Abstract
Objectives
This study used the Technology-Organization-Environment (TOE) framework to identify the factors involved in the decisions made by integrated medical and healthcare organizations to adopt artificial intelligence (AI) elderly care service resources.
Method
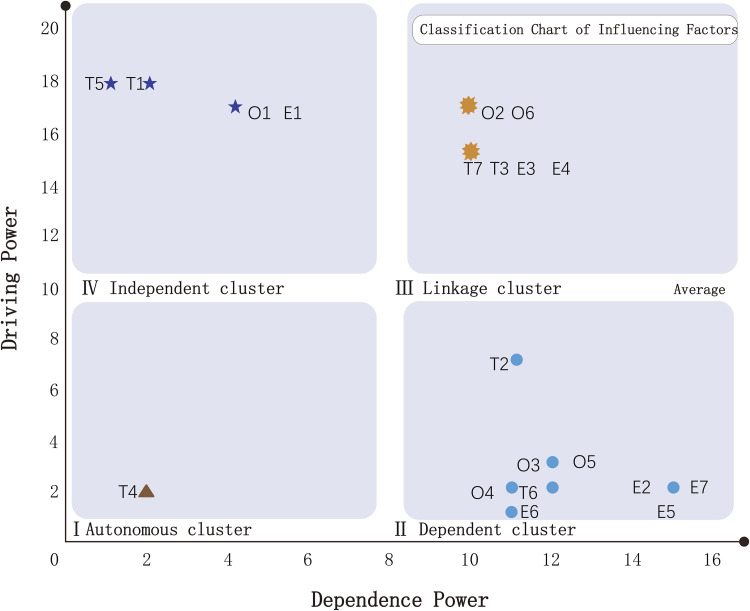
This study identified the Decision-making Trial and Evaluation Laboratory-Interpretive Structural Modeling (DEMATEL-ISM) method was used to construct a multilayer recursive structural model and to analyze the interrelationships between the levels. A MICMAC quadrant diagram was used for a cluster analysis.
Results
The ISM recursive structural model was divided into a total of seven layers. The bottom layer contained the four factors of High risk of data leakage (T1), Lack of awareness of the value and benefits of AI healthcare technology (T5), Lack of management leadership support (O1), and Government policies (E1). Having a low dependency but high driving force, these factors are the root causes of adoption by healthcare organizations. The topmost layer contained the most direct factors, which had a high dependency but the low driving force, influencing adoption: Competitive pressures (E2), Lack of patient trust (E5), and Lack of excellent partnerships (E7). Healthcare organizations are more concerned with technology and their environments when deciding to adopt intelligent healthcare resources.
Conclusion
The combination of the three methods of DEMATEL-ISM-MICMAC construction models provides new ideas for smart healthcare services for hospitals. The DEMATEL method favors the construction dimension of the micro-model, while the ISM method favors the construction dimension of the macro-model. Combining these two methods may reduce the loss of information within the system, simplify the matrix calculation workload, and improve the efficiency of operations while decomposing the complex problems into several sub-problems in a more comprehensive and detailed way. Conducting cluster analysis of the adoption determinants utilizing MICMAC quadrant diagrams may provide strong methodological guidance and decision-making recommendations for government departments, senior decision-makers in healthcare organizations, and policy-makers in associations in the senior care industry.
Keywords: Combination of medical and healthcare, medical institutions, healthcare, artificial intelligence adoption, DEMATEL, ISM, MICMAC
Introduction
In 1956, the United Nations defined the aging stage of a country or region as the time when the proportion of its population aged more than 65 years of age has exceeded 7% of its total population. 1 The 1982 Vienna World Assembly on Aging determined that a country or region was seriously aging if the proportion of people aged at least 60 years has exceeded 10% of the total population. 2 According to the results of China’s seventh census in May 2021, this proportion was 264.02 million people, which accounted for 18.70% of the total population. Of the elderly population, 190.64 million people or 13.50%, were aged 65 or above, indicating that the country’s population was significantly aging. The first two baby booms have led to a population with more than 260 million elderly people and the formation of a consumption plateau. As China’s aging population increases, the consumer power of people more than 50 years old will boom in the next 10–20 years and give rise to new industries, products, and services. The increasing number of solitary elderly people has led to an urgent demand for specialized elderly care services and an accompanying increase in the market potential of the institutions, equipment, and products required to provide such services.
Most elderly care institutions are entirely devoted either to medical or nursing care. Such a separation between these functions has failed to satisfactorily meet the needs of the elderly, who have formed rather poor impressions of such institutions. The elderly in China has poor impressions of the traditional elderly care institutions because of practices such as being constantly kept indoors in small spaces and in wheelchairs, as well as being abused by poorly trained caregivers. Moreover, faulty systems and laws have resulted in market transfers of the risks of the elderly’s survival onto the mandators of the institutions, thus strengthening the public’s poor perceptions. The disabled elderly, who make up most of the elderly population, are excluded from these institutions. The government’s lagging responses to the increased demand for elderly care resources have led to the blind expansion of medical resources and institutions by investing heavily in medical facilities and directing the public to concentrate on medical institutions, resulting in excessive financial burdens on the government and strains on medical resources while many beds in the elderly care institutions are vacant. The quality of life and care of the elderly has not significantly improved. In addition, the high prevalence of chronic diseases among the elderly and the fact that China is “aging before it gets rich” has also created tremendous social pressures. Therefore, exploring the cooperation between medical and elderly care institutions, as well as the establishment of the former within the latter, has become the focus of current efforts to solve the abovementioned problems.
Artificial intelligence healthcare service resources is considered to be the most promising type of intelligent healthcare service model at present and even in the future. The service model takes the hospital as the main body and connects multiple stakeholders such as patients, healthcare workers, pharmaceutical companies, and medical insurance institutions through information technology such as the Internet of Things and 5G communication technology, integrating upstream and downstream resources such as equipment, medical consumables, and pharmaceutical supplies in the hospital to provide various types of decision support services for doctors and patients.
The artificial intelligence healthcare service resources model being developed in China is mainly based on the smart hospital model, which is based on the construction of an electronic health record for the whole life cycle of the patient as the core, covering a series of whole-process closed-loop intelligent medical services such as consultation, triage, diagnosis, treatment, prevention and rehabilitation, etc., and incorporating big data analysis capabilities and artificial intelligence technology in every step of the service process. The model relies on resource integration and data service derivation to continuously enhance the service capability of hospitals and doctors. In contrast, in addition to the artificial intelligence healthcare service resources type for medical institutions, there is also a patient-oriented AI healthcare service resources model centered on patient services, with a resource integration-type platform as the main form of it is a one-stop health consultation and health management platform that connects the market flows between consultation services, drug distribution and medical and health insurance. The doctor-oriented AI healthcare service resources model is generally based on the hospital’s own information system and is based on the technological integration of doctor resources.
The artificial intelligence healthcare service resources model for medical institutions is mainly policy-oriented, with large medical institutions as the focus, and is a key investment and development model in China. In general, the construction of this type of intelligent healthcare service depends on a large amount of human, material and financial resources, and most hospitals lack the necessary resources to build this type of intelligent healthcare service, so the overall market adoption rate is not high. Examples include Vocera Digital Health Services and WellDoc Internet Hospital, which focuses on chronic disease management.
China’s medical institutions are in their initial stage and a spatial mismatch exists between the facilities of many medical institutions and the distribution of the elderly population. The lack of innovation in elderly care products, as well as the lack of quality products, has created a serious imbalance between supply and demand. Since 2015, the government has issued a few guidelines to promote the integration of intelligent medical and healthcare services to meet the diversified needs of the elderly groups while protecting their rights and interests. Moving away from a traditional elderly care service model to an intelligent integrated healthcare service model would help to match supply with demand more precisely and mobilize existing resources to improve the quality of life for the elderly. The transformation and upgrading of the traditional model to an innovative model of integrated intelligent medical and healthcare services are necessary for the rapid development of an intelligent and information-based society and for coping with an aging population. The combination of intelligent medical and elderly care models requires a medical insurance system with information sharing via the Internet to integrate high-quality resources, improve service efficiency and quality, produce more economic benefits, and expand the coverage of basic medical care.
The application of AI can help medical institutions to realize intelligent medical systems as soon as possible and formulate intelligent healthcare, such as hierarchical medical and healthcare, as well as digital rehabilitation treatments. Most of the current explorations in this field have focused on medical systems such as Mobile Nursing Information System (MNIS), Picture Archiving and Communication System (PACS), Clinical Information System (CIS), and Hospital Information System (HIS), whereas only a few scholars have paid attention to the adoption of intelligent healthcare and services. This study aimed to help overcome the barriers between elderly care businesses and other industries in order to realize the multilateral integration of medical and healthcare services that apply AI.
Any adoption of AI should include considerations of the hierarchies in medical institutions for the adoption of healthcare service resources. In 1990, Tornatzky et al. 3 proposed the Technology-Organization-Environment (TOE) framework for organizational-level decision-making adoption and explained three types of factors: technological, organizational, and environmental. Displayed in Figure 1, the basic TOE framework has been widely applied in both developed and developing countries to explain the development of innovative capabilities in many industries, such as manufacturing, 4 e-commerce,5–9 healthcare,10–14 and HIS adoption.10–12,14–17,7–9 According to this framework, healthcare organizations that adopt and implement AI technology innovations are influenced not only by the three relevant variables, but also by factors such as hospital sizes and financial costs.10,18,13,15 Technological factors include internal and external technologies, such as hospital information and data risks, electronic medical records, and medical source risks.10–12,14–16 The environmental factors include industrial competition, differences between urban and rural areas, and ownership attribution.13,19,16
Figure 1.
Basic Technology-Organization-Environment (TOE) framework.
The TOE framework can function as a complete system for the study of medical and healthcare issues but cannot be used to investigate the strengths of the relationships among the three influencing TOE factors, to distinguish between direct to indirect factors, or to derive logical connections between the influencing factors through stratification analysis. Therefore, this study applied the TOE framework to investigate the factors influencing the adoption of intelligent healthcare service resources in integrated healthcare institutions, used the Decision-making Trial and Evaluation Laboratory (DEMATEL) method to analyze the strengths of the interrelationships between the factors, and employed Interpretive Structural Modeling (ISM) to stratify the factors from bottom to top and from shallow to deep in order to derive the logical linkages between the factors and construct the models for adoption by intelligent healthcare institutions.
This study addressed the following questions: (1) What are the most important factors that influence the adoption of AI resources for wellness services in integrated healthcare organizations? (2) What are the logical connections and the different strengths of the interrelationships among the technological, organizational, and environmental factors in the TOE framework? (3) How to explain the logical sequences between the factors? This study aimed to apply the perspective of the TOE framework in order to establish that institutions with the integration of intelligent medical and healthcare services are the parties in cooperation agreements that have priority in the choice of personnel, materials, and information. The internal operating mechanism for decision-making on adopting AI healthcare service resources in technological, organizational, and environmental factors reveals the internal logical relationships in the decision-making process of the organizational behavior of medical institutions in the context of the integration of intelligent medical and healthcare services. This study can provide a solid, practical basis for coordinating the interests between hospitals and elderly care institutions, as well as fully utilizing resources, providing practical guidance to the providers of AI healthcare service resources, the management departments in hospitals, cooperation departments in elderly care institutions, and governmental departments for elderly-care policies. In this way, the added value and popularity of medical institutions will be improved, thereby encouraging elderly care institutions to improve their nursing, promoting the recognition of AI medical services by medical institutions and elderly care institutions, encouraging more elderly patients to go to medical institutions with integrated medical and healthcare services to seek medical advice, and providing a solid foundation for the government’s promotion of healthcare services through medical services.
This paper demonstrates the following six steps of the study. In the first step, the author summarized the research on hospital adoption of smart healthcare services, and summarized the determinants for scholars to identify the hospital adoption of smart healthcare services under the Technology-Organization-Environment (TOE) Framework. In the second step, by sorting the a forementioned determinants, the author screened the most frequently mentioned determinants by scholars under the TOE framework as variables of the questionnaires for the authoritative experts in the AI healthcare field to conduct pre-tests. Twenty determinants most closely related to the adoption of AI healthcare services in hospitals were screened. In the third step, the influencing determinants were screened according to the pre-test results of questionnaires administered to 10 experts and 20 influencing factors were identified according to the TOE framework. Then, the formal questionnaire was administered to the experts, who scored the 20 factors from 0 to 4 to form the direct influence matrix, and the macro-level analysis of the influencing factors of the adoption of regimen services was conducted by the DEMATEL method to analyze the degrees of influence, being influenced, and centrality. In the fourth step, the recursive structural model was established by the ISM method to intuitively explain the hierarchical relationships and directionality of the influencing factors, which are the root of the structure. In the fifth step, the MICMAC graphical method was used to cluster and summarize the factors in order to explain the deeper substance of the structure. In the sixth step, based on the a forementioned research findings, the author proposed relevant countermeasures and suggestions according to the development status of smart medical services to promote the development and proliferation of smart medical regimen services from the dimension of government, regimen institution managers and associations in the senior care industry.
Factors influencing adoption of AI healthcare resources
The adoption of intelligent healthcare service resources in medical and healthcare institutions is a multi-attribute, multi-factor decision-making process that is influenced by variables at different levels. First, the construction of medical IT is a long process and China’s medical institutions are still in the initial stages of their establishment. Each stage should be woven into a larger network to effectively implement health and medical care systems, as well as to solve the core medical problems. Second, medical workers go through years of professional training before facing patients. Medical industrial scenarios combined with AI are variable and complex while medical professionals face lengthy and complicated medical information every day, resulting in duplication of work, low efficiency, and constant prominent conflicts between doctors and their patients.
Intelligent medical service resources have industry characteristics, such as strong specialization, high precision, and high risk, that require hospitals to provide large number of intelligent, professional, and technological engineers to assist medical workers. Also, intelligent medical and healthcare services must go through years of clinical trials and strict evidence-based processes, 20 government agencies lack the human and material resources to regulate intelligent medical service resources, 21 and legal departments have not introduced strict regulations and policies for intelligent medical services, 10 thus causing most hospitals to worry about the generation of medical risks, intensifying doctor–patient conflicts, and strengthening resistance to the adoption of AI into healthcare service resources. Few studies have been conducted on the adoption of AI into medical and health services. We examined the literature on the factors influencing the adoption of intelligent healthcare services by medical institutions and the characteristics of AI, then summarized our findings in Table 1, which names the scholars who have applied the TOE framework to investigate the adoption of combined Healthcare + AI + Healthcare resources + Health Regimens. Social surveys, questionnaires, and group interviews are the main data sources while factor, multiple regression, cluster, and survival analyses are the main research methods.
Table 1.
Factors influencing the adoption of intelligent healthcare services by medical institutions with integrated medical care.
| Author | Country/region of data collection | Methods/models | Factors | Type of research (qualitative or quantitative) | Qualitative | Quantitative | ||
|---|---|---|---|---|---|---|---|---|
| Number of cases | Methods for data collection | Sample size | Methods for data collection | |||||
| Wang et al. 22 | USA | Multiple regression analysis. Cross-sectional analysis. Multiple regression. Cross-sectional analysis. TOE framework |
Inaccurate forecasting of market trends. High risk of data leakage. Communication channels. Managed care pressures. Competition and community needs. Financial factors. |
Quantitative | 1441 | Survey | ||
| Zheng et al. 23 | USA | Social network analysis | Gender. Medical risks. Skepticism about AI processing power. Computer experience. Computer knowledge Computer optimism. Perceived usefulness of intelligent systems and their ease of use. | Quantitative | 55 | Survey | ||
| Callaway 24 | USA | Logit regression. Survival analysis. |
Economic benefits. Financial costs. Skepticism about AI processing capabilities. Patient access perceptions. |
Quantitative | 5082 | Survey | ||
| Lian et al. 25 | China | Regression analysis. ANOVA. TOE framework. IOR framework. |
Perceived usefulness. High risk of data leakage. System service
complexity. AI infrastructure synergy. Costs. Relative advantages. Leadership management support. Inability to share information. Economic benefits. Government policies. Perceived competitive pressures. |
Quantitative | 60 | Questionnaire | ||
| Chang et al. 10 | China | Regression analysis. TOE framework. |
User participation. Inability to share information. Hospital size. Difficulty in meeting complex needs of elderly patients. Lack of excellent vendor support. Government policies. Security protection. Complexity of system services. | Quantitative | 53 | Questionnaire | ||
| Chong and Chan 18 | Malaysia | Structural equation model. TOE framework. |
Relative advantages. AI infrastructure synergy. System service complexity. Financial costs. High risk of data breaches. Leadership management support. Organization size. Economics. Lack of awareness of value and benefits of healthcare + AI technology. Competitive pressures. Inaccurate forecasting of market trends. | Quantitative | 182 | Questionnaire | ||
| Liu 26 | China | Regression analysis. TOE framework. |
AI infrastructure synergy. Relative strengths. Lack of excellent vendor support. Leadership management support. Lack of awareness of value and benefit of healthcare + AI technology. Internal needs. Government support. Competitive business pressures. | Quantitative | 70 | Questionnaire | ||
| Kazley and Ozcan 13 | USA | One-way ANOVA. Logistic regression. TOE framework. | Competitiveness. Geographical tolerance. Lack of awareness of value and advantages of AI medical technology. Hospital size. System integration. Health insurance payments. Financial support. Training support. |
Quantitative | 4606 | Survey | ||
| Lin et al. 15 | China | Factor analysis. Logistic regression. Pearson chi-square test. | Hospital size. High risk of data leakage. System integration. Lack of complex talent. Leadership management support. Competitive environment. Inaccurate forecasting of market trends. | Quantitative | 119 | Questionnaire | ||
| Hung et al. 27 | China | Factor analysis. Regression analysis. | Hospital size. Lack of complex talent. Leadership management support. Knowledge management capabilities. Relative strengths. System service complexity. | Quantitative | 97 | Questionnaire | ||
| Ahmadi et al. 28 | Malaysia | DEMATEL. ANP. AHP. TOE framework. | Relative advantages. AI infrastructure synergy. System service complexity. System integration. Government policy. Hospital size. High risk of data breaches. Leadership management support. Competitive environment. Lack of excellent vendor support. | Quantitative | 12 | Questionnaire | ||
| Greenberg et al. 29 | Israel | Expert interview. VIKOR method. | Financial costs. Efficiency improvements. Policy support. Reputation contributions. Profitability improvements. Leadership management support. Industry pressures. Employee training. | Qualitative | 26 hospitals, 132 hospital executives | Interviews | ||
| Asagbra et al. 30 | USA | OLS regression. Multivariate analysis. TOE framework. | Lack of patient trust. Health insurance support. Geographic tolerance. Complexity of system services. Hospital size. System integration. Lack of clarity of hospital ownership. Training support. | Quantitative | 4176 | Survey | ||
| Young et al. 31 | USA | Cox proportional hazards model. | Leadership management support. System service complexity. Hospital size. | Quantitative | 150 | Survey | ||
| Chen et al. 32 | China | Factor analysis. Regression analysis. | Hospital climate. Hospital size. Inability to share information. Internal needs. Leadership management support. Staff attitudes. Skepticism about AI processing capabilities. Healthcare policies. Lack of excellent vendor support. High risk of data leakage. Lack of patient trust. | Quantitative | 227 | Questionnaire | ||
| Alam et al. 33 | Bangladesh | Regression analysis. ANOVA analysis. TOE framework. | IT infrastructure. AI infrastructure synergy. Complexity. Relative strengths. Management leadership support. Unclear hospital ownership. Formalization. Perceived costs. Competitive pressures. Lack of excellent vendor support. Government policy and support. Skeptical of AI processing capabilities. Ability to lead innovation. | Quantitative | 383 | Questionnaire | ||
| Lee et al. 4 | South Korea | Multivariable analyses. Structural equation model. | Provider performance projections. Provider effort expectations. Provider attitudes. Social influence. Lack of excellent provider support. | Quantitative | 383 | Survey | ||
| Yang et al. 16 | USA | Expert interviews. TOE framework. | Lack of excellent vendor support. Relative advantages. AI infrastructure synergy. Complexity. Hospital type. Unclear hospital ownership. Hospital size. Internal needs. Inability to share information. Uncertain technological knowledge. Knowledge management capabilities. Lack of qualified teamwork capabilities. Leadership management support. Government policy support. Lack of excellent partner relationships. Competitive market pressures. National guarantees. | Qualitative | 24 | Interviews | ||
| Tsagaankhuu et al. 19 | Mongolia | Negative binomial regression. Multiple regression. | Hospital size. Number of beds. Training support. Geographic location. Unclear ownership affiliation. HMO penetration. | Quantitative | 78 | Questionnaire | ||
| Fan et al. 34 | China | Regression analysis. Case study. | Trust orientation. Social influence. Perceived substitution crisis. Job expectations. | Quantitative | 191 | Questionnaire | ||
| Hoque 35 | Bangladesh | Structural equation model. Regression analysis. | Perceived usefulness and ease of use. Subjective norms. | Quantitative | 234 | Questionnaire | ||
| Wu 36 | China | Structural equation model. Regression analysis. | Perceived service availability. Skeptical of AI processing capabilities. Perceived usefulness and ease of use. Hospital size. Lack of excellent supplier support. | Quantitative | 140 | Questionnaire | ||
| Kijsanayotin et al. 37 | Thailand | Structural equation model. Regression analysis. | Performance and effort expectations. Social impact. Employees’ computer processing capabilities. Facilitation. | Quantitative | 1323 | Questionnaire | ||
| Faber et al. 38 | Netherlands | Structural equation model. Regression analysis. | Hospital size. Number of beds, Leadership management support. IT infrastructure, human resources, government support, and security. Financial foundation. Centralization of decisionmaking. Lack of complex talent. | Quantitative | 58 | Questionnaire | ||
| Tortorella et al.39,40 | Brazil | Cluster analysis. ANOVA. Multivariate analysis. | Regulatory changes. IT infrastructure. Working against hospitals’ strategies. High risk of data breaches. Implementation costs. Lack of technological knowledge, qualified teamwork skills, and excellent partner relationships. | Quantitative | 159 | Questionnaire | ||
| Sun and Medaglia 41 | China | Expert interviews. Multi-attribute decision-making. | Perceived usefulness of intelligent systems. High costs and meager profits for hospitals. High risk of data leakage. Misconceptions and lack of awareness of value and advantages of AI medical technology. Lack of innovation. Lack of ability to read structured medical data. Skepticism of AI processing capabilities | Qualitative | 17 | Interviews | ||
| Mardani et al. 42 | Vietnam | Expert interviews. Multi- attribute decision-making. | High risk of data breaches. Skepticism about AI processing capabilities. Low-security programing. Lack of awareness of value and benefits of AI healthcare technology. Training support. Medical source risks. Unaffordable costs. | Qualitative | 24 | Interviews | ||
| Xing et al. 43 | China | Thematic analysis. Focus group. | Difficulty maintaining stability in device performance. Lack of complex talent. Skepticism about AI processing capabilities. Lack of management leadership support, qualified teamwork, and clinical value. Fear of changes in clinical workloads. Imbalances of costs and expenses. Lack of sustainable business models and government policies. High risk of data breaches. Lack of patient trust. Difficulty meeting complex needs of older patients | Qualitative | 38 | Interviews | ||
For more detailed classifications of the above influencing factors in the TOE framework and the frequencies of their occurrences, Table 2 shows the statistics of the factors in the Technological, Organizational, and Environmental Dimensions. The Technological Dimension contains 11 factors (frequency of occurrence in parentheses): High risk of data leakage (12), System service complexity (9), Skeptical of AI processing capabilities (8), Perceived usefulness of intelligent systems (7), AI infrastructure synergy (6), Lack of awareness of value and benefits of AI healthcare technology (6), System integration (5), IT infrastructure (4), Perceived ease of use of AI (3), Medically derived risks (3), and Lack of ability to read structured medical data (2).
Table 2.
Statistics on factors influencing adoption of intelligent healthcare services according to Technology-Organization-Environment (TOE) framework.
| Dimensions & factors | Wang et al. 22 | Zheng et al. 23 | Callaway 24 | Lian et al. 25 | Chang et al. 10 | Chong and Chan 18 | Liu 26 | Kazley and Ozcan 13 | Lin 15 | Hung et al. 27 | Ahmadi et al. 28 | Greenberg et al. 29 | Asagbra et al. 30 | Young et al. 31 | Chen et al. 32 | Alam et al. 33 | Lee et al. 4 | Yang et al. 16 | Tsagaankhuu et al. 19 | Fan et al. 34 | Hoque 35 | Wu et al. 36 | Kijsanayotin et al. 37 | Faber et al. 38 | Tortorella et al. 39 | Tortorella et al. 40 | Sun and Medaglia 41 | Mardani et al. 42 | Xing et al. 43 | Frequency |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Technological | ||||||||||||||||||||||||||||||
| High risk of data leakage | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 12 | |||||||||||||||||
| System service complexity | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 9 | ||||||||||||||||||||
| Skeptical of AI processing capabilities | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 8 | |||||||||||||||||||||
| Perceived usefulness of intelligent systems | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | ||||||||||||||||||||||
| Lack of awareness of value and benefits of AI healthcare technology | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | |||||||||||||||||||||||
| AI infrastructure synergy | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | |||||||||||||||||||||||
| System integration | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | ||||||||||||||||||||||||
| IT infrastructure | ✓ | ✓ | ✓ | ✓ | 4 | |||||||||||||||||||||||||
| Perceived ease of use of AI | ✓ | ✓ | ✓ | 3 | ||||||||||||||||||||||||||
| Medically derived risks | ✓ | ✓ | ✓ | 3 | ||||||||||||||||||||||||||
| Lack of ability to read structured medical data | ✓ | ✓ | 2 | |||||||||||||||||||||||||||
| Organizational | ||||||||||||||||||||||||||||||
| Lack of management leadership support | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 14 | |||||||||||||||
| Hospital size | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 13 | ||||||||||||||||
| Financial costs | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 11 | ||||||||||||||||||
| Lack of excellent supplier support | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 8 | |||||||||||||||||||||
| Relative advantages | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | ||||||||||||||||||||||
| Economic benefits | ✓ | ✓ | ✓ | ✓ | 4 | |||||||||||||||||||||||||
| Training support | ✓ | ✓ | ✓ | ✓ | 4 | |||||||||||||||||||||||||
| Inability to share information | ✓ | ✓ | ✓ | ✓ | 4 | |||||||||||||||||||||||||
| Lack of complex talent | ✓ | ✓ | ✓ | ✓ | 4 | |||||||||||||||||||||||||
| Medical insurance payments | ✓ | ✓ | 2 | |||||||||||||||||||||||||||
| Environmental | ||||||||||||||||||||||||||||||
| Government policies | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 10 | |||||||||||||||||||
| Competitive pressures | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 10 | |||||||||||||||||||
| Unclear ownership of hospitals | ✓ | ✓ | ✓ | ✓ | 4 | |||||||||||||||||||||||||
| Lack of patient trust | ✓ | ✓ | ✓ | ✓ | 4 | |||||||||||||||||||||||||
| Inaccurate forecasting of market trends | ✓ | ✓ | ✓ | ✓ | 4 | |||||||||||||||||||||||||
| Lack of qualified teamwork | ✓ | ✓ | ✓ | ✓ | 4 | |||||||||||||||||||||||||
| Geographical restrictions | ✓ | ✓ | ✓ | 3 | ||||||||||||||||||||||||||
| Lack of excellent partnerships | ✓ | ✓ | ✓ | 3 | ||||||||||||||||||||||||||
| Difficult to meet complex needs of elderly patients | ✓ | ✓ | 2 | |||||||||||||||||||||||||||
| Hospital size | ✓ | ✓ | 2 | |||||||||||||||||||||||||||
| Community needs | ✓ | 1 |
The Organizational Dimension contains 10 factors (frequency of occurrence in parentheses): Lack of management leadership support (14), Hospital size (13), Financial costs (11), Lack of excellent supplier support (8), Relative advantages (7), Economic benefits (4), Training support (4), Inability to share information (4), Lack of complex talent (4), and Medical insurance payments (2).
The Environmental Dimension contains 11 factors (frequency of occurrence in parentheses): Government policies (10), Competitive pressures (10), Unclear ownership of hospitals (4), Lack of patient trust (4), Inaccurate forecasting of market trends (4), Lack of qualified teamwork skills (4), Geographic restrictions (3), Lack of excellent partnerships (3), Difficulty meeting the complex needs of elderly patients (2), Hospital size (2), and Community needs (2).
To ensure a rigorous model by pre-testing the influencing factors, this study invited ten experts who have worked in medical and health care institutions in Hefei, Anhui Province. Some have worked at large tertiary hospitals, while others have been directors of geriatric departments and have been engaged in medical care, nursing, rehabilitation, and healthcare for the elderly for more than 15 years, so they have an excellent grasp of the needs of the elderly. Some have also been managers in hospital management and have been specifically responsible for hospital development and information construction. They have been in contact with the AI medical service industry and have in-depth thoughts on Artificial Intelligence +Health Regimen. Their responses are summarized in Table 3. Those who have been imaging doctors usually have had the earliest and most frequent contact with AI medical services because they have worked closely with medical technology, so they have witnessed the development of the intelligent medical service industry, as well as have had more experience in operating intelligent equipment and using intelligent medical services.
Table 3.
Details of experts.
| Name of expert | Medical and health facility | Department | Length of service | Familiarity with intelligent health services |
|---|---|---|---|---|
| Dean Ning | Tertiary care hospital | Senior hospital leadership | 30 years | Very familiar |
| Dean Ni | Tertiary care hospital | Chief of Geriatrics | 25 years | Familiar |
| Chief Zhang | Tertiary care hospital | Chief of Geriatrics | 28 years | More familiar |
| Chief Gao | Tertiary care hospital | Director of Medical Imaging | 30 years | Very familiar |
| Dean Wang | Tertiary care hospital | Senior hospital leadership | 30 years | Very familiar |
| Chief Ding | Tertiary care hospital | Director of Geriatric Cardiovascular Medicine | 25 years | Very familiar |
| Dean Zhao | Secondary general hospital | Nursing Home Director | 30 years | Very familiar |
| Dean Sun | Secondary general hospital | Nursing Home Director | 26 years | Familiar |
| Dean Zhang | Secondary general hospital | Nursing Home Director | 30 years | More familiar |
| Dean Shi | Secondary general hospital | Head of Finance Department | 20 years | Familiar |
Another panel of experts were managers of large combinations of medical and healthcare institutions, of which the common feature was close cooperation with hospitals. With the help of social ties, these institutions have signed market contracts or co-build agreements with hospitals to establish integrated medical and healthcare services in order to make reasonable use of each other’s resources, as well as optimize the allocation of capital. The experts in this type of elderly care institution have always been coordinated with hospitals. Their philosophies of elderly care and attitudes toward intelligent medical services have been similar to those of the hospital experts. Thus, both the experts from hospitals and nursing homes have been closely integrated and have had many years of contact experience with the AI medical industry, so they were better able to make accurate assessments for this questionnaire.
The 10 experts were asked to tick the importance of the 32 factors and, as a sign of respect for the experts completing the questionnaire, each expert who did so received a USB stick as a gift. The 7-point Likert Scale was used to assign values from 1 to 7 on a scale ranging from unimportant to very important. The 7-point Likert Scale consisted of “strongly disagree,” “rather disagree,” “disagree,” “average,” “rather agree,” “agree,” and “strongly agree” on a scale of 1 to 7 respectively.
Next, the results of the 10 questionnaires collected were entered into excel software and the scores for each factor were added up and divided by 10 to obtain the average score for that factor. As the average score on a scale of 1-7 is 4, the average score after expert scoring in this paper was greater than 4 as the final factor selected for this paper, while factors below 4 were eliminated.
In accordance with the results of these ten experts’ pre-tests, a total of 20 influencing factors most closely related to the adoption of intelligent health service resources in medical and healthcare institutions were screened out. Table 4 explains these factors in more detail.
Table 4.
Factors influencing adoption of intelligent health services by healthcare providers according to TOE framework and results of experts’ pre-tests.
| Dimensions | Factors | Coding |
|---|---|---|
| Technological | High risk of data leakage | T1 |
| System service complexity | T2 | |
| AI infrastructure synergy | T3 | |
| Skeptical of AI processing capabilities | T4 | |
| Lack of awareness of value and benefits of AI healthcare technology | T5 | |
| Medically derived risks | T6 | |
| Lack of ability to read structured medical data | T7 | |
| Organizational | Lack of management leadership support | O1 |
| Hospital size | O2 | |
| Financial costs | O3 | |
| Lack of excellent supplier support | O4 | |
| Inability to share information | O5 | |
| Lack of complex talent | O6 | |
| Environmental | Government policies | E1 |
| Competitive pressures | E2 | |
| Geographical restrictions | E3 | |
| Unclear ownership of hospitals | E4 | |
| Lack of patient trust | E5 | |
| Difficult to meet complex needs of elderly patients | E6 | |
| Lack of excellent partnerships | E7 |
The results of the pre-testing by the abovementioned ten experts revealed the important factors influencing the adoption of AI medical service resources by medical and healthcare institutions under the combined medical and health care model, but many studies have not substantially explored the interrelationships between the influencing factors and their intensity, to which our study has applied the TOE framework and DEMATEL method for further analysis.
Methodology
DEMATEL-ISM method
At the Geneva Conference in 1971, Gabus and Fontela, scholars from the Battelle Laboratory in the United State, proposed the DEMATEL method as a type of system analysis for solving complex problems by graph theory and matrix tools using directed graphs with weights. 44 The logical relationships between the factors in a system are used to formulate a direct influence matrix for calculating the degree of the influence of each factor and its degree of being influenced in order to calculate each factor’s degrees of centrality and causality, which are used to judge the connections between the factors, as well as to evaluate their strengths and weaknesses. This method is effective, especially for systems in which the relationships between the elements are uncertain. Its six main steps are as follows.
Determine the system’s influencing factors, which are designated by S1, S2–Sn.
Investigate and summarize the problem, determine the logical interrelationships between the influencing factors, and establish the direct influence matrix ( ) by using a Likert five-point scale to indicate the degree of the direct influence of factor on factor : no (0), very weak (1), weak (2), strong (3), and very strong (4) influence.
- The normalization directly affects matrix . The rows of are summed and the summed values are set to maximum thus:
Calculate the comprehensive influence matrix , where is the unitary array.
- Calculate the degrees of influence and being influenced for each factor by summing the elements of matrix by row and column, respectively:
- Calculate the degrees of the centrality and causality of each factor by adding its influence and influenced degrees together to obtain the former, but subtracting the influenced from the influence degree to obtain the latter:
Proposed by Warfield 45 in 1974, ISM is a widely used analytical method in modern systems engineering and management science. The method is divided into the following steps:
Step 1: Identify the main factors of the problem and determine the direct influences of the interrelationships between adjacent elements by means of a box plot.
Step 2: Identify the transferability of logical relationships such as cause and effect to create Boolean (reachable) matrices that reflect these relationships.
Step 3: Construct a reduced matrix of reachable matrices by considering possible strong linkages between elements and retaining only the representative elements.
Step 4: Conduct a hierarchical treatment of the reduction matrix.
Step 5: Draw multilevel, recursive, and directed graphs.
Step 6: Formulate the model after direct conversion.
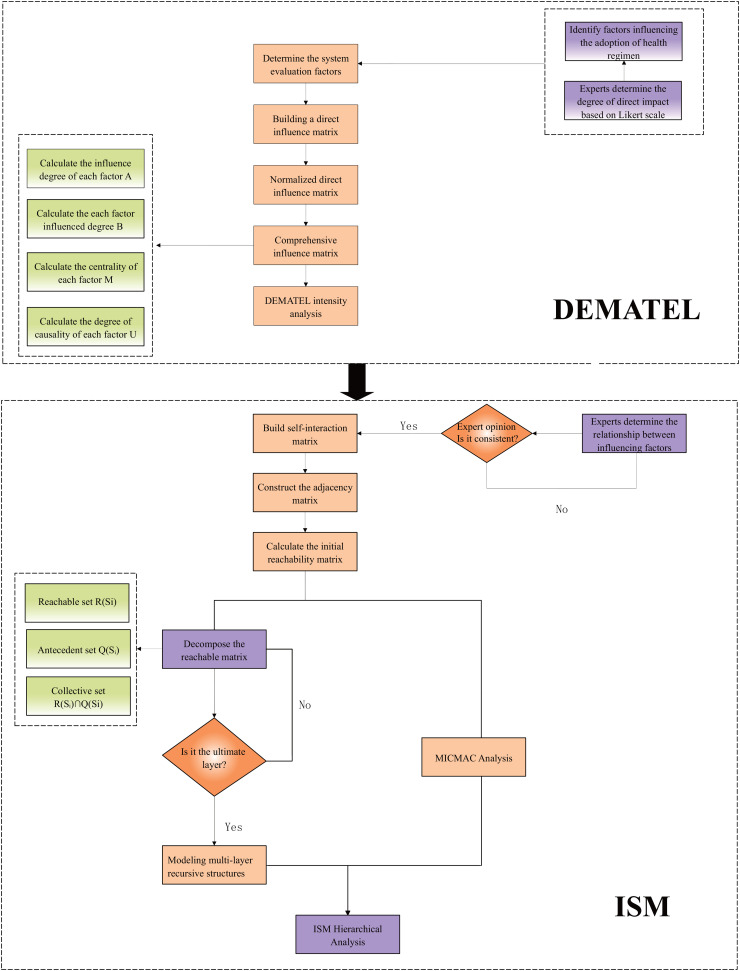
The DEMATEL method combined with ISM has developed rapidly in the past 5 years, mainly because scholars have found that each method could compensate for the other’s shortcomings in the following ways. First, the DEMATEL method is a micro-level, so it can explain more intuitively the strengths of the interrelationships between direct and indirect influences to provide a clearer indication of the importance of each factor in the system. Second, the ISM method is a macro-level, so it focuses on explaining the hierarchical relationships of each influencing factor, constructing diagrams of these relationships, analyzing the interrelationships between each hierarchical relationship, and dividing a complex problem into sub-problems. Third, the combined DEMATEL-ISM method, as shown in Figure 2, simplifies the computational steps while verifying the stability of the influencing factors. Other scholars usually cite thresholds, which are usually empirical values, to reduce the workload of the matrix computation.46–49 The introduction of such thresholds may bias the structural model, so this study used expert opinion for scoring as the data source.
Figure 2.
Decision-making Trial and Evaluation Laboratory-Interpretive Structural Modeling (DEMATEL-ISM) flowchart.
DEMATEL procedure
Step 1: The influencing factors are scored (from 0 for no influence to 4 for very strong influence) by distributing a questionnaire to 10 experts. The arithmetic mean of each value is calculated according to the following operational rules to establish the direct influence matrix, as shown in Table 5:
Table 5.
Direct influence matrix.
| T1 | T2 | T3 | T4 | T5 | T6 | T7 | O1 | O2 | O3 | O4 | O5 | O6 | E1 | E2 | E3 | E4 | E5 | E6 | E7 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | 0.0 | 3.7 | 1.5 | 3.5 | 0.8 | 3.9 | 0.4 | 0.0 | 0.0 | 4.0 | 0.0 | 3.4 | 0.0 | 3.6 | 0.4 | 0.0 | 0.0 | 4.0 | 1.4 | 0.0 |
| T2 | 1.2 | 0.0 | 1.7 | 3.6 | 4.0 | 3.6 | 0.7 | 0.0 | 0.0 | 3.9 | 3.6 | 3.5 | 0.0 | 0.1 | 0.7 | 0.0 | 0.0 | 3.6 | 3.6 | 0.8 |
| T3 | 0.0 | 0.4 | 0.0 | 3.3 | 0.7 | 3.5 | 0.1 | 0.0 | 3.7 | 3.7 | 3.2 | 3.7 | 0.0 | 3.6 | 3.0 | 0.0 | 0.0 | 3.4 | 3.7 | 0.5 |
| T4 | 0.0 | 0.4 | 0.0 | 0.0 | 3.6 | 3.3 | 0.2 | 0.0 | 0.0 | 3.6 | 0.0 | 3.5 | 0.0 | 0.1 | 0.6 | 3.5 | 3.6 | 4.0 | 3.8 | 0.0 |
| T5 | 3.4 | 0.0 | 0.0 | 3.6 | 0.0 | 3.6 | 0.1 | 0.0 | 3.3 | 3.7 | 0.2 | 3.5 | 0.0 | 3.4 | 0.4 | 0.0 | 0.6 | 3.7 | 3.5 | 0.6 |
| T6 | 0.7 | 0.0 | 0.0 | 3.8 | 0.0 | 0.0 | 0.6 | 0.0 | 0.0 | 1.7 | 0.3 | 3.4 | 0.0 | 3.6 | 0.6 | 1.3 | 3.7 | 3.6 | 3.6 | 0.0 |
| T7 | 0.8 | 0.0 | 0.0 | 3.4 | 3.5 | 3.8 | 0.0 | 0.0 | 3.7 | 3.8 | 0.1 | 3.5 | 0.4 | 0.4 | 0.3 | 1.5 | 0.6 | 3.8 | 3.9 | 3.0 |
| O1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.5 | 0.0 | 0.0 | 3.3 | 0.5 | 3.7 | 1.5 | 0.0 | 0.3 | 0.0 | 3.6 | 3.5 | 0.8 | 0.0 | 3.6 |
| O2 | 0.6 | 1.7 | 0.0 | 0.0 | 0.0 | 0.4 | 0.0 | 0.0 | 0.0 | 3.6 | 0.4 | 4.0 | 3.2 | 0.4 | 3.9 | 2.4 | 3.6 | 0.0 | 3.7 | 3.4 |
| O3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.6 | 3.5 | 2.8 | 0.0 | 3.8 | 0.2 | 3.4 | 0.3 | 0.7 | 2.6 | 3.3 | 0.0 | 2.6 | 3.3 |
| O4 | 0.4 | 3.8 | 0.0 | 0.6 | 0.0 | 1.4 | 0.5 | 0.0 | 2.5 | 0.0 | 0.0 | 4.0 | 3.6 | 0.8 | 3.4 | 0.0 | 4.0 | 3.7 | 3.7 | 3.6 |
| O5 | 0.0 | 3.5 | 3.4 | 1.7 | 2.4 | 2.5 | 0.4 | 3.5 | 2.3 | 0.0 | 3.6 | 0.0 | 0.0 | 0.1 | 3.5 | 0.0 | 0.4 | 4.0 | 3.6 | 3.1 |
| O6 | 1.5 | 1.4 | 3.4 | 1.4 | 3.7 | 3.6 | 3.6 | 0.4 | 2.7 | 0.0 | 3.5 | 3.5 | 0.0 | 0.6 | 3.7 | 0.0 | 0.4 | 0.6 | 3.5 | 2.5 |
| E1 | 0.5 | 0.0 | 3.6 | 0.4 | 0.0 | 0.0 | 0.0 | 3.5 | 3.6 | 3.5 | 0.6 | 3.5 | 0.0 | 0.0 | 3.4 | 3.9 | 1.7 | 0.7 | 0.7 | 3.9 |
| E2 | 0.0 | 0.0 | 0.0 | 0.6 | 0.0 | 0.0 | 0.0 | 0.0 | 0.4 | 0.0 | 0.6 | 3.5 | 0.0 | 0.5 | 0.0 | 1.7 | 0.7 | 0.0 | 0.3 | 1.7 |
| E3 | 0.0 | 0.4 | 3.4 | 1.8 | 2.5 | 3.1 | 0.0 | 2.6 | 3.6 | 3.4 | 3.4 | 3.5 | 3.5 | 2.6 | 0.0 | 0.0 | 2.9 | 0.0 | 3.6 | 3.7 |
| E4 | 0.0 | 0.0 | 3.6 | 0.0 | 0.0 | 3.1 | 0.0 | 4.0 | 0.0 | 3.1 | 0.0 | 3.7 | 0.0 | 0.0 | 0.4 | 0.0 | 0.0 | 3.6 | 4.0 | 3.7 |
| E5 | 0.0 | 0.4 | 0.0 | 3.5 | 3.6 | 0.7 | 0.0 | 0.0 | 0.0 | 0.9 | 0.0 | 3.4 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 2.3 | 0.0 |
| E6 | 0.8 | 0.0 | 0.0 | 3.7 | 0.0 | 0.5 | 0.0 | 0.5 | 3.4 | 0.0 | 3.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 3.4 | 0.0 | 0.5 |
| E7 | 0.4 | 0.0 | 0.5 | 0.3 | 0.0 | 3.4 | 0.6 | 0.7 | 3.5 | 0.0 | 3.7 | 3.5 | 3.6 | 0.0 | 0.0 | 0.0 | 0.0 | 3.5 | 3.5 | 0.0 |
Step 2: The direct influence matrix is normalized by the rows being summed and each element is divided by the maximum value to derive Table 6.
Table 6.
Normalized direct influence matrix.
| T1 | T2 | T3 | T4 | T5 | T6 | T7 | O1 | O2 | O3 | O4 | O5 | O6 | E1 | E2 | E3 | E4 | E5 | E6 | E7 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | 0.0000 | 0.0841 | 0.0341 | 0.0795 | 0.0182 | 0.0886 | 0.0091 | 0.0000 | 0.0000 | 0.0909 | 0.0000 | 0.0773 | 0.0000 | 0.0818 | 0.0091 | 0.0000 | 0.0000 | 0.0909 | 0.0318 | 0.0000 |
| T2 | 0.0273 | 0.0000 | 0.0386 | 0.0818 | 0.0909 | 0.0818 | 0.0159 | 0.0000 | 0.0000 | 0.0886 | 0.0818 | 0.0795 | 0.0000 | 0.0023 | 0.0159 | 0.0000 | 0.0000 | 0.0818 | 0.0818 | 0.0182 |
| T3 | 0.0000 | 0.0091 | 0.0000 | 0.0750 | 0.0159 | 0.0795 | 0.0023 | 0.0000 | 0.0841 | 0.0841 | 0.0727 | 0.0841 | 0.0000 | 0.0818 | 0.0682 | 0.0000 | 0.0000 | 0.0773 | 0.0841 | 0.0114 |
| T4 | 0.0000 | 0.0091 | 0.0000 | 0.0000 | 0.0818 | 0.0750 | 0.0045 | 0.0000 | 0.0000 | 0.0818 | 0.0000 | 0.0795 | 0.0000 | 0.0023 | 0.0136 | 0.0795 | 0.0818 | 0.0909 | 0.0864 | 0.0000 |
| T5 | 0.0773 | 0.0000 | 0.0000 | 0.0818 | 0.0000 | 0.0818 | 0.0023 | 0.0000 | 0.0750 | 0.0841 | 0.0045 | 0.0795 | 0.0000 | 0.0773 | 0.0091 | 0.0000 | 0.0136 | 0.0841 | 0.0795 | 0.0136 |
| T6 | 0.0159 | 0.0000 | 0.0000 | 0.0864 | 0.0000 | 0.0000 | 0.0136 | 0.0000 | 0.0000 | 0.0386 | 0.0068 | 0.0773 | 0.0000 | 0.0818 | 0.0136 | 0.0295 | 0.0841 | 0.0818 | 0.0818 | 0.0000 |
| T7 | 0.0182 | 0.0000 | 0.0000 | 0.0773 | 0.0795 | 0.0864 | 0.0000 | 0.0000 | 0.0841 | 0.0864 | 0.0023 | 0.0795 | 0.0091 | 0.0091 | 0.0068 | 0.0341 | 0.0136 | 0.0864 | 0.0886 | 0.0682 |
| O1 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0114 | 0.0000 | 0.0000 | 0.0750 | 0.0114 | 0.0841 | 0.0341 | 0.0000 | 0.0068 | 0.0000 | 0.0818 | 0.0795 | 0.0182 | 0.0000 | 0.0818 |
| O2 | 0.0136 | 0.0386 | 0.0000 | 0.0000 | 0.0000 | 0.0091 | 0.0000 | 0.0000 | 0.0000 | 0.0818 | 0.0091 | 0.0909 | 0.0727 | 0.0091 | 0.0886 | 0.0545 | 0.0818 | 0.0000 | 0.0841 | 0.0773 |
| O3 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0136 | 0.0795 | 0.0636 | 0.0000 | 0.0864 | 0.0045 | 0.0773 | 0.0068 | 0.0159 | 0.0591 | 0.0750 | 0.0000 | 0.0591 | 0.0750 |
| O4 | 0.0091 | 0.0864 | 0.0000 | 0.0136 | 0.0000 | 0.0318 | 0.0114 | 0.0000 | 0.0568 | 0.0000 | 0.0000 | 0.0909 | 0.0818 | 0.0182 | 0.0773 | 0.0000 | 0.0909 | 0.0841 | 0.0841 | 0.0818 |
| O5 | 0.0000 | 0.0795 | 0.0773 | 0.0386 | 0.0545 | 0.0568 | 0.0091 | 0.0795 | 0.0523 | 0.0000 | 0.0818 | 0.0000 | 0.0000 | 0.0023 | 0.0795 | 0.0000 | 0.0091 | 0.0909 | 0.0818 | 0.0705 |
| O6 | 0.0341 | 0.0318 | 0.0773 | 0.0318 | 0.0841 | 0.0818 | 0.0818 | 0.0091 | 0.0614 | 0.0000 | 0.0795 | 0.0795 | 0.0000 | 0.0136 | 0.0841 | 0.0000 | 0.0091 | 0.0136 | 0.0795 | 0.0568 |
| E1 | 0.0114 | 0.0000 | 0.0818 | 0.0091 | 0.0000 | 0.0000 | 0.0000 | 0.0795 | 0.0818 | 0.0795 | 0.0136 | 0.0795 | 0.0000 | 0.0000 | 0.0773 | 0.0886 | 0.0386 | 0.0159 | 0.0159 | 0.0886 |
| E2 | 0.0000 | 0.0000 | 0.0000 | 0.0136 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0091 | 0.0000 | 0.0136 | 0.0795 | 0.0000 | 0.0114 | 0.0000 | 0.0386 | 0.0159 | 0.0000 | 0.0068 | 0.0386 |
| E3 | 0.0000 | 0.0091 | 0.0773 | 0.0409 | 0.0568 | 0.0705 | 0.0000 | 0.0591 | 0.0818 | 0.0773 | 0.0773 | 0.0795 | 0.0795 | 0.0591 | 0.0000 | 0.0000 | 0.0659 | 0.0000 | 0.0818 | 0.0841 |
| E4 | 0.0000 | 0.0000 | 0.0818 | 0.0000 | 0.0000 | 0.0705 | 0.0000 | 0.0909 | 0.0000 | 0.0705 | 0.0000 | 0.0841 | 0.0000 | 0.0000 | 0.0091 | 0.0000 | 0.0000 | 0.0818 | 0.0909 | 0.0841 |
| E5 | 0.0000 | 0.0091 | 0.0000 | 0.0795 | 0.0818 | 0.0159 | 0.0000 | 0.0000 | 0.0000 | 0.0205 | 0.0000 | 0.0773 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0523 | 0.0000 |
| E6 | 0.0182 | 0.0000 | 0.0000 | 0.0841 | 0.0000 | 0.0114 | 0.0000 | 0.0114 | 0.0773 | 0.0000 | 0.0795 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0773 | 0.0000 | 0.0114 |
| E7 | 0.0091 | 0.0000 | 0.0114 | 0.0068 | 0.0000 | 0.0773 | 0.0136 | 0.0159 | 0.0795 | 0.0000 | 0.0841 | 0.0795 | 0.0818 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0795 | 0.0795 | 0.0000 |
Step 3: The results of Table 6 are entered into MyMatrix software to derive the integrated influence matrix shown in Table 7.
Table 7.
Comprehensive influence matrix.
| T1 | T2 | T3 | T4 | T5 | T6 | T7 | O1 | O2 | O3 | O4 | O5 | O6 | E1 | E2 | E3 | E4 | E5 | E6 | E7 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | 0.0200 | 0.1165 | 0.0770 | 0.1615 | 0.0778 | 0.1633 | 0.0233 | 0.0506 | 0.0777 | 0.1667 | 0.0796 | 0.1932 | 0.0354 | 0.1182 | 0.0655 | 0.0497 | 0.0694 | 0.1960 | 0.1547 | 0.0752 |
| T2 | 0.0529 | 0.0446 | 0.0767 | 0.1753 | 0.1487 | 0.1684 | 0.0317 | 0.0478 | 0.0905 | 0.1650 | 0.1636 | 0.2080 | 0.0447 | 0.0489 | 0.0767 | 0.0459 | 0.0778 | 0.2072 | 0.2196 | 0.0981 |
| T3 | 0.0217 | 0.0544 | 0.0459 | 0.1573 | 0.0714 | 0.1564 | 0.0181 | 0.0552 | 0.1737 | 0.1598 | 0.1583 | 0.2180 | 0.0514 | 0.1184 | 0.1392 | 0.0571 | 0.0852 | 0.1910 | 0.2197 | 0.1066 |
| T4 | 0.0220 | 0.0411 | 0.0451 | 0.0821 | 0.1306 | 0.1498 | 0.0172 | 0.0542 | 0.0810 | 0.1499 | 0.0784 | 0.1889 | 0.0396 | 0.0426 | 0.0606 | 0.1149 | 0.1447 | 0.1919 | 0.2063 | 0.0784 |
| T5 | 0.0958 | 0.0429 | 0.0459 | 0.1637 | 0.0546 | 0.1583 | 0.0168 | 0.0538 | 0.1548 | 0.1629 | 0.0839 | 0.2022 | 0.0430 | 0.1161 | 0.0711 | 0.0538 | 0.0895 | 0.1934 | 0.2052 | 0.0964 |
| T6 | 0.0298 | 0.0303 | 0.0443 | 0.1490 | 0.0482 | 0.0668 | 0.0235 | 0.0507 | 0.0695 | 0.1020 | 0.0720 | 0.1753 | 0.0305 | 0.1063 | 0.0603 | 0.0699 | 0.1383 | 0.1717 | 0.1830 | 0.0718 |
| T7 | 0.0449 | 0.0425 | 0.0453 | 0.1696 | 0.1391 | 0.1763 | 0.0172 | 0.0543 | 0.1776 | 0.1690 | 0.0943 | 0.2153 | 0.0624 | 0.0543 | 0.0702 | 0.0850 | 0.0959 | 0.2090 | 0.2347 | 0.1552 |
| O1 | 0.0135 | 0.0338 | 0.0394 | 0.0483 | 0.0341 | 0.0752 | 0.0118 | 0.0407 | 0.1391 | 0.0638 | 0.1457 | 0.1318 | 0.0482 | 0.0327 | 0.0483 | 0.1077 | 0.1339 | 0.0968 | 0.1020 | 0.1532 |
| O2 | 0.0335 | 0.0772 | 0.0533 | 0.0731 | 0.0513 | 0.0935 | 0.0204 | 0.0554 | 0.0887 | 0.1422 | 0.1044 | 0.2077 | 0.1196 | 0.0415 | 0.1459 | 0.0909 | 0.1414 | 0.1055 | 0.2075 | 0.1646 |
| O3 | 0.0190 | 0.0379 | 0.0448 | 0.0598 | 0.0422 | 0.0768 | 0.0323 | 0.1206 | 0.1472 | 0.0584 | 0.1662 | 0.1204 | 0.1271 | 0.0361 | 0.0733 | 0.0946 | 0.1395 | 0.0934 | 0.1732 | 0.1616 |
| O4 | 0.0334 | 0.1284 | 0.0547 | 0.1039 | 0.0660 | 0.1257 | 0.0327 | 0.0506 | 0.1418 | 0.0749 | 0.0937 | 0.2278 | 0.1228 | 0.0516 | 0.1421 | 0.0395 | 0.1511 | 0.2049 | 0.2231 | 0.1679 |
| O5 | 0.0259 | 0.1200 | 0.1141 | 0.1336 | 0.1130 | 0.1471 | 0.0248 | 0.1175 | 0.1452 | 0.0819 | 0.1724 | 0.1461 | 0.0477 | 0.0465 | 0.1420 | 0.0478 | 0.0863 | 0.2155 | 0.2211 | 0.1546 |
| O6 | 0.0650 | 0.0843 | 0.1246 | 0.1422 | 0.1484 | 0.1892 | 0.0995 | 0.0589 | 0.1703 | 0.0980 | 0.1761 | 0.2409 | 0.0522 | 0.0695 | 0.1611 | 0.0526 | 0.0934 | 0.1639 | 0.2421 | 0.1557 |
| E1 | 0.0286 | 0.0427 | 0.1313 | 0.0811 | 0.0489 | 0.0882 | 0.0159 | 0.1360 | 0.1822 | 0.1536 | 0.1174 | 0.2121 | 0.0613 | 0.0414 | 0.1440 | 0.1376 | 0.1169 | 0.1218 | 0.1523 | 0.1898 |
| E2 | 0.0063 | 0.0180 | 0.0217 | 0.0392 | 0.0203 | 0.0327 | 0.0056 | 0.0220 | 0.0426 | 0.0239 | 0.0478 | 0.1217 | 0.0189 | 0.0235 | 0.0243 | 0.0515 | 0.0396 | 0.0414 | 0.0552 | 0.0716 |
| E3 | 0.0328 | 0.0676 | 0.1431 | 0.1474 | 0.1233 | 0.1889 | 0.0273 | 0.1299 | 0.2137 | 0.1787 | 0.2033 | 0.2581 | 0.1482 | 0.1145 | 0.0979 | 0.0650 | 0.1696 | 0.1593 | 0.2677 | 0.2110 |
| E4 | 0.0148 | 0.0308 | 0.1124 | 0.0713 | 0.0411 | 0.1346 | 0.0125 | 0.1299 | 0.0807 | 0.1208 | 0.0839 | 0.1808 | 0.0374 | 0.0327 | 0.0568 | 0.0373 | 0.0581 | 0.1750 | 0.1940 | 0.1503 |
| E5 | 0.0144 | 0.0281 | 0.0194 | 0.1213 | 0.1100 | 0.0590 | 0.0064 | 0.0230 | 0.0411 | 0.0584 | 0.0382 | 0.1309 | 0.0152 | 0.0202 | 0.0265 | 0.0220 | 0.0335 | 0.0611 | 0.1146 | 0.0341 |
| E6 | 0.0276 | 0.0251 | 0.0167 | 0.1204 | 0.0316 | 0.0520 | 0.0073 | 0.0285 | 0.1109 | 0.0396 | 0.1103 | 0.0693 | 0.0264 | 0.0165 | 0.0329 | 0.0248 | 0.0428 | 0.1312 | 0.0682 | 0.0514 |
| E7 | 0.0290 | 0.0430 | 0.0485 | 0.0813 | 0.0506 | 0.1443 | 0.0320 | 0.0496 | 0.1493 | 0.0555 | 0.1524 | 0.1866 | 0.1182 | 0.0321 | 0.0617 | 0.0325 | 0.0612 | 0.1739 | 0.1910 | 0.0716 |
Step 4: The degrees of influence, being influenced, centrality, and causality of each factor are calculated to form a comprehensive influence relationship table, as shown in Table 8, which displays the calculations of the adoption of AI services by medical and healthcare institutions. The centrality degree represents the total relationship between each element and the others, with higher values indicating closer relationships. A causality degree greater than 0 means that the element is a causal factor, which has strong influences on the other elements, but itself is rarely influenced by other factors, whereas a degree less than 0 is known as an outcome factor, which means that the element is strongly influenced. A higher centrality ranking indicates a higher intensity of the influence on the factors affecting the adoption of AI medical services.
Table 8.
Analysis of Decision-making Trial and Evaluation Laboratory’s (DEMATEL’s) results for adoption of intelligent health service resources.
| Influencing degree A | Influenced degree B | Centrality degree M | Causality degree U | Centrality ranking | |
|---|---|---|---|---|---|
| T1 | 1.97123 | 0.63079 | 2.6020 | 1.3404 | 19 |
| T2 | 2.19213 | 1.10920 | 3.3013 | 1.0829 | 16 |
| T3 | 2.25859 | 1.30404 | 3.5626 | 0.9545 | 14 |
| T4 | 1.91948 | 2.28112 | 4.2006 | 0.3616 | 6 |
| T5 | 2.10412 | 1.55130 | 3.6554 | 0.5528 | 13 |
| T6 | 1.69308 | 2.44650 | 4.1396 | 0.7534 | 8 |
| T7 | 2.31205 | 0.47613 | 2.7882 | 1.8359 | 18 |
| O1 | 1.49990 | 1.32943 | 2.8293 | 0.1705 | 17 |
| O2 | 2.01764 | 2.47766 | 4.4953 | 0.4600 | 4 |
| O3 | 1.82454 | 2.22496 | 4.0495 | 0.4004 | 10 |
| O4 | 2.23677 | 2.34157 | 4.5783 | 0.1048 | 3 |
| O5 | 2.30303 | 3.63517 | 5.9382 | 1.3321 | 1 |
| O6 | 2.58780 | 1.25006 | 3.8379 | 1.3377 | 11 |
| E1 | 2.20288 | 1.16362 | 3.3665 | 1.0393 | 15 |
| E2 | 0.72753 | 1.70033 | 2.4279 | 0.9728 | 20 |
| E3 | 2.94718 | 1.28010 | 4.2273 | 1.6671 | 5 |
| E4 | 1.75519 | 1.96810 | 3.7233 | 0.2129 | 12 |
| E5 | 0.97737 | 3.10399 | 4.0814 | 2.1266 | 9 |
| E6 | 1.03340 | 3.63529 | 4.6687 | 2.6019 | 2 |
| E7 | 1.76453 | 2.41908 | 4.1836 | 0.6545 | 7 |
Analysis of the intensity of influencing factors
Centrality ranking analysis: according to Table 8, the top centrality rankings are: Inability to share information (O5), Difficult to meet the complex needs of elderly patients (E6), Lack of support from excellent providers (O4), Hospital size (O2), Geographical restrictions (E3), and Skeptical of AI processing capabilities (T4). Hence, these five factors are highly correlated with the other factors. The largest centrality score belongs to Inability to share information (O5), indicating that O5 plays the most significant role in the overall structural system and is most closely related to other factors.
Causality degree analysis: The higher the degree, the higher is the intensity of the influence exerted by the factor on the other factors, but the weaker is the intensity of being influenced by them. In Table 8, the highest score belongs to Lack of ability to read structured medical data (T7), indicating that this factor exerts a strong influence on other factors but is less influenced by them.
Influencing degree analysis: higher values indicate that a factor has stronger influences on the other factors. In Table 8, the strongest influence is that of Geographical restrictions (E3), followed by Lack of complex talent (O6), so these factors cannot be ignored.
Influenced degree analysis: higher values indicate that a factor is more strongly influenced by other factors.
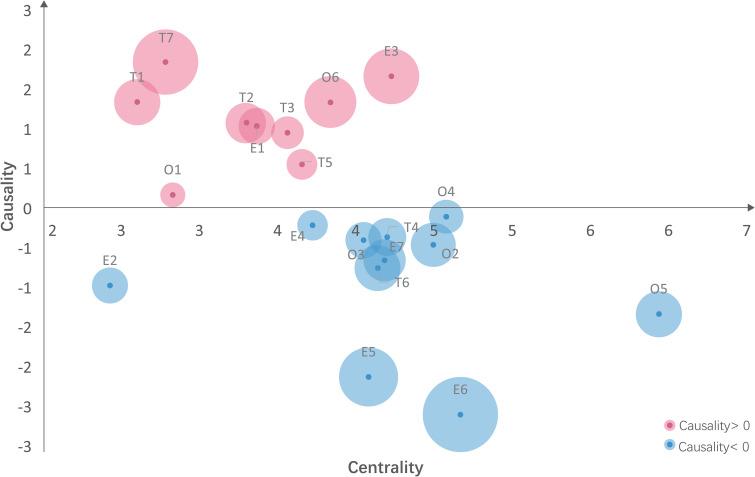
Based on Table 8, the DEMATEL cause-effect diagram of the adoption factors of intelligent healthcare service resources in medical institutions is shown in Figure 3, which more effectively distinguishes the cause and effect factors. The centrality and causality degrees are represented by the X and Y axes, respectively. The influencing factors with degrees greater than 0 are the causal factors and directly affect the adoption of AI medical services by healthcare institutions, whereas those with degrees less than 0 are the effect factors, which are influenced by the causal factors and indirectly affect the adoption. The higher the centrality of a factor, the higher is the ranking of the factor and the stronger is its correlation with the other factors.
Figure 3.
DEMATEL cause-effect diagram of factors affecting adoption of AI medical service resources. DEMATEL: Decision-making Trial and Evaluation Laboratory; AI: artificial intelligence.
Causality factors: High risk of data leakage (T1), System service complexity (T2), AI infrastructure synergy (T3), Lack of awareness of the value and benefits of AI healthcare technology (T5), Lack of ability to read structured medical data (T7), Lack of management leadership support (O1), Lack of excellent supplier support (O4), Lack of complex talent (O6), Government policies (E1), and Geographical restrictions (E3).
Outcome factors: Skeptical of AI processing capabilities (T4), Medically derived risks (T6), Hospital size (O2), Financial costs (O3), Inability to share information (O5), Competitive pressures (E2), Unclear ownership of hospitals (E4), Lack of patient trust (E5), Difficult to meet the complex needs of elderly patients (E6), and Lack of excellent partnerships (E7).
ISM procedure
- Step 1: The self-interaction matrix shown in Table 9 has been constructed from the experts’ opinions according to the following rules:
- P: variable i favors the influence variable j.
- Q: variable j favors the influence variable i.
- R: variables i and j interact directly with each other.
- V: variables i and j do not affect each other.
Step 2: The self-interaction matrix is converted by the following rules into binary format to derive the adjacency matrix shown in Table 10: P=1, Q=0, R=1, and V=1.
Step 3: The initial reachable matrix of the system is derived by matrix operations by the use of MyMatrix software according to the following conversion rule: , where is the unit matrix.
Step 4: The reachable matrix is decomposed into the reachable set R(Si), antecedent set Q(Si), and collective set . Table 11 shows the reachable matrix decomposition table. R(Si) is the set of column elements corresponding to the matrix elements containing 1 in the rows corresponding to element Si in the reachable matrix. Q(Si) is the set of row elements corresponding to the matrix elements containing 1 in the columns corresponding to element Si in the reachable matrix.
Step 5: Hierarchical classification of the reachable matrix is done by extracting the hierarchy according to the condition . For example, 15 (E2), 18 (E5), and 20 (E7) in Table 11 satisfy the condition, so these factors are in the topmost layer of the system. The set of the layer elements is: . The elements i = 15, 18, and 20 in Table 11 were extracted to produce Table 12.
Table 9.
Structured self-interaction matrix.
| E7 | E6 | E5 | E4 | E3 | E2 | E1 | O6 | O5 | O4 | O3 | O2 | O1 | T7 | T6 | T5 | T4 | T3 | T2 | T1 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | V | V | P | V | V | V | P | V | V | V | V | V | V | V | P | Q | V | V | V | |
| T2 | V | V | P | V | V | V | V | V | P | V | P | V | V | Q | P | V | V | Q | ||
| T3 | V | V | P | Q | V | V | V | V | V | V | V | P | V | V | V | V | V | |||
| T4 | V | V | P | V | V | V | V | V | V | V | V | V | V | V | V | Q | ||||
| T5 | V | P | P | V | V | V | V | P | P | V | V | P | V | P | P | |||||
| T6 | V | V | P | V | V | V | V | Q | V | V | V | V | V | V | ||||||
| T7 | V | V | V | V | V | V | V | Q | P | V | V | P | V | |||||||
| V1 | P | V | V | P | V | V | R | V | V | V | V | Q | ||||||||
| V2 | P | V | V | P | R | V | V | P | V | P | P | |||||||||
| V3 | V | V | V | V | V | P | V | V | V | V | ||||||||||
| V4 | P | V | V | V | V | V | V | V | V | |||||||||||
| V5 | V | V | V | Q | V | P | V | V | ||||||||||||
| V6 | V | P | V | V | V | V | V | |||||||||||||
| E1 | V | V | V | P | V | V | ||||||||||||||
| E2 | R | V | V | V | V | |||||||||||||||
| E3 | V | P | V | V | ||||||||||||||||
| E4 | V | V | V | |||||||||||||||||
| E5 | V | Q | ||||||||||||||||||
| E6 | V | |||||||||||||||||||
| E7 |
Table 10.
Adjacency matrix.
| T1 | T2 | T3 | T4 | T5 | T6 | T7 | O1 | O2 | O3 | O4 | O5 | O6 | E1 | E2 | E3 | E4 | E5 | E6 | E7 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 |
| T2 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| T3 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| T4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| T5 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 |
| T6 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| T7 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| O1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 |
| O2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 |
| O3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| O4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| O5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| O6 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| E1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| E2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| E3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| E4 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| E5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| E6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| E7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
Table 11.
Explanatory table of reachable matrix.
| i | Coding | Reachable set R(Si) | Antecedent set Q(Si) | Collective set R(Si) Q(Si) |
|---|---|---|---|---|
| 1 | T1 | 4 5 excluded | 1 | 1 |
| 2 | T2 | 2 6 10 12 15 18 20 | 1 2 3 5 7 8 9 13 14 16 17 | 2 |
| 3 | T3 | 1 4 5 8 14 excluded | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 4 | T4 | 4 18 | 4 5 | 4 |
| 5 | T5 | 8 14 excluded | 5 | 5 |
| 6 | T6 | 6 18 | 1 2 3 6–9 13 14 16 17 | 6 |
| 7 | T7 | 2 3 6 7 9–13 15–20 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 8 | O1 | 1 4 5 excluded | 1 8 9 14 | 8 9 14 |
| 9 | O2 | 1 4 5 excluded | 3 5 7 8 9 13 14 16 17 | 3 7 8 9 13 14 16 17 |
| 10 | O3 | 10 15 20 | 1 2 3 5 7–10 13 14 16 17 | 10 |
| 11 | O4 | 11 | 1 3 5 7 8 9 11 13 14 16 17 | 11 |
| 12 | O5 | 12 15 20 | 1 2 3 5 7 8 9 12 13 14 16 17 | 12 |
| 13 | O6 | 1 4 5 14 excluded | 1 3 5 7 8 9 13 14 16 17 | 3 7 8 9 13 16 17 |
| 14 | E1 | 1 4 5 excluded | 1 8 14 | 8 14 |
| 15 | E2 | 15 20 | 1 2 3 5 7–10 12–17 20 | 15 20 |
| 16 | E3 | 1 4 5 8 14 excluded | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 17 | E4 | 1 4 5 8 14 excluded | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 18 | E5 | 18 | 10–12 15 20 excluded | 18 |
| 19 | E6 | 18 19 | 1 3 5 7–9 13 14 16 17 19 | 19 |
| 20 | E7 | 15 20 | 4 6 11 18 19 excluded | 15 20 |
Table 12.
Matrix decomposition table with topmost layer extracted from Table 11.
| i | Coding | Reachable set R(Si) | Antecedent set Q(Si) | Collective set R(Si) Q(Si) |
|---|---|---|---|---|
| 1 | T1 | 4 5 15 18 20 excluded | 1 | 1 |
| 2 | T2 | 2 6 10 12 | 1 2 3 5 7 8 9 13 14 16 17 | 2 |
| 3 | T3 | 1 4 5 8 14 15 18 20 excluded | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 4 | T4 | 4 | 4 5 | 4 |
| 5 | T5 | 8 14 15 18 20 excluded | 5 | 5 |
| 6 | T6 | 6 | 1 2 3 6–9 13 14 16 17 | 6 |
| 7 | T7 | 2 3 6 7 9–13 16 17 19 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 8 | O1 | 1 4 5 15 18 20 excluded | 1 8 9 14 | 8 9 14 |
| 9 | O2 | 1 4 5 15 18 20 excluded | 3 5 7 8 9 13 14 16 17 | 3 7 8 9 13 14 16 17 |
| 10 | O3 | 10 | 1 2 3 5 7–10 13 14 16 17 | 10 |
| 11 | O4 | 11 | 1 3 5 7 8 9 11 13 14 16 17 | 11 |
| 12 | O5 | 12 | 1 2 3 5 7 8 9 12 13 14 16 17 | 12 |
| 13 | O6 | 1 4 5 14 15 18 20 excluded | 1 3 5 7 8 9 13 14 16 17 | 3 7 8 9 13 16 17 |
| 14 | E1 | 1 4 5 15 18 20 excluded | 1 8 14 | 8 14 |
| 16 | E3 | 1 4 5 8 14 15 18 20 excluded | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 17 | E4 | 1 4 5 8 14 15 18 20 excluded | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 19 | E6 | 19 | 1 3 5 7–9 13 14 16 17 19 | 19 |
Table 12 shows that 4, 6, 10, 11, 12, and 19 satisfy the condition and obtain the set . The second layer was extracted to produce Table 13.
Table 13.
Matrix decomposition table after extraction of the second layer.
| i | Coding | Reachable set R(Si) | Antecedent set Q(Si) | Collective set R(Si) Q(Si) |
|---|---|---|---|---|
| 1 | T1 | 1 2 3 7 8 9 13 14 16 17 | 1 | 1 |
| 2 | T2 | 2 | 1 2 3 5 7 8 9 13 14 16 17 | 2 |
| 3 | T3 | 2 3 7 9 13 16 17 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 5 | T5 | 1 2 3 57 9 13 16 17 | 5 | 5 |
| 7 | T7 | 2 3 6 7 9–13 16 17 19 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 8 | O1 | 2 3 7 8 9 13 14 16 17 | 1 8 9 14 | 8 9 14 |
| 9 | O2 | 2 3 7 8 9 13 14 16 17 | 3 5 7 8 9 13 14 16 17 | 3 7 8 9 13 14 16 17 |
| 13 | O6 | 2 3 7 8 9 13 16 17 | 1 3 5 7 8 9 13 14 16 17 | 3 7 8 9 13 16 17 |
| 14 | E1 | 2 3 7 8 9 13 14 16 17 | 1 8 14 | 8 14 |
| 16 | E3 | 2 3 7 9 13 16 17 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 17 | E4 | 2 3 7 9 13 16 17 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
Table 13 shows that 2 satisfies the condition and obtains the set . The third layer was extracted to produce Table 14.
Table 14.
Matrix decomposition table after extraction of the third layer.
| i | Coding | Reachable set R(Si) | Antecedent set Q(Si) | Collective set R(Si) Q(Si) |
|---|---|---|---|---|
| 1 | T1 | 1 3 7 8 9 13 14 16 17 | 1 | 1 |
| 3 | T3 | 3 7 9 13 16 17 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 5 | T5 | 1 3 5 7 9 13 16 17 | 5 | 5 |
| 7 | T7 | 3 6 7 9–13 16 17 19 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 8 | O1 | 3 7 8 9 13 14 16 17 | 1 8 9 14 | 8 9 14 |
| 9 | O2 | 3 7 8 9 13 14 16 17 | 3 5 7 8 9 13 14 16 17 | 3 7 8 9 13 14 16 17 |
| 13 | O6 | 3 7 8 9 13 16 17 | 1 3 5 7 8 9 13 14 16 17 | 3 7 8 9 13 16 17 |
| 14 | E1 | 3 7 8 9 13 14 16 17 | 1 8 14 | 8 14 |
| 16 | E3 | 3 7 9 13 16 17 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
| 17 | E4 | 3 7 9 13 16 17 | 1 3 5 7 8 9 13 14 16 17 | 3 7 9 13 16 17 |
Table 14 shows that 3, 7, 9, 13, 16, and 17 satisfy the condition and obtain the set . The fourth layer was extracted to produce Table 15.
Table 15.
Matrix decomposition table after extraction of the fourth layer.
| i | Coding | Reachable set R(Si) | Antecedent set Q(Si) | Collective set R(Si) Q(Si) |
|---|---|---|---|---|
| 1 | T1 | 1 8 14 | 1 | 1 |
| 5 | T5 | 1 5 | 5 | 5 |
| 8 | O1 | 8 14 | 1 8 14 | 8 14 |
| 14 | E1 | 8 14 | 1 8 14 | 8 14 |
Table 15 shows that 8 and 14 satisfy the condition and obtain the set . The fifth layer was extracted to produce Table 16.
Table 16.
Matrix decomposition table after extracting the fifth layer.
| i | Coding | Reachable set R(Si) | Antecedent set Q(Si) | Collective set R(Si) Q(Si) |
|---|---|---|---|---|
| 1 | T1 | 1 | 1 | 1 |
| 5 | T5 | 15 | 5 | 5 |
Table 16 shows that 1 satisfies the condition and obtains the set . The sixth layer was extracted to produce Table 17.
Table 17.
Matrix decomposition table after extraction of the sixth layer.
| i | Coding | Reachable set R(Si) | Antecedent set Q(Si) | Collective set R(Si) Q(Si) |
|---|---|---|---|---|
| 5 | T5 | 5 | 5 | 5 |
The bottom element from Table 17 can be derived as .
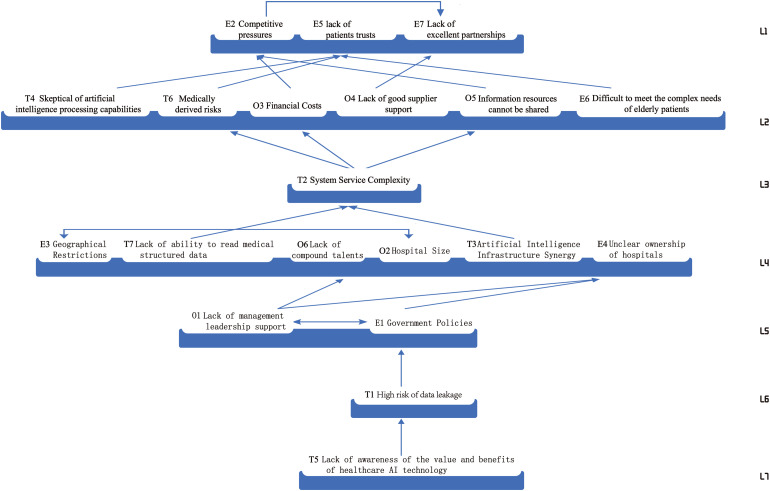
Multilayer recursive structural analysis
According to the divisions of the intervals and layers in the results of the reachable matrix decompositions in the previous section, a multilayer recursive structural model can be established, the 20 factors for the adoption of the AI medical service resources can be divided into seven layers from top to bottom, and the final multilayer recursive structural model can be represented as a directed graph, as shown in Figure 4.
Figure 4.
Directional diagram of factors for adoption of artificial intelligence (AI) healthcare services in medical institutions.
From Figure 4, the following conclusions are drawn:
(1) There are three influences at the top of the system: competitive pressures (E2), lack of patient trust (E5), and lack of excellent partnerships (E7). In China’s current healthcare system, competitive pressures (E2) are embedded in the following three models.
The current Chinese medical system has three main models that combine medical and healthcare institutions with elderly care: the departmental organizational, contractual, and network models. However, the contract model of combination of medical and health care requires larger initial investments because the invested costs are relatively high under the government’s attention and a high-return model has not yet been formulated. The bureaucratic model and the network model of integrated medical and healthcare services require smaller amounts of capital, but the quantities of services supplied by them are larger than that by the contract model, which fails to provide the expected efficiency. The adoption of AI medical services has become the key to turning around the profitability of healthcare institutions.
In addition to this, lack of patient trust (E5) is due to AI medical services are widely used and can rival doctors’ diagnoses by being more accurate, especially for heart, skin, and eye diseases.50,51 Even though AI has proven to have low rates of misdiagnoses, patients still prefer to trust their doctors’ diagnoses52,53 because they tend to believe that AI lacks flexibility and standardization, so it would be suitable only for treating patients with general illnesses. Convincing people that AI could be applied to their unique situations 54 has proven difficult. The continued lack of trust among elderly patients prevents the continued adoption of AI healthcare services.
Lack of excellent partnerships (E7): the combinations of medical and health care institutions are based on agreements between hospitals and nursing institutions, with the former taking the lead in providing medical resources and technological guidance. The hospitals are usually dominated by large secondary and tertiary institutions, whereas most nursing institutions have been formed by insurance and real estate companies, which require the rapid realization of profits and do not uphold the philosophy of sustainable development as do public hospitals.
Competitive pressures (E2) have an impact on the lack of excellent partnerships (E7), as services and products in the healthcare sector are highly specialized and high risk, and generally require rigorous long-term clinical trials before they can be adopted and applied. However, existing intelligent healthcare services themselves lack a rigorous evidence-based process and interpretation, so there is a high technological threshold for artificial intelligence healthcare service resources. Competitive pressures are forcing medical institutions to demand a high level of partner teaching, especially for first-hand information data obtained after long-term clinical trials, making excellent partnerships a valuable strategic partner resource under competitive pressure.
Furthermore, it is clear from Figure 4 directional diagram that lacks of patient trust (E5) has a close and direct relationship with the second tier of factors: skeptical of AI processing capabilities (T4), medically derived risks (T6), E6 factor of skeptical of AI processing capabilities (T4), medically derived risks (T6), and difficult to meet complex needs of elderly patients (E6) have a close and direct influence. The high complexity of their own needs can easily lead to a lack of patient trust due to older patients’ mistrust of AI processing capabilities and the emergence of an increasing number of safety incidents caused by doctors’ mishandling. Competitive pressures (E2) is closely and directly related to the second tier of influences financial costs (O3), inability to share information (O5). The asymmetry of information resources leads to the need for each medical institution to use its own data system independently, thus making research and development more difficult, and the higher the cost of investment, the more urgent the desire of investors to quickly recoup their capital, thus increasing the competitive pressure in the market. The lack of excellent partnerships (E7) is directly influenced by the lack of excellent supplier support (O4), which determines the quality of AI healthcare service resources in medical institutions. Therefore, most medical institutions sign exclusive partner agreements with excellent suppliers.
The top-level factors of the model are the most direct factors influencing the resources for AI healthcare service resources in healthcare organizations. Starting with these three areas will enable the adoption of AI healthcare service resources in healthcare organizations in the short term and enable the smooth implementation of AI healthcare service resources in hospitals. These three factors interact with each other at the top level and are the most easily identifiable in the analysis. They are also central to the goal of maintaining system balance and improving the system, which is a clear indication of its importance.
(2) The influencing factors at the second tier are skeptical of AI processing capabilities (T4), medically derived risks (T6), financial costs (O3), lack of excellent supplier support (O4), inability to share information (O5), difficulty to meet complex needs of elderly patients (E6), these six factors belong to the shallow level of influence and indirectly influence the adoption of AI healthcare service through the three factors in the top level. The adoption of the resources factor is also influenced by the next tier of factors.
Skeptical of AI capabilities: AI makes medical decisions based on data jointly labeled by hospitals and companies into a database, but the lack of industry standards results in differences in the data submitted by different companies. Thus, the data are skewed and do not represent real situations accurately. 36 As medical intelligence companies use algorithm automation, security, and confidentiality as a pretext to achieve their own interests, they embed corporate profitability and autonomous behaviors into rule-driven algorithms, thus creating “algorithmic black boxes.” 55 Such algorithms are wrapped into intelligent healthcare services through human manipulation and pass on the risks to elderly patients, physicians, and hospitals, thus resulting in lower logical interpretations, which must often be questioned by the hospitals.
Medically derived risks: this refers to the psychological or physical risks and the side effects to elderly patients caused by improper clinical practices and the misconduct of staff in medical, nursing, rehabilitation, and healthcare institutions.
Financial costs: this refers to the costs of the manpower, resources, and IT needed to build AI medical service resources for medical and healthcare institutions incorporating multiple intelligent platforms, such as 5G, cloud computing, big data, and the Internet of Things. After long-term rigorous clinical tests, the high costs of time and finances invested by the government and hospitals are important factors that the latter have to consider at the organizational level.
Lack of excellent supplier support: this refers to professional AI companies or other non-medical intelligent companies with practical experience in AI. These companies are engaged in horizontal medical extensions while attempting to transpose technological experiences from other industries to medical and healthcare institutions. In the short term, such suppliers can produce results quickly, but as patients, doctors, and hospitals continue to emerge with strong needs, the professional expertize of these suppliers cannot meet the specific requirements of intelligent medical services.
Inability to share information: this refers to the data docking ports between hospitals and nursing homes. These ports are not uniform and result in information not being transmitted or shared according to uniform standards. The variety of medical software poses another problem. Working with software manufacturers to coordinate data interface issues tends to have high costs, which are another important factor preventing the sharing of AI medical service resources.
Difficult to meet the complex needs of elderly patients: China’s population will enter the stage of rapid aging by 2035, so the elderly will become a large group. Each elderly patient has different rigid needs, so questions abound on making AI medical services meet their social, personalized, individualized, and specialized needs to realize psychological comfort, spiritual satisfaction, and social participation, as well as help them to avoid secondary injuries and chronic diseases. Current AI medical services are in a rough growth mode, which is helpful to elderly patients with general diseases but not enough to meet those with complex needs, which are an influencing factor for the adoption of intelligent medical service resources.
Among them, system service complexity (T2), medically derived risks (T6), financial costs (O3), inability to share information (O5), as smart healthcare service has unique. Due to the unique advantages and complexity of smart healthcare service, all data, people, and equipment are linked together, which tests the system hardware and the expertize of the technicians, inevitably resulting in improper operation by doctors and medically derived risks. Due to the complexity of the system, it costs a lot of money to upgrade and maintain the system hardware, and the security loopholes prevent information resources from being shared in the short term, resulting in information silos.
(3) The third and fourth layers are the deeper influencing factors, mainly including system service complexity (T2), geographical restrictions (E3), lack of ability to read structured medical data (T7), lack of complex talent (O6), hospital size (O2), AI infrastructure synergy (T3), unclear ownership of hospitals (E4), these seven factors are the deep-seated factors that healthcare organizations will consider when adopting AI recreation service resources, and healthcare organization managers need to consider the above specific factors when making adoption decisions. These are the seven factors that will be considered in the adoption of AI healthcare resources.
System service complexity: the complexity of intelligent information systems positively affects healthcare adoption decisions. 25 For medical institutions, the adoption of such systems usually consists of large projects, of which some examples are adoptions by the geriatric departments of large foreign hospitals and well-known health institutions: Vital Signs Monitoring System, MNIS, Health Level 7E-Signature, PACS, CIS, Radiology Information System (RIS), HIS, Laboratory Information System (LIS), and Radio Frequency Identification (RFID). Each system has unique advantages and complexity. If some or all of them are linked to other systems, then the capacity of a medical institution’s cloud computing platform, as well as the abilities of its professional and technological personnel, are a significant test, so the complexity of the system services is one of the important factors for hospitals to consider when adopting intelligent medical service resources.
Geographical restrictions: China’s hierarchy of hospitals is divided into three levels. The higher the city level, the larger is the population carrying capacity. The corresponding numbers of secondary and tertiary hospitals increase with the population. The hospitals are also directly supported by the local governments and the central bank, so they have considerable advantages over other medical institutions in terms of human resources, materials, and information. The institutions with integrated medical care and healthcare services are dominated by the secondary and tertiary hospitals. These institutions have signed cooperation contracts with large elderly care institutions nearby. For example, the “Better Home, Better Life” Wellness Center in Hefei, Anhui Province, signed a contract with the First Affiliated Hospital of Anhui Medical University to establish cooperative mechanisms such as green referrals, telemedicine, and expert consultations. Because of geographical constraints, the numbers of secondary and tertiary hospitals are low and their management is relatively backward in cities below the third level, which have low economic and population capacities, so geographical constraints are an influential factor in the adoption of AI medical services.
Lack of ability to read structured medical data: this refers to the conversion of unstructured data in medical records, images, and test reports into structured data that can be read by AI. According to the report of the Guanyan Research Institute, about 80% of the information in the electronic medical records of many healthcare institutions is copied and pasted while most structured medical databases are destroyed, thus restricting the development of AI medicine. 56
Lack of complex talent: as of 2021, China’s AI industry has fewer than 50,000 employes. 56 The lack of complex talent has led to slow progress in the construction of AI medical services and has hindered hospitals in using intelligent services.
Hospital size: according to the Ministry of Health’s “Hospital Grading Management Measures,” the criteria for hospital size are based on the number of beds, building capacity, number of employes, and departmental settings, whereas the sizes of foreign hospitals are mainly determined according to the number of registered beds. 22 The higher the number of beds and patient demand, the higher is the necessity of introducing intelligent medical services to alleviate mismatches between medical supply and demand.
AI infrastructure synergy: when medical information and applications are not interconnected and functionally related to each other, medical business processes can become easily disconnected, so the function of AI Infrastructure Synergy comes to the fore to unify the management of information in various medical departments and regions, as well as to optimize the sharing of information for “chimney construction,” thus avoiding the phenomenon of resource and information silos.
Unclear ownership of hospitals: in the contractual model, cooperative agreements are signed to meet the needs and improve the quality of elderly healthcare. However, a mechanism for enforcing the contracts is lacking. The signatories may have legal boundary problems while ownership and responsibilities may not be clear. When a problem arises, each side tends to blame the other, but the elderly patients are the ones who become the victims.
Two of these factors interact with each other, geographical restrictions (E3) and hospital size (O2), which are located at level 4. The higher the city rank, the larger the population and hence the number of large general hospitals such as level 2 and 3 hospitals, plus the higher the city rank, the greater the financial support from the central government and the medical institutions are dominated by mostly level 2 and 3 hospitals. Thus, the higher the city rank, the larger the hospital, the more comprehensive the hospital and the higher the geographical rank in which it is located. The lack of complex talent (O6) is directly influenced by lack of management leadership support (O1), while O1 lack of management leadership support and government policies (E1) together have a direct impact on unclear ownership of hospitals (E4). The AI healthcare service resources process is complex, capital intensive and long lasting, making it difficult to obtain senior leadership support and thus lacking the resources to develop complex talent. The lack of support from senior management and the lack of implementation of government policies can lead to unclear ownership and legal disputes when a hospital and a nursing facility enter into a joint venture agreement. There are many influencing factors at the middle level, and they become an important link between the lower and upper levels, serving as an important transmission hub for the systemic pathway, which is often brought together through the combined effect of the underlying factors.
(4) The influencing factors in layers 5 and 7 include high risk of data leakage (T1), lack of awareness of the value and benefits of AI healthcare technology (T5), lack of management leadership support (O1), government policies (E1). They are located at the bottom of the directed graph of the multi-layer recursive structural model and are fundamental factors of the AI healthcare service resources adoption system, which will continue to influence the upper layers of the structural model in the long term, especially the lack of awareness of the value and benefits of AI healthcare technology (T5), in particular, is a non-negligible factor affecting the adoption of AI healthcare service resources by medical institutions.
Lack of management leadership support: this refers to the human, material, and financial resources required for the construction of AI facilities, 5G networks, cloud computing platforms, and environments for the Internet of Things. Also, the institutions require intelligent medical service facilities, which are acquired after long periods of rigorous trials conducted before they can be applied to clinical activities. Because of the long periods, complex processes, and high financial costs involved, leadership support is difficult to acquire.
Government policies: even they are issued, they are not fully or properly implemented by local institutions and sustainable development is delayed because the policies often cannot be applied to the actual local situations, thus hindering the acquisition of AI medical service resources by healthcare institutions.
High risk of data leakage: such data include personal consultation information, identity information, privacy information, consultation records, and other service resources provided through smartphone apps, websites, and third-party medical service platforms when patients visit the medical institutions. Since AI medical services are based on the Internet, big data, and cloud computing, the degree of the informatization of intelligent medical services is increasing, so the high-value characteristics of medical data attract a large number of hackers who try to steal and trade sensitive medical data, 22 thus leading to a high degree of exposure of core business assets belonging to intelligent medical services and increasing the possibility of infringements on the rights of the patients. Data are core business assets of hospital services, so increased risks of data leakage are an important factor influencing decisions by healthcare-integrated organizations to adopt intelligent healthcare services.
Lack of ability to read structured medical data: this refers to the conversion of unstructured data in medical records, images, and test reports into structured data that can be read by AI. According to the report of the Guanyan Research Institute, about 80% of the information in the electronic medical records of many healthcare institutions is copied and pasted while most structured medical databases are destroyed, thus restricting the development of AI medicine. 56
Two factors, lack of management leadership support (O1) and government policies (E1), located at level 5, interact with each other. the E1 factor is directly influenced by the high risk of data leakage (T1) factor, while the T1 factor is directly influenced by the lack of government policies (T5) are usually developed with the support of higher management leadership, which in turn is constrained by government policies. When they are enacted do lower management leaders have a basis to only policies are enacted can they be followed. Therefore, the O1 and E1 factors influence each other. The frequent occurrence of data leakage security incidents has led to a high degree of external exposure of artificial intelligence healthcare service resources core business assets, and the high value nature of medical data has led to a large amount of medical data being stolen and sold by patients, seriously infringing on patients’ rights and interests, so the government will therefore develop policies that protect the legal rights of elderly patients. Due to the development of new technologies, the lack of complex talent and the lack of awareness of medical staff about artificial intelligence healthcare service resources technology, data integration and entry is more influenced by human intervention, non-standardized coding and non-standardized writing may result in a higher risk of data leakage.
In addition, the lack of awareness of AI technology in healthcare and the high risk of data leakage are two factors that are not very influential and central, but are at the bottom of the hierarchy. The importance of these two factors cannot be overlooked in the adoption process of medical institutions. As hospital leaders consider the adoption of artificial intelligence healthcare service resources, they should identify the changes in data breach risk and reasonable risk taking. It is also important that hospital staff are trained in AI technology and that the quality of artificial intelligence healthcare service resources is tightly controlled in conjunction with healthcare providers. The underlying factors of the system model are the source of many factors, which in turn are amplified by other factors. It is of practical importance to pay close attention to the underlying factors, the middle factors, and the important factors in the surface factors.
Matrice d’Impacts Croises Multiplication Appliqu and Classement (MICMAC) analysis
The driving force and dependencies of each factor were obtained by summing the elements with the value of 1 in the reachable matrix, as shown in Table 18. The summed values of the driving force of each variable are used as vertical coordinates, the summed values of the dependencies are used as horizontal coordinates, and the mean values of both the dependencies and driving force are used as quadrant dividers to construct the diagram for the MICMAC quadrant analysis, as shown in Figure 5, which has been divided into four quadrants designating the spontaneous, dependent, linkage, and independent factors, respectively.
Table 18.
Values of driving forces and dependencies of resource adoption factors for intelligent healthcare services.
| T1 | T2 | T3 | T4 | T5 | T6 | T7 | O1 | O2 | O3 | O4 | O5 | O6 | E1 | E2 | E3 | E4 | E5 | E6 | E7 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | 0.0200 | 0.1165 | 0.0770 | 0.1615 | 0.0778 | 0.1633 | 0.0233 | 0.0506 | 0.0777 | 0.1667 | 0.0796 | 0.1932 | 0.0354 | 0.1182 | 0.0655 | 0.0497 | 0.0694 | 0.1960 | 0.1547 | 0.0752 |
| T2 | 0.0529 | 0.0446 | 0.0767 | 0.1753 | 0.1487 | 0.1684 | 0.0317 | 0.0478 | 0.0905 | 0.1650 | 0.1636 | 0.2080 | 0.0447 | 0.0489 | 0.0767 | 0.0459 | 0.0778 | 0.2072 | 0.2196 | 0.0981 |
| T3 | 0.0217 | 0.0544 | 0.0459 | 0.1573 | 0.0714 | 0.1564 | 0.0181 | 0.0552 | 0.1737 | 0.1598 | 0.1583 | 0.2180 | 0.0514 | 0.1184 | 0.1392 | 0.0571 | 0.0852 | 0.1910 | 0.2197 | 0.1066 |
| T4 | 0.0220 | 0.0411 | 0.0451 | 0.0821 | 0.1306 | 0.1498 | 0.0172 | 0.0542 | 0.0810 | 0.1499 | 0.0784 | 0.1889 | 0.0396 | 0.0426 | 0.0606 | 0.1149 | 0.1447 | 0.1919 | 0.2063 | 0.0784 |
| T5 | 0.0958 | 0.0429 | 0.0459 | 0.1637 | 0.0546 | 0.1583 | 0.0168 | 0.0538 | 0.1548 | 0.1629 | 0.0839 | 0.2022 | 0.0430 | 0.1161 | 0.0711 | 0.0538 | 0.0895 | 0.1934 | 0.2052 | 0.0964 |
| T6 | 0.0298 | 0.0303 | 0.0443 | 0.1490 | 0.0482 | 0.0668 | 0.0235 | 0.0507 | 0.0695 | 0.1020 | 0.0720 | 0.1753 | 0.0305 | 0.1063 | 0.0603 | 0.0699 | 0.1383 | 0.1717 | 0.1830 | 0.0718 |
| T7 | 0.0449 | 0.0425 | 0.0453 | 0.1696 | 0.1391 | 0.1763 | 0.0172 | 0.0543 | 0.1776 | 0.1690 | 0.0943 | 0.2153 | 0.0624 | 0.0543 | 0.0702 | 0.0850 | 0.0959 | 0.2090 | 0.2347 | 0.1552 |
| O1 | 0.0135 | 0.0338 | 0.0394 | 0.0483 | 0.0341 | 0.0752 | 0.0118 | 0.0407 | 0.1391 | 0.0638 | 0.1457 | 0.1318 | 0.0482 | 0.0327 | 0.0483 | 0.1077 | 0.1339 | 0.0968 | 0.1020 | 0.1532 |
| O2 | 0.0335 | 0.0772 | 0.0533 | 0.0731 | 0.0513 | 0.0935 | 0.0204 | 0.0554 | 0.0887 | 0.1422 | 0.1044 | 0.2077 | 0.1196 | 0.0415 | 0.1459 | 0.0909 | 0.1414 | 0.1055 | 0.2075 | 0.1646 |
| O3 | 0.0190 | 0.0379 | 0.0448 | 0.0598 | 0.0422 | 0.0768 | 0.0323 | 0.1206 | 0.1472 | 0.0584 | 0.1662 | 0.1204 | 0.1271 | 0.0361 | 0.0733 | 0.0946 | 0.1395 | 0.0934 | 0.1732 | 0.1616 |
| O4 | 0.0334 | 0.1284 | 0.0547 | 0.1039 | 0.0660 | 0.1257 | 0.0327 | 0.0506 | 0.1418 | 0.0749 | 0.0937 | 0.2278 | 0.1228 | 0.0516 | 0.1421 | 0.0395 | 0.1511 | 0.2049 | 0.2231 | 0.1679 |
| O5 | 0.0259 | 0.1200 | 0.1141 | 0.1336 | 0.1130 | 0.1471 | 0.0248 | 0.1175 | 0.1452 | 0.0819 | 0.1724 | 0.1461 | 0.0477 | 0.0465 | 0.1420 | 0.0478 | 0.0863 | 0.2155 | 0.2211 | 0.1546 |
| O6 | 0.0650 | 0.0843 | 0.1246 | 0.1422 | 0.1484 | 0.1892 | 0.0995 | 0.0589 | 0.1703 | 0.0980 | 0.1761 | 0.2409 | 0.0522 | 0.0695 | 0.1611 | 0.0526 | 0.0934 | 0.1639 | 0.2421 | 0.1557 |
| E1 | 0.0286 | 0.0427 | 0.1313 | 0.0811 | 0.0489 | 0.0882 | 0.0159 | 0.1360 | 0.1822 | 0.1536 | 0.1174 | 0.2121 | 0.0613 | 0.0414 | 0.1440 | 0.1376 | 0.1169 | 0.1218 | 0.1523 | 0.1898 |
| E2 | 0.0063 | 0.0180 | 0.0217 | 0.0392 | 0.0203 | 0.0327 | 0.0056 | 0.0220 | 0.0426 | 0.0239 | 0.0478 | 0.1217 | 0.0189 | 0.0235 | 0.0243 | 0.0515 | 0.0396 | 0.0414 | 0.0552 | 0.0716 |
| E3 | 0.0328 | 0.0676 | 0.1431 | 0.1474 | 0.1233 | 0.1889 | 0.0273 | 0.1299 | 0.2137 | 0.1787 | 0.2033 | 0.2581 | 0.1482 | 0.1145 | 0.0979 | 0.0650 | 0.1696 | 0.1593 | 0.2677 | 0.2110 |
| E4 | 0.0148 | 0.0308 | 0.1124 | 0.0713 | 0.0411 | 0.1346 | 0.0125 | 0.1299 | 0.0807 | 0.1208 | 0.0839 | 0.1808 | 0.0374 | 0.0327 | 0.0568 | 0.0373 | 0.0581 | 0.1750 | 0.1940 | 0.1503 |
| E5 | 0.0144 | 0.0281 | 0.0194 | 0.1213 | 0.1100 | 0.0590 | 0.0064 | 0.0230 | 0.0411 | 0.0584 | 0.0382 | 0.1309 | 0.0152 | 0.0202 | 0.0265 | 0.0220 | 0.0335 | 0.0611 | 0.1146 | 0.0341 |
| E6 | 0.0276 | 0.0251 | 0.0167 | 0.1204 | 0.0316 | 0.0520 | 0.0073 | 0.0285 | 0.1109 | 0.0396 | 0.1103 | 0.0693 | 0.0264 | 0.0165 | 0.0329 | 0.0248 | 0.0428 | 0.1312 | 0.0682 | 0.0514 |
| E7 | 0.0290 | 0.0430 | 0.0485 | 0.0813 | 0.0506 | 0.1443 | 0.0320 | 0.0496 | 0.1493 | 0.0555 | 0.1524 | 0.1866 | 0.1182 | 0.0321 | 0.0617 | 0.0325 | 0.0612 | 0.1739 | 0.1910 | 0.0716 |
Figure 5.
Matrice dImpacts Croises Multiplication Appliqu and Classement (MICMAC) diagram.
The first quadrant is the Autonomous cluster, whose factors are characterized by low dependency and driving force. Only one factor, Skeptical of AI processing capabilities (T4), is in the middle layer but does play a role in the system. Therefore, an important prerequisite for the adoption of intelligent healthcare service resources by medical institutions is to start with changes in attitudes toward AI processing capabilities and establish correct perceptions of AI healthcare service resources.
The Autonomous cluster has the highest number of vulnerabilities influencing factors, followed by the Independent cluster, and the Linkage cluster has the lowest number of vulnerability influencing factors. This indicates to a certain extent that the degree of correlation between the influencing factors is weak and that it is not possible to control all the influencing factors by controlling a few of them, starting from a single or a few vulnerability influencing factors, so that medical institutions can make rational decisions on the adoption of artificial intelligence healthcare. The study also shows that the impact of a few vulnerability factors on the adoption of artificial intelligence in healthcare services is not always clear.
Autonomous cluster is in the first quadrant, with only one factor, skeptical of AI processing capabilities (T4), in the middle of a multi-layered hierarchical model, which acts as a top and bottom layer for the system. This factor is both driving and dependent, but it is not strongly correlated with the system as a whole or with other factors, suggesting that medical institutions, in adopting the artificial intelligence healthcare service resources factor, are adjusting other factors to strengthen the T4 factor to enable senior leaders of the institution to make decisions about the adoption of artificial intelligence healthcare service resources, the results of which are not applicable. Similarly, strengthening other influencing factors by adjusting the T4 factor did not have the desired effect on the adoption of artificial intelligence healthcare service resources, and both moderation approaches were less significant and effective than moderation of the Independent cluster. For example, T1 factors, due to their specific characteristics, are not as effective as the independent cluster. For example, the T1 factor, due to its specific nature and significance, relies heavily on government policy support, even if it is supported by management leadership. Conversely, government policies to safeguard against data leakage problems require implementation of the policies by management leadership.
The second quadrant is the Dependent cluster, whose factors have high dependency but a low driving force. They are generally located in the upper layers and exert their influences on the lower layers but have difficulty influencing the formation of the other factors. This quadrant includes the factors in the L1, L2, and L3 layers: (L3) System service complexity; (L2) Medically derived risks, Financial Costs, Lack of excellent supplier support, Inability to share information, and Difficult to meet the complex needs of elderly patients; (L1) Competitive pressures, Lack of patient trust, and Lack of excellent partnerships. L1, L2, and L3 are dependent on the influence degrees of the bottom layer, which coincides with the high dependence of the second quadrant.
The third quadrant is the Linkage cluster, whose factors have a high dependency and driving force. They are located in the L4 of the multilayered recursive structural model: AI infrastructure synergy, Lack of ability to read structured medical data, Hospital size, Lack of complex talent, Geographical restrictions, and Unclear ownership of hospitals. Changes in these six factors cause linkage changes in the other factors, whereas the factors in L3 depend on the explanations for those in L4, thus demonstrating that system service complexity is influenced by L4, where the Lack of ability to read structured medical data and AI infrastructure synergy is more directly related to the explanatory influences of system service complexity.
The fourth quadrant is the Independent cluster, whose factors have low dependency but high driving force. They are located in the bottom layers, so they are the fundamental factors of the whole system: (L7) Lack of awareness of the value and benefits of AI healthcare technology; (L6) High risk of data leakage; (L5) Lack of management leadership support and Government policies. Moreover, they have the highest driving forces, so they would have long-lasting impacts on the system.
Discussion and implication
Discussion
This paper investigates the analysis and strategies of influencing factors for the adoption of artificial intelligence healthcare service resources in medical institutions and describes how the three combined DEMATEL-ISM-MICMAC approaches can be applied to the adoption of this paper presents the application of the DEMATEL-ISM-MICMAC approach to the adoption of artificial intelligence healthcare service resources. Firstly, the theories of the two main approaches, DEAMTEL and ISM, are explained, the advantages and adaptability of each approach are presented, and the idea of constructing a DEMATEL-ISM model is proposed. Based on this research, the influencing factors of medical institutions’ adoption are constructed and analyzed, and a system of influencing factors of artificial intelligence healthcare service resources is formed. The study answers the “what,” “how,” and “why” of the theoretical construction. 57 Answer the “what” for the factors adopted for artificial intelligence healthcare service resources, the “how” for the relationships between the factors and the “why” for the relationships between the factors. The explanation of the relationship between the factors answers the question “why.” The study identifies a hierarchy of associations between these factors. This paper contributes to the adoption choices of hospitals and elderly care facilities. This study can also help management leaders to understand the DEMATEL-ISM-MICMAC approach and help them to apply the three combined approaches in different scenarios to make adoption decisions. The DEMATEL-ISM-MICMAC method identifies the type of inter-factor (autonomous, dependent, linkage, or independent) as well as the inter-relationship between factors and the interpretation of the inter-relationship. Understanding the factors influencing the adoption of artificial intelligence healthcare service resources will help managers and policy makers to develop and design strategies to adjust the strength of these factors in the context of the combination of medical and health care and to improve the competitiveness of intelligent medical institutions’ competitiveness. Managers and policy makers need to focus on lower level or independent factors such as lake of management leadership support, government policies, high risk of data leakage and lack of awareness of the value and benefits of healthcare AI technology. Therefore, practitioners in the retirement industry can priorities factors at the hierarchical level. Improving these factors could lead to the successful adoption of artificial intelligence healthcare service resources in hospitals and nursing homes. The main findings and conclusions of this paper are categorized and analyzed here.
(1) Project adopter (medical institutions)
During the adoption phase, medical institutions, as the initiator and responsible person for the project, must carry out a preliminary survey and feasibility study of the project and analyses the adoption factors. Once the project has been decided, the implementation of the factors considered is left to the supplier. Whether it is a hospital, a nursing home or a medical institution, the entire project is carried out. From the previous analysis of the 20 factors for the adoption of smart healthcare resources, the following six factors were identified as being closely linked to the sponsor: lack of awareness of the value and benefits of AI healthcare technology (T5), medically derived risks (T6), lack of ability to read structured medical data (T7), hospital size (O2), lack of complex talent (O6), and competitive pressures (E2). For each of these adoptions factor the following summary was made.
① Lack of awareness of the value and benefits of AI healthcare technology (T5): The lack of awareness of the advantages of healthcare information technology has led to a greater influence of human intervention in the sourcing, recording and integration of healthcare data, and the lack of AI healthcare information industry the T5 factor, with a causality of 0.5528 > 0, is the causality factor in the whole system. It is the most fundamental and deepest influencing factor in the whole adoption system, and it will affect the upper layers of the whole structural model in the long term, so it is an important factor that cannot be ignored by medical institutions when adopting artificial intelligence healthcare service resources. Therefore, it is such an important factor for medical institutions to adopt artificial intelligence healthcare service resources. Therefore, the adoption of artificial intelligence healthcare service resources by medical institutions is proposed to be addressed in the following ways.
Firstly, the healthcare information industry should develop industry standards related to data input, storage and output, and refine the standards to suit different scenarios.
Secondly, hospitals, nursing homes and medical institutions should focus on giving medical staff training in intelligent information systems, strengthening their intellectual literacy and entering data in strict accordance with standards.
Finally, government policy should encourage the development of smart healthcare. For example, the government should provide incentives in the form of procurement subsidies or tax breaks for organizations that adopt smart healthcare resources.
② Medically derived risks (T6): This factor is ranked eighth in centrality, with a cause degree of 0.7534 < 0, indicating that it is an outcome factor and is closely related to other influencing factors. As can be seen from the ISM model, the T6 factor is in the second tier and is one of the factors directly influencing the whole adoption system. It is also directly influenced by the system service complexity (T2). As smart healthcare systems test system hardware and technician expertize tremendously, they inevitably cause doctors to operate improperly and medical risks to arise. Therefore, medical technicians should improve their information technology expertize to avoid medical risks to patients.
③ Lack of ability to read structured medical data (T7): Medical technicians lack the ability to transform unstructured data in medical records, images and test reports into structured data that can be read by artificial intelligence. This factor is ranked 18th in centrality and 3rd in influence, with a causality of 1.8359 > 0, indicating that it is a causal factor and is quite closely related to other factors in the system, not only being influenced by other factors, but also influencing them. As can be seen from the ISM model, T7 factor is in the 4th layer, which is the middle layer, and the factor carries on from the top to the bottom, proving that the ISM method and DEMATEL method results tend to be consistent. In the MICMAC model, T7 factor is in the third quadrant of the Linkage cluster, and the elements in this quadrant are linkage factors, and the results are again consistent with the results of the DEMATEL and ISM methods. Therefore, in addition to their medical expertize, doctors should also develop the ability to read informative, unstructured data.
④ Hospital size (O2): Hospital size is determined by the number of registered beds, with more beds indicating greater patient demand and a higher need to introduce smart healthcare services. This factor is ranked fourth in centrality and 10th in influence. The reason degree value of 0.4600 < 0 indicates that this factor is an outcome factor and has a high centrality ranking and a median influence degree ranking, indicating that this factor is closely linked to all other factors. According to the ISM model, O2 factor is in the fourth tier, which is the middle tier, connecting the upper and lower tier factors which proving that the ISM method is consistent with the DEMATEL method. Therefore, medical institutions should adopt artificial intelligence healthcare service resources that are appropriate for their number of beds and their size.
⑤ Lack of complex talent (O6): Due to the late start of information technology construction in China, most doctors only focus on their specialties and have less exposure to artificial intelligence and information technology knowledge, resulting in the homogenization of talents. This factor ranks second in terms of influence, with a cause degree value of 1.3377 > 0, indicating that this factor is a cause factor and is closely linked to other factors. The O6 factor is in the third quadrant of the linkage cluster in the MICMAC model, which again demonstrates the reliability of the data and the consistency of the findings of the three methods. Therefore, the government and medical institutions should vigorously support the information technology training system and strengthen the training of complex talents.
⑥ Competitive pressures (E2): Due to the large upfront investment of medical institutions and the long experimental process required for artificial intelligence healthcare service resources in the early stages of operation, the supply of services cannot effectively cover the cost investment due to peer competition pressure. This factor is ranked 20th in terms of influence, indicating that this factor has less influence on other factors but is influenced by them. The ISM model shows that this factor is in the first tier, and that the first tier is influenced and constrained by the lower tier factors. And the factor has a cause degree value of 0.9728 < 0, indicating that the factor is an outcome, which is exactly in line with the findings of the ISM model. The results in the MICMAC model indicate that the factor is in the Dependent cluster, which is consistent with the conclusion that the factor is in the first tier of the ISM and has less influence on other factors. Therefore, competitive pressures are the most direct factor affecting the system, and it is recommended that medical institutions managers, when faced with competitive pressures, should take account of the situation and adopt artificial intelligence healthcare service resources in a way. It is recommended that medical institutions managers should consider the needs of patients when adopting artificial intelligence healthcare service resources in order to ensure a competitive advantage.
(2) Government sector
Government sector have an important role to play in the overall adoption of artificial intelligence healthcare service resources, and the factors associated with government units are lack of management leadership support (O1), financial costs (O3), government policies (E1), and unclear ownership of hospitals (E4).
The O1 factor is influenced by the E1 factor, which according to the results of DEMATEL has a cause degree value of 0.1705 > 0 for O1 factor and a cause degree value of 1.0393 > 0 for E1 factor, with both factors being cause factors. According to the results of the ISM model, both the O1 factor and the E1 factor have an impact on unclear ownership of hospitals (E4), which is consistent with the finding that both the O1 factor and the E1 factor are causal factors in DEMATEL. In addition to this, the O1 and E1 factors are both located in layer 5 of the ISM model and are bottom factors, which are fundamental to the artificial intelligence healthcare service resources system and will continue to influence the factors in the upper layers of the structural model over time. According to the DEMATEL results, the O3 factor has a cause degree value of 0.4004 < 0, which is the outcome factor. And the centrality ranking is 10th, indicating that the factor is not closely related to other factors, while according to the results of the ISM structural model, the factor is in the second tier and is more influenced by the lower tier factors, indicating that the DEMATEL results and the ISM results remain consistent.
In summary, these four factors in the adoption of artificial intelligence healthcare service resources require a lot of human and material resources, which in turn directly affects human and material resources, and problems with any one of these factors can cause difficulties in the adoption process. The factor of government departments is directly related to the motivation, coordination and cooperation of this adoption act. Therefore, government departments should do a good job of promoting science and technology and guiding leaders’ awareness of AI adoption from an ideological point of view. Secondly, the government should introduce rules for the allocation of financial incentives, such as adoption, which should be directly linked to incentive funding. In order to increase the motivation and cooperation of medical institutions’ leaders in the project implementation process. Finally, a monitoring system should be established during the adoption process in medical institutions, with regular third-party safety checks and operational maintenance to ensure the long-term efficient operation of artificial intelligence healthcare service resources.
(3) Suppliers: Suppliers, like government entities, play a crucial role in the success of a project. Factors related to suppliers are: unclear ownership of hospitals (T1), system service complexity (T2), AI infrastructure synergy (T3), lack of excellent supplier support (O4), inability to share information (O5), and lack of excellent partnerships (E7). According to the ISM model, the O5 factor is in the second quadrant and is not only influenced by the system service complexity (T2) in the third quadrant, but also directly affects the Competitive pressures (E2). This finding is consistent with the findings of the DEMATEL and ISM methods. In summary, the factors associated with suppliers are all negative and have a high degree of risk. The above factors give the supplier a significant influence on the supply lead time, the quality of equipment build and materials and the effectiveness of the use of artificial intelligence healthcare service resources.
Therefore, as a supplier of artificial intelligence healthcare service resources, you should consider the risks of adoption comprehensively, avoid contractual loopholes when signing procurement contracts with medical institutions, and both parties need to strictly follow the contract. In the adoption process, the quality of products should be strictly controlled, the production, delivery and entry of intelligent products should be communicated with medical institutions in a timely manner. The control policies of the region in recent years should be collected and prepared in advance, etc.
(4) Older patients: older patient subjects play an important role in the overall adoption system in terms of evaluation and monitoring. Factors related to elderly patient subjects include: skeptical of AI processing capabilities (T4), geographical restrictions (E3), lack of patient trust (E5), difficult to meet complex needs of elderly patients (E6). All four of these factors are negative and have a high level of risk. This suggests that the pressure of risk in the adoption process by medical institutions is ultimately exerted on patients. Therefore, it is recommended that medical institutions, providers, and the government actively communicate with elderly patients, adhere to professional ethics and gain relevant experience. In order to protect the rights and interests of elderly patients, it is recommended that medical institutions select highly qualified and skilled companies to undertake third-party quality assessments in the adoption of artificial intelligence healthcare service resources. It is also recommended that government departments strengthen the management of information technology, competence training and technological assessment of medical institutions.
Theoretical implications
DEMATEL, ISM, and MICMAC were used to stratify the factors influencing the adoption of intelligent healthcare services in medical and healthcare contractual medical institutions from the outer layer to the root, from the surface to the deep layers, and from the surface layer to the substance. The influencing factors were screened according to the pre-test results of questionnaires administered to 10 experts and 20 influencing factors were identified according to the TOE framework. Then, the formal questionnaire was administered to the experts, who scored the 20 factors from 0 to 4 to form the direct influence matrix, and the macro-level analysis of the influencing factors of the adoption of regimen services was conducted by the DEMATEL method to analyze the degrees of influence, being influenced, and centrality. The recursive structural model was established by the ISM method to intuitively explain the hierarchical relationships and directionality of the influencing factors, which are the root of the structure. The MICMAC graphical method was used to cluster and summarize the factors in order to explain the deeper substance of the structure.
First, the DEMATEL causal diagram shows high risk of data leakage (T1), lack of awareness of the value and benefits of AI healthcare technology (T5), lack of management leadership support (O1), and government policies (E1) to be the causal factors without subdividing the causal substance. These factors are at the bottom layers in the ISM recursive structural model, thus indicating them to be the root causes. Their classification into the fourth quadrant of the MICMAC diagram places them in the Independent cluster, which has low dependency but high driving force, thus aptly explaining why the bottom factors do not depend on the influences of other factors but do exert influences on the top factors. The consistency among the results of these three methods in identifying the root causes, divisions, structures, and natures further illustrate the advantages of combining these three methods.
Second, the ISM recursive structural model is divided into seven layers with the core middle layer as the fourth layer, which contains the factors, AI infrastructure synergy (T3), lack of ability to read structured medical data (T7), hospital size (O2), lack of complex talent (O6), geographical restrictions (E3), and unclear ownership of hospitals (E4). E3 and O2 interact with each other. Both are dependent on the influences of the lower-level factors while influencing the upper-level factors. E3 and O2 have the typical property of forming a connecting link between the preceding and the following factors. In the DEMATEL analysis and causality diagram, both positive causal factors and negative result factors are involved. They are located in the third quadrant of the MICMAC quadrant diagram and belong to the linkage family, which conforms to the characteristics of high dependence and high driving force, thus again verifying the validity and correctness of combining the three methods.
Third, the top layer of the ISM recursive model contains competitive pressures (E2), lack of patient trust (E5), and lack of excellent partnerships (E7), which are the three most direct factors and depend heavily on the influencing factors in the other six layers but are unable to influence the other factors. This outcome is consistent with the negative causality of these three factors in the DEMATEL causal diagram. The MICMAC diagram shows these three factors in the second quadrant, which is the Dependent cluster with high dependency but low driving force. This result also supports the robustness of these three methods.
Practical implications
Our findings can provide strong recommendations to government departments, senior management in healthcare organizations, and elderly care associations. The provision of intelligent healthcare services in the contractual model of medical and nursing services for elderly care is dependent on the government’s investments in people, materials, and information. Government departments should increase industrial support, strengthen multi-industry communication and cooperation, deepen the knowledge of intelligent construction in the elderly care industry, and accelerate the formulation of intelligent policies. With the continuous improvement of policies on China’s elderly service system, the reform of public elderly care institutions, the standardization of elderly services, and a unified pension insurance system, the government can support the adoption of intelligent elderly services by the following measures.
Increase policy subsidies on the demand side and capitation to improve the elderly’s ability to pay.
Accelerate the entry of social capital and strengthen the role of financial funds to guide the construction of elderly care institutions.
Guide “to capacity,” reasonably promote mergers and acquisitions, promote chain operations, and give full play to the scale effect.
Introduce excellent AI providers with high professionalism into medical institutions.
Encourage cooperation between public medical institutions and elderly care institutions, as well as implement and subsidize public and private elderly care pilot programs.
Coordinate port compatibility issues among suppliers and develop technological specification rules for AI healthcare services.
The managers of the medical institutions are the actual decision-makers for the adoption of intelligent healthcare services, so the knowledge system of senior management should keep up with the times and be forward-looking to ensure correct decisions. The following measures could be taken.
Cultivate people who have high-level medical and IT talent, as well as who understand how to use both healthcare and AI to meet the full range of the needs of the elderly.
Use accurate price positioning in a city according to its size and level of economic development in order to set the appropriate prices that ensure the normal flow of beds and avoid high vacancy rates.
Improve the treatment of healthcare workers and provide a diverse range of services for the elderly.
Establish a sound training system for nursing staff within the healthcare institutions and control staff turnover costs.
Third, elderly care associations should explore in depth the quality of life for the elderly in the following ways
Strengthen the supply of beds in the major cities, protect public service resources in suburban institutions, coordinate the ratios of urban and suburban contracted elderly care institutions to medical care institutions, and deepen the role of public elderly care institutions.
Guide the decapacitation, merging, and reorganizing of small and medium-sized elderly care institutions, promote chain operations, give full play to the scale effect, and increase the integration of elderly care institutions.
Industry associations should establish a reserve of deans and nursing staff to provide “respite care” to deans or nursing staff in training.
Encourage large elderly care institutions to develop nurse training businesses to promote the overall level of human resources in the elderly care industry.
Encourage universities, vocational and technological schools, and third-party institutions to open geriatric management and nursing programs, as well as provide full-time, adult, and distance learning methods to effectively increase the number of management and nursing staff.
Standardize the key terms of medical care integration and move from agreement to real services.
Chain and alliance-type operations should help to gradually raise the income levels of medical and nursing care, as well as establish promotional channels.
Conclusion
AI healthcare service resources is the most promising model of intelligent healthcare services at present and in the future. With the hospital as the main body, through the Internet of Things, 5G communication technology and other information technology means to link patients, medical and nursing staff, drug dealers, pharmaceutical companies, medical insurance institutions and other stakeholders, integration of hospital equipment, medical supplies, pharmaceutical supplies, and other upstream and downstream resources to provide doctors and patients with a variety of types of decision support services.
Consequently, by constructing a model of adoption of artificial intelligence healthcare service resources in medical institutions, this paper reveals that lack of awareness of value and benefits of AI (T5), high risk of data leakage (T1), lack of management leadership support (O1), government policies (E1) are the underlying factors for the adoption of artificial intelligence healthcare service resources in medical institutions. Competitive pressures (E2), lack of patient trust (E5), lack of excellent partnerships (E7) environmental factors are direct factors influencing adoption decisions at different levels of healthcare institutions. Due to the difficulty of obtaining research data, previous studies have generally explored the adoption of artificial intelligence healthcare service resources in a qualitative manner. In this study, the “how” of the relationship between factors was constructed through expert panels and the DEMATEL method. A clear hierarchy of influencing factors was developed through the ISM method to answer the “why,” and the MICMAC method was used to develop clustering relationships between factors to answer the “how.” The paper reveals the mechanisms underlying the influence of technological, organizational, and environmental factors on the adoption of medical institutions. From a theoretical perspective, the findings in this chapter contribute to the current understanding of the decision-making process of organizational behavior. From a content perspective, the use of a combined DEMATEL-ISM-MICMAC approach to constructing artificial intelligence healthcare service resources adoption problems using a pensions perspective as a context is currently a gap in academia.58–64,47,65–77 Most studies have focused on the ISM-MICMAC approach to constructing explanatory models without answering the relationships within the factors from a micro perspective, which is an incomplete study for constructing models with a large number of factors. From a contextual perspective, the context of research using a combination of the three DEMATEL-ISM-MICMAC methods is still a gap in the healthcare and elderly care field. The main research findings are as follows.
First, healthcare providers are more concerned with technological and environmental factors when deciding to adopt AI service resources. This finding is consistent with Ahmadi Hossein. 28
Second, a micro-level analysis using the DEMATEL method of the strengths of the interconnectedness of the factors and the sharp distinctions made in the system for the directionality of each factor revealed that the largest centrality value belonged to inability to share information (O5), indicating this to be the most constraining and closely linked factor.
Third, by stratifying each factor from shallow to deep at the macro-level, analyzing the logical relationships of the mutual influences of the hierarchical relationships between the influencing factors, and constructing a multilayer recursive structural model conceptual diagram, the ISM method found lack of awareness of the value and benefits of AI healthcare technology (T5) to be the most fundamental and strongest influencing factor, which affects the upper-level factors of the whole structural model for a long time. Thus, this factor is the most non-negligible factor when medical institutions decide to adopt intelligent healthcare service resources.
Fourth, the results of the DEMATEL-ISM analysis were further differentiated by the MICMAC method to obtain values for the driving forces and dependencies of each factor in order to categorize it into one of four quadrants. The findings are as follows.
(1) The deep-seated factors that influence healthcare organizations to adopt AI healthcare service resources are high risk of data leakage (T1), lack of awareness of the value and benefits of AI healthcare technology (T5), lack of management leadership support (O1), and government policies (E1), which are located in the bottom three levels of the directed graph and in the fourth quadrant of the Independent cluster in the MICMAC diagram shown in Figure 5.
(2) The most direct factors influencing healthcare organizations to adopt AI resources for wellness services are competitive pressures (E2), lack of patient trust (E5), and lack of excellent partnerships (E7), which are all located at the top level of the multilayer recursive structural model and in the second quadrant. These factors have high dependency but low driving force, thus verifying that the MICMAC’s results are consistent with the ISM’s results. The factors in the third quadrant are linkage-type factors, which have both high dependency on the influence of lower-level factors in the recursive structural model and high driving force exerting strong influences on the upper-level factors in the ISM model. Thus, coinciding with such factors being located in the middle levels of the recursive structural model. These factors play roles in the structure of the upper and lower levels, indicating again that the ISM’s results coincide with the MICMAC’s results to reinforce the high reliability and validity of the model.
Limitations and future work
In addition to discussing some key factors in the adoption of AI healthcare service resources, there are limitations to the study. Firstly, feedback from customers (elderly patients) and feedback from providers were not considered as variables to be considered. The real-life perceptions of elderly patients could help medical institutions to better improve the quality of care, while helping AI healthcare service providers to target and improve their service offerings. Furthermore, the subjectivity involved in collating the data from tools such as literature review and expert scoring to derive the 20 adoption factors in this study becomes one of the limitations of the existing research work. Although this study used a literature review to identify a broad range of factors and used expert scoring to finalize the 20 factors, the study was unable to identify all factors for the adoption of AI healthcare service resources by medical institutions. Furthermore, in the Organizational dimension, the factors hospital size, financial costs, and government policies are subject to change due to government influence. Therefore, these 20 factors will change over time.
As the data used in this study was derived through expert scoring, it is consistent with the source of data used in the empirical analysis. Therefore, future research could use Exploratory Factor Analysis (EFA) to find the number of factors for multiple variables. The correlation between each factor and each variable is then reduced in order to attempt to reveal the intrinsic structure of a relatively large set of variables. Subsequently, to validate the structure, confirmatory factor analysis (CFA) can be used to verify the soundness of the proposed framework. The methodology uses partial least squares structural equations to build an explanatory structural model (PLS-SEM) designed to establish the explanatory variance of the maximized potential variables. In addition to this, the reliability of the collected data is assessed based on the measurement model characteristics. Scholars can use qualitative methods to validate the relationships that have been established. They can include variables that were omitted or not included in the study, creating new relationships based on their research context. Scholars can explore new variables using bibliometric methods or meta-analysis. These new variables are used to construct conceptual frameworks. Interrelationships between variables can be tested using geographical restrictions (E3) and hospital size (O2). Future researchers are also encouraged to use m-TISM as a simpler and more convenient way of constructing structural explanatory models to validate their results and findings if there are fewer variables, the field of study is well established and the relevant literature is extensive.78–93
Acknowledgements
We would like to thank Mogo Edit for their assistance with polish language in this research.
Footnotes
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
Ethical approval: The experimental protocol was designed according to the ethical guidelines of the Helsinki Declaration. Ethical permissions were granted by the Human Ethics Committee of the Anhui Chinese Medical University (no. 2021-ACM026). Written informed consents were obtained from doctors.
Funding: This study was funded by the Influence Mechanism of Social Network Structures on the Diffusion of Green Consumption Behavior (grant no. 21YJA630066) and the NSFC Basic Science Center Project (grant no. 72188101).
Guarantor: Biao Luo
ORCID iD: Biao Luo https://orcid.org/0000-0002-2276-0954
References
- 1. Nations U. World Population Aging: 1950-2050. United Nations, Department of Economic and Social Affairs, Population Division. 2013, http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.
- 2.Weil DN. The economics of population aging. Handbook of Population and Family Economics 1997; 1, part b: 967–1014. [Google Scholar]
- 3.Tornatzky LG, Fleischer M, Chakrabarti AK. Processes of technological innovation. Lexington, MA: Lexington Books, 1990. [Google Scholar]
- 4.Lee K, Jung SY, Hwang H. et al. A novel concept for integrating and delivering health information using a comprehensive digital dashboard: An analysis of healthcare professionals’ intention to adopt a new system and the trend of its real usage. Int J Med Inform 2017; 97: 98–108. [DOI] [PubMed] [Google Scholar]
- 5.Kuan KK, Chau PY. A perception-based model for edi adoption in small businesses using a technology–organization–environment framework. Inform Manag 2001; 38: 507–521. [Google Scholar]
- 6.Mishra AN, Konana P, Barua A. Antecedents and consequences of internet use in procurement: An empirical investigation of us manufacturing firms. Inf Syst Res 2007; 18: 103–120. [Google Scholar]
- 7.Zhu K, Kraemer KL, Dedrick J. Information technology payoff in e-business environments: An international perspective on value creation of e-business in the financial services industry. J Manage Inf Syst 2004; 21: 17–54. [Google Scholar]
- 8.Zhu K, Kraemer KL, Xu S. The process of innovation assimilation by firms in different countries: A technology diffusion perspective on e-business. Manage Sci 2006; 52: 1557–1576. [Google Scholar]
- 9.Zhu K, Kraemer K, Xu S. Electronic business adoption by European firms: A cross-country assessment of the facilitators and inhibitors. Eur J Inf Syst 2003; 12: 251–268. [Google Scholar]
- 10.Chang IC, Hwang HG, Hung MC. et al. Factors affecting the adoption of electronic signature: Executives’ perspective of hospital information department. Decis Support Syst 2007; 44: 350–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang IC, Hwang HG, Yen DC. et al. Critical factors for adopting pacs in taiwan: Views of radiology department directors. Decis Support Syst 2006; 42: 1042–1053. [Google Scholar]
- 12.Hsiao SJ, Li YC, Chen YL. et al. Critical factors for the adoption of mobile nursing information systems in taiwan: The nursing department administrators’ perspective. J Med Syst 2009; 33: 369–377. [DOI] [PubMed] [Google Scholar]
- 13.Kazley AS, Ozcan YA. Organizational and environmental determinants of hospital emr adoption: A national study. J Med Syst 2007; 31: 375–384. [DOI] [PubMed] [Google Scholar]
- 14.Lee CP, Shim JP. An exploratory study of radio frequency identification (rfid) adoption in the healthcare industry. Eur J Inf Syst 2007; 16: 712–724. [Google Scholar]
- 15.Lin CH, Lin IC, Roan JS. et al. Critical factors influencing hospitals’ adoption of hl7 version 2 standards: An empirical investigation. J Med Syst 2012; 36: 1183–1192. [DOI] [PubMed] [Google Scholar]
- 16.Yang Z, Kankanhalli A, Ng BY. et al. Analyzing the enabling factors for the organizational decision to adopt healthcare information systems. Decis Support Syst 2013; 55: 764–776. [Google Scholar]
- 17.Zhu K, Kraemer KL. Post-adoption variations in usage and value of e-business by organizations: Cross-country evidence from the retail industry. Inf Syst Res 2005; 16: 61–84. [Google Scholar]
- 18.Chong AYL, Chan FT. Structural equation modeling for multi-stage analysis on radio frequency identification (rfid) diffusion in the health care industry. Expert Syst Appl 2012; 39: 8645–8654. [Google Scholar]
- 19.Tsagaankhuu S, Zhang X, Ayush EA. Characteristics of hospitals that adopt hospital information systems in mongolia and its impact on patient safety and quality of care. Central Asian Journal of Medical Sciences 2018; 4: 116–125. [Google Scholar]
- 20.Bradford M, Florin J. Examining the role of innovation diffusion factors on the implementation success of enterprise resource planning systems. Int J Account Inf Syst 2003; 4: 205–225. [Google Scholar]
- 21.Chen KL. Web-based electronic medical record (emr) systems: Challenges and solutions. Int J Healthc Technol Manag 2001; 3: 444–457. [Google Scholar]
- 22.Wang BB, Wan TT, Burke DE. et al. Factors influencing health information system adoption in american hospitals. Health Care Manage Rev 2005; 30: 44–51. [DOI] [PubMed] [Google Scholar]
- 23.Zheng K, Padman R, Krackhardt D. et al. Social networks and physician adoption of electronic health records: Insights from an empirical study. J Am Med Inform Assoc 2010; 17: 328–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Callaway B. The diffusion of health information technology: Practice characteristics and competition as drivers of adoption. PhD Thesis, Georgia Institute of Technology, 2010.
- 25.Lian JW, Yen DC, Wang YT. An exploratory study to understand the critical factors affecting the decision to adopt cloud computing in Taiwan hospital. Int J Inf Manage 2014; 34: 28–36. [Google Scholar]
- 26.Liu CF. Key factors influencing the intention of telecare adoption: An institutional perspective. Telemedicine and e-Health 2011; 17: 288–293. [DOI] [PubMed] [Google Scholar]
- 27.Hung SY, Hung WH, Tsai CA. et al. Critical factors of hospital adoption on crm system: Organizational and information system perspectives. Decis Support Syst 2010; 48: 592–603. [Google Scholar]
- 28.Ahmadi H, Nilashi M, Ibrahim O. Organizational decision to adopt hospital information system: An empirical investigation in the case of malaysian public hospitals. Int J Med Inform 2015; 84: 166–188. [DOI] [PubMed] [Google Scholar]
- 29.Greenberg D, Peterburg Y, Vekstein D. et al. Decisions to adopt new technologies at the hospital level: Insights from Israeli medical centers. Int J Technol Assess Health Care 2005; 21: 219–227. [PubMed] [Google Scholar]
- 30.Asagbra OE, Burke D, Liang H. Why hospitals adopt patient engagement functionalities at different speeds? A moderated trend analysis. Int J Med Inform 2018; 111: 123–130. [DOI] [PubMed] [Google Scholar]
- 31.Young GJ, Charns MP, Shortell SM. Top manager and network effects on the adoption of innovative management practices: A study of TQM in a public hospital system. Strateg Manage J 2001; 22: 935–951. [Google Scholar]
- 32.Chen YH, Liu CF, Hwang HG. Key factors affecting healthcare professionals to adopt knowledge management: The case of infection control departments of Taiwanese hospitals. Expert Syst Appl 2011; 38: 450–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alam MGR, Masum AKM, Beh LS. et al. Critical factors influencing decision to adopt human resource information system (HRIS) in hospitals. PLoS ONE 2016; 11: e0160366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fan W, Liu J, Zhu S. et al. Investigating the impacting factors for the healthcare professionals to adopt artificial intelligence-based medical diagnosis support system (aimdss). Ann Oper Res 2020; 294: 567–592. [Google Scholar]
- 35.Hoque MR. An empirical study of mhealth adoption in a developing country: The moderating effect of gender concern. BMC Med Inform Decis Mak 2016; 16: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu L, Li JY, Fu CY. The adoption of mobile healthcare by hospital’s professionals: An integrative perspective. Decis Support Syst 2011; 51: 587–596. [Google Scholar]
- 37.Kijsanayotin B, Pannarunothai S, Speedie SM. Factors influencing health information technology adoption in thailand’s community health centers: Applying the utaut model. Int J Med Inform 2009; 78: 404–416. [DOI] [PubMed] [Google Scholar]
- 38.Faber S, van Geenhuizen M, de Reuver M. ehealth adoption factors in medical hospitals: A focus on the Netherlands. Int J Med Inform 2017; 100: 77–89. [DOI] [PubMed] [Google Scholar]
- 39.Tortorella GL, Fogliatto FS, Espôsto KF. et al. Effects of contingencies on healthcare 4.0 technologies adoption and barriers in emerging economies. Technol Forecast Soc Change 2020; 156: 120048. [Google Scholar]
- 40.Tortorella GL, Fogliatto FS, Espôsto KF. et al. Measuring the effect of Healthcare 4.0 implementation on hospitals’ performance. Prod. Plan. Control 2022; 33: 386-401. [Google Scholar]
- 41.Sun TQ, Medaglia R. Mapping the challenges of artificial intelligence in the public sector: Evidence from public healthcare. Gov Inf Q 2019; 36: 368–383. [Google Scholar]
- 42.Mardani A, Saraji MK, Mishra AR. et al. A novel extended approach under hesitant fuzzy sets to design a framework for assessing the key challenges of digital health interventions adoption during the COVID-19 outbreak. Appl Soft Comput 2020; 96: 106613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xing F, Peng G, Zhang B. et al. Socio-technical barriers affecting large-scale deployment of ai-enabled wearable medical devices among the ageing population in China. Technol Forecast Soc Change 2021; 166: 120609. [Google Scholar]
- 44.Ananthanarayanan R, Sharma J, Jehanno N. et al. Study of barriers to the advancement of CNC machining in view of FIJI manufacturing industry using hybrid MCDA approach. J Multi-Criteria Decis Anal 2020; 27: 224–235. [Google Scholar]
- 45.Warfield JN. Societal systems planning, policy and complexity. Cybern Syst 1978; 8: 113–115. [Google Scholar]
- 46.Khan MI, Khan S, Khan U. et al. Modeling the Big Data challenges in context of smart cities—An integrated fuzzy ISM-DEMATEL approach. Int J Build Pathol Adapt 2021. ahead-of-print. DOI: 10.1108/IJBPA-02-2021-0027. [DOI] [Google Scholar]
- 47.Liang Y, Wang H, Zhao X. Analysis of factors affecting economic operation of electric vehicle charging station based on dematel-ism. Comput Ind Eng 2022; 163: 107818. [Google Scholar]
- 48.Song W, Zhu Y, Zhao Q. Analyzing barriers for adopting sustainable online consumption: A rough hierarchical dematel method. Comput Ind Eng 2020; 140: 106279. [Google Scholar]
- 49.Vishnu CR, Sridharan R, Kumar PR. et al. Analysis of the operational risk factors in public hospitals in an Indian state. Int J Health Care Qual Assur 2020; 33: 67–88. [DOI] [PubMed] [Google Scholar]
- 50.Gille F, Jobin A, Ienca M. What we talk about when we talk about trust: Theory of trust for AI in healthcare. Intelligence-Based Medicine 2020; 1: 100001. [Google Scholar]
- 51.von Eschenbach WJ. Transparency and the black box problem: Why we do not trust AI. Philos Technol 2021; 34: 1607–1622. [Google Scholar]
- 52.Noor P. Can we trust AI not to further embed racial bias and prejudice? BMJ 2020; 368: m363. [DOI] [PubMed] [Google Scholar]
- 53.Yousefzadeh R, Cao X. To what extent should we trust AI models when they extrapolate? arXiv preprint arXiv:220111260 2022.
- 54.Hatherley JJ. Limits of trust in medical AI. J Med Ethics 2020; 46: 478–481. [DOI] [PubMed] [Google Scholar]
- 55.Christin A. The ethnographer and the algorithm: Beyond the black box. Theory Soc 2020; 49: 897–918. [Google Scholar]
- 56.Guanyan. China smart medical industry analysis report 2021, 2021.
- 57.Sushil. Interpreting the interpretive structural model. Global J Flex Syst Manage 2012; 13: 87–106. [Google Scholar]
- 58.Priya SS, Priya MS, Jain V. et al. An assessment of government measures in combatting COVID-19 using ism and dematel modelling. Benchmarking: Int J 2022; 29: 1429–1451. [Google Scholar]
- 59.Chen JK. Improved dematel-ism integration approach for complex systems. PLoS ONE 2021; 16: e0254694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen P, Cai B, Wu M. et al. Obstacle analysis of application of blockchain technology in power data trading based on improved dematel-ism method under fuzzy environment. Energy Reports 2022; 8: 4589–4607. [Google Scholar]
- 61.De-cheng F, Xiao-mei GU. Study on health evaluation and key influencing factors of technology innovation ecosystem in high-tech industries: based on the improved entropy weight-dematel-ism method. Oper Res Manage Sci 2021; 30: 167. [Google Scholar]
- 62.He Y, Kang J, Pei Y. et al. Research on influencing factors of fuel consumption on superhighway based on dematel-ism model. Energy Policy 2021; 158: 112545. [Google Scholar]
- 63.Kumar A, Dixit G. An analysis of barriers affecting the implementation of e-waste management practices in India: A novel ism-dematel approach. Sust Prod Consumption 2018; 14: 36–52. [Google Scholar]
- 64.Li F, Wang W, Dubljevic S. et al. Analysis on accident-causing factors of urban buried gas pipeline network by combining dematel, ism and bn methods. J Loss Prev Process Ind 2019; 61: 49–57. [Google Scholar]
- 65.Manoharan S, Pulimi VSK, Kabir G. et al. Contextual relationships among drivers and barriers to circular economy: An integrated ism and dematel approach. Sust Oper Comput 2022; 3: 43–53. [Google Scholar]
- 66.Meng B, Lu N, Lin C. et al. Study on the influencing factors of the flight crew’s tsa based on dematel-ism method. Cogn Technol Work 2022; 24: 275–289. [Google Scholar]
- 67.Mishra R. An analysis of factors influencing omnichannel retailing adoption using ism-dematel approach: An Indian perspective. Int J Retail Distrib Manage 2021; 49: 550–576. [Google Scholar]
- 68.Mousavizade F, Shakibazad M. Identifying and ranking CSFs for KM implementation in urban water and sewage companies using ISM-DEMATEL technique. J Knowl Manag 2019; 23: 200–218. [Google Scholar]
- 69.Pandey P, Agrawal N, Saharan T. et al. Impact of human resource management practices on TQM: An ISM-DEMATEL approach. The TQM Journal 2022; 34: 199–228. [Google Scholar]
- 70.Qin M, Wang X, Du Y. Factors affecting marine ranching risk in China and their hierarchical relationships based on dematel, ism, and bn. Aquaculture 2022; 549: 737802. [Google Scholar]
- 71.Rajput S, Singh SP. Identifying industry 4.0 IoT enablers by integrated PCA-ISM-DEMATEL approach. Manage Decis 2019; 57: 1784–1817. [Google Scholar]
- 72.Shakeri H, Khalilzadeh M. Analysis of factors affecting project communications with a hybrid dematel-ism approach (a case study in Iran). Heliyon 2020; 6: e04430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Singh R, Bhanot N. An integrated dematel-mmde-ism based approach for analysing the barriers of iot implementation in the manufacturing industry. Int J Prod Res 2020; 58: 2454–2476. [Google Scholar]
- 74.Trivedi A, Jakhar SK, Sinha D. Analyzing barriers to inland waterways as a sustainable transportation mode in India: A dematel-ism-based approach. J Clean Prod 2021; 295: 126301. [Google Scholar]
- 75.Wang L, Cao Q, Zhou L. Research on the influencing factors in coal mine production safety based on the combination of dematel and ism. Saf Sci 2018; 103: 51–61. [Google Scholar]
- 76.Xiahou X, Wu Y, Duan T. et al. Analyzing critical factors for the smart construction site development: A dematel-ism-based approach. Buildings 2022; 12: 116. [Google Scholar]
- 77.Yadav S, Luthra S, Garg D. Internet of things (IoT) based coordination system in agri-food supply Chain: Development of an efficient framework using DEMATEL-ISM. Oper Manage Res 2022; 15: 1–27. [Google Scholar]
- 78.Arora K, Siddiqui AA. Resource capabilities and sustainable export performance: An application of m-tism for indian manufacturing msmes. Qual Manag J 2022; 29: 125–144. [Google Scholar]
- 79.Dogra N, Adil M. Identifying indicators of sustainable smart agriculture driven by big data using modified total interpretive structural modeling (mtism). In Innovations in Cyber Physical Systems. Innovations in Cyber Physical Systems, Springer, 2021. pp. 505–512.
- 80.Dwivedi A, Paul SK. A framework for digital supply chains in the era of circular economy: Implications on environmental sustainability. Bus Strateg Environ 2022; 31: 1249–1274. [Google Scholar]
- 81.Meena A, Dhir S, Sushil. An analysis of growth-accelerating factors for the indian automotive industry using modified TISM. International Journal of Productivity and Performance Management 2021; 70: 1361–1392. [Google Scholar]
- 82.Patil A, Madaan J, Chan FT. et al. Advancement of performance measurement system in the humanitarian supply chain. Expert Syst Appl 2022; 206: 117844. [Google Scholar]
- 83.Priyadarshini J, Singh RK, Mishra R. et al. Investigating the interaction of factors for implementing additive manufacturing to build an antifragile supply chain: Tism-micmac approach. Oper Manage Res 2022; 15: 567–588. [Google Scholar]
- 84.Rajan R, Dhir S. Technology management for innovation in organizations: An argumentation-based modified TISM approach. Benchmarking: Int J 2021; 28: 1959–1986. [Google Scholar]
- 85.Rajan R, Dhir S. Determinants of alliance productivity and performance: Evidence from the automobile industry. Int J Prod Perform Manage 2021. ahead-of-print. DOI: 10.1108/IJPPM-02-2020-0079. [DOI] [Google Scholar]
- 86.Rajan R, Rana NP, Parameswar N. et al. Developing a modified total interpretive structural model (m-tism) for organizational strategic cybersecurity management. Technol Forecast Soc Change 2021; 170: 120872. [Google Scholar]
- 87.Sharma K, Jain M, Dhir S. Analysing the impact of artificial intelligence on the competitiveness of tourism firms: A modified total interpretive structural modeling (m-TISM) approach. Int J Emerging Mark 2022; 17: 1067–1084. [Google Scholar]
- 88.Sindhwani R, Behl A, Sharma A. et al. What makes micro, small, and medium enterprises not adopt logistics 4.0? a systematic and structured approach using modified-total interpretive structural modelling. Int J Logist Res Appl 2022; 0: 1–26. [Google Scholar]
- 89.Sindhwani R, Hasteer N, Behl A. et al. Exploring “what, ” “why” and “how” of resilience in msme sector: A m-tism approach. Benchmarking: Int J 2022. ahead-of-print. DOI: 10.1108/BIJ-11-2021-0682. [DOI] [Google Scholar]
- 90.Sindhwani R, Kumar R, Behl A. et al. Modelling enablers of efficiency and sustainability of healthcare: A m-tism approach. Benchmarking: Int J 2021; 29: 767–792. [Google Scholar]
- 91.Singh S, Dhir S. Modified total interpretive structural modelling of innovation implementation antecedents. Int J Prod Perform Manage 2022; 71: 1515–1536. [Google Scholar]
- 92.Singh S, Sinha S, Das VM. et al. A framework for linking entrepreneurial ecosystem with institutional factors: A modified total interpretive structural modelling approach. J Global Bus Advancement 2019; 12: 382–404. [Google Scholar]
- 93.Yadav A, Sagar M. Modified total interpretive structural modeling of marketing flexibility factors for indian telecommunications service providers. Global J Flex Syst Manage 2021; 22: 307–330. [Google Scholar]