Abstract
Background
Racial and social disparities exist in outcomes related to cancer and cardiovascular disease (CVD).
Objectives
The aim of this cross-sectional study was to study the impact of social vulnerability on mortality attributed to comorbid cancer and CVD.
Methods
The Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research database (2015-2019) was used to obtain county-level mortality data attributed to cancer, CVD, and comorbid cancer and CVD. County-level social vulnerability index (SVI) data (2014-2018) were obtained from the CDC’s Agency for Toxic Substances and Disease Registry. SVI percentiles were generated for each county and aggregated to form SVI quartiles. Age-adjusted mortality rates (AAMRs) were estimated and compared across SVI quartiles to assess the impact of social vulnerability on mortality related to cancer, CVD, and comorbid cancer and CVD.
Results
The AAMR for comorbid cancer and CVD was 47.75 (95% CI: 47.66-47.85) per 100,000 person-years, with higher mortality in counties with greater social vulnerability. AAMRs for cancer and CVD were also significantly greater in counties with the highest SVIs. However, the proportional increase in mortality between the highest and lowest SVI counties was greater for comorbid cancer and CVD than for either cancer or CVD alone. Adults <45 years of age, women, Asian and Pacific Islanders, and Hispanics had the highest relative increase in comorbid cancer and CVD mortality between the fourth and first SVI quartiles, without significant urban-rural differences.
Conclusions
Comorbid cancer and CVD mortality increased in counties with higher social vulnerability. Improved education, resource allocation, and targeted public health interventions are needed to address inequities in cardio-oncology.
Key Words: disparities, epidemiology, risk factor
Abbreviations and Acronyms: AAMR, age-adjusted mortality rates; CDC, Centers for Disease Control and Prevention; CVD, cardiovascular disease; ICD, International Classification of Diseases; RR, rate ratio; SDOH, social determinants of health; SVI, social vulnerability index
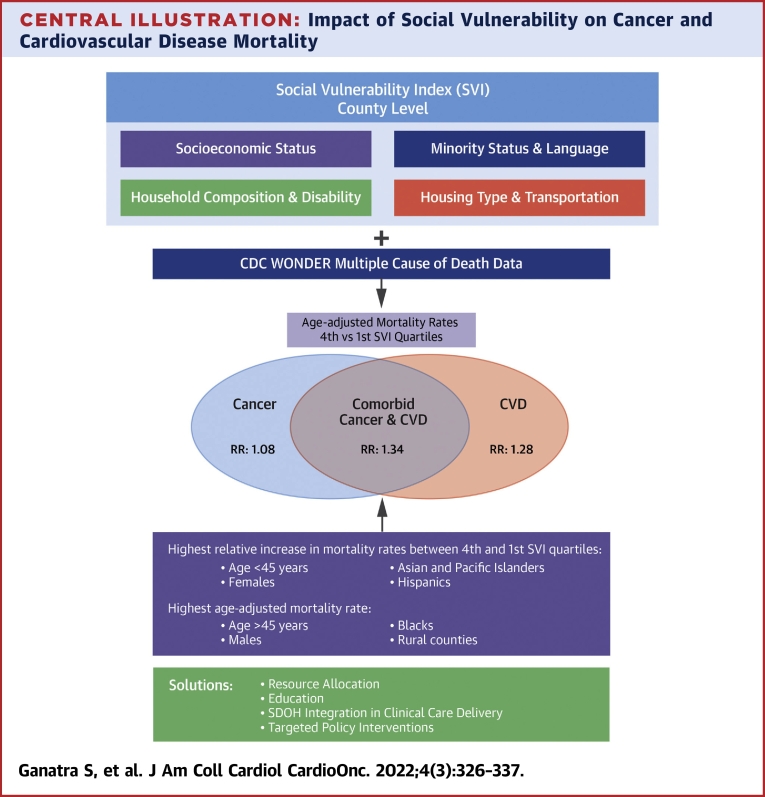
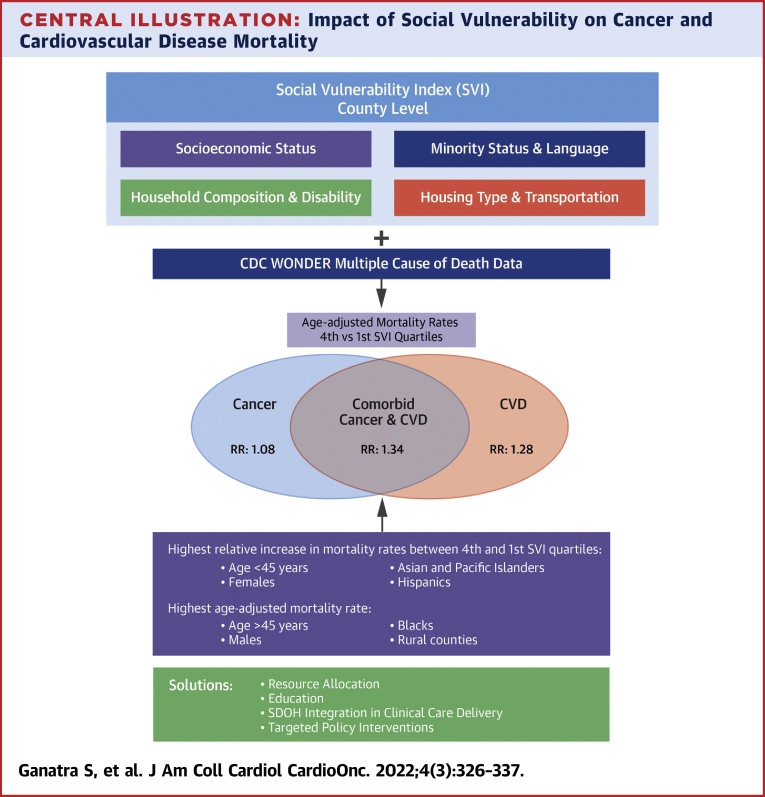
Central Illustration
Cancer and cardiovascular disease (CVD) are the 2 most common causes of morbidity and mortality in the United States. Moreover, there is a growing population of patients who have both cancer and CVD, and data suggest that the economic burden faced by those with the dual diagnoses of cancer and CVD is significantly higher than that faced by those with cancer or CVD alone.1
Existing evidence suggests that socioeconomic gradients and inequality play an important role in the incidence, treatments, and outcomes of both cancer and CVD.2, 3, 4 The conditions in the environments where people are born, live, learn, work, play, and age form social determinants of health (SDOH) that affect a wide range of health, functional, and quality-of-life risks and outcomes. The 5 major domains on which SDOH are based are: 1) economic stability; 2) educational access and quality; 3) health care access and quality; 4) neighborhood build and environment; and 5) social and community context. Despite advances in preventive and treatment strategies for CVD, a substantial increase in the prevalence of cardiometabolic risk factors (obesity, physical inactivity, diabetes, hypertension) during the past 2 decades5 has led to a rise in premature and overall cardiometabolic mortality in the United States.6 This is particularly notable among Black individuals living in poor neighborhoods of southeastern states.7,8 Although exponential growth in cancer therapeutics has improved overall outcomes for patients with many cancers, cancer-related mortality remains prominent in rural areas, with vast urban-rural differences.9 Despite advances in our understanding about the impact of SDOH on cancer and CVD individually, the magnitude of their impact on patients with the dual diagnoses of cancer and CVD remains understudied.
“Social vulnerability” refers to the negative role of external stressors on an individual’s health and, in turn, on communities at large. The social vulnerability index (SVI) is one of the most comprehensive indicators of SDOH. It encompasses socioeconomic status, household composition, disability, minority status, language, and transportation and was originally developed to measure a community’s resilience to natural disasters or disease outbreaks.10 The SVI has been previously used to study the impact of social vulnerability on health outcomes, including cognition, disability, and overall mortality.11,12
The relationship between county-level SVI and mortality attributed to the dual diagnoses of cancer and CVD has not been explored previously. We sought to assess the association between county-level SVI and mortality secondary to comorbid cancer and CVD (defined as death due to concomitant malignant neoplasm and CVD) for successively increasing levels of social adversity. We also assessed the impact of SVI on comorbid cancer and CVD mortality relative to mortality secondary to cancer or CVD alone.
Methods
Data sources
Mortality and population data
We used the Centers for Disease Control and Prevention (CDC) Wide-Ranging Online Data for Epidemiologic Research multiple-cause-of-death database to obtain U.S. county-level mortality and population estimates from 2015 to 2019.13,14 Data are based on death certificates for U.S. residents. Each death certificate contains a single underlying cause of death, up to 20 additional multiple causes, and demographic data. The underlying cause of death is defined as the “disease or injury which initiated the train of events leading directly to death.” When more than 1 cause or condition is listed on the death certificate, the underlying cause is determined by the sequence of conditions on the certificate, provisions of the International Classification of Diseases (ICD), and associated selection rules and modifications. The population estimates are U.S. Census Bureau estimates of U.S. national, state, and county resident populations.14
We defined mortality secondary to comorbid cancer and CVD as natural deaths attributed to concomitant CVD (ICD-10th Revision codes I00-I78) and malignant neoplasms (ICD-10th Revision codes C00-C97). We selected patients whose mortality was attributed to cancer or CVD or concomitant cancer and CVD. It is important to note that while selecting multiple causes of death, either 1 or both causes may have been contributory factors listed on the death certificate and not necessarily the underlying cause of death. Additionally, these cohorts are not mutually exclusive, and some degree of overlap is expected because of inherent limitations of the database.
We abstracted the number of cause-specific deaths and county population sizes by age, sex, race/ethnicity, and urban-rural classification. Race was categorized as American Indian or Alaskan Native, Asian/Pacific Islander, Black or African American, and White. Ethnicity was categorized as Hispanic and non-Hispanic. We used the National Center for Health Statistics 2013 Urban-Rural Classification Scheme and collapsed the county-level population into urban (large metropolitan [≥1 million], medium or small metropolitan [50,000-999,999]) and rural (micropolitan and noncore [nonmetropolitan counties that did not qualify as micropolitan; <50,000]) counties. Additional details are reported in the Supplemental Appendix.
Social vulnerability index
We used the 2018 SVI dataset from CDC’s Agency for Toxic Substances and Disease Registry, which outlines every U.S. county and census tract’s relative vulnerability for which the census collects statistical data. The SVI ranks these tracts and counties on 15 social factors using American Community Survey data from 2014 to 2018 and groups them into 4 themes: 1) socioeconomic status (below poverty, unemployed, income level, and no high school diploma); 2) household composition and disability (aged 65 years or older, aged 17 years or younger, individuals >5 years with a disability, and single-parent households); 3) minority status and language (minority and individual speaks English “less than well”); and 4) housing type and transportation (multiunit structure, mobile home, crowding, group quarters, and no vehicle) (Supplemental Figure 1, Supplemental Table 1).
A percentile rank, ranging from 0.00 to 1.00, was generated for each county, with higher values exhibiting greater vulnerability. Additional details on the process of percentile ranking are reported in the Supplemental Appendix. County-level representation for all 4 themes is shown in Supplemental Figures 2 to 5. For this analysis, we used overall SVI, aggregated across all 4 themes (Figure 1A).
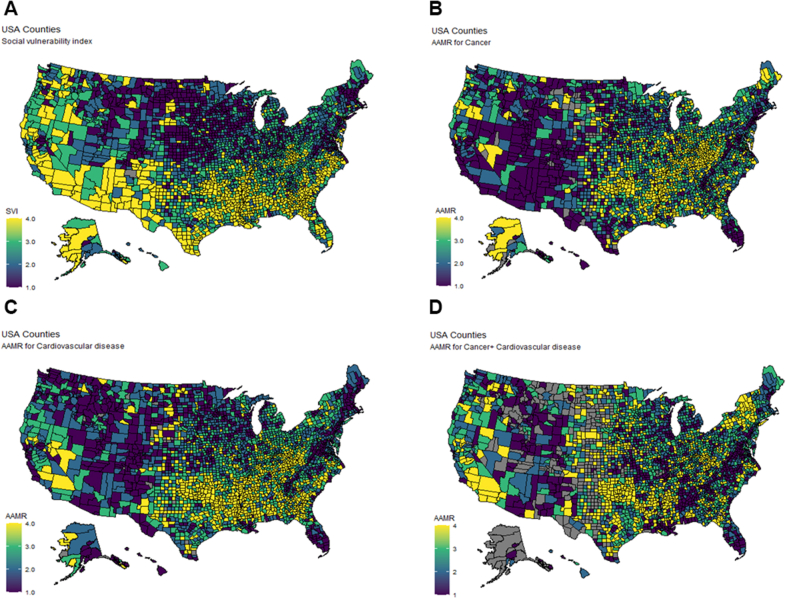
Figure 1.
Choropleth Maps of Age-Adjusted Mortality Rates (AAMRs)
These maps depict U.S. county-level age-adjusted mortality rates (AAMRs) on the basis of social vulnerability index (SVI) quartiles (A), cancer (B), cardiovascular disease (C), and comorbid cancer and CVD (D).
To understand the impact of SVI on age-adjusted mortality rate (AAMR) while adjusting for other known risk factors of adverse outcomes, we performed multivariable linear regression analysis by using county health factor data (Supplemental Appendix).
Institutional Review Board approval was not required, as the analysis used government-issued public-use data with deidentified information.
Statistical analysis
We estimated county-level AAMRs per 100,000 person-years with 95% CIs for cancer, CVD, and comorbid cancer and CVD for the overall population and stratified by demographic variables (age, sex, race, and ethnicity) and urbanization. We applied direct age adjustments to crude mortality rates using the 2000 U.S. population.
Continuous variables (eg, county attributes used in the SVI) are reported as median (IQR). We classified the percentile rankings for SVI into quartiles (first: most favorable = 0.00-0.25; fourth: least favorable = 0.75-1.00). We then aggregated counties across SVI quartiles to compare AAMRs among quartiles. To obtain aggregated data, we included all counties regardless of population size and death counts. However, rates were suppressed for data representing <10 deaths. Corresponding denominator population figures were also suppressed when the population represented <10 people. Rates were classified as unreliable for death counts <20 and were also not reported in this analysis.
We estimated rate ratios (RR) by comparing county-specific AAMRs between the fourth and first SVI quartiles for the overall population and stratified by demographic and urban-rural variables. Univariable Poisson regression was used for calculation of RRs and corresponding 95% CIs. Cause-specific RRs between CVD vs cancer plus CVD and cancer vs cancer plus CVD were compared, and P values <0.05 were considered to indicate statistical significance. We calculated rate difference as excess or fewer deaths per 100,000 person-years between the fourth and first SVI quartiles. Additionally, within the fourth quartile, sensitivity analyses were performed by comparing RR for mortality related to comorbid cancer and CVD among different racial/ethnic groups. We used the R version 4.0.3 (R Project for Statistical Computing) and Tableau version 2020.4 for all analyses.
Results
Cancer-related mortality
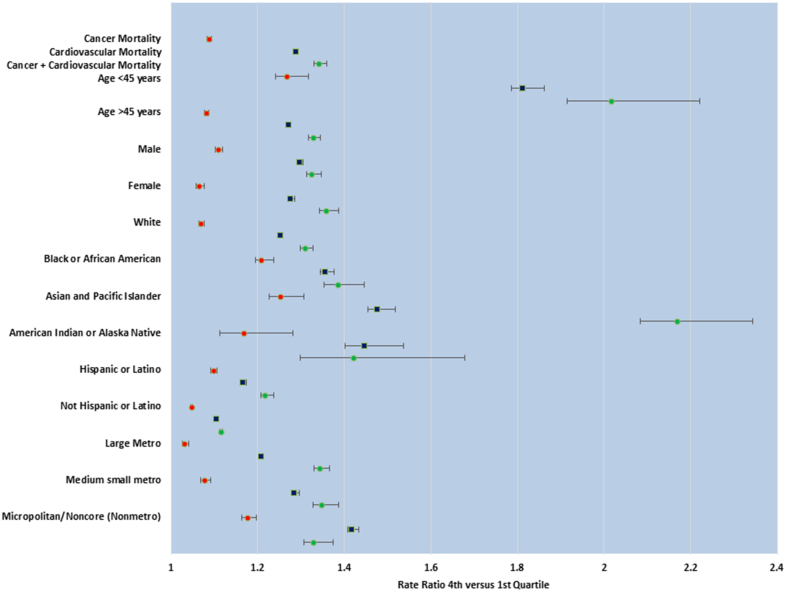
Between 2015 and 2019, the AAMR for cancer was 167.80 (95% CI: 167.62-167.99) per 100,000 person-years. The AAMRs for cancer were highest in the fourth quartile (174.09 [95% CI: 173.70-174.49] per 100,000 person-years) and lowest in the first quartile (160.11 [95% CI: 159.69-160.52] per 100,000 person-years), accounting for 13.98 excess deaths per 100,000 person-years in the fourth vs first quartiles (RR: 1.087; 95% CI: 1.084-1.091) (Table 1). Figure 1B illustrates the distribution of AAMRs for cancer across U.S. counties. The AAMRs increased across age, sex, race/ethnicity, and urbanization from the lowest to highest SVI quartiles (Table 1). Overall, AAMRs for cancer mortality were highest in adults >45 years of age, men, Black individuals, and rural areas (Table 1). Adults <45 years of age, men, Black individuals, Asian and Pacific Islanders, American Indian or Alaska natives, and rural counties had the highest relative increase in cancer mortality between the fourth vs first SVI quartiles (Figure 2).
Table 1.
Age-Adjusted Mortality Rates for Cancer Stratified by Social Vulnerability Index Quartiles
| Total | First Quartile | Second Quartile | Third Quartile | Fourth Quartile | Rate Ratio, Fourth/First Quartile | |
|---|---|---|---|---|---|---|
| Cancer mortality | 167.80 (167.62-167.99) | 160.11 (159.69-160.52) | 164.70 (164.35-165.05) | 170.59 (170.27-170.92) | 174.09 (173.70-174.49) | 1.09 (1.08-1.09) |
| Age | ||||||
| <45 y | 10.11 (10.05-10.18) | 8.92 (8.78-9.07) | 9.34 (9.22-9.46) | 10.49 (10.37-10.61) | 11.30 (11.16-11.45) | 1.27 (1.24-1.29) |
| >45 y | 462.63 (462.12-463.15) | 442.77 (441.61-443.94) | 455.18 (454.21-456.16) | 469.93 (469.02-470.84) | 478.46 (477.35-479.58) | 1.08 (1.08-1.08) |
| Sex | ||||||
| Male | 202.25 (201.94-202.55) | 191.74 (191.05-192.43) | 197.74 (197.16-198.32) | 205.40 (204.86-205.94) | 212.61 (211.94-213.28) | 1.11 (1.10-1.11) |
| Female | 142.49 (142.26-142.72) | 137.14 (136.61-137.66) | 140.43 (140.00-140.87) | 144.91 (144.51-145.32) | 145.99 (145.49-146.48) | 1.06 (1.06-1.07) |
| Race | ||||||
| White | 169.16 (168.96-169.36) | 162.71 (162.27-163.15) | 168.03 (167.65-168.41) | 171.47 (171.11-171.83) | 174.02 (173.56-174.48) | 1.07 (1.07-1.07) |
| Black or African American | 189.70 (189.08-190.31) | 164.00 (161.85-166.16) | 184.78 (183.28-186.27) | 189.53 (188.55-190.51) | 198.22 (197.18-199.27) | 1.21 (1.19-1.22) |
| Asian and Pacific Islander | 102.23 (101.58-102.87) | 85.75 (84.02-87.48) | 105.62 (104.55-106.68) | 100.73 (99.50-101.97) | 107.52 (106.13-108.90) | 1.25 (1.23-1.28) |
| American Indian or Alaska Native | 111.41 (109.74-113.07) | 99.08 (93.68-104.49) | 120.38 (116.50-124.26) | 101.69 (98.73-104.66) | 115.76 (113.13-118.38) | 1.17 (1.11-1.23) |
| Ethnicity | ||||||
| Hispanic or Latinx | 117.89 (117.38-118.40) | 95.55 (93.69-97.41) | 111.47 (110.17-112.77) | 113.26 (112.34-114.17) | 126.34 (125.57-127.10) | 1.10 (1.09-1.10) |
| Not Hispanic or Latinx | 172.59 (172.40-172.79) | 162.02 (161.59-162.45) | 167.43 (167.06-167.79) | 176.02 (175.67-176.37) | 186.09 (185.62-186.56) | 1.05 (1.05-1.05) |
| Urbanization | ||||||
| Large metropolitan | 159.93 (159.68-160.18) | 157.05 (156.53-157.58) | 158.34 (157.84-158.85) | 162.09 (161.66-162.52) | 161.79 (161.23-162.35) | 1.03 (1.03-1.04) |
| Medium small metropolitan | 171.20 (170.87-171.54) | 162.98 (162.06-163.91) | 166.23 (165.66-166.80) | 176.61 (176.02-177.21) | 175.41 (174.69-176.14) | 1.08 (1.07-1.08) |
| Micropolitan/noncore (nonmetropolitan) | 187.56 (187.08-188.04) | 169.23 (168.16-170.29) | 182.71 (181.75-183.68) | 191.20 (190.27-192.12) | 198.93 (198.02-199.83) | 1.18 (1.16-1.19) |
Age-adjusted mortality rates are presented per 100,000 adults with 95% CIs.
Figure 2.
Comparison of Age-Adjusted Mortality Rates (Fourth vs First SVI Quartiles)
This figure shows rate ratios for age-adjusted mortality between the fourth (most vulnerable) and first (least vulnerable) quartiles of the 2018 county-level social vulnerability index (SVI) for cancer (red squares), cardiovascular disease (blue squares), and comorbid cancer and cardiovascular disease (green squares), stratified by demographic and urbanization characteristics. Higher rate ratio values depict a greater impact of SVI.
CVD-related mortality
Between 2015 and 2019, the AAMR for CVD was 386.01 (95% CI: 385.73-386.29) per 100,000 person-years (Table 2). Figure 1C illustrates the distribution of AAMRs for CVD across U.S. counties. The AAMRs for CVD were lowest in the first quartile (344.25 [95% CI: 343.63-344.86] per 100,000 person-years) and highest in the fourth quartile (443.13 [95% CI: 442.49-443.77] per 100,000 person-years), accounting for 98.88 excess deaths per 100,000 person-years in the fourth vs first SVI quartiles (RR: 1.287; 95% CI: 1.284-1.290) (Table 2). Overall, AAMRs for CVD mortality were highest in adults >45 years of age, men, Black individuals, and rural areas (Table 2). AAMR increased from the first to fourth SVI quartile across all categories, including age, sex, race/ethnicity, and urbanization (Table 2). The impact of social vulnerability on CVD mortality, as measured by the RR between the fourth and first SVI quartiles, was greatest in adults <45 years of age, men, Asian and Pacific Islanders, American Indian or Alaska natives, Hispanics, and rural counties relative to their counterparts (Figure 2).
Table 2.
Age-Adjusted Mortality Rates for Cardiovascular Disease Stratified by Social Vulnerability Index Quartiles
| Total | First Quartile | Second Quartile | Third Quartile | Fourth Quartile | Rate Ratio, Fourth/First Quartile | |
|---|---|---|---|---|---|---|
| Cardiovascular mortality | 386.01 (385.73-386.29) | 344.25 (343.63-344.86) | 363.38 (362.86-363.89) | 390.37 (389.88-390.87) | 443.13 (442.49-443.77) | 1.29 (1.28-1.29) |
| Age | ||||||
| <45 y | 23.45 (23.35-23.55) | 16.59 (16.39-16.79) | 20.23 (20.05-20.41) | 25.09 (24.91-25.28) | 30.06 (29.82-30.30) | 1.81 (1.79-1.84) |
| >45 y | 1,063.90 (1,063.12-1,064.67) | 956.86 (955.15-958.58) | 1,004.96 (1,003.51-1,006.41) | 1,073.33 (1,071.96-1,074.71) | 1,215.46 (1,213.67-1,217.24) | 1.27 (1.27-1.27) |
| Sex | ||||||
| Male | 462.34 (461.87-462.81) | 410.56 (409.53-411.60) | 434.80 (433.93-435.68) | 468.75 (467.92-469.58) | 532.58 (531.50-533.66) | 1.30 (1.29-1.30) |
| Female | 323.68 (323.34-324.02) | 290.50 (289.76-291.23) | 304.80 (304.18-305.43) | 326.25 (325.66-326.85) | 370.53 (369.75-371.30) | 1.28 (1.27-1.28) |
| Race | ||||||
| White | 382.14 (381.84-382.44) | 347.22 (346.58-347.86) | 367.11 (366.55-367.67) | 385.23 (384.70-385.77) | 434.58 (433.86-435.30) | 1.25 (1.25-1.26) |
| Black or African American | 482.58 (481.58-483.58) | 394.48 (391.04-397.93) | 445.80 (443.42-448.18) | 469.65 (468.07-471.22) | 534.65 (532.91-536.39) | 1.36 (1.34-1.37) |
| Asian and Pacific Islander | 224.72 (223.74-225.70) | 174.16 (171.53-176.80) | 222.56 (221.00-224.12) | 222.46 (220.55-224.36) | 256.92 (254.75-259.08) | 1.48 (1.45-1.50) |
| American Indian or Alaska Native | 299.17 (296.36-301.97) | 235.21 (226.60-243.82) | 299.46 (293.14-305.78) | 255.36 (250.55-260.17) | 340.23 (335.62-344.83) | 1.45 (1.40-1.49) |
| Ethnicity | ||||||
| Hispanic or Latinx | 295.20 (294.37-296.04) | 214.23 (211.33-217.12) | 254.27 (252.24-256.29) | 263.41 (261.97-264.84) | 339.69 (338.40-340.97) | 1.17 (1.16-1.17) |
| Not Hispanic or Latinx | 394.44 (394.14-394.74) | 347.54 (346.92-348.17) | 368.48 (367.94-369.02) | 402.09 (401.57-402.62) | 469.90 (469.16-470.64) | 1.11 (1.10-1.11) |
| Urbanization | ||||||
| Large metropolitan | 362.51 (362.14-362.89) | 338.68 (337.91-339.45) | 347.45 (346.70-348.19) | 362.54 (361.89-363.18) | 409.12 (408.23-410.02) | 1.21 (1.20-1.21) |
| Medium small metropolitan | 395.39 (394.88-395.89) | 347.73 (346.38-349.08) | 365.62 (364.78-366.46) | 410.07 (409.16-410.98) | 446.54 (445.38-447.71) | 1.28 (1.28-1.29) |
| Micropolitan/noncore (nonmetropolitan) | 446.58 (445.84-447.33) | 362.77 (361.23-364.31) | 411.48 (410.04-412.92) | 458.03 (456.59-459.48) | 514.10 (512.62-515.58) | 1.42 (1.41-1.43) |
Age-adjusted mortality rates are presented per 100,000 adults with 95% CIs.
Mortality related to comorbid cancer and CVD
Between 2015 and 2019, there were a total of 936,947 deaths (∼187,389 deaths/year; 3,006 counties) due to comorbid cancer and CVD, corresponding to an AAMR of 47.75 (95% CI: 47.66-47.85) per 100,000 person-years (Table 3). Figure 1D illustrates AAMRs for comorbid cancer and CVD across U.S. counties. Overall AAMRs were lowest in the first SVI quartile (43.47 [95% CI: 43.25-43.69] per 100,000 person-years) and highest in the fourth SVI quartile (58.25 [95% CI: 58.02-58.48] per 100,000 person-years) (Table 3). This was associated with 10.5 excess deaths per 100,000 person-years in the fourth vs first SVI quartile (RR: 1.34; 95% CI: 1.33-1.35) (Table 3).
Table 3.
Age-Adjusted Mortality Rates for Comorbid Cancer and Cardiovascular Disease Stratified by Social Vulnerability Index Quartiles
| Total | First Quartile | Second Quartile | Third Quartile | Fourth Quartile | Rate Ratio, Fourth/First Quartile | |
|---|---|---|---|---|---|---|
| Comorbid cancer and CVD mortality | 47.75 (47.66-47.85) | 43.47 (43.25-43.69) | 44.89 (44.71-45.07) | 45.55 (45.38-45.71) | 58.25 (58.02-58.48) | 1.34 (1.33-1.35) |
| Age | ||||||
| <45 y | 1.70 (1.67-1.72) | 1.24 (1.19-1.30) | 1.37 (1.32-1.42) | 1.60 (1.56-1.65) | 2.50 (2.43-2.57) | 2.02 (1.92-2.12) |
| >45 y | 133.87 (133.59-134.15) | 122.41 (121.80-123.03) | 126.26 (125.74-126.78) | 127.71 (127.24-128.18) | 162.48 (161.83-163.13) | 1.33 (1.32-1.34) |
| Sex | ||||||
| Male | 62.26 (62.09-62.44) | 56.99 (56.61-57.37) | 58.63 (58.31-58.95) | 59.59 (59.30-59.89) | 75.48 (75.08-75.89) | 1.32 (1.31-1.34) |
| Female | 37.22 (37.10-37.33) | 33.72 (33.46-33.97) | 34.88 (34.66-35.09) | 35.30 (35.10-35.50) | 45.82 (45.55-46.10) | 1.36 (1.34-1.37) |
| Race | ||||||
| White | 47.56 (47.46-47.67) | 44.08 (43.86-44.31) | 45.60 (45.40-45.80) | 45.24 (45.05-45.42) | 57.72 (57.46-57.98) | 1.31 (1.30-1.32) |
| Black or African American | 57.10 (56.76-57.45) | 47.63 (46.44-48.82) | 51.78 (50.97-52.59) | 53.22 (52.69-53.75) | 65.94 (65.34-66.55) | 1.38 (1.35-1.42) |
| Asian and Pacific Islander | 30.80 (30.44-31.16) | 20.16 (19.29-21.02) | 28.71 (28.15-29.27) | 27.52 (26.86-28.18) | 43.73 (42.84-44.62) | 2.17 (2.08-2.26) |
| American Indian or Alaska Native | 34.02 (33.08-34.97) | 27.21 (24.24-30.18) | 34.86 (32.70-37.01) | 28.88 (27.25-30.50) | 38.66 (37.11-40.20) | 1.42 (1.30-1.56) |
| Ethnicity | ||||||
| Hispanic or Latinx | 37.62 (37.33-37.92) | 25.82 (24.82-26.81) | 32.54 (31.82-33.26) | 28.89 (28.42-29.36) | 46.65 (46.18-47.12) | 1.22 (1.21-1.23) |
| Not Hispanic or Latinx | 48.56 (48.45-48.66) | 43.92 (43.70-44.14) | 45.41 (45.22-45.59) | 46.99 (46.81-47.17) | 60.86 (60.59-61.12) | 1.11 (1.11-1.12) |
| Urbanization | ||||||
| Large metropolitan | 45.96 (45.83-46.09) | 43.45 (43.18-43.73) | 43.24 (42.98-43.50) | 42.48 (42.26-42.70) | 58.36 (58.02-58.70) | 1.34 (1.33-1.36) |
| Medium small metropolitan | 47.53 (47.36-47.71) | 41.68 (41.21-42.14) | 44.65 (44.36-44.94) | 47.00 (46.70-47.31) | 56.16 (55.75-56.57) | 1.35 (1.33-1.37) |
| Micropolitan/noncore (nonmetropolitan) | 53.91 (53.65-54.16) | 45.84 (45.30-46.39) | 50.80 (50.30-51.31) | 54.22 (53.74-54.71) | 60.94 (60.44-61.43) | 1.33 (1.31-1.35) |
Age-adjusted mortality rates are presented per 100,000 adults with 95% CIs.
Overall, AAMRs were higher for adults >45 years of age, men, Black individuals, and rural counties compared with their counterparts. AAMR increased from the first to fourth SVI quartile across all categories, including age, sex, race/ethnicity, and urbanization (Table 3). The impact of social vulnerability on comorbid cancer and CVD mortality, as measured by the RR between the fourth and first SVI quartiles, was greatest in adults <45 years of age, women, Asian and Pacific Islanders, and Hispanics relative to their counterparts (Figure 2).
Mortality related to comorbid cancer and CVD compared with mortality from cancer or CVD alone
Between 2015 and 2019, although overall mortality rates for cancer and CVD were high, and exceeded the rate for comorbid cancer and CVD, the impact of social vulnerability, measured by the RR between the fourth and first SVI quartiles, was highest for mortality related to comorbid cancer and CVD compared with mortality related to cancer (1.340 [95% CI: 1.330-1.349] vs 1.087 [95% CI: 1.084-1.091]; P < 0.001) or CVD (1.287; 95% CI: 1.284-1.289; P < 0.001) alone (Table 4, Figure 2).
Table 4.
Comparison of Rate Ratios Between the Fourth and First SVI Quartiles
| Rate Ratio Between the Fourth and First SVI Quartiles |
||||
|---|---|---|---|---|
| CVD vs Cancer Plus CVD | P Value | Cancer vs Cancer Plus CVD | P Value | |
| Overall | 1.29 vs 1.34 | <0.001 | 1.09 vs 1.34 | <0.001 |
| Age | ||||
| <45 y | 1.81 vs 2.02 | <0.001 | 1.27 vs 2.02 | <0.001 |
| >45 y | 1.27 vs 1.33 | <0.001 | 1.08 vs 1.33 | <0.001 |
| Sex | ||||
| Male | 1.30 vs 1.32 | <0.001 | 1.11 vs 1.32 | <0.001 |
| Female | 1.28 vs 1.36 | <0.001 | 1.06 vs 1.36 | <0.001 |
| Race | ||||
| White | 1.25 vs 1.31 | <0.001 | 1.07 vs 1.31 | <0.001 |
| Black or African American | 1.36 vs 1.38 | 0.08 | 1.21 vs 1.38 | <0.001 |
| Asian and Pacific Islander | 1.48 vs 2.17 | <0.001 | 1.25 vs 2.17 | <0.001 |
| American Indian or Alaska Native | 1.45 vs 1.42 | 0.70 | 1.17 vs 1.42 | <0.001 |
| Ethnicity | ||||
| Hispanic or Latinx | 1.17 vs 1.22 | <0.001 | 1.10 vs 1.22 | <0.001 |
| Not Hispanic or Latinx | 1.11 vs 1.11 | <0.001 | 1.05 vs 1.11 | <0.001 |
| Urbanization | ||||
| Large metropolitan | 1.21 vs 1.34 | <0.001 | 1.02 vs 1.34 | <0.001 |
| Medium small metropolitan | 1.28 vs 1.35 | <0.001 | 1.08 vs 1.35 | <0.001 |
| Micropolitan/noncore | 1.42 vs 1.33 | <0.001 | 1.18 vs 1.33 | <0.001 |
CVD = cardiovascular disease; SVI = social vulnerability index.
Sensitivity analyses: role of race
We performed a sensitivity analysis to assess whether mortality was affected by race within the most socially vulnerable counties. Using White individuals as control subjects, we analyzed the RR for AAMR for comorbid cancer and CVD mortality among different racial groups within the fourth SVI quartile. Only Black individuals had a significantly higher RR for mortality related to cancer (1.139; 95% CI: 1.132-1.146), CVD (1.230; 95% CI: 1.225-1.234), and comorbid cancer and CVD (1.142; 95% CI: 1.131-1.154).
Discussion
Our large population-based study of U.S. adults demonstrates, for the first time, the graded increase in county-level mortality secondary to comorbid cancer and CVD with greater social vulnerability. The incremental impact of social vulnerability was higher for mortality related to comorbid cancer and CVD than for mortality related to either cancer or CVD alone. Additionally, we found that adults <45 years of age, women, Asian and Pacific Islanders, and Hispanics had a higher relative increase in mortality related to comorbid cancer and CVD when comparing populations with the least (first SVI quartile) and most (fourth SVI quartile) social vulnerability (Central Illustration). Last, among those with the greatest social vulnerability (ie, within the fourth SVI quartile), Black individuals had significantly higher AAMRs secondary to cancer, CVD, and comorbid cancer and CVD compared with White individuals. These findings emphasize the impact of social vulnerability and race/ethnicity on mortality related to comorbid cancer and CVD and highlight populations that would benefit from targeted public health and policy interventions.
Central Illustration.
Impact of Social Vulnerability on Cancer and Cardiovascular Disease Mortality
This figure illustrates the methodology, key findings, and potential interventions.
CDC = Centers for Disease Control and Prevention; CVD = Cardiovascular Disease; SDOH = Social Determinants of Health; SVI = Social Vulnerability Index; WONDER = Wide-Ranging Online Data for Epidemiologic Research.
To our knowledge, no prior studies have assessed the association between mortality related to comorbid cancer and CVD and SDOH. Previous studies have shown strong associations between SDOH and CVD outcomes, including stroke,15 myocardial infarction,16 and heart failure.17 A similar relationship between SDOH and cancer-related mortality has been demonstrated in patients with breast cancer,18 resected lung and colon cancers,19 and head and neck cancers.20 Our results build on these prior studies and similarly show higher CVD and cancer-related mortality in more socially vulnerable counties. A recent study by Youmans et al21 demonstrated a significant association between SVI and CVD mortality; however, the investigators did not assess changes in CVD mortality across gradients of social vulnerability. Our study uniquely examines and demonstrates an association between nationwide cancer, CVD, and comorbid cancer and CVD mortality and county-level graded social vulnerability, stratified by demographic and urbanization characteristics.
We determined that mortality related to comorbid cancer and CVD was significantly more affected by social vulnerability gradients than mortality related to either cancer or CVD alone. Patients with cancer are already burdened by treatment, side effects of therapies, and health care visits. Concomitant CVD requires additional visits and medications. An area that needs further exploration is whether patients from the most socially vulnerable areas have difficulty establishing and maintaining the adherence to medications and follow-up required for comorbid cancer and CVD.
We examined the unadjusted associations between cancer, CVD, and comorbid cancer and CVD mortality and individual demographic characteristics that were most affected by social vulnerability. Overall cancer, CVD, and comorbid cancer and CVD mortality was higher in individuals >45 years of age. However, the impact of increasing levels of social vulnerability on mortality from any of these causes was more pronounced in those <45 years of age. An increase in the prevalence of traditional CVD risk factors in younger adults over the past 2 decades,5,22 rising unemployment and poverty, lack of affordable health insurance and limited access to health care, higher prevalence of risky behaviors (tobacco, alcohol, and drug use), and nonadherence23 may in part explain the heightened differences in observed mortality among younger individuals living in the least and most vulnerable counties. Additionally, premature coronary artery disease and early cancer (age ≤45 years) may lead to loss of lifetime productivity, increase lifetime health care use and portend a poor prognosis.24,25
In our analysis, overall cancer, CVD, and comorbid cancer and CVD mortality was higher in men than in women. However, women were more susceptible to social vulnerability gradients with regard to mortality related to comorbid cancer and CVD. A recent analysis by Khan et al26 showed a rise in mortality related to CVD and cancer in young and middle-aged women in the United States. In addition to a higher incidence of traditional risk factors (hypertension, diabetes, and stroke), as seen in the ARIC (Atherosclerosis Risk in Communities) study,27 women are unequally affected by psychosocial factors such as stress, social isolation, and depression that may intensify the relationship between sex and mortality.28,29
Although a graded increase in AAMR from the first to fourth SVI quartiles was noted for both cancer and CVD mortality, no significant difference in AAMR was noted on the basis of urbanization for comorbid cancer and CVD. This is likely due to the smaller sample size of patients with comorbid cancer and CVD compared with cancer or CVD alone. Additionally, it is noted that race/ethnicity plays a larger role in determining outcomes for the most vulnerable (in the fourth SVI quartile) population, emphasizing that geographic proximity to high-quality subspecialized care (in urban areas) may not be enough, and other SDOH may play a crucial role in access to health care.
Racial/ethnic groups, including Black individuals, Hispanics, and American Indians, have had poor CVD outcomes for decades.30, 31, 32, 33 Structural racism, social stigma, barriers to access to care, poverty, poor neighborhood conditions, lack of insurance, and food insecurity34 are all impediments to healthy living and reasons for increased CVD mortality. Furthermore, screening for breast, cervical, and colorectal cancers is lower among Hispanics, Asians, and American Indians and Alaska natives relative to White and Black individuals, making them vulnerable to poor cancer-related outcomes.35
In our analysis, Black individuals had the highest rates of mortality related to CVD, cancer, and comorbid cancer and CVD. This was observed within the most socially vulnerable counties. A prior retrospective analysis examined the effect of race and socioeconomic status (income, educational attainment, and insurance status) on the risk for cancer therapy–induced cardiotoxicity in women with early-stage, HER-2+ breast cancer.36 In this retrospective study, socioeconomic status was consistently lower among Black women compared with White and other women. However, although Black women had a 2-fold higher risk for cardiotoxicity, the assessed socioeconomic factors were not associated with cardiotoxicity and did not affect the magnitude of the association between race and cardiotoxicity.36 These results highlight the importance of examining and addressing additional factors that may enhance the impact of systemic racism and social inequities leading to racial disparities in mortality related to comorbid cancer and CVD.
The findings of our study emphasize the adverse outcomes associated with comorbid cancer and CVD, particularly among the most vulnerable. Although our study is based on data from the pre-COVID-19 era (2015-2019), the COVID-19 pandemic has further exposed health care disparities and associated adverse outcomes. Patients with comorbid cancer and CVD had worse outcomes of COVID-19, including more severe disease and higher mortality, compared with those with cancer or CVD alone.37
This study highlights the negative outcomes faced by vulnerable populations with cancer and CVD, particularly those who with both diseases. To improve health care outcomes in these patients, we need investment in health care infrastructure in socially vulnerable areas. We need to educate health care providers about the impact of SDOH on outcomes and integrate these considerations into health care delivery systems to effectively intervene on the highest risk and most socially vulnerable populations (Central Illustration). Preventive services for marginalized populations need to be prioritized. Policies also need to be recalibrated to extend the provision of health care outside the acute care setting to communities and at home. Finally, solutions need to be individualized for each community/group considering their unique social and cultural norms.
Study limitations
First, we used SVI to assess social vulnerability, rather than other indexes such as the Area Deprivation Index or Social Deprivation Index. The Area Deprivation Index focuses predominantly on economic deprivation, whereas the Social Deprivation Index covers limited social characteristics (poverty, <12 years of education, single-parent household, rented housing unit, the overcrowded housing unit, households without a car, and nonemployed adults <65 years of age), making the SVI a more comprehensive measure of social risk within communities. However, we acknowledge that although the SVI is a comprehensive measure, it is by no means inclusive of all social disadvantages. For example, it does not account for several critical factors such as food insecurity, community and social contextual factors, and health care access barriers such as proximity to quality health care centers, insurance status, and others.
Second, we conducted a cross-sectional analysis and therefore could not draw causal relationships between county-level characteristics and mortality. Third, we reported crude estimates of AAMR because data limitations did not permit examination of individual clinical risk factors or adjustment for them.
Fourth, death certificates are susceptible to potential miscoding regarding the cause of death, as they are based on ICD codes and not adjudicated mortality events. However, this is a systematic issue that should have affected all counties equally, thus balancing its effects.
Fifth, these are exclusively mortality data and do not have information regarding disease diagnosis and treatments. Sixth, although documentation of White and Black race has been identified as accurate on death certificates, classification as Hispanic, Asian, and Pacific Islander has been identified as a minor issue.38
Last, because the CDC SVI database provides aggregated and not individual-level data, it is not possible to perform adjusted analyses. However, to overcome this limitation, we conducted subgroup analyses stratified by various demographic and population-level variables. Additionally, we performed multivariable linear regression analysis by using county health factor data as a sensitivity analysis to understand the impact of SVI on AAMR while adjusting for other known risk factors of adverse outcomes.
Conclusions
This analysis demonstrates a graded increase in mortality related to cancer, CVD, and comorbid cancer and CVD in U.S. counties with worsening social vulnerability. The incremental impact of social vulnerability was greater for mortality related to comorbid cancer and CVD than for mortality related to cancer or CVD alone. Our findings demonstrate the fragility of the population with the dual diagnoses of cancer and CVD and the incremental adverse impact of SDOH on this highly vulnerable population. These findings emphasize the need for an improved strategy for education, resource allocation, and targeted public health interventions to address social inequities and improve cancer, CVD, and cardio-oncology outcomes in the United States.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: Social vulnerability affects comorbid cancer and CVD mortality more than cancer or CVD mortality alone. Adults <45 years of age, women, Asian and Pacific Islanders, and Hispanics had the highest relative increase in comorbid cancer and CVD mortality when comparing populations with the least (first SVI quartile) and most (fourth SVI quartile) social vulnerability. Among those with the greatest social vulnerability, Black individuals had significantly higher mortality secondary to cancer, CVD, and comorbid cancer and CVD compared with White individuals.
TRANSLATIONAL OUTLOOK: Improved education, resource allocation, and public health interventions are needed to address social inequities in cardio-oncology.
Funding Support and Author Disclosures
Dr Gupta is supported in part by National Institutes of Health/National Cancer Institute grant P30CA008748. Dr Nohria is supported by the Catherine Fitch Fund and the Gelb Master Clinician Fund at Brigham and Women’s Hospital. All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
Charlotte Manisty, PhD, served as the Guest Editor for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental methods, figures, and tables, please see the online version of this paper.
Appendix
References
- 1.Valero-Elizondo J., Chouairi F., Khera R., et al. Atherosclerotic cardiovascular disease, cancer, and financial toxicity among adults in the United States. J Am Coll Cardiol CardioOnc. 2021;3(2):236–246. doi: 10.1016/j.jaccao.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Havranek E.P., Mujahid M.S., Barr D.A., et al. Social determinants of risk and outcomes for cardiovascular disease. Circulation. 2015;132(9):873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 3.Social determinants of health (SDOH) NEJM Catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0312
- 4.Alcaraz K.I., Wiedt T.L., Daniels E.C., Yabroff K.R., Guerra C.E., Wender R.C. Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J Clin. 2020;70(1):31–46. doi: 10.3322/caac.21586. [DOI] [PubMed] [Google Scholar]
- 5.Andersson C., Vasan R.S. Epidemiology of cardiovascular disease in young individuals. Nat Rev Cardiol. 2018;15(4):230–240. doi: 10.1038/nrcardio.2017.154. [DOI] [PubMed] [Google Scholar]
- 6.Shah N.S., Molsberry R., Rana J.S., et al. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999-2018: observational analysis of vital statistics. BMJ. 2020;370:m2688. doi: 10.1136/bmj.m2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaughan A.S., Ritchey M.D., Hannan J., Kramer M.R., Casper M. Widespread recent increases in county-level heart disease mortality across age groups. Ann Epidemiol. 2017;27(12):796–800. doi: 10.1016/j.annepidem.2017.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y., Freedman N.D., Albert P.S., et al. Association of cardiovascular disease with premature mortality in the United States. JAMA Cardiol. 2019;4(12):1230. doi: 10.1001/jamacardio.2019.3891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yabroff K.R., Han X., Zhao J., Nogueira L., Jemal A. Rural cancer disparities in the United States: a multilevel framework to improve access to care and patient outcomes. JCO Oncol Pract. 2020;16(7):409–413. doi: 10.1200/OP.20.00352. [DOI] [PubMed] [Google Scholar]
- 10.Flanagan B.E., Gregory E.G., Hallisey E.J., Heitgerd J.L., Lewis B. A social vulnerability index for disaster management. J Homeland Security Emerg Manage. 2011;8(1):3. [Google Scholar]
- 11.Wallace L.M.K., Theou O., Pena F., Rockwood K., Andrew M.K. Social vulnerability as a predictor of mortality and disability: cross-country differences in the survey of health, aging, and retirement in Europe (SHARE) Aging Clin Exper Res. 2015;27(3):365–372. doi: 10.1007/s40520-014-0271-6. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong J.J., Andrew M.K., Mitnitski A., Launer L.J., White L.R., Rockwood K. Social vulnerability and survival across levels of frailty in the Honolulu-Asia Aging Study. Age Ageing. 2015;44(4):709–712. doi: 10.1093/ageing/afv016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Friede A., Reid J.A., Ory H.W. CDC WONDER: a comprehensive on-line public health information system of the Centers for Disease Control and Prevention. Am J Public Health. 1993;83(9):1289–1294. doi: 10.2105/ajph.83.9.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention Underlying cause of death, 1999-2018. https://wonder.cdc.gov/ucd-icd10.html
- 15.Reshetnyak E., Ntamatungiro M., Pinheiro L.C., et al. Impact of multiple social determinants of health on incident stroke. Stroke. 2020;51(8):2445–2453. doi: 10.1161/STROKEAHA.120.028530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Safford Monika M., Reshetnyak E., Sterling Madeline R., et al. Number of social determinants of health and fatal and nonfatal incident coronary heart disease in the REGARDS study. Circulation. 2021;143(3):244–253. doi: 10.1161/CIRCULATIONAHA.120.048026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sterling M.R., Ringel J.B., Pinheiro L.C., et al. Social determinants of health and 90-day mortality after hospitalization for heart failure in the REGARDS study. J Am Heart Assoc. 2020;9(9) doi: 10.1161/JAHA.119.014836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kantor O., Wang M.L., Bertrand K., et al. Racial and socioeconomic disparities in breast cancer outcomes within the AJCC Pathologic Prognostic Staging System. Ann Surg Oncol. 2022;29(1):686–696. doi: 10.1245/s10434-021-10527-8. [DOI] [PubMed] [Google Scholar]
- 19.Diaz A., Dalmacy D., Hyer J.M., Tsilimigras D., Pawlik T.M. Intersection of social vulnerability and residential diversity: postoperative outcomes following resection of lung and colon cancer. J Surg Oncol. 2021;124(5):886–893. doi: 10.1002/jso.26588. [DOI] [PubMed] [Google Scholar]
- 20.Sharma R.K., Del Signore A., Govindaraj S., Iloreta A., Overdevest J.B., Gudis D.A. Impact of socioeconomic status on paranasal sinus cancer disease-specific and conditional survival. Otolaryngol Head Neck Surg. 2022;166(6):1070–1077. doi: 10.1177/01945998211028161. [DOI] [PubMed] [Google Scholar]
- 21.Youmans Q.R., McCabe M.E., Yancy C.W., et al. Abstract 16562: association of county-level social vulnerability index and cardiovascular disease in the United States, 1999-2018. Circulation. 2020;142(suppl_3) [Google Scholar]
- 22.Jain V., Rifai M.A., Brinzevich D., et al. Association of premature atherosclerotic cardiovascular disease with higher risk of cancer: a Behavioral Risk Factor Surveillance System study. Eur J Prev Cardiol. 2022;29(3):493–501. doi: 10.1093/eurjpc/zwab084. [DOI] [PubMed] [Google Scholar]
- 23.Kang H., Lobo J.M., Kim S., Sohn M.-W. Cost-related medication non-adherence among U.S. adults with diabetes. Diabetes Res Clin Pract. 2018;143:24–33. doi: 10.1016/j.diabres.2018.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Collet J.P., Zeitouni M., Procopi N., et al. Long-term evolution of premature coronary artery disease. J Am Coll Cardiol. 2019;74(15):1868–1878. doi: 10.1016/j.jacc.2019.08.1002. [DOI] [PubMed] [Google Scholar]
- 25.Song M., Hildesheim A., Shiels M.S. Premature years of life lost due to cancer in the United States in 2017. Cancer Epidemiol Biomarkers Prev. 2020;29(12):2591–2598. doi: 10.1158/1055-9965.EPI-20-0782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan S.U., Yedlapati S.H., Lone A.N., et al. A comparative analysis of premature heart disease- and cancer-related mortality in women in the USA, 1999-2018. Eur Heart J Qual Care Clin Outcomes. 2022;8(3):315–323. doi: 10.1093/ehjqcco/qcaa099. [DOI] [PubMed] [Google Scholar]
- 27.Arora S., Stouffer G.A., Kucharska-Newton A.M., et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139(8):1047–1056. doi: 10.1161/CIRCULATIONAHA.118.037137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hagström E., Norlund F., Stebbins A., et al. Psychosocial stress and major cardiovascular events in patients with stable coronary heart disease. J Intern Med. 2018;283(1):83–92. doi: 10.1111/joim.12692. [DOI] [PubMed] [Google Scholar]
- 29.Sumner J.A., Khodneva Y., Muntner P., et al. Effects of concurrent depressive symptoms and perceived stress on cardiovascular risk in low- and high-income participants: findings from the Reasons for Geographical and Racial Differences in Stroke (REGARDS) study. J Am Heart Assoc. 2016;5(10) doi: 10.1161/JAHA.116.003930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Graham G. Disparities in cardiovascular disease risk in the United States. Curr Cardiol Rev. 2015;11(3):238–245. doi: 10.2174/1573403X11666141122220003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Graham G. Racial and ethnic differences in acute coronary syndrome and myocardial infarction within the United States: from demographics to outcomes. Clin Cardiol. 2016;39(5):299–306. doi: 10.1002/clc.22524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carnethon M.R., Pu J., Howard G., et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393–e423. doi: 10.1161/CIR.0000000000000534. [DOI] [PubMed] [Google Scholar]
- 33.Glynn P., Lloyd-Jones D.M., Feinstein M.J., Carnethon M., Khan S.S. Disparities in cardiovascular mortality related to heart failure in the United States. J Am Coll Cardiol. 2019;73(18):2354–2355. doi: 10.1016/j.jacc.2019.02.042. [DOI] [PubMed] [Google Scholar]
- 34.Wang S.Y., Eberly L.A., Roberto C.A., Venkataramani A.S., Groeneveld P.W., Khatana S.A.M. Food insecurity and cardiovascular mortality for nonelderly adults in the United States from 2011 to 2017. Circ Cardiovasc Qual Outcomes. 2021;14(1) doi: 10.1161/CIRCOUTCOMES.120.007473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zavala V.A., Bracci P.M., Carethers J.M., et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. 2021;124(2):315–332. doi: 10.1038/s41416-020-01038-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al-Sadawi M., Hussain Y., Copeland-Halperin R.S., et al. Racial and socioeconomic disparities in cardiotoxicity among women with HER2-positive breast cancer. Am J Cardiol. 2021;147:116–121. doi: 10.1016/j.amjcard.2021.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ganatra S., Dani S.S., Redd R., et al. Outcomes of COVID-19 in patients with a history of cancer and comorbid cardiovascular disease. J Natl Compr Canc Netw. 2021;19(13):1–10. doi: 10.6004/jnccn.2020.7658. [DOI] [PubMed] [Google Scholar]
- 38.Arias E., Heron M., National Center for Health Statistics, Hakes J., U.S. Census Bureau The validity of race and Hispanic-origin reporting on death certificates in the United States: an update. Vital Health Stat. 2016;(172):1–21. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.