Abstract
Objectives
To evaluate the performance of four experimental multifocal gas permeable contact lens (MFGPCL) designs and their impact on visual function in young adults.
Methods
Seventeen young adults (age, 23.17 ± 4.48 years) enrolled in the study. Each participant was randomly assigned to wear two of four MFGPCL designs. They wore the first type of the assigned lens binocularly for one week and, after one week of washout period, wore another design on both eyes for another week. The four MFGPCL designs were as follows: design A (distance zone [DZ] 1.5 mm / add 3.0 D), B (DZ 1.5 mm / add 1.5 D), C (DZ 3.0 mm / add 3.0 D), and D (DZ 3.0 mm / add 1.5 D). Baseline visual acuity, contrast sensitivity function, and accommodation data were collected at baseline and repeated after one week of MFGPCL daily wear.
Results
Distance and near visual acuities were not significant affected with the four MFGPCL designs. Contrast sensitivity was significantly lower in design A across all measured spatial frequencies (p < 0.05), with no significant impact from other designs on all frequencies. No significant effect was observed on accommodation measured at 33 cm (p > 0.05).
Conclusions
Three of the investigated MFGPCL designs preserve satisfactory visual performance. Lens design A incorporated with higher add and smaller center zone diameter had a stronger impact on the visual performance.
Keywords: Multifocal, Gas-permeable contact lens, Visual performance, Myopia
Introduction
Myopia prevalence worldwide has become a public health concern, particularly due to its associated risks of developing serious ocular pathologies such as retinal detachment, cataract, and glaucoma.1
It is established from landmark animal studies and clinical studies that imposed hyperopic retinal defocus has been identified to promote ocular growth while myopic defocus, either imposed with a strong bias towards peripheral retina or superimposed with hyperopic defocus, may inhibit excessive ocular growth and control myopia. Consistent with findings from experimental myopia models, converging evidence from clinical studies have shown significant myopia inhibiting effect of optical treatments such as overnight orthokeratology or daytime multifocal contact lenses (MFCL), which shared common features of inducing myopic defocus to the retina while correcting central myopia.
Comparing to that achieved with spectacle corrections, the use of contact lenses is preferred because of their gaze-independent property hence providing a relatively constant peripheral myopic defocus.2 In recent years, the use of MFCLs for myopia management has increased dramatically both off-label or with official FDA approval.
Although MFSCL with a center distance (center D) design is more commonly used clinically for myopia control, lenses with center near (center N) design, which impose opposite defocus profiles and patterns of spherical aberrations relative to a center D design, have also been shown to be highly effective in slowing axial elongation in animal models.3,4 Additionally, although it tends to be positive dose-dependent relationships between the overall anti-myopia effect and both the magnitude of plus power incorporated into the lenses and allocated area, higher add power in MFCLs may lead to adaptation issues, reduced vision, and induced optical aberrations.5 As a result, it is critical and highly clinically relevant to study the ideal balance in MFCL designs in which the add power and the relative area distribution between the distance and near optics offer effective anti-myopia dosage without inducing a significant impact on visual performance.
Even though MFCL in soft materials are more commonly prescribed in children for myopia management,6,7 lenses made in gas permeable materials (MFGPCL) provide a viable alternative in certain myopes. First of all, MFGPCL offers great potential for customization comparing to MFSCL. Both the size of each optic zone and the magnitude of the plus power can be easily modified with great reproducibility and fast turnover. Additionally, the back surface toric design enables ideal fitting and minimizes large residual astigmatism in patients with significant corneal toricity, who are often excluded from MFSCL studies or clinical treatment. Finally, like MFSCL, MFGPCL provides full distance correction to a wide range of myopia, which can be challenging in overnight OrthoK treatment. Overall, the unique combination of its customizability and its application to a wide range of astigmatic and myopic refractive errors made MFGPCL an essential option in the whole myopia management toolbox. Despite all of its advantages, the popularity of MFGPCL is mostly limited by its initial discomfort and longer adaptation periods compared to soft lenses. More importantly, the lack of efficacy of standard single vision (SV) GP lenses as a myopia controlling option had left an impression among clinicians that GPCL was ineffective as an anti-myopia treatment. It is worth clarifying that the optical design of SVGPCL is drastically different than that of MFGPCL, in which no competing myopic defocus is incorporated in the optics of the lens and is believed to be the underlying reason of its apparent lack of anti-myopia efficacy.8,9 Nonetheless, recent studies demonstrated the efficacy of MFGPCL in generating a significant myopic shift in peripheral refraction, which was greater than the magnitude produced by MFSCLs.10,11 With its great potential as an anti-myopia option, a complete assessment of visual performance functions provided by MFGPCLs is critical to improve MFGPCLs’ tolerance and long-term compliance.
The present study, which was the first phase of a two-phase project, aimed to investigate the effect of several center-distance MFGPCL designs on visual performance and optical quality. Its short-term impact on the change of the choroidal thickness, a potential surrogate marker for the long-term axial inhibiting effect, will be reported elsewhere.
Methods
Subjects
The participants had a range of racial backgrounds, including Caucasian (n = 9), Asian (n = 4), and Hispanic (n = 4). The refractive error and ocular health of the participants were assessed by performing non-cycloplegic subjective refraction and slit-lamp examination. Only participants with best-corrected distance visual acuity of 0.0 logMAR were recruited. The maximum value of astigmatism was −1.75 D. All participants had no history of past ocular surgeries and were not using any systemic or topical medications known to contraindicate contact lens wear.
Study design
Study protocol
This prospective randomized incomplete balanced block design study tested the visual performance in young adults with four center-distance multifocal GP lenses; each lens design varies in the center zone diameter or the add powers. Only two lens designs were randomly assigned for each subject to minimize incomplete data and unnecessary drop-out. They wore each allocated lens for 7 days over four scheduled visits (baseline/dispense lens 1, one week lens 1, baseline/dispense lens 2, one week lens 2) with a one-week washout period between the two lens types. Baseline measurements were obtained at the beginning prior to dispensing the lenses. Pupil size and angle kappa were measured using Nidek OPD Scan III (Nidek Technologies, Gamagori, Japan). To allow for adaptation, the follow-up measurements were taken after one week of lens wear. Subjects were instructed to wear the lenses for at least 4 h per day and not to sleep with the lenses. During the one-week-long washout period between the two lens-wearing treatments, subjects wore their spectacles.
This study followed the tenets of the Declaration of Helsinki, and approval was obtained from the Institutional Review Board (IRB) of Pacific University before the commencement of the study. All participants gave their informed written consent prior to study participation after being informed about the nature and possible consequences of participating in the study. Subjects were screened before enrolment and found to be in good ocular health and free from ocular disease.
Multifocal gas-permeable lens (MFGPCL) designs and fitting
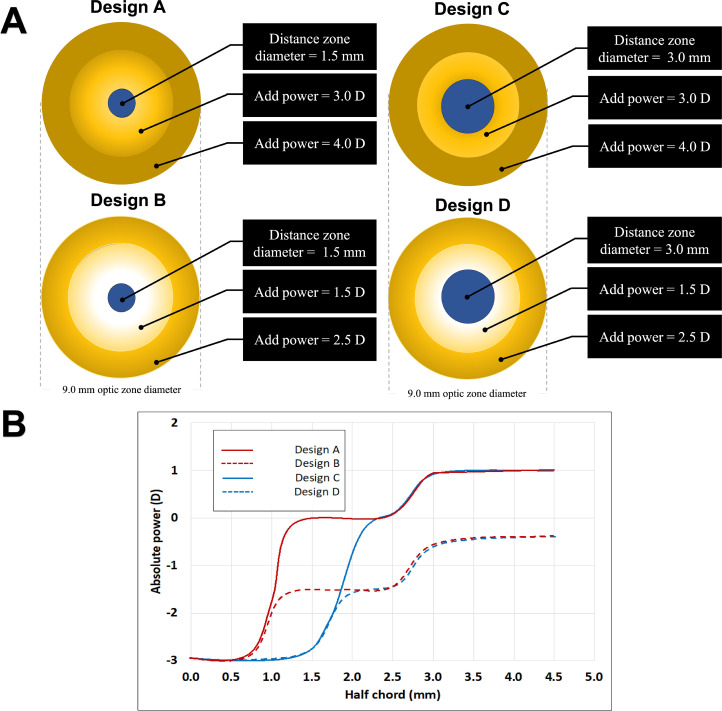
Four experimental center-distance MFGPCL designs (A, B, C, and D) were investigated in this study. All designs have a total optic zone diameter of 9 mm with a distance zone (DZ) that has the full distance correction. With these four optical designs, two add powers (+ 1.50 vs. + 3.00 D), and two center zone diameters (1.5 mm vs. 3.0 mm) were tested. Lens design A and B have an identical DZ diameter of 1.5 mm with the add power starting at the central geometric endpoint of DZ and provide +3.00 D (design A) or +1.50 D (design B) add plus power (5.0-mm chord diameter) to achieve approximately +4.00 D add (design A) and +2.50 D add (design B) at the edge of the optical zone (9-mm chord diameter). Lens designs C and D shared a 3.0 mm DZ diameter with the add power starting at the central geometric endpoint of DZ and providing +3.00 D (design C) or +1.50 D (design D) add plus power (5.0-mm chord diameter) to achieve approximately +4.00 D (design C) or +2.50 D (design D) at the edge of the optical zone (9-mm chord diameter). Fig. 1A and B show the schematic diagrams of the four designs and their power profiles. ConTest II (Rotlex, Omer, Israel) was used to confirm the contact lens power profile. All MFGPCLs were made of Boston XO (Hexafocon A) material with Dk of 100 (ISO/FATT cgs unit) and a refractive index of 1.415. The overall diameter of the MFGPCLs was 0.80 mm less than the participant's horizontal visible iris diameter. The fluorescein pattern and the topographic map of the lens anterior surface are presented in Fig. 2.
Figure 1.
Schematic diagram of optical zone geometries and power profile (B) of the MFGPCL designs used in the study.
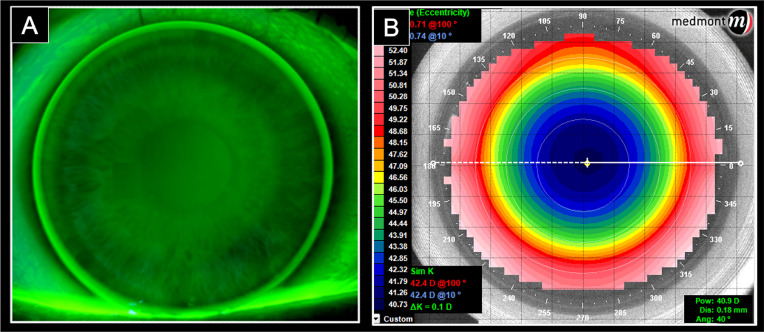
Figure 2.
An image illustrates the fluorescein pattern with an optimal fittinig of large diameter MFGPCL (A) and a topographic map of the MFGPCL anterior surface (B).
The MFGPCL was fitted based on the participant's subjective refraction, corneal curvature, and visible iris diameter. The corneal topography was obtained using a Medmont E300 corneal topographer (Medmont Pty, Ltd., Melbourne, Australia). Over-refraction was done at the trial visit and adjustments to the final prescription were made, and a new lens was ordered if discrepancies greater than ± 0.25 D were found. The lens fitting was evaluated for centration on lateral gaze movements using the slit-lamp biomicroscope. All lenses were fitted within the desired limits of less than 0.50 of decentration on blink.
Measurements and data collection procedures
Visual acuity (VA) and contrast sensitivity (CS)
Visual acuity and contrast sensitivity measurements were obtained after one week of lens wear and were compared with the subject's best spectacle correction. Distance visual acuity was measured monocularly using a ClearChart 2 (Reichert, Inc.) subtended 4.75° x 6.05° at 3.6 m. Snellen optotypes were presented for the subject to identify (display luminance was approximately 220 cd/m2). Near visual acuity was measured with Lighthouse Near Visual Acuity Card (2nd ed.; Lighthouse International) placed at 40 cm.
Contrast sensitivity test was performed monocularly using static sinusoidal gratings (stimulus size: 1.8° x 1.8°) at five spatial frequencies of 1.5, 3.0, 6.0, 12, and 18 cycles per degree using ClearChart 2. The stimuli were presented under photopic conditions (the display luminance was approximately 85 cd/m2) in three possible orientations: vertical and tilted 45 ° to the left or right. Each of the tested spatial frequencies had 14 different levels of contrast. The threshold value was determined using a descendent psychophysical procedure. The subjects were asked to identify the orientation of the sinusoidal gratings. The contrast level of the last correct response was defined as the contrast threshold. The results were recorded as contrast sensitivity levels and subsequently expressed as logarithmic values for each spatial frequency. The area under the logarithmic contrast sensitivity function (AULCSF) was calculated as an index of the overall contrast sensitivity.
Accommodative response
The monocular accommodative response was measured in the right eyes with the multifocal GP lens designs. The accommodation measurements were obtained while occluding the left eye and the subjects reading a high contrast text presented at 33 cm (3 D) subtended 8.6° x 1.7°. The size of the text used was adjusted to ensure the letters subtended at 7.5 min arc (20/30). Target luminance was 25 cd/m2. Refraction was measured using an open-field Grand Seiko WAM-5500 auto-refractor (Grand Seiko Co. Ltd., Hiroshima, Japan). Subjects were instructed to view the target and keep the text as clear as possible at all times. When the subject reported that the target was clear, 20 readings were taken with the auto-refractor. The accommodative response was taken as the recorded spherical equivalent with the sign reversed. It, therefore, included the combined effects of the eye and any lens worn. The accommodation measurements were compared to ones obtained with single vision soft contact lenses (SVSCL). All SVSCLs were comfilcon A Si-Hy material (Biofinity™, CooperVision, Rochester, NY) and contained the subject's distance correction. Participants with astigmatic refractive error < −0.75 D, Biofinity toric single vision soft contact lenses were used.
Subjective response
After seven days of lens wear, participants rated each lens design binocularly for comfort and vision using a questionnaire developed by Fedtke et al.12,13 The questionnaire contained seven questions evaluating distance, intermediate and near vision, as well as visual performance in dim illumination and overall comfort. The questionnaire used a numeric rating scale, ranging from 0 to 10 in 1-unit steps, where 0 indicates worst visual performance, and 10 indicates best performance.
Statistical analysis
Descriptive statistics were calculated for demographic and baseline data. A within-subject analysis of variance of score change was performed to assess changes in visual acuity, contrast sensitivity, and accommodative response by MFGPCL type. Post-hoc multiple comparisons with Bonferroni adjustment were used to compare differences between four MFGPCLs. A p-value of < 0.05 was considered to be statistically significant. All statistical analyses were conducted using SPSS version 26 (SPSS, Chicago, IL).
Results
Seventeen healthy young adults with a mean age of 23.17 ± 4.48 years and a spherical equivalent of −3.18 ± 2.59 D were recruited.
Effects on distance and near visual acuities (VAs)
The change in distance VA and near VA (logMAR) obtained with each MFGPCL design are presented in Table 1. All four experimental MFGPCLs showed no statistical significant difference on distance visual acuity (main effect: F (3, 44) = 1.5, p = 0.22). All MFGPCL designs did not impact near VA (main effect: F (3, 53) = 1.5, p = 0.21). Means of change ± standard errors are shown in Table 1.
Table 1.
Mean and SE of change in DVA, NVA, and AULCSF with the four MFGPCL designs.
|
DVA (logMAR) |
NVA (logMAR) |
AULCSF |
||||
|---|---|---|---|---|---|---|
| mean ± SE | p-value | mean ± SE | p-value | mean ± SE | p-value | |
| A (DZ1.5/add3.0) | 0.058±0.058 | 0.22 | 0.017±0.006 | 0.21 | −4.3 ± 0.67† | <0.001* |
| B (DZ1.5/add1.5) | 0.022±0.022 | 0.006±0.005 | −1.5 ± 0.58 | |||
| C (DZ3.0/add3.0) | 0.034±0.034 | 0.005±0.006 | −1.9 ± 0.64 | |||
| D (DZ3.0/add1.5) | 0.027±0.027 | 0.002±0.005 | −0.9 ± 0.58 | |||
* p < 0.05.
† statistically significant difference compared to other MFGPCL designs based on Post-hoc multiple comparisons with Bonferroni adjustment (p-value<0.05).
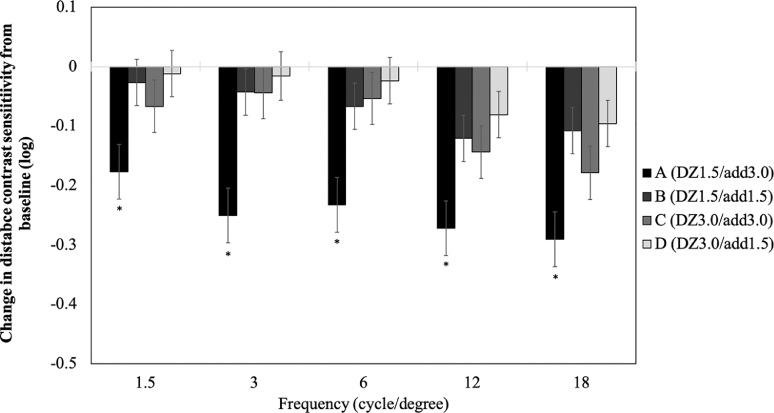
Effects on distance contrast sensitivity
In Table 1, which represented the change in area under the logarithmic contrast sensitivity function (AULCSF) with each MFGPCL design, it was noticeable that the mean change contrast sensitivity was significantly reduced (main effect of lens design: F (3,50) = 10.1, p < 0.001). The posthoc test showed that a significant reduction in AULCSF occurred only with lens design A, which had high add (+3.00 D) and a small center zone (1.50 mm) when compared to the other three tested designs. Change score analysis was also performed to investigate the impact of the lenses on five spatial frequencies. The change in each of the five spatial frequencies (Fig. 3) showed that the deterioration of distance contrast sensitivity in the case of lens A (main effect of lens design: F (3260) = 19.7, p < 0.001). It also showed that lens designs were independent of spatial frequency (lens design x frequency interaction: F(12,271) = 0.30, p = 0.99). The pupil size and angle kappa data were collected and included in the analysis. Our results showed pupil size and angle kappa tested not significant on visual acuity and distance contrast sensitivity (p = 0.36 and p = 0.12, respectively). Considering the highly clinical importance of those two variables, it is worth pursuing the potential association in a larger study.
Figure 3.
Mean ± SE of change in contrast sensitivity as a function of spatial frequency measured with four MFGPCL designs. Error bars represent standard errors, the asterisk (*) symbols indicate a statistically significant difference compared to other MFGPCL designs based on Post-hoc multiple comparisons with Bonferroni adjustment (p-value<0.05).
Effects on accommodation
The change in accommodative lag was recorded with the single vision soft contact lens (SVSCL) and the four MFGPCL designs at a 33 cm test distance. Subjects exhibited no significant change in accommodative lag between the four experimental MFGPCL designs (main effect: F (3,21.7) = 0.90, p = 0.46) (Table 2).
Table 2.
Mean and SD (standard deviation) of accommodative lag with SVCL and Mean and SE (standard error) of change in accommodative lag obtained with the four MFGP lens designs.
| Single vision Contact lens (mean ± SD) | 0.64 ± 0.23 D |
|---|---|
| Contact Lens Design | Mean ± SE |
| A (DZ1.5/add3.0) | 0.37 ± 0.19 D |
| B (DZ1.5/add1.5) | 0.64 ± 0.15 D |
| C (DZ3.0/add3.0) | 0.43 ± 0.17 D |
| D (DZ3.0/add1.5) | 0.34 ± 0.15 D |
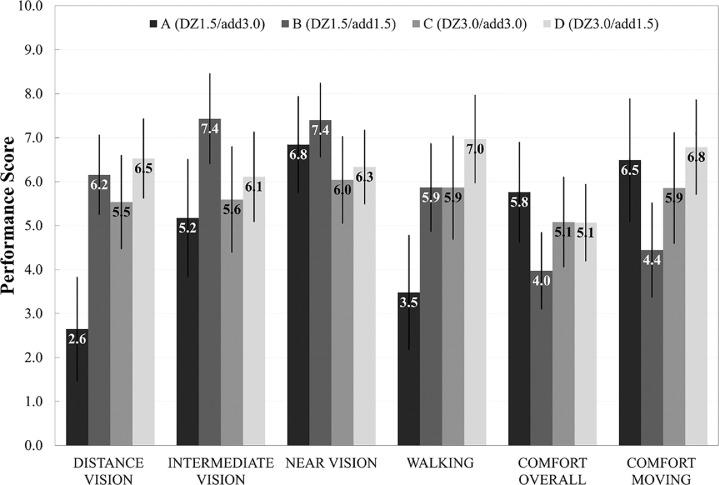
Subjective response to vision and comfort
Fig. 4 shows significant effect of lens design on the subjective ratings of lens performance after one-week lens adaptation (F(3,20.5) = 5.73, p < 0.01). Post hoc comparison showed that distance vision and vision while walking were significantly worse with design A (DZ1.5/add3.0) than with other designs. No significant effect of MFGPCL design was observed on intermediate and near vision performance.
Figure 4.
Mean scores for the subjective responses obtained on one week of lens wear. Error bars represent 84% confidence interval. Asterisks denote a statistically significant difference (p <0.05).
Discussion
MFSCLs are one of the evidence-based optical treatments used for myopia control. The use of center distance with peripheral add designs has been increasing in recent years. The impact of MFSCL on visual function was investigated in several studies; however, similar optical concepts applying to GP modality and their impact on myopia progression and visual functions have been poorly explored. It has been reported that acceptable visual performance with MFCLs is critical to good long-term compliance. This pilot study aimed to examine the effect of several center-distance peripheral-near MFGPCLs, designed specifically for myopia control, on visual functions including visual acuity, contrast sensitivity, and accommodation, using four MFGPCL optical designs with two different peripheral near additions (+1.50 and +3.00 D) and two center zone sizes (1.5 and 3.0 mm).
This pilot study did not find a significant impact of either the add power or the relative area of distance vs. center optics on DVA, likely due to the smaller sample size hence reduced statistical power. However, the subjective rating showed that design A deteriorated distance vision more than other lens designs. Kang et al.14 found a reduction of 3.5 letters in distance VA with MFSCL with +3.00 D add power. Another study by Sanchez et al. noticed one line decline in distance VA when MFSCL with low and high add powers (+1.50 D and +2.50 D) were used in young adults.15 Schulle et al. found that an overcorrection of 0.50 to 0.75 D is required to improve the declined distance VA with MFSCLs with +2.50 D add power to best-corrected VA.16 All MFGPCL designs in the current study showed no significant reduction in near visual acuity. Participants’ responses to intermediate and near vision showed similar performance scores among all designs.
The discrepancy between change in distance VA and CS with lens A could primarily be explained by the fact that it was easier to resolve fine details at distance. It also indicated that distance VA only measured the ability of the eye to resolve details at a specific distance with high contrast. Studies have indicated that VA alone is less informative to assess visual function than contrast sensitivity.17 Distance contrast sensitivity (CS) provides more insights in evaluating the visual function. In this study, distance CS function was measured at five spatial frequencies. As expected, contrast sensitivity function was higher for single vision spectacles than MFGPCLs. A significant reduction in contrast sensitivity function was found with MFGPCL design A (DZ1.5/add3.0). Similar findings have been reported in other studies. It seems the contrast sensitivity function is largely dependent on MFCL design and add power. Sanchez et al. found a reduced contrast sensitivity function in subjects wearing MFSCLs with low to medium add power (+1.50 and +2.50 D).15 A similar reduction was reported in children wearing MFSCL (center distance with +2.50 D add).18 Przekoracka and colleagues19 investigated the effect of MFSCL designs with two add powers (2.00 and 4.00 D) as well as two center zone sizes (3.0 and 4.5 mm) on contrast sensitivity. Add power of 2.0 D reduced contrast sensitivity function significantly but not with 4.0 D add. The two zone diameters did not differ in contrast sensitivity function. Pauné et al. tested contrast sensitivity function with MFGPCL with 1.50 D add power and found no significant difference when compared to single vision GP lens or MFSCL with the same power profile.10 Our results showed a combination of 3D add power and 1.5 mm zone impacted contrast sensitivity across all tested frequencies, while the impact from the other three designs (B, C, and D) did not reach statistical significance.
Generally, myopes exhibit larger accommodative lag compared to emmetropes and hyperopes.20,21 One of the hypotheses regarding myopia development in children is that the retinal hyperopic defocus experienced with accommodative errors during near work stimulates ocular elongation. The use of multifocal spectacle and contact lens may reduce the accommodative focusing error. Some previous studies reported a reduced accommodative response (more accommodative lag) with MFSCLs,14,18 whereas others found an increased accommodative response (reduced lag).22 Ruiz-Alcocer et al. and Montes et al. measured accommodative response measured at different accommodative stimuli with two center- near MFSCLs designs [low (up to +1.50 D) and high add (greater than +1.75 D)]. Their results showed non-presbyopic young adults were accommodating normally and found no significant change in accommodation with MFSCL compared to single vision soft contact lens (SVSCL).23,24 The inconsistent findings from previous studies may have been partially attributable to different experimental setup and measurement techniques. Nonetheless, that suggests accommodative changes with MF optics may not play an essential role in its myopia controlling effect. Our data revealed no difference in accommodative lag measured at 33 cm between all MFGPCL designs. It is worth noting that single vision GP would offer a closer comparison to the tested MFGPCL designs. However, the significant lens awareness, reflex tearing, and excessive lens movement would significantly increase the variability of accommodative measurements. Future studies in a longer duration could benefit from a longer run-in period of single vision GP wear, followed by an accommodative measurement prior to switching to MFGPCL treatment.
The current study had three important limitations. First, the longer-term impact of MFGPCL on visual functions was not measured due to the short follow-up duration of the study, which should be monitored in future studies since myopia control treatments typically extend for years during childhood. Second, the current study only involved young adults with stable myopia or emmetropia. Same designs offered to progressing myopic children may show different behavior in visual performance such as accommodation and subjective response. Last, this pilot study suffered from a relatively small sample size nonetheless provided an overview on how manipulating the add power and center zone diameter in center-distance MFGPCL designs could impact visual performance in young adults. Furthermore, it is noted that this is a preliminary study exploring the important parameters of MFGP designs in impacting visual performance. Due to the consequence of dropout, not all subjects were worn all lens designs which may impact the power of the analysis. Future studies with a larger sample is suggested.
To our knowledge, this was the first study to explore the impact of several experimental center-distance MFGPCL on visual functions in non-presbyopes. The impact on visual function was similar to what was found with MFSCLs in visual acuity, contrast sensitivity function, and accommodation. The results of this study indicated that MFGPCL in various distance zone sizes and add powers, fitted to young myopes, were quickly adapted and well-tolerated without significant visual compromise as observed by visual acuity and contrast sensitivity except with design A (DZ1.5/add3.0). A longer study using the three promising designs (B, C, and D) in the pediatric population is warranted to confirm its long-term tolerance and anti-myopia efficacy.
Source of funding
There is no funding to report for this submission. The result of this work has been presented at the American Academy of Optometry annual meeting as a poster in October 2020.
Conflicts of interest
We wish to confirm that there are no known conflicts of interest associated with this publication. There has been no significant financial support for this work that could have influenced its outcome.
Acknowledgements
The authors extend their appreciation to Dr. Richard Wu (Brighten Optix Laboratory, New Taipei City, Taiwan) for the help in designing and providing the contact lens used in this study.
References
- 1.Saw S.-.M., Gazzard G., Shih-Yen E.C., Chua W.-.H. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25(5):381–391. doi: 10.1111/j.1475-1313.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- 2.Smith E.L. Optical treatment strategies to slow myopia progression: effects of the visual extent of the optical treatment zone. Exp Eye Res. 2013;114:77–88. doi: 10.1016/j.exer.2012.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu Y., Wildsoet C. The effect of two-zone concentric bifocal spectacle lenses on refractive error development and eye growth in young chicks. Invest Opthalmol Vis Sci. 2011;52(2):1078. doi: 10.1167/iovs.10-5716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Y., Wildsoet C. The effective add inherent in 2-zone negative lenses inhibits eye growth in myopic young chicks. Invest Ophthalmol Vis Sci. 2012;53(8):5085–5093. doi: 10.1167/iovs.12-9628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kollbaum P.S., Dietmeier B.M., Jansen M.E., Rickert M.E. Quantification of ghosting produced with presbyopic contact lens correction. Eye Contact Lens. 2012;38(4):252–259. doi: 10.1097/ICL.0b013e31825aa879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anstice N.S., Phillips J.R. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118(6):1152–1161. doi: 10.1016/j.ophtha.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 7.Sankaridurg P., Holden B., Smith E., et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Opthalmol Vis Sci. 2011;52(13):9362. doi: 10.1167/iovs.11-7260. [DOI] [PubMed] [Google Scholar]
- 8.Walline J.J. A randomized trial of the effects of rigid contact lenses on myopiaprogression. Arch Ophthalmol. 2004;122(12):1760. doi: 10.1001/archopht.122.12.1760. [DOI] [PubMed] [Google Scholar]
- 9.Katz J., Schein O.D., Levy B., et al. A randomized trial of rigid gas permeable contact lenses to reduce progression of children's myopia. Am J Ophthalmol. 2003;136(1):82–90. doi: 10.1016/S0002-9394(03)00106-5. [DOI] [PubMed] [Google Scholar]
- 10.Pauné J., Queiros A., Quevedo L., Neves H., Lopes-Ferreira D., González-Méijome J.M. Peripheral myopization and visual performance with experimental rigid gas permeable and soft contact lens design. Contact Lens Anterior Eye. 2014;37(6):455–460. doi: 10.1016/j.clae.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Pauné J., Queiros A., Lopes-Ferreira D., Faria-Ribeiro M., Quevedo L., Gonzalez-Meijome J.M. Efficacy of a gas permeable contact lens to induce peripheral myopic defocus. Optom Vis Sci. 2015;92(5):596–603. doi: 10.1097/OPX.0000000000000582. [DOI] [PubMed] [Google Scholar]
- 12.Fedtke C., Ehrmann K., Thomas V., Bakaraju R.C. Visual performance with multifocal soft contact lenses in non-presbyopic myopic eyes during an adaptation period. Clin Optom. 2016:37. doi: 10.2147/OPTO.S96712. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fedtke C., Bakaraju R.C., Ehrmann K., Chung J., Thomas V., Holden B.A. Visual performance of single vision and multifocal contact lenses in non-presbyopic myopic eyes. Contact Lens Anterior Eye. 2016;39(1):38–46. doi: 10.1016/j.clae.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Kang P., Wildsoet C.F. Acute and short-term changes in visual function with multifocal soft contact lens wear in young adults. Contact Lens Anterior Eye. 2016;39(2):133–140. doi: 10.1016/j.clae.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Sanchez I., Ortiz-Toquero S., Blanco M., Martin R. A new method to analyse the effect of multifocal contact lenses on visual function. Contact Lens Anterior Eye. 2018;41(2):169–174. doi: 10.1016/j.clae.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 16.Schulle K.L., Berntsen D.A., Sinnott L.T., et al. Visual acuity and over-refraction in myopic children fitted with soft multifocal contact lenses. Optom Vis Sci. 2018;95(4):292–298. doi: 10.1097/OPX.0000000000001207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeri F., Calcatelli P., Funaro E., Martelli M., Naroo S.A. How accurate is an lcd screen version of the Pelli–Robson test? Int Ophthalmol. 2018;38(4):1473–1484. doi: 10.1007/s10792-017-0609-0. [DOI] [PubMed] [Google Scholar]
- 18.Gong C.R., Troilo D., Richdale K. Accommodation and phoria in children wearing multifocal contact lenses. Optom Vis Sci. 2017;94(3):353–360. doi: 10.1097/OPX.0000000000001044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Przekoracka K., Michalak K., Olszewski J., et al. Contrast sensitivity and visual acuity in subjects wearing multifocal contact lenses with high additions designed for myopia progression control. Contact Lens Anterior Eye. 2020;43(1):33–39. doi: 10.1016/j.clae.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Gwiazda J., Thorn F., Held R. Myopic children show insufficient accommodative response to blur. Invest Ophthalmol Vis Sci. 1993;34(3):5. [PubMed] [Google Scholar]
- 21.Gwiazda J., Thorn F., Held R. Accommodation, accommodative convergence, and response ac/a ratios before and at the onset of myopia in children. Optom Vis Sci. 2005;82(4):273–278. doi: 10.1097/01.OPX.0000159363.07082.7D. [DOI] [PubMed] [Google Scholar]
- 22.Tarrant J., Severson H., Wildsoet C.F. Accommodation in emmetropic and myopic young adults wearing bifocal soft contact lenses: accommodation wearing bifocal soft contact lenses. Ophthalmic Physiol Opt. 2008;28(1):62–72. doi: 10.1111/j.1475-1313.2007.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruiz-Alcocer J., Madrid-Costa D., Radhakrishnan H., Ferrer-Blasco T., Montés-Micó R. Changes in accommodation and ocular aberration with simultaneous vision multifocal contact lenses. Eye Contact Lens. 2012;38(5):288–294. doi: 10.1097/ICL.0b013e3182654994. [DOI] [PubMed] [Google Scholar]
- 24.Montés-Micó R., Madrid-Costa D., Radhakrishnan H., Charman W.N., Ferrer-Blasco T. Accommodative functions with multifocal contact lenses: a pilot study. Optom Vis Sci. 2011;88(8):998–1004. doi: 10.1097/OPX.0b013e31821c0ed8. [DOI] [PubMed] [Google Scholar]