Abstract
Self-medication (SM) is a global and growing phenomenon. It represents a public health problem due to antibiotic resistance, risk of adverse drug reactions, drug–drug interactions, disease masking, and increased morbidity. There is not a consensus on the definition of SM. The definitions found in different studies make it difficult to address this problem from a theoretical perspective and therefore find an adequate solution to this public health problem. The aim of this article is to search the medical literature to characterize the current understanding of SM in the medical community. We conducted a scoping review of definitions of SM by searching on PubMed – Medline, Embase, and LILACS using the following combination of keywords: ‘self-prescription’ or ‘self prescription’, ‘self-medication’ or ‘self medication’, or ‘automedication’ and ‘definition’ or ‘explanation’. The search was limited to articles containing the definition of SM, with no limit on language or year. Duplicate studies and those that did not mention the definition of SM were excluded from the final review. A total of 65 studies were included in the final selection. We found a vast heterogeneity in the definition of SM. Most articles based their definition of SM on the process of obtaining the drug, the nonparticipation of a specific health professional, the source of the medication, and the reason for SM. Other interesting concepts such as self-care, nonadherence to a prescription, reuse of stored drugs, and sharing and lending medicines were also considered forms of SM by other authors, however. This study highlights the need to reach a consensus regarding the definition of SM to adequately propose strategies to address this global health problem. This study shows the diverse concepts that need to be included in a future definition of SM.
Plain Language Summary
Definition of self-medication: a review with systematic methodology
Self-medication (SM) is a global and growing phenomenon that represents a public health problem due to antibiotic resistance, risk of dangerous side effects, interactions between drugs, and disease masking. Currently, there is not a consensus on the definition of SM, which makes it difficult to address this problem and therefore find an adequate solution. Making a standard definition would allow the development of programs focused on addressing drug-related problems associated with self-medication behavior. The purpose of this article is to search the medical literature to define the current understanding of SM in the medical community. We included a total of 65 studies and found a great variance in the definition of SM. Most articles based their definition of SM on the process of obtaining the drug, the nonparticipation of a specific health professional, the source of the medication, and the reason for SM. Other interesting concepts such as self-care, not following a prescription, reuse of stored drugs, and sharing and lending medicines were also considered forms of SM by other authors, however. Furthermore, this study highlights that SM is a wider concept that goes beyond aiming to promote and restore health, as aesthetic and recreational purposes are also reasons for SM that can put individuals at risk and compromise the correct and safe use of medications.
Keywords: adverse drug reactions, concept formation drug safety, drug interactions, pharmacovigilance, self-medication
Introduction
Self-medication (SM) is a phenomenon that has a much more complex definition than is currently proposed. It is a complex behavior that has an evolutionary and adaptive foundation. It has manifested itself in various species from arthropods to the first humans, to combat the threats that their context imposes on them, one of which is disease and the symptoms that accompany it. It has been observed in various mammals, such as the great apes of Africa, who use substances without nutritional value from plants to treat or control parasitic diseases. 1 Likewise, it has been shown in arthropods such as monarch butterflies, who fight parasitic infection by deliberately consuming the plant Asclepias curassavica. 2
In addition, it has been proposed that the first humans who were able to observe this animal behavior learned the different properties of nature and began to self-medicate to alleviate their symptoms. 1 Among them, we take as an example the Neanderthals, a species belonging to the Hominidae family and an ancestor to modern humans, who consumed and ingested plants such as yarrow and chamomile, which have little nutritional value and a bitter taste, but have various medicinal properties, the first as an astringent and the second as an anxiolytic, in addition to its anti-inflammatory properties. 3 The deliberate consumption of these bitter plants, usually avoided due to their potential danger, is considered as evidence of SM in this ancestor species. 3 This adaptive behavior was conserved throughout the evolution of the species, as demonstrated by the finding of a fungus (Fomitopsis betulina) with purgative and antibiotic properties within the belongings of the ‘ice man’, a specimen of homo sapiens mummified around the year 3300 BC who was infested with Trichuris trichiura; it is thought that man used the aforementioned fungus for the purpose of alleviating the illness. 4
Therefore, it is possible to understand SM as a self-care behavior 5 that also functioned as the first origin of health care, which was passed from generation to generation. Compilations of information on the use of different plants and substances for the treatment of various diseases in the ancient world have been found. In Egypt, papyri from 2000 BC described more than 900 prescriptions of different types of plants and mineral materials for the resolution of various symptoms. Likewise, similar documents have been found in China and India. 5 In medieval times in Europe, SM gained importance, demonstrated by the publication of the popular poem ‘Regimen Sanitatis’, in which health advice and treatment for diseases were given. This text appeared around the 13th century, went through multiple editions, was translated into English in the 16th century, and in fact some editions have appeared in our time. 5
This behavior has a high prevalence worldwide. Globally, the prevalence of SM ranges from 11.2% to 93.7%, depending on the country being analyzed and the target population. 6 The prevalence varies by country, with a more pronounced prevalence observed in developing countries. Among the most used medications are analgesics and antipyretics (44.3%), followed by nonsteroidal anti-inflammatory drugs (36.4%) and antihistamines (8.5%). 7 It should be noted that easy access to the Internet and smartphones has allowed the general population to have medical/pharmacological information at their disposal, avoiding the need to turn to an expert. 8 This behavior can have risks and disadvantages such as drug interactions, intoxication, bacterial resistance, and liver or kidney disease, among others. It can also be understood as a useful practice to control the high demand on health-care systems, however. 9
Attempts have been made to give different definitions to this concept over time, one of them given by the World Health Organization (WHO) as ‘the selection and use of medicines by individuals to treat self-recognized illnesses or symptoms’ 10 or by health personnel such as the self-prescription of drugs not prescribed by a doctor. 11 Although SM can be seen as a self-care behavior, there are circumstances in which this definition cannot be restricted to the context of health. An example of this is seen in doping, in which athletes or the student population seek an increase in physical or cognitive performance, but also in the recreational use of substances, in their use for aesthetic purposes, weight reduction, and the termination of unwanted pregnancy, among others.12–14 The first step to obtain a complete definition of SM is to reach a consensus about this concept in the medical community, however, in order to adequately study the practices and behaviors associated with it. Reaching a unified consensus about SM will allow us to:
Promote a better understanding and awareness of the practice of SM.
Categorize SM outside of the health context, for a better understanding and approach to the problem.
Help to identify and prevent the incidence of adverse events associated with this behavior.
Identify individuals with risk factors for SM and be able to promote the safe use of medications or substances.
Therefore, it is pertinent to carry out a scoping review of the definitions of SM in the medical literature, to observe what the academic community understands by SM, and finally to reach a consensus of experts in which a broader definition of this behavior can be given beyond self-administration of medication not prescribed by a physician or in a manner not directed by a physician.
Methods
Search strategy
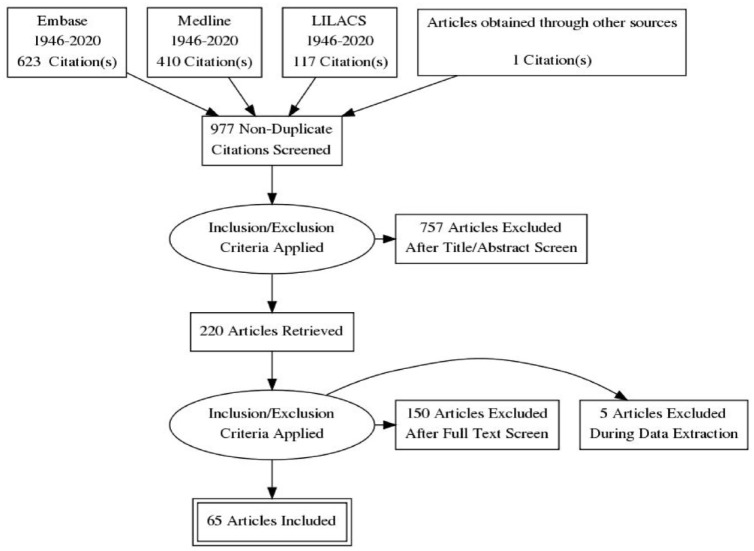
We conducted a scoping review of definitions of SM. The search was conducted in Medline, Embase, and LILACS databases from inception to 9 August 2020, for articles containing a definition of SM. One additional article was found by other sources. The search was conducted with the following keywords: ‘self-prescription’ or ‘self prescription’, ‘self-medication’ or ‘self medication’, or ‘automedication’ and ‘definition’ or ‘explanation’. The search was limited to articles which defined the concept of SM, with no limit on language or year. Articles with only abstracts available were not included in the final selection. A total of 1151 articles were found: 623 from Embase, 410 from Medline, 117 from LILACS, and 1 from other sources. After the removal of duplicates, 977 articles remained for abstract and title screening as can be seen in Figure 1.
Figure 1.
PRISMA diagram.
Screening and data extraction
The inclusion criteria were articles that provided a definition of SM in the abstract or title, in any language or any year. The exclusion criteria were the articles that were not found in full text or those that did not provide a definition of SM. One author (J.E.F.-A.) conducted the initial database search. Thereafter, he and another five authors were assigned to select or exclude the articles based on the presence of a definition or a possible explanation of SM. At least two authors independently screened the title and abstract of each article found in the search. After the initial selection, the results were compared and the percentage of agreement was 76%, with a Cohen’s k of 0.43 suggesting a moderate agreement. The articles that were selected by one evaluator but not the other were assessed by a third evaluator (F.S.). After this initial screening, 757 articles were excluded for not having a definition of SM. Thereafter, the selected 220 full-text articles were downloaded and reviewed by the 6 evaluators independently, including only articles that contained an explicit definition of SM. Articles in a language different from Spanish or English were translated and included if they met the inclusion criteria. One hundred and fifty articles were excluded because the full-text version was not available (they were only found as posters) or because they did not include a definition of SM. Data items extracted included country, type of article, definition of SM, reference, and year of the definition provided, and the context in which SM was being considered. Once the data extraction was complete, all authors reviewed the content analysis for each of the extracted studies, and during an expert meeting, the categories shown in Table 1 were extracted. Five more articles were excluded during data extraction because they did not provide an explicit definition of SM. Considering that several of the articles did not correspond to studies (e.g. narrative reviews and guidelines), the quality assessment was not carried out for the articles that were part of this review (Figure 2).
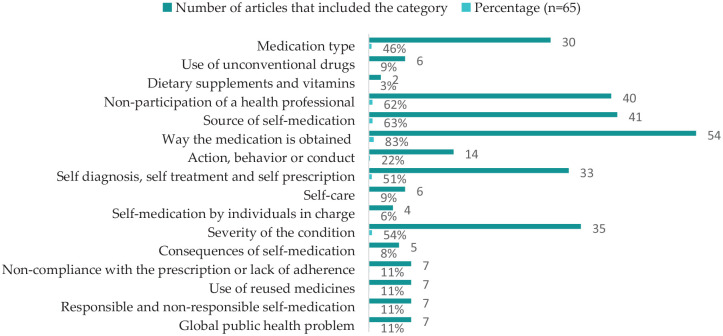
Table 1.
Terms used in the concept of SM proposed by the authors of the 65 selected articles.
| Category | Number of articles that included the category | Percentage (n = 65) | Reference |
|---|---|---|---|
| Medication type | 30 | 46 | 15–43 |
| Use of unconventional drugs | 6 | 9 | 15,18,24,30,44,45 |
| Dietary supplements and vitamins | 2 | 3 | 19,24 |
| Nonparticipation of a health professional | 40 | 62 | 15,18–22,24,26–30,32–37,39,43,44,46–64 |
| Source of self-medication | 41 | 63 | 8,18,22,23,25,26,28–31,33,36–38,40–42,44,45,47,48,50,52,54–57,60,61,63,65–75 |
| Way the medication is obtained | 54 | 83 | 8,15,16,18–20,22,23,25,27–42,44,45,47–53,55–61,63,65–76 |
| Action, behavior or conduct | 14 | 22 | 15,32,35,36,44–46,48,49,54,56,57,62,77 |
| Self-diagnosis, self-treatment, and self-prescription | 33 | 51 | 8,15,22,25,26,29,37,38,40,41,43–48,53,55,56,61,63–72,74,76,77 |
| Self-care | 6 | 9 | 37,50,52,56,67,72 |
| Self-medication by individuals in charge | 4 | 6 | 23,28,45,66 |
| Severity of the condition | 35 | 54 | 8,15,18,22,23,25,28,29,31,35–37,39–42,48,50,54,56,57,60,61,63,65–72,74–76 |
| Consequences of self-medication | 5 | 8 | 15,22,67,69,78 |
| Noncompliance with the prescription or lack of adherence | 7 | 11 | 8,41,43,45,62,68,71 |
| Use of reused medicines | 7 | 11 | 29,33,45,47,51,55,56 |
| Responsible and nonresponsible self-medication | 7 | 11 | 23,30,35,42,49,51,69 |
| Global public health problem | 7 | 11 | 15,23,27,40,41,51,68 |
Figure 2.
Terms used in the concept of SM proposed by the authors of the 65 selected articles.
Results
The definitions found in the 65 selected articles were categorized into 16 categories which can be seen in Table 1.
Forty-six percent (n = 30) of the articles considered the type of medication when defining SM behavior, for example, over-the-counter (OTC) medications, allopathic medications, prescription medications, synthetic medications, industrialized medications, or conventional products. Nine percent (n = 6) included the use of nonconventional medications such as home remedies, handmade medications, or herbal products. Only 3% (n = 2) included the use of dietary supplements or vitamins.
Sixty-two percent (n = 40) included the nonparticipation of a health professional, that is, not having a prior consultation, specifically not having the participation of a doctor, or not having a prescription, indication, or surveillance by a health professional. In addition, 63% (n = 41) of the articles included the source of the SM, taking into account self-treatment, advice from unauthorized persons, or medication sharing among family and friends.
The way the medication was obtained was included by 83% (n = 54) of the articles, including the selection, the act of buying and obtaining, the use and consumption, or lending or borrowing the drugs or substances. Furthermore, 22% (n = 14) of the articles included the terms action, behavior, or conduct when defining SM. This included concepts like searching for help, the willingness or ability to participate intelligently, autonomously, and in a self-informed way in preventative, diagnostic, and therapeutic decisions, and the description of SM as a self-appointed practice.
Likewise, 51% (n = 33) of the articles included terms such as self-diagnosis, self-treatment, and self-prescription in the definition of SM, and 9% (n = 6) considered it as a form of self-care. In addition, SM to third parties such as children or older adults by their care takers was included in 6% (n = 4) of the articles.
The severity of the condition was included by 54% (n = 35) of the articles, taking into account SM as a response to minor ailments, common problems, prevention of minor disorders, chronic or recurrent diseases or symptoms, or even to imaginary pathologies. Eight percent (n = 5) included the consequences of SM, such as the use of inadequate doses, the inappropriate choice of medication or substance, or polypharmacy.
Notably, 9% (n = 6) included nonadherence to the prescription, including intermittent use of prescribed medications, not fully complying with the prescription, altering the time of treatment, or changing the dose. Eleven percent (n = 7) of the articles included the use of recycled medications, considering the use of old prescriptions for previous symptoms, or the use of medications available at home.
Eleven percent (n = 7) of the articles also included the term responsible and nonresponsible SM, considering nonresponsible SM as that which led to risks, masking of symptoms and complications, or responsible as that which was safe and effective. Finally, 11% (n = 7) of the articles considered SM as a public health problem, including that it is more frequent in developing countries, that it is a growing health problem and a global phenomenon.
Discussion
The main common aspect found in the definitions in the reviewed academic literature on SM corresponds to the idea of individual action. This coincides with the conceptual reflections that have been published about SM62,79 in which this phenomenon is usually described in principle as an individual human action, behavior or conduct, with impacts at various levels, from a family to a global level. It, however, should be mentioned that the phenomenon has also been studied as an individual action, but in other animal species. 80 In that sense, it is an individual human action, but with a phylogenetic background. 81 In line with the above, the SM Behavior Observatory of the Universidad del Rosario (Bogotá, Colombia) has defined the phenomenon of SM as an ‘individual behavior’ in a broad sense, without restriction to our species. 11
The prefix ‘self-’ refers to ‘himself/herself’, that is, SM is a medication behavior directed toward the same subject who performs the action. The same individual, however, can intentionally orient his behavior toward other subordinate individuals, such as children (SM in the pediatric setting) 82 or pet SM in the veterinary setting. 83 Interestingly, this SM behavior directed at others can be observed in other species. 84
When considering SM in humans, the WHO has created a series of criteria to further classify this behavior as responsible SM. Responsible SM is defined by the WHO as ‘the practice whereby individuals treat their ailments and conditions with medicines which are available and approved without prescription, and which are safe and effective when used as directed’. 10 In addition, it requires the use of medicines that are of proven safety, quality, and efficacy, and used for the indicated condition. Furthermore, the condition must be self-recognizable, or in the case of chronic conditions, it requires an initial medical diagnosis. To be considered responsible SM, it also needs to involve an appropriate dose and dose forms. 10 This definition, however, has some problems and limitations. First, a self-recognizable condition is a broad concept that would imply some degree of knowledge by the individual. Second, there would be no limit in determining what is a self-recognizable condition and what is not, and it further confers a power of self-diagnosis to nonmedical individuals. It would be more accurate to classify responsible SM when mild and recurrent symptoms occur in young patients without comorbidities, for example, the treatment of a headache or a cold with the adequate medicine and dose. Furthermore, the initial contact with the pharmacist when self-medicating is crucial and should be more relevant in the context of self-care. When managing mild symptoms, the pharmacist should be able to correctly advice the individual when it is necessary to consult a doctor, such as giving warning signs to common symptoms. We found that only 11% (n = 7) of the analyzed articles took responsible SM into account in their definition.
We, however, found that 62% (n = 40) of the articles considered that SM involved the nonparticipation of a specific health professional. Indeed, not all health professionals are suitable to prescribe. In the United States, advanced registered nurse practitioners, dentists, osteopathic physicians, physicians, and podiatric physician can prescribe medicines without restrictions, while other professionals such as optometrists, naturopathic doctor, pharmacists, and physician assistants can only prescribe under certain conditions (under agreement with the authorized prescriber, or as approved by the medical commission, among others). 85
Furthermore, we found that some authors used the terms self-recognition, self-prescription, and self-administration to define SM. This suggests an association between SM and self-care. SM, but specifically responsible SM, forms a part of self-care because it is a behavior that involves practices to promote and maintain one’s health. The WHO defines self-care as ‘the ability of individuals, families and communities to promote health, prevent disease, maintain health, and cope with illness and disability with or without the support of a health worker’ implicitly including SM. 86
The source of SM is an important parameter to be analyzed in this behavior. One of the most under-considered sources is the sharing of medicines between family and friends. Sharing of medications can be defined as borrowing or lending medication in which the receiver of the medicines is not the individual for whom the medicine was initially prescribed. A study aimed to explore the reasons for sharing prescription analgesics and the awareness of the risks of this behavior. 73 They found that lending prescription pain medication was more common than lending nonprescription medications, and most participants admitted lending analgesics to family, friends, neighbors, and sometimes with work colleagues. The reasons for sharing medications were distrust in physicians, inconvenience of contacting a physician, no access to a health-care professional, or an emergency situation such as severe pain.
During the literature search, the definition of SM varied significantly between different authors. Despite the heterogeneity found in our results, it was also found that many authors made reference to the definition proposed by the WHO. In multiple occasions, however, there was misquoting of this source, giving incomplete definitions compared with the one stated by the WHO, leaving behind important information.37,49,76 Furthermore, some authors quoted the definition given by the WHO directly, but made completely unrelated postulations, adding new terms not mentioned in the original definition.36,64
We further encountered another very important aspect of SM not commonly mentioned in the existing literature. Poor adherence to the prescription is also a type of SM because when patients do not follow the instructions provided by the health professional, they are consuming the medication based on their own knowledge and with no supervision regarding dose, length of the treatment, adverse drug reactions 61 approved uses, and whether the medicine is safe and effective for such use.18,78 Poor adherence is also seen when patients fail to adhere to an already established treatment duration, prolonging or shortening the treatment. 45
An additional feature of SM concerns the reuse and recycling of medication, whether this involves acquiring medicines based on old prescriptions recommended under different symptoms and circumstances47,55,56 or using leftover medicines stored at home (already in one’s possession).29,33,45 This aspect of SM is not largely explored in the literature, yet it describes a situation that presents itself very commonly in daily life, and is a practice that can broaden the contexts in which SM is practiced; it is an important aspect that should be included in the definition of SM.
Furthermore, the use of nonconventional medicine, namely, home remedies, handmade medications and, more significantly, herbal products was also evaluated. Including these types of medications in the definition of SM is crucial as the use of herbal remedies is constantly increasing throughout the world, 87 and in some regions of the world, it is the main approach to healing. It is usually regarded as a harmless, or as a natural method for treating diseases; however, it is of great relevance to the field of pharmacology, because different herbal products can interact with traditional medicine, causing serious adverse effects, like hepatotoxic effects, described with more than 300 plant species. 88 It also affects certain demographic groups, such as the elderly, pregnant/menopausal women, and dermatological patients, among others. This topic was unexplored and under-considered in the publications reviewed. It is worth mentioning the use of these products in the definition of SM because they can cause clinically relevant interactions, and most of the population do not consider the use of these products as a form of SM, usually omitting this type of information.
SM is not only a response for acute symptoms, such as fever, pain, or flu-like symptoms16,89,90 but also for recurring symptoms in chronic diseases; 41 in such cases, patients are usually familiarized with their condition and prefer to self-medicate rather than getting proper reassessment for their symptoms. Patients with chronic diseases or their significant others may also believe they have accurate knowledge on how to manage certain symptoms or syndromes, increasing the likelihood of them giving advice on how to self-medicate to others. This is another field that is worth intervening in, in order to prevent drug misuse.
Finally, we have the vastly unexplored topic of SM with vitamins, supplements, and other products 19 not aimed toward healing a symptom or disease, but rather to satisfy non-health-related problems, or for treating problems that lie at the margins of health and well-being. The main difference is that people who engage in this particular kind of SM are trying to accomplish unfulfilled desires or aspirations; examples are many, for instance, the use of minoxidil to reduce baldness, erythropoietin to enhance athletic performance, or hormones for physical culturism. One of the hallmarks of this kind of situation is that it is aimed at improving physical, cognitive, or aesthetic performance; in spite of this, information on this kind of SM was not detected in the review, meaning that we are lacking valuable information on SM beyond the health-care system. The scarcity of data concerning this topic prevents people and health professionals from getting pertinent information and education about the side effects and risks they might encounter, or the alternative, safer solutions they should consider. 91
Given the above, we propose that the definition of SM should be carefully revised, and a new and broader definition should be implemented. The definition should include various concepts regarding the type of medications being used, the purpose of SM, the source of the medication, the severity of the condition, the type of individual who is self-medicating, and the professional prescribing or recommending the medication, among others. Therefore, we propose that the following concepts should be included in a future consensus regarding the definition of SM.
We believe SM should be regarded as a process in which OTC and prescription medications, herbal products, home-made remedies, nutritional supplements and vitamins are purchased, selected, used, and consumed; it is a behavior in which the individual aims to treat self-recognized disorders or symptoms 48 or tries to alleviate third parties’ ailments. The purpose of SM includes the promotion of health, 50 the satisfaction of a non-health goal 91 such as enhancement of cognitive and physical performance, and for aesthetic and recreational purposes. 11 It also includes the consumption of a drug without professional advice, prescription and supervision regarding indication, dose, duration of treatment for chronic or acute symptoms, or not adhering correctly to a prescription 66 favoring drug misuse, such as over-dosing, under-dosing, or polypharmacy. 70 SM also includes taking a prescription or advice from a nonauthorized health-care professional such as by suggestion of a pharmacist/pharmacy attendant, relative, friend, neighbor, or by the patient’s own initiative. 55
SM includes acquiring medicines based on old prescriptions recommended under different symptoms and circumstances (resubmitting old prescriptions from past treatments), or using leftover medicines stored at home (already in one’s possession), 56 sharing medicines with relatives or members of one’s social circle, borrowing or lending medications in situations in which the receiver of these drugs is not the individual to whom the medications were allocated, 73 or giving medication to members of the individuals’ relatives like the elderly or children. It is also a global health problem, common in developing countries, in which this trend is becoming more frequent due to low accessibility to health care, scarcity of medical personnel, and poverty. 51
The limitations of this study include restricting our search to Embase, LILACS, and Medline, considering that some important definitions may not be included in these databases. Furthermore, some articles that included a definition of SM were not found in full text and were therefore not included.
Future studies should perform a search involving more databases and include articles that are beyond the medical literature, as SM is a broad and interdisciplinary concept that can have different definitions according to a specific field. Nonetheless, SM has important implications in pharmacovigilance, and future studies should aim to generate a universal consensus around the definition that aims to identify more behaviors of inappropriate SM, in order to address them as potential medication errors.
Conclusion
In conclusion, this study highlights the need to reach a consensus regarding the definition of SM, in order to adequately propose strategies to address this global health problem. This study shows the diverse concepts that need to be included in a future definition of SM. The proper definition of SM would allow for the development of pharmacovigilance programs focused on addressing drug safety related to SM behavior. SM is a wider concept that goes beyond the purpose of promoting and restoring health; aesthetic and recreational purposes are also examples of SM that can put individuals at risk and compromise the correct and safe use of medications.
Supplemental Material
Supplemental material, sj-docx-1-taw-10.1177_20420986221127501 for Definition of self-medication: a scoping review by Daniela Baracaldo-Santamaría, Maria José Trujillo-Moreno, Andrés M. Pérez-Acosta, John Edwin Feliciano-Alfonso, Carlos-Alberto Calderon-Ospina and Franklin Soler in Therapeutic Advances in Drug Safety
Supplemental material, sj-xlsx-2-taw-10.1177_20420986221127501 for Definition of self-medication: a scoping review by Daniela Baracaldo-Santamaría, Maria José Trujillo-Moreno, Andrés M. Pérez-Acosta, John Edwin Feliciano-Alfonso, Carlos-Alberto Calderon-Ospina and Franklin Soler in Therapeutic Advances in Drug Safety
Acknowledgments
The authors thank Tim Hiley for English language editing.
Footnotes
ORCID iD: Carlos-Alberto Calderon-Ospina  https://orcid.org/0000-0002-7305-8727
https://orcid.org/0000-0002-7305-8727
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Daniela Baracaldo-Santamaría, Pharmacology Unit, Department of Biomedical Sciences, School of Medicine and Health Sciences, Universidad del Rosario, Bogota, Colombia.
Maria José Trujillo-Moreno, Pharmacology Unit, Department of Biomedical Sciences, School of Medicine and Health Sciences, Universidad del Rosario, Bogota, Colombia.
Andrés M. Pérez-Acosta, Observatory of Self-Medication Behavior, School of Medicine and Health Sciences, Universidad del Rosario, Bogotá, Colombia
John Edwin Feliciano-Alfonso, Department of Internal Medicine, School of Medicine, Universidad Nacional de Colombia, Bogota, Colombia.
Carlos-Alberto Calderon-Ospina, Pharmacology Unit, Department of Biomedical Sciences, School of Medicine and Health Sciences, Universidad del Rosario, Bogota, Colombia; Observatory of Self-Medication Behavior, School of Medicine and Health Sciences, Universidad del Rosario, Bogotá, Colombia; Center for Research in Genetics and Genomics - CIGGUR, GENIUROS Research Group, School of Medicine and Health Sciences, Universidad del Rosario, Bogotá, Colombia.
Franklin Soler, Observatory of Self-Medication Behavior, School of Medicine and Health Sciences, Universidad del Rosario, Ak. 24 #63C-69 Bogotá 111221, Colombia.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Author contributions: Daniela Baracaldo-Santamaría: Conceptualization; Formal analysis; Investigation; Methodology; Writing – original draft; Writing – review & editing.
Maria José Trujillo-Moreno: Conceptualization; Formal analysis; Investigation; Methodology; Writing – original draft.
Andrés M. Pérez-Acosta: Conceptualization; Formal analysis; Investigation; Methodology; Writing – original draft; Writing – review & editing.
John Edwin Feliciano-Alfonso: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Software; Supervision; Validation; Writing – review & editing.
Carlos-Alberto Calderon-Ospina: Conceptualization; Formal analysis; Investigation; Methodology; Supervision; Writing – review & editing.
Franklin Soler: Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Supervision; Writing – original draft; Writing – review & editing.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by the Universidad del Rosario.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Not applicable.
References
- 1. Huffman MA. Animal self-medication and ethno-medicine: exploration and exploitation of the medicinal properties of plants. Proc Nutr Soc 2003; 62: 371–381. [DOI] [PubMed] [Google Scholar]
- 2. Choisy M, de Roode JC. The ecology and evolution of animal medication: genetically fixed response versus phenotypic plasticity. Am Natur 2015; 184(Suppl. 1), https://www.journals.uchicago.edu/doi/abs/10.1086/676928 [DOI] [PubMed] [Google Scholar]
- 3. Hardy K, Buckley S, Huffman M. Neanderthal self-medication in context. Antiquity 2013; 87: 873–878, https://www.cambridge.org/core/journals/antiquity/article/neanderthal-selfmedication-in-context/D08B14AC3BF8630A7D1C1FF6B4432875 [Google Scholar]
- 4. Capasso L. 5300 years ago, the Ice Man used natural laxatives and antibiotics. Lancet 1998; 352: 1864, https://pubmed.ncbi.nlm.nih.gov/9851424/ [DOI] [PubMed] [Google Scholar]
- 5. Leake CD. The history of self-medication. Ann N Y Acad Sci 1965; 120: 815–822, https://onlinelibrary.wiley.com/doi/full/10.1111/j.1749-6632.1965.tb56713.x [Google Scholar]
- 6. Chautrakarn S, Khumros W, Phutrakool P. Self-medication with over-the-counter medicines among the working age population in metropolitan areas of Thailand. Front Pharmacol 2021; 12: 726643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paudel S, Aryal B. Exploration of self-medication practice in Pokhara valley of Nepal. BMC Public Health 2020; 20: 1–5, https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-08860-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patel J, Jha R, Totade S, et al. Antibiotics as self medication amongst medical students. Res J Pharm Biol Chem Sci 2012; 3: 661–665, https://www.rjpbcs.com/pdf/2012_3(3)/[71].pdf [Google Scholar]
- 9. López J, Dennis R, Moscoso S. [A study of self-medication in a neighborhood in Bogotá]. Revista de salud publica (Bogota, Colombia) 2009; 11: 432–442, https://pubmed.ncbi.nlm.nih.gov/20027516/ [DOI] [PubMed] [Google Scholar]
- 10. World Health Organization. The role of the pharmacist in self-care and self-medication [Internet]. Report of the fourth WHO consultative group on the role of the pharmacist, 1998, http://apps.who.int/iris/bitstream/handle/10665/65860/WHO_DAP_98.13.pdf?sequence=1
- 11. Calderon CA, Perez-Acosta A. Farmacovigilancia y automedicación [Internet]. Editorial de la UAA, 2019, https://www.urosario.edu.co/Observatorio-del-Comportamiento-de-Automedicacion/documentos/farmacologia-11252019094300.pdf
- 12. al Rasheed F, Naqvi A, Ahmad R, et al. Academic stress and prevalence of stress-related self-medication among undergraduate female students of health and non-health cluster colleges of a public sector university in Dammam, Saudi Arabia. J Pharm Bioallied Sci 2017; 9: 251–258, https://pubmed.ncbi.nlm.nih.gov/29456376/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pradhan MR. ICTs application for better health in Nepal. Kathmandu Univ Med J (KUMJ) 2004; 2: 157–163. [PubMed] [Google Scholar]
- 14. Subashini N, Udayanga L. Demographic, socio-economic and other associated risk factors for self-medication behaviour among university students of Sri Lanka: a cross sectional study. BMC Pub Heal 2020; 20: 1–13, https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-08622-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aguado MI, Nuñez MB, Dos L, et al. Automedicación en estudiantes de Farmacia de la Universidad Nacional del Nordeste, Argentina. Acta Farmacéutica Bonaerense 2005; 24: 271–276. [Google Scholar]
- 16. Al-Maaz S, Abu-Dahab R, Shawagfeh M, et al. Prevalence and pattern of substance use and misuse among anesthesia health-care personnel in Jordan. J Subst Use 2019; 24: 317–322. [Google Scholar]
- 17. Almeida M, Castro LLC, Caldas E. sKnowledge, practices and risk perception in relation to the use of medicaments in the Federal District, Brazil. Revista de Ciencias Farmaceuticas Basica e Aplicada 32: 225–232, https://www.researchgate.net/publication/283247897_Knowledge_practices_and_risk_perception_in_relation_to_the_use_of_medicaments_in_the_Federal_District_Brazil [Google Scholar]
- 18. Anandhasayanam A. Assessment of self medication practices, consumers drug knowledge and consumption patterns at Tirur City, Malapuram (Dt) in Kerala. Int J Pharm Sci Rev Res 2016; 40: 78–83. [Google Scholar]
- 19. Berenzon S, Navarro S. El uso de las terapias alternativas y complementarias en población mexicana con trastornos depresivos y de ansiedad: Resultados de una encuesta en la Ciudad de México. Salud Mental 2009; 31: 107–115. [Google Scholar]
- 20. Bergmann J. Self-medication: from European regulatory directives to therapeutic strategy. Fundam Clin Pharmacol 2003; 17: 275–280, https://pubmed.ncbi.nlm.nih.gov/12803567/ [DOI] [PubMed] [Google Scholar]
- 21. Brusa P, Allais G, Scarinzi C, et al. Self-medication for migraine: a nationwide cross-sectional study in Italy. PLoS ONE 2019; 14: e0211191, https://pubmed.ncbi.nlm.nih.gov/30673780/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Carmona-Torres JM, Cobo-Cuenca AI, Recio-Andrade B, et al. Prevalence and factors associated with polypharmacy in the older people: 2006–2014. J Clin Nurs 2018; 27: 2942–2952, https://onlinelibrary.wiley.com/doi/full/10.1111/jocn.14371 [DOI] [PubMed] [Google Scholar]
- 23. Chanturia Z, Chumburidze T, Eriashvili B, et al. [Trends and risks of self-medication in Georgia]. Georgian Med News 2015: 240: 82–87. [PubMed] [Google Scholar]
- 24. da Costa I, Silva R, Carlos J, et al. Potentially inappropriate medications in older kidney transplant recipients: a Brazilian prevalence study. Int J Clin Pharm 2019; 41: 888–894, https://pubmed.ncbi.nlm.nih.gov/31093938/ [DOI] [PubMed] [Google Scholar]
- 25. Delouya S, Crosnier G, Lacombe J, et al. Pharmacist-led medication for pain in France: what population are we talking about? Results of the Optymed study. Presse Med 2019; 48: e273–e283, https://pubmed.ncbi.nlm.nih.gov/31734048/ [DOI] [PubMed] [Google Scholar]
- 26. Denisova LG, Denisova MN, Tyranovets S, et al. Popularity and reasons of Russian teenagers’ self-medication, 4 November 2021, https://www.jpsr.pharmainfo.in/Documents/Volumes/vol10Issue09/jpsr10091827.pdf
- 27. Dönmez S, Güngör K, Göv P. Knowledge, attitude and practice of self-medication with antibiotics among nursing students. Int J Pharmacol 2018; 14: 136–143. [Google Scholar]
- 28. Du Y, Knopf H. Self-medication among children and adolescents in Germany: results of the National Health Survey for Children and Adolescents (KiGGS). Br J Clin Pharmacol 2009; 68: 599–608, https://pubmed.ncbi.nlm.nih.gov/19843063/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fainzang S. The other side of medicalization: self-medicalization and self-medication. Cult Med Psych 2013; 37: 488–504, https://link.springer.com/article/10.1007/s11013-013-9330-2 [DOI] [PubMed] [Google Scholar]
- 30. Ferraz S, Grunewald T, Silva Rocha F, et al. Comportamento de uma amostra da população urbana de Juiz de Fora MG perante a automedicação, 2008, https://docplayer.com.br/49601601-Comportamento-de-uma-amostra-da-populacao-urbana-de-juiz-de-fora-mg-perante-a-automedicacao-re-s-u-m-o.html (accessed 4 November 2021).
- 31. Jain P. Statistical study on self medication pattern in Haryana, India, https://www.researchgate.net/publication/231292638_Statistical_Study_on_Self_Medication_Pattern_in_Haryana_India (accessed 4 November 2021).
- 32. Mahrous MS. Frequency of use of non-prescribed medication among population sample from Al Madina City and its impact on quality of care in Saudi Arabia. Int J Health Sci (Qassim) 2018; 12: 3–9. [PMC free article] [PubMed] [Google Scholar]
- 33. Mumtaz Y, Jahangeer A, Mujtaba T, et al. Self medication among University students of Karachi, https://www.lumhs.edu.pk/jlumhs/Vol10No03/pdfs/v10n3oa13.pdf (accessed 4 November 2021).
- 34. Napolitano F, Izzo M, di Giuseppe G, et al. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS ONE 2013; 8(12): e84177, https://pubmed.ncbi.nlm.nih.gov/24376793/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nunes de Melo M, Madureira B, Nunes Ferreira AP, et al. Prevalence of self-medication in rural areas of Portugal. Pharm World Sci 2006; 28: 19–25, https://link.springer.com/article/10.1007/s11096-005-2222-y [DOI] [PubMed] [Google Scholar]
- 36. Ouédraogo DD, Zabsonré Tiendrebeogo JW, Zongo E, et al. Prevalence and factors associated with self-medication in rheumatology in Sub-Saharan Africa. Euro J Rheumatol 2015; 2: 52–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Papakosta M. Investigating factors of self-care orientation and self-medication use in a Greek rural area. Rural Remote Health, 2014, https://pubmed.ncbi.nlm.nih.gov/24712873/ [PubMed]
- 38. Pereira C. Self-medication in health students from two Brazilian universities. RSBO, 2012, http://revodonto.bvsalud.org/scielo.php?script=sci_abstract&pid=S1984-56852012000400003&lng=pt&nrm=iso&tlng=en
- 39. Pochhi M, Agrawal JN, Gupta VK. Comparative analysis of practice of self medication among second year dental and nursing students, https://www.rjpbcs.com/pdf/2017_8(3)/[273].pdf
- 40. Sado E, Kassahun E, Bayisa G, et al. Epidemiology of self-medication with modern medicines among health care professionals in Nekemte town, western Ethiopia. BMC Res Notes 2017; 10: 1–5, https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-017-2865-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sarahroodi Maleki-Jamshid A, Sawalha AF, Mikaili P, et al. Pattern of self-medication with analgesics among Iranian University students in central Iran. J Fam Commun Med 2012; 19: 125, https://www.jfcmonline.com/article.asp?issn=2230-8229;year=2012;volume=19;issue=2;spage=125;epage=129;aulast=sarahroodi [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Urrunaga-Pastor D, Benites-Zapata VA, Mezones-Holguín E. Factors associated with self-medication in users of drugstores and pharmacies in Peru: an analysis of the National Survey on User Satisfaction of Health Services, ENSUSALUD 2015. F1000Res 2020; 8: 23, https://f1000research.com/articles/8-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Machado-Alba JE, Echeverri-Cataño LF, Londoño-Builes MJ, et al. Social, cultural and economic factors associated with self-medication. Biomedica 2014; 34: 580–588, http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-41572014000400011&lng=en&nrm=iso&tlng=en [DOI] [PubMed] [Google Scholar]
- 44. Hernandez-Juyol M, Job-Quesada J. Dentistry and self-medication: a current challenge, https://pubmed.ncbi.nlm.nih.gov/12415218/ (accessed 4 November 2021). [PubMed]
- 45. Shaghaghi A, Asadi M, Allahverdipour H. Predictors of self-medication behaviour: a systematic review, https://pubmed.ncbi.nlm.nih.gov/26060736/ (accessed 4 November 2021). [PMC free article] [PubMed]
- 46. Aldeeri A, Alzaid H, Alshunaiber R, et al. Patterns of self-medication behaviour for oral health problems among adults living in Riyadh, Saudi Arabia. Pharmacy (Basel) 2018; 6: 15, https://pubmed.ncbi.nlm.nih.gov/29389869/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ayub M. Prevalence and consequences associated with self medication in our society: a global issue. Int Res J Pharm 2015, www.jppcm.org (accessed 23 September 2021).
- 48. Beyene M, Worku Beza S. Self-medication practice and associated factors among pregnant women in Addis Ababa, Ethiopia. Trop Med Health 2018; 46: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Biudes M, Galato D. Self-medication in patients living with HIV/AIDS: little measured reality. Int J Pharm Sci Rev Res 2014; 22: 115–119. [Google Scholar]
- 50. Catrib M, Soares A, Holanda-Batista M, et al. Concepções e práticas sobre automedicação na escola profissionalizante: um estudo de caso no estado do Ceará, Brasil. Rev baiana saúde pública 2013; 37: 117–132. [Google Scholar]
- 51. da Rocha CE, Lessa FAS, Venceslau DO, et al. Development of a decision support system for the practice of responsible self-medication. Int J Clin Pharm 2015; 38: 152–161, https://link.springer.com/article/10.1007/s11096-015-0223-z [DOI] [PubMed] [Google Scholar]
- 52. Dias IM, Guedes LA, Cordeiro PC, et al. Self-medication in patients with temporomandibular disorders. Brazilian Dental Science 2014; 17: 82. [Google Scholar]
- 53. Gordon SM, Mosure DJ, Lewis J, et al. Prevalence of self-medication with antibiotics among patients attending a clinic for treatment of sexually transmitted diseases. Clin Infect Dis 1993; 17: 462–465, https://academic.oup.com/cid/article/17/3/462/363017 [DOI] [PubMed] [Google Scholar]
- 54. Jamshed S, Wong P, Yi H, et al. Self-medication practices among female students of higher educational institutions in Selangor, Malaysia: a quantitative insight. J Pharm Bioallied Sci 2016; 8: 217–222, https://pubmed.ncbi.nlm.nih.gov/27413350/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Jerez-Roig J, Medeiros LFB, Silva VAB, et al. Prevalence of self-medication and associated factors in an elderly population: a systematic review. Drugs Aging 2014; 31: 883–896, https://link.springer.com/article/10.1007/s40266-014-0217-x [DOI] [PubMed] [Google Scholar]
- 56. Karthik R, Gopalakrishnan S, Uma Devi D. Self-medication and its challenges: a review. Res J Pharm Biol Chem Sci 2015; 6: 388–392. [Google Scholar]
- 57. Klemenc-Ketis Z. The effect of demographic characteristics on self-medication patterns: a cross-sectional nationwide study from Slovenia. Coll Antropol 2011, https://pubmed.ncbi.nlm.nih.gov/22397266/ [PubMed]
- 58. Madhusudan M, Imran M, Mahadev Murthy TS. Self medication pattern among housewives in rural field practice area of MVJ MC & RH, Hoskote. Indian J Publ Heal Res Develop 2015; 6: 17–20. [Google Scholar]
- 59. Montastruc JL, Bondon-Guitton E, Abadie D, et al. Pharmacovigilance: risques et effets indésirables de l’automédication. Therapies 2016; 71: 249–255. [Google Scholar]
- 60. Mortazavi SS, Shati M, Khankeh HR, et al. Self-medication among the elderly in Iran: a content analysis study. BMC Geriatr 2017; 17: 198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Parihar A, Sharma D, Malhotra P. Questionnaire based assessment of knowledge attitude and practice of self medication among medical undergraduates of a medical college in North India, 2018, https://www.researchgate.Net/publication/329865550_Questionnaire_based_assessment_of_knowledge_attitude_and_practice_of_self_medication_among_medical_undergraduates_of_a_medical_college_in_North_India (accessed 5 November 2021).
- 62. Ruiz-Stenberg A, Perez-Acosta A. Automedicación y términos relacionados: una reflexión conceptual. Rev Cienc Salud 2011; 9: 83–97. [Google Scholar]
- 63. Srikanth Somashekara S, Hooli T. Self-medication of antibiotics among medical undergraduates in South India. Gulbarga, India: Department of Pharmacology, ESIC Medical College. [Google Scholar]
- 64. Gras M, Champel V, Masmoudi K, et al. Self-medication practices and their characteristics among French university students. Therapie 2020; 75, https://pubmed.ncbi.nlm.nih.gov/32204933/ [DOI] [PubMed] [Google Scholar]
- 65. Ateshim Y, Bereket B, Major F, et al. Prevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea: a descriptive cross sectional survey. BMC Public Health 2019; 19, https://pubmed.ncbi.nlm.nih.gov/31182071/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. World Health Organization. Guidelines for the regulatory assessment of medicinal products for use in self-medication. Geneva: World Health Organization, 2000. [Google Scholar]
- 67. Domingues PHF, Galvão TF, Andrade KRC, et al. Prevalência e fatores associados à automedicação em adultos no Distrito Federal: estudo transversal de base populacional. Epidemiologia e Serviços de Saúde 2017; 26: 319–330, http://www.scielo.br/j/ress/a/FD7s5rP6RwrhLqLVBThgGQR/?lang=pt [DOI] [PubMed] [Google Scholar]
- 68. el Ezz N, Ez-Elarab H. Knowledge, attitude and practice of medical students towards self medication at Ain Shams University, Egypt. J Prev Med Hyg 2011; 52: 196–200, https://pubmed.ncbi.nlm.nih.gov/22442925/ [PubMed] [Google Scholar]
- 69. Escalona C CE, Scarpeccio O RD, Quiñonez M B. Automedicación analgésica en pacientes que acuden al Servicio de Odontología del Hospital General Dr. Luis Razetti. Barinas estado Barinas, Venezuela. Revista del Instituto Nacional de Higiene ‘Rafael Rangel’ 2018; 48, http://saber.ucv.ve/ojs/index.php/rev_inhrr/article/view/15103 [Google Scholar]
- 70. Fidelis C, Kanmodi KK, Olajolumo J. Prevalence, sources and purpose of self-prescribed non-opioid analgesic among health professionals in Sokoto metropolis, Nigeria: a cause for concern. Curr Iss Pharm Med Sci 2018; 31: 13–17. [Google Scholar]
- 71. Jorgji K, Bebeci E, Apostoli P, et al. Evaluation of use of antibiotics without prescription among young adults in Albania case study: Tirana and Fier District. Hippokratia 2014; 18: 217–220, https://pubmed.ncbi.nlm.nih.gov/25694754/ [PMC free article] [PubMed] [Google Scholar]
- 72. Mansouri A, Sarayani A, Ashouri A, et al. Is ‘self-medication’ a useful term to retrieve related publications in the literature? A systematic exploration of related terms. PLoS ONE 2015; 10, https://pubmed.ncbi.nlm.nih.gov/25932634/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Markotic F, Vrdoljak D, Puljiz M, et al. Risk perception about medication sharing among patients: a focus group qualitative study on borrowing and lending of prescription analgesics. J Pain Res 2017; 10: 365–374, https://pubmed.ncbi.nlm.nih.gov/28243140/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Marquez GE, Torres VE, Sanchez VM, et al. Self-medication in ophthalmology: a questionnaire-based study in an Argentinean population. Ophthal Epidemiol 2012; 19: 236–241, https://www.tandfonline.com/doi/abs/10.3109/09286586.2012.689076 [DOI] [PubMed] [Google Scholar]
- 75. Ruiz ME. Risks of self-medication practices. Curr Drug Saf 2010; 5: 315–323, https://pubmed.ncbi.nlm.nih.gov/20615179/ [DOI] [PubMed] [Google Scholar]
- 76. Brata C, Gudka S, Schneider C, et al. A review of the provision of appropriate advice by pharmacy staff for self-medication in developing countries. Res Social Adm Pharm 2015; 11: 136–153, https://pubmed.ncbi.nlm.nih.gov/25139059/ [DOI] [PubMed] [Google Scholar]
- 77. Potts J. Developing a patient self-medication program for the rehabilitation setting. Rehabil Nurs 1994; 19: 344–347, https://pubmed.ncbi.nlm.nih.gov/7855401/ [DOI] [PubMed] [Google Scholar]
- 78. Hounsa A, Kouadio L, de Mol P. [Self-medication with antibiotics obtained from private pharmacies in Abidjan, Ivory Coast]. Medecine et maladies infectieuses 2010; 40: 333–340, https://pubmed.ncbi.nlm.nih.gov/19951830/ [DOI] [PubMed] [Google Scholar]
- 79. Caamaño Isorna F, Figueiras A, Lado Lema E, et al. La automedicación: concepto y perfil de sus ‘usuarios’. Gaceta Sanitaria 2000; 14: 294–299. [DOI] [PubMed] [Google Scholar]
- 80. Huffman MA. Primate self-medication, passive prevention and active treatment – a brief review. Int J Multidiscip Stud 2017; 3: 1, http://ijms.sljol.info/articles/10.4038/ijms.v3i2.1/ [Google Scholar]
- 81. Hardy K. Paleomedicine and the evolutionary context of medicinal plant use. Revista brasileira de farmacognosia: orgao oficial da Sociedade Brasileira de Farmacognosia 2020; 31, https://pubmed.ncbi.nlm.nih.gov/33071384/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ortiz M, Martinez-Jimenez B, Ramirez-Hernandez R, et al. Self-medication in Mexican pediatric patients. Iran J Public Health 2019; 48: 2293–2295, https://pubmed.ncbi.nlm.nih.gov/31993399/ [PMC free article] [PubMed] [Google Scholar]
- 83. Diniz P, Sousa M, Gerardi D, et al. Amphetamine poisoning in a dog: case report, literature review and veterinary medical perspectives. Vet Hum Toxicol 2003, https://pubmed.ncbi.nlm.nih.gov/14640484/ (accessed 9 November 2021). [PubMed]
- 84. Gasco A, Perez-Acosta A, Monticelli P. Ring-tailed coatis anointing with soap: a new variation of self-medication culture? Int J Comp Psychol 2016, https://escholarship.org/uc/item/1dq4s4p5 (accessed 9 November 2021).
- 85. Washington State Department of Health. Who can prescribe and administer prescriptions. Washington State Department of Health, https://www.doh.wa.gov/LicensesPermitsandCertificates/FacilitiesNewReneworUpdate/Pharmacy/WhoCanPrescribeandAdministerPrescriptions (accessed 9 November 2021). [Google Scholar]
- 86. WHO Guideline on Self-Care Interventions for Health and Well-Being. WHO guideline on self-care interventions for health and well-being, 2021, https://www.ncbi.nlm.nih.Gov/books/NBK572699/ (accessed 9 November 2021).
- 87. Singh J, Gautam C, Singh R. Self-medication with herbal remedies amongst patients of type 2 diabetes mellitus: a preliminary study. Indian J Endocrinol Metab 2012; 16: 662, https://pubmed.ncbi.nlm.nih.gov/22837942/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Eichhorn T, Greten HJ, Efferth T. Self-medication with nutritional supplements and herbal over-the-counter products. Nat Prod Bioprospec 2011; 1: 62–70, https://link.springer.com/article/10.1007/s13659-011-0029-1 [Google Scholar]
- 89. Nasir M, Mannan M, Chowdhury ASMS, et al. Prevalence, pattern and impact of self medication of anti-infective agents during COVID-19 outbreak in Dhaka City. Global J Med Res 2020; 1–8, https://medicalresearchjournal.org/index.php/GJMR/article/view/2260
- 90. Nasir M, Chowdhury ASMS, Zahan T. Self-medication during COVID-19 outbreak: a cross sectional online survey in Dhaka city. Int J Basic Clin Pharmacol 2020; 9: 1325–1330, https://www.ijbcp.com/index.php/ijbcp/article/view/4308 [Google Scholar]
- 91. Flower R. Lifestyle drugs: pharmacology and the social agenda. Trends Pharmacol Sci 2004; 25: 182–185, https://pubmed.ncbi.nlm.nih.gov/15063081/ [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-taw-10.1177_20420986221127501 for Definition of self-medication: a scoping review by Daniela Baracaldo-Santamaría, Maria José Trujillo-Moreno, Andrés M. Pérez-Acosta, John Edwin Feliciano-Alfonso, Carlos-Alberto Calderon-Ospina and Franklin Soler in Therapeutic Advances in Drug Safety
Supplemental material, sj-xlsx-2-taw-10.1177_20420986221127501 for Definition of self-medication: a scoping review by Daniela Baracaldo-Santamaría, Maria José Trujillo-Moreno, Andrés M. Pérez-Acosta, John Edwin Feliciano-Alfonso, Carlos-Alberto Calderon-Ospina and Franklin Soler in Therapeutic Advances in Drug Safety