INTRODUCTION
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1) After first being identified in 2019 in Wuhan, China, COVID-19 has spread rapidly to other countries, resulting in the ongoing 2019–2020 coronavirus pandemic (Table 1, Figure 1).2)-4) It has become a global health problem with severe socio-economic impact.3) According to the World Health Organization (WHO) report, people over the age of 60 years are considered a high-risk group if they have an underlying disease, including cardiovascular, respiratory, and metabolic disease.1),2),5) However, patients in the high-risk group often avoid the use of medical facilities or have difficulties due to concerns about COVID-19.4),6) In April 2020, the Korean Society of Heart Failure released clinical recommendations regarding COVID-19 infection in heart failure (HF) patients.
Table 1. Comparison of number of confirmed cases and fatality rate among different countries.
| Nations | Confirmed cases | No. of deaths | Fatality rate (%) |
|---|---|---|---|
| China | 81,518 | 3,305 | 4.1 |
| UK | 25,150 | 1,785 | 7.1 |
| Iran | 44,606 | 2,898 | 6.5 |
| Italy | 105,792 | 12,428 | 11.7 |
| Korea | 9,887 | 165 | 1.7 |
| Spain | 94,417 | 8,214 | 8.7 |
| USA | 186,265 | 3,810 | 2.0 |
Modified from Korea Centers for Disease Control & Prevention report, 31 March 2020.4)
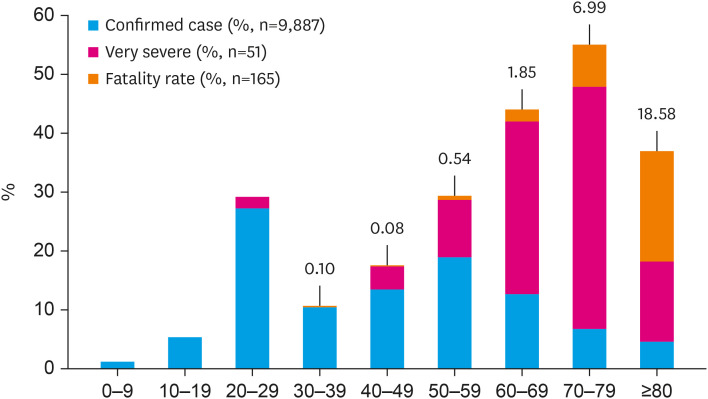
Figure 1. Distribution of confirmed cases, fatality rate, and very severe cases by age for COVID-19 in Korea (modified from Korea Centers for Disease Control & Prevention report, 31 March 2020,4) number is fatality rate).
COVID-19 = coronavirus disease 2019.
CLINICAL RECOMMENDATIONS IN HF PATIENTS REGARDING COVID-19
These recommendations are based on clinical papers and case reports, as well as released public reports from Korea and the WHO, and offer early clinical guidance for the management of HF patients given the current knowledge of COVID-19 (Table 2).
Table 2. COVID-19 implications for patients with heart failure.
| 1. Reduce infections, including influenza and COVID-19, to prevent HF aggravation |
| 2. Reduce the frequency of hospital visits and avoid healthcare-associated infection |
| 3. Maintain adherence to guideline-directed therapy |
| 4. Continue routine use of ACE inhibitors or ARBs to treat HF |
| 5. Check for the development of myocardial damage in COVID-19 patients |
ACE = angiotensin converting enzyme; ARB = angiotensin receptor blocker; COVID-19 = coronavirus disease 2019; HF = heart failure.
First, infection is one of the major precipitating factors of acute decompensation in HF and patients admitted with acute HF precipitated by infection showed a high 90‐day risk of death.7)-9) Therefore, special effort is needed to reduce the risk of SARS-CoV-2 infection; vaccination, frequent handwashing, and breaking the chain of transmission are recommended.10)
Second, in consideration of social distancing measures taken in response to the active COVID-19 outbreak, it may be reasonable to use telephonic visits or proxy prescriptions for patients with stable HF to avoid possible healthcare-associated SARS-CoV-2 infection.4),6),10)
Third, medication based on treatment guidelines in patients with chronic HF is important and continued adherence to guideline-directed therapy is highly recommended. Medications can be continued following telephonic consultation; proxy prescription may be temporarily permitted for patients with HF who have difficulties communicating or a lack of family support.6),10)
Fourth, there are insufficient clinical data in humans to show that angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) either worsen susceptibility to SARS-CoV-2 infection or affect clinical outcomes.11),12) While there may be a theoretical hypothesis that the use of these drugs may increase ACE2 expression, which may make individuals more vulnerable when exposed to SARS-CoV-2, it could lead to a conflict because ACE2 reduces inflammation and enhances the cardio-protective effect.5),13)-15) Therefore, we strongly recommend continuation of the routine use of ACE inhibitors and/or ARBs to treat HF, without being influenced by concerns regarding SARS-CoV-2 infection. It is important to continue using critical drugs prescribed in HF treatment until further animal study data and concrete clinical evidence become available.
Fifth, the development of myocardial damage must be monitored in COVID-19 patients. Although respiratory symptoms are the major clinical manifestations, some patients have cardiovascular damage. Moreover, some patients with underlying cardiovascular disease (CVD) might have an increased risk of death.1),16) Understanding the damage caused by COVID-19 to the cardiovascular system is of the greatest importance.10) However, due to limited clinical data and the lack of a precise method to confirm SARS-CoV-2-induced myocardial injury, it is currently unclear whether patients with COVID-19 and underlying CVD who develop myocardial injury during hospitalization face greater risk and have worse in-hospital outcomes. Therefore, cardiovascular risk assessment in COVID-19 is concerned with recognizing the risk or development of myocardial depression aggravating HF, serious arrhythmia, and acute coronary syndrome; monitoring drug-related heart damage; and providing adequate treatment.5),10),16)
CONCLUSION
HF patients, most of whom are elderly patients, need to be aware that they are a high-risk group with respect to COVID-19 and take precautionary measures to prevent infection. Healthcare providers should help HF patients prevent SARS-CoV-2 infection by educating them on the importance and recommended measures, and the medical team and HF patients should continue using their prescribed medications for HF in accordance with treatment guidelines.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: Cho DH, Yoo BS, Son JW, Kim IC, Park SM.
- Data curation: Yoo BS.
- Investigation: Yoo BS.
- Methodology: Yoo BS.
- Resources: Son JW.
- Supervision: Choi DJ.
- Visualization: Cho DH.
- Writing - original draft: Cho DH, Yoo BS, Kim IC, Park SM.
- Writing - review & editing: Yoo BS.
References
- 1.Lam TT, Shum MH, Zhu HC, et al. Identifying SARS-CoV-2 related coronaviruses in Malayan pangolins. Nature. doi: 10.1038/s41586-020-2169-0. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) [Internet] Geneva: WHO; 2020. [cited 2020 Mar 31]. Available from https://www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19) [Google Scholar]
- 3.World Health Organization (WHO) Coronavirus disease 2019 [Internet] Geneva: WHO; 2020. [cited 2020 Mar 31]. Available from https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Google Scholar]
- 4.Korea Centers for Disease Control and Prevention (KCDC) The updates on COVID-19 in Korea as of 31 March [Internet] Cheongju: KCDC; 2020. [cited 2020 Mar 31]. Available from https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030. [Google Scholar]
- 5.Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (US) Coronavirus disease 2019 (COVID-19) guideline documents [Internet] Washington, D.C.: CDC; 2020. [cited 2020 Mar 31]. Available from https://www.cdc.gov/coronavirus/2019-ncov/communication/guidance-list.html?Sort=Date%3A%3Adesc. [Google Scholar]
- 7.Lee SE, Lee HY, Cho HJ, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF) Korean Circ J. 2017;47:341–353. doi: 10.4070/kcj.2016.0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arrigo M, Gayat E, Parenica J, et al. Precipitating factors and 90-day outcome of acute heart failure: a report from the intercontinental GREAT registry. Eur J Heart Fail. 2017;19:201–208. doi: 10.1002/ejhf.682. [DOI] [PubMed] [Google Scholar]
- 9.Vardeny O, Solomon SD. Influenza and heart failure: a catchy comorbid combination. JACC Heart Fail. 2019;7:118–120. doi: 10.1016/j.jchf.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 10.American College of Cardiology. COVID-19 clinical guidance for the cardiovascular care team [Internet] Washington, D.C.: American College of Cardiology; 2020. [cited 2020 Mar 31]. Available from https://www.acc.org//~/media/Non-Clinical/Files-PDFs-Excel-MS-Word-etc/2020/02/S20028-ACC-Clinical-Bulletin-Coronavirus.pdf. [Google Scholar]
- 11.European Society of Cardiology. Position statement of the ESC council on hypertension on ACE-inhibitors and angiotensin receptor blockers [Internet] Sophia Antipolis Cedex: ESC; 2020. [cited 2020 Mar 31]. Available from https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang. [Google Scholar]
- 12.American College of Cardiology. HFSA/ACC/AHA statement addresses concerns. Re: using RAAS antagonists in COVID-19 [Internet] Washington, D.C.: American College of Cardiology; 2020. [cited 2020 Mar 31]. Available from https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19. [Google Scholar]
- 13.Ferrario CM, Jessup J, Chappell MC, et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111:2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 14.Kuba K, Imai Y, Rao S, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Imai Y, Kuba K, Rao S, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]