambique and Uganda, respectively, and can double vitamin A intakes in children (50). A modeling study of food-based interventions showed that, in India, mass media campaigns and complementary food processing interventions would be more cost effective than a household horticulture intervention (US$90 and US$41, compared with US$644 per life-year saved) (51).
We conclude that NSA interventions have cost efficiency and effectiveness similar to those for nutrition-specific women's group interventions but may be less cost effective at improving nutrition than other approaches, such as mass media campaigns, complementary food processing, and food fortification. However, NSA can have added benefits of improved agricultural productivity, which nutrition-specific interventions would be less likely to achieve. In contrast, addition of agricultural components to nutrition and health education interventions, such as home-gardens (52) and community vegetable gardens (53), is prohibitively expensive, at ∼2014 US$918 per beneficiary in Bangladesh (52) and EUR 1525 per beneficiary household in Zimbabwe (53).
Policy implications: scalability and affordability
Before we conducted the trial, some components of the UPAVAN interventions were already being implemented at scale in several states in India. Participatory agriculture extension videos have been scaled up across several states in India, in collaboration with National and State Livelihood Missions and with the use of a women's self-help group platform reaching ∼2 million smallholder farmers (54). Participatory nutrition-specific videos have been scaled up across 5 states in India, in collaboration with State Livelihood Missions, the National Health Mission, and other state-level institutions, reaching around half a million pregnant women and mothers of children aged 0–23 mo (55). In addition, supported by the National Health Mission, PLA groups have been scaled up across all districts in Jharkhand and one-third of districts in the Madhya Pradesh states, through incentivized ASHAs and ASHA supervisors (56, 57). Evidence on statewide scaleups of PLA groups in Jharkhand showed that employing incentivized ASHAs and ASHA supervisors and using an innovative approach for training at scale resulted in a substantial reduction in implementation costs, without compromising the impact of the intervention (58, 59). Similar models could be tested for participatory video–based NSA interventions.
Although there is clearly policy interest in the UPAVAN components, their implementation at scale is currently only being conducted by government frontline workers from single sectors. Scaleup of the UPAVAN interventions and other multisectoral approaches will require coordination of multiple stakeholders across sectors, for which the challenges are well recognized (12). It is hoped that our economic evaluation will provide further impetus to increase collaboration across sectors, but stakeholder analyses may be needed to further support this goal.
Limitations
Some limitations of this study are notable. First, adoption of practices promoted by the UPAVAN interventions, or collective actions taken by participating communities, might have caused direct and indirect costs and benefits to participants and the communities that were not accounted for. As with any complex economic evaluation, it is difficult to determine the direction of bias in our overall conclusions because it was also not possible to fully identify and measure all of the benefits associated with the interventions. The trial measured only effects on children 0–23 mo of age and their mothers and families and did not measure effects on the communities as a whole. The trial also did not include other possible short- and long-term consequences for participants, such as improvements in soil quality, micronutrient adequacy, intrahousehold relationships, social support, mental health, or overall wellbeing. In addition, some community members and government frontline health and nutrition care workers were involved in the production of NSA and nutrition-specific videos. The costs of their involvement have not been included here but are likely to have been small and would not have seriously affected the study findings. Third, as is standard practice, the trial was powered to detect differences only in the primary outcomes. Statistically insignificant effects in other outcomes, such as household food expenditures and healthcare seeking or utilization may have been due to lack of statistical power rather than lack of effect. Finally, we do not report cost-effectiveness in terms of outcomes commonly used in cost-effectiveness analyses of nutrition interventions (such as DALYs or life-years saved), which limits comparisons with other nutrition interventions. The outcomes that the interventions aimed to change cannot be easily translated to DALYs or other common outcomes for.
Conclusions
In this study we estimated the cost of designing and implementing 3 participatory NSA interventions in rural India, responding to the gap in evidence on the costs of multisectoral NSA interventions and providing useful data to inform their potential scaleup. Our findings show that the costs per primary intervention participant of implementing the interventions are comparable with the results from a limited set of evaluated multisectoral NSA interventions. Considering that a substantial investment has already been made to develop the UPAVAN interventions, costs at scale could be decreased with a less intensive information monitoring system, reduced startup costs, integration within existing programs, and possible economies of scale. We recommend scaleup of AGRI-NUT + PLA, which had the lowest cost per unit increase in dietary diversity. This scaleup should be feasible, given that participatory videos on agriculture, nutrition, and PLA groups are already being implemented at scale in several settings, and because the intervention approach is designed to be responsive to local contexts.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Avinash Upadhyay, Vinay Kumar and S. Kaushik from Digital Green; Kristina Granger, Sarah Hogan and Ashley Thompson from JSI SPRING, and the accountants at VARRAT and Digital Green for their contribution in setting up and collection of cost data. We thank Joanna Sturgess, Diana Elbourne, and Emma Beaumont for their contributions to the impact evaluation. We also thank all VARRAT, EKJUT, and DCOR field staff for delivering the intervention and conducting the impact evaluation surveys.The authors’ responsibilities were as follows—HH-B, JS: conceived and designed this economic evaluation study; HH-B: designed/adapted the cost data collection tools; MO, AK, SF, RP, SKa, SKr, HH-F: provided input for design/adaptation of the cost data collection tools; AK, AKO, SF, SN, NKM, ShP, PJ, SM, SNM: contributed to setting up and/or collection of cost data. HH-B: led the cost analyses; TP, EF, HH-F: contributed to cost analyses; HH-B: wrote the first draft of the manuscript; with critical contributions from HH-F, TP, JS, SKa, AP: made critical contributions to the manuscript; SKa, EA, AP: developed UPAVAN trial evaluation design; HH-F: provided support for UPAVAN trial evaluation design; EA: led the statistical analysis of the UPAVAN impact evaluation; SKa, HH-F, EF, PJ: helped with statistical analysis; SKa, AP, HH-F, RP, ShP, SuR, PKB, NN, NKM, ShR, HD, SKr, MO, PT: designed the interventions; SM: led the impact and process evaluation data collection; SKa, SKr, HHF, AP, EA, PJ, EF: supported the impact and process evaluation data collection; ShP, RP, SuR, NN, NKM: led the supervision of all implementation activities for all interventions; and all authors: read and approved the final manuscript.
Notes
The UPAVAN trial was funded by the Bill & Melinda Gates Foundation and UK Aid (award number OPP1136656). Substantial cofunding was also provided by the USAID-funded project Digital Integration to Scale Gender-Sensitive Nutrition Social and Behavior Change Communication, implemented by Digital Green (Cooperative Agreement No. AID-386-A-15–00008). Additional technical inputs were provided by the SPRING project contributing funds from USAID's Bureau for Food Security (BFS) and Bureau for Global Health (GH) (under Cooperative Agreement No. AID-OAA-A-11-00031). The trial funders had no role in study design, data collection, analysis, interpretation or writing of the paper.
Author disclosures: The authors report no conflicts of interest.
Supplemental Material Tables S1–S4, Supplemental Material–data collection tools, Supplemental Material - Sensitivity and scenario analyses, and Supplemental Figure 1 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn/.
HH-B and HH-F are joint first authors.
Abbreviations used: ASHA, accredited social health activist; JSI RTI, John Snow Inc. Research and Training Institute; LSHTM, London School of Hygiene & Tropical Medicine; Mama SASHA, Sweetpotato Action for Security and Health in Africa; NEEP-IE, Nutrition Embedded Evaluation Programme Impact Evaluation; NSA, nutrition-sensitive agriculture; PLA, participatory learning and action; SHG, self-help group; UCL, University College London; UPAVAN, Upscaling Participatory Action and Videos for Agriculture and Nutrition; VARRAT, Voluntary Association for Rural Reconstruction and Appropriate Technology; DALYs, Disability-Adjusted Life Years
Contributor Information
Hassan Haghparast-Bidgoli, University College London, Institute for Global Health, London, United Kingdom.
Helen Harris-Fry, London School of Hygiene & Tropical Medicine, London, United Kingdom.
Abhinav Kumar, Digital Green, New Delhi, India.
Ronali Pradhan, Digital Green, New Delhi, India.
Naba Kishore Mishra, Voluntary Association for Rural Reconstruction and Appropriate Technology (VARRAT), Kendrapada, Odisha, India.
Shibananth Padhan, Voluntary Association for Rural Reconstruction and Appropriate Technology (VARRAT), Kendrapada, Odisha, India.
Amit Kumar Ojha, Ekjut, Chakradharpur, Jharkhand, India.
Sailendra Narayan Mishra, Voluntary Association for Rural Reconstruction and Appropriate Technology (VARRAT), Kendrapada, Odisha, India.
Emily Fivian, London School of Hygiene & Tropical Medicine, London, United Kingdom.
Philip James, London School of Hygiene & Tropical Medicine, London, United Kingdom.
Sarah Ferguson, Devoted Health, Waltham, MA, USA.
Sneha Krishnan, Jindal School of Environment and Sustainability, OP Jindal Global University and ETCH Consultancy Services, Mumbai, Maharashtra, India.
Meghan O'Hearn, Tufts University Friedman School of Nutrition Science and Policy, Boston, MA, USA.
Tom Palmer, University College London, Institute for Global Health, London, United Kingdom.
Peggy Koniz-Booher, SI Research & Training Institute, Inc. Arlington, VA, USA.
Heather Danton, SI Research & Training Institute, Inc. Arlington, VA, USA.
Sandee Minovi, SI Research & Training Institute, Inc. Arlington, VA, USA.
Satyanarayan Mohanty, DCOR Consulting Pvt. Ltd. Bhubaneshwar, India.
Shibanand Rath, Ekjut, Chakradharpur, Jharkhand, India.
Suchitra Rath, Ekjut, Chakradharpur, Jharkhand, India.
Nirmala Nair, Ekjut, Chakradharpur, Jharkhand, India.
Prasanta Tripathy, Ekjut, Chakradharpur, Jharkhand, India.
Audrey Prost, University College London, Institute for Global Health, London, United Kingdom.
Elizabeth Allen, London School of Hygiene & Tropical Medicine, London, United Kingdom.
Jolene Skordis, University College London, Institute for Global Health, London, United Kingdom.
Suneetha Kadiyala, London School of Hygiene & Tropical Medicine, London, United Kingdom.
Data Availability
Aggregated cost data are provided in the tables within paper and in supplemental tables. Trial outcome data will be available from the LSHTM Data Compass, an open-assess institutional research data repository, at https://datacompass.lshtm.ac.uk/.
References
- 1. Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton Set al. . Lancet nutrition interventions review group tM, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost?. Lancet North Am Ed. 2013;382(9890):452–77. [DOI] [PubMed] [Google Scholar]
- 2. Gyles CL, Lenoir-Wijnkoop I, Carlberg JG, Senanayake V, Gutierrez-Ibarluzea I, Poley MJet al. . Health economics and nutrition: a review of published evidence. Nutr Rev. 2012;70(12):693–708. [DOI] [PubMed] [Google Scholar]
- 3. Ramponi F, Tafesse W, Griffin S. Economic evaluation of interventions to address undernutrition: a systematic review. Health Policy Plan. 2021;36(4):533–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Njuguna RG, Berkley JA, Jemutai J. Cost and cost-effectiveness analysis of treatment for child undernutrition in low- and middle-income countries: a systematic review. Wellcome Open Research. 2020;5:62: doi: 10.12688/wellcomeopenres.15781.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. United Nations . SDG2: zero hunger. Available from[Internet]: https://www.un.org/sustainabledevelopment/hunger/. [Google Scholar]
- 6. Ruel MT, Alderman H, Maternal G CNS. Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition?. Lancet North Am Ed. 2013;382(9891):536–51. [DOI] [PubMed] [Google Scholar]
- 7. 2020 Global Nutrition Report: Action on equity to end malnutrition . 2020. Development Initiatives: Bristol, UK [Google Scholar]
- 8. Kadiyala S, Harris-Fry H, Pradhan R, Mohanty S, Padhan S, Rath Set al. . Effect of nutrition-sensitive agriculture interventions with participatory videos and women's group meetings on maternal and child nutritional outcomes in rural Odisha, India (UPAVAN trial): a four-arm, observer-blind, cluster-randomised controlled trial. Lancet Planetary Health. 2021;5:e263–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ruel MT, Quisumbing AR, Balagamwala M. Nutrition-sensitive agriculture: what have we learned so far?. Global Food Security. 2018;17:128–53. [Google Scholar]
- 10. Levin CE, Self JL, Kedera E, Wamalwa M, Hu J, Grant Fet al. . What is the cost of integration? Evidence from an integrated health and agriculture project to improve nutrition outcomes in Western Kenya. Health Policy Plan. 2019;34(9):646–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Margolies A, Gelli A, Daryanani R, Twalibu A, Levin C. When communities pull their weight: the economic costs of an integrated agriculture and nutrition home-grown preschool meal intervention in malawi. Food Nutr Bull. 2021;42(1):3–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gelli A, Cg Kemp, Margolies A, Twalibu A, Katundu M, Levin C. Economic evaluation of an early childhood development center–based agriculture and nutrition intervention in Malawi. Food Secur. 2022;14(1):67–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. International Institute for Population Sciences (IIPS) and ICF . 2017. National Family Health Survey (NFHS-4), 2015-16. IIPS: Mumbai, India. [Google Scholar]
- 14. Avula R, Raykar N, Menon P, Laxminarayan R. Reducing stunting in India: what investments are needed?. Maternal & Child Nutrition. 2016;12(S1):249–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gaihre S, Kyle J, Semple S, Smith J, Marais D, Subedi Met al. . Bridging barriers to advance multisector approaches to improve food security, nutrition and population health in Nepal: transdisciplinary perspectives. BMC Public Health. 2019;19(1):961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Levin C, Masters W, Gelli A, Harris-Fry H, Kadiyala S, Kalamatianou Set al. . Economic evaluation of multisectoral actions for health and nutrition. Agriculture, nutrition and health academy working group of economic evaluations. Agriculture, Nutrition and Health Academy; 2019. [Google Scholar]
- 17. NICE . How NICE measures value for money in relation to public health interventions. London: NICE; (www.nice.org.uk)2013. [Google Scholar]
- 18. Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes: Oxford University Press; 2015. [Google Scholar]
- 19. Kadiyala S, Prost A, Harris-Fry H, O'Hearn M, Pradhan R, Pradhan Set al. . Upscaling participatory action and videos for agriculture and nutrition (UPAVAN) trial comparing three variants of a nutrition-sensitive agricultural extension intervention to improve maternal and child nutritional outcomes in rural Odisha, India: study protocol for a cluster randomised controlled trial. Trials. 2018;19(1):176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Harris-Fry H, O'Hearn M, Pradhan R, Krishnan S, Nair N, Rath Set al. . How to design a complex behaviour change intervention: experiences from a nutrition-sensitive agriculture trial in rural India. BMJ Global Health. 2020;5(6):e002384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Census Organization of India . 2011. Census of India 2011, Odisha, District Census Handbook, Kendujhar, Village and Town Wise Primary Census Abstract (PCA). Odisha: Directorate of Census Operations. [Google Scholar]
- 22. Gandhi R, Veeraraghavan R, Toyama K, Ramprasad V. Digital Green: participatory video and mediated instruction for agricultural extension. 2007 International Conference on Information and Communication Technologies and Development. 2007:1–10.. doi: 10.1109/ICTD.2007.4937388 [Google Scholar]
- 23. WHO . Indicators for assessing infant and young child feeding practices: definitions and measurement methods. World Health Organization; 2021. [Google Scholar]
- 24. FAO and FHI 360 . Minimum dietary diversity for women: a guide for measurement. Rome: Food and Agriculture Organization of the United Nations; 2016. [Google Scholar]
- 25. WHO and UNICEF . WHO child growth standards and the identification of severe acute malnutrition in infants and children: a joint statement. 2009. [PubMed] [Google Scholar]
- 26. Haghparast-Bidgoli H, Skordis J, Harris-Fry H, Krishnan S, O'Hearn M, Kumar Aet al. . Protocol for the cost-consequence and equity impact analyses of a cluster randomised controlled trial comparing three variants of a nutrition-sensitive agricultural extension intervention to improve maternal and child dietary diversity and nutritional status in rural odisha, india (UPAVAN trial). Trials. 2019;20(1):287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fiedler JL, Villalobos CA, De Mattos AC. An activity-based cost analysis of the Honduras community-based, integrated child care (AIN-C) programme. Health Policy Plan. 2008;23(6):408–27. [DOI] [PubMed] [Google Scholar]
- 28. Johns B, Baltussen R, Hutubessy R. Programme costs in the economic evaluation of health interventions. Cost Effectiveness and Resource Allocation. 2003;1(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hutton G, Baltussen R. Cost valuation in resource-poor settings. Health Policy Plan. 2005;20(4):252–9. [DOI] [PubMed] [Google Scholar]
- 30. Walker D. Cost and cost-effectiveness guidelines: which ones to use?. Health Policy Plan. 2001;16(1):113–21. [DOI] [PubMed] [Google Scholar]
- 31. Sethi V, Tiwari K, Sareen N, Singh S, Mishra C, Jagadeeshwar Met al. . Delivering an integrated package of maternal nutrition services in Andhra Pradesh and Telangana (India). Food Nutr Bull. 2019;40(3):393–408. [DOI] [PubMed] [Google Scholar]
- 32. Engel N, Ganesh G, Patil M, Yellappa V, Vadnais C, Pai NPet al. . Point-of-care testing in India: missed opportunities to realize the true potential of point-of-care testing programs. BMC Health Services Research. 2015;15:(1):550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Menon P, McDonald CM, Chakrabarti S. Estimating the cost of delivering direct nutrition interventions at scale: national and subnational level insights from India. Matern Child Nutr. 2016;11(Suppl 1):169–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Prinja S, Bahuguna P, Mohan P, Mazumder S, Taneja S, Bhandari Net al. . Cost effectiveness of implementing integrated management of neonatal and childhood illnesses program in district faridabad, PLoS One. 2016;11(1):e0145043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Prinja S, Gupta A, Verma R, Bahuguna P, Kumar D, Kaur Met al. . Cost of delivering health care services in public sector primary and community health centres in North India. PLoS One. 2016;11(8):e0160986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Prinja S, Jeet G, Verma R, Kumar D, Bahuguna P, Kaur Met al. . Economic analysis of delivering primary health care services through community health workers in 3 North Indian states. PLoS One. 2014;9(3):e91781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Minimum Wage – Odisha 2020. Available from [Internet]: https://paycheck.in/salary/minimumwages/19709-odisha/19710-agriculture. [Google Scholar]
- 38. World Bank . Consumer price index: World Bank; 2020; [cited 2020 29/05/2020]. Available from [Internet]: https://data.worldbank.org/indicator/FP.CPI.TOTL?locations=IN. [Google Scholar]
- 39. Bank W. Official exchange rate. 2020; [cited 2020 29/05/2020]. Available from [Internet]: https://data.worldbank.org/indicator/PA.NUS.FCRF. [Google Scholar]
- 40. Tan-Torres Edejer T, Baltussen R, Adam T, Hutubessy R, Acharya A, Evans DBet al. . Making choices in health: WHO guide to cost-effectiveness analysis. Geneva: World Health Organization; 2003. [Google Scholar]
- 41. Claxton K, Revill P, Sculpher M, Wilkinson T, Cairns J, Briggs A. The Gates Reference Case for Economic Evaluation. The Bill and Melinda Gates Foundation; 2014. [Google Scholar]
- 42. Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg Det al. . Consolidated Health Economic Evaluation Reporting Standards (CHEERS)–explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013;16(2):231–50. [DOI] [PubMed] [Google Scholar]
- 43. Odisha Government . Odisha budget: finance department, Odisha Government; 2021; [cited 2021 16/04/2021]. Available from [Internet]: https://budget.odisha.gov.in/previous-yearly-budget/2021. [Google Scholar]
- 44. Gelli A, Nguyen PH, Santacroce M, Twalibu A, Margolies A, Katundu M. A community-based early childhood development center platform promoting diversified diets and food production increases the mean probability of adequacy of intake of preschoolers in Malawi: a cluster randomized trial. J Nutr. 2020;150(2):350–5. [DOI] [PubMed] [Google Scholar]
- 45. Gelli A, Margolies A, Santacroce M, Roschnik N, Twalibu A, Katundu Met al. . Using a community-based early childhood development center as a platform to promote production and consumption diversity increases children's dietary intake and reduces stunting in Malawi: a cluster-randomized trial. J Nutr. 2018;148(10):1587–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cole DC, Levin C, Loechl C, Thiele G, Grant F, Girard AWet al. . Planning an integrated agriculture and health program and designing its evaluation: experience from Western Kenya. Eval Program Plann. 2016;56:11–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Low J. Integrating health and agriculture to maximize the nutritional impact of orange-fleshed sweetpotato: results from the Mama SASHA. Nairobi (Kenya): International Potato Center (CIP); 2015. [Google Scholar]
- 48. Nair N, Tripathy P, Sachdev HS, Pradhan H, Bhattacharyya S, Gope Ret al. . Effect of participatory women's groups and counselling through home visits on children's linear growth in rural eastern India (CARING trial): a cluster-randomised controlled trial. Lancet Global Health. 2017;5(10):e1004–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gupta S, Kumar N, Menon P, Pandey S, Raghunathan K. Engaging women's groups to improve nutrition: findings from an evaluation of the JEEViKA multisectoral convergence pilot in Saharsa, Bihar. Washington, DC: World Bank; 2019. [Google Scholar]
- 50. de Brauw A, Eozenou P, Gilligan DO, Hotz C, Kumar N, Meenakshi JV. Biofortification, crop adoption and health information: impact pathways in Mozambique and Uganda. Am J Agric Econ. 2018;100(3):906–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Webb P, Danaei G, Masters WA, Rosettie KL, Leech AA, Cohen Jet al. . Modelling the potential cost-effectiveness of food-based programs to reduce malnutrition. Globe Food Sec. 2021;29:100550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Schreinemachers P, Patalagsa MA, MN. U. Impact and cost-effectiveness of women's training in home gardening and nutrition in Bangladesh. J Dev Eff. 2016;8(4):473–88. [Google Scholar]
- 53. Puett C, Salpeteur C, Lacroix E, Zimunya SD, Israel AD, Ait-Aissa m. Cost-effectiveness of community vegetable gardens for people living with HIV in Zimbabwe. Cost Eff Resour Alloc. 2014;12(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. New Delhi India: Digital Green; [cited 2021 01/04/2021]. Available from [Internet]: https://www.digitalgreen.org/india/URL. [Google Scholar]
- 55. Digital Green . SAMVAD project. 2021; [cited 2021 01/04/2021]. Available from [Internet]: https://www.digitalgreen.org/samvad/. [Google Scholar]
- 56. EKJUT[Internet] . 2021; [cited 2021 01/04/2021]. Available from [Internet]: http://www.ekjutindia.org/. [Google Scholar]
- 57. National Health Mission . Annual Report. National Health Mission Department of Health & Family Welfare; 2018. [Google Scholar]
- 58. CIFF . Sustainable child health solutions: for the community, by the community: Children Investment Fund Foundation; 2019; [cited 2021 20 Jan]. Available from [Internet]: https://ciff.org/news/sustainable-child-health-solutions-community-community/. [Google Scholar]
- 59. Nair N, Tripathy PK, Gope R, Rath S, Pradhan H, Rath Set al. . Effectiveness of participatory women's groups scaled up by the public health system to improve birth outcomes in Jharkhand, Eastern India: a pragmatic cluster non-randomised controlled trial. BMJ Global Health. 2021;6(11):e005066. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Aggregated cost data are provided in the tables within paper and in supplemental tables. Trial outcome data will be available from the LSHTM Data Compass, an open-assess institutional research data repository, at https://datacompass.lshtm.ac.uk/.