Abstract
Introduction
Establishing a diagnosis in patients with olfactory disturbances has always been challenging for physicians.One reason for this is the rarity of some of the diseases that affect this sense, such as Kallmann's syndrome and post-viral olfactory loss.
Objective
To identify the major causes of olfactory disturbances and to describe the diagnostic evaluation in outpatients attended to at an ambulatory clinic specialized in olfaction disorders.
Methods
A retrospective analysis was performed in outpatients with primary olfactory complaint attended to between June 1, 2011 and September 30, 2013 in a center specialized in olfactory disorders. Patient history, nasofibroscopy, and the University of Pennsylvania Smell Identification Test (UPSIT) comprised the examination.
Results
Sixty-two patients were evaluated. The major causes were chronic rhinosinusitis (31%); rhinitis, primarily the allergic type (19%); post-viral olfactory loss (13%); and post-traumatic loss (8%). UPSIT scores were statistically different among different etiologies (p = 0.01).
Conclusions
The major diagnoses that should be part of the physician assessment when a patient complains of olfactory disturbance are chronic rhinosinusitis with and without polyps, allergic rhinitis, post-viral olfactory loss, and post-traumatic loss.
Keywords: Smell, Olfaction disorders, Diagnosis, Olfactory nerve injuries, Olfactory bulb
Resumo
Introdução
Estabelecer um diagnóstico em pacientes com distúrbios olfatórios foi sempre um desafio aos médicos. Uma das razões para isso é a raridade de algumas doenças que afetam esse sentido como a Síndrome de Kallmann e a perda olfatória pós-viral.
Objetivo
Identificar as principais causas das doenças olfatórias e descrever sua condução diagnóstica em um ambulatório direcionado a esses distúrbios.
Método
Análise retrospectiva de pacientes ambulatoriais com queixa olfatória primária atendida entre 1° de junho de 2011 e 30 de setembro de 2013 em centro especializado. História clínica, nasofibroscopia e o Teste de Identificação do Olfato da Universidade da Pensilvânia (UPSIT) compuseram a avaliação. Sempre que necessário, foram solicitadas tomografia de seios paranasais e ressonância magnética de crânio.
Resultados
Sessenta e dois pacientes foram avaliados. As causas mais comuns encontradas foram respectivamente: rinossinusite crônica (31%), rinites (19%), principalmente a rinite alérgica, perda olfatória pós-viral (13%) e pós-traumática (8%). As pontuações no UPSIT foram estatisticamente diferentes entre as cinco principais causas (p = 0,01).
Conclusões
Os principais diagnósticos que devem fazer parte na investigação médica diante de um paciente com queixa olfatória são: rinossinusite crônica com e sem polipose nasal, rinite alérgica, perda olfatória pós-viral e pós-traumática.
Palavras-chave: Olfato, Transtornos do olfato, Diagnóstico, Traumatismos do nervo olfatório, Bulbo olfatório
Introduction
Patients who complain of olfactory symptoms at the first consultation have always been a diagnostic and treatment challenge for physicians and especially for otolaryngologists. This is understandable, as there is scarce available knowledge of the diagnostic methods and treatments of these diseases, and they are are difficult to access.Despite significant decrease in the quality of life of patients with olfactory complaints, few centers in the world are exclusively dedicated to the management of this problem. In most medical practices and academic environments, there are no validated tools for precise definitions of the severity and etiology of these disorders. As a result, few studies have described the main causes and treatments of these conditions.1, 2, 3, 4
In a review of 750 patients with chemosensory complaints, Deems et al. observed that three categories represented 60% of the causes of these disorders: nasal-sinus disease, post-influenza olfactory loss, and olfactory loss following head trauma.1 Harris et al., in a sample of 1,000 patients, identified post-viral olfactory loss as the main etiology in the elderly and women, whereas post-traumatic loss was the main cause in patients younger than 20 years.2 In a retrospective study of 428 patients with primary olfactory complaints, the most common causes were head trauma (18%), post-viral loss 18%, and nasal-sinus disease (14%).4
The prevalence of qualitative changes such as parosmia (distorted olfactory perception) and phantosmia (olfactory perception in the absence of odor molecules) enriches the diagnostic possibilities. Approximately 40% of patients with hyposmia and/or anosmia present these disturbances. In Taiwan, in a study to determine the prevalence of olfactory disorders with 211 participants between 19 and 89 years, the frequency of olfactory dysfunction was 12.3% with an incidence of parosmia and phantosmia of 10% and 30.8%, respectively.5
The causes of olfactory dysfunction can be divided into conductive and sensorineural. The first occurs when there is airflow obstruction to the olfactory cleft, including chronic rhinosinusitis with polyps, septal deviation, rhinitis and tumors. In cases of post-viral olfactory loss or after brain injury or trauma, neural damage occurs. In some diseases, as chronic rhinosinusitis, both forms can be present.4, 6
The objective of the present study was to identify the main causes and describe the diagnostic procedures utilized in an outpatient clinic specialized in the management of patients with olfactory disorders.
Methods
This was a retrospective study conducted in ambulatory patients with primary olfactory complaints treated between June 1, 2011 and September 30, 2013 in a specialized center. Complete demographic data, medical history, nasal endoscopy, and the University of Pennsylvania Smell Identification Test (UPSIT) results were collected from all subjects. When necessary, paranasal sinus tomography and magnetic resonance imaging were requested. Patients who did not have olfactory dysfunction as the initial complaint were excluded. The retrospective nature of the study did not require the signing of the informed consent form as established by the local Research Ethics Committee.
History, physical examination and nasofibroscopy
During the investigation of olfactory complaint of the patients, the first focus was to identify deficits caused by nasal obstruction through nasal endoscopy and to evaluate the patency of the olfactory cleft. A second aspect of the investigation was directed toward identifying possible neuronal damage through the history, consisting of questions on reports of head trauma, prior use of olfactory-toxic medications, upper respiratory infections, and other systemic comorbidities (Table 1, Table 2).
Table 1.
Anamnesis questions.
| General information: name, age, gender, ethnicity, occupation, monthly income, educational level |
|---|
| Unilateral or bilateral loss? |
| Previous nasal surgeries performed |
| Personal history |
| Smoker or ex-smoker? How many cigarettes a day? |
| Do you have difficulty feeling the taste of things? |
| Current medications |
| Did your loss begin after medication use? |
| Exposure to toxic agents to the olfactory system (aminoglycosides, alcohol, formaldehyde, inhalation drugs, sulfur dioxide, carbon monoxide, acrylates, and methacrylates) |
| Did your loss begin after a cold or the flu? |
| If it begined after a cold or flu, how many days after did it begin? |
| History of head trauma? |
| Did you loose your sense of smell after a trauma to the head? |
| Previous nasal disease diagnosed by a physician? |
| Neurological diseases: Parkinson's, Alzheimer's, epilepsy, stroke, severe memory disorder. |
| Previous treatment of olfactory disorder? |
| Olfactory symptoms followed by seizure? |
| Duration or alteration of olfactory loss |
Table 2.
Examinations performed.
| Type of examination | Indications |
|---|---|
| General: oroscopy, anterior rhinoscopy, otoscopy. | All |
| Nasofibroscopy (focus on the olfactory fossa) | All |
| Alcohol test | All |
| Mini-mental state examination | Patients older than 65 years |
| UPSIT | All |
| Laboratory tests (levels of vitamin B12, TSH, free T4, AST, ALT, GGT, full coagulation test, urea, creatinine, fasting glycemia) | When necessary |
| CT of the paranasal sinuses | Patients with chronic rhinosinusitis and olfactory fossa difficult to be visualized by endoscopy |
| Head MRI | Suspected central nervous system etiology for loss of smell and measure of olfatory bulbs |
University of Pennsylvania Smell Identification Test
The UPSIT (commercially known as Smell Identification TestTM, Sensonics, Inc. - Haddon Hts, NJ) is a smell assessment test used worldwide. The test can be self-administered and consists of forty microencapsulated odors that are inhaled after scraping the indicated strip (Fig. 1). Based on the score, it is possible to classify olfactory function of the individual as normosmia, microsmia, or anosmia. It was created by Doty et al.7 in 1984 and recently adapted for the Brazilian population by Fornazieri et al.8, 9 This is an easy-to-use method with adequate reliability, suitable for outpatient use.
Fig. 1.
Male patient undergoing smell identification test (SIT) with booklet positioned at 1 cm from the nose.
Established treatments
The main treatments used in our clinic are described in Table 3.
Table 3.
Main established treatments.
| Treatment | Indications | Posology |
|---|---|---|
| Oral corticoid therapy | Rhinosinusitis, idiopathic | prednisolone 40 mg for 7 days, 20 mg for 7 days, and 10 mg for 7 days |
| Budesonide nasal wash | Rhinosinusitis, idiopathic | 0.5 mg of budesonide per day |
| Alpha lipoic acid | Post-viral, idiopathic | 300 mg 2×/day for 1 month |
| Olfactory training with cloves, rose-scented perfume, eucalyptus and lemon. | Post-viral, post-trauma, idiopathic | 10 seconds every substance 2 × day |
Recommendations to patients
Regardless of the cause of the olfactory loss, patients were instructed to adapt certain everyday practices. The loss of smell often prevents patients from identifying proper food conservation, thus causing accidental ingestion of spoiled foods, with unfavorable consequences to their health. Patients were instructed to frequently assess the quality of the food they ingest and to have a family member at meal times in order to aid with this process. The addition of spicy condiments, such as herbs, vinegar, or lemon, as well as more acid flavors, can improve the pleasure of tasting some foods. Patients with proven olfactory deficit were discouraged from cooking or handling appliances that use gas without the presence of a family member with an intact sense of smell. The risk of serious accidents due to gas leak is emphasized.10
Statistical analysis
Statistical analysis was performed with SPSS 22.0 (SPSS Inc - Chicago, Ill., USA) software. The normality of data distribution was assessed by Shapiro-Wilk's test, and the homogeneity of variances was assessed by Bartlett's test. Afterwards, analysis of variance (ANOVA) and Tukey's and Scheffe multiple comparison tests were used to compare the UPSIT score among the studied diseases. Comparison of the proportions of certain variables among patients with different diagnoses was performed by Fisher's exact test. Multiple linear regression was used to assess the association of the dependent variable “UPSIT score” with age, gender, educational level (more than eight or less than eight years of study), ethnicity (white or non-white), olfactory loss underlying disease, and duration of the problem.
Results
A total of 62 patients with primary complaints of olfactory disorder were evaluated. The demographic characteristics of the study population are described in Table 4.
Table 4.
Demographic characteristics of the study population.
| Variable | Category | n (%) |
|---|---|---|
| Gender | Male | 31 (50%) |
| Female | 31 (50%) | |
| Age (years) | 44.2 ± 19.4 | |
| Smoking | 8 (13%) | |
| Ethnicity | White | 39 (63%) |
| Non-white | 23 (37%) |
Most common causes
The most common causes found were: chronic rhinosinusitis (31%), rhinitis (mainly allergic rhinitis; 19%), and post-viral (13%) and post-traumatic olfactory loss (8%) (Table 5). Among the other causes, two patients had schizotypal personality, three had olfactory loss following use of medications (two reported frequent use of topical vasoconstrictors and olfactory deficits after hospitalization with intravenous antibiotic treatment), one patient had anosmia after influenza vaccine, and one patient presented olfactory loss after endonasal pituitary surgery. One patient had airflow-dependent phantosmia in the right nasal cavity and continuously used adhesive tape to block the ipsilateral nostril for symptom control.
Table 5.
Etiology of olfactory complaints and mean score at the University of Pennsylvania Smell Identification Test (UPSIT).
| Etiology | n | Percentage | Mean UPSIT score | SD |
|---|---|---|---|---|
| Chronic rhinosinusitis with nasal polyps | 11 | 18% | 22 | 9.9 |
| Chronic rhinosinusitis without nasal polyps | 8 | 13% | 26.4 | 6.5 |
| Post-viral infection loss | 8 | 13% | 14.6 | 6.9 |
| Olfactory loss after head trauma | 5 | 8% | 13.8 | 4.6 |
| Rhinitis | 12 | 19% | 27 | 8.1 |
| Other causes | 18 | 29% | 16.7 | 9.8 |
| Total | 62 | 100% | 20.6 | 9.2 |
SD, standard deviation; n, number of patients.
Olfactory test scores
Scores in the UPSIT were statistically different among the five leading causes (p = 0.01). The mean score in patients with rhinitis (27 ± 8.1) was significantly higher when compared to patients with head trauma (13.8 ± 4.6; p = 0.04).
Influence of variables on the olfactory test
The mean age of patients with each disease were: chronic rhinosinusitis, 47.1 ± 17.1 years; post-viral olfactory loss, 57.6 ± 16.5, post-trauma olfactory loss, 47.5 ± 19.3; and rhinitis, 31.8 ± 20.1. There was no statistically significant difference among them (p = 0.06), but there was a trend towards older age in patients with post-viral olfactory loss (Fig. 2).
Fig. 2.
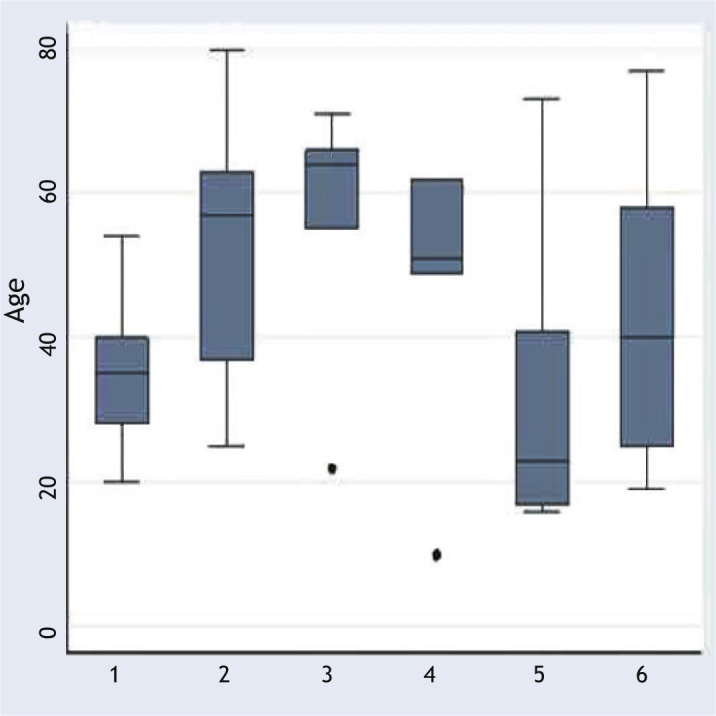
Boxplot of age range of individuals divided by etiology. Chronic rhinosinusitis without (1) and with(2) nasal polyps, post-viral(3), post-trauma(4), rhinitis (5) and other causes (6).
No difference was observed between the proportions of males and females in the groups (p = 0.26).
The multivariate analysis showed no association of age (p = 0.36), gender (p = 0.57), ethnicity (p = 0.59), educational level (p = 0.4), etiology of olfactory loss (p = 0.9), and duration of the olfactory disorder (p = 0.77) with UPSIT scores.
Discussion
The main causes of olfactory loss were similar to those found in previous studies: nasal-sinus disease, post-viral, and post-traumatic olfactory loss.1, 2, 4, 11 Emphasis should be given to nasal and paranasal sinus disease; together, they accounted for over 50% of patients. This information helps guide the initial diagnostic procedure, by focusing the history on the signs and symptoms of rhinosinusitis and other nasal obstructive diseases.
As expected, the scores between the different etiologies were different. The post-hoc analysis identified a difference in scores between patients with rhinitis, who had significantly higher scores than those with post-traumatic head trauma disorder. It is believed that patients with prior head trauma loose the sense of smell both due to rupture of olfactory fibers along the cribriform plate, as well as the improper posterior healing of the nasal mucosa, preventing the penetration of regenerated bipolar olfactory neurons.12
Causes for olfactory loss that are easily treated can be readily recognized and removed; cessation of the use of drugs that can damage the olfactory epithelium and septal defects that prevent the arrival of odors to the nasal roof are one example. In this series, three patients reported olfactory loss after drug use. However, the confirmation of this etiology is a complex process, and many studies are still needed, with animal models, in order to demonstrate the deleterious effect of topical and systemic medications on olfaction.
Although no differences were observed between the age ranges in the groups with different etiologies, there was a trend towards older age in patients with post-viral olfactory loss. Studies have shown that post-viral olfactory loss is more common in women and typically over 50 years.1, 13 The reason for this fact is unclear. Colds are more common in women, particularly between 20 and 30 years, which may reflect greater contact with children in this age group. Conversely, colds are less common in patients over 60 years, who experience an average of one per year.13 Of the eight patients analyzed, six were females, confirming the trend of a higher proportion of this gender. A larger sample of patients would probably statistically confirm these two findings, as observed in previous studies.1, 14
A decreased sense of smell is associated with advancing age, and has been well documented after the sixth decade of life.6 Gradually, olfactory bulb degeneration occurs and there is an exchange of olfactory by respiratory epithelium, caused by continuous metaplasia.15 This fact results from the accumulation of injuries that decrease the capacity of olfactory tissue to regenerate. It occurs partially through the natural aging process, surgical trauma, malnutrition, or cumulative exposure to toxic agents throughout life.16 Unfortunately, the elderly rarely seek medical help for olfactory symptoms, either due to acceptance of their situation with older age or not realizing that an abnormal condition is developing.
The lack of influence of age, sex, ethnicity, education, etiology and duration of olfactory disorder on odor identification ability that was observed in the present study is explained by the fact that most individuals had a score of less than 19 points, which is considered anosmia.17 This score can be achieved by chance, with the analyzed variables having no influence on the olfactory evaluation, as shown in previous studies.8, 18 The relatively low number of individuals may also have been a limiting factor for greater accuracy of this analysis.
It is important to emphasize that patients with olfactory loss treated at this clinic showed exemplary adherence to appointments and follow-up. As their quality of life was impaired by the olfactory deficit, they had a clear desire to improve and made this very clear at each appointment. Regarding treatment, the present data are still limited and a longer follow-up is needed for more accurate inferences.
Although etiology is identified as a prognostic factor by physicians,2, 19 this finding has not been confirmed in the literature.18 Further studies with large, multicenter samples, as well as monitoring of patients are needed in order to confirm the association of the cause of olfactory loss with its best or worse clinical outcome.
Conclusion
The main diagnoses that should be taken into account by the physician when treating a patient with olfactory complaints are chronic rhinosinusitis with and without nasal polyps, allergic rhinitis, post-viral, and post-traumatic olfactory loss.
Conflict of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Fornazieri MA, Borges BBP, Bezerra TFP, Pinna FR, Voegels RL. Main causes and diagnostic evaluation in patients with primary complaint of olfactory disturbances. Braz J Otorhinolaryngol. 2014;80:202-7.
References
- 1.Deems D.A., Doty R.L., Settle R.G., Moore-Gillon V., Shaman P., Mester A.F., et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg. 1991;117:519–528. doi: 10.1001/archotol.1991.01870170065015. [DOI] [PubMed] [Google Scholar]
- 2.Harris R., Davidson T.M., Murphy C., Gilbert P.E., Chen M. Clinical evaluation and symptoms of chemosensory impairment: one thousand consecutive cases from the Nasal Dysfunction Clinic in San Diego. Am J Rhinol. 2006;20:101–108. [PubMed] [Google Scholar]
- 3.Nordin S., Murphy C., Davidson T.M., Quiñonez C., Jalowayski A.A., Ellison D.W. Prevalence and assessment of qualitative olfactory dysfunction in different age groups. Laryngoscope. 1996;106:739–744. doi: 10.1097/00005537-199606000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Seiden A.M., Duncan H.J. The diagnosis of a conductive olfactory loss. Laryngoscope. 2001;111:9–14. doi: 10.1097/00005537-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Lin S.H., Chu S.T., Yuan B.C., Suh C.H. Survey of the frequency of olfactory dysfunction in Taiwan. J Chin Med Assoc. 2009;72:68–71. doi: 10.1016/S1726-4901(09)70025-5. [DOI] [PubMed] [Google Scholar]
- 6.Wrobel B.B., Leopold D.A. Clinical assessment of patients with smell and taste disorders. Otolaryngol Clin North Am. 2004;37:1127–1142. doi: 10.1016/j.otc.2004.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doty R.L., Shaman P., Dann M. Development of the University of Pennsylvania Smell Identification Test: A standardized microencapsulated test of olfactory function. Physiol Behav (Monograph). 1984;32:489–502. doi: 10.1016/0031-9384(84)90269-5. [DOI] [PubMed] [Google Scholar]
- 8.Fornazieri M.A., Doty R.L., Santos C.A., Bezerra T.F., Pinna F.R., Voegels R.L. A New Cultural Adaptation of the University of Pennsylvania Smell Identification Test. Clinics (São Paulo). 2013;68:65–68. doi: 10.6061/clinics/2013(01)OA10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fornazieri M.A., Pinna F., de R., Bezerra T.F., Antunes M.B., Voegels R.L. Applicability of the University of Pennsylvania Smell Identification Test (SIT) in Brazilians: pilot study. Braz J Otorhinolaryngol. 2010;76:695–699. doi: 10.1590/S1808-86942010000600004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Souder E., Youder L. Olfaction: the neglected sense. J Neurosci Nurs. 1992;24:273–280. doi: 10.1097/01376517-199210000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Seiden A. In: Smell and Taste Disorders. Seiden A., editor. Thieme; New York: 1997. Olfactory loss secondary to nasal and sinus pathology; pp. 52–71. [Google Scholar]
- 12.Hawkes C.H., Doty R.L. Cambridge University Press; Cambridge: 2009. The Neurology of Olfaction; p. 244. [Google Scholar]
- 13.Seinden A.M. Postviral olfactory loss. Otolaryngol Clin North Am. 2004;37:1159–1166. doi: 10.1016/j.otc.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Seo B.S., Lee H.J., Mo J.H., Lee C.H., Rhee C.S., Kim J.W. Treatment of postviral olfactory loss with glucocorticoids. Ginkgo biloba, and mometasone nasal spray. Arch Otolaryngol Head Neck Surg. 2009;135:1000–1004. doi: 10.1001/archoto.2009.141. [DOI] [PubMed] [Google Scholar]
- 15.Doty R.L., Shaman P., Applebaum S.L., Giberson R., Siksorski L., Rosenberg L. Smell identification ability: changes with age. Science. 1984;226:1441–1443. doi: 10.1126/science.6505700. [DOI] [PubMed] [Google Scholar]
- 16.Seiberling K.A., Conley D.B. Aging and olfactory and taste function. Otolaryngol Clin North Am. 2004;37:1209–1228. doi: 10.1016/j.otc.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 17.Doty R.L. Sensonics, Inc; Haddon Heights, New Jersey: 1995. The Smell Identification TestTM Administration Manual. [Google Scholar]
- 18.London B., Nabet B., Fisher A.R., White B., Sammel M.D., Doty R.L. Predictors of prognosis in patients with olfactory disturbance. Ann Neurol. 2008;63:159–166. doi: 10.1002/ana.21293. [DOI] [PubMed] [Google Scholar]
- 19.Davidson T.M., Murphy C., Jalowayski A.A. Smell impairment. Can it be reversed? Postgrad Med. 1995;98:107–109. 112-8. [PubMed] [Google Scholar]


