Abstract
Objective
Medical care and weight related experiences have been challenged by the coronavirus disease 2019 (COVID‐19) pandemic for those living with obesity. The magnitude of this impact requires further attention in order to optimize patient care and outcomes. The aim of this study was to assess the impact of the COVID‐19 pandemic and lockdown on access to, and experience of, medical care, weight gain and management strategies, as well as predictors of weight gain.
Methods
An online survey (June–October 2020) was conducted with two samples; one representative of Canadians living with overweight and obesity (n = 1089) and a second of individuals recruited through obesity clinical services or patient organizations (n = 980).
Results
Less than half of the total respondents thought that their providers were available for their medical care and most preferred in‐person appointments over telemedicine. Only one quarter were satisfied with their obesity care. Sixty percent of the respondents reported weight gain (on average 5.65 kilograms [kg] gained), with 39.0% gaining more than 5% of their body weight (10.2% gained more than 10%). Over half of the respondents experienced decreased motivation for healthy eating or exercise. One third experienced more frequent and greater food consumption. Although worsening sleep occurred in approximately 20%, there was no significant increase in smoking, alcohol, or cannabis use. Predictors of weight gain were younger patients, higher weight categories, those who struggled with obtaining medical care during the pandemic, as well as those who struggled with eating.
Conclusion
These results suggest that the COVID‐19 pandemic negatively impacted patient care for those living with overweight and obesity and was associated with weight gain and interfered with weight management strategies. Greater attention to personalized weight management and interventions that focus on the predictors of weight gain should be undertaken.
Keywords: COVID‐19 pandemic, obesity, weight gain, weight management
1. INTRODUCTION
Obesity is highly prevalent, seen in over 650 million, or 13% of individuals worldwide 1 ; including 26.8% 2 in Canada and 40%–44.8% 3 in the United States. Its incidence has tripled since 1975. 1 , 3 In addition, obesity increases the risk and response to infection. 4 Obesity is a risk factor for COVID‐19 infection with increased severity, Intensive Care Unit admissions, and death due to multiple factors including alterations in gut microbiota, decreased pulmonary capacity and reserve, hypercoagulabilty, and altered physiologic and immune responses. 5 , 6 , 7 , 8 , 9 This pandemic has led to disruption in normal activities might affect medical care and outcomes for those living with obesity.
The COVID‐19 pandemic has been linked to weight gain associated with stress related eating and has affected many different groups of individuals in a variety of ways. Between 19 and 24 February 2021, the American Psychological Association undertook a “Stress in America” survey of 3013 adults. 10 Weight gain in the general population was reported in 42% (average gain 13.2 kilograms [kg]) with 10% gaining more than 22 kg. Further, 67% reported sleep disturbances and 23% reported increased alcohol consumption to manage stress. Mulugeta et al. examined the weight changes in over 11,000 adults in Boston between 3 months prior to the onset of the pandemic and 3 months after the start of the lockdown. 11 At least 40% of the sample gained weight, with younger individuals and women gaining more than men (both in overall weight as well as >5% weight gain). The mean weight gain for those who increased weight during the pandemic was 3.41 kg (SD = 3.54; 95% CI = 3.29, 3.58) in men and 3.09 kg (SD = 3.08; 95% CI = 2.98, 3.19) in women. The disproportional impact of the COVID‐19 pandemic on women's weight may be explained due to female dominated areas of employment including hospitality, restaurants and retail which were more severely affected by the pandemic. Unhealthy weight gain during the COVID‐19 pandemic has also been associated with increased smoking and an increased sedentary lifestyle with diminished physical activity and formal exercise. 12 , 13
The effect of the pandemic further challenged those living with overweight and obesity. Increased stress, anxiety and loneliness resulted in disordered eating behaviors including stress eating and nocturnal eating contributing to weight gain during this pandemic. 14 , 15 , 16 , 17 , 18 Almandoz et al retrospectively reviewed 123 patients involved in specialized obesity medicine and community based bariatric surgical programs. 14 Approximately 70% of respondents reported through survey analysis to have increased difficulty in achieving their weight loss goals during the stay‐at‐home orders imposed by the pandemic. The inability to achieve healthy eating and stress eating was experienced by the majority of respondents and half engaged in stock piling food. Despite most patients cooking at home, healthy food choices were less frequent. The stay‐at‐home orders also impacted on decreased exercise time and intensity by approximately 50%. Evidence also suggests that the pandemic and lockdown has also resulted in increased substance use and sleep interference, possibly related to increased stress, stress eating and struggles with weight control. 19 , 20 In a longitudinal study the past experience of weight bias and stigma was associated with increased stress, depressive symptoms, binge eating, and maladaptive eating during the pandemic. 21
COVID‐19 has also impacted persons undergoing bariatric surgery. Many bariatric surgical programs were halted in an attempt to reduce the spread of COVID‐19 and free up resources for those infected. A review of 50 patients awaiting bariatric surgery revealed weight gain in 62% from March to June 2020 due to increased snacking, emotional eating, and intake of high sugar foods, fast food, and liquid calories. 22 As a result of many bariatric surgical program staff being redeployed, ongoing professional support was unable to be provided, which not only impacted upon patient care but also added emotional burden to staff (moral injury) due to their inability to provide the appropriate required care. 23
To further understand the psychosocial and behavioral impact of the pandemic on persons living with overweight and obesity (PWO) the E valuation of the P andemic on Obesity C are and Health (EPOCH) survey was conducted. This survey included a broad assessment of the pandemic on behavior, emotions, and psychosocial functioning. In this paper, the impact of the pandemic was reported on accessing medical care and medical support for obesity, self‐reported weight changes, specific weight management strategies including motivation, eating, substance use, activity and sleep and the predictors of weight gain during the lockdown.
This study evaluated the hypothesis that the COVID‐19 pandemic negatively impacted the clinical management of obesity by interfering with access to medical care resulting in weight gain due to challenges following healthy eating, motivation with exercise, and increased food consumption.
2. METHODS
2.1. Sample
EPOCH was an English only, online survey conducted between June 22 and 9 October 2020. It was disseminated via an email link through snowball sampling to medically supervised participants of obesity clinics/organizations throughout Canada and abroad: the clinical sample. It was distributed by Inet International (http://www.inet-international.com), an online consumer panel of approximately of 300,000 members, to representative Canadians: the survey sample.
2.2. Survey
The EPOCH survey included 154 questions. Demographics included age, gender, marital status, residence, self‐reported height and current weight, highest weight, lowest weight in past 6 months, weight gain in past 3 months, comorbidities, medication use, and history of bariatric surgery. For this study, information was collected on four aspects of living through the pandemic (see Table 1 for specific questions). These included the impact of the pandemic on accessing medical (virtual) care, weight management strategies and additional health behaviors (sleep, activity, and substance use), and weight changes. The survey also assessed psychological impact of the pandemic, including: attitudes to managing weight (Theoretical Domains Framework 24 ), the impact of social distancing on relationships and mental health indicators (General Anxiety Disorder Scale, 25 the Center for Epidemiology Studies Depression Scale, 26 the Perceived Weight Discrimination Scale, 27 the Vaccine Hesitancy Scale 28 and the Fear of Corona Virus Scale 29 ). These results will be published elsewhere. 30 Final questions asked about experiences about contracting COVID‐19. This study was reviewed and approved by Veritas Institutional Review Board review panel: 16576‐09:19:5811‐06‐2020.
TABLE 1.
Survey questions on medical care, weight and weight management strategies and additional health behaviours during the pandemic
| Items | |
|---|---|
| For all of the rating items (“to what extent”) respondents used a 7‐point Likert scale where 1 was not at all, 4 was moderately and 7 extremely. | |
| Scale | To what extent: |
| Impact of the pandemic on accessing medical care (virtual care) | Have you experienced struggles in getting medical attention during this pandemic? |
| Do you feel satisfied that you are getting adequate medical attention for your obesity during this pandemic? | |
| Are you more hesitant to seek medical attention during the COVID‐19 pandemic because of your obesity? | |
| Do you think your doctor of nurse practitioner, or any health care professional has been available for your care during this pandemic? | |
| Do you think you DID NOT receive the medical care you needed during this pandemic? | |
| Do you think that your health care practitioners DO NOT BELIEVE that treating YOUR OBESITY is important during this pandemic? | |
| Do you prefer telephone or video appointments over in person visits for your medical care during this pandemic? | |
| Do you feel telephone or video appointments are an advantage? | |
| Do you prefer video appointments to telephone appointments during this pandemic? | |
| How weight is being impacted through the pandemic | Did you regain weight in the last 3 months (yes/no)? |
| Please indicate your weight gain (lbs) | |
| To what extent has your desire for weight loss been affected by COVID‐19? | |
| To what extent has your thoughts about the need to lose weight increased as a result of the COVID‐19 pandemic? | |
| To what extent have your attempts to manage your weight been more difficult during COVID‐19? | |
| To what extent are you concerned about your current weight and body shape during this pandemic? | |
| Compared with other concerns in your life to what extent is your weight a concern for you during this pandemic? | |
| The impact of the pandemic on weight management strategies | Do you feel it is challenging to follow a healthy eating schedule during this pandemic? In follow up to this question respondents indicated whether or not the following issues were associated with struggling to eat healthily [lack of motivation; lack of caring about healthy eating; restricted access to shopping; shortage of food; change of routine; increased hunger and cravings; mood changes; increased costs; none] |
| Has your overall food consumption increased during this pandemic? | |
| Are you eating more frequently during this pandemic? | |
| Are you eating healthier during this pandemic compared with before? | |
| Has your consumption of [home cooked meals; pre‐made meals; pick up takeout; home delivery fast food] increased during this pandemic? | |
| The impact of the pandemic on additional health behaviors | How many minutes of physical activity are you doing per week? (Number) |
| To what extent have you struggled with motivation to do physical activity during this pandemic? | |
| How many hours per night on average do you sleep? (Number) | |
| Overall, to what extent has your sleep become worse due to the COVID‐19 pandemic? | |
| Overall, to what extent has your sleep become better due to the COVID‐19 pandemic? | |
| To what extent has your alcohol/cannabis/cigarette consumption increased during this pandemic? |
2.3. Data analyses
Descriptive analyses were used for data on access to medical care, weight changes, eating and health behaviors. To facilitate interpretation, the data from the rating scales was recategorized into high (scale scores 5–7) or low impact (scale scores 1–4). Further, survey versus clinical samples as well as weight category (overweight, Class 1, Class 2, Class 3) scores were compared using a two‐factor analysis of variance on raw scores for continuous data or chi‐square analyses for categorical data. To address compounding error rates, multivariate analyses of variance using all dependent measures were run. If significant, univariate analyses were conducted. Finally, a step‐wise regression analysis evaluated predictors of weight gain (Step 1: gender, age, BMI class, survey vs. clinical; Step 2: access to and satisfaction with medical care; Step 3: eating behaviors; Step 4: the experience of managing weight; Step 5: activity, sleep, and substance use).
3. RESULTS
3.1. Respondents
The survey was completed by 2078 respondents (Table 2), with 1098 from the survey group and 980 from the clinical group. The clinical group typically consisted of individuals in medical or surgical obesity treatment programs with or without the use of behavioral or pharmacological interventions. For the clinical group, a total of 2742 individuals accessed the survey. Of these, 248 (9.0%) did not complete the consent form, had a BMI less than 27 or did not provide gender information, and 1514 (55.2%) did not complete the full survey, leaving 980 (35.7% response rate) with complete data. Of survey responders, 6531 accessed the survey (the survey company was contracted to obtain at least 1000 respondents). Of these 4055 (62.1%) did not complete the consent, had a BMI less than 27 or did not provide gender information, and 1378 (21.1%) did not complete the full survey, leaving 1098 (16.8% response rate) with complete data. Survey respondents were older, more geographically representative of Canadians, and more balanced in gender than the clinical sample (ps < 0.001). The clinical sample had a higher BMI (49.5% BMI >40% and 70.3% BMI >35, p < 0.001). Finally, few survey respondents had bariatric surgery (2.6%); whereas 22.9% of the clinical sample had had bariatric surgery, and another 22.4% were waiting or considering surgery (vs. 1.8% for survey respondents; p < 0.001).
TABLE 2.
Demographic characteristics of the samples
| Clinical (N = 980) | Survey (N = 1098) | Significance (p value) | ||
|---|---|---|---|---|
| Gender | Male | 17.5% (170) | 49.8% (546) | p < 0.001 |
| Female | 82.5% (804) | 50.8% (550) | ||
| Age | 51.2 (11.8) | 58.6 (10.6) | p < 0.001 | |
| Marital status | Single/Separated/Divorced | 37.7% (351) | 37.8% (415) | ns |
| Married/Common Law | 61.5% (602) | 61.5% (675) | ||
| Location | British Columbia | 25.9% (412) | 10.2% (112) | p < 0.001 |
| Prairies | 4.1% (38) | 19.0% (215) | ||
| Ontario | 67.3% (627) | 34.3% (377) | ||
| Quebec | 0.6% (6) | 16.8% (185) | ||
| East/North | 2.0% (19) | 19.1% (209) | ||
| United States | 1.8% (37) | ‐‐‐‐ | ||
| Other a | 0.6% (12) | ‐‐‐‐‐ | ||
| Weight status | Overweight | 9.3% (91) | 9.4% (103) | p < 0.001 |
| Class 1 | 20.4% (200) | 56.0% (615) | ||
| Class 2 | 20.8% (204) | 19.5% (214) | ||
| Class 3 | 49.5% (485) | 15.1% (166) | ||
| Bariatric surgery | No surgery | 54.7% (536) | 95.5% (1049) | p < 0.001 |
| Had surgery | 22.9% (224) | 2.6% (29) | ||
| Waiting/Considering surgery | 22.4% (220) | 1.8% (20) | ||
South America and Europe.
3.2. Impact of the pandemic on access to medical care
Access to care data were analyzed in two ways. First, overall results were reported as the proportion of the sample scoring above four on the scale. Second, mean scores for samples (survey/clinical) and weight categories were compared using analyses of variance.
Figure 1 shows that from all respondents very few experienced difficulty accessing care (15.2%), were hesitant to seek medical care (13.1%), believed that the required care was not received (12.9%), or that providers de‐priorized obesity management during the pandemic (15.6%). Yet less than half of respondents (44.0%) thought providers were available for care and around one‐quarter (27.1%) were satisfied with the obesity care received. Regarding virtual care, less than half of respondents (42.3%) preferred the telehealth care; most (56.7%) preferred in‐person care. Approximately one‐half of the sample considered telehealth an advantage and only 31.7% preferred video to telephone contact.
FIGURE 1.
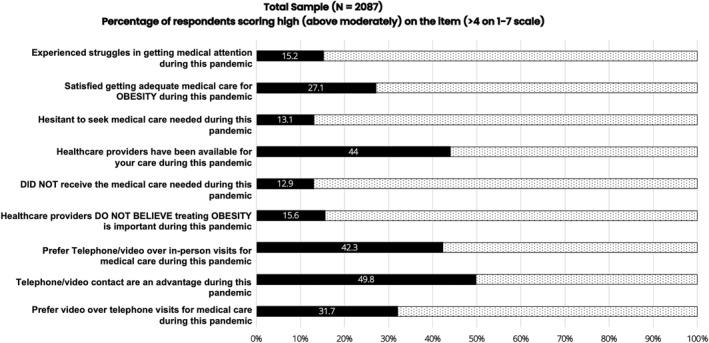
Access to care during pandemic
An initial two‐factor multivariate analysis of variance with all survey items as dependent measures yielded differences both between survey/clinical respondents (F = 14.12, p < 0.001) and different weight categories (F = 3.83, p < 0.001), justifying follow‐up univariate analyses.
Regarding struggling to get medical attention and believing that one did not get needed medical attention during the pandemic, there were no differences between survey/clinical samples, weight categories, and no interaction (all p's ns). Regarding the opinion that health care providers (HCPs) do not believe that treating obesity is important during the pandemic there were significant differences based on weight categories (F = 3.55, p = 0.014) but not survey/clinical samples (p ns). Those with Class 3 obesity more strongly believed HCPs did not think treating obesity was important (2.33) than those with overweight (1.92) or Class 1 obesity (1.95, p < 0.05).
Regarding the perception of medical care being available during the pandemic, survey respondents thought medical care was less available than the clinical respondents (3.58 vs. 4.22, F = 3.59, p = 0.013). Those with Class 2 and 3 obesity thought medical care was more available (4.05 and 4.18, respectively) than those with overweight or Class 1 obesity (3.46 and 3.66, respectively; F = 16.21, p < 0.001). A similar result occurred for satisfaction with care received. Survey respondents were less satisfied (2.00) than clinical respondents (3.42, F = 2.98, p = 0.03) and those with Class 3 obesity were more satisfied than all other BMI groups (F = 89.8, p < 0.001). Regarding hesitancy to seek care because of obesity, clinical respondents expressed greater hesitancy than survey respondents (2.42 vs. 1.88, p = 0.042) and those with Class 3 obesity reported greater hesitancy (2.72) than those with Class 2, Class 1 or overweight (2.16, 1.78, and 1.61, respectively, p < 0.001)
Regarding preference for telehealth over in‐person visits during the pandemic, clinical respondents had a stronger preference for telehealth than the survey sample. This was true for preference for telehealth over in‐person (4.46 vs. 3.87, p < 0.001), advantages of telehealth (4.81 vs. 4.25, p < 0.001) and preference for video over telephone contacts (3.88 vs. 3.29, p < 0.001). There were no differences in preference scores between the different weight category respondents on any of these items (ns).
3.3. Impact of the pandemic on weight
Sixty percent of the total sample reported weight gain over the past 3 months. The average weight gain for the entire 2078 respondents was 3.39 kg (SD = 4.36, range 0–31.82 kg). For those reporting gaining weight, mean weight gain was 5.66 kg (SD = 4.35; 42.3% gained 5% or more of their body weight, and 13.2% gained 10% or more). Further, for those gaining weight, females gained more weight (5.46 SD = 3.94 kg) than males (4.54 SD = 3.23 kg, p < 0.001). For females, 43.1% gained 5% or more (12.3% gained 10% or more) where 30.7% of males gained 5% or more (6.7% gained 10% or more; p < 0.001).
Figure 2 shows the risk of weight gain based on the sample (survey/clinical) and weight category. More clinical respondents reported gaining weight (64.6%) than survey respondents (55.9%, p < 0.001) and clinical, but not survey, respondents in the higher weight categories were more likely to report weight gain (67.6% of Class 2 and 70.3% of Class 3 vs. 48.4% of overweight and 55% of Class 1 respondents, p < 0.001).
FIGURE 2.
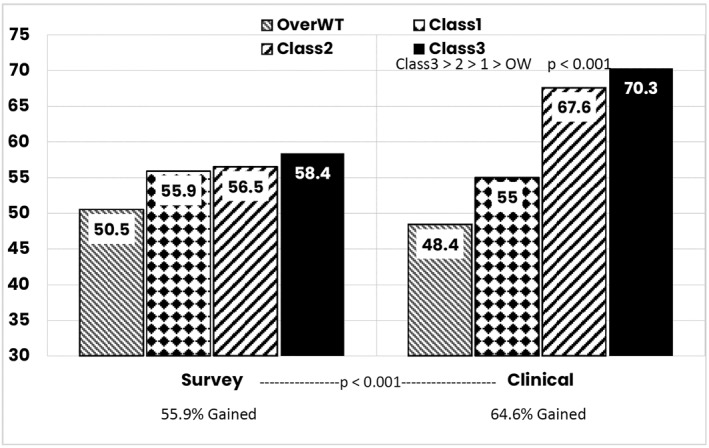
Person who report weight gain during pandemic
Comparing the amount of weight gained based on sample (survey/clinical) and weight category indicated no significant difference in weight gain between survey and clinical respondents (F = 1.06, ns) and no interaction between sample and weight category (F = 0.893, ns). However, more weight gain occurred in the higher weight categories (F = 30.05, p < 0.001); those with Class 3 gained 4.83 (SD = 5.50) compared to 3.28 kg (SD = 3.95) for Class 2, 2.67 kg (SD = 3.46) for Class 1 and 1.79 kg (SD = 2.64) for those with overweight. Further, 30.3% of those with Class 3 obesity gained 5% or more of their body weight over 3 months compared to 25.9.% of Class 2, 23.5% of Class 1 and 15.0% of those overweight (p < 0.001).
3.4. Impact of the pandemic on weight management behaviors
3.4.1. Eating experiences and weight management strategies
Regarding weight and eating experiences, 55.7% of respondents reported being concerned about their current weight and 57.9% reported that weight was a more important concern than other issues in their lives. Further, 44.7% reported that managing weight was more difficult during the pandemic, 29.6% reported that their desire for weight loss was affected by the pandemic and 35.1% reported increased thoughts about needing to lose weight.
Overall, 51% of respondents struggled to follow a healthy eating plan. Further, 43.9% were quite concerned about their eating habits, 35.6% reported eating more frequently and 29% reported increased food consumption. Only 20% of the respondents reported eating healthier. Regarding food preparation, 57.4% reported preparing more home cooked meals whereas increases in premade meals (15.5%), take‐out meals (16%) and take out fast food (12.1%) were not common.
In a follow up question, respondents were asked about specific challenges with maintaining a healthy eating routine. Figure 3 shows that there were a number of challenges to healthy eating; only 5.4% reported no challenges. The most common challenges (pertaining to approximately 25% or more) were lack of motivation, lack of routine, issues associated with mood, food cravings and caring about healthy eating, as well as practical issues associated with restricted access to, and costs of, food.
FIGURE 3.
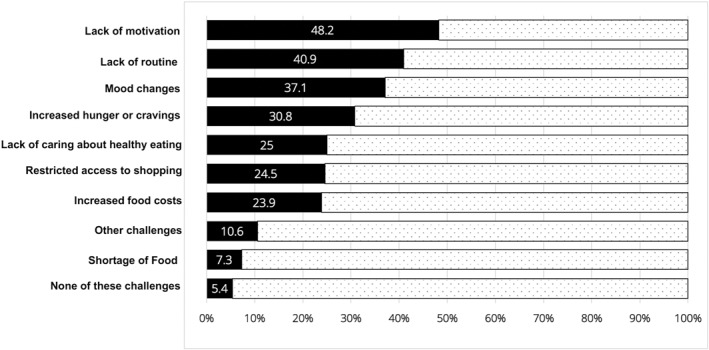
Pandemic impact of healthy eating
Apart from eating related experiences 52.4% of respondents reported struggling with motivation to exercise, 21.8% reported worsening sleep, whereas 7.7% reported improved sleep. Few respondents reported increased use of alcohol (10.4% of users), cannabis (17.0% of users) or cigarettes (27.1% of smokers) during the pandemic.
3.4.2. Weight categories and sample groups
To examine differences between survey and clinical respondents and between weight categories a two factor (survey vs. clinical; weight category) analyses of variance for continuous data (Chi square for categorical data) were conducted. An initial MANOVA was significant for survey type (F = 14.69, p < 0.001) and weight category (F = 4.02, p < 0.001).
Table 3 illustrates strong differences between survey and clinical respondents and between respondents in different weight categories. The clinical respondents scored higher on: concern about current weight (general concern as well as relative to other life issues); difficulty managing weight during the pandemic; challenges following a healthy eating plan; being concerned about eating habits; eating more frequently; and eating more food in general. Clinical respondents also reported being more likely to prepare home cooked meals. Regarding other health behaviors, clinical respondents reported spending more time in physical activity but also struggling more with motivation than survey respondents. There were no differences between groups in reported sleep time, but clinical respondents reported sleeping worse than survey respondents. No differences were found on measures of increased substance use.
TABLE 3.
Eating and self‐care during the pandemic
| Item (1–7 rating) | Survey sample (N = 1098) | Clinical sample (N = 980) | ANOVA results | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overweight | Class 1 | Class 2 | Class 3 | Mean | Overweight | C1 | Class 2 | Class 3 | Mean | S/C | Wt | S/C X Wt | |
| To what extent are you concerned about your current weight and body shape during this pandemic? | 3.65 | 4.08 | 4.39 | 4.69 | 4.19 | 4.49 | 5.06 | 5.44 | 5.79 | 5.45 | F = 102.2 p < 0.001 | F = 22.65 p < 0.001 | ns |
| Compared with other concerns in your life to what extent is your weight a concern for you during this pandemic? | 3.49 | 3.98 | 4.36 | 4.65 | 4.11 | 4.93 | 5.20 | 5.35 | 5.89 | 5.55 | F = 194.28 p < 0.001 | F = 24.68 p < 0.001 | ns |
| To what extent have your attempts to manage your weight been more difficult during COVID‐19? | 3.18 | 3.53 | 3.88 | 4.00 | 3.64 | 3.79 | 4.36 | 4.74 | 4.96 | 4.68 | F = 63.41 p < 0.001 | F = 15.72 p < 0.001 | ns |
| To what extent do you feel it is challenging to follow a healthy eating schedule during this pandemic? | 3.62 | 3.97 | 4.44 | 4.38 | 4.09 | 4.30 | 4.63 | 5.06 | 5.16 | 4.95 | F = 43.56 p < 0.001 | F = 12.33 p < 0.001 | ns |
| To what extent are you concerned about your eating habits during this pandemic? | 3.19 | 3.50 | 3.91 | 4.01 | 3.63 | 3.93 | 4.44 | 4.69 | 4.84 | 4.64 | F = 63.25 p < 0.001 | F = 11.75 p < 0.001 | ns |
| To what extent are you eating more frequently during this pandemic? | 3.07 | 3.22 | 3.39 | 3.36 | 3.26 | 3.71 | 3.83 | 4.03 | 4.12 | 4.00 | F = 41.97 p < 0.001 | ns | ns |
| To what extent has your overall food consumption increased during this pandemic? | 3.04 | 3.17 | 3.40 | 3.32 | 3.22 | 3.38 | 3.65 | 3.84 | 3.99 | 3.83 | F = 26.43 p < 0.008 | F = 4.06 p < 0.001 | ns |
| To what extent are you eating healthier during this pandemic compared with before the pandemic? | 3.21 | 3.14 | 3.33 | 3.04 | 3.17 | 3.31 | 3.24 | 3.24 | 3.20 | 3.23 | ns | ns | ns |
| To what extent has the consumption of home cooked meals increased during this pandemic? | 4.50 | 4.39 | 4.53 | 4.52 | 4.45 | 5.13 | 4.96 | 5.12 | 4.81 | 4.94 | F = 23.98 p < 0.001 | ns | ns |
| To what extent has the consumption of pre‐made meals increased during this pandemic? | 2.68 | 2.57 | 2.46 | 2.81 | 2.60 | 2.24 | 2.52 | 2.60 | 2.81 | 2.65 | ns | F = 3.24 p = 0.021 | |
| To what extent has the consumption of pick up takeout food increased during this pandemic? | 2.63 | 2.51 | 2.48 | 2.49 | 2.51 | 2.33 | 2.50 | 2.67 | 3.10 | 2.82 | ns | F = 3.11 p = 0.025 | F = 4.42 p = 0.004 |
| To what extent has the consumption of home delivery fast food increased during this pandemic? | 2.01 | 1.93 | 1.93 | 2.09 | 1.96 | 1.79 | 1.97 | 2.07 | 2.63 | 2.30 | ns | F = 6.73 p < 0.001 | F = 3.12 p = 0.025 |
| How many minutes of physical activity are you doing per week? | 146.8 | 137.1 | 105.2 | 92.1 | 124.9 | 188.5 | 165.3 | 151.5 | 103.9 | 134.3 | F = 16.67 p < 0.001 | F = 16.01 p < 0.001 | ns |
| To what extent have you struggled with motivation to do physical activity during the pandemic? | 3.59 | 3.90 | 4.51 | 4.73 | 4.12 | 4.15 | 4.51 | 5.19 | 5.44 | 5.08 | F = 36.60 p < 0.001 | F = 28.20 p < 0.001 | ns |
| How many hours per night on average do you sleep? | 6.92 | 6.91 | 6.79 | 6.62 | 6.84 | 6.62 | 6.78 | 6.77 | 6.58 | 6.67 | ns | F = 2.73 p = 0.042 | ns |
| OVERALL, to what extent has your sleep become WORSE due to the COVID‐19 pandemic? | 2.44 | 2.59 | 2.78 | 3.10 | 2.69 | 2.98 | 2.72 | 3.04 | 3.31 | 3.10 | F = 7.78 p = 0.005 | F = 8.17 p < 0.001 | ns |
| OVERALL, to what extent has your sleep become BETTER due to the COVID‐19 pandemic? | 2.29 | 2.05 | 2.00 | 1.78 | 2.02 | 1.91 | 1.83 | 2.05 | 2.00 | 1.97 | ns | ns | F = 2.92 p = 0.033 |
| To what extent has your tobacco smoking increased during this pandemic (for smokers)? | 3.43 | 2.89 | 3.54 | 3.42 | 3.14 | 2.50 | 3.36 | 3.09 | 2.50 | 2.79 | ns | ns | ns |
| To what extent has your alcohol consumption increased during this pandemic (for drinkers)? | 2.15 | 2.24 | 2.20 | 2.27 | 2.23 | 2.33 | 2.49 | 2.60 | 2.11 | 2.33 | ns | ns | ns |
| To what extent has cannabis intake increased during this pandemic (for users)? | 2.21 | 2.32 | 3.35 | 2.51 | 2.51 | 2.26 | 2.54 | 2.87 | 2.55 | 2.59 | ns | F = 3.09, p = 0.27 | ns |
There were also differences between the different weight categories. First, considering weight and eating issues, those living with Class 2 or Class 3 obesity reported higher scores on a number of variables. Those living with Class 3 obesity scored higher than those with Class 2, who in turn scored higher than those in Class 1 and overweight (the latter were not different) on concerns about weight (both general and relative to other issues in life) and difficulty managing weight during the pandemic. Similarly, those in the higher weight categories reported more challenges in following a healthy eating plan, being concerned about eating habits, and eating more food in general. Those with Class 3 obesity were more likely to make use of pre‐made meals. Finally, clinical respondents with Class 3 obesity were more likely to use pick up and takeout food and fast‐food deliveries than others.
Regarding activity, those in the higher weight categories engaged in less activity and also reported greater struggles with motivation. The pattern of results here were consistent. Class 3 differed from Class 2 which differed from Class 1 and those overweight (the latter two not differing). The same pattern occurred for worsening sleep; those in higher weight categories reported worse sleep. Regarding substance use, there were no differences in tobacco or alcohol use, although those with Class 2 obesity increased cannabis use more than others.
The analysis of the data on the struggles experienced in following a healthy eating regimen during the pandemic between survey/clinical respondents, and respondents in different weight categories, yielded remarkably consistent results. When comparing the survey and clinical respondents, more clinical than survey respondents reported: lack of motivation (54.2% vs. 42.8%, p < 0.001), change of routine (53.5% vs. 29.6%, p < 0.001), mood issues (50.3% vs. 25.2%, p < 0.001), increased cravings or hunger (36.9% vs. 25.2%, p < 0.001), reduced caring about healthy eating (28.0% vs. 22.4%, p < 0.005), restricted access to shopping (32.1% vs. 18.2%, p < 0.001), food shortage (9.2% vs. 5.6%, p = 0.001) and other challenges (16.9% vs. 5.0%, p < 0.001). Fewer clinical than survey respondents reported no challenges to healthy eating (2.2% vs. 8.3%, p < 0.001).
Consistent results also occurred on comparison of weight categories. For the following experiences greater challenges were reported for those in the higher weight classes, with overweight and Class 1 scoring lower than Class 2 and especially Class 3 obesity: lack of motivation (34.0%, 43.4%, 53.1%, 55.1% for overweight, Class 1, Class 2, Class 3, p < 0.001), change of routine (37.1%, 33.5%, 43.8%, 49.3%, p < 0.001), mood changes (28.4%, 28.5%, 38.3%, 49.6%, p < 0.001), increased cravings or hunger (23.7%, 26.7%, 30.4%, 38.1%, p < 0.001), lack of caring about eating healthy (18.6%, 21.7%, 27.0%, 29.8%, p < 0.001), restricted access to shopping (19.1%, 19.1%, 25.6%, 33.0%, p < 0.001), increased costs (20.6%, 21.6%, 23.9%, 27.6%, p = 0.36), other challenges (8.2%, 8.5%, 13.6%, 12.1%, p = 0.013). The opposite pattern occurred for the item indexing no challenges experienced, where those living with Class 3 obesity reported lowest rate of endorsement (3.5%), followed by those living with Class 2 obesity (3.6%), Class 1 obesity (7.2%) and overweight (8.2%, p = 0.001).
3.4.3. Predictors of weight gain
Predictors of weight gain were evaluated using a step‐wise multiple regression model (demographics in Step 1, access to care in Step 2, eating behaviors in Step 3, managing weight in Step 4 and activity, sleep and substance use in Step 5). Results are shown in Table 4.
TABLE 4.
Predictors of weight gain during the pandemic
| Weight gain in past 3 months | ||
|---|---|---|
| p value | Beta | |
| Step 1—demographics | <0.001 | ‐‐‐ |
| Age | <0.001 | −0.108 |
| BMI category | 0.033 | 0.050 |
| Survey versus clinical sample | 0.012 | 0.064 |
| Step 2—medical care factors | <0.001 | ‐‐‐ |
| Struggled to get medical attention during pandemic | <0.001 | 0.120 |
| Extent more hesitant to seek medical attention | <0.001 | 0.159 |
| Satisfied getting adequate medical care for OBESITY during pandemic | 0.009 | −0.064 |
| Extent DID NOT get needed medical attention | 0.020 | −0.074 |
| Extent healthcare providers DO NOT BELIEVE treating OBESITY is important during pandemic | 0.001 | 0.079 |
| Step 3—Eating behaviors | <0.001 | ‐‐ |
| Extent to which food consumption increased | <0.001 | 0.235 |
| Extent to which eating more frequently | <0.001 | 0.137 |
| Extent to which eating more healthy | <0.001 | −0.070 |
| Step 4—Eating concerns | <0.001 | ‐‐‐ |
| Extent to which managing weight has been more difficult | <0.001 | 0.124 |
| Extent to which desire for weight loss has been affected by COVID‐19 | 0.012 | 063 |
| Step 5—Exercise, sleep and substance use | ns | |
A number of factors were associated with self‐reported weight gain over the past 3 months. First, clinical respondents gained more weight than survey respondents and those in the higher BMI weight categories gained more weight. Older respondents reported less weight gain. Novel results indicated that weight gain was associated with experiencing struggles in getting medical attention, being hesitant to seek medical care, and thinking that health care providers do not believe that treating obesity during the pandemic was important. Additionally, those satisfied with their medical care were less likely to report weight gain. Further, greater weight gain was associated with increased food consumption, increase frequency of eating and eating less healthily. Weight gain was also associated with experiencing greater difficulty with weight management and finding one's desire for weight loss impacted by the pandemic. Respondent's level of activity, sleep or alcohol variables were not related to weight gain in this analysis.
4. DISCUSSION
The results of the EPOCH survey suggest that those with obesity experience ambivalence about care that impacts weight gain. On the one hand, few respondents felt that the required medical care was not adequately provided, were hesitant or struggled to seek care during this pandemic. However, the majority of respondents considered health care professionals unavailable and were unsatisfied with medical obesity care during this pandemic. This may reflect a sense that non‐obesity care was priorized despite feeling that obesity was perceived by HCP to be important to treat during the pandemic. Of concern, is that those with higher BMIs felt that health care professionals did not prioritize obesity as an important condition to treat. This may highlight an area to which greater attention must be directed. Participation in weight management services (our clinical sample) did mitigate somewhat the degree of dissatisfaction in medical care and in hesitancy to seek care. Resources and perhaps a more structured approach to care may have accounted for this response.
Some studies report patient satisfaction with telemedicine 31 however, the majority of the respondents preferred in‐person care to telemedicine. Only one‐half of respondents perceived virtual care to be an advantage and video appointments were not preferable to telephone appointments, discounting the benefit of visual interactions with telemedicine and explaining the importance of the physical encounter preferred by the respondents. Often age is provided as an explanation for satisfaction with telemedicine, but a post hoc analysis of those under 45 found that the majority also prefer in‐person care (53.7%).
COVID‐19 has changed social norms, including working from home, limiting access to exercise facilities and restaurants, and preventing social gatherings. The impact of these factors on weight is critical for those with obesity. Studies show that there are strong impacts on dietary behaviors. 32 , 33 , 34 , 35 In this study, most respondents gained weight during this pandemic; for approximately 40% of respondents, weight gain was greater than 5% (13% gained more than 10%). This is not attributed to a lack of concern with body weight, the desire to lose weight, nor the recognition that their weight particularly during this pandemic is not a priority. Other factors, in particular, weight management behaviors, may be more significant determinants of weight gain. Clinical respondents, especially with higher BMIs, experienced greater challenges and struggles and may be more greatly affected by the changes that have occurred with this pandemic. This trend may worsen as the pandemic progresses.
Almost no one (<5%) reported having no challenges with healthy eating (only 20% maintained healthy eating during lockdown). Lack of motivation, mood changes, boredom and the challenges in establishing and maintaining a healthy eating routine have contributed to increased weight. Each new wave of the pandemic has proven to be disruptive to establishing routines. In the study sample, over half of respondents increased home cooking while many others, especially those of higher BMI's, utilized premade, take out or fast‐food meals. The economic consequences from this pandemic need to be considered, as 23.9% of the respondent's report cost as an impediment to healthy eating. Disinterest in healthy eating (48.2% report reduced motivation) may stem from a sense of distress (37.1% report mood changes) contributing to weight gain as well.
In individuals with higher BMI's, the increased vulnerabilities seen in this study include greater concerns about weight, increased difficulty in managing weight, more challenges to meal planning following a healthy eating plan, and concerns around their eating habits. This likely contributed to increase weight seen in this category. Interventions particularly directed to these behaviors might possibly counteract the observation seen.
Maintaining physical activity was challenging for respondents (52.4% struggled with motivation). This was greater for clinical respondents and those with higher BMIs. Interfering with physical activity is a truly unfortunate consequence of the pandemic. Stay at home orders might have unintentionally contributed to these findings. Sleep was similarly impacted, with clinical and higher BMI respondents sleeping worse, although sleep was not a predictor of weight gain. Of interest, there was very little reported increase in substance use, during the pandemic (only 6.1% scored above 4 for increased alcohol; 4% for increased smoking and 3.9% for increased cannabis) by respondents.
The results of this study reflect a significant risk for weight gain in people with overweight and obesity. This has significant health implications. Weight gain during the initial phases of the pandemic was related to an inability to access medical care and the perception that health care practitioners did not perceive the treatment of obesity a priority during this pandemic. This may elicit the perception of alienation for the patient. Less weight gain was seen in those individuals who were satisfied with their medical care and perceived increased focus on treating obesity during this pandemic. Weight gain was more prominent in those having difficulty with weight management, who were concerned about weight and shape, and in those where overeating occurred. This may be due to the multiple struggles and challenges delineated above. Physical activity, sleep and alcohol had no impact on predicting weight gain.
Although the clinical sample respondents reported better experiences with healthcare providers than the survey sample respondents, they were more likely to gain weight and struggled more with eating related behaviors. These results further emphasize the importance of providing support to individuals seeking care for their obesity. These factors do highlight the need that greater attention to personalized weight management and coping mechanisms should be implemented in order to minimize weight gain.
Limitations of this study include that it was a cross‐sectional self‐reported assessment during the first wave of the COVID‐19 pandemic. As there have been multiple waves it is not possible to comment on the ongoing effect that this has had on access to medical care of weight gain for people living with overweight and obesity. In addition, the impact of the pandemic continues and may alter specific weight management strategies and have ongoing psychological and social impact for individuals living with obesity. In individuals utilizing pharmacologic agents for weight loss, compliance or discontinuation of medications was not assessed, which may also have contributed to weight gain. The impact of job loss and economic difficulties were also not evaluated as a contributor to weight changes during the early pandemic. The study link for participation was circulated to both survey and clinical participants across obesity clinics/organizations in Canada and parts of the United States. The total number of individuals who received the invitation is unknown, limiting a report of the true response rate for the study. As well, the majority of the data (including all of the survey respondents) are Canadian, and a global generalization is not possible.
Among the strengths of this study include a large sample of individuals living with obesity and overweight for the general population as well as those involved in clinical settings dedicated to the care of obesity. Representation in the sample includes individuals in all BMI categories.
The COVID‐19 pandemic remains a significant challenge for those living with overweight and obesity. It has had devastating effects both in medical care as well as in the psychological and social domains studied within the EPOCH trial. Significant weight gain has occurred in the first wave of COVID‐19 and those with higher BMIs and those involved in clinical settings are the most vulnerable and significantly impacted. Further, health promotion and weight management initiatives addressing greater access to care, greater attention to the treatment of obesity, greater intervention regarding coping mechanisms and motivation for healthy eating are necessary. Health care providers may be more effective through enhancing practice, policies and research addressing the ongoing impact of the COVID‐19 pandemic on those living with overweight and obesity.
CONFLICT OF INTEREST
The authors have no relevant conflict of interest for this manuscript.
ACKNOWLEDGMENTS
We would like to acknowledge our medical colleagues who promoted the study within their clinical services. We would also like to acknowledge the respondents, who willingly completed this extensive survey.
Glazer SA, Vallis M. Weight gain, weight management and medical care for individuals living with overweight and obesity during the COVID‐19 pandemic (EPOCH Study). Obes Sci Pract. 2022;8(5):556‐568. 10.1002/osp4.591
REFERENCES
- 1. World Health Organization . Obesity and Overweight; 2018. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [Google Scholar]
- 2. Government of Canada SC . Overweight and Obese Adults; 2018. Published June 25, 2019. Accessed June 23, 2021. https://www150.statcan.gc.ca/n1/pub/82-625-x/2019001/article/00005-eng.htm [Google Scholar]
- 3. NCD Risk Factor Collaboration; 2017. http://www.ncdrisc.org/d-adiposity.html [Google Scholar]
- 4. Ghilotti F, Bellocco R, Ye W, Adami HO, Trolle Lagerros Y. Obesity and risk of infections: results from men and women in the Swedish National March Cohort. Int J Epidemiol. 2019;48(6):1783‐1794. 10.1093/ije/dyz129 [DOI] [PubMed] [Google Scholar]
- 5. Louie JK, Acosta M, Samuel MC, et al. A novel risk factor for a novel virus: obesity and 2009 pandemic influenza A (H1N1). Clin Infect Dis Off Publ Infect Dis Soc Am. 2011;52(3):301‐312. 10.1093/cid/ciq152 [DOI] [PubMed] [Google Scholar]
- 6. Fezeu L, Julia C, Henegar A, et al. Obesity is associated with higher risk of intensive care unit admission and death in influenza A (H1N1) patients: a systematic review and meta‐analysis. Obes Rev Off J Int Assoc Study Obes. 2011;12(8):653‐659. 10.1111/j.1467-789X.2011.00864.x [DOI] [PubMed] [Google Scholar]
- 7. Fuhrman C, Bonmarin I, Bitar D, et al. Adult intensive‐care patients with 2009 pandemic influenza A(H1N1) infection. Epidemiol Infect. Published online. 2010;139:1202‐1209. 10.1017/S0950268810002414 [DOI] [PubMed] [Google Scholar]
- 8. Demeulemeester F, de Punder K, van Heijningen M, van Doesburg F. Obesity as a risk factor for severe COVID‐19 and complications: a review. Cells. 2021;10(4):933. 10.3390/cells10040933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) requiring invasive mechanical ventilation. Obesity. 10.1002/oby.22831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. American Psychological Association . One Year on: Unhealthy Weight Gains, Increased Drinking Reported by Americans Coping with Pandemic Stress. Accessed September 2, 2021. https://www.apa.org/news/press/releases/2021/03/one‐year‐pandemic‐stress [Google Scholar]
- 11. Mulugeta W, Desalegn H, Solomon S. Impact of the COVID‐19 pandemic lockdown on weight status and factors associated with weight gain among adults in Massachusetts. Clin Obes. 2021;11(4):e12453. 10.1111/cob.12453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jia P, Zhang L, Yu W, et al. Impact of COVID‐19 lockdown on activity patterns and weight status among youths in China: the COVID‐19 Impact on Lifestyle Change Survey (COINLICS). Int J Obes. 2021;45(3):695‐699. 10.1038/s41366-020-00710-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Caputo EL, Reichert FF. Studies of physical activity and COVID‐19 during the pandemic: a scoping review. J Phys Act Health. 2020;17(12):1275‐1284. 10.1123/jpah.2020-0406 [DOI] [PubMed] [Google Scholar]
- 14. Almandoz JP, Xie L, Schellinger JN, et al. Impact of COVID‐19 stay‐at‐home orders on weight‐related behaviours among patients with obesity. Clin Obes. 2020;10(5):e12386. 10.1111/cob.12386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Marchitelli S, Mazza C, Lenzi A, Ricci E, Gnessi L, Roma P. Weight gain in a sample of patients affected by overweight/obesity with and without a psychiatric diagnosis during the Covid‐19 lockdown. Nutrients. 2020;12(11):E3525. 10.3390/nu12113525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pellegrini M, Ponzo V, Rosato R, et al. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID‐19 virus emergency. Nutrients. 2020;12(7):E2016. 10.3390/nu12072016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rotenberg KJ, Flood D. Loneliness, dysphoria, dietary restraint, and eating behavior. Int J Eat Disord. 1999;25(1):55‐64. [DOI] [PubMed] [Google Scholar]
- 18. Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: cross‐sectional & longitudinal analyses. Health Psychol. 2009;28(3):354‐363. 10.1037/a0014400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID‐19 pandemic—United States, June 24‐30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049‐1057. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Almandoz JP, Xie L, Schellinger JN, et al. Substance use, mental health and weight‐related behaviours during the COVID‐19 pandemic in people with obesity. Clin Obes. 2021;11(2):e12440. 10.1111/cob.12440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Puhl RM, Lessard LM, Larson N, Eisenberg ME, Neumark‐Stzainer D. Weight stigma as a predictor of distress and maladaptive eating behaviors during COVID‐19: longitudinal findings from the EAT study. Ann Behav Med. 2020;54(10):738‐746. 10.1093/abm/kaaa077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Naran V, Namous N, Eddy VJ, Le Guen CL, Sarwer DB, Soans RS. The effects of the COVID‐19 pandemic on patients with obesity undergoing bariatric care. Surg Obes Relat Dis. Published online May. 2021;27(21):S155000261‐S155017206. 10.1016/j.soard.2021.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Graham Y, Mahawar K, Riera M, et al. Emotional resilience and bariatric surgical teams: a priority in the pandemic. Obes Surg. 2021;31(4):1887‐1890. 10.1007/s11695-020-05083-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Huijg JM, Gebhardt WA, Crone MR, Dusseldorp E, Presseau J. Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement Sci. 2014;9:11. 10.1186/1748-5908-9-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD‐7. Arch Intern Med. 2006;166(10):1092‐1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 26. Radloff LS. The CES‐D Scale: a self‐report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385‐401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- 27. Hunger JM, Major B. Weight stigma mediates the association between BMI and self‐reported health. Health Psychol. 2015;34(2):172‐175. 10.1037/hea0000106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Luyten J, Bruyneel L, van Hoek AJ. Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine. 2019;37(18):2494‐2501. 10.1016/j.vaccine.2019.03.041 [DOI] [PubMed] [Google Scholar]
- 29. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID‐19 scale: development and initial validation. Int J Ment Health Addict. Published online March 27. 2020. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vallis M, Glazer S. Protecting individuals living with overweight and obesity: attitudes and concerns towards COVID‐19 vaccination in Canada. Obes Silver Spring Md. Published online March 28, 2021. 10.1002/oby.23182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ramaswamy A, Yu M, Drangsholt S, et al. Patient satisfaction with telemedicine during the COVID‐19 pandemic: Retrospective Cohort Study. J Med Internet Res. 2020;22(9):e20786. 10.2196/20786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID‐19 lockdown: an Italian survey. J Transl Med. 2020;18(1):229. 10.1186/s12967-020-02399-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rodríguez‐Pérez C, Molina‐Montes E, Verardo V, et al. Changes in dietary behaviours during the COVID‐19 outbreak confinement in the Spanish COVIDiet study. Nutrients. 2020;12(6):E1730. 10.3390/nu12061730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reyes‐Olavarría D, Latorre‐Román PÁ, Guzmán‐Guzmán IP, Jerez‐Mayorga D, Caamaño‐Navarrete F, Delgado‐Floody P. Positive and negative changes in food habits, physical activity patterns, and weight status during COVID‐19 confinement: associated factors in the Chilean population. Int J Environ Res Public Health. 2020;17(15):E5431. 10.3390/ijerph17155431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Keel PK, Gomez MM, Harris L, Kennedy GA, Ribeiro J, Joiner TE. Gaining The Quarantine 15: perceived versus observed weight changes in college students in the wake of COVID‐19. Int J Eat Disord. 2020;53(11):1801‐1808. 10.1002/eat.23375 [DOI] [PMC free article] [PubMed] [Google Scholar]


