Human monkeypox is known as a self-limiting zoonotic illness, characterised by a distinct febrile prodrome accompanied by skin eruptions.1 However, this classic clinical course of human monkeypox could be altered by several factors, including source and route of infection,2, 3 previous smallpox vaccination, age, pregnancy, and immunosuppression (including HIV infection).1, 4 The global spread of human monkeypox among men who have sex with men (MSM) has shown sexual contact as a new mode of human monkeypox transmission. The associated novel clinical and epidemiological patterns deserve comprehensive investigations.
In The Lancet, Eloy José Tarín-Vicente and colleagues5 provide some useful data on the sexual behaviour, clinical presentation, and virological outcomes for 181 patients with PCR-confirmed human monkeypox who were consecutively selected from three sexual health clinics in Spain. The participants in Tarín-Vicente and colleagues' study5 had a median age of 37·0 years (IQR 31·0–42·0); 166 (92%) identified as gay men, bisexual men, or other MSM and 15 (8%) identified as heterosexual men or heterosexual women; and 161 (89%) were Spanish or from south and central America (20 [11%] participants were other ethnicities or had missing data]). The monkeypox infections were linked to previous sexual exposures and the median number of sexual partners in the past 3 months was 6·5 (IQR 3·0–16·0). 72 (40%) participants were HIV-positive (of whom 71 [99%] were on antiretroviral therapy [ART]), 31 (17%) had concurrent sexually transmitted infections, and 57 (31%) had used recreational drugs during sex. The types of sexual practices reported were oral insertive sex (160 [88%] participants), oral receptive sex (158 [87%]), anal insertive sex (131 [72%]), anal receptive sex (108 [60%]), and vaginal insertive sex (11 [6%]). 32 (18%) participants had received the childhood smallpox vaccination. Monkeypox virus was detected by PCR in 178 (99%) of 180 skin lesion swabs, 43 (78%) of 55 anal swabs, and 82 (70%) of 117 throat swabs. After a median incubation period of 7·0 days (IQR 5·0–10·0), all participants developed skin lesions, mainly in the anogenital (in 141 [78%] participants) and the oral and perioral regions (78 [43%]). 94 (52%) participants had no distinct systemic prodromes and 70 (39%) developed complications that required medical treatment, mainly painful proctitis, tonsillitis, penile oedema, and skin abscesses. Compared with other types of sexual practices, anal receptive sex was associated with higher frequency of viral prodrome (67 [62%] of 108 vs 16 [28%] of 58; p<0·0001), more frequent proctitis (41 [38%] vs four [7%]; p<0·0001), but with no significant difference in incubation period. 18 (95%) of the 19 participants with ulcerative tonsillitis had practised oral receptive sex. Viral load was higher in skin lesion than throat swabs (mean cycle threshold value 23 [SD 4] vs 32 [6]; p<0·0001). It took a median of 10 days (IQR 7–13) from the onset of lesions for a dry crust to form, and the clinical outcomes were not different in relation to HIV status and childhood smallpox vaccination.
The findings of Tarín-Vicente and colleagues' study5 are similar to studies outside countries where human monkeypox is endemic.6, 7, 8 There have been no previous reports of proctitis from countries where monkeypox is endemic, but atypical presentations, such as genital rash as the first symptom and lack of distinct febrile prodrome, have been reported from Nigeria.4, 9 Sexual contact was suspected as a mode of transmission during the 2017 outbreak of human monkeypox in Nigeria, but this was not proven.10 The lack of complete protective benefit of childhood smallpox vaccination as observed by Tarín-Vicente and colleagues is not unusual.1, 11 Similar to other studies outside countries where monkeypox is endemic,6, 7, 8 HIV status did not affect the clinical outcomes of human monkeypox in the study by Tarín-Vicente and colleagues.5 By contrast, patients in Nigeria with human monkeypox who were HIV-positive had low CD4 cell count and more severe disease.4 Further studies are needed to understand the protective benefit of effective ART among patients co-infected with HIV and human monkeypox virus, if any.
Two observational studies on the clinical course of human monkeypox have been recently published,7, 8 and although their findings are largely similar to those of Tarín-Vicente and colleagues, there are some differences. In Thornhill and colleagues' study,8 528 patients with human monkeypox were enrolled from 16 countries outside regions where the virus is endemic. Monkeypox virus was detected in 29 of 32 semen samples, although the authors noted that it is not known whether the viral DNA detected in these specimens was replication competent; there were complications such as conjunctival lesions, acute kidney injury, and a self-limiting myocarditis,8 which were not observed by Tarín-Vicente and colleagues. The study by Patel and colleagues7 investigated 197 patients with human monkeypox in central London, UK, and described a biphasic appearance of lesions, a few patients with more than 100 lesions (eight [4·1%] participants), and a patient with rectal perforation managed conservatively. However, Tarín-Vicente and colleagues report novel findings regarding specific types of sexual practice (eg, anal receptive sex) and how these practices related to clinical outcomes (ie, more frequent proctitis and systemic symptoms). Compared with studies outside countries where monkeypox is endemic,8, 12, 13 Tarín-Vicente and colleagues used a larger sample size (n=144) to define the viral prodrome and incubation period of human monkeypox, and to estimate the differences in viral load in relation to different mucocutaneous sites. On the basis of history of sexual exposures, predominant anogenital skin lesions, and higher viral loads in skin than throat swabs, the authors proposed skin-to-skin contact rather than respiratory route as the dominant mode of human monkeypox transmission outside countries where the virus is endemic. However, Tarín-Vicente and colleagues did not test other bodily fluids, such as blood and semen, although it is still unclear whether these bodily fluids contribute to monkeypox virus transmission. The authors also did not evaluate longitudinal changes in cycle threshold values that could have differential peaks at the different lesion sites during the natural history of human monkeypox.11, 13
Nonetheless, Tarín-Vicente and colleagues have improved our understanding of the clinical and epidemiological characteristics of human monkeypox outside countries where the virus is endemic, especially regarding the relationship between sexual behaviour and the clinical course of the disease. Future prospective clinical studies are needed to fully define the specifics of the natural history of human monkeypox for all affected countries. Additionally, with the declaration of monkeypox as a Public Health Emergency of International Concern,14 global collaboration is needed to understand and address behavioural drivers of the global spread of human monkeypox and to ensure interventions strengthen surveillance, improve awareness and clinical management and infection prevention and control skills regarding human monkeypox, especially among health-care workers, address stigma and discrimination in the most affected social groups, and ensure equitable access to treatments and vaccines.
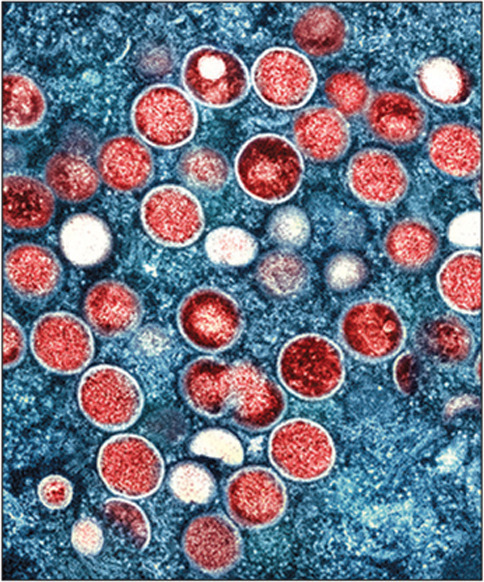
© 2022 Niaid, National Institutes Of Health/SPL
Acknowledgments
I declare no competing interests. I am the President of the Nigerian Infectious Diseases Society (unpaid).
References
- 1.Jezek Z, Szczeniowski M, Paluku KM, Mutombo M. Human monkeypox: clinical features of 282 patients. J Infect Dis. 1987;156:293–298. doi: 10.1093/infdis/156.2.293. [DOI] [PubMed] [Google Scholar]
- 2.Jezek Z, Grab B, Szczeniowski M, Paluku KM, Mutombo M. Clinico-epidemiological features of monkeypox patients with an animal or human source of infection. Bull World Health Organ. 1988;66:459–464. [PMC free article] [PubMed] [Google Scholar]
- 3.Reynolds MG, Yorita KL, Kuehnert MJ, et al. Clinical manifestations of human monkeypox influenced by route of infection. J Infect Dis. 2006;194:773–780. doi: 10.1086/505880. [DOI] [PubMed] [Google Scholar]
- 4.Ogoina D, Iroezindu M, James HI, et al. Clinical course and outcome of human monkeypox in Nigeria. Clin Infect Dis. 2020;71:e210–e214. doi: 10.1093/cid/ciaa143. [DOI] [PubMed] [Google Scholar]
- 5.Tarín-Vicente EJ, Alemany A, Agud-Dios M, et al. Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study. Lancet. 2022 doi: 10.1016/S0140-6736(22)01436-2. published online Aug 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bragazzi NL, Kong JD, Mahroum N, et al. Epidemiological trends and clinical features of the ongoing monkeypox epidemic: a preliminary pooled data analysis and literature review. J Med Virol. 2022 doi: 10.1002/jmv.27931. published online June 12. [DOI] [PubMed] [Google Scholar]
- 7.Patel A, Bilinska J, Tam JCH, et al. Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: descriptive case series. BMJ. 2022;378 doi: 10.1136/bmj-2022-072410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thornhill JP, Barkati S, Walmsley S, et al. Monkeypox virus infection in humans across 16 countries—April–June 2022. N Engl J Med. 2022 doi: 10.1056/NEJMoa2207323. published online July 21. [DOI] [PubMed] [Google Scholar]
- 9.Yinka-Ogunleye A, Aruna O, Dalhat M, et al. Outbreak of human monkeypox in Nigeria in 2017–18: a clinical and epidemiological report. Lancet Infect Dis. 2019;19:872–879. doi: 10.1016/S1473-3099(19)30294-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ogoina D, Izibewule JH, Ogunleye A, et al. The 2017 human monkeypox outbreak in Nigeria—report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. PLoS One. 2019;14 doi: 10.1371/journal.pone.0214229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pittman PR, Martin JW, Kingebeni PM, et al. Clinical characterization of human monkeypox infections in the Democratic Republic of the Congo. medRxiv. 2022 doi: 10.1101/2022.05.26.22273379. published online May 29. (preprint). [DOI] [Google Scholar]
- 12.Miura F, van Ewijk CE, Backer JA, et al. Estimated incubation period for monkeypox cases confirmed in the Netherlands, May 2022. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.24.2200448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adler H, Gould S, Hine P, et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022;22:1153–1162. doi: 10.1016/S1473-3099(22)00228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO WHO Director-General declares the ongoing monkeypox outbreak a Public Health Emergency of International Concern. July 23, 2022. https://www.who.int/europe/news/item/23-07-2022-who-director-general-declares-the-ongoing-monkeypox-outbreak-a-public-health-event-of-international-concern


