Abstract
Objective
Giant cell arteritis (GCA) is a rare granulomatous vasculitis, affecting medium and large vessels, usually in old patients. The incidence of GCA has been higher during current COVID-19 pandemia and COVID-19 is recognized for its immune dysregulation. Lower limbs involvement is uncommon but can be limb threatening, resulting in limb loss.
Method
A 43-year-old man presented with a sudden pain in his right calf and foot associated with pallor and hypothermia, and there was objective evidence of ischemia. Symptoms began few days after he received the first dose of a COVID-19 mRNA vaccine and COVID-19 asymptomatic infection 20 days after vaccination. He had no history of any signs of claudication pre-COVID or limb trauma and was very fit.
Enhanced computed tomography and magnetic resonance imaging (MRI)suggest diagnosis of popliteal artery cystic adventitial disease. We resected the affected popliteal artery with interposition using a right great saphenous vein graft, through a posterior approach. On the fourth postoperative day, he was discharged.
Histopathological examination revealed patchy intramural inflammatory infiltrates composed of lymphocytes and rare multinucleated giant cells at the internal lamina and adventitia consistent with a diagnosis of GCA.
Conclusion and Result
Our case represents the first reported case of isolated popliteal GCA following vaccination with a COVID-19 mRNA vaccine and COVID-19 infection. We propose that the upregulated immune response to the vaccine acted as a trigger for GCA in this patient with predisposing risk factors and recurrent and repetitive microtrauma in popliteal fossa (the patient is a professional runner). Our case suggests the need for further studies about real world incidence of GCA associated vaccination and COVID-19 infection. Currently, data is limited regarding this relationship. We continue to encourage COVID-19 vaccination, even in elderly patients because the benefits of vaccination far outweigh any theoretical risk of immune dysregulation following administration.
Keywords: vaccine, immunization, covid-19, giant cell arteritis
Introduction
Giant cell arteritis (GCA) is a rare granulomatous vasculitis, affecting medium and large vessels, usually in patients older than 50 years.1 Giant cell arteritis should be considered as a systemic disease with extracranial involvement and complications.2 It has variable presentations, including fever, myalgias, headache, jaw claudication, and transient vision loss. It must be recognized promptly to prevent serious consequences,3 most notably irreversible vision loss.3 Lower limbs involvement is uncommon but can be limb-treatening, resulting in limb loss.4
The triggering events associated with GCA are not completely clarified, but literature data shows that the innate and adaptive immune systems play a significant role in the amplification of inflammatory pathways that lead to vessel inflammation, remodeling, and occlusion.5 The incidence of GCA has been higher during current COVID-19 pandemia. COVID-19 is recognized for its immune dysregulation. Interleukins seem to have a strong association with rheumatic diseases during the COVID-19 pandemic. For instance, interleukin-6 and interleukin-17 showed association with giant cell arteritis and arthritis among those infected with COVID-19.6
Many researchers reported COVID-19 triggering systemic vasculitis and giant cell arteritis, with variable and largely unmodifiable risk factors.7,8
We describe a case of successful treatment of an isolated popliteal artery affected by GCA after COVID-19 vaccination and subsequently COVID-19 infection.
Case
A 43-year-old man presented with a sudden pain in his right calf and foot associated with pallor and hypothermia; peripheral right left pulses were absent and there was objective evidence of ischemia. He started anticoagulation with low molecular weight heparin (LMWH) subcutaneously twice daily; however, his symptoms persisted and he was referred to our vascular department 2 days after. He had no history of any signs of claudication pre-COVID or limb trauma and was very fit and was a professional runner, but his maximum walking distance was approximately 20 m. On physical examination, the right popliteal, posterior tibial, and dorsalis pedis arteries were not palpable. The ankle-brachial index on the right leg was 0.30. No significant laboratory findings except for mild transaminitis. Symptoms began a few days after he received the first dose of a COVID-19 mRNA vaccine and COVID-19 asymptomatic infection 20 days after vaccination.
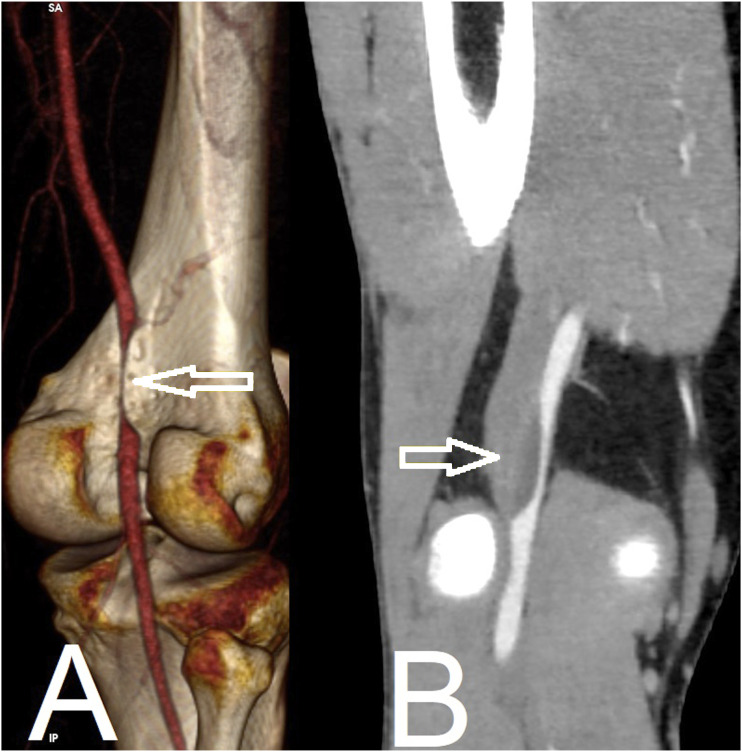
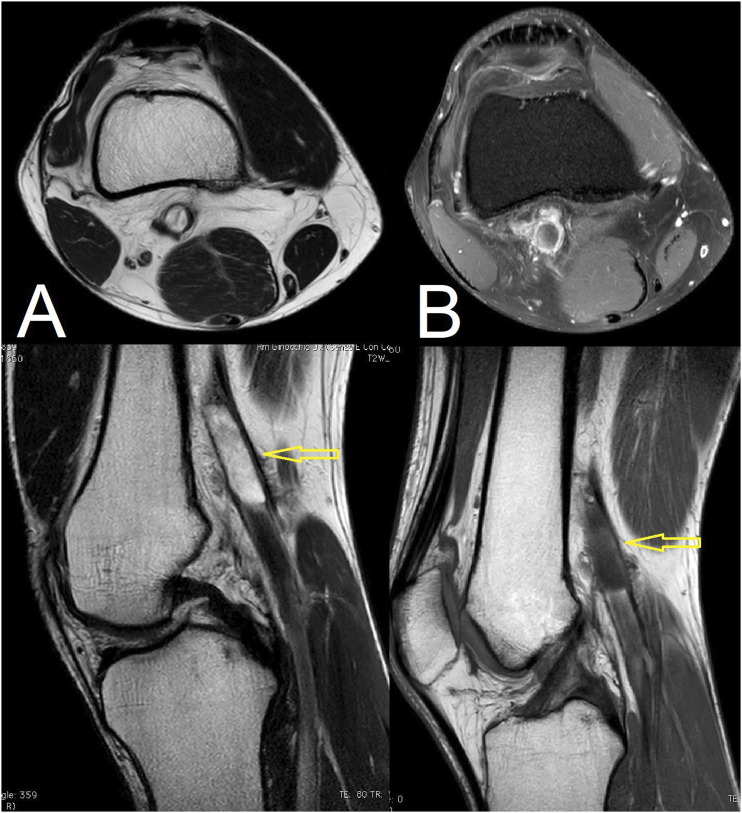
Enhanced computed tomography showed a sub-occlusion of the right popliteal artery with a 45-mm-long parietal cystic arterial lesion occupying the intravascular lumen, but preservation of arterial flow below the knee (Figure 1). No signs of arteriosclerosis were found in contralateral popliteal and aorto-iliac regions. Magnetic resonance imaging (MRI) proceeded in the axial and sagittal planes: T2-weighted imaging revealed a bi-loculated cystic mass with high signal intensity measuring 15 × 13 × 45 mm in the popliteal fossa of the right knee. A cystic mass was adjacent to and encircled the popliteal artery (Figure 2(a)). The cyst had a thin wall and no solid contents (Figure 2(b)).
Figure 1.
TC (A): 3D CT scan reconstruction shows the typical hourglass sign of popliteal artery (white arrow). (B): MPR CT reconstruction shows arterial lumen is encircled by cyst and laterally compressed (white arrow).
Figure 2.
A: T2-weighted magnetic resonance images. Multi-loculated, high-intensity cystic mass measuring 25 × 30 × 45 mm is located in right popliteal fossa, under: Sagittal view shows popliteal artery surrounded and compressed by cystic mass (white arrow). (B): T1-weighted magnetic resonance images. Multi-loculated, high-intensity cystic mass measuring 25 × 30 × 45 mm is located in right popliteal fossa, under: Sagittal view shows popliteal artery surrounded and compressed by cystic mass (white arrow).
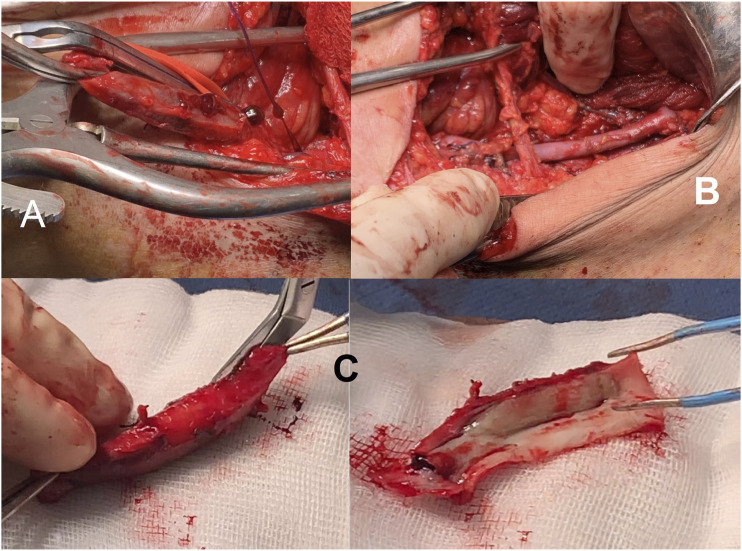
We decided upon surgical treatment. Under general anesthesia, in the prone position and through a posterior approach, the right popliteal artery was exposed. No popliteal arterial pulse was palpable below the knee. Patients received a heparin bolus of 100 IU/kg based on the real weight of body weight intravenously prior to cross-clamping and an additional dose of heparin was administered depending on the activated clotting time (ACT) (set at ≥ 200 s). We resected the affected popliteal artery with interposition using a right great saphenous vein graft (Figures 3). The operative time was 3 h 12 min, and blood loss was 90 mL. The ankle-brachial index after revascularization improved to 1.15 in the right leg, and the right posterior tibial and dorsalis pedis pulses became palpable. On the fourth postoperative day, he was discharged.
Figure 3.
Intra-operative findings and surgical specimen. (A): Popliteal artery surrounded by loculated lesion is laterally compressed and severely narrowed. (B): Segment of popliteal artery surrounded by lesion has been resected and reconstructed using interposing vein graft. (C): Surgical specimen comprising resected and longitudinally opened segment of popliteal artery with adjacent lesion.
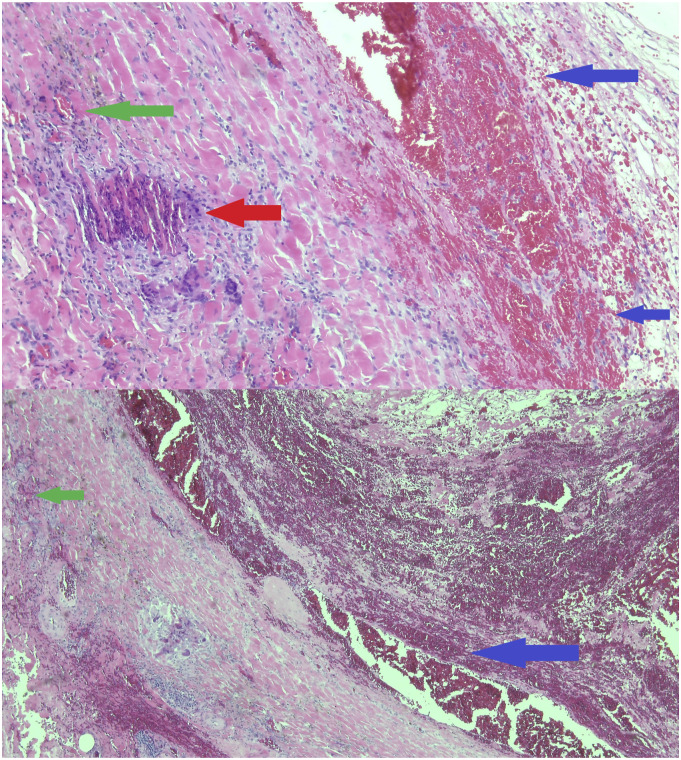
Histopathological examination revealed patchy intramural inflammatory infiltrates composed of lymphocytes and rare multinucleated giant cells at the internal lamina and adventitia (Figures 4) consistent with a diagnosis of GCA. Non-pharmacological treatment was recommended by rheumatologist. The patient has had no walking difficulties for 1 year since the operation.
Figure 4.
Microscopy with hematoxylin-eosin shows preparation shows irregular intimal thickening with area of luminal blockage with recanalization, with scarce lymphocytes in intima and media. Consistent with old lesion of giant cell arteritis, typical transmural mononuclear cell infiltration (green arrow), internal elastic lamina breakdown and intimal hyperplasia (blue arrow), and giant cells (red arrows).
Discussion
Extracranial vasculitis is a well-recognized feature of GCA. Data from literature revealed an incidence of extracranial GCA up to 83%.9,10
The SFA is the most common vessel affected in lower limb, often bilaterally.11 However, symptomatic lower limb GCA appears to be a rare entity, and it presents with claudication. Extracranial GCA was typically a circumferential involvement,10 but in our case presented with a loculated lesion, this finding could be due to particular anatomic and biomechanics zone (repetitive extension and hyperflexion of the knee). Giant cell arteritis should be considered, always, in patients with lower limb ischemia without significant atherosclerosis risk factors, even in the clinical absence of cranial GCA, especially because in some patients, large-vessel vasculitis may progress despite corticosteroids therapy.12 In these cases, indication for surgical treatment should be considered. Open surgery in the acute inflammatory phase should be avoided due to high risk of early thrombosis13 and balloon angioplasty with drug eluting devices may be useful for their anti-inflammatory effect.
Concerns have been raised about the relationship between vaccinations and autoimmune disease, including vasculitis. Vaccines could increase the innate immune response to foreign antigens, which cause concerns that they may induce reactivity to self-antigens.14 The COVID-19 mRNA vaccine has intrinsic adjuvant activity, which induces a strong innate immune response.15 Only 15 cases of GCA following influenza vaccination were reported in the literature.16 Schoenfeld et al. described varying autoimmune diseases after vaccination and coins the term autoimmune/inflammatory syndrome induced by adjuvants (ASIA syndrome) to describe a spectrum of immune dysregulation following vaccination.17 Although a small number of case reports have been published, no epidemiologic studies have shown a definitive increase in autoimmune disease following vaccination. Furthermore, data from literature suggest the association of COVID-19 and giant cell arteritis.18,19
Other viruses such as Varicella Zoster Parvovirus B19 and Epstein Barr have been suggested to trigger GCA.20 In addition, other vasculitis, such as Kawasaki and CNS vasculitis-like pattern, have been link to COVID-19,21 supporting our hypothesis.
Our case represents the first reported case of isolated popliteal GCA following vaccination with a COVID-19 mRNA vaccine and COVID-19 infection. We propose that the upregulated immune response to the vaccine acted as a trigger for GCA in this patient with predisposing risk factors and recurrent and repetitive microtrauma in popliteal fossa (the patient is a professional runner). However, causation cannot be reliably determined based solely on the timing of symptoms in this isolated case. Our case suggests the need for further studies about real world incidence of GCA associated vaccination and COVID-19 infection. Currently, data is limited regarding this relationship and it could just be a coincidence. We continue to encourage COVID-19 vaccination, even in elderly patients because the benefits of vaccination far outweigh any theoretical risk of immune dysregulation following administration.
Acknowledgments
Dr Stefano Fratoni and Professor Gian Franco Zannoni for accurate anatomo-pathological evaluation and diagnosis.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Statement of patient’s consent: Consent of patients regarding publication of his images or personal history was obtained.
ORCID iD
Roberto Gabrielli https://orcid.org/0000-0001-7192-5076
Referencies
- 1.Crowson CS, Matteson EL, Myasoedova E, et al. The lifetime risk of adult-onset rheumatoid arthritis and other inflammatory autoimmune rheumatic diseases. Arthritis Rheum 2011; 63: 633–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tatò F, Hoffmann U. Giant cell arteritis: a systemic vascular disease. Vasc Med 2008; 13: 127–140. [DOI] [PubMed] [Google Scholar]
- 3.Danesh-Meyer H, Savino PJ, Gamble GG. Poor prognosis of visual outcome after visual loss from giant cell0020arteritis. Ophthalmology 2005; 112: 1098–1103. [DOI] [PubMed] [Google Scholar]
- 4.Kermani TA, Matteson EL, Hunder GG, et al. Symptomatic lower extremity vasculitis in giant cell arteritis: a case series. J Rheumatol 2009; 36: 2277–2283. [DOI] [PubMed] [Google Scholar]
- 5.Terrades-Garcia N, Cid MC. Pathogenesis of giant-cell arteritis: how targeted therapies are influencing our understanding of the mechanisms involved. Rheumatology 2018; 57: 51–62. [DOI] [PubMed] [Google Scholar]
- 6.Manzo C, Castagna A, Ruotolo G. Can SARS-CoV-2 trigger relapse of polymyalgia rheumatica? Joint Bone Spine 2021; 88: 105150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riera-Martí N, Romaní J, Calvet J. SARS-CoV-2 infection triggering a giant cell arteritis. Med Clin 2021; 156: 253–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giollo A, Bixio R, Gatti D, et al. Challenge of diagnosing ANCA-associated vasculitis during COVID-19 pandemic: a missed ‘window of opportunity. Ann Rheum Dis. Published online August 19, 2020. [DOI] [PubMed]
- 9.Prieto-González S, Arguis P, García-Martínez A, et al. Large vessel involvement in biopsy-proven giant cell arteritis: prospective study in 40 newly diagnosed patients using CT angiography. Ann Rheum Dis 2012; 71: 1170–1176. [DOI] [PubMed] [Google Scholar]
- 10.Blockmans D, Ceuninck LD, Vanderschueren S, et al. Repetitive 18F-fluorodeoxyglucose positron emission tomography in giant cell arteritis: a prospective study of 35 patients. Arthritis Rheum 2006; 55: 131–137. [DOI] [PubMed] [Google Scholar]
- 11.Czihal M, Tato F, Rademacher A, et al. Involvement of the femoropopliteal arteries in giant cell arteritis: clinical and color duplex sonography. J Rheumatol 2012; 39: 314–321. [DOI] [PubMed] [Google Scholar]
- 12.Weyand CM, Goronzy JJ. Medium- and large-vessel vasculitis. N Engl J Med 2003; 349: 160–169. [DOI] [PubMed] [Google Scholar]
- 13.Joyce JW. The giant cell arteritides: diagnosis and the role of surgery. J Vasc Surg 1986; 3: 827–833. [DOI] [PubMed] [Google Scholar]
- 14.Perricone C, Colafrancesco S, Mazor RD, et al. Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) 2013: unveiling the pathogenic, clinical and diagnostic aspects. J Autoimmun 2013; 47: 1–16. [DOI] [PubMed] [Google Scholar]
- 15.Mulligan MJ, Lyke KE, Kitchin N, et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature 2020; 586: 589–593. [DOI] [PubMed] [Google Scholar]
- 16.Guimarães LE, Baker B, Perricone C, et al. Shoenfeld Y vaccines, adjuvants and autoimmunity. Pharmacol Res 2015; 100: 190–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shoenfeld Y, Agmon-Levin N. ‘ASIA’ - autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun 2011; 36: 4–8. [DOI] [PubMed] [Google Scholar]
- 18.Monti S, Delvino P, Bellis E, et al. Impact of delayed diagnoses at the time of COVID-19: increased rate of preventable bilateral blindness in giant cell arteritis. Ann Rheum Dis 2020; 79: 1658–1659. [DOI] [PubMed] [Google Scholar]
- 19.Jonathan GL, Scott FM, Matthew KD. A case of post-COVID-19-associated paracentral acute middle maculopathy and giant cell arteritis-like vasculitis. J Neuroophthalmol 2021; 41: 351–355. [DOI] [PubMed] [Google Scholar]
- 20.Ostrowski R.A., Metgud S., Tehrani R., et al. Varicella zoster virus in giant cell arteritis: a review of current medical literature. Neuroophthalmology 2019; 43: 159–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanafi R, Roger P-A, Perin B, et al. COVID-19 neurologic complication with CNS vasculitis-like pattern. Am J Neuroradiol 2020; 41: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]