Abstract
Background:
While adolescents in the United States are one of the most affected groups by the opioid crisis, their perceptions on opioid misuse and preferences for education are rarely studied. Although it is critical to educate adolescents on proper opioid use and storage, many educational tools need easy measurement scales to systematically document learning of targeted programs. It is essential to understand adolescents’ knowledge about opioid risks and perceptions about the opioid crisis to design effective preventive interventions.
Objective:
The purpose of this study was to develop an effective scale that measures adolescents’ knowledge about opioid misuse and interest in learning about prescription opioid safety.
Methods:
Using survey data from 188 high school students in the Midwest, exploratory factor analysis (EFA) was used to examine the underlying structure of an initial 68 items. Items were adapted from a statewide survey previously designed to document awareness of prescription drug misuse and abuse in the state of Wisconsin. Refinement of the scale used factor analysis iterations and internal consistency measures. Cronbach’s alpha was used to determine internal consistency among the items.
Results:
Three exploratory factor analysis iterations resulted in a 16-item four-factor structure describing adolescents’ knowledge of misuse and harm, their interest in learning about prescription opioids, and their tendency to practice misuse behaviors. Internal consistency and the correlation among factors were examined and strong (Cronbach’s α > 0.8). The final 16-item instrument was termed the Adolescent Opioid Safety and Learning (AOSL) Scale.
Conclusions:
When combined with adolescent opioid education tools, the AOSL Scale can help assess and document medication safety learning. The four subscales could support researchers and practitioners in measuring adolescents’ orientation towards prescription opioid misuse. The AOSL Scale may also be used in developing targeted educational materials on prevention of opioid misuse for adolescents.
Keywords: Adolescents, Opioid safety, Exploratory factor analysis (EFA), Adolescent opioid safety and learning (AOSL), scale, Opioid education information
Introduction
Opioid epidemic in adolescents
The opioid epidemic affects adolescents in the US, with 7.6% of this population reporting misuse in 2019, primarily related to prescription opioids.1,2 Unfortunately, 64% of clinicians do not have a protocol for prescribing pain management, which contributes to this misuse.3 Several of these clinicians also believed medications that work for adults also work for adolescents and that adolescents will not be negatively affected by these medications.3 Yet, many clinicians in other studies believe that adolescents may use opioids not only to relieve pain, but also to get high.4-6 Despite the black box warning on codeine for this population, the most commonly prescribed opioids to children and adolescents are hydrocodone, oxycodone, and codeine,.7-9 As a result, there is an increase in the hospitalizations of children and adolescents, increase in opioid abuse calls, and an increase in the mortality rate from opioids.10-12 What is most concerning is that adolescents prescribed opioids before 12th grade are more likely to misuse opioids later in life than those without a prescription; those with a prescription are three times more likely to misuse than those without.2,13-17 Furthermore, lifetime opioid misuse is not only correlated with unsafe medication storage in the household, 86.3% of intentional opioid exposures occurred in the adolescents’ household, but also with the notion that peers of adolescents are also abusing opioids.2,15-18
Opioid mismanagement by parents
Despite 72.6% of parents stating they believe children can overdose on opioids more easily than adults, unsafe opioid practices and storage still occur in the home.19 Safe storage is more common in households with children under the age of seven, even though it is more common for older adolescents to misuse opioids and share them with others.20-23 One contributing factor to opioid mismanagement is that a majority of parents did not think their children would take opioids and did not store opioids properly in the home. Only 6% of parents are counseled on how to dispose of opioids properly, 54.8% of adults are unaware of secure places to store opioids or the proper disposal routes, and there are conflicting recommendations for disposal.10,24,25 Additionally, parents do not intend to dispose of expired or unused opioids. Common reasons for retention of unused opioid medications are that parents do not know how to properly dispose of opioids, think their children may need the drug in the future, and paid for the medication.26
International opioid use among adolescents
Opioid misuse poses an important health problem worldwide. A longitudinal study sought to explore adolescent drug misuse on an international level by using data from the Researched Abuse Diversion and Addiction-Related Surveillance (RADARS®) System, which included all intentional calls for prescription opioids and stimulants for persons 13 through 19 years old from 2007-2009.17 The study found that 68% of the reported adolescent experiences with prescription drugs were opioid related.17 In Europe, prescription opioids account for three-quarters of overdose deaths, which represent 3.5% of total deaths among adolescents.27 Another study found that between 2006 and 2012, the prevalence of prescribed opioid use by adolescents significantly increased among adolescents in Denmark, Norway, and Sweden.28 Other studies have shown that adolescent opioid misuse is prevalent in the Middle East and Africa.29-32 Furthermore, there has been a worldwide increase of deaths from prescription opioids, establishing that opioid misuse remains is a universal issue.33
Opioid educational interventions
With the opioid epidemic increasingly affecting adolescents, new educational materials have been developed to help support their learning and understanding of opioids. For example, the National Institute on Drug Abuse (NIDA) created a teen program to educate adolescents, parents, and teachers via online games, videos, drug facts, and lesson plans on prescription drug use, misuse, and its effects.34,35 An organization called ‘Opioid Lifeline’ developed This is (Not) About Drugs which educates adolescents in a classroom session on how addiction can stem from misuse, symptoms of an overdose, the use of naloxone, and general resources on supporting adolescents’ decision-making when it comes to opioid use.34,36 Other organizations, ‘Rx for Addiction’ and ‘Medication Safety’, created a 3-h program with interactive sessions that focuses on medication safety and signs of misuse, withdrawal, and overdose by utilizing role-play, case scenarios, and social media.20 Furthermore, Operation Prevention educates students through providing classroom resources to help begin the conversation surrounding the potential impacts that opioids can have on adolescents and also provides a toolkit for parents about misuse and prevention.37,38 While there have been several interventions that proved to be helpful for adolescents’, none of them incorporated a scale to efficiently measure adolescents’ preferences for opioid misuse education.25,37,39-42
Medication knowledge scales
Currently, there are no scales that measure adolescents’ preferences for opioid safety education regarding safe storage of opioids, where they learn about safe opioid practices, and what they have already know about opioid misuse. Surveys like the National Survey on Drug Use and Health and CRAFFT Screening Questions can measure opioid use and misuse prevalence in youth, but neither incorporate storage or educational questions on opioids.18,43,44 The Medication Attitude Questionnaire surveys for adults measure their attitudes about using pain medications for their children.45 There are other broader medication use surveys that are currently available such as the Beliefs about Medicines Questionnaire, which measures overuse, harm, and benefits, and the Perceived Sensitivity to Medicines Scale, which measures a person’s beliefs about the beneficial and harmful effects of medicines.46 Thus, the purpose of this study is to develop the Adolescent Opioid Safety and Learning (AOSL) Scale, a scale that measures adolescents’ knowledge of and preferences for opioid safety, current misuse, and storage practice of opioids.
Methods
Study participants, recruitment, setting
Participants were recruited from three Wisconsin high schools in rural, urban, and suburban geographic areas of the state. Inclusion criteria for participation in the study was that participants were enrolled in 9th to 12th grade, could speak and understand English, and that English or Spanish were their parent’s or guardian’s first language. In one school, recruitment materials were distributed to 112 eligible students enrolled in a required health course. In the other two schools, recruitment materials were distributed to all 1100 students fitting the study inclusion criteria. Students who were younger than 18 years old were required to assent and to obtain parent or guardian consent to participate; students 18 and older could consent for themselves. Of the 1212 students who were eligible to partake in the study, 190 students consented to and took the survey. The survey was administered electronically using REDCap, a secure Internet platform for building and managing online surveys and databases. Students were reminded to complete the survey on their own and were spread out in classrooms to limit the ability to see peers’ responses. Survey answers remained anonymous, and each survey was given a code that did not correspond to specific students. The responses were collected and managed using REDCap electronic data capture tools hosted at University of Wisconsin-Madison.47,48 At the time of survey completion, participants received a $15 cash payment.
Survey development and measures
The study team developed a survey to capture high school students’ attitudes and knowledge about misuse of prescription opioids, safe handling, storage, information seeking behaviors, and their preferences for education about medication safety practices. The survey consisted of 84 items in total: 68 instrument items and 16 demographic questions (Appendix A). The 68 items were used for this analysis to assess adolescents’ knowledge of opioid misuse behaviors, how much harm misuse of opioids can do, how likely adolescents are to engage in misuse behavior, and their interest in learning more about opioid medication topics. Survey responses options consisted of close-ended questions (i.e., Likert scales or dichotomous responses). Question structure and content were adapted from a statewide survey previously designed to increase awareness of prescription drug misuse and abuse in the state of Wisconsin, which was adapted from a survey used by State of Maryland for similar purpose.49,50 Questions from the Wisconsin state-wide survey were revised in structure and content to meet the needs of a high school adolescent target audience and objectives of the study. The survey was pilot tested in two afterschool youth programs and revised based on their feedback. This draft of the survey was then reviewed by the University of Wisconsin Survey Center and revised based on their feedback to create the final survey instrument. The final survey took approximately 10 min to complete. The revised study instrument and study protocol were approved by the University’s Health Sciences Institutional Review Board.
Data analysis and internal consistency
Overall, 190 survey responses were collected. Data were cleaned of any non-response or missingness, resulting in two surveys being excluded from data analysis, leaving 188 complete responses. All analyses were performed in R version 4.0.0 using the psych package for factor and internal consistency analyses.51,52 We focused on an iterative exploratory process to help understand what factor structure might be most stable within the data and groups of questions/themes within the survey that appear most strongly related with one another.
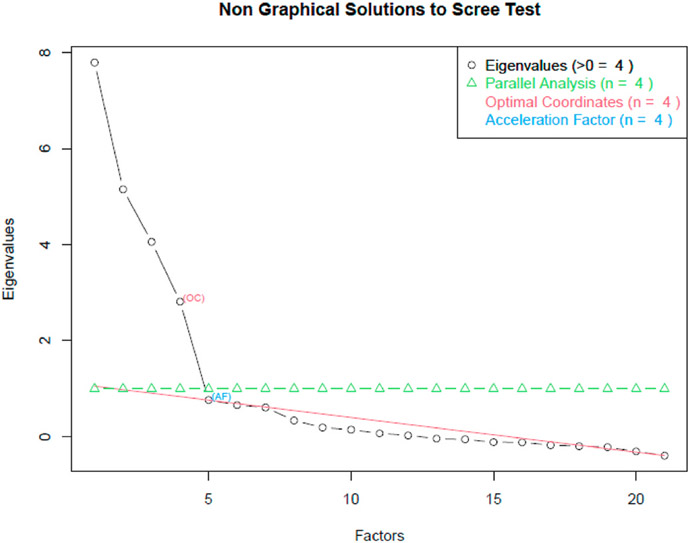
A combination of scree and parallel analyses were used to determine the number of factors to fit in any given iteration (Fig. 1). After the number of factors to fit was selected, the data were fit by minimizing residuals and using oblique rotation (oblimin method). After fitting, the loading of items across the factors was examined, along with the distributions of the estimated factors and their correlations, to aid in which item groupings (i.e., question themes) or individual items within a theme should be removed before the next exploratory iteration. In addition to factor analyses, summary scores of each theme present in the instrument were created by standardizing each item in the theme (creating means of 0 and standard deviations of 1) then summing the standardized items within theme. These theme summary measures were then analyzed for internal consistency using Cronbach’s α, and for the change in α and α′s standard error of the summary measure for dropping each individual item from the summary measure. Cronbach’s alpha above 0.70 was considered acceptable for internal consistency.
Fig. 1.
PCA Plot used to determine the number of factors to fit in any given iteration.
Results
Participant characteristics
A total of 188 completed surveys were included for the final analyses. The demographic characteristics of the survey respondents are described in Table 1.
Table 1.
Participant demographics (N = 188).
| Demographics | N (%) |
|---|---|
| Grade a | |
| 9th | 30 (16.7) |
| 10th | 79 (43.9) |
| 11th | 33 (18.3) |
| 12th | 38 (21.1) |
| Gender b | |
| Female | 102 (53.7) |
| Male | 74 (38.9) |
| Other | 12 (6.4) |
| Race/Ethnicity c | |
| White | 101 (53.2) |
| Black | 2 (1.1) |
| Hispanic | 60 (31.6) |
| Other | 25 (13.3) |
| RUCA 3.0 Zip Code Designation d,e | |
| 1 or 2: Metropolitan area core/high commuting | 128 (71.9) |
| 7: Small town core | 45 (25.3) |
| 10.3: Rural areas | 5 (2.8) |
| Age (mean (SD)) | 16.21 (1.02) |
| People under 18 living in your household? (mean (SD)) | 2.19 (1.16) |
Grade was missing for 8 participants.
Gender identity choices of “male,” “female” and “in another way” were not mutually exclusive in the survey. As such, “male” is defined as select “male” while not selecting other choices; “female” is defined as selecting “female” while not selecting other choices; “other” was defined as all other combination of choices that occurred.
Race/ethnicity were not mutually exclusive choices between 7 different options. As such, “white,” “black,” and “Hispanic” were defined as selecting only one of those associated options and selecting none of the other 6; “other” was defined as any other combination of selections.
Small town core is defined as primary flow within an urban cluster of 2500 to 9999 (small UC); Rural areas are defined as primary flow to a tract outside a UA or UC; Secondary flow 30%–50% to a small UC.
Zip Code was missing for 10 participants.
Preliminary item reduction using EFA
EFA was used for item reduction as well as to understand the underlying factor structure. The first exploratory analysis utilized all 68 items across the 188 student responses, resulting in a suggested number of factors to fit from 3 to 11, depending upon the method given priority. The first iteration fit a maximum number of factors of 6. When examining which survey items or item groupings should be removed in the next iteration, the following observations were considered: items with small loadings on all factors, items with loadings distributed evenly across several factors, items whose removal improved internal consistency measures of the theme, and items loading onto factors that had highly non-normal distributions or factors that had correlations counter to how we would expect them to correlate with other factors, were considered for removal. Items that were important to the fundamental understanding of opioid knowledge, opinions, and behavior within high school students were retained, regardless of the above behavior they might exhibit (i.e., the scientific goal of the instrument was always paramount).
After several iterations and reduction in the items used, the suggested number of factors to fit was stable at four across all the methods examined, with each factor “isolating” to each of the four themes. These four themes included items about opioid misuse, interest in learning about opioids, things you might do when using opioids, and harm caused by opioids. Table 2 describes items under each of these four categories, which were then used to run the final analysis.
Table 2.
Item codes and items used in EFA analysis after preliminary item reduction.
| Item code |
Item |
|---|---|
| Opioid Learning Interest | |
| Even if you have learned about these topics before, how interested (not at all, a little, somewhat, very, extremely) would you be in learning more about each of the following topics on opioid use and safety? | |
| 16a | What are opioids |
| 16b | How to practice safe use of opioids |
| 16c | What are negative consequences of opioid misuse |
| 16d | How can we safely store and dispose opioid medications? |
| 16e | Resources to refer to learn more about opioid safety? |
| Opioid Misuse Behavior | |
| We would like your opinion on what you would consider the misuse of opioids. Is someone misusing opioids if (yes/no) … | |
| 7a | … they are using an opioid they had a prescription for, but after it expired?a |
| 7b | … they use someone else’s prescription to get opioids for themselves? |
| 7c | … they use someone else’s opioid medication? |
| 7d | … they use opioids at a higher dose, or more often than their prescription calls for? |
| 7e | … they share their opioid medications with others? |
| 7f | … they return their unused opioid medication to the pharmacy when it expires? a |
| Likelihood to Misuse Opioids | |
| Next, we would like you to think about how likely (not at all, slightly, somewhat, very, extremely) you might be to do each of the following How likely would you be to … | |
| 9a | … use an opioid that was prescribed to your friend for your own pain relief? |
| 9b | … offer an opioid that you have a prescription for to a friend for their pain relief? |
| 9c | … use a prescription opioid medication your grandparents have in their house? |
| 9d | … use someone else’s opioid pain relief medication that you find in your house? |
| 9e | … stop your friend from using an opioid medication for non-medical purposes? (reverse coded) |
| Opioid Harm | |
| How much harm (none, a little, some, quite a bit, a great deal) does the misuse of opioids do to a person’s … | |
| 8a | … physical health? a |
| 8b | … mental health? a |
| 8c | … ability to do well in school? |
| 8d | … relationships with their family? |
| 8e | … relationships with their peers or friends? |
Items dropped from final analysis.
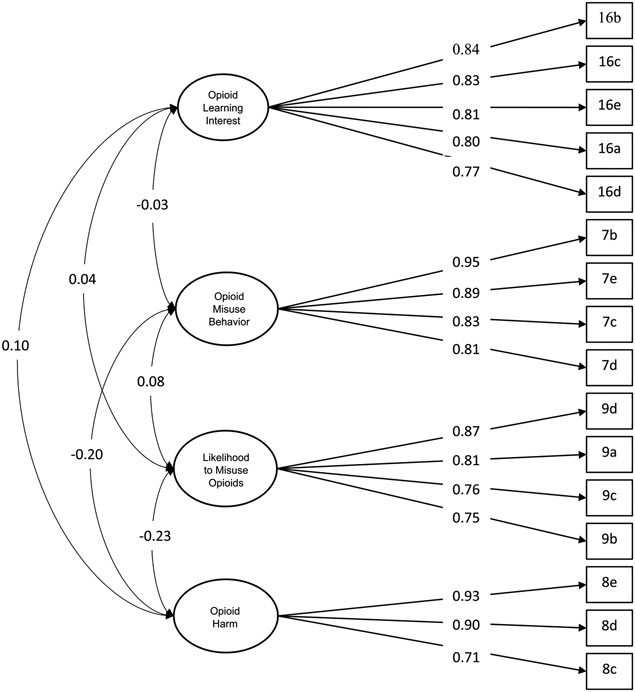
Factor structure and AOSL scale item using EFA
Given the four-factor structure, we turned attention to identifying the strength of loading of each item within each factor. Five of the 21 items which loaded poorly (less than 0.60)53 were dropped in this step: two non-misuse items (0.38 and 0.26, respectively), two physical and mental health harm items (0.53 and 0.55, respectively) and one item about using opioids after they expire (0.57). Thus, the final analysis utilized 16 items with a 4-factor structure, which constituted the final AOSL Scale (Fig. 2). Item loadings for this model are presented in Table 3. High internal consistency was observed between the items loading on each factor (see Table 4).
Fig. 2.
Factor structure with standardized loading for the 16-item Adolescent Opioid Safety and Learning scale. The Adolescent Opioid Safety and Learning scale.
Table 3.
Item loadings of 16 items in the final four-factor model.
| Item | F1: Opioid Learning Interest |
F2: Opioid Misuse Behavior |
F3: Likelihood to Misuse Opioids |
F4: Opioid Harm |
|---|---|---|---|---|
| 16b | 0.840 | −0.024 | 0.003 | 0.059 |
| 16c | 0.828 | 0.008 | −0.060 | −0.106 |
| 16e | 0.813 | 0.020 | 0.057 | 0.093 |
| 16a | 0.803 | −0.035 | 0.005 | −0.002 |
| 16d | 0.772 | 0.032 | 0.000 | 0.003 |
| 9d | −0.090 | 0.044 | 0.870 | 0.107 |
| 9a | 0.075 | −0.037 | 0.813 | −0.101 |
| 9c | −0.021 | −0.069 | 0.757 | 0.067 |
| 9b | 0.071 | 0.061 | 0.749 | −0.187 |
| 8e | 0.049 | 0.037 | −0.009 | 0.934 |
| 8d | −0.031 | −0.041 | 0.021 | 0.898 |
| 8c | 0.032 | −0.029 | −0.104 | 0.708 |
| 7b | −0.043 | 0.952 | 0.018 | 0.033 |
| 7e | 0.016 | 0.892 | 0.065 | 0.039 |
| 7c | 0.078 | 0.825 | −0.010 | −0.025 |
| 7d | −0.038 | 0.805 | −0.104 | −0.088 |
Shading indicates significance.
Table 4.
Cronbach’s alpha among items.
| Theme | alpha | se | item | dropped alpha |
dropped se |
|---|---|---|---|---|---|
| Opioid Learning Interest | 0.905 | 0.011 | 16a | 0.886 | 0.013 |
| 16b | 0.878 | 0.015 | |||
| 16c | 0.885 | 0.014 | |||
| 16d | 0.891 | 0.013 | |||
| 16e | 0.882 | 0.014 | |||
| Opioid Misuse Behaviors | 0.924 | 0.009 | 7b | 0.882 | 0.015 |
| 7c | 0.912 | 0.011 | |||
| 7d | 0.915 | 0.011 | |||
| 7e | 0.898 | 0.013 | |||
| Likelihood to Misuse Opioids | 0.868 | 0.015 | 9a | 0.796 | 0.025 |
| 9b | 0.830 | 0.021 | |||
| 9c | 0.864 | 0.017 | |||
| 9d | 0.827 | 0.019 | |||
| Opioid Harm | 0.892 | 0.014 | 8c | 0.911 | 0.013 |
| 8d | 0.820 | 0.026 | |||
| 8e | 0.801 | 0.029 |
Factor one was named ‘Opioid Learning Interest’ and measures the extent to which teens are interested in learning about opioids, how to practice safe use of opioids, the negative consequences of opioid misuse, how to safely store and dispose of opioid medications, and resources to learn more about opioid safety. Cronbach’s alpha showed strong internal consistency among the 5 items (α = 0.905, se = 0.011).
Factor two was named ‘Opioid Misuse Behavior’ and measures the ability to recognize the following behaviors as opioid misuse: using someone else’s prescription to get opioids, using someone else’s opioid medication, using opioids at a higher dose, or more often than their prescription calls for, and sharing opioid medications with others. Cronbach’s alpha showed strong internal consistency among the 4 items (α = 0.924, se = 0.009). This factor was weakly and negatively correlated with ‘Opioid Harm’ (r = −.20).
Factor three was named ‘Likelihood to Misuse Opioids’ and measures the extent to which participants are likely to engage in the following misuse behaviors: using an opioid that was prescribed to a friend for their own pain relief, offering an opioid that they have a prescription for to a friend for their pain relief, using a prescription opioid medication their grandparents have in their house, and using someone else’s opioid pain relief medication that they find in their house. Cronbach’s alpha showed strong internal consistency among the 5 items (α = 0.868, se = 0.015). This factor was weakly and negatively correlated with ‘Opioid Harm’ (r = −.23).
Factor four was named ‘Opioid Harm’ and indicated the amount of harm misuse of opioids does to a person’s ability to do well in school, relationships with their family, and relationships with their peers or friends. Cronbach’s alpha showed strong internal consistency among the 5 items (α = 0.892, se = 0.014).
Discussion
One in four adolescents in the United States have misused a prescription opioid at least once in their life,14 and nearly one in four high school students in the United States are exposed to opioids, medically or non- medically.14 The opioid crisis in this age group is not adequately addressed in empirical literature. A need to understand adolescents’ perceptions about opioid misuse and safety has been recognized.34 This warrants the requirement of a scale to understand how adolescents perceive the opioid epidemic, their perceptions on what constitutes misuse, how harmful opioid misuse is, and their preferences for education to help combat this epidemic in their population. This study recognized this need and, using EFA, developed the Adolescent Opioid Safety and Learning (AOSL) Scale, which measures adolescents’ knowledge of and preferences for opioid safety, current misuse, and storage practice of opioids.
Four factors emerged from the EFA. These factors were named ‘Opioid Learning Interest’, ‘Opioid Misuse Behavior’, ‘Likelihood to Misuse Opioids’, and ‘Opioid Harm’. Fifty-two of the original 68 items were dropped due to poor loadings in the process of EFA, resulting in a 16-item scale. Based on the EFA conducted in this study, adolescents were aware of the opioid crisis in their age group and could identify harms of opioid misuse and behaviors related to it. Interestingly, ‘opioid learning interest’ and ‘likelihood of misuse opioids’ were not strongly related. Similarly, ‘Opioid Harm’ and ‘opioid misuse behavior’ were not strongly related. Relationships between these factors should be confirmed using confirmatory factor analysis.
Adolescents who report misuse of prescription opioids indicated medical use of prescription opioids before they started using them nonmedically.54 In the last forty years, lifetime use of nonmedical prescription opioids was reported to be highly correlated with medical use of prescription opioids.55 It is estimated that 17.6% of high school seniors reported lifetime medical use of prescription opioids, while 12.9% reported nonmedical use of prescription opioids.14 Understanding what factors constitute opioid misuse according to adolescents is important to understand adolescents perceptions about misuse.
Misuse of opioids has not been accurately defined yet.34 The CDC describes various actions that constitute opioid misuse, such as using someone else’s opioid medication, using opioids at a higher dose, or more often than their prescription calls for, and sharing opioid medications with others.56 Adolescents involved in this study correctly recognized these three items as constituting the opioid epidemic. This factor, Opioid Misuse Behavior, helps researchers better understand adolescents’ ideas of what constitutes opioid misuse and can be used to develop educational interventions specific to adolescents. Additionally, though the magnitude of correlation was not large in our results, the negative correlation between “opioid Harm” and both “opioid misuse behavior” and “likelihood to misuse opioids” indicates that one can enact practical change in opioid misuse views and behaviors through education about opioid harm.
It is also important to understand the role parental behaviors play in adolescent opioid misuse prevention. Parental monitoring, family structures, and social ties have been reported to affect an adolescents’ motives for misusing prescription drugs.57 While there is some evidence available about the effects family and friends can have on adolescents’ intentions to misuse opioids, nothing is known about how adolescents perceive the effect of misusing opioids on their relationships with family and friends. Items under factor four ‘Opioid Harm’ capture this gap in literature, thus making this survey instrument a new addition to this field.
This study adds to the literature an important survey instrument which will help capture adolescents’ perceptions about opioid misuse and safety. Without a definition available for opioid misuse, and lack of consensus of opioid safety practices, there is a need to understand how exactly adolescents perceive opioid misuse and safety.24,25 Therefore, using the final validated version of this scale will be useful to future scholarship. Future studies should test the AOSL Scale on a national and international sample of adolescents to examine if the scale is applicable to a more diverse sample. Once tested, the validated scale will allow for researchers to gain better insight on adolescents’ knowledge of and preferences for opioid safety, current misuse, and storage practice of opioids. A validated final version of the AOSL Scale will guide the development of adolescent specific interventions, which will be more effective than general interventions for adolescents and will help combat the opioid epidemic. This instrument can be used in schools to assess adolescents’ perceptions and knowledge before offering an opioid safety session in health class or by researchers to understand their audience before developing interventions to combat the opioid crisis in adolescents.
Limitations and implications
While the items removed from factor analyses could be construed as unstable or inconsistent, this does not indicate that those items are less useful or less valuable. Removed items could be due to several reasons that might be of scientific importance or interest and may be more variable with respect to the knowledge, behavior, or opinions adolescents have around what the item is asking. These items might also be less correlated with other items in the survey. Such items could represent unique themes, factors, or students’ thoughts, and if more items were related to it, they might have been retained. If such items are overly variable and noisy, they could also represent areas ripe for improvement in opioid education and understanding within adolescents. Additionally, there is always the possibility that certain important items were removed because of the overfitting scenario present here and might be retained given more data. Common heuristics in factor analyses are to have a number of observations that are at least 10 times the number of parameters being estimated in EFA, highlighting the need for additional study and testing of the AOSL scale in larger samples.58 Due to the differences among reported adolescent opioid misuse between grades and US states, there is a need to test the full 68 item AOSL scale among additional grade levels and on a national scale, to examine if the removed items are of scientific significance.1,59 There is also a need to test the scale on an international level as adolescent opioid misuse is prevalent globally.17,27-33 A confirmatory factor analysis should be conducted on a larger national and international sample of participants to verify the factor structure.
Conclusion
There is a lack of scientific literature that measures adolescents’ preferences for learning about safe storage of opioids, correct opioid practices, and what preexisting knowledge about opioids they have. This study sought to explore this gap in the literature by creating the Adolescent Opioid Safety and Learning (AOSL) Scale and testing it on a group of adolescents. A four-factor structure, including a 16-item scale, was obtained through EFA. The four factors identified were: Opioid Learning Interest, Opioid Misuse Behavior, Likelihood to Misuse Opioids, and Opioid Harm. Validating this study in other states, and on a national and international level, would help adapt this scale to broader groups of adolescents. In doing so, this will help us understand adolescent perceptions and opinions about opioid safety education, which can help researchers and educators design targeted educational materials on prevention of opioid misuse, specifically for adolescents.
Supplementary Material
Acknowledgements
The authors thank Laura Stephenson, PhD, for assistance with data analysis and for reviewing and editing the manuscript; Lisa Szela, BS, for her assistance with data collection and for reviewing and editing the manuscript; Katherine Mijal, and Gwen Salm for their assistance with data collection.
Funding
This study was supported by KL2 grant KL2 TR002374-03 and grant UL1TR002373 to UW ICTR by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. This study was also supported by the University of Wisconsin-Madison, Department of Family Medicine and Community Health Small Grants Program and Innovation Funds.
Footnotes
Declaration of competing interest
All authors report that they have no financial disclosures and no conflict of interest.
Credit author statement
Olufunmilola Abraham: Conceptualization, Methodology, Writing - Review & Editing Tanvee Thakur: Investigation, Writing - Original Draft, Writing - Review & Editing Kelsey Brasel:Investigation, Writing - Original Draft, Writing - Review & Editing Derek Norton: Formal analysis, Writing - Original Draft, Writing - Review & Editing Claire Rosenberger: Writing - Original Draft, Writing - Review & Editing.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sapharm.2021.06.007.
Data statement
Due to the sensitive nature of the questions asked in this study, survey respondents were assured raw data would remain confidential and would not be shared.
References
- 1.High School YRBS. The center for disease and prevention. https://nccd.cdc.gov/youthonline/App/Results.aspx?. Accessed June 1, 2021.
- 2.Groenewald CB. Opioid-prescribing patterns for pediatric patients in the United States. Clin J Pain. 2019;35:515–520. 10.1097/AJP.0000000000000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang JS, Kuelbs CL. Clinician opioid prescribing practices and patient utilization of prescribed opioids in pediatrics. J Opioid Manag. 2018;14:309–316. 10.5055/jom.2018.0463. [DOI] [PubMed] [Google Scholar]
- 4.Young A, McCabe SE, Cranford JA, Ross-Durow P, Boyd CJ. Nonmedical use of prescription opioids among adolescents: subtypes based on motivation for use. J Addict Dis. 2012;31:332–341. 10.1080/10550887.2012.735564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCabe SE, Boyd CJ, Cranford JA, Teter CJ. Motives for nonmedical use of prescription opioids among high school seniors in the United States: self-treatment and beyond. Arch Pediatr Adolesc Med. 2009;163:739–744. 10.1001/archpediatrics.2009.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Voepel-Lewis T, Boyd CJ, McCabe SE, et al. Deliberative prescription opioid misuse among adolescents and emerging adults: opportunities for targeted interventions. J Adolesc Health. 2018;63:594–600. 10.1016/j.jadohealth.2018.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Groenewald CB, Rabbitts JA, Gebert JT, Palermo TM. Trends in opioid prescriptions among children and adolescents in the United States: a nationally representative study from 1996 to 2012. Pain. 2016;157:1021–1027. 10.1097/j.pain.0000000000000475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allen JD, Casavant MJ, Spiller HA, Chounthirath T, Hodges NL, Smith GA. Prescription opioid exposures among children and adolescents in the United States: 2000-2015. Pediatrics. 2017;139, e20163382. 10.1542/peds.2016-3382. [DOI] [PubMed] [Google Scholar]
- 9.Matson KL, Johnson PN, Tran V, Horton ER, Sterner-Allison J. Advocacy committee on behalf of pediatric pharmacy advocacy group. Opioid use in children. J Pediatr Pharmacol Therapeut. 2019;24:72–75. 10.5863/1551-6776-24.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Madden K, Reddy AS, De La Cruz MJ, Liu DD, Bruera E. Patterns of storage, use, and disposal of prescription opioids by parents of children with cancer. J Pain Symptom Manag. 2020;59:320–326. 10.1016/j.jpainsymman.2019.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Gaither JR, Leventhal JM, Ryan SA, Camenga DR. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997 to 2012. JAMA Pediatr. 2016;170:1195–1201. 10.1001/jamapediatrics.2016.2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Creswell PD, Gibson C, Theobald J, Meiman JG. Exposures to opioids among Wisconsin children and adolescents, 2002-2016. WMJ. 2019;118:9–15. [PubMed] [Google Scholar]
- 13.Sheridan DC, Laurie A, Hendrickson RG, Fu R, Kea B, Horowitz BZ. Association of overall opioid prescriptions on adolescent opioid abuse. J Emerg Med. 2016;51:485–490. 10.1016/j.jemermed.2016.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, Boyd CJ. Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976-2015. Pediatrics. 2017;139, e20162387. 10.1542/peds.2016-2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miech R, Johnston L, O’Malley PM, Keyes KM, Heard K. Prescription opioids in adolescence and future opioid misuse. Pediatrics. 2015;136:e1169–e1177. 10.1542/peds.2015-1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nalven T, Spillane NS, Schick MR. Risk and protective factors for opioid misuse in American Indian adolescents. Drug Alcohol Depend. 2020;206:107736. 10.1016/j.drugalcdep.2019.107736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zosel A, Bartelson BB, Bailey E, Lowenstein S, Dart R. Characterization of adolescent prescription drug abuse and misuse using the researched abuse diversion and addiction-related surveillance (RADARS(®)) System. J Am Acad Child Adolesc Psychiatry. 2013;52:196–204. 10.1016/j.jaac.2012.11.014. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hudgins JD, Porter JJ, Monuteaux MC, Bourgeois FT. Prescription opioid use and misuse among adolescents and young adults in the United States: a national survey study. PLoS Med. 2019;16, e1002922. 10.1371/journal.pmed.1002922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McDonald EM, Kennedy-Hendricks A, McGinty EE, Shields WC, Barry CL, Gielen AC. Safe storage of opioid pain relievers among adults living in households with children. Pediatrics. 2017;139, e20162161. 10.1542/peds.2016-2161. [DOI] [PubMed] [Google Scholar]
- 20.Patry E, Bratberg JP, Buchanan A, Paiva AL, Balestrieri S, Matson KL. Rx for addiction and medication safety: an evaluation of teen education for opioid misuse prevention. Res Soc Adm Pharm. 2019;15:917–924. 10.1016/j.sapharm.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Edlund MJ, Forman-Hoffman VL, Winder CR, et al. Opioid abuse and depression in adolescents: results from the national survey on drug use and health. Drug Alcohol Depend. 2015;152:131–138. 10.1016/j.drugalcdep.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 22.Griesler PC, Hu MC, Wall MM, Kandel DB. Nonmedical prescription opioid use by parents and adolescents in the US. Pediatrics. 2019;143, e20182354. 10.1542/peds.2018-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beyene K, Aspden T, McNeill R, Sheridan J. Modifiable risk factors for prescription medicine sharing behaviours. Res Soc Adm Pharm. 2019;15:154–163. 10.1016/j.sapharm.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Garbutt JM, Kulka K, Dodd S, Sterkel R, Plax K. Opioids in adolescents’ homes: prevalence, caregiver attitudes, and risk reduction opportunities. Acad Pediatr. 2019;19:103–108. 10.1016/j.acap.2018.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCauley JL, Back SE, Brady KT. Pilot of a brief, web-based educational intervention targeting safe storage and disposal of prescription opioids. Addict Behav. 2013;38:2230–2235. 10.1016/j.addbeh.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Voepel-Lewis T, Farley FA, Grant J, et al. Behavioral intervention and disposal of leftover opioids: a randomized trial. Pediatrics. 2020;145, e20191431. 10.1542/peds.2019-1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martins SS, Ghandour LA. Nonmedical use of prescription drugs in adolescents and young adults: not just a Western phenomenon. World Psychiatr. 2017;16(1):102–104. 10.1002/wps.20350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahic M, Fredheim OM, Borchgrevink PC, Skurtveit S. Use of prescribed opioids by children and adolescents: differences between Denmark, Norway and Sweden. Eur J Pain. 2015;19(8):1095–1100. 10.1002/ejp.632. [DOI] [PubMed] [Google Scholar]
- 29.Nazarzadeh M, Bidel Z, Carson KV. The association between tramadol hydrochloride misuse and other substances use in an adolescent population: phase I of a prospective survey. Addict Behav. 2014;39(1):333–337. 10.1016/j.addbeh.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 30.Maiga DD, Seyni H, Moussa AO, Sidikou A. Mesusage du tramadol par les adolescents et jeunes adultes en situation de rue [Tramadol misuse by adolescents and young adults living on the streets]. Pan Afr Med J. 2012,13:55. [PMC free article] [PubMed] [Google Scholar]
- 31.Bassiony MM, Salah El-Deen GM, Yousef U, et al. Adolescent tramadol use and abuse in Egypt. Am J Drug Alcohol Abuse. 2015;41(3):206–211. 10.3109/00952990.2015.1014959. [DOI] [PubMed] [Google Scholar]
- 32.Alblooshi H, Hulse GK, El Kashef A, et al. The pattern of substance use disorder in the United Arab Emirates in 2015: results of a National Rehabilitation Centre cohort study. Subst Abuse Treat Prev Pol. 2016;11(1):19. 10.1186/s13011-016-0062-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Opioid Overdoes. The world health organization. https://www.who.int/news-room/fact-sheets/detail/opioid-overdose. Accessed May 17, 2021. [Google Scholar]
- 34.Abraham O, Thakur T, Brown R. Prescription opioid misuse and the need to promote medication safety among adolescents. Res Soc Adm Pharm. 2019;15:841–844. 10.1016/j.sapharm.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Prescription drugs. National Institute on drug abuse for teens. Updated may 12, 2020. https://teens.drugabuse.gov/drug-facts/prescription-drugs. Accessed June 1, 2021. [Google Scholar]
- 36.This is not about drugs. Overdose lifeline. https://www.overdoselifeline.org/opioid-heroin-prevention-education-program.html; 2020. Accessed June 1, 2021. [Google Scholar]
- 37.Pattison-Sharp E, Estrada RD, Elio A, Prendergast M, Carpenter DM. School nurse experiences with prescription opioids in urban and rural schools: a cross-sectional survey. J Addict Dis. 2017;36:236–242. 10.1080/10550887.2017.1361725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.About the Program. Operation Prevention; 2020. https://www.operationprevention.com/#about. Accessed June 1, 2021. [Google Scholar]
- 39.Rodriguez DM, Teesson M, Newton NC. A systematic review of computerised serious educational games about alcohol and other drugs for adolescents. Drug Alcohol Rev. 2014;33:129–135. 10.1111/dar.12102. [DOI] [PubMed] [Google Scholar]
- 40.Reconstructors: a plaguing problem. OER commons. Updated 2020 https://www.oercommons.org/courses/reconstructors-a-plaguing-problem; 2007. Accessed June 1, 2021. [Google Scholar]
- 41.Heroin Prevention Program Research and Evaluation. Heroin Prevention Education; 2012. https://www.robertcrown.org/Heroin/researchandeval.html. Accessed June 1, 2021.
- 42.Espino SR. Robert crown center for health education: heroin & prescription drug abuse prevention program spring 2015. Robert crown center for health education. https://www.robertcrown.org/Heroin/pdfs/Heroin%20Program%20Outcomes%20Brief%20Final%20FY15.pdf. Accessed June 1, 2021. [Google Scholar]
- 43.Winstanley EL, Stover AN. The impact of the opioid epidemic on children and adolescents. Clin Therapeut. 2019;41:1655–1662. 10.1016/j.clinthera.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Geisen E, McHenry G, Kroutil L. National Survey on Drug Use and Health (NSDUH): For Cai Specifications for Programming (English Version). Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality; 2018, 2017. Updated September 6, 2017 https://www.samhsa.gov/data/sites/default/files/NSDUHmrbScreenerSpecs2018.pdf. Accessed June 1, 2021. [Google Scholar]
- 45.Huth MM, Broome ME, Mussatto KA, Morgan SW. A study of the effectiveness of a pain management education booklet for parents of children having cardiac surgery. Pain Manag Nurs. 2003;4:31–39. 10.1053/jpmn.2003.7. [DOI] [PubMed] [Google Scholar]
- 46.Andersson Sundell K, Jönsson AK. Beliefs about medicines are strongly associated with medicine-use patterns among the general population. Int J Clin Pract. 2016;70:277–285. 10.1111/ijcp.12781. [DOI] [PubMed] [Google Scholar]
- 47.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–381. 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019;95:103208. 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Linnan S, Walsh-Fez A, Moberg P. Perceptions, awareness, and use of substances in Wisconsin: results of a survey conducted for the Wisconsin strategic prevention framework partnerships for success 2015. Available at: https://uwmadison.app.box.com/s/jo0pmtxljqpisbut4zky2nsw83z2rly3; 2018. Accessed June 1, 2021. [Google Scholar]
- 50.Admassu HG, Tom SE, Sealfon N, Gibson MM, Pradel FG. Summary Report. In: Maryland Public Opinion Survey on Opioids. Baltimore (MD): University of Maryland, Baltimore; 2015; 2015:38. Contract No.: BHA 15-043G/M00B5400484. Supported by the Maryland Department of Health and Mental Hygiene, Behavioral Health Administration. [Google Scholar]
- 51.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. https://www.R-project.org/. Accessed June 1, 2021. [Google Scholar]
- 52.Revelle W. Psych: Procedures for Personality and Psychological Research. Evanston, Illinois, USA: Northwestern University; 2019. https://CRAN.R-project.org/package=psych Version1.9.12. [Google Scholar]
- 53.Guadagnoli E, Velicer WF. Relation of sample size to the stability of component patterns. Psychol Bull. 1988;103(2):265–275. 10.1037/0033-2909.103.2.265. [DOI] [PubMed] [Google Scholar]
- 54.McCabe SE, West BT, Teter CJ, Boyd CJ. Medical and nonmedical use of prescription opioids among high school seniors in the United States. Arch Pediatr Adolesc Med. 2012;166:797–802. 10.1001/archpediatrics.2012.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mazer-Amirshahi M, Mullins PM, Rasooly IR, van den Anker J, Pines JM. Trends in prescription opioid use in pediatric emergency department patients. Pediatr Emerg Care. 2014;30:230–235. 10.1097/PEC.0000000000000102. [DOI] [PubMed] [Google Scholar]
- 56.The Center for Disease and Prevention. Opioid overdose. https://www.cdc.gov/drugoverdose/data/prescribing.html. Accessed June 1, 2021.
- 57.Donaldson CD, Nakawaki B, Crano WD. Variations in parental monitoring and predictions of adolescent prescription opioid and stimulant misuse. Addict Behav. 2015;45:14–21. 10.1016/j.addbeh.2015.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Knekta E, Runyon C, Eddy S. One Size doesn’t fit all: using factor analysis to gather validity evidence when using surveys in your research. CBE-Life Sci Educ. 2019;18 (1):rm1. 10.1187/cbe.18-04-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance - United States, 2017. MMWR Surveill Summ. 2018;67(8):1–114. 10.15585/mmwr.ss6708a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Due to the sensitive nature of the questions asked in this study, survey respondents were assured raw data would remain confidential and would not be shared.