Abstract
Background
The optimization of surgical procedures and the management of surgical quality and safety have become the focus of attention of hospital managers. The application of multimodal identification technology in the innovative management mode of hospital operating department has made remarkable progress.
Methods
To investigate the effect of the upgraded multimodal identification technology on the innovative management of the operating department, 2,280 cases of laparoscopic surgery using traditional surgical management procedures from January to December 2019 before the management upgrade were set as the control group, and 2,350 laparoscopic surgeries with the upgraded multimodal identification management process from January to December 2020 were selected as the experimental group. The operating efficiency, material management efficiency, and patient experience and satisfaction of the two groups were investigated and compared.
Results
Compared with traditional procedures, the upgraded multimodal surgical management system significantly improves the efficiency of laparoscopic surgery and reduces surgical consumption and costs. In addition, the multimodal surgical information identification system significantly improves the surgical experience for patients undergoing laparoscopic surgery.
Conclusion
Application of multimodal identification technology improves the innovative management of operation department compared with traditional surgery management procedure.
Keywords: laparoscopic surgery, operation department, multimodal identification technology, operating efficiency, frequency
Introduction
Operating room management is a complex subject (1). The optimization of surgical procedures and the management of surgical quality and safety have become the focus of attention of hospital managers around the world (2, 3). As a public service platform for hospital surgery, the operating department is the core of the surgical management process (4). The management process of the operating department, the behavior of surgical staff, the quality of material supply, and the operational efficiency all affect the quality and safety of surgical patients and their medical experience to varying degrees (5, 6).
The multi-modal surgical information identification system builds an intelligent management platform for the operating department (7). The surgical department of our hospital has upgraded the traditional operating room management system to a multi-modal surgical information identification system since 2020. Our multi-modal surgical information identification system establishes a data connection with the hospital management information system, realizes real-time information update and ensures that all patient information is true and accurate (8). The multi-modal surgical information identification system can also reduce manual operations as much as possible through operations such as staff card swiping, mobile application scanning code identification, and system-side appointments, so as to minimize human interference factors and ensure the standardization, efficiency and safety of the entire surgical process information.
With the rapid development of medical technology, laparoscopic surgery has been widely used in the treatment of general surgery patients (9, 10). Laparoscopic surgery has the advantages of small incision, less blood loss and quick recovery (11, 12). However, various complications of laparoscopic surgery, such as postoperative infection, bleeding, nausea and vomiting, and shock, will affect the patient's physical recovery (13). Therefore, formulating an effective procedure and nursing management process is a necessary means to reduce the waiting time of patients, improve the efficiency of laparoscopic surgery, and accelerate the recovery of patients (14, 15).
In this study, we hypothesized that our upgraded multi-model information management technology can effectively prompt laparoscopic surgery efficiency and reduce consumables consumption compared with our previous traditional surgical management. Our research aims to solve the problems in actual hospital management by comparing the traditional operation turnover process and the innovative management mode of multi-information identification technology, and improve the patient's surgical experience, reduce the cost of laparoscopic surgery, and reduce the occurrence of negative events in the operation.
Methods
Study design
The First Hospital of Qinhuangdao City began to upgrade the multimodal recognition technology in January 2020 to carry out innovative management of surgical departments. To investigate the effect of our upgraded multimodal identification technology in the innovative management operation department on laparoscopic surgery efficiency, surgical cost, and patient experience compared with our previous traditional management procedure, we conducted a cohort of laparoscopic surgeries. 2,280 cases of laparoscopic surgery using traditional surgical management procedures from January to December 2019 were set as the control group, and 2,350 laparoscopic surgeries from January to December 2020 with an information-based management process were selected as the experimental group. The sampling method of this study was cluster sampling. The control group was the traditional process group, and the experimental group was the multimodal practice group. The study was approved by the ethics committee of the First Hospital of Qinhuandao.
Participant recruitment
Patient inclusion criteria: (1) hospitalized patients (2) patients who were transported to and from field staff (3) surgical patients requiring laparoscopic equipment. Participants were divided into traditional process groups and multimodal practice groups. The multimodal practice group is based on the entire operation process, and designs an intelligent information recognition system for the problems existing in weak links and key points, so that the information-based process can be compared with the traditional manual management mode for research. All participants have signed informed consent.
Surgery management procedure
The multimodal surgical information recognition system is a part of the operating room information management. The information systems used in this study were already available and directly used. The multimodal surgical information recognition system establishes a data connection with the hospital management information system to create an intelligent management platform for the operating department and realize real-time information update. The specific content of the multi-modal surgical information recognition system includes staff card swiping, mobile phone application scanning code recognition, system-side appointments, reduced personnel operations, and reduced human interference factors (16).
Traditional group (control group): The traditional group uses traditional manual surgery management, including manual ordering before surgery, taking patients from the ward to the operating department, and then connecting to the operating room, manual arrangement of surgical laparoscopic equipment, and no nodes for the circulation and use of surgical equipment. After the patients were returned to the ward after surgery, the researchers collected data from multiple links and manually analyzed the relevant factors that restricted efficiency (17).
Multi-model group: Patients in the Multi-model group were managed by a multimodal surgical information recognition system. The multimodal surgical information recognition system adopts information technology for surgical management, and designs intelligent information processes, including task release process, task acceptance process, data statistics module, and function setting module (18). Before and after the operation, the nurses of the operating department use the mobile phone application to make an appointment to dispatch the order to the ward to pick up the patient. Field nurses start performing tasks by taking orders on the surgical line. The target time has been designed by the system prior to surgery, and the reasons for exceeding the time will be collected. When a patient is connected to the operating department, the order is deemed complete, and the computer in the background automatically aggregates the data. Laparoscopic devices are set up to share modules. Surgical instruments are positioned by scanning codes. Laparoscope usage times are accurately calculated and staggered. Data collection is carried out in multiple links, and the data is automatically analyzed in the background.
The time and human constraints of all setting links before, during, and after surgery were monitored, and data was collected and analyzed by the operation management department.
Statistical analysis
Frequency or percentage was used to show the categorical variables. Mean and standard deviation were used for the presentation of continuous variables. Statistical analysis in this research was performed by student test and one-way ANOVA test with mean ± SD or SEM. p < 0.05 was considered as statistical difference.
Results
Demographics characteristics
The baseline data in the surgical department between 2,280 surgical patients in traditional procedure group and 2,350 surgical patients in multimodal practice group are presented in Table 1. As shown in Table 1, there is no statistical difference of the characteristics including gender, age, and primary diseases (p > 0.05).
Table 1.
Demographic and clinical characteristics of patients under traditional process group and multimodal practice group.
| Characteristics | Study group |
p | |
|---|---|---|---|
| Tradition (n = 2,280) | Multi-model (n = 2,350) | ||
| Gender | |||
| Male | 1,245 (54.6%) | 1,247 (53.1%) | 0.302 |
| Female | 1,035 (45.4%) | 1,103 (46.9%) | |
| Age (years) | 50.6 ± 15.2 | 51.9 ± 16.7 | 0.137 |
| Primary disease | |||
| Hepatobiliary surgery | 673 (29.5%) | 625 (26.6%) | 0.082 |
| Gynecological operation | 248 (10.9%) | 286 (12.2%) | |
| Gastrointestinal surgery | 846 (37.1%) | 911 (38.8%) | |
| Urologic surgery | 485 (21.3%) | 487 (20.7%) | |
| Others | 28 (1.2%) | 41 (1.7%) | |
Values were expressed as n (percentage, %) or mean ± SD. p values for each group were derived from Mann–Whitney test. Chi-square test or Fisher's exact test was used for assessing distribution of observations or phenomena between two groups.
Clinical characteristics of operation departments
The indexes in operation department under traditional process group and multimodal practice group are shown in Table 2. The number of first operations and consecutive operations, the number of sterile items, the number of packages of high-value consumables, the number of pieces of clothing consumed, the number of specimens submitted for inspection, and the number of bags of transfused blood products between the two groups were counted and analyzed.
Table 2.
Clinical characteristics of operation department under traditional process group and multimodal practice group.
| Characteristics | Study group |
|
|---|---|---|
| Tradition (n = 2,280) | Multi-model (n = 2,350) | |
| Operation room (no.) | 21 | 21 |
| The first operation | 251 | 248 |
| The continuous operations | 2,029 | 2,102 |
| Sterile medical device (bag) | 6,787 | 7,093 |
| High-value consumable (unit) | 905 | 895 |
| Clothing consumption (unit) | 2,737 | 2,518 |
| Clinical samples (no.) | 1,217 | 1,395 |
| Blood product (bag) | 551 | 496 |
Operating efficiency of operating room
Evaluation of operating efficiency of operating room between traditional process group and multimodal practice group is shown in Table 3. Among the 251 cases in the control group, 198 cases were on time, and the rate of on-time operation was 78.9%; in the multimodal practice group, 229 cases were on time, and the rate of on-time operation was 92.3%. There was a significant difference in the rate of on-time operation between the two groups. The waiting times for consecutive surgeries were compared between the two groups. The multimodal practice group had significantly shorter waiting times for consecutive surgeries relative to the traditional group. In addition, the mean operative time for all procedures was significantly shorter in the multimodal practice group relative to the traditional group.
Table 3.
Evaluation of operating efficiency of operating room between traditional process group and multimodal practice group.
| Characteristics | Study group |
p | |
|---|---|---|---|
| Tradition (n = 2,280) | Multi-model (n = 2,350) | ||
| Punctually cut skin rate (the first operation) | 198/251 (78.9%) | 229/248 (92.3%) | <0.001 |
| Waiting time (min) (the continuous operations) | 58.6 ± 12.2 | 37.9 ± 13.7 | <0.001 |
| Operation time (min) | 136.8 ± 31.2 | 112.5 ± 28.3 | <0.001 |
Values were expressed as n (percentage, %) or mean ± SD. p values for each group were derived from Mann–Whitney test. Fisher's exact test was used for assessing distribution of observations or phenomena between two groups.
Material management efficiency
Evaluation of material management efficiency between traditional process group and multimodal practice group is presented in Table 4. There is a statistical difference between the two groups in the billing omission rate of high-value consumables. The multimodal practice group also significantly improved the quality tracking of sterile items used in surgery, such as instruments, consumables, etc. The wear of clothing accessories and other materials was significantly reduced in the multimodal practice group.
Table 4.
Evaluation of material management efficiency between traditional process group and multimodal practice group.
| Characteristics | Study group |
p | |
|---|---|---|---|
| Tradition (n = 2,280) | Multi-model (n = 2,350) | ||
| Missing accounts of high value consumables | 8 (0.35%) | 0 (0%) | 0.003 |
| Tracking of sterile items | 1,847 (81.0%) | 2,248 (95.7%) | <0.001 |
| Detrition of clothing | 286/2,737 (10.4%) | 124/2,518 (4.9%) | <0.001 |
Values were expressed as n (percentage, %). p values for each group were derived from Fisher's exact test.
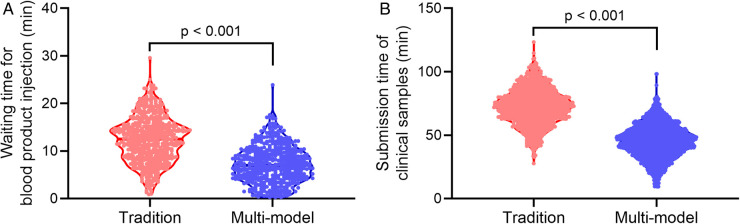
Comparison of waiting time for blood product injection and submission time of clinical samples
The time of blood product verification and specimen submission time of the two groups of surgical patients was compared between the two groups. As shown in Figure 1, the multimodal practice group was able to significantly reduce blood product verification time and specimen delivery time compared with the traditional group.
Figure 1.
Comparison of waiting time for blood product injection (A) and submission time of clinical samples (B) between traditional process group (tradition) and multimodal practice group (multi-model). Violin plot. Mann–Whitney test.
Patients’ satisfaction
Comparison of patients’ satisfaction between traditional process group and multimodal practice group was shown in Table 5. The patient experience and satisfaction were surveyed by the operating room nurses who performed the preoperative visit during the postoperative return visit (within 3 days after the operation), and the patients were asked about their satisfaction with the whole operation from admission to the operation and the nursing process after the operation. The multimodal practice group was able to significantly improve patient satisfaction.
Table 5.
Comparison of patients’ satisfaction between traditional process group and multimodal practice group.
| Characteristics | Study group |
p | |
|---|---|---|---|
| Tradition (n = 2,280) | Multi-model (n = 2,350) | ||
| Very satisfied | 708 (31.1%) | 974 (41.5%) | <0.001 |
| Satisfied | 964 (42.3%) | 893 (38%) | |
| Basically satisfied | 477 (20.9%) | 386 (16.4%) | |
| Not satisfied | 131 (5.7%) | 97 (4.1%) | |
Values were expressed as n (percentage, %). p values for each group were derived from Chi-square test.
Discussion
The optimization of surgical procedures and the management of surgical quality and safety have been the focus of current multinational hospital managers (19–21). Patient information and surgical consumables can be connected to the hospital's Internet platform for information exchange and communication, through radio frequency identification (RFID), two-dimensional codes, infrared sensors, laser scanners, mobile personal digital assistants and other information sensing devices (22, 23). The big data-based surgical management method can realize the intelligent identification, positioning, tracking, monitoring and management of single surgical equipment (24). The multimodal surgical information identification system integrates and interconnects the multi-source data and information island systems of various departments in the hospital, and builds the quality and safety information management system of the hospital operation department together with the management process of the operation department (25).
Our hospital has launched multimodal recognition technology to carry out innovative management of the surgical department since 2019. Our multimodal surgical information recognition system is a part of the operating room information management. The multimodal surgical information recognition system establishes a data connection with the hospital management information system to create an intelligent management platform for the operating department and realize real-time information update (26). The specific content of the multi-modal surgical information recognition system includes staff card swiping, mobile phone application scanning code recognition, system-side appointments, reduced personnel operations, and reduced human interference factors (27).
We believe that our multi-model identification system has important implications for improving the efficiency of clinical work. We hope to realize the evaluation of information accuracy through the application of the multimodal surgical information recognition system, thereby greatly reducing the time and labor cost. For instance, the quality of the preparation of laparoscopic surgery-related instruments directly affects the operation and the effect of the operation. Therefore, laparoscopic surgery should strengthen the management of the preparation of laparoscopic surgical instruments. In this study, we investigate the effect of application of multimodal identification technology in the innovative management operation department on laparoscopic surgery efficiency, surgical cost, and patient experience. Patients in our hospital were currently managed by a multimodal surgical information recognition system. The multimodal surgical information recognition system adopts information technology for surgical management, and designs intelligent information processes, including task release process, task acceptance process, data statistics module, and function setting module. Before and after the operation, the nurses of the operating department use the mobile phone application to make an appointment to dispatch the order to the ward to pick up the patient. Field nurses start performing tasks by taking orders on the surgical line. The target time has been designed by the system prior to surgery, and the reasons for exceeding the time will be collected. When a patient is connected to the operating department, the order is deemed complete, and the computer in the background automatically aggregates the data. Laparoscopic devices are set up to share modules. Surgical instruments are positioned by scanning codes. Laparoscope usage times are accurately calculated and staggered.
Conclusion
In conclusion, we demonstrate that application of multimodal identification technology in the innovative management operation department on laparoscopic surgery efficiency, surgical cost, and patient experience. Our findings show that the newly implemented multimodal surgical information recognition system in our hospital can significantly improve the operating efficiency of laparoscopic operating room compared to traditional surgery and nursing procedures. The multimodal surgical information recognition system can also significantly improve material management efficiency and reduce the wastage of surgical instruments in the laparoscopic operating room. We also demonstrated that the multimodal practice group was able to significantly reduce blood product verification time and specimen delivery time in surgical patients. In addition, patients who were managed by the multimodal surgical information recognition system had significantly lower waiting time for surgery, and their surgical experience was significantly improved. We hope that our study can provide new research evidence for the generalized use of multimodal surgical information recognition systems.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the First Hospital of Qinhuangdao. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YZ and YZ: conceptualization, methodology, writing—original draft preparation, investigation, methodology, writing—reviewing and editing. XS: software, validation. YH, LF and LL: visualization, data curation. YZ: conceptualization, writing—original draft preparation, supervision, writing—reviewing and editing. XS: conceptualization. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Lee DJ, Ding J, Guzzo TJ. Improving operating room efficiency. Curr Urol Rep. (2019) 20(6):28. 10.1007/s11934-019-0895-3 [DOI] [PubMed] [Google Scholar]
- 2.Moitra VK, Einav S, Thies KC, Nunnally ME, Gabrielli A, Maccioli GA, et al. Cardiac arrest in the operating room: resuscitation and management for the anesthesiologist: part 1. Anesth Analg. (2018) 126(3):876–88. 10.1213/ANE.0000000000002596 [DOI] [PubMed] [Google Scholar]
- 3.Allo MD, Tedesco M. Operating room management: operative suite considerations, infection control. Surg Clin North Am. (2005) 85(6):1291–7. 10.1016/j.suc.2005.09.001 [DOI] [PubMed] [Google Scholar]
- 4.Levine WC, Dunn PF. Optimizing operating room scheduling. Anesthesiol Clin. (2015) 33(4):697–711. 10.1016/j.anclin.2015.07.006 [DOI] [PubMed] [Google Scholar]
- 5.Tsai MH, Sanford JA, Black IH, Boggs SD, Urman RD. Operating room management at the edge of order and chaos. J Med Pract Manage. (2017) 32(4):250–5. [PubMed] [Google Scholar]
- 6.Marjamaa R, Vakkuri A, Kirvela O. Operating room management: why, how and by whom? Acta Anaesthesiol Scand. (2008) 52(5):596–600. 10.1111/j.1399-6576.2008.01618.x [DOI] [PubMed] [Google Scholar]
- 7.Glasser MF, Coalson TS, Robinson EC, Hacker CD, Harwell J, Yacoub E, et al. A multi-modal parcellation of human cerebral cortex. Nature. (2016) 536(7615):171–8. 10.1038/nature18933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rogers DA, Lingard L, Boehler ML, Espin S, Mellinger JD, Schindler N, et al. Surgeons managing conflict in the operating room: defining the educational need and identifying effective behaviors. Am J Surg. (2013) 205(2):125–30. 10.1016/j.amjsurg.2012.05.027 [DOI] [PubMed] [Google Scholar]
- 9.Wormser C, Runge JJ. Advances in laparoscopic surgery. Vet Clin North Am Small Anim Pract. (2016) 46(1):63–84. 10.1016/j.cvsm.2015.08.001 [DOI] [PubMed] [Google Scholar]
- 10.Cullinan DR, Schill MR, DeClue A, Salles A, Wise PE, Awad MM. Fundamentals of laparoscopic surgery: not only for senior residents. J Surg Educ. (2017) 74(6):e51–e4. 10.1016/j.jsurg.2017.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang L, Li TJ. Laparoscopic surgery for gastric cancer: where are we now and where are we going? Expert Rev Anticancer Ther. (2018) 18(11):1145–57. 10.1080/14737140.2018.1520098 [DOI] [PubMed] [Google Scholar]
- 12.Mari G, Scanziani R, Auricchio S, Crippa J, Maggioni D. Laparoscopic surgery in patients on peritoneal dialysis: a review of the literature. Surg Innov. (2017) 24(4):397–401. 10.1177/1553350617708723 [DOI] [PubMed] [Google Scholar]
- 13.Hata K, Kazama S, Nozawa H, Kawai K, Kiyomatsu T, Tanaka J, et al. Laparoscopic surgery for ulcerative colitis: a review of the literature. Surg Today. (2015) 45(8):933–8. 10.1007/s00595-014-1053-7 [DOI] [PubMed] [Google Scholar]
- 14.Lai JH, Law WL. Laparoscopic surgery for colorectal cancer. Br Med Bull. (2012) 104:61–89. 10.1093/bmb/lds026 [DOI] [PubMed] [Google Scholar]
- 15.Ferrufino F L, Cohen J V, Schaffner E B, Eulufi F C, Muller F P, Castillo J M, et al. Simulation in laparoscopic surgery. Cir Esp. (2015) 93(1):4–11. 10.1016/j.ciresp.2014.02.011 [DOI] [PubMed] [Google Scholar]
- 16.Manickam P, Mariappan SA, Murugesan SM, Hansda S, Kaushik A, Shinde R, et al. Artificial intelligence (AI) and internet of medical things (IoMT) assisted biomedical systems for intelligent healthcare. Biosensors. (2022) 12(8):562. 10.3390/bios12080562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper EA, Hodder RJ, Finlayson A, Filgate R, Coveney A, Balasuriya HD, et al. Cost analysis of a watch-and-wait approach in patients with a complete clinical response to chemoradiotherapy for rectal cancer. ANZ J Surg. (2022). 10.1111/ans.17914. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Loftus TJ, Shickel B, Balch JA, Tighe PJ, Abbott KL, Fazzone B, et al. Phenotype clustering in health care: a narrative review for clinicians. Front Artif Intell. (2022) 5:842306. 10.3389/frai.2022.842306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kong V, Cheung C, Ko J, Xu W, Bruce J, Liang G, et al. The management of penetrating neck injury with retained knife: 15-year experience from a major trauma center in South Africa. Am Surg. (2021):31348211065127. 10.1177/00031348211065127. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Shem Tov L, Ronel I, Matot I. Escort of older people into the operating room: a feasibility study. Int J Older People Nurs. (2021) 17(3):e12437. 10.1111/opn.12437 [DOI] [PubMed] [Google Scholar]
- 21.Abraham J, Meng A, Holzer KJ, Brawer L, Casarella A, Avidan M, et al. Exploring patient perspectives on telemedicine monitoring within the operating room. Int J Med Inform. (2021) 156:104595. 10.1016/j.ijmedinf.2021.104595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright KD, Kim J, Ratcliffe CRD, Walker KL, Sharpe D, Wilson S, et al. Pilot examination of the efficacy of the internet-delivered, preoperative, preparation program (I-PPP). J Clin Psychol Med Settings. (2021) 28(3):627–36. 10.1007/s10880-020-09754-0 [DOI] [PubMed] [Google Scholar]
- 23.Cefalu JN, Joshi TV, Spalitta MJ, Kadi CJ, Diaz JH, Eskander JP, et al. Methemoglobinemia in the operating room and intensive care unit: early recognition, pathophysiology, and management. Adv Ther. (2020) 37(5):1714–23. 10.1007/s12325-020-01282-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsai MH, Haddad DJ, Friend AF, Bender SP, Davidson ML. A web-based operating room management educational tool. A A Case Rep. (2016) 7(3):60–2. 10.1213/XAA.0000000000000343 [DOI] [PubMed] [Google Scholar]
- 25.Ushimaru Y, Takahashi T, Souma Y, Yanagimoto Y, Nagase H, Tanaka K, et al. Innovation in surgery/operating room driven by internet of things on medical devices. Surg Endosc. (2019) 33(10):3469–77. 10.1007/s00464-018-06651-4 [DOI] [PubMed] [Google Scholar]
- 26.Chen S, Huang J, Gao Z. Development of intelligent management system for high value consumable material in operating room. Zhongguo Yi Liao Qi Xie Za Zhi. (2021) 45(1):42–5. 10.3969/j.issn.1671-7104.2021.01.009 [DOI] [PubMed] [Google Scholar]
- 27.Wasilko SM, Giordano C. Operating room management and the business of anesthesia: innovative solutions to bridge the educational gap in residency training programs. A A Case Rep. (2017) 8(9):246. 10.1213/XAA.0000000000000475 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.