Abstract
Background:
A challenge for evaluating alcohol treatment efficacy is determining what constitutes a “good” outcome or meaningful improvement. Abstinence at the end of treatment is an unambiguously good outcome; however, a focus on abstinence ignores the potential benefits of patients reducing their drinking to less problematic levels. Patients may be drinking at low risk levels at the end of treatment but may be high-functioning and impose few social costs. In this study, we estimate the relationship between drinking at the end of COMBINE treatment and subsequent health care costs with an emphasis on heavy and non-heavy drinking levels.
Methods:
Indicators of heavy drinking days (HDDs) (5+ drinks for men, 4+ for women) and non-heavy drinking days (non-HDDs) during the last 30 days of COMBINE treatment were constructed for 748 patients enrolled in the COMBINE Economic Study. Generalized linear models were used to model total costs following COMBINE treatment as a function of drinking indicators. Different model specifications analyzed alternative counts of HDDs (e.g., 1 HDD and 2–30 HDDs) and groups having both Both non-HDDs and HDDs.
Results:
Patients with HDDs had 66.3% (p<.01) higher health care costs than those who were abstinent. Having more than 2 HDDs was associated with the highest costs (76.1%, p<.01). Having non-HDDs was associated with costs less than or equal to abstainers’ costs. Patients with HDDs and non-HDDs had substantially lower HCCs (31.5% less than abstainers) than those with HDDs only (91.8% higher than abstainers) (p<.05).
Conclusions:
Having HDDs at the end of treatment is associated with higher costs. Patients who had Only HDDs at the end of treatment had worse subsequent outcomes than those who had Both non-HDDs and HDDs. These findings offer new context for evaluating treatment outcomes and provide new information on the association of drinking with consequences.
Keywords: Costs, Treatment, Low-risk, Heavy Drinking
BACKGROUND
A challenge for evaluating alcohol treatment efficacy is determining what constitutes a “good” outcome or meaningful improvement. Abstinence at the end of treatment is an unambiguously good outcome; however, a focus on abstinence ignores the potential benefits of patients reducing their drinking to less problematic levels (Sobell and Sobell, 2011; Marlatt 2002; Dawson et al., 2008; Mertens et al., 2012). Falk et al. (2010) compared heavy drinkers to non-heavy drinkers at the end of treatment in two randomized controlled trials of pharmacotherapy by assessing alternative post-treatment drinking outcomes (e.g., percentage of subjects with no heavy drinking days [HDDs], percent days abstinent, drinks per day and per drinking week) up through 1-year post treatment. They found that subjects with no HDDs at the end of COMBINE treatment had significantly lower levels of all drinking outcomes and fewer alcohol-related consequences than patients with HDDs. Similar drinking measures were evaluated by Kline-Simon et al. (2014) in an observational study of outpatients. They found higher subsequent health care utilization and costs for patients with heavy drinking immediately following treatment and little difference in costs between abstinence and low-risk drinking.
As we have noted elsewhere (Zarkin et al., 2010), looking at other outcomes in addition to alcohol use is important to understand the social impact of alcohol dependence and the benefits of alcohol treatment. Patients may be drinking at low risk levels at the end of treatment and even post-treatment, but they may function at high levels and impose few costs on themselves or others. Such patients may be relatively healthy and have fewer accidents and healthcare emergencies.
In this study, we estimate the relationship between drinking outcomes at the end of COMBINE treatment with subsequent health care costs (costs). We focus on HDDs (5+ drinks for men, 4+ for women) and non-heavy drinking days (non-HDDs) in the last 30 days of treatment. We examine costs during 1-year and 3-year periods following treatment. Our goal is to estimate how alcohol use at the end of treatment predicts future costs.
METHODS
Data
We used data from the COMBINE trial, which randomized 1,383 adult participants with alcohol dependence to 9 different combinations of 2 pharmacotherapies (Acamprosate and Naltrexone) and a combined behavioral intervention (CBI). All of the medication/placebo arms received medication management. The ninth arm provided only the combined behavioral intervention with no medication or placebo. Randomization took place within 11 treatment sites in the United States between 2001 and 2003, and participants were followed for 12 months after the end of COMBINE treatment. In addition to estimating the costs of COMBINE treatment, the COMBINE Economic Study collected social and economic outcomes from patients during the main COMBINE study and extended data collection for an additional 24 months (Bray et al., 2007).
The analysis sample used for the current study is based on the COMBINE Economic Study participants. Two of the original 11 sites chose not to participate in the Economic Study. Of the 991 participants who completed 16 weeks of treatment in those 9 sites, 792 chose to participate and completed a total of 6,138 interviews, including an interview at randomization and at the end of 16 weeks of trial treatment. This sample corresponds to the sample used in Zarkin et al. (2010). Interviews were conducted at weeks 16 (the end of the COMBINE treatment episode), 26, 52 and 68 (one year after the end of COMBINE treatment). Drinking data are only used from the Week 16 interview. Cost data used as the dependent variable in our analyses come from the subsequent interview weeks. Attrition within this group was limited.1 Moreover, there were relatively few missing data points because the data collection instruments were designed to capture outcomes since the previous interview. Although this approach to data collection increases the likelihood of recall bias, it has the advantage of removing intermittent missing information. We removed patients with inconsistent or incomplete data, primarily based on having gaps in drinking data at the end of COMBINE treatment. The remaining analysis sample size is 752 (95% of the eligible sample).
One of the strengths of this study is the quality of its measures. The data were collected using the Economic Form 90 instrument (Bray et al., 2007), which collected detailed daily alcohol use in standard drinking units using the Timeline Follow-back (TLFB) method (Sobell and Sobell, 1992). In the TLFB method, a trained clinician works with the patient to construct a calendar of infrequent life events, work schedules and other activities, and weekends and holidays that occurred during the period of interest. Patients are then prompted to reconstruct daily drinking and drinking habits that are informed by and consistent with these memory anchors. In addition, the instrument recorded outpatient and emergency room visits and inpatient nights for general health and behavioral health, and residential treatment nights for any substance use or mental health. These were all collected as total counts since a patient’s previous interview.
Measures
Our analysis focused on drinking occurring during the last 30 days of COMBINE treatment collected using TLFB. Each day in this period was defined as an HDD if 5 or more drinks for men or 4 or more drinks for women were consumed that day; a non-HDD if drinking was reported but at a quantity less than the HDD threshold; or a day with no drinking. To reflect overall drinking behaviors in the last 30 days of COMBINE treatment, we used these daily definitions to create several categorical variables. First, we created an indicator of whether a patient had 1 or more non-HDDs in the last 30 days of COMBINE treatment (Any non-HDDs) and an indicator of having 1 or more HDDs in the last 30 days of COMBINE treatment (Any HDDs). These two variables are not mutually exclusive as a patient may have had both non-HDDs and HDDs in the past 30 days. Following convention, we use these two indicators as the only drinking variables in our first statistical model with Abstinent as the excluded reference group. However, to better reflect distinct types of drinkers at the end of COMBINE, we combined these variables to create a categorical variable with mutually exclusive groups: those who (1) had Only non-HDDs, (2) had Only HDDs, (3) had Both non-HDDs and HDDs, or (4) were Abstinent (no non-HDDs and no HDDs). The first three categories are used in our second set of statistical models as indicator variables with the Abstinent group as the reference category.
Participants with different numbers of HDDs might have different subsequent costs. To test this, we created additional indicator variables by splitting the Any HDDs indicator into smaller categories based on the number of HDDs. We started by creating an indicator for each number of HDDs from 1 to 30. However, because of small cell sizes and a lack of variation in costs across the indicators, we settled on “Low” and “High” categories and analyzed 2 different thresholds: 1 HDD vs 2–30 HDDs and 1–2 HDDs vs 3–30 HDDs. When we investigated similar categories for non-HDDs, we found no substantial variation in outcomes by non-HDD categories and thus do not include them in our analyses. Using these Low and High indicators, we then created mutually exclusive categories that incorporated non-HDDs similar to those above except that the Low and High indicators were used instead of simply Any HDDs.
Costs were calculated using self-reported counts of visits to outpatient care and emergency departments, and nights in inpatient and residential treatment facilities for any reason (physical or behavioral health). These counts are aggregated across the interviews from weeks 26–68 and thus reflect all costs from the end of COMBINE treatment (beginning the day after the end of the 30-day drinking outcomes described above) through 12 months later. These units were multiplied by $US unit costs reported in Zarkin et al. (2010) and summed to produce a single total healthcare cost. As in Zarkin et al., costs were adjusted to 2007 dollars using the medical services consumer price index for health care. We analyzed 1-year and 3-year costs post-COMBINE. One-year costs are based on healthcare activity reported during the 12-month period following the last day of COMBINE treatment. We therefore do not include costs occurring during the COMBINE trial treatment, which may have been confounded by regular health care visits. Three-year costs include the 1-year costs but add costs that occurred throughout the remainder of the data collection period for the Economic Study, totaling 36 months following the end of COMBINE treatment.
Demographic covariates included in the models are gender, race/ethnicity, and age at the time of COMBINE enrollment. Other characteristics were indicators of unemployment and whether the participant was married. We also included indicators of whether participants had ever used marijuana, whether they had ever used illicit drugs not including marijuana, continuous years of education reported at the beginning of COMBINE, logged baseline costs reflecting the 4-month period prior to randomization, and physical and psychological health domain scores from the WHO Quality of Life Instrument (The WHOQOL Group, 1998). We controlled for the study site where the patient received combine treatment. Because there was some attrition over the 3 years of data collection, we included the number of days for which each patient reported their costs as a covariate in the 3 year cost models.
Statistical Model
Because costs have a positively skewed distribution, ordinary least squares (OLS) may yield biased and inefficient estimates. Two common solutions to this skewness are using OLS with log transformation of costs which yields a distribution more amenable to OLS assumptions (although a retransformation of estimates, “smearing,” is required to obtain correct estimates), and generalized linear models (GLM) with a log-link function. An advantage of the GLM specification is that it provides consistent estimates even in the face of heteroskedasticity (Manning and Mullahy, 2001). The appropriateness of one approach over the other depends on the exact shape of the distribution in terms of skewness, kurtosis, and overall heteroskedasticity (Manning and Mullahy, 2001). We used GLM rather than log OLS because we found no evidence of heavy-tails in the log-scale residuals from our GLM model. We present the results from a GLM with a gamma distribution and a log-link function for 1-year. Because the majority of patients have costs (more than 75% in the 1-year period and over 90% over the 3-year period), we do not present estimates from a 2-part model which separately estimates the probability of having any costs and the non-zero costs themselves.
We estimate parameters for six models that use the different drinking variables described above. The first three models follow the convention of including non-interacted drinking indicators with Abstinent as a reference category. The first model includes Any HDDs and Any non-HDDs, while the second and third models replace Any HDDs with the subcategories of 1 HDD and 2–30 HDDs and then 1–2 HDDs and 3–30 HDDs, respectively. The latter three models use the mutually exclusive categorical drinking indicators: Only non-HDDs, Only HDDs, and Both non-HDDs and HDDs, again with Abstinent as the reference category. Following a pattern, the fifth and sixth models use the 1 HDD and 2–30 HDDs and 1–2 HDDs and 3–30 HDDs breakouts of Any HDDs to construct the HDD categories. For example, instead of Both non-HDDs and HDDs, the fifth model now uses two separate variables: Both non-HDDs and 1 HDD and Both non-HDDs and 2–30 HDDs.
For brevity, we report only the estimates for drinking status covariates and include model-adjusted percentage differences that are easier to interpret. Specifically, these percent estimates are produced by exponentiating the unadjusted estimates (producing Incident Rate Ratios) and subtracting 1. They reflect the average percentage difference associated with being in each drinking group relative to the abstinent group. For each covariate and each specification, we also report the untransformed coefficient and standard error. Because we are also interested in how different drinking variables compare to each other and not just to Abstinence, we calculated Wald statistics to test whether their coefficients were significantly different from each other.
We conducted several sensitivity analyses. First, we estimated the alternative log-transformed models instead of our GLMs. Second, for 1-year costs, we estimated a two-part model and compared results with our models that included zero-cost patients. Finally, we re-estimated our models using the same drinking measures but constructed for the 30 days after the end of COMBINE treatment.
RESULTS
Table 1 provides descriptive statistics for the covariates used in our models. Table 2a describes drinking characteristics (the number of drinking days, drinks per drinking day, number of HDDs and drinks per HDD). We provide these statistics for patients by the non-mutually exclusive categories of Any non-HDDs and Any HDDs and also HDDs broken out by 1 HDD and 2–30 HDDs and 1–2 HDDs and 3–30 HDDs. Of the 794 patients, 294 were abstinent at the end of treatment, 275 had a non-HDD and 351 had an HDD. 103 were Only non-HDDs, and 179 were Only HDDs. We also included rows for the mutually exclusive categories created by interacting these sets of indicators. Patients with Any non-HDDs had 4 fewer drinking days than patients with Only HDDs. Among patients with Any HDDs, having any non-HDDs was associated with a minimal difference in the number of drinking days (13.2 versus 12.1) but 4.4 fewer HDDs and more than 3 fewer drinks per HDD. Nonetheless, the Only HDDs group cannot be characterized by daily or almost daily drinking.
Table 1.
Descriptive Statistics for the Three-Year Economic Study Participants
| Characteristic | Mean | Std. Dev. |
|---|---|---|
|
| ||
| Unemployed | 16.2% | 36.8% |
| Marijuana use | 19.4% | 38.8% |
| Illicit drug use excluding marijuana | 27.0% | 44.4% |
| WHO Physical Health Domain Score | 27.1 | 4.3 |
| WHO Psychological Health Domain Score | 20.8 | 4.0 |
| Female | 29.9% | 45.8% |
| Age in years | 44.8 | 10.3 |
| White | 78.5% | 41.1% |
| Black | 10.4% | 30.6% |
| Hispanic | 6.3% | 24.3% |
| Non-white/non-black/non-Hispanic | 4.8% | 21.4% |
| Married | 45.1% | 49.8% |
| Years of education | 14.5 | 2.7 |
| Observations | 748 | |
Table 2a.
Drinking Characteristics by End-of-Treatment Drinking Status
| Drinking Characteristics during the 30 Days before the Last Day of COMBINE Treatment |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drinking Days |
Drinks per Drinking Day |
Heavy Drinking Days (HDDs) |
Drinks per HDD |
||||||||||
| Drinking Category in the Last 30 days of COMBINE Treatment | N | Mean | (Std. Dev.) | Median | Mean | (Std. Dev.) | Median | Mean | (Std. Dev.) | Median | Mean | (Std. Dev.) | Median |
|
| |||||||||||||
| Main Drinking Indicators | |||||||||||||
| Abstinent | 294 | — | — | — | — | — | — | — | — | — | — | — | — |
| Any non-Heavy Drinking Days (non-HDDs) | 275 | 11.3 | (9.3) | 8.0 | 4.7 | (3.0) | 4.0 | 4.8 | (6.8) | 2.0 | 8.2 | (3.9) | 7.0 |
| Any Heavy Drinking Days (HDDs) | 351 | 12.6 | (9.9) | 10.0 | 9.1 | (5.6) | 7.2 | 9.9 | (9.4) | 6.0 | 10.1 | (5.4) | 8.1 |
| 1 HDD | 58 | 3.8 | (5.1) | 1.5 | 7.8 | (6.3) | 5.7 | 1.0 | — | 1.0 | 9.4 | (6.7) | 6.4 |
| 2–30 HDDs | 293 | 14.4 | (9.7) | 12.0 | 9.3 | (5.4) | 7.6 | 11.7 | (9.4) | 8.0 | 10.2 | (5.1) | 8.5 |
| 1–2 HDDs | 93 | 3.9 | (4.7) | 2.0 | 8.0 | (5.6) | 6.0 | 1.4 | (0.5) | 1.0 | 9.5 | (5.8) | 7.2 |
| 3–30 HDDs | 258 | 15.8 | (9.3) | 14.0 | 9.4 | (5.5) | 7.7 | 13.0 | (9.2) | 10.0 | 10.3 | (5.3) | 8.5 |
| Mutually Exclusive Categories | |||||||||||||
| Only non-HDDs | 103 | 8.1 | (9.0) | 3.0 | 2.4 | (1.0) | 2.4 | — | — | — | — | — | — |
| Both non-HDDs and HDDs | 172 | 13.2 | (8.9) | 10.0 | 6.1 | (2.9) | 5.3 | 7.7 | (7.2) | 5.0 | 8.2 | (3.9) | 7.0 |
| Only HDDs | 179 | 12.1 | (10.8) | 8.0 | 11.9 | (6.0) | 10.2 | 12.1 | (10.8) | 8.0 | 11.9 | (6.0) | 10.2 |
| Any non-HDDs and 1 HDD | 29 | 6.7 | (6.1) | 4.0 | 4.0 | (2.1) | 3.7 | 1.0 | — | 1.0 | 7.4 | (5.8) | 6.0 |
| Any non-HDDs and 2–30 HDDs | 143 | 14.6 | (8.8) | 12.0 | 6.5 | (2.8) | 5.7 | 9.0 | (7.1) | 6.0 | 8.4 | (3.4) | 7.2 |
| Any non-HDDs and 1–2 HDDs | 47 | 6.3 | (5.7) | 4.0 | 4.8 | (2.7) | 4.0 | 1.4 | (0.5) | 1.0 | 7.9 | (5.2) | 6.4 |
| Any non-HDDs and 3–30 HDDs | 125 | 15.9 | (8.5) | 14.0 | 6.6 | (2.8) | 5.8 | 10.1 | (7.1) | 7.0 | 8.3 | (3.3) | 7.2 |
| No non-HDDs and 1 HDD | 29 | 1.0 | — | 1.0 | 11.5 | (6.9) | 8.4 | 1.0 | — | 1.0 | 11.5 | (6.9) | 8.4 |
| No non-HDDs and 2–30 HDDs | 150 | 14.2 | (10.5) | 12.0 | 12.0 | (5.9) | 10.2 | 14.2 | (10.5) | 12.0 | 12.0 | (5.9) | 10.2 |
| No non-HDDs and 1–2 HDDs | 46 | 1.4 | (0.5) | 1.0 | 11.2 | (5.9) | 10.0 | 1.4 | (0.5) | 1.0 | 11.2 | (5.9) | 10.0 |
| No non-HDDs and 3–30 HDDs | 133 | 15.8 | (10.1) | 14.0 | 12.1 | (6.1) | 10.2 | 15.8 | (10.1) | 14.0 | 12.1 | (6.1) | 10.2 |
Notes: HDDs are defined as a day in which 5 or more drinks are consumed for men, 4 or more for women. All other drinking days are defined as non-HDDs. N=748.
In terms of health care use, Any non-HDDs patients had lower average costs ($1,716) than the Abstinent group ($2,147, Table 2b) during the 12 months following COMBINE. Among patients with Any HDDs, there were large cost differences based on whether they also had any non-HDDs ($1,799 for Both non-HDDs and HDDs versus $3,064 for Only HDDs ). Conversely, among Any non-HDDs, the presence of HDDs was not associated with significantly different costs ($1,799 versus $1,579). Three-year costs are larger than 1-year costs but were otherwise similar among the different drinking statuses.
Table 2b.
Cost Characteristics by End-of-Treatment Drinking Status and Period of Costs
| HealthCare Prevalence and Costs Following End of COMBINE Treatment |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1-Year Health Care Costs |
3-Year Health Care Costs |
||||||||
| Drinking Category in the Last 30 Days of COMBINE Treatment | N | % with Any Costs | Unconditional |
% with Any Costs | Unconditional |
||||
| Mean | (Std. Dev.) | Median | Mean | (Std. Dev.) | Median | ||||
|
| |||||||||
| Main Drinking Indicators | |||||||||
| Abstinent | 294 | 76.2% | $2,147 | ($5,824) | $492 | 91.5% | $5,752 | ($11,934) | $1,988 |
| Any non-Heavy Drinking Days (non-HDDs) | 275 | 81.1% | $1,716 | ($3,038) | $710 | 94.5% | $4,878 | ($7,902) | $2,367 |
| Any Heavy Drinking Days (HDDs) | 351 | 80.3% | $2,444 | ($6,327) | $793 | 93.2% | $6,748 | ($13,368) | $2,482 |
| 1 HDD | 58 | 84.5% | $1,718 | ($2,982) | $769 | 96.6% | $7,690 | ($11,332) | $2,683 |
| 2–30 HDDs | 293 | 79.5% | $2,588 | ($6,792) | $793 | 92.5% | $6,563 | ($13,473) | $2,414 |
| 1–2 HDDs | 93 | 84.9% | $1,650 | ($2,888) | $710 | 94.6% | $6,497 | ($9,901) | $2,556 |
| 3–30 HDDs | 258 | 78.7% | $2,730 | ($7,157) | $793 | 92.7% | $6,838 | ($14,423) | $2,402 |
| Interacted, Mutually Exclusive Categories | |||||||||
| Only non-HDDs | 103 | 78.6% | $1,579 | ($5,824) | $492 | 93.3% | $4,821 | ($8,126) | $2,015 |
| Both non-HDDs and HDDs | 172 | 82.6% | $1,799 | ($3,026) | $749 | 95.3% | $4,913 | ($7,789) | $2,463 |
| Only HDDs | 179 | 78.2% | $3,064 | ($8,315) | $793 | 91.2% | $8,491 | ($16,899) | $2,497 |
| Any non-HDDs & 1 HDD | 29 | 93.1% | $1,977 | ($3,234) | $710 | 100.0% | $6,878 | ($7,886) | $2,815 |
| Any non-HDDs and 2–30 HDDs | 143 | 80.4% | $1,763 | ($2,993) | $754 | 94.4% | $4,515 | ($7,736) | $2,414 |
| Any non-HDDs and 1–2 HDDs | 47 | 89.4% | $1,482 | ($2,643) | $568 | 95.7% | $4,994 | ($6,717) | $2,438 |
| Any non-HDDs and 3–30 HDDs | 125 | 80.0% | $1,918 | ($3,159) | $793 | 95.2% | $4,882 | ($8,181) | $2,565 |
| No non-HDDs and 1 HDD | 29 | 75.9% | $1,459 | ($2,739) | $798 | 93.1% | $4,812 | ($8,126) | $2,015 |
| No non-HDDs and 2–30 HDDs | 150 | 78.7% | $3,374 | ($8,977) | $793 | 90.7% | $8,480 | ($17,428) | $2,438 |
| No non-HDDs and 1–2 HDDs | 46 | 80.4% | $1,822 | ($3,138) | $793 | 93.5% | $8,029 | ($12,229) | $2,857 |
| No non-HDDs and 3–30 HDDs | 133 | 77.4% | $3,493 | ($9,442) | $794 | 90.4% | $8,648 | ($18,256) | $2,232 |
Notes: HDDs are defined as a day in which 5 or more drinks are consumed for men, 4 or more for women. All other drinking days are defined as non-HDDs. N=748.
Model Results
In column 1 of Table 3a, having Any HDDs is associated with 66% higher costs than Abstinent (p<.001), and Any non-HDDs (while controlling for Any HDDs) is associated with 24% lower costs than Abstinent (p= 0.054). Looking at column 2, the overall Any HDDs coefficient is decomposed into 55.7% for 1 HDD (p >.05) and 68.4% (p<.01) for 2–30 HDDs. Although the 1 HDD coefficient is smaller in magnitude, it is not significantly different from its 2–30 HDDs counterpart. The higher p-value for 1 HDD is in part due to a loss of power as the cell sizes decrease. In column 3, the difference in coefficient size for 1–2 HDDs (39.4%) and 3–30 HDDs (75.9%) is larger than for 1 HDD and 2–30 HDDs. Although they are not statistically significantly different from each other, 3–30 HDDs is significantly different from abstinence (p<.01). Across all three models, the estimate for Any non-HDDs is negative but only significant in the third specification (p<.05).
Table 3a.
Estimatesa from Six Modelsb of Total Health Care Costs during the Yearc Following COMBINE Treatment Using the COMBINE Economic Study Sample (No Interactions)
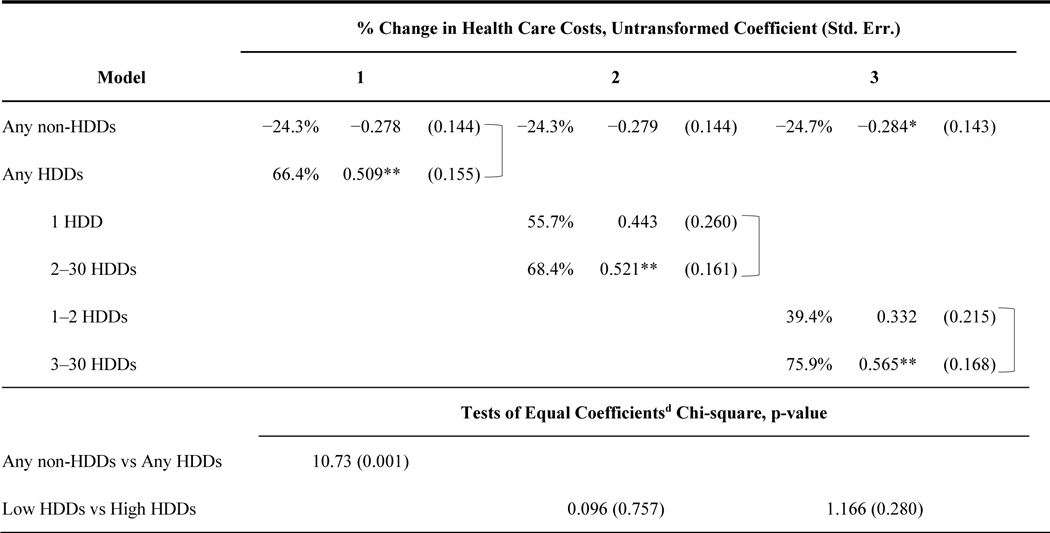
|
p<0.05,
p<0.01 , N=748, Full model results showing the coefficients for these covariates are included in Appendix A.
Estimates are % changes in HC Costs (Incident Rate Ratios – 1) transformed from unadjusted estimates from a GLM with a log-link function and gamma distribution. Robust standard errors for adjusted and unadjusted estimates are in parentheses.
The models comprise three past 30 day Heavy Drinking Day and Non-heavy Drinking Day measures. Heavy drinking days are defined as a day in which 5 or more drinks are consumed for men, 4 or more for women. All other drinking days are defined as Non-heavy Drinking Days.
Based on healthcare use reported from the end of COMBINE treatment through 12 months later.
Wald tests of the null hypotheses are that the estimated coefficients are equal (Chi-sq distribution, 1 d.f.). The Low HDDs category refers to 1 HDD or 1–2 HDDs. The High HDDs category refers to 2–30 HDDs or 3–30 HDDs. Compared coefficients are linked with brackets.
The columns in Table 3b show estimates for the mutually exclusive categories of drinkers, with Abstinent as the reference group. From model 4, having Only HDDs is associated with 91.8% higher costs (p<.001) than being Abstinent. Only non-HDDs patients’ costs were not statistically significantly different from Abstinent. Patients with Both non-HDDs and HDDs had costs that were not statistically different from Abstinent. From models 5 and 6, among patients with Only HDDs, we do not find evidence that a low number of HDDs is better than a higher number of HDDs, with all estimates ranging between 83% and 92%.
Table 3b.
Estimatesa from Six Modelsb of Total Health Care Costs during the Yearc Following COMBINE Treatment Using the COMBINE Economic Study Sample (Categorical Drinking Categories)
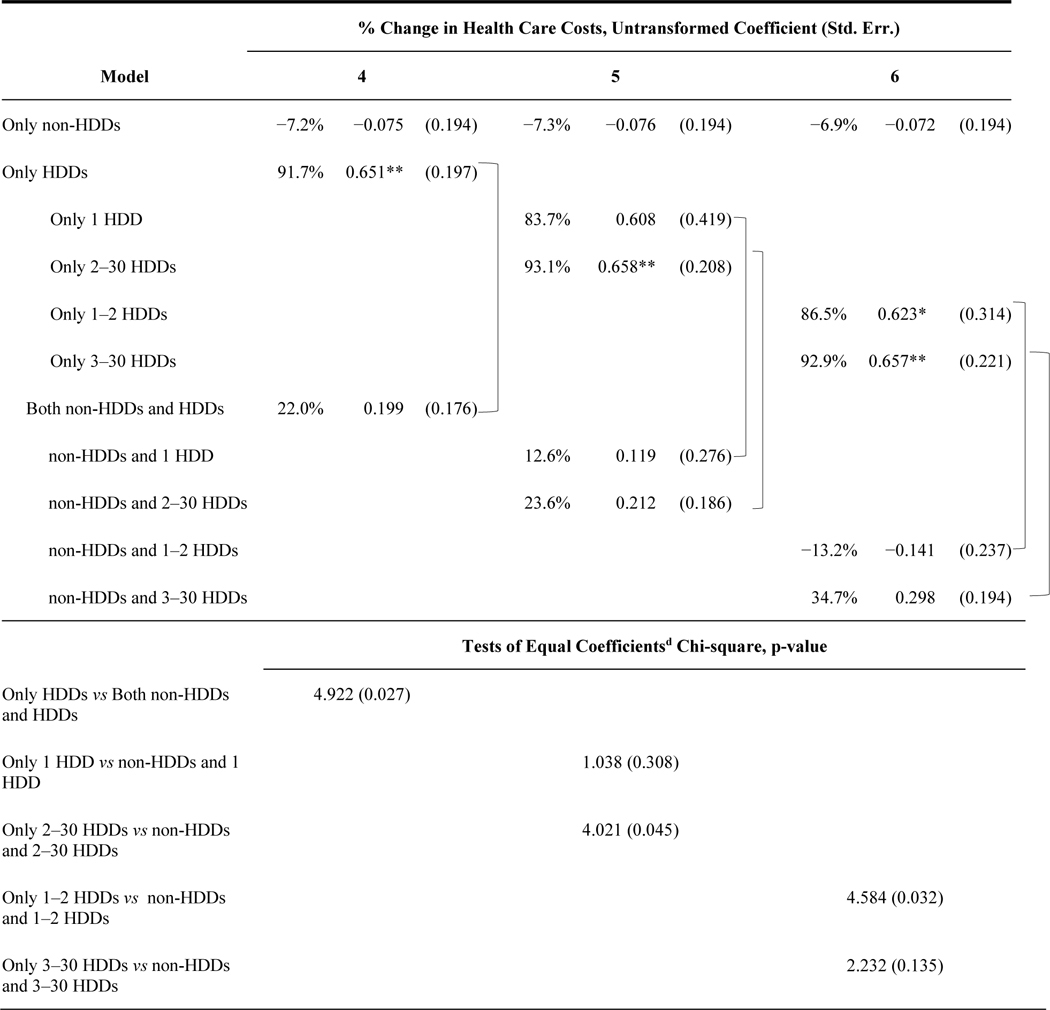
|
p<0.05,
p<0.01 , N=748, Full model results showing the coefficients for these covariates are included in Appendix A.
Estimates are % changes in HC Costs (Incident Rate Ratios – 1) transformed from unadjusted estimates from a GLM with a log-link function and gamma distribution. Robust standard errors for adjusted and unadjusted estimates are in parentheses.
The models comprise three past 30 day Heavy Drinking Day and Non-heavy Drinking Day measures. Heavy drinking days are defined as a day in which 5 or more drinks are consumed for men, 4 or more for women. All other drinking days are defined as Non-heavy Drinking Days.
Based on healthcare use reported from the end of COMBINE treatment through 12 months later.
Wald tests of the null hypotheses for these tests are that the estimated coefficients are equal (Chi-sq distribution, 2 d.f.). Compared coefficients are linked with brackets.
In all three of these models, we find large and statistically significant differences between the Only HDDs and the Both non-HDDs and HDDs. In all cases, having non-HDDs along with HDDs is associated with lower costs than Only HDDs. The Chi-squared test in column 4 comparing the HDDs-only coefficient (91.8%) with the coefficient on Both non-HDDs and HDDs (22.0%) was significant (p=.027). In the largest contrast, Both non-HDDs and 1–2 HDDs has a coefficient of −13.2% versus 86.5% for Only 1–2 HDDs (p=.032).
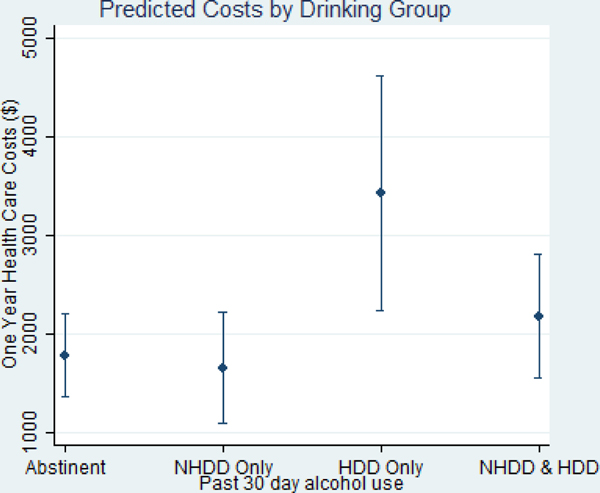
Although not included in Tables 3a and 3b, we also estimated models for HDD categories of 1–3 and 4–30 and 1–4 and 5–30, etc., as well as several broader categories described in the Methods section. We did not include these results as main findings because we did not find significant differences between the lower HDD and higher HDD groups beyond the 1–2 HDDs category. Figure 1 presents the model-adjusted costs based on estimates from the first model of Table 3b. The costs are calculated at covariate means and stratified by the four key analysis groups: Abstinent, Only non-HDDs, Only HDDs, and Both non-HDDs and HDDs. Only HDDs has the largest cost compared with the other three groups whose confidence intervals overlap.
Figure 1.
Model Adjusted Costs by Mutually Exclusive Drinking Groups
Three-Year Costs
The coefficients for Any non-HDDs and Any HDDs from 3-year models are smaller than for 1-year models (e.g., 33% versus 66% for Any HDDs and −18% versus −24% for Any non-HDD). Consistent with what was described in Table 2, the direction of the differences in costs did not change between the two periods. However, because overall costs increased for everyone, the percentage differences between the groups fell. The main effects for Any non-HDDs and Any HDDs in the interactive models (column 3) show the same attenuation (dropping to −1.8% and 53.2%), although the coefficient on their interaction term is almost identical (−31% versus −30%). Chi-squared tests of the coefficients for only HDDs versus Both HDDs and non-HDDs were significant at p<.10. Full model results for 3-year costs are included in Appendix A.2.
Sensitivity Analyses
Our findings were robust to several alternative analytical approaches. First, as part of the distributional analysis (which favored use of the GLM), we reviewed estimates from log-transformation models. Estimates from these models did not yield any coefficient differences larger than 4 percentage points. All post-estimation comparisons yielded the same statistically significant differences.
Second, even though the majority of patients had costs, we estimated a 2-part model as a robustness check. Out of our 6 models, all of our main GLM estimates are consistent in sign with the conditional costs from the 2-part model. All but one of the estimates are consistent with respect to statistical significance (relative to abstinence). All of the post–estimation comparisons of coefficients have the same sign and statistical significance (when jointly testing both the first and second part models).
Finally, we used drinking variables constructed from the 30-day period following the end of COMBINE treatment rather than the last 30 days of treatment. These drinking measures did not change substantially between the two 30-day periods, and results were very similar with .05 statistical significance achieved for all the same estimates as our primary models.
CONCLUSION
Our goal was to evaluate a set of drinking measures as useful and meaningful treatment outcomes based on their association with costs. We used data from the COMBINE Economic Study to estimate the relationship between end-of-treatment drinking status and subsequent 1-year costs. Having HDDs in the past 30 days was associated with 66.4% (p<.01) higher costs relative to abstinence; in particular, having 3 or more HDDs was associated with the highest costs (75.9%, p<.01). Having non-HDDs was associated with costs less than being abstinent, though the difference was not statistically significant. Notably, among patients with HDDs, those who also had non-HDDs had costs that did not significantly differ from those who were abstinent. In contrast, those with Only HDDs had costs that were 91.8% higher than abstainers (p<.05).
By the end of treatment in a trial such as COMBINE, patients achieve different drinking outcomes based on the interaction between treatment and patient characteristics. Our results suggest that patients who end treatment in different drinking groups (Abstinence, Only non-HDDs, Both non-HDDs and HDDs, and Only HDDs) have different subsequent costs. Strikingly, patients with Only HDDs at the end of treatment had poor subsequent outcomes, whereas those with Both non-HDDs and HDDs had relatively good outcomes. This is in spite of the fact that those two groups were otherwise similar in the number of drinking days and drinks per drinking day. This finding suggests that the main difference between the two groups is that the Only HDDs group shows no ability or preference to drink without drinking heavily; they are uncontrolled. In contrast, the heavy drinkers who also have non-HDDs demonstrated that they could drink in moderation on almost half of their drinking days and thus achieve a middle ground between uncontrolled and controlled drinking.
Conversely, because our results are not causal, they do not provide insight into counterfactual outcomes. We cannot say that Only HDDs patients could have lower costs if they could add some non-HDDs. We are unable to rule out the possibility that patient characteristics that led them to have Only HDDs at the end of treatment are also the determinants of their higher costs. Understanding how heterogeneous treatment responses and the typologies of drinking disorders mediate subsequent costs is beyond the scope of the current study.
A related point is that our results do not imply that non-HDDs should be recommended as a treatment goal. The COMBINE trial explicitly targeted abstinence as a treatment goal. We do not have evidence that targeting non-HDDs as a treatment goal would achieve either a similar pattern of abstinence, non-HDDs, and HDDs seen in our sample or a similar relationship between those drinking patterns and subsequent costs. In other words, outcomes with non-HDDs resulting from a different treatment experience might have a completely different relationship with subsequent costs.
However, our results provide useful information for evaluating drinking outcomes at the end of treatment (with cost as a proxy for recovery or overall improvement) and the value of those outcomes to society. They add to the broader tradition of searching for ideal outcome measures that balance clinical relevance, societal benefit, and utility for use by researchers, policy makers, and practitioners (Kadden and Litt, 2004). They address a research need laid out by the Alcohol Clinical Trials Initiative (Litten et al., 2012) for evaluating and improving the scientific landscape around treatment of alcohol use disorders. Specifically, they provide an assessment of the potential value of “lower bars” of treatment success, such as low-risk drinking. Our results complement Falk et al. (2010) and Kline-Smith et al. (2014) who found that patients with non-HDDs were better off than those with HDDs. In other words, abstinence and “low risk” non-heavy drinking were associated with outcomes superior to heavy drinking. We have added to those findings by demonstrating that a single “heavy drinking” measure may overlook 2 distinct types of heavy drinkers.
Finally, our study was limited by a combination of small cell sample sizes (e.g., Only 1 HDD had an N of 58), and the skewness in the distribution of costs makes statistical testing difficult. As such, we were unable to estimate separate results for smaller mutually exclusive categories of HDDs and non-HDDs. Nonetheless, based on the diagnostics leading to the use of the GLM and the reasonably balanced subgroup sample sizes on which we ultimately focused, we feel confident that the magnitude of differences and standard errors that we observe provide strong evidence for our findings. Ideally, future work on this topic would be supported by expanded data sets with similar measures of drinking outcomes and costs. Such data would permit replication of these findings and allow for a more in-depth investigation of the relationship between end-of-treatment drinking patterns and subsequent costs.
Sources of Support:
NIAAA grants R21AA022121 and 1RC4AA020096-01
Footnotes
The reasons include the frequency of follow-up interviews, incentives, the rapport established between the study participants and the study staff during the main study period, and the amount of grant resources provided to the study sites to support data collection. Finally, the participants eligible for the follow-up study had successfully completed 16 weeks of study treatment and thus may have been selected on unobserved characteristics that were correlated with study adherence.
REFERENCES
- Bray JW, Zarkin GA, Miller WR, Mitra D, Kivlahan DR, Martin DJ, Couper DJ & Cisler RA. (2007) Measuring economic outcomes of alcohol treatment using the Economic Form 90 *. J. Stud. Alcohol Drugs, 248. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Li T & Grant BF. (2008) A prospective study of risk drinking: at risk for what? Drug Alcohol Depend., 95, 62–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk D, Wang XQ, Liu L, Fertig J, Mattson M, Ryan M, Johnson B, Stout R & Litten RZ. (2010) Percentage of Subjects With No Heavy Drinking Days: Evaluation as an Efficacy Endpoint for Alcohol Clinical Trials. Alcohol. Clin. Exp. Res, 34, 2022–2034. [DOI] [PubMed] [Google Scholar]
- Kadden RM & Litt MD. (2004) Searching for treatment outcome measures for use across trials *. J. Stud. Alcohol, 145. [DOI] [PubMed] [Google Scholar]
- Kline-Simon AH, Weisner CM, Parthasarathy S, Falk DE, Litten RZ & Mertens JR. (2014) Five-Year Healthcare Utilization and Costs Among Lower-Risk Drinkers Following Alcohol Treatment. Alcohol. Clin. Exp. Res, 38, 579–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litten RZ, Egli M, Heilig M, Cui C, Fertig JB, Ryan ML, Falk DE, Moss H, Huebner R & Noronha A. (2012) Medications development to treat alcohol dependence: a vision for the next decade. Addict. Biol, 17, 513–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning WG & Mullahy J. (2001) Estimating log models: to transform or not to transform? J. Health Econ, 20, 461–494. [DOI] [PubMed] [Google Scholar]
- Marlatt GA & Witkiewitz K. (2002) Harm reduction approaches to alcohol use. Health promotion, prevention, and treatment. Addict. Behav., 27, 867–886. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Kline-Simon AH, Delucchi KL, Moore C & Weisner CM. (2012) Ten-year stability of remission in private alcohol and drug outpatient treatment: Non-problem users versus abstainers. Drug Alcohol Depend., 125, 67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC & Sobell MB. (1992) Timeline follow-back. Measuring alcohol consumption. Springer. [Google Scholar]
- Sobell MB & Sobell LC. (2011) It is time for low-risk drinking goals to come out of the closet. Addiction, 106, 1715–1717. [DOI] [PubMed] [Google Scholar]
- The WHOQOL Group (1998) The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc. Sci. Med, 46, 1569–1585. [DOI] [PubMed] [Google Scholar]
- Zarkin GA, Bray JW, Aldridge A, Mills M, Cisler RA, Couper D, Mckay JR & O’malley S. (2010) The effect of alcohol treatment on social costs of alcohol dependence: results from the COMBINE study. Med. Care, 48, 396–401. [DOI] [PMC free article] [PubMed] [Google Scholar]