Abstract
Background and Objectives
During the coronavirus disease 2019 (COVID-19) pandemic, virtual visits (VVs) were recommended as an innovative and necessary alternative for patients with heart failure (HF). To assess the feasibility and acceptability of VVs in patients with HF, pulmonary hypertension (PH), and heart transplant (HT).
Methods
We designed a single-centre cohort study. Consecutive VVs performed in our HF unit were analysed. The period comprehended between January 1st and March 19th (before COVID-19) and March 20th and June 30th (during COVID-19) was compared. We assessed acceptability, feasibility and the need for diagnostic studies, in-person medical evaluation, and hospitalization at 30 days.
Results
HF unit medical doctors conducted 22 VVs in the pre-COVID period and 416 VVs during the COVID period. The VV was able to be performed in all patients scheduled for it and 44% answered the survey. Ninety percent of the patients who answered the survey strongly agreed that VVs were easy to be carried out. All the patients “strongly agreed” or “agreed” that their health problem could be resolved. Most patients (95%) rated the global experience as very good or excellent, with an overall average rate of 9.76±0.5 out of 10. We found no differences regarding the requirement of diagnostic studies, in-person medical evaluation and hospitalization during the first month after VVs between the 2 periods.
Conclusions
VVs were feasible, presented high acceptability, and the overall experience was positive in patients with HF, PH, and HT, being this modality a valuable tool that complements in-person care.
Keywords: Heart failure, Telehealth, COVID-19, SARS-CoV-2, Pandemic
INTRODUCTION
Coronavirus disease 2019 (COVID-19) has caused an unprecedented crisis for patients, clinicians, and healthcare systems in different regions of the world. The evolution of the disease has motivated implementing preventive measures in the population. Argentina declared a preventive and compulsory social isolation with the aim of slowing the progression of the disease. However, a collateral adverse consequence of the lockdown was the limited access to health system facilities, affecting the management and treatment of both acute and chronic cardiovascular diseases.1),2),3),4),5),6),7) The high adherence of the population to this effective measure to reduce the spread and impact of the COVID-19 pandemic, caused a significant decrease in medical consultations. Moreover, many hospitals have reduced or even cancelled ambulatory outpatient clinic appointments, although being essential to the follow-up and care of chronic diseases, such as heart failure (HF), which requires frequent medical contact and presents higher probability of hospitalization.8)
Synchronized audio/video interactions, also known as virtual visits (VVs), have been suggested as innovative and necessary alternatives to in-person care.9) VVs provide a platform for real-time interactive telehealth interactions between patients and clinicians, using commonly-available devices. Telehealth has a critical role in emergency responses, including the ability to rapidly deploy large numbers of providers; facilitate triage; supply clinical services when clinics are unable to meet demand; and enable to maintain an uninterrupted diagnosis, management and follow-up of chronic diseases.10)
North and South American countries have become intense zones for COVID-19 transmission, and in Argentina there is an increasing number of daily confirmed cases. On March 19th, a nation-wide lockdown was established in Argentina. The government later extended the strict lockdown due to a large number of diagnosed COVID-19 cases. We present our HF unit's transformation from in-person outpatient visits to a largely virtual practice in response to the COVID-19 pandemic lockdown to provide care to patients with HF, pulmonary hypertension (PH) and heart transplant (HT) in a specialized cardiovascular centre in Argentina. The objective was to assess the feasibility and acceptability of VVs. Diagnostic studies, in-person medical evaluation, and hospitalization were evaluated at 30 days during the pandemic.
METHODS
Design
Single-centre cohort study, performing a retrospective analysis of prospectively collected data.
Population
All VVs performed in our HF, PH or HT unit were included consecutively. The number of VVs conducted over the period comprehended between January 1st and March 19th (before COVID-19) were compared to the amount performed throughout the period between March 20th and June 30th (during COVID-19) while lockdown established. Consultations for medical prescriptions were excluded.
VVs
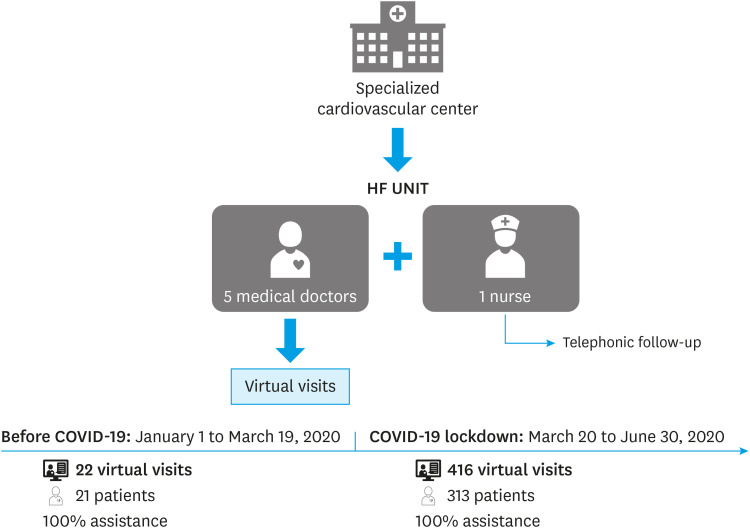
The consultations were conducted by 5 doctors specialized in HF. All patients were trained on how to record vital signs and weight and detect signs of congestion, and written information about care during the pandemic. In the case of HT patients, a nurse specialized in HF also made telephonic follow-up.
To avoid possible difficulties with accessibility or capacity to use different virtual platforms, we based the VVs system in video calls.
Endpoints
During the COVID-19 pandemic a self-administered survey was sent to the patient after each VV. The acceptability was evaluated using the Consumer Assessment of Healthcare Providers and Systems survey. The questionnaire included queries with various response options (e.g. Likert scale, multiple choice, and free text form).
- Was it easy for you to do the VV? 5-point Likert scale ranging from “strongly agree” to “strongly disagree”
- The VV allowed you to solve the problem for which you consulted? 5-point Likert scale ranging from “strongly agree” to “strongly disagree”
- The doctor showed interest in your problem? 5-point Likert scale ranging from “strongly agree” to “strongly disagree”
- Please rate your overall experience. Multiple choice from 1 to 10 where 1 is bad and 10 is excellent.
- Additional comments and observations: free text form.
During the COVID-19 period, the feasibility was evaluated based on the proportion of completed VVs.
We compared the proportion of patients that required laboratory, radiographic, tomographic, ultrasound, and coronary angiography studies during the first month after the VV as well as the number of patients that required in-person medical evaluation and hospitalization over the range of 30 days during each analyzed period.
Statistical analysis
Continuous variables were expressed as mean and standard deviation or median and interquartile range according to the observed distribution. Kolmogorov Smirnov or Shapiro-Wilk test according to the sample size was used to determine distribution. Categorical variables were expressed as numbers and percentages. To compare continuous variables, the Student's t-test or the Mann-Whitney U test was used, according to the distribution. Categorical variables were expressed as numbers and percentages. Comparisons between proportions were performed using the χ2 test or Fisher's exact test, according to the frequency of expected values. Two-tailed p values <0.05 were considered statistically significant.
SPSS statistics, version 23.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis.
RESULTS
The HF unit medical doctors made 22 VVs (0.28 per day) and 416 (4.16 per day) in the before and during COVID-19 period respectively. This represents an increase of 2,077% in the group of patients with HF as main diagnosis, 1,400% in those with PH and 200% in HT patients.
The VV was able to be performed in all patients scheduled for it (Figure 1).
Figure 1. HF unit and number of VVs in before and during COVID-19 period.
COVID-19 = coronavirus disease 2019; HF = heart failure; VV = virtual visit.
Patient's VVs baseline characteristics during the period before and during COVID-19 are shown in Table 1. We found a statistical difference in the main diagnosis of patients assisted during the pandemic, finding an increase in those with HF (81.8% vs. 94.2%; p=0.005).
Table 1. Baseline characteristics in the before and during COVID-19 period.
| Before COVID-19 | During COVID-19 | p value | ||
|---|---|---|---|---|
| Age (years) | 60.7±15.0 | 65.7±15.0 | 0.13 | |
| Male (sex) | 16 (72.7) | 279 (67.1) | 0.58 | |
| Hypertension | 9 (40.9) | 205 (49.3) | 0.44 | |
| Dyslipidaemia | 12 (54.5) | 204 (49) | 0.61 | |
| Current smoker | 1 (4.5) | 33 (7.9) | 0.56 | |
| Main diagnosis | 0.005 | |||
| Heart failure | 18 (81.8) | 392 (94.2) | ||
| PH | 1 (4.5) | 15 (3.6) | ||
| Heart transplant | 3 (13.6) | 9 (2.2) | ||
| First time visit | 2 (9.1) | 42 (10.1) | 0.8 | |
Data are shown as mean±standard deviation or number (%).
COVID-19 = coronavirus disease 2019; PH = pulmonary hypertension.
In both periods, we observed the same proportion of patients referred for medical consultations in the unit for the first time.
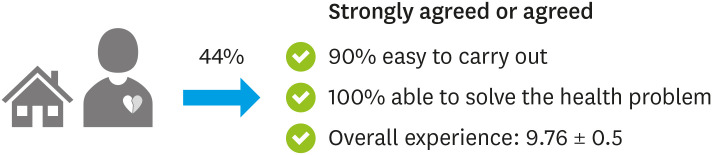
Out of 313 patients evaluated during the pandemic, 44% answered the survey. Ninety percent of the patients strongly agreed or agreed that the VV was easy to be carried out. All patients “strongly agreed” or “agreed” that their health problem was able to be solved through the VV, and that the doctor showed interest in their health problem (Figure 2).
Figure 2. Virtual visit acceptability coronavirus disease 2019 pandemic.
The vast majority of patients (95%) rated the experience as very good or excellent (9 or 10 points), with an overall average rate of 9.76±0.5 out of 10.
We found no differences regarding the requirement of diagnostic studies, in-person medical evaluation and hospitalization during the first month after the VV between both periods (Table 2).
Table 2. In-person evaluation, diagnostic studies and hospitalization at 30 days in the before and during COVID-19 period.
| Events at 30 days | Before COVID-19 | During COVID-19 | p value |
|---|---|---|---|
| In-person evaluation | 8 (36.4) | 109 (26.2) | 0.20 |
| Diagnostic studies | 5 (22.7) | 136 (32.7) | 0.33 |
| Hospitalization | 1 (4.5) | 24 (5.8) | 0.80 |
Data are shown as number (%).
COVID-19 = coronavirus disease 2019.
DISCUSSION
In a hospital specialized in cardiovascular diseases in Argentina, during the lockdown, a mass migration to VVs took place in a HF unit. VVs has rapidly moved to the frontline of clinical practice due to the need for prevention and mitigation strategies to continue caring and monitoring our patients with HF. VVs were feasible, with high acceptability among HF patients. Overall, the VVs experience was positive, with high ability to solve the health problems for which the patient consulted. Furthermore, our study shows the usefulness of this modality to request diagnostic studies. VVs were essential to maintain our HF unit standards of care in patients recently hospitalized for acute decompensated HF, in order to carry out the medical follow-up 1 week after discharge.
Although the increase in VVs in the group of patients with HT was considerable, it was not as high as in patients with other diseases, probably due to the fact that there is a specialized nurse in our unit who monitors these patients via telephone.
The rate of requirement for complementary studies, in-person medical evaluation and hospitalization was remarkably similar in both periods. It is important to mention that more than a quarter of the patients required in-person medical evaluation, which reflects that VVs are a complementary modality for this group. We believe that in-person healthcare cannot be entirely replaced by remote healthcare, but in a pandemic context, telehealth is valuable since it minimizes the risk of infection in patients, their relatives and healthcare personnel.
As previously reported, our patients showed very high acceptability with VVs. Randomized trials have also shown that clinical consultations conducted through a video link tend to be associated with high satisfaction among patients and staff; with no difference in disease progression and lower transactional costs compared with traditional clinic based care.11),12)
Telehealth for HF management during COVID-19 outbreak was recommended in a recent statement from Heart Failure Society of America9) and European Society of Cardiology.13) Prior to the advent of COVID-19, impediments to the establishment of VV programs were considerable, including political, regulatory, reimbursement, social barriers and lack of familiarity with technologies among both clinicians and patients.14)
The value of VVs was recently demonstrated in a pilot randomized clinical trial, comparing 7-day post-discharge VVs to in-person outpatient clinic visits among patients hospitalized for HF. The no-show rate in the VV trended lower than the one observed in the in-person modality. There was no difference in the rate of hospital readmissions, emergency room visits or death, even though the study was not powered for clinical outcomes.15) In our study, the no-show rate was much lower than the previously reported, probably because during the pandemic the alternatives to VVs were limited.
As seen from early data from Asia, then in Europe, we were prepared for the worst scenario, a pandemic with sick healthcare workers: quarantined at home due to exposure to COVID-19, or absent due to the presence of risk factors for COVID-19 (advanced age, comorbidities), resulting in patients with chronic diseases being unable to receive medical healthcare. Our centre is a third level national reference site, located in the city of Buenos Aires, the area that concentrates the largest number of COVID-19 cases in the country. We carried out a rotating in-person and virtual medical scheme, and rapidly deployed VVs as a way of providing longitudinal care to patients with cardiovascular diseases while also reducing patient's exposure and slowing the spread of disease. This modality was particularly useful for monitoring patients who could not travel to Buenos Aires due to the national lockdown, greatly limiting travel and exposure and permitting uninterrupted care. It was also especially useful for HT patients, in combination with nurse telephonic follow-up, as they are at higher risk for severe forms of COVID-19 due to immunosuppression.
VVs provided access to health care when it was significantly reduced or even absent, by providing a platform to continue receiving medical care.9) Telehealth emerged as an innovative and necessary alternative. We demonstrated the role of telehealth integrated into a HF disease management unit during COVID-19 pandemic lockdown. Pandemics pose unique challenges to the delivery of health care, although telehealth will not solve them all. VVs are an essential tool, especially in settings where the infrastructure remains intact and physicians are available, allowing continuous follow-up of HF patients in the course of a public health emergency.16)
Based on our experience, recommendations are summarized in Table 3 for those units looking forward to deploying VVs.
Table 3. Recommendations for VVs in patients with heart failure, pulmonary hypertension, and heart transplant.
| Recommendations for VVs |
|---|
| 1) Use simple virtual platforms for VVs |
| 2) Educate about the recording of vital signs/daily weight |
| 3) Instruct patients prior to hospital discharge about VVs |
| 4) Use this modality as a complement to in-person medical consultation |
| 5) Multidisciplinary work with specialized nurses |
| 6) VVs to avoid the trip of immunosuppressed transplant patients when possible |
| 7) VVs as triage to guide patients to in-person evaluation in ambulatory clinic or emergency department |
| 8) In each VVs, remind patients the alarm signs and symptoms for consultation in the emergency department |
VV = virtual visit.
In conclusion, a pandemic constitutes a challenge to continue medical care of patients with chronic diseases, making the establishment of telehealth systems a vital strategy to ensure continued delivery of healthcare. In a specialized HF unit, VVs have rapidly moved to the front line of clinical practice during COVID-19 pandemic lockdown. VVs were feasible, presented high acceptability, and the overall experience was positive in patients with HF, PH and HT, being this modality a valuable tool that complements in-person care.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Burgos LM, Benzadón M, Candiello A, Alves de Lima A.
- Data curation: Burgos LM, Cabral MH.
- Formal analysis: Burgos LM, Benzadón M, Candiello A.
- Investigation: Burgos LM, Benzadón M.
- Methodology: Burgos LM, Benzadón M.
- Project administration: Benzadón M, Conde D.
- Resources: Burgos LM, Candiello A, Cabral MH, Alves de Lima A, Diez M.
- Software: Burgos LM, Candiello A.
- Supervision: Conde D, Alves de Lima A, Diez M.
- Validation: Diez M.
- Visualization: Cabral MH, Conde D, Alves de Lima A, Belardi J, Diez M.
- Writing - original draft: Burgos LM, Benzadón M, Candiello A, Diez M.
- Writing - review & editing: Candiello A, Cabral MH, Conde D, Alves de Lima A, Belardi J, Diez M.
References
- 1.Bozovich GE, Alves de Lima A, Fosco M, et al. Collateral damage of COVID-19 pandemic in private healthcare centres of Argentina. Medicina (B Aires) 2020;80 Suppl 3:37–41. [PubMed] [Google Scholar]
- 2.De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Solomon MD, McNulty EJ, Rana JS, et al. The COVID-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 4.Bromage DI, Cannatà A, Rind IA, et al. The impact of COVID-19 on heart failure hospitalization and management: report from a heart failure unit in London during the peak of the pandemic. Eur J Heart Fail. 2020;22:978–984. doi: 10.1002/ejhf.1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Hamamsy I, Brinster DR, DeRose JJ, et al. The COVID-19 pandemic and acute aortic dissections in New York: a matter of public health. J Am Coll Cardiol. 2020;76:227–229. doi: 10.1016/j.jacc.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall ME, Vaduganathan M, Khan MS, et al. Reductions in heart failure hospitalizations during the COVID-19 pandemic. J Card Fail. 2020;26:462–463. doi: 10.1016/j.cardfail.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burgos LM, Diez M, Villalba L, Miranda RM, Belardi J. Impact of the COVID-19 pandemic on heart failure hospitalizations. Medicina (B Aires) 2020;80:315–316. [PubMed] [Google Scholar]
- 8.Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2:407–413. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 9.Gorodeski EZ, Goyal P, Cox ZL, et al. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail. 2020;26:448–456. doi: 10.1016/j.cardfail.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020;26:309–313. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ignatowicz A, Atherton H, Bernstein CJ, et al. Internet videoconferencing for patient-clinician consultations in long-term conditions: a review of reviews and applications in line with guidelines and recommendations. Digit Health. 2019 doi: 10.1177/2055207619845831. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Armfield NR, Bradford M, Bradford NK. The clinical use of Skype--For which patients, with which problems and in which settings? A snapshot review of the literature. Int J Med Inform. 2015;84:737–742. doi: 10.1016/j.ijmedinf.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 13.The European Society of Cardiology (ESC) ESC guidance for the diagnosis and management of CV disease during the COVID-19 pandemic [Internet] Sophia Antipolis: ESC; 2020. [cited 2020 Jun 24]. Available from https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance. [Google Scholar]
- 14.Fraiche AM, Eapen ZJ, McClellan MB. Moving beyond the walls of the clinic: opportunities and challenges to the future of telehealth in heart failure. JACC Heart Fail. 2017;5:297–304. doi: 10.1016/j.jchf.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 15.Gorodeski EZ. Virtual visits in heart failure care transitions (ViV-HF) [Internet] Philadelphia (PA): Heart Failure Society of America; 2019. [cited 2020 Jul 1]. Available from https://www.tctmd.com/news/virtual-doctor-visits-reduce-missed-appointments-after-hf-hospitalizations-viv-hf. [Google Scholar]
- 16.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]